Abstract
Objectives
This study aimed to assess the dietary patterns of adolescents to develop targeted medical and organizational interventions for optimizing nutrition and physical activity.
Methods
Research was conducted in Astana in the fall of 2024 and involved 162 adolescents aged 15–19 years (mean age: 17.8 ± 0.41 years) who were classified into special medical groups based on preventive health examinations. Dietary data were collected using the World Health Organization-recommended 24-h recall method, and nutrient intake was assessed against national dietary recommendations and Food and Agriculture Organization/World Health Organization standards.
Results
The analysis demonstrated that adolescents in special medical groups had significantly reduced daily caloric intake (p<0.001) and an imbalanced macronutrient profile, characterized by excessive consumption of animal fats and simple carbohydrates alongside insufficient intake of polysaccharides and dietary fiber. Widespread deficiencies in essential micronutrients were observed, particularly in vitamins A, D, B1, B6, B9, C, and E, as well as calcium, iodine, phosphorus, magnesium, and iron. These nutritional inadequacies were closely associated with reduced physical endurance, increased fatigue, and lower academic and physical performance, underscoring the urgent need for targeted nutritional interventions.
Conclusions
These findings emphasize the necessity of dietary interventions and tailored physical activity programs to enhance the overall health and functional capacity of adolescents requiring specialized medical supervision.
Introduction
Optimal nutrition is essential for health, particularly throughout adolescence, a period marked by fast development, metabolic alterations, and heightened physiological requirements. Ensuring sufficient nutrition is crucial for adolescents in specialised medical groups, since their health conditions and physical capacities may necessitate tailored dietary approaches to promote optimal growth and functional capacity. Based on the data from the 2023 Annual Report [1], the proportion of adolescents in Kazakhstan facing health issues remains alarmingly high. Official figures indicate that only a small fraction of adolescents can be classified as having optimal health, while a significant proportion exhibit various risk factors associated with chronic diseases. Among the key contributors to these negative trends are inadequate physical activity levels and suboptimal dietary patterns. The national assessment of school nutrition highlighted concerns regarding the prevalence of both undernutrition and excessive weight gain, emphasizing the need for targeted interventions. Recognizing these pressing issues, ensuring proper nutrition and promoting an active lifestyle have become essential strategies for safeguarding the well-being and overall quality of life of school-aged children in Kazakhstan.
Kalmakova et al. [2] underscore the critical role of systematic exercise in adolescence, suggesting that regular engagement with varied physical activities can notably reduce the onset of chronic conditions. Similarly, Beisembayev et al. [3] highlight how balanced dietary patterns: encompassing sufficient intake of complex carbohydrates, lean proteins, and micronutrients, are instrumental in preventing both undernutrition and obesity. In their view, nutritional deficits established early in life can profoundly influence metabolic health later on, heightening susceptibility to obesity-related complications. Berezka et al. [4] focus on motivational and psychological factors, emphasizing that interventions incorporating both intrinsic (e.g., personal growth, self-efficacy) and extrinsic (e.g., peer support, structured curricula) incentives yield better adherence to lifestyle changes among adolescents. These authors note that insufficient motivation frequently results in intermittent participation, which diminishes the effectiveness of any health-focused program.
Abdrakhmanova et al. [5], analyzing the anthropometric measurements of primary school children across multiple regions, found that 20.6 % exhibited overweight (including obesity), while 5 % showed inadequate body weight. Notably, 6.6 % were clinically obese, of whom 1.6 % were classified as having severe obesity. The study also documented regional variations, indicating that some areas showed rates of underweight as high as 8.3 % and overweight prevalence peaking at nearly 29.3 %. These alarming statistics reveal the dual burden of malnutrition, encompassing both undernutrition and obesity, that poses significant risks to children’s academic performance, psychological well-being, and overall developmental trajectory. The findings also suggest that multifaceted interventions, ranging from targeted dietary guidelines to environment-specific activity programs, are urgently needed to mitigate these risks.
According to the National Center for Public Health study [6] the frequency of daily breakfast decreases as girls grows older, from 11 to 15 years old (from 67.9 to 42.6 %), and in boys the decrease starts from 13 years old (66.8 %) to 15 years old (59.2 %). By age 15, about one-third of girls (30.8 %) and about one-fifth of boys (18 %) never eat breakfast on weekdays. The rate of daily fruit consumption declines among boys from age 11 to 15 (from 29 to 25.8 %). Daily consumption of sweetened and energy drinks, sugary foods such as candy and chocolate increase overall among children from age 11 to age 15. The older children get, the more often they consume junk food.
Despite considerable efforts to investigate dietary habits and related health outcomes, many existing studies have relied on small or regionally restricted samples, focused narrowly on specific food groups, or merely documented the consequences of insufficient or excessive nutrition (such as overweight and obesity). Consequently, a substantial knowledge gap persists regarding the comprehensive evaluation of adolescents’ nutritional status, including both macronutrient and micronutrient intake, and the extent to which these factors align with national and international dietary recommendations. Moreover, the absence of detailed, population-level data has hindered the development of targeted public health strategies that address the dual burden of nutrient deficiencies and excessive energy consumption.
The aim of this study is to provide a comprehensive assessment of the nutritional status of adolescents assigned to special medical groups, with a focus on evaluating not only overall energy intake but also the balance of macro- and micronutrients as well as characteristic dietary patterns. The research seeks to identify the prevalence and severity of nutritional deficiencies, to analyze their impact on physical development, cognitive performance, and psychosocial well-being, and to generate evidence-based recommendations for medical, organizational, and educational interventions designed to optimize nutrition and support the health and physical activity of this vulnerable group.
Materials and methods
This cross-sectional study was conducted in Astana (Republic of Kazakhstan) in the fall season, focusing on the dietary intake and overall nutritional status of adolescents who had been assigned to special medical groups due to health considerations. Ethical approval was obtained from the local bioethics committee of the Astana Medical University, protocol number 7, dated October 16, 2023, ensuring that the research adhered to the principles outlined in relevant national regulations and the Declaration of Helsinki [7], 8].
A total of 162 participants, ranging in age from 15 to 19 years (mean age: 17.8 ± 0.41 years), were included in the study. Of these, 27.2 % were male, and 72.8 % were female. All participants resided in Astana and were selected based on having official medical exemptions from physical education classes (form 026/u), issued according to the directives outlined in Order No. KR DSM-175/2020 of the Ministry of Health of the Republic of Kazakhstan [9]. Such exemptions arise from permanent or temporary health deviations that necessitate modifying or limiting physical activity levels. By focusing exclusively on adolescents in special medical groups, the study aimed to capture data on a population particularly vulnerable to health risks associated with inadequate diet and physical inactivity.
Data collection procedures emphasized detailed assessments of actual nutrition. Participants completed the 24-h dietary recall method recommended by the World Health Organization on typical weekdays during the fall period. This approach enabled the researchers to document specific food items, portion sizes, meal frequencies, and cooking methods. Additionally, a frequency analysis of overall dietary patterns was carried out to identify common consumption habits for specific food groups. The information gathered through both techniques was then compared with recommended dietary intake norms for the population of the Republic of Kazakhstan, as well as nutrient intake guidelines established by the World Health Organization, Food and Agriculture Organization of the United Nations [10], 11].
All collected data were entered into Microsoft Excel spreadsheets and subsequently analyzed using IBM SPSS Statistics version 28.0 (IBM Corp., Armonk, NY, USA). Prior to conducting inferential analyses, the dataset was carefully checked for missing values, outliers, and logical inconsistencies. Cases with incomplete dietary recalls were excluded from the final analysis. Continuous variables were assessed for normality using the Shapiro–Wilk test, while distributional properties were additionally evaluated through histograms and Q–Q plots. Where necessary, variables exhibiting skewed distributions (e.g., micronutrient intakes with extreme values) were normalized using logarithmic transformation to meet the assumptions of parametric testing.
For descriptive statistics, measures of central tendency (mean, median) and variability (standard deviation, interquartile range) were calculated. Group comparisons between male and female participants were conducted using Student’s independent samples t-test for normally distributed variables and the Mann-Whitney U test for non-normally distributed variables. Categorical variables, such as meal frequency categories and food preference patterns, were analyzed using the Chi-square test of independence.
To explore associations between nutrient intake and health-related indicators (e.g., body mass index, reported energy levels, and mood state), correlation analyses were performed. Pearson’s correlation coefficient (r) was applied to normally distributed continuous variables, whereas Spearman’s rank correlation coefficient (ρ) was used for non-normally distributed data. The strength of correlations was interpreted according to established conventions (weak: r=0.1–0.3, moderate: r=0.3–0.5, strong: r>0.5).
