Growing Research Among Osteopathic Residents and Medical Students: A Consortium-Based Research Education Continuum Model
-
Grace D. Brannan
Abstract
In general, physicians’ interest in research continues to be a challenge. The lack of research culture is more pronounced in the osteopathic medical profession, which is historically not research oriented. With increasing focus on evidence-based medicine and with the single accreditation system for graduate medical education in motion, growing research and scholarly activities among osteopathic physicians and students and residents becomes imperative. This article illustrates how an educational consortium, such as an osteopathic postdoctoral training institution, can play a pivotal role in creating a culture of research through broad-based training of medical students and residents.
Expanding the number of physician scientists continues to be a challenge,1-3 and early exposure to medical research is crucial to continuously feed the physician-researcher pipeline.2 A dual-degree program, such as one that awards a DO or MD degree combined with a PhD or master’s degree (ie, MS or MPH), is a traditional and important pathway for research-focused undergraduate medical education; however, the dual degree caters to a small percentage of the medical student and resident populations. A continuum of training from medical school to residency has been proposed.3 Training students and residents increases the likelihood of having future clinical faculty and program directors with the necessary research skill sets to create a culture of research for future medical students and residents. However, residents must balance between tending to clinical duties and conducting research and may have limited interest in research or lack protected time, research skills, mentors, or adequate funding.4,5
To confound the physician-researchers’ challenge, the American Osteopathic Association (AOA), the American Association of Colleges of Osteopathic Medicine, and the Accreditation Council for Graduate Medical Education (ACGME) signed a memorandum of understanding in 2014 that outlined a single accreditation pathway for graduate medical education.6 The ACGME common and program-specific residency requirements emphasize research and scholarly work by both faculty and residents.7
The challenge of training physician researchers is more pronounced in the osteopathic medical profession, which is historically not research oriented.8 The disparate locations of the osteopathic medical schools and clinical training sites compound the issue. Community hospital–based training is the predominant model in osteopathic medical schools. Growing research among residents is a huge effort but can be done with the shared resources and efforts of a consortium. Osteopathic medical schools and community hospitals can form an osteopathic postdoctoral training institution (OPTI) to deliver the clinical training component of medical education for students and residents.4 The Ohio University Heritage College of Osteopathic Medicine (OU-HCOM) partners with 27 community hospitals around Ohio and with 6 colleges of osteopathic medicine across the nation to form an educational consortium known as the Centers for Osteopathic Research and Education (CORE).
The purpose of this article is to outline examples of how consortium-based shared resources and efforts can help grow a research culture during medical school and through residency and fellowship in addition to providing training and support for hospital-based clinical faculty. Because the tenure-track clinical faculty at OU-HCOM receive training and support from the Office of Research and Grants, they were not included as a target group. The CORE Research Office, which was established to provide a continuum of research education, training, and support to students, residents (including interns and fellows), and clinical faculty of the CORE consortium member community teaching hospitals in Ohio, is also described herein.
Research Challenges in Community Hospital–Based Training
The CORE consortium was established in 1995 to increase interest and engagement in research and to support a research culture among students and residents. In 1998, the CORE consortium designated a research committee to report directly to the leadership, which formally integrated research activities into the CORE system. An annual budget of $25,000 was allocated by the hospitals to directly support resident research projects through a competitive seed grant program and support travel reimbursement for dissemination activities. However, 3 challenges prevented full use of the research funding and interrupted the anticipated research growth: (1) the lack of medical residents’ research knowledge and skills, (2) inadequate support services, and (3) the lack of research mentors.
Research Knowledge and Skills
Although active research is conducted by tenure-track faculty at OU-HCOM, few studies have been conducted in the partner community hospitals in which education is provided by volunteer clinical faculty. Students may have engaged in research involving biomedical science in medical school, but there was a weak research infrastructure to nurture their interest in research once they transitioned to hospitals for clinical rotation and residency.
In my experience, unlike nonmedical scientists who are immersed in research training during graduate school, the majority of osteopathic clinical faculty and residents have little or no research experience and training, and few possess master’s or nonmedical doctorate degrees. Similar situations exist at the CORE OPTI and at other clinical training sites. Novice researchers may find developing a research idea or a full research proposal and applying statistical and research design concepts to the process to be difficult. The education of medical students and residents in basic research concepts fills a tremendous need for broad-based research education as a critical foundation to establishing and growing a culture of research.
