Percutaneous-assisted laparoscopic bilateral salpingo-oophorectomy in BRCA-mutated patients: a retrospective comparative study
-
Benito Chiofalo
, Sara Boccassi
Abstract
Objectives
Prophylactic salpingo-oophorectomy in BRCA-mutated patients reduces the risk of breast and ovarian cancer. This study aimed to compare peri-operative outcomes of BRCA-mutated patients who underwent prophylactic salpingo-oophorectomy via traditional laparoscopy or percutaneous assisted laparoscopy.
Methods
In this single-center retrospective cohort study, BRCA-mutated patients submitted to laparoscopic prophylactic bilateral salpingo-oophorectomy were enrolled. We compared traditional laparoscopy and percutaneous-assisted laparoscopy, which was performed using the Percuvance grasp.
Results
We enrolled 59 patients submitted to prophylactic salpingo-oophorectomy from September 2017 to September 2022. Thirty-nine underwent a conventional laparoscopic procedure (LPS) and 20 a percutaneous-assisted laparoscopy (PERC). Similar clinical characteristics were found in the two groups, furthermore, no differences were noticed in terms of peri-operative complication, intraoperative blood loss (p=0.7), and hospital stay (p=0.6). A significantly lower post-operative pain, using VAS score, was noticed in the PERC group compared with the LPS group, on both the first and second days after surgery. Moreover, better cosmetic results have been highlighted in the PERC group.
Conclusions
Percutaneous-assisted laparoscopy seems an effective and safe procedure for laparoscopic prophylactic adnexectomy in BRCA-mutated patients. Furthermore, the percutaneous procedure showed better aesthetic outcomes and reduced post-operative pain, compared to traditional laparoscopy.
Introduction
BRCA1 and 2 mutations are an autosomal-dominant inherited trait predisposing women to breast and ovarian cancer, with a 75 and 40 % lifetime risk of developing cancer respectively if compared to the BRCA wild-type gene [1], [2], [3]. The role of BRCA gene mutations as a prognostic factor is controversial. Some studies support the theory that BRCA-related breast cancer has a better prognosis compared to other cancer types, while, others suggest the opposite [3], 4].
Considering the high risk of developing ovarian and breast cancer for BRCA-mutated patients, it is appropriate to introduce prevention options for patients. Regarding ovarian cancer, primary prevention, for BRCA-mutated patients, although radical, is represented by surgery. Prophylactic bilateral salpingo-oophorectomy (BSO) is the gold standard.
International guidelines recommend prophylactic BSO as the most effective method for lowering the risk of breast and ovarian cancer in women with BRCA mutations. Esteemed organizations, including the NCCN (National Comprehensive Cancer Network), ESMO (European Society for Medical Oncology), and ASCO (American Society of Clinical Oncology), support this approach as a standard risk-reduction measure [5], 6]. Prophylactic salpingo-oophorectomy is generally recommended for women with a BRCA1 mutation between the ages of 35 and 40, and for those with a BRCA2 mutation between 40 and 45, or after they have completed their reproductive plans. This procedure reduces the risk of ovarian cancer by up to 96 % and the risk of breast cancer by up to 56 %.
Genetic and psychological counseling are crucial before surgery, particularly for women of reproductive age, as ovary removal leads to early surgical menopause, significantly impacting bone health, cardiovascular health, and overall quality of life [7]. Today, BSO is usually performed with a minimally invasive approach, using laparoscopy. Indeed, many clinical findings regarding surgical approaches (laparoscopy vs. laparotomy) support the use of minimally invasive surgery [8]. Percutaneous instruments are one of the evolutions of minimally invasive surgery. They have a smaller diameter than laparoscopic standard instruments and don’t require the use of a laparoscopic trocar.
Many previous reports support the use of percutaneous instruments in laparoscopic gynecologic surgery [9], [10], [11], [12], [13], [14]. Hence, the purpose of the study was to test the use of percutaneous-assisted laparoscopy in prophylactic salpingo-oophorectomy in a cohort of BRCA-mutated patients.
