Use of the Spencer Technique on Collegiate Baseball Players: Effect on Physical Performance and Self-Report Measures
-
Janine E. Curcio
Abstract
Context: Repeated overhead throwing in baseball players alters range of motion (ROM), contributing to shoulder injury. The Spencer technique has been used, anecdotally, to reduce the effects of throwing-induced limitations in ROM.
Objective: To quantify the effects of a single administration of the Spencer technique on the ROM and performance of collegiate baseball pitchers.
Methods: Pitchers from the Seton Hill University men’s baseball team were randomly assigned to 2 treatment groups: Spencer technique or sham therapy. The first week consisted of baseline outcome measurements (1 week before treatment), including ROM (flexion, extension, abduction, adduction, internal rotation, and external rotation) of the dominant throwing arm, 10 maximum velocity throws, and self-reported performance using the Kerlan-Jobe Orthopaedic Clinic Shoulder and Elbow Score (KJOC-SES). The second week consisted of pretreatment ROM measurement, followed by a single treatment and repeated measurement of all outcomes.
Results: Of 16 players, 15 met inclusion criteria. An effect of training on ROM between weeks 1 and 2 for all players consisted of significantly decreased internal rotation (P=.02) and increased external rotation (P=.04). A differential effect of treatment was found on the mean difference in internal rotation after treatment, compared with the mean difference before treatment on the same day (P=.01). Additionally, a trend toward statistical significance for abduction (P=.08) was noted. Analyses reveal that these effects were caused by significant increases in the internal rotation and abduction for the Spencer group only (P=.02). All other analyses of ROM, as well as performance measured by maximum velocity throws and the KJOC-SES, revealed no differential effect of treatment.
Conclusion: The results of this study support the use of the Spencer technique in counteracting the potentially negative effects of repeated throwing on internal rotation. However, a single administration did not affect functional ability in this study. Future studies of longer duration and including differing levels of play, injury status, and playing position will be needed to further evaluate the full potential of the Spencer technique in athletes who engage in repeated overhead arm movements.
Keywords: baseball, osteopathic manipulative treatment, shoulder injuries, Spencer technique, sports medicine
The upper body, specifically the shoulder, is the most frequently injured body region in high school,1 collegiate,2 and professional baseball players.3,4 Shoulder and elbow injuries are the leading causes of baseball players needing time away from the sport (≥21 days).4,5 Pitchers sustain most of their injuries to the upper body,3,4 spend the most days on the disabled list,3,4,6 and receive most of their injuries from noncontact mechanisms.1 Throwing in baseball causes the most injuries of the shoulder, with 59.5% of all shoulder injuries resulting from throwing and 73% of such injuries occurring in pitchers.5 Preventing and managing such injuries requires an understanding of the mechanisms by which both throwing activity and manipulation can alter the physiology and function of the shoulder joint. The literature, in general, provides a great deal of information on the possible effects of throwing on the shoulder. However, evidence for the impact of osteopathic manipulative treatment techniques in preventing or managing shoulder injuries is limited, to our knowledge.
The overhead throwing motion used in baseball is a dynamic activity that requires precision at exceptional velocities. A balance between mobility and functional stability of the shoulder must be achieved for movement to occur without injury.7 Even with technically sound motion, overuse injuries to the shoulder can arise from large forces and torques applied during sequential abduction, maximal external rotation, and maximal internal rotation.8-10 Internal rotation during a pitch is one of the fastest human movements recorded,11 and the maximum internal rotation torque during arm cocking and compressive force during arm deceleration are viewed as critical in overuse injuries of the shoulder.
One potential mechanism contributing to shoulder injuries in overhead-throwing athletes involves limitations in range of motion (ROM) of the glenohumeral joint. In baseball players, alterations in internal and external rotation have been reported in the throwing arm compared with the nonthrowing arm.12-18 Such changes illustrate an imbalance in the stabilizing musculature of the glenohumeral joint of the throwing arm, which may contribute to the development of conditions such as total rotational motion deficit or glenohumeral internal rotation deficit.15 Relative weakness of external rotators, in relation to internal rotators,19 as well as insufficient external rotation18 have been noted in professional pitchers. Overall, deficits may result from adaptive changes in bone,12-14,20 soft tissue,7,15,21 and sensorimotor acuity22 produced by repetitive overhead throwing. Studies have more specifically pointed toward humeral retroversion as an additional contributing factor in the development of rotational deficits.17,20 Although the specific contributions of each rotational motion remain debated, various studies have indicated a risk of injury with internal rotation, total rotational motion, or external rotation deficits23; therefore, alterations in ROM of the glenohumeral joint due to repetitive throwing are highly suspect in injury development.
Given that alterations in the function of the glenohumeral joint may contribute to injury, decreasing the deficits associated with this joint has become an area of focus to many researchers and clinicians. Manual interventions that strengthen or lengthen muscles (ie, muscle energy) can address these deficits.24 One particular osteopathic manipulative treatment technique that incorporates muscle energy is the Spencer technique. Originally developed by C. H. Spencer in 1916, the Spencer technique was used to manage nonsurgical soft tissue injuries by slowly stretching the shoulder while putting it through its normal range of motion.25 Modern use of the Spencer technique consists of a multistep process that typically uses muscle energy with postisometric contraction and relaxation to facilitate stretching and mobility of the entire shoulder, including the glenohumeral joint and rotator cuff.9 The Spencer technique is primarily used in the outpatient setting to improve functional ROM in patients with either shoulder pain or decreased ROM and subsequent identification of somatic dysfunction.26,27 This technique is also used by medical staff in professional baseball training rooms to enhance shoulder strength, motion, and throwing performance before practice and games (J.A. Tuck, DO, written communication, August 2016).