Methodologic and Other Support Services
The CORE’s community hospital partners vary in size and resources. A few have access to limited research resources, and most have no access. Methodologists and statisticians are often not available to develop well-designed studies and analyze and interpret data, and hospital staff are not available to monitor research activity, gauge productivity, and oversee compliance. The lack of resources in these areas pose huge challenges and create barriers to the development of a research culture.
Training Physician Research Mentors
The AOA’s research requirements that focus on research conducted by residents instead of physician faculty contributes to an environment of diminished interest in research by potential mentors. In my experience at CORE, focusing requirements on mentors and residents rather than on residents alone provides a more longitudinal approach to creating a sustainable research culture. However, mentor research training depends on hospital resources and faculty interest. Although some physicians are involved in case reports and quality improvement projects, their efforts rarely reach the publication or dissemination stage. Training community-based physician mentors in research and developing their skills can help build the culture of research within the hospital and consortium.
The CORE Research Office Model: An Approach to Creating a Research Culture
In 2003, CORE established a research office through generous support from osteopathic foundations. The office comprises experienced researchers and methodologists and complements efforts by the OU-HCOM Office of Research and Grants, whose main focus is to help tenure-track faculty secure research grants. To add to the existing research mentors at OU-HCOM, the CORE Research Office nurtures budding research mentors, creates opportunities at the clinical sites, and facilitates those at other institutions.
Clinical Research Mentorship Triangle
The CORE Research Office complements and supports the work of physician mentors. A student or resident (implementer), physician mentor (clinical expert), and the research education office (methodologic experts and research mentors) make up a research triangle model (Figure 1). Through this collaborative approach, the research task is less daunting, and the clinical and methodologic soundness of the study is strengthened. The constraints and challenges discussed previously compelled the CORE Research Office’s decision to focus on growing the residents’ interest and skills in research while co-mentoring with physician faculty.
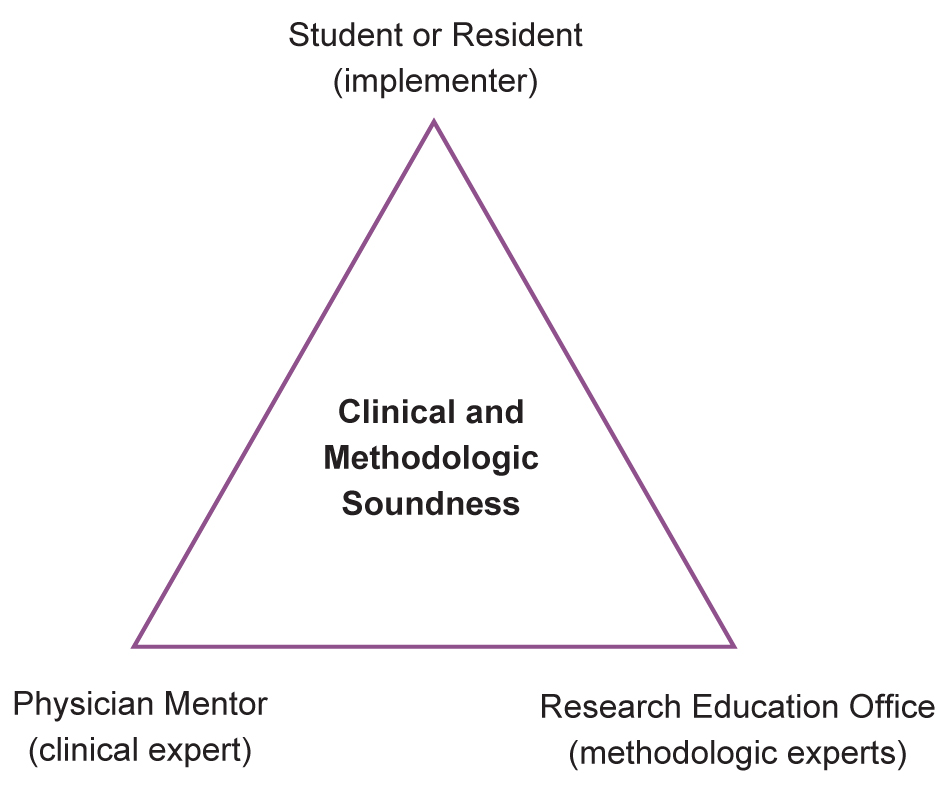
Clinical research mentorship triangle. The student or resident, physician mentor, and research education office collaborate to achieve clinical and methodologic soundness in research.