Materials and methods
Study design
This single-center retrospective, cohort study was carried out in the National Cancer Institute of Rome “Regina Elena”, following the STROBE guideline (Supplementary material 1). The Institutional Review Board of the Regina Elena National Cancer Institute in Rome approved the study (CE RS1847/23(3726)). The study’s design, data analysis, interpretation, writing, and revisions adhered to the principles outlined in the Helsinki Declaration, the Committee on Publication Ethics guidelines (http://publicationethics.org/), and the statements on reporting studies using routinely collected observational health data [15], which are available through the Enhancing the Quality and Transparency of Health Research Network (www.equator-network.org/). There was no advertising, and patients were not offered any remuneration. Each patient was informed about the study’s objectives and procedures and provided written consent for research purposes.
Inclusion criteria were: age>18 years, a confirmed pathological mutation of BRCA1 or BRCA2 genes, after genetic and oncologic counseling has chosen to undergo prophylactic BSO, from September 2017 to September 2022 at the Gynecologic Oncology Unit of the “Regina Elena” hospital, National Cancer Institute of Rome. We included all women who underwent the procedure using either conventional laparoscopy or laparoscopy with percutaneous forceps grasping. All the surgeries were performed by gynecologists who specialized in minimally invasive surgery. To avoid biases, patients submitted to other concurrent surgical procedures and any kind of surgical accesses different from the aforementioned were excluded.
The choice of how to perform the procedure was not dependent on surgeons’ or patients’ preferences. We started to use percutaneous instruments in 2019, before this period all procedures were performed with traditional laparoscopy, on the contrary from 2019 we performed almost all procedures with the percutaneous grasp.
Treatments
Patients were associated with the LPS group (traditional laparoscopy) or the PERC group (percutaneous-assisted laparoscopy), depending on the type of surgery to which they had been subjected. As standard practice, salpingo-oophorectomy via conventional laparoscopy was performed using three laparoscopic trocars: a 10-mm trocar in the umbilical region, a 5-mm suprapubic trocar, and another 5-mm trocar positioned in the left iliac area. Conventional laparoscopic instruments, including traumatic and non-traumatic graspers, scissors, and bipolar forceps, were utilized.
For the percutaneous-assisted laparoscopy, a percutaneous grasping forceps was placed in the left iliac region, in place of a 5 mm trocar. The percutaneous grasping forceps feature a sharp tip when closed, enabling insertion through the skin without requiring a scalpel. Once inside the abdomen, the instrument deploys a grasping mechanism, making it ready for use (MiniLap percutaneous surgical system, Teleflex Inc., USA) (Figure 1).
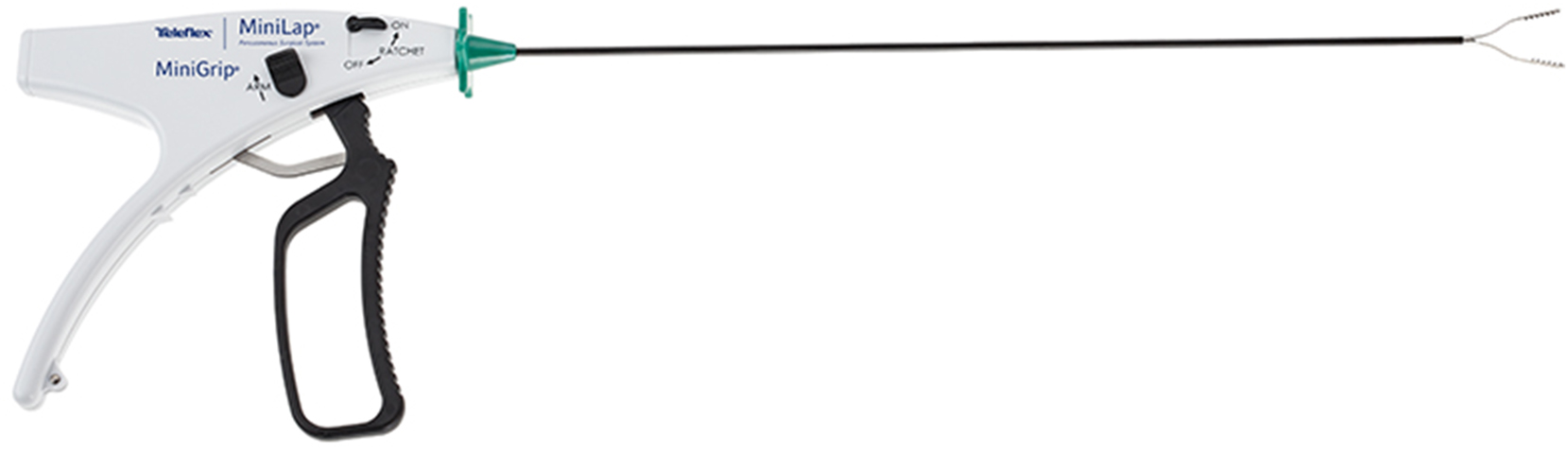