In general, use of muscle energy or long-term stretching protocols have been found to increase ROM of the glenohumeral joint in competitive baseball players.21,28 However, evidence describing the efficacy of the Spencer technique on pitchers is lacking. The present study aimed to quantify the effects of a single administration of the Spencer technique in healthy collegiate baseball players with respect to maintaining ROM of the glenohumeral joint and improving athletic performance.
Methods
Participants were recruited from pitchers on the 2015-2016 Seton Hill University men’s baseball team. To ensure that techniques were only administered on healthy shoulder joints, players were subject to selection criteria related to current and past injury. Current injuries to the shoulder excluded a player from the study. Past injuries to the shoulder, as well as current and past injuries to other body regions, were evaluated by a physician researcher (S.E.) to determine eligibility. Such injuries did not preclude participation as long as the players’ personal physician had cleared them to participate in sport-related activities. The physician researcher also monitored the use of the Apley scratch test, which examines external rotation, abduction, internal rotation, and adduction29 to identify gross ROM deficits that would preclude participation. All experimental methods were approved by the institutional review board at the Lake Erie College of Osteopathic Medicine and Seton Hill University. Measures were in place to reduce risk, and all participants provided signed informed consent before study involvement. Each participant was randomly assigned to receive a single administration of the Spencer technique or sham therapy to the dominant throwing arm.
The Spencer technique consisted of maintaining the shoulder joint into the restrictive barrier and creating isometric contraction of the muscles in each stage. This method has been thoroughly described in osteopathic texts and is part of standard osteopathic medical education.30,31 The isometric variety of the Spencer technique was used as described by DiGiovanna et al.30(pp444-447) The postisometric contraction replication steps consisted of 3 cycles of isometric contraction (at 3-5 lb subjective force) followed by a 2-second relaxation phase and subsequent movement of the joint to the new restrictive barrier.
The sham therapy was designed to simulate the Spencer technique without engaging restrictive barriers or activating muscle contractions. Similarities between the Spencer technique and sham therapy include participant positioning, clinician positioning, number of steps, stabilization of the shoulder, and hand placement. One student researcher was responsible for all administrations of the Spencer technique, and another student researcher administered the sham therapy. Administration of each technique was completed under the supervision of an osteopathic physician (S.E.).
Assessment
Outcome assessment consisted of measuring players’ physical performance and self-reported abilities. Physical measures included ROM and maximum velocity throwing (MVT), and self-reported ability was assessed using the previously validated Kerlan-Jobe Orthopaedic Clinic Shoulder and Elbow Score (KJOC-SES).32,33 Researchers measuring ROM, MVT, and KJOC-SES were blinded to the group assignment of each player.
The active ROM of the throwing arm was measured using a commercially available goniometer with bubble inclinometer, which limits measurement variability by ensuring appropriate placement of the goniometer arm relative to the ground. Goniometers may be used for the assessment of flexion, extension, abduction, adduction, internal rotation, and external rotation of the shoulder34 and have been used successfully in other studies that assessed ROM of the glenohumeral joint.7,13-15,21,35,36 As goniometry for shoulder measurements can be done effectively from either a seated or supine position,37 measurements were conducted with the player seated on the edge of a chair, with feet flat on the floor. Internal and external rotation was measured with the shoulder at 90º of abduction and elbow flexed to 90º. Two student researchers were involved in each ROM station; one stabilizing the scapula, while the other measured ROM and recorded results. All researchers measuring ROM received the same training and were monitored by a physician during each session. Players were measured at the same ROM station before and after treatment, and researchers were blinded to treatment.
Consistent with a previous study,38 the MVT session consisted of 10 overhand throws at the player’s maximal velocity. Each throw was restricted to a 1-step motion with normal follow-through. Throws were measured using the Seton Hill baseball team’s radar gun and immediately recorded by a single investigator. The average velocity of the 10-throw session was calculated and used for subsequent analysis. A previous study39 has suggested the potential for a short-term decrease in athletic performance after passive stretching during regular warm-up activities; this decline can be avoided using practice movements at a submaximum velocity before measuring maximum velocity.39 Because players engaged in stretching of the upper extremities during routine warm-up, each player performed 10 practice throws at a subjective 80% maximum velocity before MVT measurements.
In further assessing functional abilities, players completed the KJOC-SES, a 10-item self-report measure that asks players to rate their abilities during game and practice conditions from 1 to 10 by placing a mark along an answer spectrum that ranged from low to high level of performance.32,33 A score of 90 of 100 on the KJOC-SES is considered “normal” at the professional level.33 This method is considered superior to other self-report measures, such as the Disabilities of the Arm, Shoulders and Hand questionnaire and the American Shoulder and Elbow Surgeons standard assessment form, because of its ability to specifically quantify functional status in overhead-throwing athletes.40
Study Duration and Schedule
The study was conducted during winter training to allow for the most control of the study schedule and experimental variables (ie, limited travel and competitive play and consistency of training schedules). Each player participated in 1 baseline visit (1 week before treatment) plus a 20-minute study session 1 week later. A single treatment using muscle energy can produce immediate effects on ROM,28 and the effects of the Spencer technique on ROM in nonathletes have been shown to occur in 2 bursts, with the first burst starting immediately and beginning to plateau around 2 to 3 weeks.41 Accordingly, a 2-week study involving a single administration of the technique allowed for focus on the early effect of treatment.
The baseline visit consisted of (1) acquisition of informed consent; (2) completion of a prestudy questionnaire that addressed basic demographic information, involvement with baseball and other athletic activities, sports-related injuries and treatment, and current sports conditioning schedule; and (3) baseline measurements of ROM, MVT, and the KJOC-SES. The subsequent study session consisted of both pre- and posttreatment measurements of ROM. The MVT and KJOC-SES were completed once per session because repeated MVT sessions could have fatigued the arm, and KJOC-SES scores reflect global functioning for which changes would not be immediately evident during the study session.