Seamless Education
Rivera et al4 discovered that residents find research skills to be important in achieving successful completion of a research project. However, “only 19% to 38% felt these skills are thoroughly taught at their residency program.”4(p367) On inception, the focus of the CORE Research Office was to work with third- and fourth-year students and residents at clinical sites. However, it is my experience that research education has to start with all first- and second-year medical students to provide a seamless transition to the clinical sites. The CORE Research Office has integrated research orientation and training into the student and resident curricula and conducts 1-on-1 consultations in person, electronically, and by phone. This model offers a continuum of customized research education, training, and support for all members of the CORE community—students, interns, residents, fellows, and CORE clinical faculty (Figure 2).
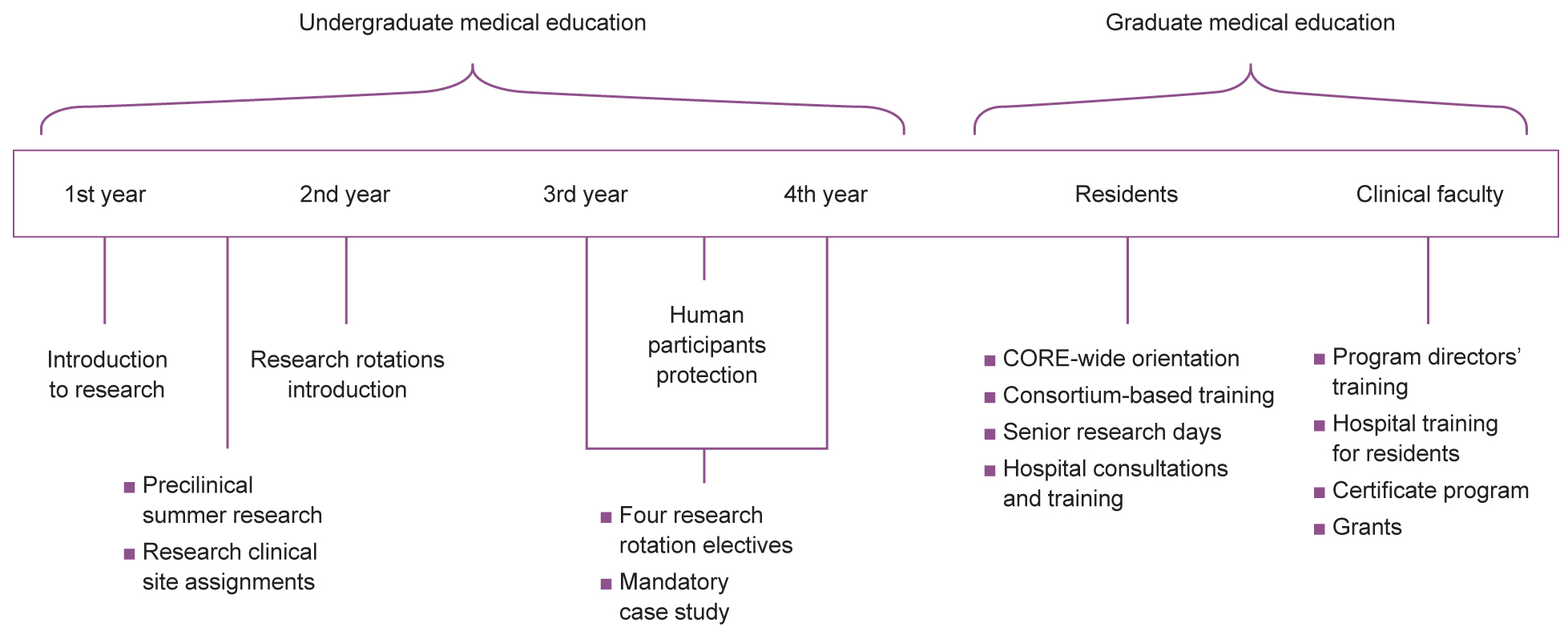
Timeline of research education and support at the Centers for Osteopathic Research and Education (CORE). Travel and seed funding was provided before the CORE Research Office was established, and 1-on-1 project assistance was provided after the CORE Research Office was established. Opportunities for students, residents, and faculty include Ohio Osteopathic Symposium regional and state poster competitions, publications, and CORE multisite studies; support includes an institutional review board liaison and project tracking.