The percutaneous grasp used for bilateral salpingo-oophorectomy. MiniLap® percutaneous surgical system, Teleflex Inc., USA.
All patients underwent a preoperative interview, where the surgical technique was fully exposed, and written consent was signed by the patient and the surgeon. Regardless of the type of procedure, in all patients, a peritoneal washing for cytological examination was performed prior to prophylactic salpingo-oophorectomy.
Patients’ evaluation
We evaluated clinical and surgical data in both groups, including age, body mass index (BMI), BRCA mutation, previous breast cancer, previous abdominal surgeries, intraoperative blood loss amount, and operative times. Perioperative complications were classified according to the Clavien-Dindo classification [16]. Post-operatively we evaluated: days of hospitalization and aesthetic outcomes. The level of pain was measured using a 0–10 visual analog scale (VAS) on the day of surgery (within the first four postoperative hours) and again on the first and the second postoperative days (at 24 and 48 h respectively). During follow-up at two months, aesthetic outcomes were evaluated by asking all patients to rate their personal satisfaction on a scale from 0 to 10.
Statistical analysis
Descriptive statistics were calculated for all the variables of interest: specifically, we reported the continuous variables with their means and standard deviations (±SD) and the categorical variables with absolute and percentage frequencies. We performed the Kolmogorov-Smirnov normality test for all continuous variables. To compare the continuous variables, we used the Mann-Whitney test whereas we applied the Chi-Square test to compare the categorical variables. We considered as statistically significant a p-value<0.05. All statistical analyses were performed with the aid of SPSS version 21 statistical software (IBM Corp., NY, USA).
Results
We enrolled a total of 59 patients who underwent surgery from September 2017 to September 2022. Thirty-nine underwent a traditional laparoscopic procedure (LPS) and 20 a percutaneous-assisted laparoscopy (PERC). The mean age was less than 60 years old and it was similar in the two groups (51.6 ± 9.7 in LAP vs. 49.2 ± 9.0 in PERC); no significant differences in BMI were found, with a mean BMI less than 30 (24.8 ± 5.8 LPS vs. 23.3 ± 3.6 PERC) (Table 1).
Clinical and peri-operative data.
| LPS (total number=39), mean ± SD | PERC (total number=20), mean ± SD | p-Value (Mann-Whitney test) (p < 0.05) | |
|---|---|---|---|
| Age | 51.6 ± 9.7 | 49.2 ± 9.0 | 0.414 |
| BMI | 24.8 ± 5.8 | 23.3 ± 3.6 | 0.461 |
| VAS G0 | 1.0 ± 0.8 | 1.1 ± 0.6 | 0.493 |
| VAS G1 | 1.1 ± 0.9 | 0.5 ± 0.5 | 0.006 |
| VAS G2 | 0.8 ± 0.6 | 0.3 ± 0.4 | 0.002 |
| Aesthetic results | 8.3 ± 1.6 | 9.5 ± 1.0 | <0.001 |
| Operative time | 35.5 ± 11.2 | 34.6 ± 11.1 | 0.698 |
| Intraoperative blood loss | 5.4 ± 1.3 | 5.2 ± 1.1 | 0.699 |
| Hospital stay | 2.3 ± 0.8 | 2.1 ± 0.5 | 0.553 |
-
LPS, traditional laparoscopy; PERC, percutaneous assisted laparoscopy; SD, standard deviation.