The baseball team coaches and athletic trainers were consulted in the study design to ensure viability of procedures in conjunction with team training schedules. To avoid injury and ensure consistency with regular training and subsequent study procedures, each player underwent his normally scheduled warm-ups before exposure to any study procedures. Such activities included stretching, jogging and cardiovascular warm-ups, armband work, and warm-up throwing. The training schedule during the study consisted of conditioning and practice sessions 6 days per week, with players each having 1 maximum pitching day per week. To limit the potential effect of fatigue on measurements of MVT, study methods were conducted on the player’s maximum pitching day, after warm-up but before pitching practice.
Data Analysis
Initial data records were completed by hand for each of the measurement methods, ensuring that no identifying information was present on any paper form. Data from each of the forms was coded and compiled into a spreadsheet for later analysis. Basic descriptive measures were calculated in Microsoft Excel (Microsoft Corporation), and additional statistical tests were carried out using the statistical computing program R version 3.2.3 (R Foundation for Statistical Computing). Statistical analyses of differences between groups were completed using student t tests and Fisher exact tests, with the criterion for significance set at P<.05 (2-tailed).
Results
Of 16 players, 15 met inclusion criteria. The mean (SD) age was 20.1 (1.5) years. All players reported playing at the competitive level throughout both high school and college. Every player had participated in another sport at some point while playing competitive baseball. Two players, 1 from the Spencer group and 1 from the sham therapy group, reported current participation in another sport. These other activities were seasonal, with both players reporting participation in golf and one also participating in bowling. The Table provides additional player characteristics. No statistically significant differences were found between the treatment groups with respect to any of these characteristics (all P>.05). Although 2 players from the Spencer group and 5 from the sham therapy group had missed playing time in the past year because of a shoulder or elbow injury, all had been treated and were cleared for full participation at the time of the study. No players reported the development or treatment of any injuries during the study. Equipment malfunction occurred during the study session for 1 player. As such, the week-2 MVT and KJOC-SES data for this player were unavailable for analysis.
Demographic Characteristics of Collegiate Baseball Players by Treatment Group (N=15)a
| Characteristics | Spencer Technique Group (n=7) | Sham Therapy Group (n=8) |
|---|---|---|
| Age, y, mean (SD) | 20.1 (1.6) | 20.1 (1.5) |
| Hand Dominance | ||
| Left | 1 | 1 |
