Abstract
The current study provides a comprehensive analysis of the management and policy framework governing medical education in Germany, with a focus on aligning training programs with evolving societal needs and regulatory standards. Key areas of emphasis include medical training, admissions processes, residency programs, and continuing medical education, reflecting the dynamic interplay between technological advancements, policy reforms, and the demands of modern healthcare systems. Additionally, this study critically examines the structure, effectiveness, and inclusivity of Germany’s medical education programs, particularly their capacity to equip future healthcare professionals with the skills necessary to navigate the complexities of contemporary healthcare. The analysis highlights the importance of equitable admission and residency selection criteria in fostering diversity within the medical workforce, alongside the role of ongoing professional development in enhancing healthcare quality. Recommendations are proposed to refine curricula, integrate interdisciplinary approaches, and incorporate contemporary medical practices, ensuring that medical education remains responsive to current and future healthcare challenges. Our study offers valuable insights into the strengths and limitations of Germany’s medical education system, providing evidence-based policy suggestions for stakeholders committed to advancing educational outcomes and optimizing healthcare delivery.
Introduction
Germany’s medical education system operates within a dynamic framework shaped by technological advancements, policy reforms, and the evolving demands of modern healthcare. This study examines the structure and governance of medical training, admissions, residency programs, and continuing education, emphasizing their alignment with societal needs and regulatory standards. Lessons drawn from Germany’s successful practices can offer valuable insights for countries like China, where addressing multifaceted challenges in medical education is critical to strengthening healthcare systems. By evaluating Germany’s approaches to admissions equity, residency selection, interdisciplinary integration, and professional development, this analysis identifies strategies for enhancing educational outcomes. These include aligning theoretical knowledge with clinical practice, improving internship effectiveness, and ensuring sustainable resource allocation. The discussion underscores the importance of evidence-based reforms to meet international benchmarks and equip future healthcare professionals to navigate the complexities of global health demands effectively.
Medical education management and policy in Germany
Germany operates a “social health insurance-based, supplemented by private health insurance” system, characterized by the following features: (1) cost-sharing between employers and employees through payroll deductions; (2) social solidarity, with funds redistributed among different generations and groups; (3) a pay-as-you-go financing model; and (4) compulsory insurance alongside various group projects.
To become a physician in Germany, students must complete high school, undergo over six years of medical education, pass three national exams, and obtain a medical degree and license. Following this, they undergo training as assistant doctors in institutions such as university hospitals, ultimately becoming specialists.
The hierarchy among hospital doctors in Germany is well-defined. Trainee doctors, referred to as “Ärzte im Praktikum” (resident doctors), progress to junior physicians upon completing their training, which allows them to treat patients independently. As they gain experience, they may advance to senior doctors, who possess significant autonomy and are responsible for training junior doctors. The most senior physician in a clinical department oversees its management and fosters a competitive environment emphasizing seniority.
Germany faces a chronic shortage of doctors for several reasons: approximately one-third of medical students do not graduate annually. At the same time, doctors suffer from mental health impairments. Research by Unrath et al. [1] shows that around 23 % of primary care physicians in Germany have depression. Among those who do graduate, many pursue medical-related careers in research, administration, or private enterprises rather than clinical practice. Some graduates work part-time or seek better training or remuneration abroad. Better income and less working hours or pressure may be potential reasons [2]. In China, condition is a little bit different. The number of medical graduates and workforce experience a big rise from 2008 to 2018 [3]. The University of Heidelberg, established in 1386, was the first German university to include a medical school, and by 1474, it had implemented a six-year medical program that remains largely unchanged today [4]. The 18th century saw the German National Health Service mandate higher medical education and national examinations for physicians.
The six-year medical program comprises four stages:
Pre-clinical stage (1 year): This includes first aid training and two months of clinical nursing practice, culminating in a preparatory exam.
First clinical phase (2 years): Involves a four-month clinical internship and doctoral thesis work, concluding with a phased exam.
Second clinical phase (2 years): Features small-class teaching and a second clinical stage exam.
Internship (1 year): Consists of full-day hospital practice for at least 48 weeks, with mandatory courses in Internal Medicine and Surgery, plus 16 weeks of electives. Students must complete over 90 % of practical tasks and pass multiple exams, including oral and written assessments on patient history, diagnosis, treatment planning, and prognosis.
After graduation, students must undergo 18 months of full-time training in qualified institutions, including 12 months in non-surgical departments and six months in surgical departments, along with eight practical teaching activities [5].
In 2002, Germany introduced a new medical education policy [6], [7], [8]. Reports indicated that German medical education lagged behind European Union (EU) standards [9], 10], prompting further reforms. A significant change was the elimination of the 18 months of low-paid intern training (AiP) in 2004 [11], along with the shift from simple “pass” or “fail” grades to specific grading for internships and courses. Medical training in Germany involves the federal and state governments, along with professional bodies. Key federal institutions include the Federal Assembly, the Federal Council, and the Federal Ministry of Health, which oversees health policy, disease control, health insurance, and biotechnology. The Federal Ministry of Justice enacts laws related to physician training.
State governments implement health plans and services according to federal guidelines and collaborate with the Institut für medizinische und pharmazeutische Prüfungsfragen (IMPP), which manages undergraduate medical exams. Specific powers are delegated to autonomous community bodies, managing funding and compulsory membership under state government support. The German Medical Association (GMA) oversees education quality, reform, curriculum development, medical examinations, and simulated patient training [12]. Professional chambers for doctors and dentists, regulated by the state, handle continuing education and certification. The Higher Education Foundation coordinates medical specialty admissions, while the GMA ensures unified standards and liaises with upper management.
Germany hosts 36 public and 5 private medical schools (Figure 1). German universities are primarily funded by the government and taxes, with minimal changes over decades. Students pay only 50 to 90 Euros per semester for administrative fees and 50 to 200 Euros for public transport tickets [13]. Education loans offer up to 670 Euros per month to support students from disadvantaged families [14]. EU students and non-EU applicants meeting specific criteria (such as completing high school in Germany, having permanent residence, or having an EU spouse working in Germany) can apply directly through the University Application Service website and take the Nationwide Medical Admission Test (TMS) for better ranking. Non-EU students must apply via the International Student Services website, providing a TestAS score and other materials.