For comparisons of nutrient intakes with established national and international dietary reference values, one-sample t-tests were applied where normality was satisfied; otherwise, Wilcoxon signed-rank tests were used. Effect sizes (Cohen’s d for t-tests, r for non-parametric comparisons) were calculated to quantify the magnitude of differences.
The threshold for statistical significance was set at p<0.05 for all analyses. Adjustments for multiple comparisons were applied using the Bonferroni correction in cases where large numbers of micronutrients were simultaneously tested against dietary reference values. This analytical framework ensures that all data processing steps and statistical procedures can be fully reproduced by independent researchers working with comparable datasets.
Statistical analysis accounted for both descriptive and inferential elements. Preliminary evaluation of the dataset involved assessing normality through tests such as the Shapiro-Wilk test [12]. Data conforming to normal distribution were further examined using parametric analyses, including calculations of mean values, standard deviations, and Student’s t-tests for group comparisons. Variables that did not meet normality assumptions were explored via nonparametric methods. The significance threshold for all analyses was set at p<0.05. Correlation analysis (Pearson’s or Spearman’s rank correlation, depending on normality) was also performed to explore potential relationships between nutrient intake levels, caloric balance, and selected health indicators like body mass index, endurance capacity, and subjective well-being. The results were used to identify patterns of macro- and micronutrient insufficiency and to suggest targeted nutritional interventions, thereby forming the basis for subsequent medical and educational recommendations aimed at improving the health and performance of adolescents requiring specialized care.
Results
The analysis of adolescents’ dietary patterns revealed pronounced imbalances in both energy and nutrient intake, highlighting a complex picture of insufficient caloric supply, inadequate consumption of key macronutrients, and multiple micronutrient deficiencies. Overall, daily energy intake in both boys and girls was significantly below recommended levels, while protein and carbohydrate consumption fell short of normative standards, often leading to a compensatory reliance on simple sugars. Lipid intake showed partial alignment with dietary guidelines but was characterized by excessive saturated fat consumption. Particularly concerning were deficits in calcium, vitamin D, folate, and dietary fiber, which point to long-term risks for skeletal development, metabolic health, and immune resilience. These nutritional inadequacies were compounded by low consumption of fruits, vegetables, and fish, alongside a high prevalence of refined carbohydrate and sugar intake.
According to the data in Table 1, respondents typically consumed food 3.11 ± 0.02 times per day. A statistically significant gender difference was identified (t=2.5; p<0.05), indicating differences in eating behavior between boys and girls. The majority of participants (66.2 ± 0.51 %) described their overall eating pattern as regular, yet 22.4 ± 1.64 % expressed uncertainty about mealtime consistency, and 11.4 ± 1.79 % reported that they occasionally skipped or delayed specific meals. Notably, nearly half of the respondents (49 ± 0.88 %) finished eating 2–3 h before bed, which is often considered a more balanced practice and may reduce the likelihood of late-night snacking. This is significant as late-night snacking can negatively affect sleep quality and metabolic health. However, 42.4 ± 1.02 % had their final intake closer to 1–2 h before sleeping, 5.3 ± 2.35 % did so immediately prior to rest, and only 3.3 ± 5.11 % allowed a longer interval of 4–5 h between their last meal and bedtime, possibly indicating divergent habitual or cultural norms that might affect sleep quality and metabolic function.
Daily intake of nutrients and energy by respondents compared to the recommended intake of essential nutrients in adolescents.
| Nutrient | Daily intake rates | Girls | Boys | ||
|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | ||
| Calories, kcal | Male: 3,000 Female: 2,400 |
1927c | 50.73 | 1855c | 43.52 |
| Protein total, g | Male: 90 Female: 72 |
66.7 | 15.8 | 76.0 | 26.4 |
| Animal proteins, g | Male: 54 Female: 43 |
32.3 | 13.5 | 40.1 | 19.7 |
| Fats, g | Male: 93 Female: 75 |
64.6 | 31.6 | 75.5 | 33.7 |
| Vegetable lipids, g | Male: 28 Female: 23 |
23.3 | 10.4 | 25.6 | 16.8 |
| Saturated fatty acids, g | <11 | 21.91 | 8.5 | 27.28 | 10.1 |
| Polyunsaturated fatty acids, g | Male: 10 Female: 8 |
12.64 | 6.3 | 13.87 | 9.1 |
| Trans fatty acids (T TRANS), g | 0 | 0.669 | 0.93 | 0.781 | 0.95 |
| Cholesterol, mg | <300 | 209.80 | 75.2 | 216.70 | 66.3 |
| Carbohydrates, g | Male: 450 Female: 360 |
197.9a | 63.4 | 229.1b | 78.2 |
| Starch, g | 270–500 | 155.8c | 31.4 | 145.2b | 46.3 |
| Simple carbohydrates, g | Male: 25 Female: 25 |
85.3 | 37.1 | 80.3 | 42.6 |
| Dietary fiber, g | Male: 38 Female: 26 |
6.7c | 3.7 | 7.09c | 3.4 |
| Sodium, g | Male: 1.5 Female: 1.5 |
2.9 | 49.7 | 2.5 | 33 |
| Potassium, mg | Male: 2,400 Female: 2,400 |
2062.1c | 73 | 2,252.8 | 79.1 |
| Calcium, mg | Male: 1,300 Female: 1,300 |
472.3c | 88.2 | 502.3c | 53.9 |
| Magnesium, mg | Male: 300 Girls −300 |
243.8 | 83.3 | 262.6 | 94.2 |
| Phosphorus, mg | Male: 1,200 Female: 1,200 |
905.2a | 81 | 1,089.0a | 30.5 |
| Iron, mg | Male: 15 Female: 20 |
11.89 | 7.2 | 15.64 | 7.1 |
| Copper, mg | Male: 800 Female: 850 |
1113c | 1.08 | 930c | 1.19 |
| Zinc, mg | Male: 10 Female: 8 |
7.02 | 3.03 | 7.35 | 3.67 |
| Manganese, mg | Male: 2.5 Female: 2.5 |
2.77 | 0.88 | 3.41 | 1.27 |
| Selenium, mcg | Male: 40 Female: 40 |
34.96 | 14.8 | 40.55 | 23.9 |
| Iodine, mcg | Male: 150 Female: 150 |
72.98a | 32.8 | 81.01a | 30.6 |
| Retinol (A), mcg | Male: 800 Female: 800 |
401.8 c | 45.5 | 389.7 c | 40.9 |
| Vitamin D, mcg | Male: 10 Female: 10 |
1.73c | 1.15 | 1.22c | 1.74 |
| Vitamin E, mg | Male: 15 Female: 15 |
13.7 | 4.61 | 13.32 | 5.40 |
| Thiamine, B1), mg | Male: 1.2 Female: 1.1 |
0.81 | 0.35 | 0.88 | 0.31 |
| Riboflavin (B2), mg | Male: 1.3 Female: 1.1 |
1.09 | 0.55 | 1.19 | 0.67 |
| Niacin (PP/B3), mg | Male: 16 Female: 16 |
13.39 | 3.54 | 18.7 | 5.15 |
| Pyridoxine (B6), mg | Male: 1.3 Female: 1.2 |
0.85 | 0.51 | 1.06 | 0.74 |
| Cyanocobalamin (B12), mg | Male: 2.4 Female: 2.4 |
2.79 | 4.08 | 2.17 | 7.09 |
| Folate (B9), mcg | Male: 400 Female: 400 |
109.5c | 45.5 | 142.6c | 58.3 |
| Pantothenic acid (B5), mg | Male: 5 Female: 5 |
2.12 | 1.76 | 2.57 | 2.02 |
| Biotin (H/B7), mg | Male: 25 Female: 25 |
22.47 | 7.22 | 26.73 | 8.48 |
| Vitamin C, mg | Male: 75 Female: 65 |
50.75 | 48.5 | 71.36 | 77.4 |
-
aReliability p<0.05 of the index compared with the norm; breliability p<0.01 of the index compared with the norm; creliability p<0.001 of the index compared with the norm. Source: compiled by the authors.