| Right | 6 | 7 |
| Throwing Shoulder | ||
| Left | 1 | 1 |
| Right | 6 | 7 |
| Missed Time for Shoulder or Elbow Injury in the Past Year | 2 | 5 |
| Average Height, cm, mean (SD) | 186.9 (4.8) | 190.8 (7.6) |
| Average Weight, kg, mean (SD) | 89.7 (7.5) | 92.4 (7.2) |
| Average Body Mass Index, mean (SD) | 25.7 (2.2) | 25.4 (2.3) |
| Class Year | ||
| Freshman | 2 | 1 |
| Sophomore | 1 | 3 |
| Junior | 2 | 3 |
| Senior | 2 | 1 |
| Previous Positions Played During Competitive Career | ||
| Catcher | 2 | 1 |
| Infield | 7 | 6 |
| Outfield | 3 | 5 |
a Data are given as number of participants unless otherwise indicated.
Range of Motion
Initial analyses involving ROM consisted of comparing the difference between the baseline measurements in week 1 with the pretreatment measurements from week 2 for all players combined. Given that no treatment was applied between these 2 measurements, this analysis allowed us to investigate changes in ROM from a week of training alone. A significant decrease in internal rotation (t14=2.53, P=.02) and increase in external rotation (t14=−2.25, P=.04) were noted (Figure 1). No significant differences were found in total rotational motion, flexion, extension, abduction, or adduction from week 1 to week 2 (all P>.05).
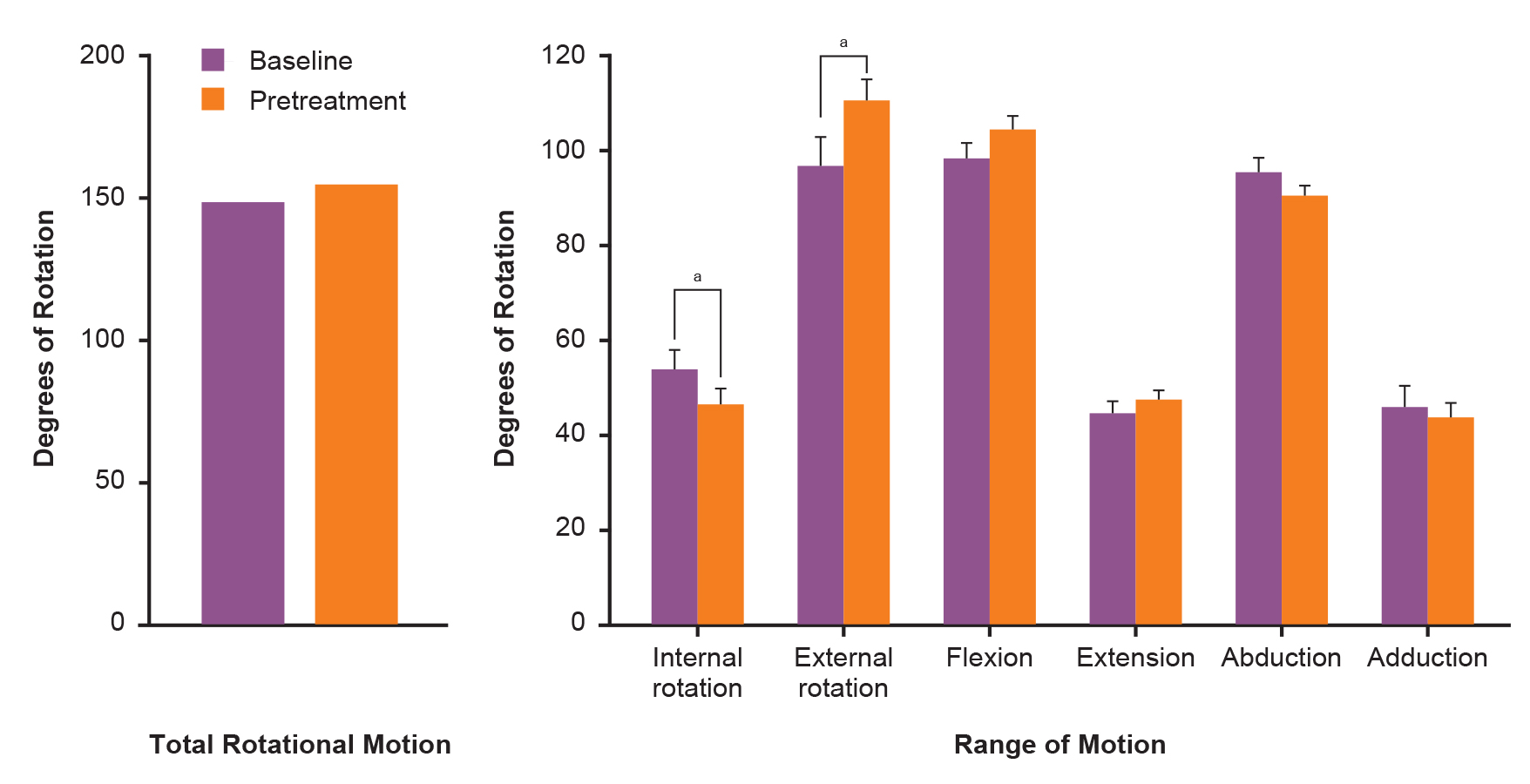
Effect of training on range of motion in collegiate baseball pitchers (N=15). Mean (SE) degrees of movement during week-1 baseline measurements and week-2 pretreatment measurements are illustrated for total rotational motion and range of motion. aP<.05.
Evaluation of the effect of treatment occurred in 2 stages: (1) evaluation of paired week-2 pre- vs posttreatment measurements for each treatment condition and (2) comparison of the mean difference between paired pre- and posttreatment ROM measurements as a function of treatment type. Significant differences were found between the paired pre- and posttreatment measurements of internal rotation (t6=3.24, P=.02) and abduction (t6=3.04, P=.02) in the Spencer group (Figure 2A), whereas no such differences were noted within the sham therapy group (Figure 2B). Figure 3 displays the mean paired difference (ie, posttreatment minus pretreatment) in ROM during week 2 for each condition. Analysis revealed a differential effect of treatment on the mean difference in ROM for internal rotation (t7=−3.11, P=.01) and a trend toward statistical significance for abduction (t7=−1.89, P=.08). No additional effects were reported for any other ROM measurement.
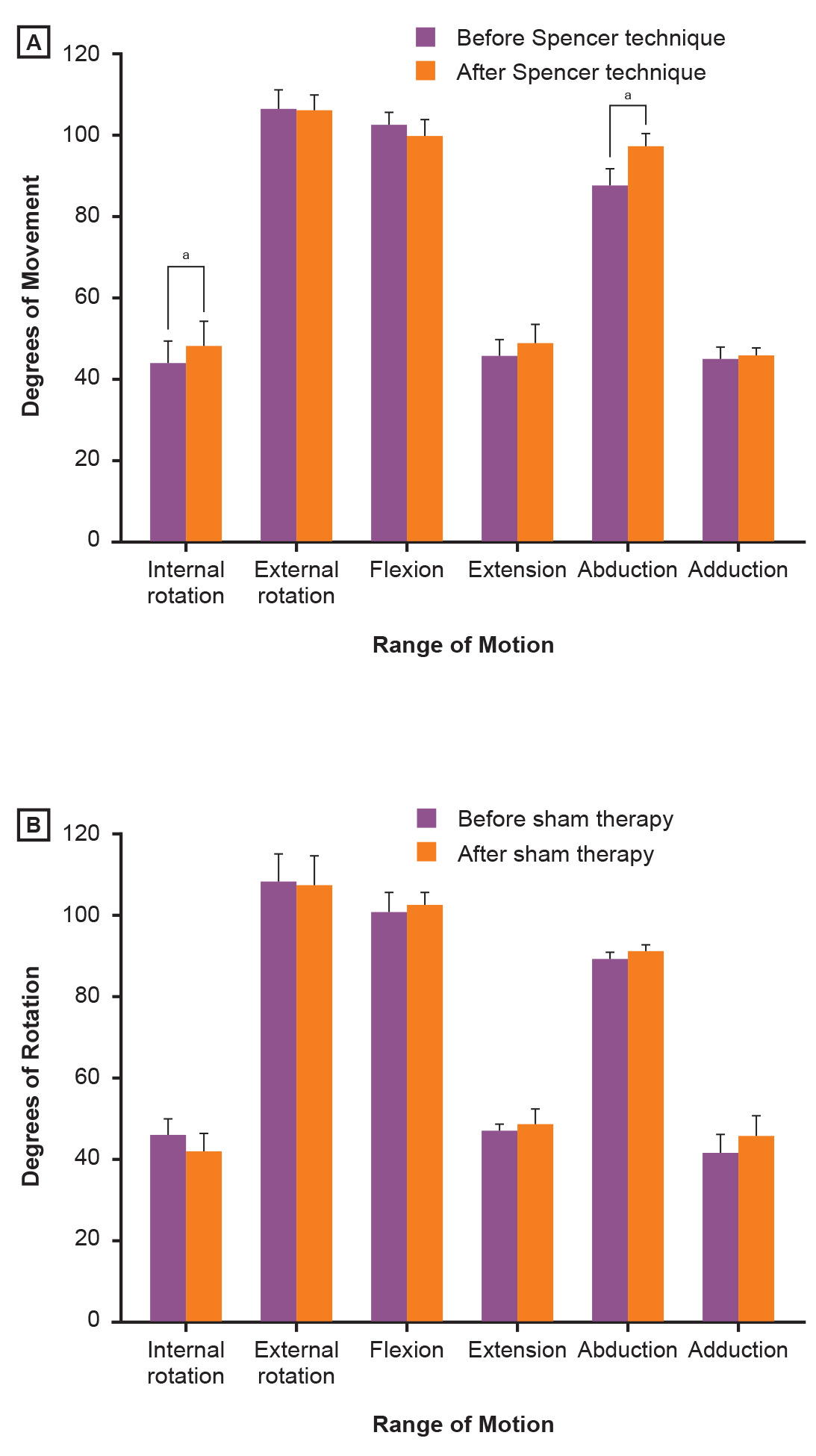
Effect of treatment on range of motion in collegiate baseball pitchers (N=15). Mean (SE) degrees of movement from week-2 pretreatment and posttreatment range of motion measurements are illustrated for (A) the Spencer group and (B) the sham therapy group. Significant changes in range of motion after treatment were noted for internal rotation and abduction of the Spencer group only. aP<.05.