All the patients underwent BSO for BRCA mutation (35 BRCA1 and 24 BRCA2) and some of these patients had previous breast cancer in their personal anamnesis. We enrolled 21 BRCA1 mutated patients and 18 BRCA2 in the LPS group, 14 BRCA1 mutated patients, and 6 BRCA2 in the PERC group (Table 2).
Distribution of BRCA mutations, previous abdominal surgery, previous breast cancer in the two groups, and use of analgesic drugs during the first post-operative day.
| LPS (total number=39), n (%) | PERC (total number=20), n (%) | p-Value (Chi-Square test) (p < 0.05) | |
|---|---|---|---|
| BRCA genes | |||
| BRCA1 | 21 (53.8) | 14 (70.0) | 0.232 |
| BRCA2 | 18 (46.2) | 6 (30.0) | |
| Previous abdominal surgery | 19 (48.7) | 13 (65) | 0.235 |
| Previous breast cancer | 24 (61.5) | 13 (65) | 0.533 |
| Use of analgesic drug on day 1 | 10 (25.6) | 4 (20) | 0.232 |
We usually administer analgesic opioids immediately after surgery (tramadol 100 mg) and then we administer 1 g of paracetamol at the patient’s request. No differences were found in terms of the use of analgesic drugs on the first post-operative day between the two groups (Table 2).
No significant differences were found in the two groups in terms of operative time, intra-operative blood loss, and hospital stay (mean hospital stay of two days) (Table 1). No significant differences between the two groups were found in VAS scores at the end of surgery. However, there was a significant difference in further two postoperative days (first post-operative day 1.1 ± 0.9 LPS vs. 0.5 ± 0.5 PERC; p=0.006, second post-operative day 0.8 ± 0.6 LPS vs. 0.3 ± 0.4; p=0.002). Both groups reported good cosmetic results with median personal satisfaction >8, however, it was significantly higher with the PERC approach (LPS 8.3 ± 1.6 vs. PERC 9.5 ± 1.0; p<0.001) (Table 1, Figure 2).
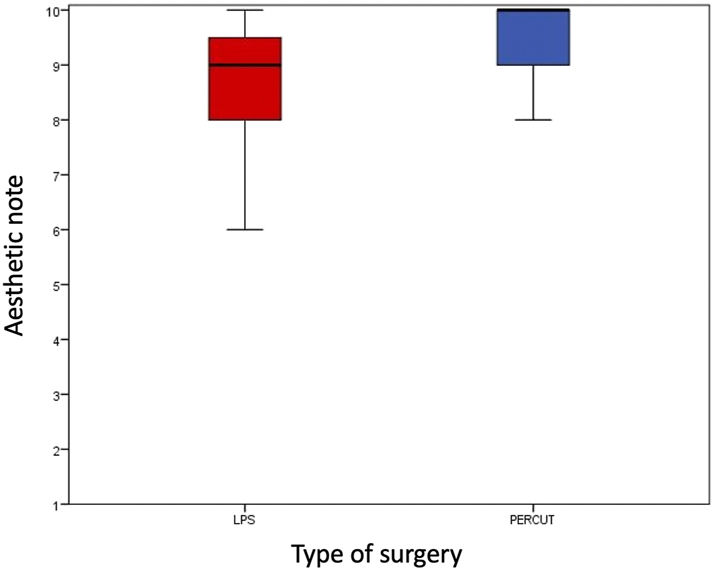
Aesthetic outcomes, comparison between traditional laparoscopy and the percutaneous assisted approach. A Mann-Whitney test was conducted for multiple comparisons analysis.