Table 1 provides a detailed comparison of the daily intake of energy and essential nutrients among adolescent boys and girls in special medical groups against recommended dietary standards. The data show that overall caloric intake was significantly lower than required for both sexes, with girls averaging 1927 kcal compared to the recommended 2,400 kcal and boys averaging 1855 kcal compared to the recommended 3,000 kcal. Protein consumption also fell short of recommended levels, particularly from animal sources, while fat intake was closer to the norm but characterized by a pronounced excess of saturated fatty acids. Carbohydrate intake was notably inadequate, with both starch and dietary fiber consumption far below recommended levels, whereas simple sugars were consumed in excessive amounts. The micronutrient profile revealed severe deficiencies in calcium, vitamin D, folate, iodine, and vitamins A and C, accompanied by insufficient intake of several B-vitamins and minerals such as zinc and iron. At the same time, copper intake exceeded recommended thresholds, which may interfere with the absorption of other trace elements. Collectively, these findings illustrate a dietary pattern marked by energy insufficiency, widespread micronutrient deficits, and imbalances in macronutrient quality, highlighting considerable risks to the health and development of this adolescent population.
When exploring preferences for protein sources, more than 60 % chose beef or horse meat. Mutton and chicken were considerably less prevalent, while pork and game combined barely reached 4.7 %. An additional 5.3 ± 1.21 % excluded meat entirely, reflecting a small yet pertinent vegetarian contingent. About one-third of respondents (34.3 ± 2.76 %) reported consuming fatty meat (including ham, lard, or other high-lipid products) 2–3 times weekly, whereas 17.6 ± 2.11 % restricted intake to holiday occasions, and 17.1 ± 2.07 % included such items daily. These findings highlight different approaches to rich-protein or high-fat meats, pointing to an array of dietary philosophies. Of further interest is the near absence of fish in many diets, eliminating a notable source of long-chain polyunsaturated fatty acids and certain micronutrients that could bolster cardiovascular and neural health.
In interpreting the findings, it is important to distinguish between macronutrients and micronutrients. Macronutrients – such as proteins, fats, and carbohydrates – are required in large amounts and serve as the primary sources of energy and structural components for growth and physical performance. In this study, their imbalance was reflected in insufficient caloric intake, inadequate consumption of complex carbohydrates and dietary fiber, and excessive intake of animal fats and simple sugars. By contrast, micronutrients – including vitamins (A, D, B-group, C, E) and minerals (calcium, iodine, iron, magnesium, phosphorus) – are needed in much smaller quantities but are essential for regulatory and protective functions. Deficiencies identified in the present sample, particularly in calcium, vitamin D, folate, and iodine, compromise skeletal development, immune resilience, and cognitive capacity. Together, the inadequacy of both macro- and micronutrients underscores the dual burden faced by adolescents in special medical groups, where insufficient energy supply is compounded by critical regulatory deficits.
Refined carbohydrates also appeared to predominate in daily menus. White bread and other refined flour products overshadowed whole-grain alternatives, and rye bread was virtually unused. On average, participants ate 4.11 ± 0.06 slices of bread per day, a pattern that reduces potential benefits from fiber and associated vitamins or minerals. The elevated popularity of sweets and caffeinated drinks was similarly evident: tea, for instance, often contained 1.95 ± 0.05 tablespoons of sugar per cup, implying a significant cumulative sugar load that might increase the risk of overweight, metabolic disturbances, or dental issues [13], 14].
Daily fluid intake generally hovered around 1–2 L (56.7 ± 2.93 %), though 28.1 ± 2.76 % drank 2–3 L, and 15.2 ± 2.02 % ingested only 0.5–1.0 L. While many presumably achieved standard hydration targets when accounting for water from food items, nearly one out of six individuals consumed minimal volumes, which could compromise thermoregulation, renal excretion, and cognitive performance. Regarding dietary sodium, 45 ± 0.13 % of respondents indicated a preference for low-salt options, while 55 ± 0.98 % admitted to favoring more heavily salted food. Among the latter, around 68 % specifically chose iodized salt, which helps counteract iodine deficiency yet may not fully balance out the elevated sodium level in the rest of the diet.
Only 27.4 ± 3.1 % of respondents reported consuming fruit at least once a day, and an even smaller segment, 20.5 ± 3.1 %, did the same for vegetables. Consequently, nearly three quarters were missing out on consistent intake of fresh plant-based foods, a gap that can lead to elevated risks of chronic conditions such as cardiovascular disease or metabolic syndrome. In addition, such dietary patterns may adversely affect day-to-day functioning and physical resilience, especially among adolescents in special medical groups who often have existing health challenges.
Further analysis showed that these adolescents were more likely to consume processed meats and deli products instead of fruit and vegetable dishes. Although this substitution might satisfy immediate energy requirements, it offers limited support for micronutrient adequacy and dietary fiber intake [15], 16]. Individuals who, by contrast, integrated cheese, milk, and cottage cheese into their meals more frequently demonstrated better concentration during academic tasks (r=0.35, p<0.01) and higher perceived energy levels (r=0.45, p<0.01). They also tended to exhibit fewer episodes of irritability (r=0.45, p<0.02) and a notably lower frequency of negative moods (r=0.55, p<0.01). These associations may reflect the stabilizing roles of high-quality proteins, calcium, and certain bioactive peptides in modulating neurotransmitter function and preventing abrupt fluctuations in blood glucose.
Nuts could provide similar benefits, yet 28 % of surveyed individuals excluded them from their diets entirely. Participants who did incorporate fruits, vegetables, and nuts more often showed both a modest sugar intake (r=−0.29, p<0.01) and an enhanced capacity to cope with stress (r=−0.46, p<0.01). Such results are consistent with evidence linking complex nutrients, including polyunsaturated fatty acids, vitamins, and phytochemicals, to protective effects on mood regulation and overall metabolic health.
The most critical inadequacies were observed in the intake of calcium, vitamin D, folate, and dietary fiber, where actual consumption remained significantly below the recommended levels, potentially exacerbating risks of metabolic disturbances and impaired physiological development, which presented on Figure 1.
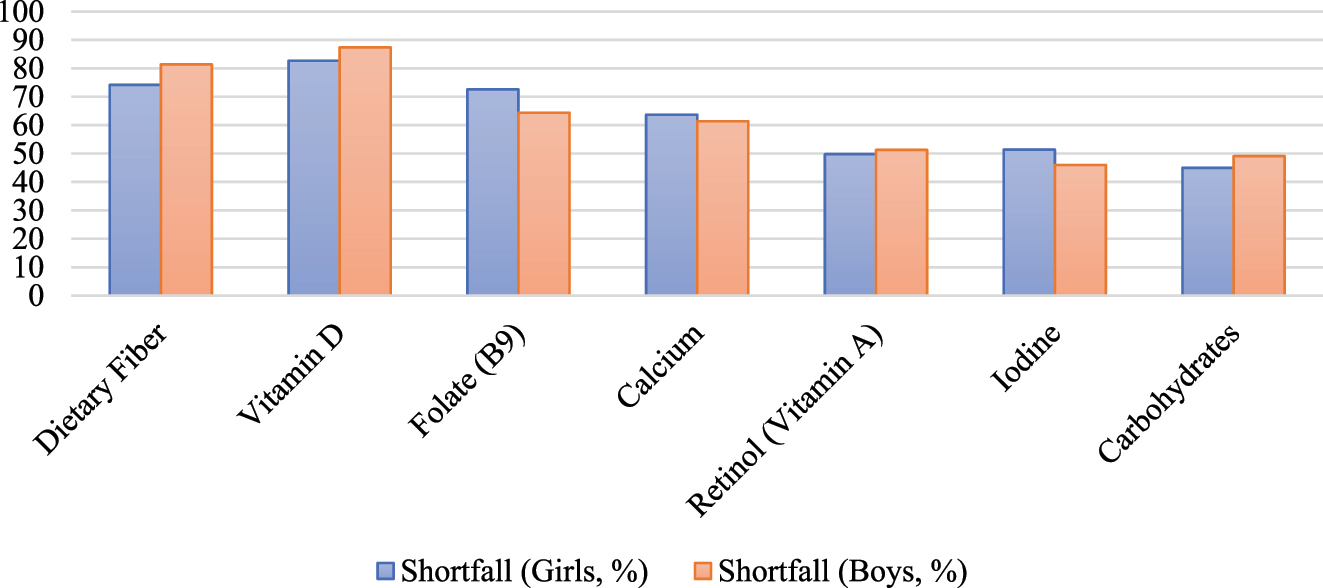
Micronutrients with the most pronounced deficiency in adolescents compared to recommended intake levels. Source: compiled by the authors.