Research Services
Providing funding for research projects and dissemination is not enough. The CORE Research Office collaborates with novice researchers to develop ideas, design studies, navigate the institutional review board process of assessing studies involving human participants, analyze statistics, interpret data, and offer editorial and dissemination support. Research opportunities are generated by providing project seed funding, partnering on projects, linking clinical mentors with medical students, and creating fellowships with external partners. The chance of approval during the first submission increases when the CORE Research Office’s team of experienced researchers scrutinizes a proposal. Although providing poster templates and editing assistance may seem elementary, this work often makes the difference in enabling researchers to disseminate their research. Travel funding is available to offset researchers’ expenses when presenting at conferences. These individual support services do not create a research culture, but weaving all of them together removes barriers and creates a strong support system on which to build well-designed, successful projects with a greater likelihood of dissemination.
Broad-Based Training
Every student, resident, and clinical faculty member should have hands-on experience in research and scholarly activities regardless of whether they are interested in a dual-degree program. The Centers for Osteopathic Research and Education equips residents with research experience through broad-based training with the goal of increasing the number of physician scientists. These efforts complement the dual-degree program and other research initiatives at OU-HCOM.
Database System
A critical piece in the CORE Research Office’s approach to research education is documentation. An online database was created to track research projects conducted at all levels. Students and residents register each research and scholarly work project with CORE by entering their contact information, mentors, affiliation, and research design in the database. Reports can be generated for administrative, gap analysis, accreditation inspection, and planning purposes. Reports are shared with partner hospitals and residency programs so that they can monitor their own research productivity. This reporting mechanism creates a level of accountability and contributes to the overall research culture growth. In addition, an electronic shared drive is used to house individual student and resident folders so that each member of the CORE staff can access documents as they provide assistance.
Lessons Learned
As with other OPTIs, when CORE started building a culture of research, few physicians at the clinical sites were interested, possibly because of the lack of research culture and because clinical faculty at hospitals are not required to do research by the AOA. Focus was turned to students and residents, and programs for current physician faculty were created. Some of the students and residents trained through CORE have now assumed program director and academic roles.
Successes
Over the past decade, CORE has seen unprecedented growth and development in research education, training, and activity (Table). Through internal surveys, research education was identified as one of the most recognizable and important programs within the consortium. The CORE Research Office has received commendations for exemplary efforts and support from osteopathic accrediting bodies at both the undergraduate and graduate levels.
Centers for Osteopathic Research and Education (CORE) Growth and Development in Research Activity
| Fiscal Yeara | ||||
|---|---|---|---|---|
| Research Outcomes | Before 2000-2001 | 2000-2001b to 2004-2005 | 2005-2006c to 2009-2010 | 2010-2011 to 2013-2014 |
| Registered projectsd | 3 | 196 | 710 | 838 |
| Posters | 0 | 6 | 78 | 445 |
| Peer-reviewed publications | 0 | 0 | 29 | 27 |
| Regional poster competition participants | NA | 0 | 132 | 319 |
a New CORE Research Office directors are hired at the start of the fiscal year.
b The CORE Research Office expanded.
c The annual mandatory amount of case reports (approximately 100) administered by the CORE Research Office is not included here.
d A small fraction of projects are collaborations and may be registered more than once.
Abbreviation: NA, not available.
Medical Students’ Research Education Program Growth
Research Orientation for Students
The CORE Research Office created orientation and training for all first- and second-year students to demonstrate the strong support and mentorship services provided by OU-HCOM. Since 2007, 100% of students have received research orientation and training. Ethics, proposal development, opportunities, and resources are some of the topics discussed.
Summer Preclinical Research
The CORE Research Office has assisted 57 first-year medical students since this program’s creation in 2010, with a 71% increase from 2012 to 2013. This success represents additional opportunities for early exposure to research.
Research Rotation Electives
Launched in 2005 and restructured in 2008, research rotation electives were created to provide protected time for students to conduct research for academic credit. The electives were expanded into 4 categories to better serve the specific needs of students: (1) introduction to research, 1 week; (2) case report, up to 3 weeks; (3) literature review, up to 3 weeks; and (4) retrospective, prospective, meta-analysis research, 3 to 12 weeks. Third- and fourth-year student research rotations have grown from 7 in the 2005-2006 school year to 19 in the 2012-2013 school year, with a total of 68 rotations since inception (a growth of 871%).
Residents’ Research Education Program Growth
Residents’ main goal is to meet or exceed their AOA specialty college’s research requirement. This consortium-wide objective has been met, and 100% of residents have received annual research orientation and training since 2009. Residents participate in program-specific “Annual Research Days,” in areas such as emergency medicine, orthopedics, obstetrics and gynecology, otolaryngology and head and neck surgery, internal medicine, and general surgery. Through CORE, about 5000 staff contact hours are provided to residents to support collaborative multisite and individual projects.