Discussion
The future of gynecological surgery is to reduce more and more invasiveness. This is particularly significant for prophylactic surgery and can be possible thanks to the use of smaller and more advanced instruments compared with the past. As reported in one of our previous studies, the use of percutaneous instruments reduces postoperative pain compared to the conventional laparoscopic approach in oncologic patients undergoing ovarian tissue explantation for fertility preservation. Additionally, it enhances aesthetic outcomes [10]. The BRCA mutation increases women the risk of developing ovarian and breast cancer, compared with the general female population. To reduce this oncological risk, it is recommended to submit women to prophylactic surgery (salpingo-oophorectomy ∓ mastectomy) at the age of 35 or 45 years respectively for BRCA1 and BRCA2 mutation [17]. This prophylactic surgery reduces cancer risk, but may negatively impact patients’ quality of life, with all the possible effects related to menopause, and even more can compromise the psychological state, reducing self-confidence [18], 19].
According to our data, post-operative pain, measured by VAS score, in the PERC group has a rapid and progressive decrease. Salpingo-oophorectomy with percutaneous instruments seems to be less painful than conventional laparoscopy, particularly 24 and 48 h after the intervention. Post-operative pain reduction is particularly relevant in these patients who underwent surgery for prophylactic reasons.
Another important point to analyze in these patients is the cosmetic result. Actually, laparoscopic scars, caused by trocars even if are small, are visible and unpleasant, especially in patients susceptible to keloid [20]. Minimizing the use of trocars and the use of percutaneous instruments reduces the number of scars in the abdomen thanks to a smaller diameter (2.4 mm) and to the possibility of introducing instruments directly, without the use of further trocars.
No complications were observed in either group, confirming that percutaneous-assisted laparoscopy is as safe and effective as conventional laparoscopy for BSO, with no significant differences in blood loss or hospital stay duration. The operative times were not statistically different in the two groups, even though a small gap was registered in favor of the PERC group, probably because there is one less trocar to introduce in the abdomen.
In recent years, minimally invasive surgery has replaced classic laparotomy in many fields of gynecological surgery, where it is preferred. The laparoscopic approach for adnexectomy has faster operating time, fewer complications, safety, efficiency, and effectiveness. Reduced hospitalization in patients submitted to laparoscopy resulted in an optimal cost-benefit ratio, with shorter convalescence and earlier return to normal activities and employment, with respect to classic laparotomic surgery [8]. In recent years, numerous studies have been published regarding the laparoscopic percutaneous technique in the treatment of several benignant and oncologic diseases, with the aim of minimizing invasiveness, therefore the percutaneous approach responds to this logic, reducing skin incisions and obtaining better post-operative outcomes [9], [10], [11], [12], [13], [14]. Percutaneous-assisted laparoscopy demonstrated advantages over other ultra-minimally invasive techniques, such as single-site laparoscopy, by reducing postoperative pain, lowering the risk of umbilical hernias, and providing better cosmetic outcomes. Moreover, the single-site approach appears to have a steeper learning curve [12], 21]. Furthermore, there is a lack of evidence regarding the comparison between transvaginal natural orifice transluminal endoscopic surgery (vNOTES) and percutaneous assisted laparoscopy for prophylactic surgery in BRCA mutated women.
Reducing invasiveness in this type of surgery, through the routine use of percutaneous instruments, may help decrease post-operative pain in patients submitted to prophylactic salpingo-oophorectomy. Additionally, by enhancing aesthetic results, it would improve compliance with prophylactic surgery and the well-being of this particular group of patients.
Based on our experience, the use of percutaneous instruments requires only a single demonstration for surgeons experienced in laparoscopy. We started to use the percutaneous grasp in BRCA-mutated patients, as it is a simple surgical procedure, so it required a very short learning curve. Regarding cost analysis, the price of the percutaneous grasp is very similar to that of a disposable trocar. Also, when compared to robotic surgery, the percutaneous approach is much cheaper. For the above reasons, this seems a repeatable procedure even in peripheral and less specialized centers.