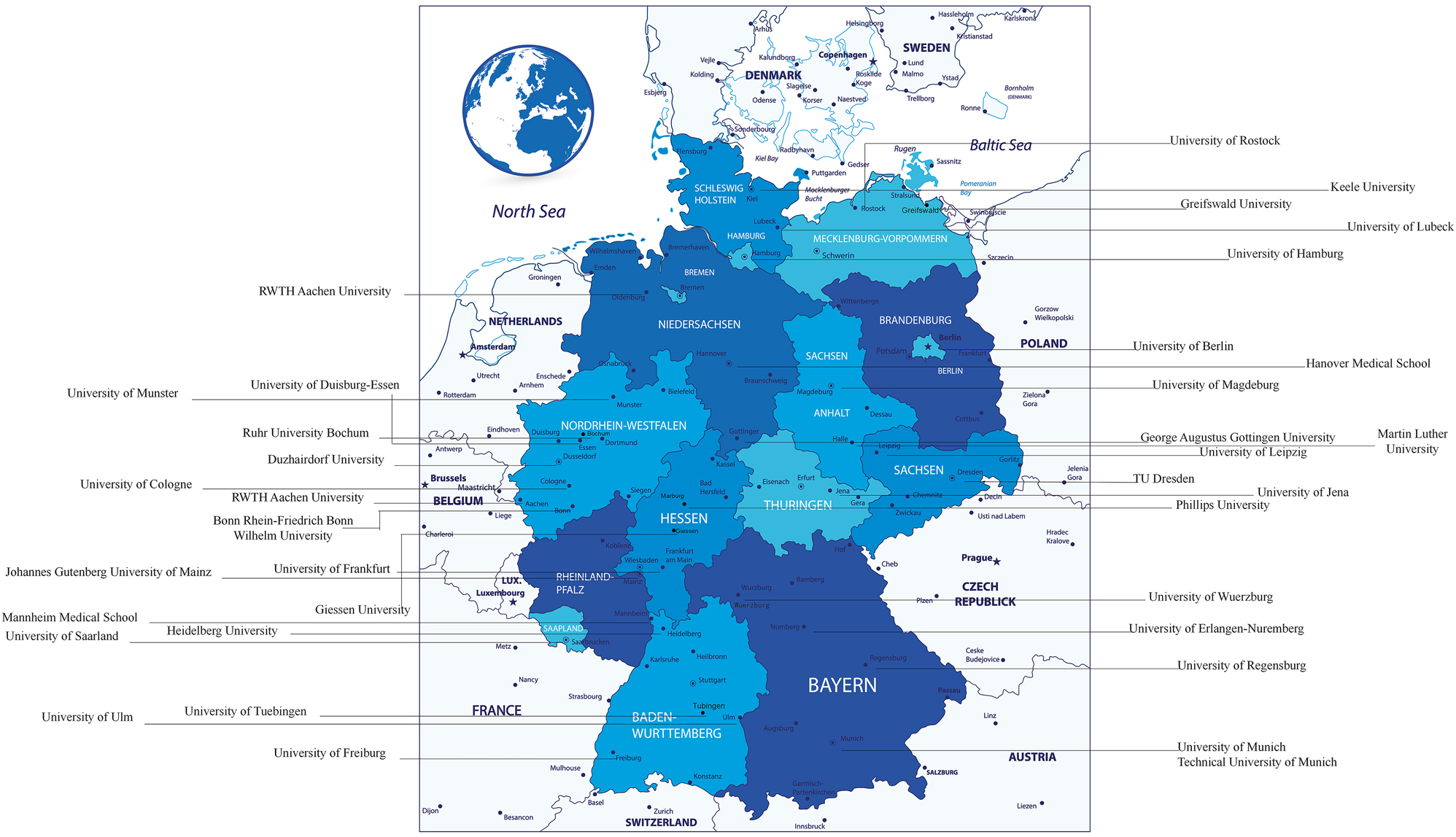
Directory of medical schools in Germany. (Map source: https://www.veer.com/illustration/167181753.html).
Medical examination system in Germany
To gain admission to a university in Germany, students must first obtain a certificate demonstrating their aptitude for higher education [15], which generally requires 12–13 years of study and is comparable to an advanced high school diploma. Although there is no strict age limit for medical school admission, the age of 40 is commonly perceived as the upper threshold [16]. Admission to medical programs is highly competitive, with only a small fraction of applicants succeeding. Selection is primarily based on a student’s Grade Point Average (GPA), which is calculated from their final high school grades, as well as performance in research and examinations.
High school graduates are permitted to select six universities for their applications. The higher education foundation allocates 9,000 medical school spots annually based on the following distribution: 20 % for applicants with the top GPAs in each state, 60 % for those accepted through internal procedures of medical schools, and 20 % for candidates based on their waiting semesters [15]. The admission process involves three rounds and is lengthy, with applicants typically notified in October. In recent years, medical schools have increasingly exercised autonomy in student selection, often utilizing self-cover letters and interviews [17]. However, this process can be time-consuming and constrained by limited staff resources. Additionally, the absence of standardized evaluation criteria has led some institutions to reintroduce the TMS [18]. The TMS is an optional annual examination designed for students from Germany and other EU countries that can enhance applicants’ grades and assesses scientific and medical comprehension. It does not test university-specific knowledge but focuses on skills such as comprehension, information extraction, signal processing, concentration, memory, and visual ability (Table 1). The points of every part are almost the same. The score of TMS will be a number between 70 and 130. It is calculated using a specific formula according to students’ ranking in a single TMS test and higher points refers to better grades (https://www.tms-info.org/ergebnis-und-auswertung/). Many medical schools prioritize TMS scores during the admissions process and students’ GPA can get improved at different extent when they apply for these schools. Some schools have quota called Zusätzliche Eignungsquote (ZEQ) which only consider TMS scores, performance in interview and special activity or training students have taken (https://www.studymed.de/medizinertest).