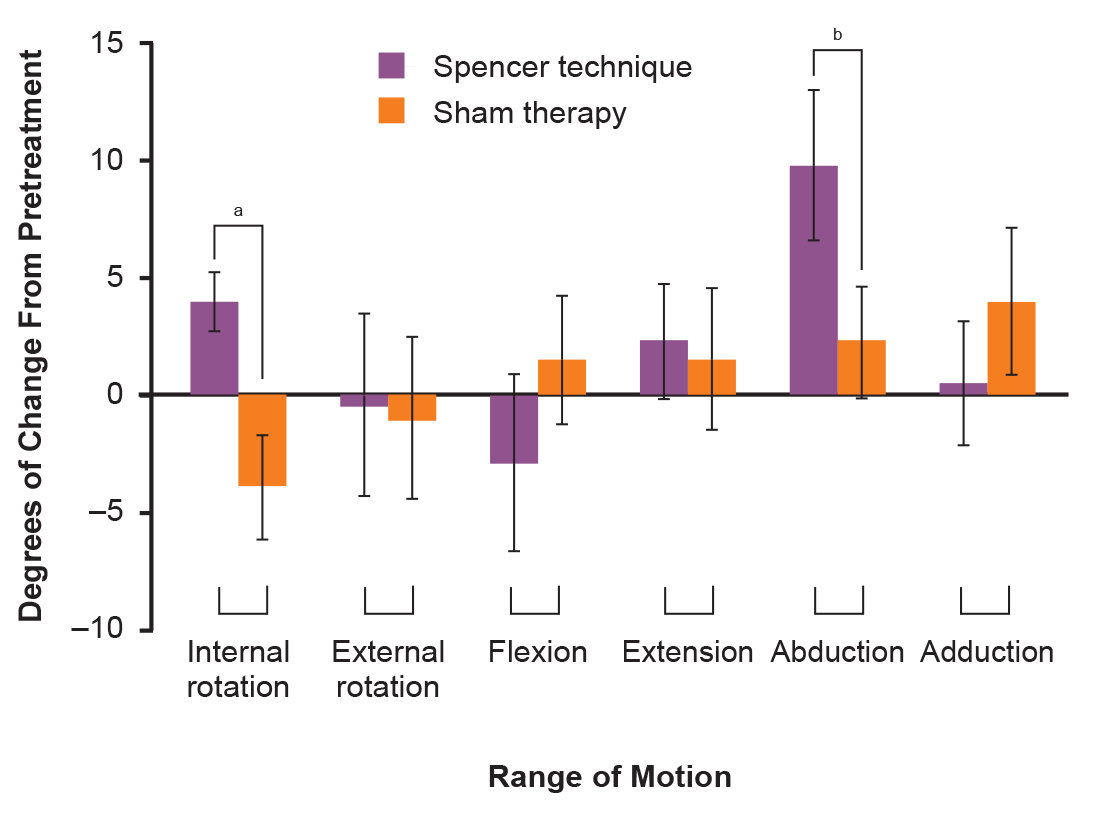
Effect of treatment on range of motion in collegiate baseball pitchers (N=15). The mean (SE) difference between paired pre- and posttreatment measurements for each group (ie, Spencer vs sham therapy). aP<.05. bP<.1.
Maximum Velocity Throwing
With respect to MVT, a significant difference in speed was found between paired week 1 and week 2 velocities for all players combined (t13=4.14, P=.001), as well as within each individual treatment condition (Spencer: t6=2.83, P=.03 vs sham: t6=2.79, P=.03). Speeds decreased similarly for both treatment groups, with the average speed decreasing by 2.81 mph in the Spencer group and 2.94 mph in the sham therapy group. No evidence was found for an effect of treatment with respect to the amount of change in velocity between week 1 and week 2 (t12=−0.09, P=.93).
Self-Report of Function
The mean (SE) KJOC-SES score for the sham therapy group was 83.90 (4.73) in week 1 and 81.70 (6.90) in week 2. For the Spencer group, the mean (SE) for week 1 was 92.21 (3.01) and 91.33 (3.57) in week 2. No significant difference was found between week 1 and week 2 measurements overall (t13=1.11, P=.29) or when separated by group (Spencer: t6=0.59, P=.58 vs sham: t6=0.90, P=.40). Additionally, no effect of treatment was reported in either week (week 1: t12=1.48, P=.16 vs week 2: t12=1.23, P=.24). Exploratory analyses revealed no strong relationships between the week 2 KJOC-SES and posttreatment MVT (Pearson r=0.43) or internal rotation (Pearson r=0.41). Of the 14 players for which both weeks of data were available, 6 were below 90 on at least 1 of the 2 days (3 from each treatment group).