Across the Continuum Throughout Medical School and Residency
In addition to student- and resident-specific services, 1-on-1 project assistance and collaboration is offered. In addition, the CORE Research Office cosponsors an annual poster event with the Ohio Osteopathic Association, which started internally in 2006 with 6 participants. In 2014, the fourth Regional Ohio Osteopathic Symposium Poster Competition had national representation, with 104 abstracts submitted from 11 states, 11 hospitals, and 9 colleges of osteopathic medicine, which marked a 13% increase from the previous year. In addition, the CORE Research Office collaborates with hospital partners on hosting research days.
Sustainability
Over the years, the CORE Research Office has evolved from an office of 1 to a staff of 5 to provide the specialized skills necessary to accommodate the influx of the research and scholarly work of more than 500 students, 700 residents, and their clinical faculty mentors. After foundational grants were expended, the consortium’s board and OU-HCOM committed funding for operations and personnel to sustain the ongoing research education, training, and support for its medical residents. By pooling funds, they obtained quality shared research support services that none could sustain independently. An independent business consultant compared the CORE Research Office’s service rates with industry and other academic institutions and found that consortium institutions were saving around 60% in cost by sharing research resources and services. The report indicated that the value of the CORE Research Office is not only in the statistical support it provides, but it is also in the quality of the research education and contribution to the college’s mission.
Conclusion
Future challenges include building a cadre of clinical mentors and creating focused research at the community hospitals. For some mentors, that could include research training and increasing confidence in scholarly writing, as many do not receive formal training or instruction in this process.9 The Centers for Osteopathic Research and Education continues to expand programming to include quality improvement initiatives at the hospitals to tightly link research and scholarly efforts with hospital goals and patient needs. It is also working closely with clinical faculty in understanding and operationalizing ACGME requirements.
Acknowledgment
I thank Karen Collins, MPA, for editorial assistance and Cara Acksel, MS, for literature review assistance. Above all, many thanks to the Osteopathic Heritage Foundations for the financial grant support for the CORE Research Office.
References
1. Rothberg MB . Overcoming the obstacles to research during residency: what does it take? JAMA . 2012;308(21):2191-2192. doi:10.1001/jama.2012.14587.10.1001/jama.2012.14587Search in Google Scholar PubMed
2. Donath E , FilionKB, EisenbergMJ. Improving the clinician-scientist pathway: a survey of clinician-scientists. Arch Intern Med. 2009;169(13):1242-1244. doi:10.1001/archinternmed.2009.173.10.1001/archinternmed.2009.173Search in Google Scholar PubMed
3. Cornfield DN , LaneR, AbmanSH. Creation and retention of the next generation of physician-scientists for child health research. JAMA. 2013;309(17):1781-1712. doi:10.1001/jama.2013.2258.10.1001/jama.2013.2258Search in Google Scholar PubMed
4. Rivera JA , LevineRB, WrightSM. Completing a scholarly project during residency training: perspectives of residents who have been successful. J Gen Intern Med. 2005;20(4):366-369. doi:10.1111/j.1525-1497.2005.04157.x.10.1111/j.1525-1497.2005.04157.xSearch in Google Scholar PubMed PubMed Central
5. Strong EA , De CastroR, SambucoD, et al. Work-life balance in academic medicine: narratives of physician-researchers and their mentors [published online June 14, 2013]. J Gen Intern Med. 2013;28(12):1596-1603. doi:10.1007/s11606-013-2521-2.10.1007/s11606-013-2521-2Search in Google Scholar PubMed PubMed Central
6. Buser BR , SwartwoutJ, GrossC, BiszewskiM. The single graduate medical education accreditation system. J Am Osteopath Assoc. 2015;115(4):251-255. doi:10.7556/jaoa.2015.049.10.7556/jaoa.2015.049Search in Google Scholar PubMed
7. ACGME Common Program Requirements . Chicago, IL: Accreditation Council for Graduate Medical Education; 2014. http://acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs_07012015.pdf. Accessed March 16, 2016.Search in Google Scholar
8. Gevitz N . Researched and demonstrated: inquiry and infrastructure at osteopathic institutions. J Am Osteopath Assoc. 2001;101(3):174-179.Search in Google Scholar
9. Pololi L , KnightS, DunnK. Facilitating scholarly writing in academic medicine. J Gen Intern Med. 2004;19(1):64-68. doi:10.1111/j.1525-1497.2004.21143.x.10.1111/j.1525-1497.2004.21143.xSearch in Google Scholar PubMed PubMed Central
© 2016 American Osteopathic Association
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in the same Issue
- BOOK REVIEWS
- A View From the Inside: A Collection of Medically Oriented Short Stories
- EDITORIAL
- ENGAGE Initiative: Showcasing Osteopathic Scholarly Activity
- Building Primary Care Research Capacity in a College of Osteopathic Medicine
- Correction
- Correction
- LETTERS TO THE EDITOR
- Interstate Medical Licensure Compact: Pernicious Myths and Inescapable Facts
- AOA COMMUNICATION
- Proposed Amendments to the AOA Constitution, Bylaws, and Code of Ethics
- ORIGINAL CONTRIBUTION
- Effectiveness of Home Blood Pressure Monitoring Among Low-Income Adults in Rural Appalachia
- CLINICAL REVIEW
- Is Meat Killing Us?