Introduction of Nationwide Medical Admission Test (TMS) examination content and process.
| Task | Number of questions | Time, min |
|---|---|---|
| Matching the whole complex image with its parts | 24 | 22 |
| Basic cognition of medicine and science (testing the ability to learn and understand the content of the given scientific material on the spot) | 24 | 60 |
| Hose graphics (spatial imagination) | 24 | 15 |
| Quantitative and form problems (ability to solve basic mathematical problems) | 24 | 60 |
| Concentration (according to the rule, mark a specific character among 1,600 characters under a time limit) | 1 | 8 |
| Break (1 h) | ||
| Memory test (memory stage) | ||
| Numerical memory (memorizing 20 numbers in 5 areas and the area where the numbers are located in 4 min) | 20 | 4 |
| Factual memory (memorizing 5 groups of facts, each group including the name, age, occupation, gender, other characteristics and other information of 3 patients) | 15 | 6 |
| Reading comprehension (medical or scientific text) | 24 | 60 |
| Memory test (recall stage) | ||
| Number recall | 20 | 5 |
| Fact recall | 20 | 7 |
| Charts and tables (ability to read charts on medical topics) | 24 | 60 |
TestAS is a standardized test designed for non-EU foreign students aspiring to study in Germany and these students have to pass TestAS to get the access to apply for universities in Germany. It consists of a core test covering fundamental areas such as calculation, language, numbers, graphics, and logic, as well as a professional thinking test tailored to the applicant’s chosen major. Students will get a rank in the percentage form and an average score of core test and professional thinking test (https://www.testas.de). For medical schools, the Math, Computer Science, and Natural Sciences (MINT) track is typically selected.
Before commencing clinical studies, students must pass a national examination with a score of 4 or higher on a scale from 1 to 5, where 1 represents the highest score. The first examination comprises both written and oral components (Table 2). The second examination is exclusively written, consisting of 320 multiple-choice questions administered over three days [19] (Table 3). The third examination is an oral assessment spanning two days, evaluating the candidate’s ability to handle patients independently.
Outline of the first national examination.
| Subject | Outline |
|---|---|
| Biophysics & physiology |
|
| Biochemistry & molecular biology |
|
| Anatomy |
|
Outline of the second national examination.
| Key point | Main examination method |
|---|---|
|
|
For international medical graduates to practice in Germany, the process varies depending on the country of their medical degree. EU physicians are required to obtain a license and membership in the regional medical association. Specialists must also possess certification that validates their training. The application process generally entails submitting necessary documents, completing examinations, and, in some cases, undertaking internships.
Medical education in colleges and universities in Germany
Upon completing approximately six years of study and passing all three state examinations, students may apply to the state medical association for a license to practice medicine and to obtain the title of “doctor,” provided they have successfully passed a medical examination and possess no criminal background. Many medical students opt to engage in research activities to obtain an academic doctorate in medicine, which is advantageous for future career advancement and patient attraction. Additionally, physicians interested in research and teaching may pursue postgraduate studies to earn a Master of Medical Education (MME), qualifying them for teaching positions in medical schools [20].
The German medical education program spans six years and is divided into two stages: a two-year preclinical basic stage followed by a four-year clinical stage. The final year of the clinical stage consists exclusively of departmental rotations, known as the internship year [21]. The preclinical basic stage requires students to complete fundamental science courses, utilizing three primary teaching methods: large lectures (voluntary participation), discussion classes (mandatory participation), and practical classes. After two years, students must complete first aid training, acquire 16 credits, and complete a mandatory three-month unpaid nursing internship before applying for the first national examination. However, graduates have evaluated the relevance of basic sciences in clinical practice as limited, prompting ongoing efforts from medical schools to enhance educational quality [22]. For example, medical schools can consider strengthening the clinical relevance of basic science courses, such as by introducing problem-based learning (PBL) and case discussions to link basic science knowledge with clinical practice and improve students’ practical application ability; designing the courses as interdisciplinary modules, highlighting the application scenarios of basic sciences in the clinic, and increasing the systematicity and relevance of teaching; or enhance the proportion of practical teaching and increase the number of laboratory courses and practice opportunities, such as arranging students to enter clinical environments in early courses to strengthen the connection between basic knowledge and practical work through observation and practice.
During the first three years of the clinical stage, students cover 21 specialized subjects. Traditionally taught in isolation, interdisciplinary modules that integrate various disciplines through a disease-centric approach have gained popularity, with approximately 14 such modules currently in use (Table S1). Assessment for these courses remains unchanged, with the first year of the clinical stage focusing on basic clinical knowledge and techniques. Historically, this knowledge was delivered through large lectures and discussions with minimal patient interaction. To improve clinical experience, mandatory clinical internships are required for courses in Internal Medicine, Surgery, Pediatrics, Obstetrics and Gynecology, and Family Medicine, each lasting from one to six weeks, along with a minimum of 476 h of bedside teaching, whereas the remaining other disciplines such as Ophthalmology, Osteopathic Medicine, and Pathology do not require mandatory internships [23]. It is worth noting that psychiatry, which is a mandatory internship in many countries, is not mandatory in German internships. Many medical schools have also established new laboratories for skill training [24]. Furthermore, students participate in a four-month rotating internship during winter and spring holidays, allowing autonomy in subject and location selection, although with an unclear syllabus. Students interested in subjects that do not require mandatory internships can still gain clinical practice in those areas during this stage.
Upon completing these educational components, students are eligible to take the second state examination after their fifth year. Recent years have seen a shift towards incorporating innovative simulations into the clinical stage of medical education, alongside student evaluations of the curriculum to enhance teaching quality. Some universities have fully transitioned to “model programs” (Table S1), where curricula encompass both theoretical knowledge and clinical skills from the outset and require all students to engage in research [25].
During the internship year, students assume greater responsibilities and perform many tasks typically handled by assistant nurses in other countries. Various initiatives are underway to improve teaching quality. In response to the increasing shortage of physicians in Germany, many teaching hospitals offer special allowances to students to encourage their retention for postgraduate training.