Discussion
Repeated overhead throwing motions can alter the stability and flexibility of the glenohumeral joint,9,12-15 and studies specifically involving pitchers have reported increased external rotation and decreased internal rotation in the throwing arm.12-15 In concordance with the literature, the present study revealed increased external rotation and decreased internal rotation between week 1 and week 2 pretreatment measurements (Figure 1). The lack of diminished total rotational motion identified in the current study also lends support to previous literature indicating that similar levels of decreased internal rotation and increased external rotation can balance out total rotational motion,13,16 possibly limiting any appreciable differences in function or injury.23 As no treatment had been performed between the week-1 baseline and week-2 pretreatment measurements, the effects noted are considered to be those of training alone.
The purpose of the Spencer technique is to assist in returning the glenohumeral joint to its normal structural and functional balance by managing restrictions in ROM. Thus, we anticipated alterations in internal rotation to be in direct opposition of the observed training-induced effects. Our results confirmed this expectation, showing a differential effect of treatment on internal rotation. Specifically, internal rotation was statistically significantly increased after administration of the Spencer technique, whereas no such effect was found as a result of sham therapy. A trend toward a differential increase in abduction as a result of treatment was also found, with a statistically significant difference from pre- to posttreatment ROM being found in the Spencer group only. This additional finding is not surprising given that abduction is one of the movements for which large force is applied during overhead throwing8-10 and is also addressed by the Spencer technique.30,31 No such treatment effects were found with respect to external rotation, although training alone had altered this movement. Given that the goal of the Spencer treatment in the present study was to reduce diminished rotation created by repeated use of the throwing arm, the lack of effect on a rotation that had been previously increased by training is not entirely unexpected. However, as alterations in both strength and rotational motion of the external rotators have been implicated in overuse injuries18,19 and recognized as potentially beneficial in the prevention of injury,41 additional techniques focused on the assessment and alteration of the external rotators remain an important area for future investigation.
The differential effects on internal rotation found in the present study are proposed as a function of muscle relaxation and lengthening around the glenohumeral joint produced by the Spencer technique. In short, the Spencer technique involves the creation of isometric contraction of the muscles while maintaining the shoulder joint into the restrictive barrier. This contraction has historically been thought to activate the Golgi tendon apparatus of the agonist muscles, causing reflex inhibition of contraction and allowing muscle lengthening. Further promotion of lengthening may occur because of the creation of heat31 and temporary muscle fatigue30 that occur during contraction and relaxation. In the current study, players exposed to sham therapy were not actively resisting motion and, although motions toward the restrictive barrier were completed, care was taken to not engage this barrier. Thus, the Golgi tendon apparatus was not activated, heat was not generated, and muscular fatigue did not occur.
With respect to performance, no differential effect of treatment was reported in MVT or KJOC-SES scores. This finding is consistent with previous investigation of static stretching41 and other manipulation of the glenohumeral joint before throwing.38 Williams et al38 suggested that a reason for the lack of differential effect of treatment could be the complexity of the overhead throwing motion, which has the potential to be influenced by many factors. According to previous literature, restoring internal rotation may have the potential to affect injuries related to rotational imbalance.7,21 Although a single administration of the Spencer technique immediately increased internal rotation in the present study, our findings do not support the potential of this technique to immediately improve throwing ability. Additional factors that have the potential to explain these results include the short nature of the study and the fact that both the Spencer technique and KJOC-SES are generally reserved to assess and manage injuries.
One limitation of the present study is that we used a single manipulation of the glenohumeral joint. Future studies should examine the impact of repeated administration of the Spencer technique on structural and functional outcomes. Additionally, all players in the present study were healthy and medically cleared to participate in athletic activities, even though nearly half would have been considered to be functioning below full capacity because of KJOC-SES scores below 90.33 Of note, the study by Kraeutler et al33 was specific to professional baseball pitchers, and the current study focused on collegiate athletes. As such, it is possible that the normal range could be different between these 2 populations. Because the players in the present study were all healthy and asymptomatic, the low responses further highlight the importance of evaluating shoulder function before reported injury. Subsequent reevaluation after injury and treatment would assist in better understanding the differences between normal functional ability, injured ability, and recovery.
Future studies should investigate the impact of the Spencer technique on symptomatic players. Safety and feasibility studies within both asymptomatic and symptomatic populations, followed by well-designed randomized controlled trials and longitudinal follow-up, are necessary before claims regarding efficacy of the Spencer technique can be made. Such findings would be imperative in determining the potential of the Spencer technique to assist injured players in returning to normal sporting activities and prevent injury in noninjured players. Additionally, the present study is limited by size, and power analysis will be an important consideration for ensuring that an adequate number of pitchers are evaluated in future studies aiming to make claims on the efficacy of this technique.
Conclusion
The Spencer technique appeared to counteract the potentially detrimental effects of repeated throwing on the internal rotation of the glenohumeral joint in collegiate baseball players. Future studies of longer duration should allow for assessment of the long-term implications of treatment, including the potential for improved performance and decreased injury rates. Additionally, studies that investigate the safety and effectiveness of this method on returning players to the sport after injury are important. Taken together, studies of this nature will allow for a much more thorough understanding of the capabilities of the Spencer technique and its appropriate use in baseball players.
Author Contributions
All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
We acknowledge Kevin A. Thomas, DO, for his contributions to the development of the research project and critical analysis of the final manuscript. Additionally, we acknowledge Rachel M. Amador, OMS III; Marc A. Bozych, OMS III; Anthony J. Cocciolone, OMS III; Briana N. Kretz, OMS III; Kirsten J. Lederer, OMS III; Austin R. Oblack, OMS III; and Nancy Y. Xia, OMS III, for their participation in the data collection process.