The retrospective design is the major limit of the study, prospective well-designed trials are expected to validate or disprove our findings and to assess the true impact of percutaneous procedures on this selected group. The small sample and the lack of long-term follow-up are other important limits. Comparative studies with other ultra-minimally invasive approaches are expected, to choose the best surgical approach for prophylactic BSO in BRCA carriers [22].
Conclusions
When compared to traditional laparoscopy, percutaneous-assisted laparoscopy seems an effective, safe, and painless procedure for prophylactic salpingo-oophorectomy in BRCA-mutated patients, and offers excellent post-operative aesthetic results. Further and well-designed studies are desired, to encourage this procedure in these selected groups of patients.
-
Research ethics: All procedures conducted in studies involving human participants complied with the ethical standards of the institutional and/or national research committee, as well as the 1964 Helsinki Declaration and its subsequent amendments or equivalent ethical guidelines. The study received approval from the Institutional Review Board of the Regina Elena National Cancer Institute of Rome (CE RS1847/23(3726)) on March 28, 2023.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission. Conceptualization, writing – original draft preparation, Benito Chiofalo; data curation, Sara Boccassi, Giuseppe Scibilia; formal analysis, Valentina Bruno; writing – review and editing, Mario Russo, Paolo Scollo; Methodology, Basilio Pecorino; supervision, Enrico Vizza, Paolo Scollo.
-
Use of LLM, AI and MLT: None declared.
-
Conflict of interest: The author states no conflict of interest.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Hall, JM, Lee, MK, Newman, B, Morrow, JE, Anderson, LA, Huey, B, et al.. Linkage of early-onset familial breast cancer to chromosome 17q21. Science 1990;250:1684–9. https://doi.org/10.1126/science.2270482.Suche in Google Scholar PubMed
2. Antoniou, A, Pharoah, PD, Narod, S, Risch, HA, Eyfjord, JE, Hopper, JL, et al.. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003;72:1117–30. https://doi.org/10.1086/375033.Suche in Google Scholar PubMed PubMed Central
3. Cortesi, L, Masini, C, Cirilli, C, Medici, V, Marchi, I, Cavazzini, G, et al.. Favourable ten-year overall survival in a Caucasian population with high probability of hereditary breast cancer. BMC Cancer 2010;10:90. https://doi.org/10.1186/1471-2407-10-90.Suche in Google Scholar PubMed PubMed Central
4. Maksimenko, J, Irmejs, A, Nakazawa-Miklasevica, M, Melbarde-Gorkusa, I, Trofimovics, G, Gardovskis, J, et al.. Prognostic role of mutation in patients with triple-negative breast cancer. Oncol Lett 2014;7:278–84. https://doi.org/10.3892/ol.2013.1684.Suche in Google Scholar PubMed PubMed Central
5. Liu, YL, Breen, K, Catchings, A, Ranganathan, M, Latham, A, Goldfrank, DJ, et al.. Risk-reducing bilateral salpingo-oophorectomy for ovarian cancer: a review and clinical guide for hereditary predisposition genes. JCO Oncol Pract 2022;18:201–9. https://doi.org/10.1200/op.21.00382.Suche in Google Scholar PubMed PubMed Central
6. Bradbury, AR, Ibe, CN, Dignam, JJ, Cummings, SA, Verp, M, White, MA, et al.. Uptake and timing of bilateral prophylactic salpingo-oophorectomy among BRCA1 and BRCA2 mutation carriers. Genet Med 2008;10:161–6. https://doi.org/10.1097/gim.0b013e318163487d.Suche in Google Scholar PubMed PubMed Central
7. Zilski, N, Speiser, D, Bartley, J, Roehle, R, Blohmer, JU, Keilholz, U, et al.. Quality of life after risk-reducing salpingo-oophorectomy in women with a pathogenic BRCA variant. J Sex Med 2023;21:33–9. https://doi.org/10.1093/jsxmed/qdad143.Suche in Google Scholar PubMed
8. Vilos, GA, Alshimmiri, MM. Cost-benefit analysis of laparoscopic versus laparotomy salpingo-oophorectomy for benign tubo-ovarian disease. J Am Assoc Gynecol Laparoscopists 1995;2:299–303. https://doi.org/10.1016/s1074-3804(05)80112-4.Suche in Google Scholar PubMed