According to the World Health Organization [17], 18], insufficient or unbalanced nutrition correlates with a substantial proportion of diseases, largely because 75–80 % of harmful factors can enter the human body through contaminated or suboptimal dietary sources. Thus, the chronic intake of micronutrient-deficient meals not only compounds infection risks but also compromises systemic health indicators, from demographic trends to socioeconomic stability. In the present sample, the daily caloric intake for adolescent girls averaged 1927 ± 50.73 kcal compared to the recommended 2,400 kcal, whereas boys consumed 1855.0 ± 43.52 kcal compared to the recommended 3,000 kcal. Both values fell considerably below recommended dietary energy levels (p<0.001), implying that these young individuals may be receiving insufficient nutrients for optimal growth, cognitive performance, and immune resilience.
Recent data indicate that overall protein consumption remains slightly below recommended daily intake, with girls and boys averaging 66.7 g/1,000 kcal and 76.0 g/1,000 kcal, respectively. These values also suggest that adolescents are not obtaining adequate quantities of high-quality proteins, particularly those of animal origin. Such deficits may compromise growth trajectories, reduce muscle development, and potentially contribute to an elevated prevalence of stunting [19], 20]. Moreover, the body often reallocates existing protein stores to meet energy demands when carbohydrates are lacking, which can diminish protein’s role in supporting tissue repair, enzymatic processes, and the immune system.
Insufficient carbohydrate intake appears to be a principal driver of these imbalances. Daily carbohydrate consumption stood at 197.9 g for girls and 229.1 g for boys – significantly below the target range of 360 g (girls) and 450 g (boys). This shortfall translates to 102.7–123.5 g/1,000 kcal, whereas dietary guidelines call for a density of 140–190 g/1,000 kcal. Such chronic carbohydrate deficits frequently result in proteins being diverted for energy production instead of tissue synthesis or functional maintenance. The ensuing low energy availability can undermine academic performance, physical endurance, and overall metabolic stability.
Regarding lipids, the proportion of vegetable-based lipids was determined by calculating their share of total fat intake, amounting to (23.3 g/64.6 g) × 100≈31 % in girls and (25.6 g/75.5 g) × 100≈27.5 % in boys, which appears moderately favorable. However, total fatty acid consumption slightly exceeded recommended limits, reaching 21.91–27.28 g per 1,000 kcal, whereas contemporary research indicates that intake should remain below 11 g per 1,000 kcal to align with current dietary guidelines [21], 22]. This excess likely stems from the high intake of animal products, as well as convenience foods containing partially hydrogenated fats. Nevertheless, the observed ratio between polyunsaturated and saturated fatty acids ranged from 0.5 to 0.6, staying within the generally acceptable interval of 0.6–1. Additionally, the daily cholesterol consumption for both sexes remained under 300 mg/day, aligning with World Health Organization guidance. Trans fats, however, though minimal at 0.03–0.04 % of daily calories, pose a concern, given World Health Organization’s call for their complete exclusion from adolescent diets [23], 24].
Analyzing carbohydrate quality reveals further imbalances. Simple carbohydrates – primarily sugars – contribute approximately 17.3–17.7 % of total energy intake, surpassing the recommended ceiling of 10 %. Meanwhile, polysaccharides such as starch and dietary fiber remain notably underrepresented, with starch hovering around 145.2–155.8 g/day compared to recommended values of 270–500 g/day, and fiber intake stuck at 6.7–7.09 g/day instead of the 26–38 g/day range. These deficits not only diminish satiety and glycemic control, but also curtail the supply of beneficial phytochemicals and gut microbiota substrates that support gastrointestinal health.
Ultimately, the existing dietary profile – marked by low protein from animal sources, modest vegetable fats, excessive reliance on simple sugars, and insufficient polysaccharides – may impede adolescents’ growth, academic performance, and long-term health outcomes. Addressing these imbalances demands multifaceted interventions that encourage greater incorporation of complex carbohydrates, a more precise balance of lipids, and sufficient, high-quality protein sources.
A pronounced inadequacy in multiple micronutrients was identified in the present study. Calcium intake, for instance, averaged only 472.3 ± 88.2 mg/day in girls and 502.3 ± 53.9 mg/day in boys, whereas adolescents are expected to receive approximately 1,300 mg/day. When analyzed as nutritional density per 1,000 kcal, the values were 245.1 mg in girls and 270.8 mg in boys, underscoring a substantial shortfall relative to targets essential for healthy skeletal growth and mineralization. Potassium intake, which averaged 2062.1 ± 73.0 mg/day in girls and 2,252.8 ± 79.1 mg/day in boys, also remained below the recommended 2,400 mg/day. This discrepancy is particularly concerning since low potassium intake tends to coincide with elevated sodium consumption, a combination that can disrupt fluid balance and potentially contribute to hypertensive tendencies.
Iodine deficiency emerged as well, with daily consumption measured at 72.98 ± 32.8 µg/day in girls and 81.01 ± 30.6 µg/day in boys, compared to a recommendation of 150 µg/day. Notably, this figure excludes the contribution of iodized salt, although even with fortified sources of sodium chloride, these levels seem insufficient. At the same time, copper intake overshot the norm, averaging 1,113 ± 1.08 µg/day in girls and 930 ± 1.19 µg/day in boys, surpassing the usual requirement of 800–850 µg/day. Such excess in copper can potentially inhibit zinc and iron absorption, thereby risking an additional deficiency of essential trace elements and possibly encouraging anemia.
Phosphorus consumption was likewise below the ideal threshold. Daily amounts averaged 905.2 ± 81 mg/day in girls and 1,089.0 ± 30.5 mg/day in boys, rather than the suggested 1,200 mg/day. This situation may hamper normal bone mineralization and energy metabolism. Parallel deficits in vitamins further amplify these vulnerabilities. Vitamin A intake among girls and boys, recorded at 401.8 ± 45.5 µg/day and 389.7 ± 40.9 µg/day respectively, fell conspicuously short of the 800 µg/day target. Vitamin D levels were equally insufficient, around 1.73 ± 1.15 µg/day in girls and 1.22 ± 1.74 µg/day in boys, quite distant from the 10 µg/day benchmark. Vitamin D is a key regulator of calcium metabolism, facilitating its absorption in the intestines and maintaining bone mineralization [25]. Insufficient levels of this fat-soluble vitamin have been associated with impaired calcium uptake, which may lead to suboptimal skeletal development and increased risk of bone demineralization in adolescents [26], 27]. Given the already insufficient calcium intake observed in the present study, a concurrent deficiency in vitamin D is likely to further exacerbate these inadequacies, potentially contributing to long-term musculoskeletal complications [28]. This interplay underscores the importance of adequate vitamin D status in mitigating calcium insufficiency and highlights the need for targeted dietary interventions to address these overlapping nutritional deficiencies.
Folate consumption likewise registered below acceptable norms, averaging 109.5 ± 45.5 µg/day in girls and 142.6 ± 58.3 µg/day in boys, rather than the 400 µg/day guideline. Analyzing the intake per 1,000 kcal revealed a parallel pattern, indicating that adolescents do not receive adequate dietary folate density. Meanwhile, a cluster of other vitamins appeared compromised. Vitamin B1 dropped as low as 0.81 ± 0.35 mg/day in girls and 0.88 ± 0.31 mg/day in boys, with recommended levels at 1.1 mg/day and 1.2 mg/day. Pyridoxine (B6) was also suboptimal: 0.85 ± 0.51 mg/day and 1.06 ± 0.74 mg/day in girls and boys, respectively, instead of the 1.2–1.3 mg/day ideal. Pantothenic acid (B5) hovered around 2.12 ± 1.76 mg/day in girls and 2.57 ± 2.02 mg/day in boys, less than half of the 5 mg/day benchmark. A parallel deficit emerged in vitamin C, which measured 50.75 ± 48.5 mg/day for girls and 71.36 ± 77.4 mg/day for boys, instead of the respective targets of 65 mg/day and 75 mg/day. Vitamin E levels were similarly underrepresented at 13.7 ± 4.61 mg/day in girls and 13.32 ± 5.40 mg/day in boys, rather than the recommended 15 mg/day.