The internship year consists of three 16-week rotations in Internal Medicine, Surgery, and an optional subject. These rotations can occur in hospitals affiliated with the medical school or in other recognized medical institutions, including those abroad [26]. The choice of elective subjects depends on whether the hospital where the internship is conducted has the corresponding department and sufficient educational resources. If the hospital lacks the necessary resources, students may seek opportunities at other hospitals that can provide the required educational facilities. Recent changes to national medical licensing regulations now allow students to complete their final-year rotations at any accredited academic medical center across Germany. Other specifics are determined by individual medical schools based on their conditions. At the conclusion of the internship year, students will undertake the third state examination. Previously, all undergraduate courses and internships were graded simply as pass/fail; however, reforms now require specific grades on a scale from 1 (excellent) to 5 (fail). Some schools employ the Objective Structured Clinical Examination (OSCE) model to evaluate students’ skills, consisting of 18 stations presenting realistic clinical scenarios that candidates must complete sequentially, covering various bodily examinations and diseases. A summary of undergraduate medical education in Germany is provided in Table 4, while the summary of elective subjects is shown in Table S2.
Summary table of undergraduate medical education in Germany [4].
| Semester | Stage | Course | Internship |
|---|---|---|---|
| 1 | Preclinical basic stage | –Anatomy | –3-month nursing internship |
| –Histological | –First aid internship | ||
| 2 | –Biology | ||
| –Chemistry | |||
| 3 | –Biochemistry | ||
| –Physiological | |||
| 4 | –Social psychology | ||
| –Medical terminology | |||
| First national examination (physikum) | |||
| 5 | Clinical stage | –Anaesthesiology | Compulsory internship: |
| –Occupational medicine & social medicine | –Internal medicine | ||
| –Ophthalmology | –Surgery | ||
| –General medicine | –Paediatrics | ||
| 6 | –General surgery | –Obstetrics and gynaecology | |
| –Dermatology | –General medicine | ||
| –Obstetrics and gynaecology | Elective internship | ||
| –Otolaryngology | |||
| 7 | –Medical genetics | ||
| –Hygiene | |||
| –Microbiology & virology | |||
| –Internal medicine | |||
| 8 | –Paediatrics | ||
| –Orthopaedics | |||
| –Clinical chemistry & laboratory medicine | |||
| –Neurology | |||
| 9 | –Pathology | ||
| –Pharmacology & toxicology | |||
| –Psychiatry | |||
| –Psychosomatic medicine | |||
| 10 | –Forensic | ||
| –Urology | |||
| –Orthopaedics | |||
| –Elective courses | |||
| –Interdisciplinary modules | |||
| Second national examination | |||
| Last year | Clinical internship year | Internal medicine | |
| General surgery and (or) orthopaedics | |||
| Specialisation of the student’s own choice | |||
| Third national examination | |||
Postgraduation medical education
Students who opt to commence residency training in Germany must apply to qualified medical institutions, with residency training lasting at least 48–72 months. Residency programs can start at any time of the year, contingent upon available positions in the institution. Although standardized criteria govern the duration of training and remuneration, specific details are subject to negotiation between the resident and the institution, resulting in a lack of a clear written teaching schedule. Overall, residency training in Germany is characterized by its variability and flexibility.
The primary objective of postgraduation education is to prepare assistant physicians to specialize in a particular field of medicine (Table 5). The role of a physician assistant represents the initial stage of a physician’s career. After completing a medical degree and passing the national examination, medical graduates can apply to become physician assistants. The primary responsibility of a physician assistant is to undergo specialized training in a hospital or medical institution, preparing for a future role as a specialist. Physician assistants can transition into specialists after completing a residency in a relevant field and passing a specialty examination. Once they become specialists, they gain the ability to practice independently and enjoy greater professional autonomy. Residents are responsible for securing training positions in the labor market, and only experienced physicians may undertake postgraduate education. Throughout the training process, residents must diligently document the content and context of their training in a logbook, and an annual exchange with their supervisor is required. These discussions are also documented and submitted with the application for the Specialist Board of Medical Specialties Examination [27]. Residents are expected to participate in training on a full-time basis unless granted special permission. The average workweek across hospitals is 46 h, excluding night and weekend overtime, with residents studying various components of their specialty. Learning is competency-based, with minimal centralized activities and limited exposure to intensive care units in the first year. Residents may participate in interventional care, with opportunities contingent upon departmental requirements and staff availability.
List of majors.
| Majors | |
|---|---|
| 1. Family medicine | 14. Pediatrics |
| 2. Anesthesiology | 14.1. Pediatric hematology and oncology |
| 3. Anatomy | 14.2. Pediatric cardiology |
| 4. Occupational medicine | 14.3. Neonatology |
| 5. Ophthalmology | 14.4. Pediatric neurology |
| 6. Biochemistry | 15. Pediatric and adolescent psychology and psychotherapy |
| 7. Surgery | 16. Laboratory medicine |
| 7.1. General surgery | 17. Microbiology, virology and infectious diseases |
| 7.2. Vascular surgery | 18. Oral and maxillofacial surgery |
| 7.3. Cardiac surgery | 19. Neurosurgery |
| 7.4. Pediatric surgery | 20. Neurology |
| 7.5. Orthopedics and traumatology | 21. Nuclear medicine |
| 7.6. Cosmetic surgery | 22. Public health |
| 7.7. Thoracis surgery | 23. Pathology |
| 7.8. Visceral surgery | 23.1. Neuropathology |
| 8. Obstetrics and gynecology | 23.2. Pathology |
| 8.1. Gynecologic endocrinology and reproductive medicine | 24. Pharmacology |
| 8.2. Gynecologic oncology | 24.1. Clinical pharmacology |
| 8.3. Obstetrics and perinatal medicine | 24.2. Pharmacology & toxicology |
| 9. Ear, nose and throat surgery | 25. Physical therapy & rehabilitation medicine |
| 9.1. Ear, nose and throat medicine | 26. Physiology |
| 9.2. Speech disorders, vocal disorders and pediatric hearing disorders | 27. Forensic psychiatry |
| 10. Dermatology and venereology | 28. Psychosomatic medicine and psychotherapy |
| 11. Human genetics | 29. Radiation medicine |
| 12. Health and environmental medicine | 29.1. Pediatric radiology |
| 13. Internal medicine | 29.2. Neuroradiology |
| 13.1. Internal medicine | 30. Forensic medicine |
| 13.2. Vascular medicine | 31. Radiotherapy medicine |
| 13.3. Endocrinology and diabetology | 32. Blood transfusion medicine |
| 13.4. Gastroenterology | 33. Urology |
| 13.5. Hematology & oncology | |
| 13.6. Cardiology | |
| 13.7. Nephrology | |
| 13.8. Pulmonary medicine | |
| 13.9. Rheumatology | |
-
Source: specialty training regulations, revised 2015.