References
1. Collins CL , ComstockRD. Epidemiological features of high school baseball injuries in the United States, 2005-2007. Pediatrics . 2008;121(6):1181-1187. doi:10.1542/peds.2007-257210.1542/peds.2007-2572Search in Google Scholar PubMed
2. McFarland EG , WasikM. Epidemiology of collegiate baseball injuries. Clin J Sport Med . 1998;8(1):10-13.10.1097/00042752-199801000-00003Search in Google Scholar PubMed
3. Posner M , CameronKL, WolfJM, Belmont PJ Jr, OwensBD. Epidemiology of major league baseball injuries. Am J Sports Med . 2011;39(8):1676-1680. doi:10.1177/036354651141170010.1177/0363546511411700Search in Google Scholar PubMed
4. Li X , ZhouH, WilliamsP, et al. The epidemiology of single season musculoskeletal injuries in professional baseball. Orthop Rev (Pavia) . 2013;5(1):e3. doi:10.4081/or.2013.e310.4081/or.2013.e3Search in Google Scholar PubMed PubMed Central
5. Dick R , SauersEL, AgelJ, et al. Descriptive epidemiology of collegiate men’s baseball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train . 2007;42(2):183-193.Search in Google Scholar
6. Conte S , RequaRK, GarrickJG. Disability days in major league baseball. Am J Sports Med . 2001;29(4):431-436.10.1177/03635465010290040801Search in Google Scholar PubMed
7. Wilk KE , MeisterK, AndrewsJR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med . 2002;30(1):136-151.10.1177/03635465020300011201Search in Google Scholar PubMed
8. Calabrese GJ. Pitching mechanics, revisited. Int J Sports Phys Ther . 2013;8(5):652-660.Search in Google Scholar
9. Kibler WB , WilkesT, SciasciaA. Mechanics and pathomechanics in the overhead athlete. Clin Sports Med . 2013;32(4):637-651. doi:10.1016/j.csm.2013.07.00310.1016/j.csm.2013.07.003Search in Google Scholar PubMed
10. Weber AE , KontaxisA, O’BrienSJ, BediA. The biomechanics of throwing: simplified and cogent. Sports Med Arthrosc . 2014;22(2):72-79. doi:10.1097/JSA.000000000000001910.1097/JSA.0000000000000019Search in Google Scholar PubMed
11. Fleisig GS , AndrewsJR, DillmanCJ, EscamillaRF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med . 1995;23(2):233-239.10.1177/036354659502300218Search in Google Scholar PubMed
12. Osbahr DC , CannonDL, SpeerKP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med . 2002;30(3):347-353.10.1177/03635465020300030801Search in Google Scholar PubMed
13. Reagan KM , MeisterK, HorodyskiMB, WernerDW, CarruthersC, WilkK. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med . 2002;30(3):354-360.10.1177/03635465020300030901Search in Google Scholar PubMed
14. Wilk KE , MacrinaLC, ArrigoC. Passive range of motion characteristics in the overhead baseball pitcher and their implications for rehabilitation. Clin Orthop Relat Res . 2012;470(6):1586-1594. doi:10.1007/s11999-012-2265-z10.1007/s11999-012-2265-zSearch in Google Scholar PubMed PubMed Central
15. Wilk KE , MacrinaLC, FleisigGS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med . 2011;39(2):329-335. doi:10.1177/036354651038422310.1177/0363546510384223Search in Google Scholar PubMed
16. Ellenbecker TS , RoetertEP, BailieDS, DaviesGJ, BrownSW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc . 2002;34(12):2052-2056.10.1097/00005768-200212000-00028Search in Google Scholar PubMed
17. Noonan TJ , ShanleyE, BaileyLB, et al. Professional pitchers with glenohumeral internal rotation deficit (GIRD) display greater humeral retrotorsion than pitchers without gird. Am J Sports Med . 2015;43(6):1448-1454. doi:10.1177/036354651557502010.1177/0363546515575020Search in Google Scholar PubMed
18. Wilk KE , MacrinaLC, FleisigGS, et al. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: a prospective study. Am J Sports Med . 2015;43(10):2379-2385. doi:10.1177/036354651559438010.1177/0363546515594380Search in Google Scholar PubMed
19. Byram IR , BushnellBD, DuggerK, CharronK, HarrellFEJr, NoonanTJ. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. Am J Sports Med . 2010;38(7):1375-1382. doi:10.1177/036354650936040410.1177/0363546509360404Search in Google Scholar PubMed
20. Chant CB , LitchfieldR, GriffinS, ThainLM. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther . 2007;37(9):514-520.10.2519/jospt.2007.2449Search in Google Scholar PubMed
21. Lintner D , MayolM, UzodinmaO, JonesR, LabossiereD. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sports Med . 2007;35(4):617-621.10.1177/0363546506296736Search in Google Scholar PubMed
22. Tripp BL , YochemEM, UhlTL. Recovery of upper extremity sensorimotor system acuity in baseball athletes after a throwing-fatigue protocol. J Athl Train . 2007;42(4):452-457.Search in Google Scholar
23. Manske R , WilkeKE, DaviesG, EllenbeckerT, ReinoldM. Glenohumeral motion deficits: friend or foe? Int J Sports Phys Ther . 2013;8(5):537-553.Search in Google Scholar
24. Goodridge JP. Muscle energy technique: definition, explanation, methods of procedure. J Am Osteopath Assoc . 1981;81(4):249-254.10.1515/jom-1981-811211Search in Google Scholar
25. Spencer CH. Shoulder technique. J Am Osteopath Assoc . 1916;15:218-220.Search in Google Scholar
26. D’Amato KE , RogersM. “Frozen shoulder” – a difficult clinical problem. Osteopath Fam Phys . 2012;4(3):72-80.10.1016/j.osfp.2011.12.001Search in Google Scholar
27. Patriquin DA. The evolution of the osteopathic manipulative technique: the Spencer technique. J Am Osteopath Assoc . 1992;92(9):1134-1146.10.7556/jaoa.1992.92.9.1134Search in Google Scholar