The dietary patterns observed among adolescents in special medical groups can be explained through a combination of nutritional, physiological, and psychosocial theories that account for both causal relationships and broader developmental implications. From a nutritional physiology perspective, the chronic energy deficit detected in both sexes may be directly linked to impaired growth, reduced physical capacity, and diminished cognitive function. Theories of energy balance emphasize that inadequate caloric intake forces the body to prioritize essential metabolic functions at the expense of physical performance and learning outcomes. The protein–energy malnutrition framework suggests that when carbohydrate intake is insufficient, proteins are diverted from anabolic processes toward energy production, thereby undermining muscle development, immune function, and tissue repair. This mechanism was evident in the present study, where inadequate carbohydrate intake coincided with suboptimal protein utilization.
The significant micronutrient deficiencies – notably in calcium, vitamin D, folate, and iodine – can be interpreted through the life course theory of nutritional programming, which posits that nutritional inadequacies during adolescence, a critical developmental stage, may have long-term effects on bone density, metabolic resilience, and cognitive functioning. The lack of calcium and vitamin D is particularly concerning, as these nutrients are interdependent: vitamin D facilitates intestinal calcium absorption, and deficiency in both compounds accelerates risks of stunting, skeletal fragility, and later osteoporosis. This finding aligns with global literature, including WHO reports, which emphasize that insufficient intake of these nutrients in adolescence correlates with a heightened burden of musculoskeletal disorders in adulthood.
The overreliance on simple sugars and refined carbohydrates reflects broader socio-cultural dietary trends, often explained by the nutrition transition theory [29]. This framework highlights the global shift toward energy-dense, nutrient-poor diets rich in refined carbohydrates and processed foods, particularly in urbanizing regions such as Central Asia. The predominance of white bread and sweets, coupled with low consumption of fruits, vegetables, and fish, mirrors findings from studies in Eastern Europe and Central Asia, where accessibility, affordability, and cultural food preferences contribute to limited dietary diversity.
Psychological and behavioral theories also provide insight into the correlations observed between dietary habits and emotional or cognitive outcomes [30]. The biopsychosocial model of nutrition and mental health posits that nutrient availability, particularly of vitamins, minerals, and high-quality proteins, influences neurotransmitter synthesis and neural regulation. For example, the study’s finding that higher dairy intake correlated with improved concentration and mood stability supports evidence linking calcium, tryptophan, and bioactive peptides with serotonin regulation and reduced irritability. Similarly, greater intake of fruits, vegetables, and nuts was associated with reduced sugar consumption and enhanced stress resilience, echoing the diet-mood interaction theory, which emphasizes the protective role of phytochemicals, antioxidants, and omega-3 fatty acids in stabilizing emotional well-being.
At the macro level, the results resonate with the social determinants of health model, which explains nutritional disparities as outcomes of socioeconomic, cultural, and institutional factors. Adolescents in special medical groups may face compounded vulnerabilities: limited opportunities for physical activity, higher health-related stress, and reliance on readily available processed foods. This structural dimension helps explain why nutrient insufficiencies persist even when certain fortified products, such as iodized salt, are present in the diet.
Although certain antioxidants, such as vitamins B2 and B3, selenium, and manganese, remained within acceptable limits, the deficiency of multiple nutrients with pronounced antioxidant capacity, including vitamins A, C, B9, and E, underscores a pattern of polyhypovitaminosis. Such a broad spectrum of missing micronutrients threatens to curtail normal developmental processes, impair immune responses, and accelerate oxidative stress, ultimately undermining the physical and cognitive performance of affected adolescents.
The results demonstrate that adolescents in special medical groups exhibit a nutritional profile characterized by insufficient energy intake, inadequate consumption of proteins and complex carbohydrates, and widespread deficiencies in essential micronutrients such as calcium, vitamin D, folate, and iodine, accompanied by excessive intake of simple sugars and saturated fats. These imbalances not only threaten optimal growth and skeletal development but also have measurable associations with cognitive performance, emotional well-being, and long-term metabolic health. The findings underscore the urgent need for targeted nutritional interventions, including the promotion of balanced school meal programs, dietary education tailored to adolescents and their families, and broader public health initiatives to increase access to nutrient-rich foods. Future research should incorporate longitudinal and biochemical assessments to confirm causal pathways and explore the long-term effects of sustained nutrient inadequacy in this vulnerable group. By bridging empirical data with practical recommendations, this study provides a foundation for evidence-based strategies aimed at improving dietary habits and supporting the overall health and resilience of adolescents with medical limitations.
Based on the results obtained, several corrective measures for adolescents in special medical groups can be suggested. It is important to increase total caloric intake to align with age- and sex-specific requirements, as the current levels are substantially below recommended norms. The diet should emphasize complex carbohydrates (whole grains, legumes, and vegetables) to replace the excess of simple sugars and to ensure adequate fiber intake, which is critical for gastrointestinal health and stable energy supply. The proportion of animal fats should be reduced in favor of unsaturated vegetable fats, including sources such as vegetable oils, nuts, and seeds, while simultaneously minimizing foods high in saturated and trans fats. To address the widespread micronutrient deficiencies, the diet must be enriched with dairy products (for calcium), fatty fish and fortified foods (for vitamin D), fresh fruits and vegetables (for vitamins C, A, folate, and other antioxidants), and iodized salt to prevent iodine insufficiency.
Discussion
A comprehensive evaluation of the collected data reveals a complex interaction between poor dietary patterns and micronutrient deficiencies in adolescents assigned to special medical groups. The predominance of saturated fats and simple carbohydrates in their diets coincides with an insufficient intake of essential micronutrients, particularly calcium, vitamin D, and folate. These deficiencies raise significant concerns regarding their potential impact on skeletal development, metabolic stability, and neurological function. Moreover, an imbalanced macronutrient composition may further exacerbate micronutrient insufficiencies by limiting the diversity of nutrient-rich foods available in daily meals.
Another critical aspect is the observed deficiency in dietary fiber, which, combined with excessive intake of refined sugars, may contribute to glycemic instability. This imbalance could induce compensatory metabolic shifts, including increased reliance on protein catabolism for energy, potentially worsening protein and micronutrient shortages. As a result, these interconnected dietary inadequacies may not only compromise physical endurance but also affect cognitive performance and mood regulation. While direct causality could not be established, the simultaneous deficits in calcium, vitamin D, iron, and folate underscore the multifaceted nature of adolescent malnutrition. This issue is particularly pronounced in individuals with pre-existing medical conditions, further emphasizing the need for targeted nutritional interventions to mitigate long-term health risks.
The dietary imbalances identified in this study are shaped not only by individual choices but also by school nutrition and family eating practices. Schools strongly influence adolescents’ diets, and the lack of structured meal programs or the availability of low-nutrient snacks often reinforces unhealthy habits, such as high sugar intake and insufficient consumption of fruits, vegetables, and dairy [31], 32]. By contrast, evidence from international programs shows that balanced school meals and fortified products can significantly improve micronutrient status and reduce reliance on processed foods. Family factors are equally important, as food preferences and habits are formed within the household. Limited parental awareness of the link between nutrition and physical performance often results in reliance on high-fat and preservative-rich foods, while financial and time constraints encourage the use of inexpensive processed products. Conversely, families that prioritize balanced home-cooked meals, encourage dairy, fruits, vegetables, and fish, and model healthy behaviors contribute to improved nutritional outcomes.
The study revealed a clear caloric deficit, likely linked to irregular meal patterns and reliance on snacks or refined products over balanced meals. Adolescents often prioritize convenience and taste, mirroring global trends where skipping meals, especially breakfast, leads to lower energy intake and later dependence on calorie-dense foods [33]. Protein intake was below recommendations, especially from animal sources. While beef and horse meat were common, fish and poultry consumption was low, reflecting both cultural traditions and limited access. This contrasts with Western diets, where poultry and fish dominate adolescent protein intake. A consistent finding was the excessive consumption of simple sugars and refined carbohydrates, with white bread, sweets, and sweetened tea replacing whole grains and fiber-rich foods. This reflects the global “nutrition transition” but is amplified by local cultural habits.
Micronutrient deficiencies – particularly calcium, vitamin D, iodine, and folate – stem from low intake of dairy, fruits, and vegetables, combined with limited fortified foods [34], [35], [36]. Vitamin D deficiency is common worldwide in adolescents but is exacerbated here by low dietary sources. The calcium shortfall mirrors global evidence of reduced dairy consumption during adolescence, replaced by sweetened drinks. Gender differences were minor, with both sexes showing similar deficiencies, suggesting structural rather than individual causes. Compared with international data, these findings align with global patterns of high sugar and low fiber intake but also reveal regional specifics, such as the near absence of fish and unusually high copper intake, likely from red meat and organ foods.