Specialty examinations are a minimum of 30 min and assess knowledge, experience, and skills, with certification granted within three months. Failure to pass the examination may necessitate an extension of the training period. Training undertaken in other regions may be validated as equivalent to German training if it meets the requisite criteria.
General practitioner specialist training, overseen by qualified physicians, spans five years, comprising three years in inpatient internal medicine (including 1.5 years of direct patient care) and two years in outpatient general medicine (including six months in surgery). Additionally, completion of an 80 h basic psychosomatic medicine program is mandatory. Surgeons complete two years of basic trunk training (including six months in the emergency department, six months in surgical intensive care, and twelve months in surgery, with an optional six months in outpatient care), followed by four years of specialized training. Internal Medicine physicians undergo three years of basic trunk training and two years of specialized training. Specialty training in fields such as Occupational Medicine, Radiotherapy Medicine, Microbiology, Virology and Infectious Diseases, and Forensic Medicine can take up to four years to complete.
Continuing medical education (CME)
The primary aim of CME is to maintain and enhance physicians’ professional competence to ensure high-quality medical care for patients. Essential learning content encompasses specialist and interdisciplinary knowledge, clinical practical skills, communication skills, and social competence. Physicians may select their preferred learning methods [28].
Various medical associations and organizations serve as the main supporters of CME in Germany. Both on-site classes and distance learning modalities are employed. CME credits are predominantly calculated based on the hours of participation in CME activities, as detailed in Table 6. Continuing medical education conducted abroad can be recognized upon submission of the relevant certificates, provided they comply with German regulations. Physicians are mandated to accumulate a specified number of CME credits regularly, with potential penalties for noncompliance, including fines or temporary revocation of their medical practice license [29]. A CME certificate is awarded upon earning a minimum of 250 credits within a five-year timeframe.
Methods of German continuing medical education (CME) score assignments.
| Forms of study | Scoring rules |
|---|---|
| A – reporting and discussion | 45 min – 1 credit Documented assessment of learning for each CME unit – 1 credit |
| B – meetings | Half day −3 credits |
| C – balint panels, seminars, peer reviews, case study sessions, etc. | Each CME unit – 1 credit Documented assessment of learning for each CME unit – 1 credit 4 h or more – 1 credit (maximum 2 credits per day) |
| D – paper or online learning | 45 min – 1 credit, learning assessment required |
| E – individual study of specialized literature, monographs, and instructional materials | Up to 50 credits in 5 years |
| F – publication of scientific papers or scientific monographs, scholarly reports | 5 credits per presentation Academic activities such as each academic presentation – 1 credit A maximum of 50 credits will be granted in this category over a period of 5 years |
| G – doing visits to doctors | 1 credit per hour Up to 8 credits per day |
| H – classroom learning specialty content | 45 min – 1 credit |
| I – online instructor training | 45 min – 1 credit If the online learning quality improvement evaluation criteria of the German physicians association are met, then 1 credit for every 45 min |
| K – blended learning model | 45 min – 1 credit If the online learning quality improvement evaluation criteria of the German physicians association are met, then 1 credit for every 45 min |
-
Source: regulations on continuing medical education, 2013.
In Germany, medical schools align teaching achievements with postdoctoral qualifications, offering various professional training programs. Notably, Baden-Württemberg provides a respected training method that meets international standards, leading to an official certification in higher medical pedagogy. The pinnacle qualification is the MME program, established in 2004. The highest attainable teaching faculty level is the postdoctoral teaching license (Habilitation), requiring a doctoral degree with professor qualification (Dr. habil.) or lecturer status (Privatdozent), with consistent standards across German universities [30]. There is an increasing emphasis on small class sizes, necessitating the involvement of residents and senior faculty in teaching, with Habilitation-qualified faculty responsible for training to uphold high educational standards for all medical students.
Discussion and conclusion
The United States has a strong focus on research-driven training and early exposure to clinical practice, while the United Kingdom emphasizes a more integrated approach, where students enter clinical training earlier in their education. These comparisons could provide valuable insights into best practices that China could consider adopting [31]. According to the 2022 China Health and Wellness Statistics Yearbook, the number of undergraduate medical students in Chinese universities increased from 230,000 in 2002 to 1.25 million in 2021, while the number of graduate medical students grew from 17,000 to 140,000 over the same period [32]. This rapid expansion, coupled with varying training models and excessively large enrollment at some institutions, has led to disparities in the quality of medical education across different schools. Limited clinical practice resources, including inadequate practical training hours, insufficient numbers of clinical teachers, outdated teaching equipment, and a lack of diverse teaching models, have further hindered the effectiveness of medical education. Additionally, the prevailing traditional, teacher-centered teaching methods, coupled with an overly broad curriculum, have failed to adequately foster critical thinking, clinical skills, and the development of students’ professional competencies. These challenges, including the insufficient focus on practical training and comprehensive student development, underscore the need for comprehensive reforms in China’s medical education system to better equip future healthcare professionals.
Enhancing the scientific planning and macro-control of medical school enrollment is crucial for optimizing the supply of healthcare professionals and improving training efficacy. In China, the current fragmentation in decision-making regarding medical education enrollment has led to a lack of clarity in defining a rational enrollment scale and establishing effective control measures. In contrast, Germany employs a centralized approach, with the Foundation for Higher Education overseeing the allocation of medical school seats nationwide. This system ensures equitable distribution based on state needs and projected healthcare demands. It’s important to consider the growing demand for healthcare professionals due to an aging population and rising health concerns, alongside the challenges of ensuring quality education amidst a high volume of applicants [33]. Additionally, disparities in medical education resources between urban and rural areas, as well as the need for reforms in curriculum and teaching methods to keep pace with advancements in medical science and technology, are significant challenges facing the system today [34]. While it is debatable whether China should adopt a similar model of precise control akin to that of Germany or the United Kingdom, the emphasis must shift towards evidence-based enrollment planning that evolves from a broad, less defined framework to a more nuanced, strategic management approach.