28. Moore SD , LaudnerKG, McLodaTA, ShafferMA. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther . 2011;41(6):400-407. doi:10.2519/jospt.2011.329210.2519/jospt.2011.3292Search in Google Scholar
29. Hoppenfeld S. Physical Examination of the Spine and Extremities . Upper Saddle River, NJ: Prentice Hall; 1976.Search in Google Scholar
30. DiGiovanna EL , SchiowitzS, DowlingDJ, eds. An Osteopathic Approach to Diagnosis and Treatment . 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.Search in Google Scholar
31. Nicholas AS , NicholasEA. Atlas of Osteopathic Techniques . 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.Search in Google Scholar
32. Alberta FG , ElAttrachNS, BissellS, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med . 2010;38(5):903-911. doi:10.1177/036354650935564210.1177/0363546509355642Search in Google Scholar
33. Kraeutler MJ , CiccottiMG, DodsonCC, FrederickRW, CammarotaB, CohenSB. Kerlan-Jobe Orthopaedic Clinic overhead athlete scores in asymptomatic professional baseball pitchers. J Shoulder Elbow Surg . 2013;22(3):329-332. doi:10.1016/j.jse.2012.02.01010.1016/j.jse.2012.02.010Search in Google Scholar
34. Norkin C , WhiteD. Measurement of Joint Motion: A Guide to Goniometry . 3rd ed. Philadelphia, PA: F.A. Davis Company; 2003.Search in Google Scholar
35. Aldridge R , GuffeyJS, WhiteheadMT, HeadP. The effects of a daily stretching protocol on passive glenohumeral internal rotation in overhead throwing collegiate athletes. Int J Sports Phys Ther . 2012;7(4):365-371.Search in Google Scholar
36. Freehill MT , EbelBG, ArcherKR, et al. Glenohumeral range of motion in major league pitchers: changes over the playing season. Sports Health . 2011;3(1):97-104.10.1177/1941738110374627Search in Google Scholar
37. Sabari JS , MaltzevI, LubarskyD, LiszkayE, HomelP. Goniometric assessment of shoulder range of motion: comparison of testing in supine and sitting positions. Arch Phys Med Rehabil . 1998;79(6):647-651.10.1016/S0003-9993(98)90038-7Search in Google Scholar
38. Williams M , HarvesonL, MeltonJ, DelobelA, PuenteduraEJ. The acute effects of upper extremity stretching on throwing velocity in baseball throwers. J Sports Med (Hindawi Publ Corp) . 2013;2013:481490. doi:10.1155/2013/48149010.1155/2013/481490Search in Google Scholar PubMed PubMed Central
39. Young WB , BehmDG. Effects of running, static stretching and practice jumps on explosive force production and jumping performance. J Sports Med Phys Fitness . 2003;43(1):21-27.Search in Google Scholar
40. Hegedus EJ , VidtME, TararaDT. The best combination of physical performance and self-report measures to capture function in three patient groups. Phys Ther Rev . 2014;19(3):196-203.10.1179/1743288X13Y.0000000121Search in Google Scholar
41. Knebl JA , ShoresJH, GamberRG, GrayWT, HerronKM. Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: a randomized, controlled trial. J Am Osteopath Assoc . 2002;102(7):387-396.Search in Google Scholar
42. Hurd WJ , KaufmanKR. Glenohumeral rotational motion and strength and baseball pitching biomechanics. J Athl Train . 2012;47(3):247-256. doi:10.4085/1062-6050-47.3.1010.4085/1062-6050-47.3.10Search in Google Scholar PubMed PubMed Central
43. Haag SJ , WrightGA, GilletteCM, GreanyJF. Effects of acute static stretching of the throwing shoulder on pitching performance of national collegiate athletic association division III baseball players. J Strength Cond Res . 2010;24(2):452-457. doi:10.1519/JSC.0b013e3181c06d9c10.1519/JSC.0b013e3181c06d9cSearch in Google Scholar PubMed
© 2017 American Osteopathic Association
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in the same Issue
- EDITORIAL
- History of Osteopathic Medicine: Still Relevant?
- STILL RELEVANT?
- Opening the Doors of Medicine to Women
- ORIGINAL CONTRIBUTION
- Predictors of Sunburn Risk Among Florida Residents
- Dermascope Use by Osteopathic Primary Care Physicians
- Use of the Spencer Technique on Collegiate Baseball Players: Effect on Physical Performance and Self-Report Measures
- MEDICAL EDUCATION
- Osteopathic Medical Student Practice of Osteopathic Manipulative Treatment During School Break
- SPECIAL COMMUNICATION
- A Qualitative, Interview-Based Study of the Health Policy Fellowship’s Osteopathic Identity
- CASE REPORT
- Gabapentin-Induced Bullous Pemphigoid
- Osteopathic Manipulative Treatment in the Management of Isaacs Syndrome
- CLINICAL IMAGES
- Recurrent Painful Calcium Pyrophosphate Arthropathy
Articles in the same Issue
- EDITORIAL
- History of Osteopathic Medicine: Still Relevant?
- STILL RELEVANT?
- Opening the Doors of Medicine to Women
- ORIGINAL CONTRIBUTION
- Predictors of Sunburn Risk Among Florida Residents
- Dermascope Use by Osteopathic Primary Care Physicians
- Use of the Spencer Technique on Collegiate Baseball Players: Effect on Physical Performance and Self-Report Measures
- MEDICAL EDUCATION
- Osteopathic Medical Student Practice of Osteopathic Manipulative Treatment During School Break
- SPECIAL COMMUNICATION
- A Qualitative, Interview-Based Study of the Health Policy Fellowship’s Osteopathic Identity
- CASE REPORT
- Gabapentin-Induced Bullous Pemphigoid
- Osteopathic Manipulative Treatment in the Management of Isaacs Syndrome
- CLINICAL IMAGES
- Recurrent Painful Calcium Pyrophosphate Arthropathy