Al Shaikh et al. [37] determined, using serum analyses, that 95.6 % of children had deficient or suboptimal vitamin D levels, with 64.2 % of obese participants displaying marked deficiency. Their findings also indicated that 21.5 % of children were overweight or obese. By contrast, the present work examined a special medical group and recorded a mean daily vitamin D intake of 1.73 ± 1.15 mcg for girls and 1.22 ± 1.74 mcg for boys, which approximates 17 and 12 %, respectively, of the 10 mcg reference value. Those markedly lower proportions may be connected to the smaller sample size of 162 adolescents with health deviations, whereas authors examined 3,613 children from various demographic backgrounds. An additional limitation in this research was reliance on a single cross-sectional measurement of serum 25(OH)D, without a multi-season approach to capture yearly fluctuations. Bacchetta et al. [38] recommended a daily vitamin D intake of 400–800 IU for children, implying 10 to 20 mcg. The present data revealed under 70 IU daily for girls and under 50 IU for boys, indicating intakes substantially lower than the recommended levels described by researchers. That consensus focused on expert-based guidance, rather than a population-based trial with measured dietary contributions to vitamin D status.
Miller [39] provided a global review of whole grain and fiber guidelines that differ markedly across regions. The present data noted deficits in daily fiber, with intakes averaging around 6.7–7.09 g for adolescent girls and boys, which is well below typical national and international recommendations exceeding 20 g. The Miller’s work showed that achieving such standards remains problematic in many countries, partly because of varying definitions for whole grains and the absence of uniform cut-offs for fiber. This situation parallels the findings that adolescents in special medical groups consumed insufficient fiber and micronutrient levels, potentially exacerbating nutritional risks.
Golloso-Gubat et al. [40] underscored the importance of dietary patterns: particularly traditional vs. Western diets, for modulating the gut microbiota in Filipino children. Their study indicated that higher fiber intake, especially from whole or complex carbohydrates, correlated with beneficial microbiota shifts, while lower fiber and increased fat intake tended to reduce microbial diversity. The present work identified an overreliance on saturated fats and limited consumption of fresh fruits and vegetables, reflecting a gradual shift away from more balanced traditional patterns. Comparisons to researchers work suggest that addressing these underlying dietary imbalances may prove pivotal for improving both gut health and overall functional capacity in adolescents.
Okuda et al. [41] reported a prevalence of functional constipation in Japanese adolescents that ranged from about 3.7 to 8.3 %, aligning with the lower boundary of the values observed in the present analysis. The study found that higher dietary fiber intake and increased water from foods were linked to fewer symptoms of constipation. Vegetables and fruits exerted a protective effect, though the significance was partly reduced after adjusting for total fiber. These findings resemble the current observation that a deficiency in fruit and vegetable consumption tends to coincide with a greater risk of suboptimal bowel patterns.
Ascaso et al. [42] investigated the iodine status of Spanish children aged 3 to 14 and noted that 37.8 % showed urinary iodine concentrations under 100 μg per liter, indicating mild to moderate deficiency. They additionally highlighted that only 59.5 % of families consumed iodized salt, yet iodine sufficiency generally remained within acceptable limits, mostly through dairy product consumption. The present dataset aligns with that pattern, confirming that suboptimal iodine intakes are more likely when neither iodized salt nor adequate daily servings of milk are included in a child’s routine diet. The importance of systematic access to iodized salt and consistent consumption of dairy products thus emerges as a shared theme across both studies, pointing to simple preventive strategies to avert nutrient deficiencies in pediatrics.
A multi-country European review Bath et al. [43] reported that, depending on the specific region and dataset, up to 80 % of adult women and 47 % of adult men fell below recommended dietary iodine intake levels. Meanwhile, another systematic investigation in a developing countries context complied by Khan et al. [44] documented that 37.8 % of studied children and adolescents had urinary iodine concentrations under 100 μg/L, signifying mild or moderate iodine deficiency. Comparing those findings to the present research, several parallels and disparities become evident. The European review highlighted that a substantial proportion of adolescents and adults fail to meet even the lower thresholds for iodine consumption, often linked to underuse of iodized salt, unawareness of iodine requirements, and a reliance on processed foods. Similarly, the developing-country sample found that more than one-third of participants were below 100 μg/L of urinary iodine, which closely matches the daily intakes of only 72–81 μg/day reported here, far below the 150 μg/day recommendation. This overlap indicates that, regardless of a nation’s economic status, inadequate iodine intake can persist if iodized salt policies are insufficient or if dietary patterns exclude key iodine sources (e.g., dairy or marine products).
According to European study, many adolescents in Europe experience two core problems: excessive simple sugars and saturated fats, and insufficient complex carbohydrates and dietary fiber. The present study shows a simple carbohydrate share of 17.3–17.7 % of total energy, nearly doubling the 10 % upper limit recommended by WHO, while dietary fiber stands at merely 6.7–7.09 g/day against a reference of 26–38 g/day. Meanwhile, the research from D.S.A. Khan et al. in a developing world context recorded similarly unbalanced eating, with only about one-third of daily calories derived from nutrient-dense meals, plus a notable shortfall in fruits and vegetables. In the present data, fewer than 30 % of adolescents consumed vegetables regularly, and around 20 % did so for fruit, intensifying the risk for micronutrient gaps. Such patterns mirror the “dual burden” phenomenon, where many are simultaneously calorie-deficient overall but reliant on “empty calories” for the bulk of their energy. The European review noted that around 50 % of adolescents in certain regions were missing recommended benchmarks for iron, calcium, and fat-soluble vitamins (A, D, E). The present findings similarly reveal shortfalls: calcium intake at roughly 470–500 mg/day (vs. 1,300 mg recommended), vitamin D at just 1.2–1.7 μg/day (vs. ≥10 μg recommended), and folate intake only 25–35 % of the target. The parallel patterns in also indicated frequent vitamin D and folate insufficiencies, especially in adolescents shifting to high-sugar, low-nutrient meals. This near-universal gap in micronutrient coverage suggests that new or revised interventions might be needed: not just iodized salt or fortification programs, but also dietary education focusing on plant-based diversity, quality proteins, and, for many, improved overall caloric adequacy.
Both the broader European data and the developing-world sample found direct correlations between poor nutrient intake and negative health indicators, such as suboptimal school performance, irritability, or immunological weaknesses. The present study substantiates these correlations by documenting that student with diets higher in dairy and nuts correlated with greater perceived energy (r=0.45, p<0.01) and lower irritability (r=0.45, p<0.02). Conversely, those with particularly low micronutrient or fiber intake exhibited increased fatigue and reduced academic engagement, reiterating the same synergy that and observed between nutritional adequacy and functional capacity in adolescents.
Across all referenced studies, a pronounced and systemic deficiency of essential micronutrients: including iodine, calcium, vitamin D, folate, and dietary fiber, was consistently observed, irrespective of geographic or socioeconomic context. The data indicate that both high-income and developing regions face widespread inadequacies, with adolescents frequently failing to meet dietary recommendations for key vitamins and minerals. This trend is compounded by excessive consumption of simple carbohydrates and saturated fats, further exacerbating metabolic imbalances. Despite regional differences in food availability and nutritional policies, the commonality of these deficiencies underscores the global nature of adolescent malnutrition, highlighting its direct impact on physical endurance, cognitive function, and long-term health outcomes.
Conclusions
The findings of this study demonstrate that adolescents in special medical groups exhibit pronounced nutritional imbalances characterized by excessive consumption of animal fats and rapidly digestible carbohydrates, combined with insufficient intake of complex carbohydrates, dietary fiber, and essential micronutrients. Deficiencies were identified across both fat-soluble vitamins (retinol, cholecalciferol, tocopherol) and water-soluble vitamins (thiamine, pyridoxine, folic acid, ascorbic acid), alongside markedly low levels of key minerals. These inadequacies, compounded by insufficient overall caloric intake and pre-existing health limitations, contribute to diminished physical performance, particularly in activities requiring endurance and flexibility.
The study highlights a limited level of awareness among adolescents regarding the direct relationship between diet and physical capacity, which results in insufficient motivation to make healthier food choices. A persistent reliance on high-fat, salty, and preservative-rich products not only fails to provide the necessary nutrients for growth and development but also creates cumulative risks for obesity, cardiovascular disease, and metabolic disorders later in life. These dietary preferences reflect both individual habits and broader socio-cultural factors, including the influence of peers, family eating traditions, and the widespread availability of inexpensive processed foods. The research contributes by providing a comprehensive picture of macro- and micronutrient intake in a vulnerable group, linking dietary inadequacies with functional outcomes. These findings highlight the need for targeted interventions such as school nutrition programs, family education, and policies to expand access to nutrient-rich foods. Future research should employ longitudinal and biochemical approaches, assess regional differences, and test intervention models to identify effective strategies for correcting deficiencies. Overall, the study underscores the importance of addressing adolescent nutrition as a determinant of long-term health and resilience.