Furthermore, it is imperative to reform pedagogical methods to enhance the integration of foundational medical education with clinical practice. German medical schools emphasize contextualized learning, where modular courses focus on organ systems and physiological functions, thereby promoting the application of fundamental knowledge within clinical settings. In contrast, many Chinese medical institutions adhere to a traditional, compartmentalized teaching model that prioritizes theoretical knowledge over practical application. This disconnection undermines the educational process, as students may struggle to translate theoretical understanding into clinical competence. Modular teaching methods, as successfully implemented in Germany, could be introduced into Chinese traditional discipline-based medical education model by starting with pilot programs in select universities [35]. This shift could help integrate theory with practical skills, making education more adaptable to the evolving healthcare needs [36]. Therefore, an expedited reform towards an integrated curriculum aligned with international best practices is essential.
Moreover, improving the clinical practice system and its overall effectiveness is a pressing necessity. Germany’s successful measures – including economic incentives, structured assessment systems, and well-organized internship frameworks – serve as a model for enhancing the quality of clinical placements. In China, medical education follows the “5 + 3” model, comprising five years of undergraduate education and three years of standardized residency training. While this framework provides a structured pathway for developing medical professionals, challenges remain, particularly in the undergraduate phase. Clinical practice during the five-year undergraduate program is often limited to less than one year, which restricts students’ opportunities to apply theoretical knowledge in real-world settings. This insufficiency, compounded by various systemic issues, leads to suboptimal clinical training outcomes. Therefore, enhancing medical students’ clinical abilities during internships should be a priority. This can be achieved by fostering improved teaching proficiency among hospital clinicians and encouraging active student participation in patient diagnosis and treatment, thereby establishing a robust foundation for future residency training. To adapt Germany’s incentive measures and internship evaluation system to China’s specific circumstances, it is essential to consider the regional disparities in healthcare infrastructure and the varying levels of clinical exposure across different medical institutions [37]. China could establish a more standardized clinical practice evaluation system, ensuring that all medical students, regardless of their location, have access to high-quality training [38]. This would not only improve the quality of clinical training but also help address the shortage of healthcare providers in underserved regions [39].
Additionally, strengthening financial support for clinical practice is essential for advancing medical education quality. Historically, higher education institutions in China have received inadequate funding for clinical training, and the absence of standardized management regarding clinical practice fees has further exacerbated disparities. As the costs associated with internships continue to rise, schools face increasing challenges in maintaining quality teaching environments. Moreover, inconsistent and often arbitrary use of practice funds within teaching hospitals has led to outdated equipment and inadequate resources, which severely compromise the quality of clinical education. To address these challenges, it is imperative for China to allocate specialized financial resources for medical students’ practical training, thereby enhancing the compensation for clinical educators and mobilizing their engagement in teaching. Establishing uniform standards for clinical practice fees will also promote equity across institutions. Building on Germany’s successful approach to managing internship funding, China could implement a more structured funding model where hospitals receive government subsidies or incentives for hosting interns, thereby reducing the financial burden on healthcare institutions [40].
Addressing the shortage of medical students in Germany requires targeted strategies to attract and retain talent in the medical profession. National outreach campaigns can promote medical careers, particularly among underrepresented groups and in underserved regions, to diversify the talent pool. Financial incentives, such as scholarships or tuition reductions, should be offered to students who commit to working in areas with limited healthcare access. Additionally, increasing medical school capacities through enhanced funding for faculty and infrastructure can ensure a balanced supply of healthcare professionals while maintaining educational quality. Improving clinical practice in medical education necessitates a more structured and standardized framework. Developing comprehensive internship programs with clear objectives, adequate supervision, and regular evaluations can help address inconsistencies in clinical training. Teaching hospitals should receive increased funding to expand clinical placement opportunities and enhance training facilities. Incorporating advanced simulation technologies into medical education can complement hands-on clinical practice by allowing students to develop critical skills in a controlled environment, thus improving their readiness for real-world scenarios. Ensuring the quality of CME requires a nationally standardized accreditation system to maintain consistency across programs. Mandatory CME participation, tied to licensure renewal, can incentivize lifelong learning among healthcare professionals. Government and institutional subsidies can help alleviate the financial burden on participants. Emphasizing interdisciplinary training in CME programs fosters collaboration among healthcare professionals, enabling them to address complex medical challenges more effectively.
The German medical examination system can benefit from a balance between standardization and flexibility. While maintaining rigorous assessment standards, incorporating flexibility for diverse student backgrounds and learning paths can enhance inclusivity. Revising examinations to focus more on clinical competencies and problem-solving skills, alongside theoretical knowledge, can better prepare students for practical challenges in healthcare. In resident physician training, mentorship programs can provide residents with guidance and support from senior physicians, fostering both clinical and professional growth. Transitioning from time-based to competency-based training models allows residents to progress based on their demonstrated skills and knowledge, ensuring readiness for independent practice. Regular feedback mechanisms between residents and supervisors can help address weaknesses promptly and reinforce strengths. To improve continuing medical education, adopting digital platforms can make learning more accessible, especially for professionals in remote areas. Offering specialized CME tracks tailored to emerging medical fields and contemporary healthcare challenges ensures relevance to practitioners’ needs. Drawing from Germany’s strengths, such as its modular teaching methods, other medical education systems can benefit by adopting integrated, organ-system-based curricula. Additionally, incentivized regional deployment strategies and regular policy reviews can ensure that the education system adapts dynamically to technological advancements and workforce trends. By addressing these challenges and implementing these solutions, Germany’s medical education system can be further strengthened, producing highly skilled healthcare professionals equipped to meet the evolving demands of modern healthcare.
In conclusion, addressing the multifaceted challenges within medical education is vital for strengthening China’s healthcare system. By prioritizing scientific planning and macro-control of medical school enrollment, reforming pedagogical approaches to integrate theoretical knowledge with clinical practice, improving the effectiveness of clinical internships, and bolstering financial support for practical training, China can significantly enhance the quality of its medical education. Drawing lessons from the successful practices of countries like Germany may guide the reformative efforts toward achieving higher educational standards, improved training efficiency, and, ultimately, superior healthcare outcomes. By committing to these reforms and strategically investing in the necessary resources, China can cultivate a medical education system that aligns with international benchmarks, effectively equipping future healthcare professionals to meet the evolving demands of global health.