9. Rosati, A, Fedele, C, Fagotti, A, Lafuenti, L, Gioè, A, Chieffo, DPR, et al.. Needleoscopic-assisted risk-reducing bilateral salpingo-oophorectomy in BRCA1/2 mutation carriers: peri-operative outcomes and psychological impact. Eur J Obstet Gynecol Reprod Biol 2022;273:1–6. https://doi.org/10.1016/j.ejogrb.2022.03.040.Suche in Google Scholar PubMed
10. Chiofalo, B, Bruno, V, Calandra, M, Savone, D, Mancini, E, Baiocco, E, et al.. Percutaneous-assisted laparoscopy for ovarian tissue cryopreservation: a single-center experience. Arch Gynecol Obstet 2022;306:1329–35. https://doi.org/10.1007/s00404-022-06684-0.Suche in Google Scholar PubMed
11. Gueli, AS, Perrone, E, Cretì, A, Cianci, S, Uccella, S, Fedele, C, et al.. Feasibility and perioperative outcomes of percutaneous-assisted laparoscopic hysterectomy: a multicentric Italian experience. Eur J Obstet Gynecol Reprod Biol 2020;245:181–5. https://doi.org/10.1016/j.ejogrb.2019.12.020.Suche in Google Scholar PubMed
12. Rossitto, C, Cianci, S, Gueli Alletti, S, Perrone, E, Pizzacalla, S, Scambia, G. Laparoscopic, minilaparoscopic, single-port and percutaneous hysterectomy: comparison of perioperative outcomes of minimally invasive approaches in gynecologic surgery. Eur J Obstet Gynecol Reprod Biol 2017;216:125–9. https://doi.org/10.1016/j.ejogrb.2017.07.026.Suche in Google Scholar PubMed
13. Rossitto, C, Gueli Alletti, S, Rotolo, S, Cianci, S, Panico, G, Scambia, G. Total laparoscopic hysterectomy using a percutaneous surgical system: a pilot study towards scarless surgery. Eur J Obstet Gynecol Reprod Biol 2016;203:132–5. https://doi.org/10.1016/j.ejogrb.2016.05.007.Suche in Google Scholar PubMed
14. Restaino, S, Finelli, A, Pellecchia, G, Biasioli, A, Mauro, J, Ronsini, C, et al.. Scar-free laparoscopy in BRCA-mutated women. Medicina (Kaunas) 2022;58:943. https://doi.org/10.3390/medicina58070943.Suche in Google Scholar PubMed PubMed Central
15. Benchimol, EI, Smeeth, L, Guttmann, A, Harron, K, Moher, D, Petersen, I, et al.. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015;12:e1001885. https://doi.org/10.1371/journal.pmed.1001885.Suche in Google Scholar PubMed PubMed Central
16. Dindo, D, Demartines, N, Clavien, PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.Suche in Google Scholar PubMed PubMed Central
17. Franceschini, G, Di Leone, A, Terribile, D, Sanchez, MA, Masetti, R. Bilateral prophylactic mastectomy in BRCA mutation carriers: what surgeons need to know. Ann Ital Chir 2019;90:1–2.10.5152/ejbh.2019.4651Suche in Google Scholar PubMed PubMed Central
18. Hoga, L, Rodolpho, J, Gonçalves, B, Quirino, B. Women’s experience of menopause: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep 2015;13:250–337. https://doi.org/10.11124/jbisrir-2015-1948.Suche in Google Scholar PubMed
19. Vitale, SG, Angioni, S, D’Alterio, MN, Ronsini, C, Saponara, S, De Franciscis, P, et al.. Risk of endometrial malignancy in women treated for breast cancer: the BLUSH prediction model – evidence from a comprehensive multicentric retrospective cohort study. Climacteric 2024;27:482–8. https://doi.org/10.1080/13697137.2024.2376189.Suche in Google Scholar PubMed
20. Lee, HJ, Jang, YJ. Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci 2018;19:711. https://doi.org/10.3390/ijms19030711.Suche in Google Scholar PubMed PubMed Central
21. LA Russa, M, Liakou, C, Burbos, N. Ultra-minimally invasive approaches for endometrial cancer treatment: review of the literature. Minerva Med 2021;112:31–46. https://doi.org/10.23736/s0026-4806.20.07073-1.Suche in Google Scholar
22. Mereu, L, Pecorino, B, Ferrara, M, Siniscalchi, M, Garraffa, G, D’Agate, MG, et al.. Cumulative sum analysis of learning curve process for vaginal natural orifice transluminal endoscopic surgery hysterectomy. J Minim Invasive Gynecol 2023;30:582–6. https://doi.org/10.1016/j.jmig.2023.03.013.Suche in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/oncologie-2025-0029).