A key limitation is the inability to correlate specific nutrient deficiencies with health or performance parameters. The study’s cross-sectional design and geographically limited sample reduce generalizability. Self-reported dietary recall may introduce bias, and seasonal data collection may not reflect year-round dietary patterns, necessitating further multi-seasonal research for greater accuracy.
Addressing the nutritional status of these adolescents is inherently multidisciplinary. Corrective strategies that target macro- and micronutrient deficiencies not only meet short-term educational objectives, but also form the basis for long-term health benefits. Ongoing monitoring of dietary habits, body composition, and micronutrient levels is crucial to tailor interventions that match the evolving metabolic and physiological needs of this population. Future investigations should explore the specific effects of customized meal plans and physical activity regimens on metabolic indicators, psychosocial outcomes, and overall readiness for higher education and professional pursuits.
Funding source: Science Committee of the Ministry of Science and Higher Education of the Republic of Kazakhstan
Award Identifier / Grant number: AP22685615
Acknowledgements
This research is funded by the Science Committee of the Ministry of Science and Higher Education of the Republic of Kazakhstan (Grant No. AP22685615).
-
Research ethics: We confirm that all the research meets ethical guidelines and adheres to the legal requirements of the study country. A study was approved by the local bioethics committee of the Astana Medical University, protocol No. 7, dated October 16, 2023.
-
Informed consent: Not applicable.
-
Author contributions: G.D.: Methodology, Conceptualization, Formal Analysis, Writing – Review & Editing, Writing – Original Draft Preparation. A.A.: Conceptualization, Methodology, Supervision, Project Administration, Writing – Original Draft Preparation, Writing – Review & Editing. S.I.: Software, Validation, Investigation, Writing – Review & Editing. D.I.: Methodology, Formal Analysis, Data Curation, Writing – Review & Editing. G.K.: Resources, Data Curation, Visualization, Writing – Review & Editing.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors declare that there is no conflict of interests.
-
Research funding: This research is funded by the Science Committee of the Ministry of Science and Higher Education of the Republic of Kazakhstan (Grant No. AP22685615).
-
Data availability: The authors confirm that the data supporting the findings of this study are available in the article.
References
1. United Nations Children’s Fund (UNICEF). Annual report 2023 Children’s well-being, education, and health in Kazakhstan. Kazakhstan: UNICEF; 2023. Available from: https://www.unicef.org/kazakhstan/media/11831/file/%D0%93%D0%BE%D0%B4%D0%BE%D0%B2%D0%BE%D0%B8%CC%86_%D0%BE%D1%82%D1%87%D0%B5%D1%82_2023_RUS.pdf.pdfSuche in Google Scholar
2. Kalmakova, ZA, Szh, S, Kispaev, TA. Physical activity and prevention of a sedentary lifestyle: methodological recommendations. Astana: National Center for Public Health; 2022.Suche in Google Scholar
3. Beisembayev, GB, Baubekova, GD, Tukbekova, BT, Tardzhibayeva, SK. Determinants of preschool children’s health from the perspective of developing a nutrition culture. Trends Sci Educ Dev 2021;78–1:9–13. https://doi.org/10.18411/trnio-10-2021-02.Suche in Google Scholar
4. Berezka, VO, Dyu, Z, Stepanova, GA. Motivational and value-based attitudes towards physical education among younger schoolchildren in the context of updated educational content. Phys Educ Sports Educ Syst Curr State Pros 2022:58–64.Suche in Google Scholar
5. Abdrakhmanova, SZ, Slazhnyova, TI, Adayeva, AA, Imasheva, BS, Aringazina, AM, Akimbaeva, AA, et al.. Anthropometric indicators of insufficient and excessive body weight among younger schoolchildren in the Republic of Kazakhstan. Sci Healthcare 2021;23:76–87. https://doi.org/10.34689/SH.2021.23.6.009.Suche in Google Scholar
6. Kalmakova, ZA, Abdrakhmanova, SZ, Adaeva, AA, Slazhneva, TI, Nazarova, SA, Raisova, KA, et al.. Lifestyle factors of Kazakhstani schoolchildren, their physical and mental health, and well-being: national report. Astana–Almaty: National Center for Public Health; 2023.Suche in Google Scholar
7. Sawicka-Gutaj, N, Gruszczyński, D, Guzik, P, Mostowska, A, Walkowiak, J. Publication ethics of human studies in the light of the Declaration of Helsinki–a mini-review. J Med Sci 2022;91:e700. https://doi.org/10.20883/medical.e700.Suche in Google Scholar
8. Bibbins-Domingo, K, Brubaker, L, Curfman, G. The 2024 revision to the Declaration of Helsinki: modern ethics for medical research. JAMA 2025;333:30–1. https://doi.org/10.1001/jama.2024.22530.Suche in Google Scholar PubMed
9. Ministry of Health of the Republic of Kazakhstan. Order No. KR DSM-175/2020: about approval of forms of accounting documentation in the field of health care and also instructions for their filling; 2020. Available from: https://cis-legislation.com/document.fwx?rgn=139077#.Suche in Google Scholar
10. Comerford, KB, Miller, GD, Boileau, AC, Masiello Schuette, SN, Giddens, JC, Brown, KA. Global review of dairy recommendations in food-based dietary guidelines. Front Nutr 2021;8:671999. https://doi.org/10.3389/fnut.2021.671999.Suche in Google Scholar PubMed PubMed Central
11. World Health Organization, Food and Agriculture Organization of the United Nations. Sustainable healthy diets: guiding principles; 2019. Available from: https://www.who.int/publications/i/item/9789241516648.Suche in Google Scholar
12. González-Estrada, E, Villaseñor, JA, Acosta-Pech, R. Shapiro-Wilk test for multivariate skew-normality. Comput Stat 2022;37:1985–2001. https://doi.org/10.1007/s00180-021-01188-y.Suche in Google Scholar
13. Lagerweij, M, Van Loveren, C. Sugar and dental caries. In: The Impact of Nutrition and Diet on Oral Health. Basel: S. Karger AG; 2020:68–76 pp.10.1159/000455373Suche in Google Scholar PubMed
14. Mahboobi, Z, Pakdaman, A, Yazdani, R, Azadbakht, L, Montazeri, A. Dietary free sugar and dental caries in children: a systematic review on longitudinal studies. Health Promot Perspect 2021;11:271–80. https://doi.org/10.34172/hpp.2021.35.Suche in Google Scholar PubMed PubMed Central
15. Bleiweiss-Sande, R, Chui, K, Wright, C, Amin, S, Anzman-Frasca, S, Sacheck, JM. Associations between food group intake, cognition, and academic achievement in elementary schoolchildren. Nutrients 2019;11:2722. https://doi.org/10.3390/nu11112722.Suche in Google Scholar PubMed PubMed Central
16. Jung, T, Huang, J, Eagan, L, Oldenburg, D. Influence of school-based nutrition education program on healthy eating literacy and healthy food choice among primary school children. Int J Health Promot Educ 2019;57:67–81. https://doi.org/10.1080/14635240.2018.1552177.Suche in Google Scholar
17. Kiani, AK, Dhuli, K, Donato, K, Aquilanti, B, Velluti, V, Matera, G, et al.. Main nutritional deficiencies. J Prev Med Hyg 2022;63:E93. https://doi.org/10.15167/2421-4248/jpmh2022.63.2S3.2752.Suche in Google Scholar PubMed PubMed Central
18. Order of the Chairman of the Committee for Sanitary and Epidemiologic Control of the Ministry of Health of the Republic of Kazakhstan No. 69-NK. Norms of physiological needs in energy and food substances for different population groups of the Republic of Kazakhstan; 2023. Available from: https://online.zakon.kz/Document/?doc_id=38710734.Suche in Google Scholar