Funding source: The National Natural Science Foundation of China
Award Identifier / Grant number: No. 82301768
Funding source: International Joint Laboratory on Tropical Diseases Control in Greater Mekong Subregion
Award Identifier / Grant number: No. 21410750200
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: Conception and design: Yaqian Xu, Xiangwei Li; writing, review, and/or revision of the manuscript: Yaqian Xu, Yuqi Hao, Tiancheng Chen. All authors read and approved the final version of the manuscript.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors declare that they have no relevant financial interests.
-
Research funding: The National Natural Science Foundation of China (NO. 82301768) and International Joint Laboratory on Tropical Diseases Control in Greater Mekong Subregion (NO. 21410750200).
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Unrath, M, Zeeb, H, Letzel, S, Claus, M, Pinzon, LCE. The mental health of primary care physicians in Rhineland-Palatinate, Germany the prevalence of problems and identification of possible risk factors. Dtsch Arztebl Int 2012;109:201–7. https://doi.org/10.3238/arztebl.2012.0201.Suche in Google Scholar PubMed PubMed Central
2. Dettmer, S, Kuhlmey, A, Schulz, S. KARRIERE-UND LEBENSPLANUNG: Gehen oder bleiben? Dtsch Ärztebl 2010;Jg 107:A30–1.Suche in Google Scholar
3. Frenk, J, Chen, LC, Chandran, L, Groff, EOH, King, R, Meleis, A, et al.. Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet 2022;400:1539–56. https://doi.org/10.1016/s0140-6736(22)02092-x.Suche in Google Scholar PubMed PubMed Central
4. Chenot, JF. Undergraduate medical education in Germany. GMS Ger Med Sci 2009;7:Doc02. https://doi.org/10.3205/000061.Suche in Google Scholar PubMed PubMed Central
5. Zeng, J. Recent situation of higher medical education in Germany. Fudan Educ Forum 1994;2:55–9.Suche in Google Scholar
6. Health BfGGMo. Licensing regulation for doctors; 2003 [Online]. http://bundesrecht.juris.de/_appro_2002/index.html [Accessed 5 Oct 2024].Suche in Google Scholar
7. Justice BdJMo. Approbationsordnung für Ärzte-ÄApprO [Regulation of the licensing of doctors]; 2002 [Online]. https://www.gesetze-im-internet.de/_appro_2002/BJNR240500002.html [Accessed 5 Oct 2024].Suche in Google Scholar
8. Pabst, R. Medical education and reform initiatives in Germany. Acad Med 1995;70:1006–11. https://doi.org/10.1097/00001888-199511000-00019.Suche in Google Scholar PubMed
9. Fragen der Neuordnung des Medizinstudiums. Kurzfassung des Berichtes der Sachverst ändigengruppe beim Bundesminister für Gesundheit (März 1993). [Topics in revision of medical education: short report of the expert commission of the ministry of health (March 1993)]. Unfallchirurgie 1993;19:190–3.10.1007/BF02588044Suche in Google Scholar
10. Haage, H. Medical education in Germany: past successes and future challenges. An overview. Bund Gesundh Forsch 2006;49:325–9. https://doi.org/10.1007/s00103-006-1237-4.Suche in Google Scholar PubMed
11. Haage, H. Abolishment of the AiP. Transformation and further regulations. Bund Gesundh Forsch 2006;49:351–7. https://doi.org/10.1007/s00103-006-1236-5.Suche in Google Scholar PubMed
12. Gesellschat fur Medizinische. Ziele der GMA [Online] [2019-07-07]. https://gesellschaf-medizinische-ausbildung.org/gma/ziele.html [Accessed 5 Oct 2024].Suche in Google Scholar
13. Studienfinanzierung-Stiftungen bzwStipendien im Detail. Hamburg: oliver+Katrin lost GbR [Online] [2017-04-24]. https://www,studis-online,de/StudInfo/Studienfinanzierung/stipendien.php?seite=2 [Accessed 5 Oct 2024].Suche in Google Scholar
14. Bundesministerium für Bildung und Forschung. Bundesausbildungsförderungsgesetz-BAföG.Bonn [Online] [2017-04-20]. https://www.xn—bafg-7qa,de/de/bundesausbildungs-foerderungsgesetz-bafoeg-204.php [Accessed 5 Oct 2024].Suche in Google Scholar
15. Zavlin, D, Jubbal, KT, Noe, JG, Gansbacher, B. A comparison of medical education in Germany and the United States: from applying to medical school to the beginnings of residency. GMS Ger Med Sci 2017;15:Doc15. https://doi.org/10.3205/000256.Suche in Google Scholar PubMed PubMed Central
16. Hibbeler, B. Medizinstudium: 4, 8 Bewerber pro Studienplatz.Dtsch Arztebl. Dtsch Arztebl Int 2012;109:A-1674-A/B-1358/C-1338.Suche in Google Scholar
17. Waydhas, CHM, Nast-Kolb, D. Strukturierte lnterviews zur Studienplatzvergabe in der Medizin: Erste Erfahrungen (structured interviews of applicants at a medical school: first experiences). GMS Z Med Ausbild 2007;24:Doc186.Suche in Google Scholar
18. TMS. Test für Medizinische Studiengänge (test for medical education) [Online]. Heidelberg: TMS; 2008. http://www.tms-info.org [Accessed 5 Oct 2024].Suche in Google Scholar
19. lfmup, P. Informationen zu den schriftlichen Prüfungen Mainz: Institut für medizinische und pharmazeutische Prüfungsfragen [Online] [2017-04-22]. https://flexikon.doccheck.com/de/Institut_f%C3%BCr_medizinische_und_pharmazeutische_Pr%C3%BCfungsfragen [Accessed 5 Oct 2024].Suche in Google Scholar
20. Wissenschaftsrat. Empfehlungen zur Weiterentwicklung des Medizinstudiums in Deutschland auf Grundlage einer Bestandsaufnahme der humanmedizinischen Modellstudiengänge. Dresden; 2014 [Online] [2017-07-28]. https://www.wissenschaftsrat.de/download/archiv/4017-14.pdf [Accessed 5 Oct 2024].Suche in Google Scholar