- MEDICAL EDUCATION
- Premedical Students’ Attitudes Toward Primary Care Medicine
- SPECIAL COMMUNICATION
- Growing Research Among Osteopathic Residents and Medical Students: A Consortium-Based Research Education Continuum Model
- CASE REPORT
- Intact Cornual Ectopic Pregnancy and Dermoid Cyst With Intraoperative Rupture
- Transient Ischemic Attack After Foam Sclerotherapy in a Woman With a Patent Foramen Ovale
- THE SOMATIC CONNECTION
- Eye Contact, Appetite, and Vomiting Improved in Children With Autism Spectrum Disorder After Visceral Osteopathic Technique
- Postural Balance and Gait Improved With an Osteopathic Intervention in a Special Needs Population
- Significant Benefit Shown After Lumbar Disk Surgery Rehabilitation by Inclusion of Osteopathic Intervention
- Spinal Mobilization Has Peripheral Vasodilation Effects
- Multidisciplinary Biopsychosocial Rehabilitation Improves Outcomes for Patients With Chronic Low Back Pain
- Manual Therapy for Hamstring Hypertonicity Improves Temporomandibular Dysfunction in Athletes
- CLINICAL IMAGES
- Aseptic Splenic Abscess and Sweet Syndrome
- IN YOUR WORDS
- The Benefits of Being a Patient
Articles in the same Issue
- BOOK REVIEWS
- A View From the Inside: A Collection of Medically Oriented Short Stories
- EDITORIAL
- ENGAGE Initiative: Showcasing Osteopathic Scholarly Activity
- Building Primary Care Research Capacity in a College of Osteopathic Medicine
- Correction
- Correction
- LETTERS TO THE EDITOR
- Interstate Medical Licensure Compact: Pernicious Myths and Inescapable Facts
- AOA COMMUNICATION
- Proposed Amendments to the AOA Constitution, Bylaws, and Code of Ethics
- ORIGINAL CONTRIBUTION
- Effectiveness of Home Blood Pressure Monitoring Among Low-Income Adults in Rural Appalachia
- CLINICAL REVIEW
- Is Meat Killing Us?
- MEDICAL EDUCATION
- Premedical Students’ Attitudes Toward Primary Care Medicine
- SPECIAL COMMUNICATION
- Growing Research Among Osteopathic Residents and Medical Students: A Consortium-Based Research Education Continuum Model
- CASE REPORT
- Intact Cornual Ectopic Pregnancy and Dermoid Cyst With Intraoperative Rupture
- Transient Ischemic Attack After Foam Sclerotherapy in a Woman With a Patent Foramen Ovale
- THE SOMATIC CONNECTION
- Eye Contact, Appetite, and Vomiting Improved in Children With Autism Spectrum Disorder After Visceral Osteopathic Technique
- Postural Balance and Gait Improved With an Osteopathic Intervention in a Special Needs Population
- Significant Benefit Shown After Lumbar Disk Surgery Rehabilitation by Inclusion of Osteopathic Intervention
- Spinal Mobilization Has Peripheral Vasodilation Effects
- Multidisciplinary Biopsychosocial Rehabilitation Improves Outcomes for Patients With Chronic Low Back Pain
- Manual Therapy for Hamstring Hypertonicity Improves Temporomandibular Dysfunction in Athletes
- CLINICAL IMAGES
- Aseptic Splenic Abscess and Sweet Syndrome
- IN YOUR WORDS
- The Benefits of Being a Patient