19. Richter, M, Baerlocher, K, Bauer, JM, Elmadfa, I, Heseker, H, Leschik-Bonnet, E, et al.. Revised reference values for the intake of protein. Ann Nutr Metab 2019;74:242–50. https://doi.org/10.1159/000499374.Suche in Google Scholar PubMed PubMed Central
20. Burd, NA, McKenna, CF, Salvador, AF, Paulussen, KJ, Moore, DR. Dietary protein quantity, quality, and exercise are key to healthy living: a muscle-centric perspective across the lifespan. Front Nutr 2019;6:83. https://doi.org/10.3389/fnut.2019.00083.Suche in Google Scholar PubMed PubMed Central
21. Rong, S, Liao, Y, Zhou, J, Yang, W, Yang, Y. Comparison of dietary guidelines among 96 countries worldwide. Trends Food Sci Technol 2021;109:219–29. https://doi.org/10.1016/j.tifs.2021.01.009.Suche in Google Scholar
22. Ter, BS, Steenbergen, E, Milder, IE, Temme, EH. Evaluation of Nutri-Score in relation to dietary guidelines and food reformulation in The Netherlands. Nutrients 2021;13:4536. https://doi.org/10.3390/nu13124536.Suche in Google Scholar PubMed PubMed Central
23. WHO Scientific Update on trans fatty acids. 2024. Available from: https://www.who.int/ru/news-room/fact-sheets/detail/trans-fatSuche in Google Scholar
24. Pipoyan, D, Stepanyan, S, Stepanyan, S, Beglaryan, M, Costantini, L, Molinari, R, et al.. The effect of trans fatty acids on human health: regulation and consumption patterns. Foods 2021;10:2452. https://doi.org/10.3390/foods10102452.Suche in Google Scholar PubMed PubMed Central
25. Tulewicz-Marti, EM, Lewandowski, K, Rydzewska, G. Bone metabolism alteration in patients with inflammatory bowel disease. J Clin Med 2022;11:4138. https://doi.org/10.3390/jcm11144138.Suche in Google Scholar PubMed PubMed Central
26. Berezenko, VS, Mykhailiuk, HZ, Dyba, MB, Tkalik, OM, Krat, VV, Krechko, YV. Vitamin D supply in children with chronic viral hepatitis B. Mod Ped Ukr 2021;5:23–8. https://doi.org/10.15574/SP.2021.117.23.Suche in Google Scholar
27. Antipikin, Y, Berezenko, V, Dyba, M, Tkalik, E, Krat, V, Mikhailuk, K. Comparative assessment of the availability of vitamin D in children with chronic viral and autoimmune hepatitis. Paed East Eur 2019;7:181–91.Suche in Google Scholar
28. Tulewicz-Marti, E, Szwarc, P, Więcek, M, Lewandowski, K, Korcz, T, Cicha, M, et al.. Effect of intravenous iron administration on bone mineral and iron homeostasis in patients with inflammatory bowel disease—results of a prospective single-centre study. J Personalized Med 2023;13:458. https://doi.org/10.3390/jpm13030458.Suche in Google Scholar PubMed PubMed Central
29. Turmagambetova, AS, Sokolova, NS, Bogoyavlenskiy, AP, Berezin, VE, Lila, MA, Cheng, DM, et al.. New functionally-enhanced soy proteins as food ingredients with anti-viral activity. Virus (Tokyo) 2015;26:123–32. https://doi.org/10.1007/s13337-015-0268-6.Suche in Google Scholar PubMed PubMed Central
30. Estrada-Araoz, EG, Farfán-Latorre, M, Lavilla-Condori, WG, Avendaño-Cruz, CE, Quispe-Aquise, J, Yancachajlla-Quispe, LI, et al.. Mental health and life satisfaction in university students: a correlational study. Gac Med Caracas 2024;132:S125–33. https://doi.org/10.47307/GMC.2024.132.s1.17.Suche in Google Scholar
31. Pashova, S, Radev, R. Labeling of fresh fruits and vegetables. Qual Acc Succ 2021;22:148–52. Available from: https://www.researchgate.net/publication/350515216_Labeling_of_Fresh_Fruits_and_Vegetables.Suche in Google Scholar
32. Bogoyavlenskiy, A, Alexyuk, M, Alexyuk, P, Amanbayeva, M, Anarkulova, E, Imangazy, A, et al.. Metagenomic exploration of Koumiss from Kazakhstan. Microbio Res Announce 2022;11:e01082–21. https://doi.org/10.1128/mra.01082-21.Suche in Google Scholar PubMed PubMed Central
33. Astary, F, Indriasari, R, Hadju, V, Khuzaimah, A, Hidayanty, H, Bahar, B. Effect of multiple micronutrient supplements and nutritional education based on the “Aksi Bergizi” program on hemoglobin levels of adolescent girls. Gac Med Caracas 2024;132:665–73. https://doi.org/10.47307/GMC.2024.132.3.9.Suche in Google Scholar
34. Dmitrova, E, Smiyan, O, Holubnycha, V, Smiian, K, Bynda, T, Reznychenko, Y, et al.. State of immunity in preschoolers with acute respiratory viral infections associated with adenoid vegetations. Proceed Shevch Sci Soc Med Sci 2021;65:174–80. https://doi.org/10.25040/NTSH2021.02.17.Suche in Google Scholar
35. Serikbaeva, A, Tnymbaeva, B, Mardar, M, Tkachenko, N, Ibraimova, S, Uazhanova, R. Determining optimal process parameters for sprouting buckwheat as a base for a food seasoning of improved quality. East Eur J Enter Tech 2021;4:6–16. https://doi.org/10.15587/1729-4061.2021.237369.Suche in Google Scholar
36. Adamkulova, C, Zhakshylykova, K, Asanov, R, Akylbekova, N, Mambetkazieva, N. Dairy industry as a driver of economic growth. Sci Horiz 2025;28:70–83. https://doi.org/10.48077/scihor4.2025.70.Suche in Google Scholar
37. Al Shaikh, A, Aseri, K, Farahat, F, Abaalkhail, BA, Kaddam, I, Salih, Y, et al.. Prevalence of obesity and overweight among school-aged children in Saudi Arabia and its association with vitamin D status. Acta Bio Med Atenei Parmensis 2020;91:e2020133. https://doi.org/10.23750/abm.v91i4.10266.Suche in Google Scholar PubMed PubMed Central
38. Bacchetta, J, Edouard, T, Laverny, G, Bernardor, J, Bertholet-Thomas, A, Castanet, M, et al.. Vitamin D and calcium intakes in general pediatric populations: a French expert consensus paper. Arch Pediatr 2022;29:312–25. https://doi.org/10.1016/j.arcped.2022.02.008.Suche in Google Scholar PubMed
39. Miller, KB. Review of whole grain and dietary fiber recommendations and intake levels in different countries. Nutr Rev 2020;78:29–36. https://doi.org/10.1093/nutrit/nuz052.Suche in Google Scholar PubMed
40. Golloso-Gubat, MJ, Ducarmon, QR, Tan, RCA, Zwittink, RD, Kuijper, EJ, Nacis, JS, et al.. Gut microbiota and dietary intake of normal-weight and overweight Filipino children. Microorganisms 2020;8:1015. https://doi.org/10.3390/microorganisms8071015.Suche in Google Scholar PubMed PubMed Central
41. Okuda, M, Kunitsugu, I, Yoshitake, N, Sasaki, S. The relationship between functional constipation and dietary habits in school-age Japanese children. J Nutr Sci Vitaminol 2019;65:38–44. https://doi.org/10.3177/jnsv.65.38.Suche in Google Scholar PubMed
42. Ascaso, MTG, Pérez, PR, Alcol, EC, López, AL, de Lucas Collantes, C, Santos, IM, et al.. Nutritional status of iodine in children: when appropriateness relies on milk consumption and not adequate coverage of iodized salt in households. Clin Nutr ESPEN 2019;30:52–8. https://doi.org/10.1016/j.clnesp.2019.02.007.Suche in Google Scholar PubMed
43. Bath, SC, Verkaik-Kloosterman, J, Sabatier, M, Ter Borg, S, Eilander, A, Hora, K, et al.. A systematic review of iodine intake in children, adults, and pregnant women in Europe – comparison against dietary recommendations and evaluation of dietary iodine sources. Nutr Rev 2022;80:2154–77. https://doi.org/10.1093/nutrit/nuac032.Suche in Google Scholar PubMed PubMed Central
44. Khan, DSA, Das, JK, Zareen, S, Lassi, ZS, Salman, A, Raashid, M, et al.. Nutritional status and dietary intake of school-age children and early adolescents: systematic review in a developing country and lessons for the global perspective. Front Nutr 2022;8:739447. https://doi.org/10.3389/fnut.2021.739447.Suche in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