21. Ludwig-Maximilians-Universität. Medizinstudium am Beispiel der LMU in München. München [Online] [2017-04-20]. http://www.unimuenchen.de/studium/studienangebot/studiengaenge/studienfaecher/medizin_1/staatsexam/index.html [Accessed 5 Oct 2024].Suche in Google Scholar
22. Strate, JRH, Pabst, R. Wie beurteilen Medizinstudenten das vorklinische Studium? Ergebnisse von Befragungennach dem 1.und 2. Stduienjahr [how do medical students judge preclinical studies? Results of questionnaire analysis after the first and second year of studies]. Dtsch Med Wochenschr 1998;123:1093–6. https://doi.org/10.1055/s-2007-1024129.Suche in Google Scholar PubMed
23. Zeuner, S, Henke, T, Achilles, E, Kampmeyer, D, Schwanitz, P. 36 different ways to study medicine. GMS Z Med Ausbild 2010;27:Doc20. https://doi.org/10.3205/zma000657.Suche in Google Scholar PubMed PubMed Central
24. Segarra, LMSA, Weih, M, Hahn, EG, Schmidt, A. Der Einsatz von medizinischen Trainingszentren für die Ausbildungzum Arzt in Deutschland, Österreich und der deutschsprachigen Schweiz [clinical skills labs in medical education in Germany, Austria and German Speaking Switzerland]. GMS Z Med Ausbild 2008;25:Doc80.Suche in Google Scholar
25. Gerst, TRKE. Medizinstudium: Wissenschaftsratempfiehlt Reform. Dtsch Ärztebl 2014;111:A–1280.Suche in Google Scholar
26. Ebrahimi-Fakhari, D, Agrawal, M, Wahlster, L. International electives in the final year of German medical school education--a student’s perspective. GMS Z Med Ausbild 2014;31:Doc26. https://doi.org/10.3205/zma000918.Suche in Google Scholar PubMed PubMed Central
27. Association, GM. (Model) Specialty training regulations 2003. Amended on 23/10/2015. https://www.dgthg.de/upload/download/MWBO_Englisch_.amended_23.10.2015.pdf [Accessed 5 Oct 2024].Suche in Google Scholar
28. Association, GM. (Model) Regulations on continuing medical education; 2013. https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/MFBO2013en.pdf [Accessed 5 Oct 2024].Suche in Google Scholar
29. Maisonneuve, H, Matillon, Y, Negri, A, Pallares, L, Vigneri, R, Young, HL. Continuing medical education and professional revalidation in Europe: five case examples. J Continuing Educ Health Prof 2009;29:58–62. https://doi.org/10.1002/chp.20007.Suche in Google Scholar PubMed
30. Weineck, SB, Koelblinger, D, Kiesslich, T. Medical habilitation in German-speaking countries. Quantitative assessment of content and elaboration of habilitation guidelines. Chirurg 2015;86:355–64.10.1007/s00104-014-2766-2Suche in Google Scholar PubMed
31. Stefanoyiannis, AP, Psichis, C, Gerogiannis, I, Christofides, S, Kaplanis, PA, Geronikola-Trapali, X, et al.. Education and training of medical physicists in europe and the countries of North America: similarities-differences-general guidelines. In: 11th international congress of the IUPESM/world congress on medical physics and biomedical engineering: 2009 Sep 07-12 2009. Munich, Germany; 2009:97–100 pp.10.1007/978-3-642-03893-8_28Suche in Google Scholar
32. China NHCotPsRo. 2022 China health and wellness statistics yearbook (in Chinese); 2023 [Online]. http://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/202305/6ef68aac6bd14c1eb9375e01a0faa1fb.shtml [Accessed 5 Dec 2024].Suche in Google Scholar
33. Ren, T, Li, M, Song, J, Qin, X, Wu, Y, Wang, T, et al.. Study on the current status of postgraduates training in public health and preventive medicine in China in 2016. Zhonghua Yufang Yixue Zazhi 2019;53:625–7. https://doi.org/10.3760/cma.j.issn.0253-9624.2019.06.016.Suche in Google Scholar PubMed
34. Li, D, Zhang, W, Wang, S, Lai, Y, Tao, Y. Comparative study of Medical Technology development in China and abroad. J Shanghai Jiaotong Univ, Med Sci 2021;41:1551–6.Suche in Google Scholar
35. Liu, R, Han, X. Research on the teaching of communication courses based on the Sub-type modular teaching approach. In: International seminar on education management and engineering: 2009 Jun 25 2009. Henan Province, Peoples R China; 2009:433–6 pp.Suche in Google Scholar
36. Askarova, MA, Kazez, E. Principles of teaching mathematics with modular technologies and their relationship with the basic principles of didactic teaching mathematics. Bull Kazakh Natl Pedagog Univ Phys Math 2013;26–33.Suche in Google Scholar
37. Murray, E, Gruppen, L, Catton, P, Hays, R, Woolliscroft, JO. The accountability of clinical education: its definition and assessment. Med Educ 2000;34:871–9. https://doi.org/10.1046/j.1365-2923.2000.00757.x.Suche in Google Scholar PubMed
38. Maria, S, Colbeck, M, Wilkinson-Stokes, M, Moon, A, Thomson, M, Ballard, J, et al.. Paramedic clinical practice guideline development in Australia and New Zealand: a qualitative descriptive analysis. Australas Emerg Care 2024;27:259–67. https://doi.org/10.1016/j.auec.2024.06.003.Suche in Google Scholar PubMed
39. Anderson, JL, Heidenreich, PA, Barnett, PG, Creager, MA, Fonarow, GC, Gibbons, RJ, et al.. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures a report of the American College of Cardiology/American heart association task force on performance measures and task force on practice guidelines. J Am Coll Cardiol 2014;63:2304–22. https://doi.org/10.1016/j.jacc.2014.03.016.Suche in Google Scholar PubMed
40. Ling, LJ, Meier, G. The medical education funding gap. One hospital’s perspective. Minn Med 2003;86:46–9.Suche in Google Scholar
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/gme-2024-0016).
© 2024 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