© 2025 the author(s), published by De Gruyter on behalf of Tech Science Press (TSP)
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Review Articles
- Unveiling the hidden role of tumor-educated platelets in cancer: a promising marker for early diagnosis and treatment
- Multiple roles of mitochondria in tumorigenesis and treatment: from mechanistic insights to emerging therapeutic strategies
- The impact of JMJD5 on tumorigenesis: a literature review
- Research Articles
- A case-matched comparison of ER-α and ER-β expression between malignant and benign cystic pancreatic lesions
- Salivary gamma-glutamyltransferase activity as an indicator of redox homeostasis in breast cancer
- Cancer can be suppressed by alkalizing the tumor microenvironment: the effectiveness of “alkalization therapy” in cancer treatment
- Percutaneous-assisted laparoscopic bilateral salpingo-oophorectomy in BRCA-mutated patients: a retrospective comparative study
- ACAT2 contributes to cervical cancer tumorigenesis by regulating the expression of the downstream gene LATS1
- Rapid Communication
- Efficacy of mild hyperthermia in cancer therapy: balancing temperature and duration
- Case Report
- Orbital marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue with amyloidosis: a case series and review of the literature
- Commentary
- Palliative external beam radiotherapy for dysphagia management in advanced esophageal cancer: a narrative perspective
- Endometriosis and endometriosis-associated ovarian cancer, possible connection and early diagnosis by evaluation of plasma microRNAs
Artikel in diesem Heft
- Frontmatter
- Review Articles
- Unveiling the hidden role of tumor-educated platelets in cancer: a promising marker for early diagnosis and treatment
- Multiple roles of mitochondria in tumorigenesis and treatment: from mechanistic insights to emerging therapeutic strategies
- The impact of JMJD5 on tumorigenesis: a literature review
- Research Articles
- A case-matched comparison of ER-α and ER-β expression between malignant and benign cystic pancreatic lesions
- Salivary gamma-glutamyltransferase activity as an indicator of redox homeostasis in breast cancer
- Cancer can be suppressed by alkalizing the tumor microenvironment: the effectiveness of “alkalization therapy” in cancer treatment
- Percutaneous-assisted laparoscopic bilateral salpingo-oophorectomy in BRCA-mutated patients: a retrospective comparative study
- ACAT2 contributes to cervical cancer tumorigenesis by regulating the expression of the downstream gene LATS1
- Rapid Communication
- Efficacy of mild hyperthermia in cancer therapy: balancing temperature and duration
- Case Report
- Orbital marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue with amyloidosis: a case series and review of the literature
- Commentary
- Palliative external beam radiotherapy for dysphagia management in advanced esophageal cancer: a narrative perspective
- Endometriosis and endometriosis-associated ovarian cancer, possible connection and early diagnosis by evaluation of plasma microRNAs


