A 50-year-old male was admitted to our hospital due to “recurrent back pain for 18 years, aggravated with numbness and weakness of the right lower limb for 3 months.” After admission, his physical examination showed that his spine activity was significantly limited. His HLA-B27 test was positive, and X-ray showed that his bilateral sacroiliac joint space had disappeared, hip joints were narrowed and femoral head was necrotized (Figure 1). Bone destruction was observed on the lower edge of T10 vertebral body and the upper edge of T11 vertebral body. Subsequent biopsy result revealed that the damage was not caused by tumor or infection. The patient was diagnosed as Ankylosing Spondylitis (AS) with Andersson lesion (AL). AL is a rare complication of AS, first described by Andersson in 1937.[1, 2] AL is a lesion of the intervertebral disk–vertebral interface at the late stage of AS, which can be characterized as a combination of bone hyperplasia and bone destruction. AL can be easily misdiagnosed as an infectious disease (such as spinal tuberculosis) or a neoplastic disease in clinical practice. The patient adopted surgical treatment and underwent standardized tumor necrosis factor antagonist (Etanercept) treatment after operation. So far, the patient's pain and numbness of right lower limbs have significantly reduced.
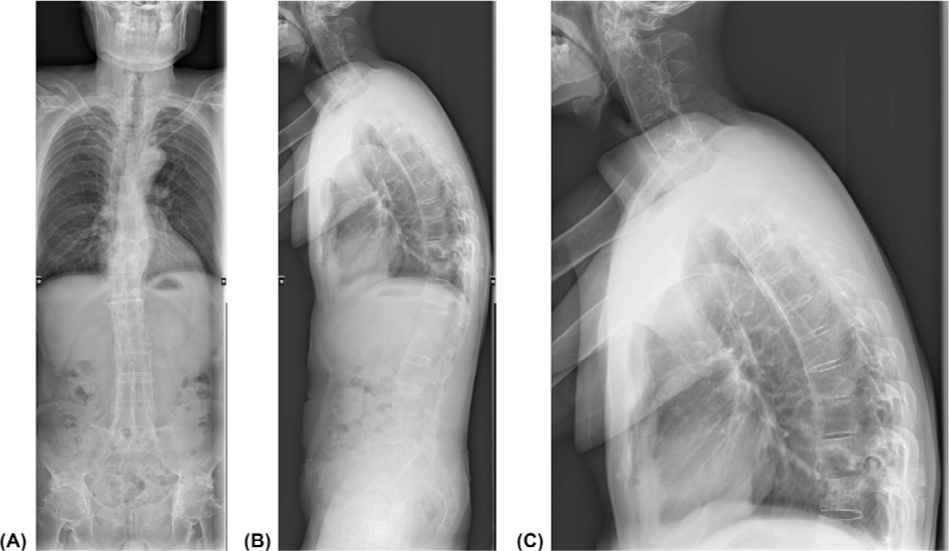
Full spine X-ray showed the patient's spinal changes. From the full spine X-ray, thoracic kyphotic deformity and bamboo-like changes in the thoracolumbar spine were observed. The lower edge of T10 vertebral body and the upper edge of T11 vertebral body showed bone destruction. The structure of attachment area bone was disordered and the density was uneven. The bilateral sacroiliac joint space had disappeared, the bilateral hip joints were narrowed and bilateral femoral head was necrotized. (A) Full Spine X-ray (PA); (B) Full Spine X-ray(LAT); (C) T-Spine X-ray (LAT).
Conflict of Interest
Huji Xu is an Editorial Board Member of the journal. The article was subject to the journal's standard procedures, with peer review handled independently of this member.
References
[1] Bron JL, de Vries MK, Snieders MN, et al. Discovertebral (Andersson) Lesions of the Spine in Ankylosing Spondylitis Revisited. Clin Rheumatol. 2009;28(8):883–892.10.1007/s10067-009-1151-xSearch in Google Scholar PubMed PubMed Central
[2] Kim SK, Shin K, Song Y, et al. Andersson Lesions of Whole Spine Magnetic Resonance Imaging Compared with Plain Radiography in Ankylosing Spondylitis. Rheumatol Int. 2016;36(1.2):1663–1670.10.1007/s00296-016-3542-zSearch in Google Scholar PubMed
© 2022 Xin Wu et al., published by Sciendo
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in the same Issue
- Review
- Myositis-specific antibodies: Overview and clinical utilization
- Interleukin-6 blocking therapy for COVID-19: From immune pathogenesis to clinical outcomes
- Contribution of impaired DNASE1L3 activity to anti-DNA autoantibody production in systemic lupus erythematosus
- Original Article
- Effects of conventional rehabilitative and aerobic training in patients with idiopathic inflammatory myopathy
- Effectiveness of SB4 transition from originator etanercept in rheumatoid arthritis and axial spondyloarthritis: A subgroup analysis from the BENEFIT study
- Special Report
- The challenges and future perspective for the management of systemic lupus erythematosus in China: A concise annual report of 2020
- Images
- Andersson lesion in ankylosing spondylitis
- Letter
- A 16-year-old boy with arthritis, rash, and hemoptysis: Beyond “undifferentiated connective tissue disease”?
Articles in the same Issue
- Review
- Myositis-specific antibodies: Overview and clinical utilization
- Interleukin-6 blocking therapy for COVID-19: From immune pathogenesis to clinical outcomes
- Contribution of impaired DNASE1L3 activity to anti-DNA autoantibody production in systemic lupus erythematosus
- Original Article
- Effects of conventional rehabilitative and aerobic training in patients with idiopathic inflammatory myopathy
- Effectiveness of SB4 transition from originator etanercept in rheumatoid arthritis and axial spondyloarthritis: A subgroup analysis from the BENEFIT study
- Special Report
- The challenges and future perspective for the management of systemic lupus erythematosus in China: A concise annual report of 2020
- Images
- Andersson lesion in ankylosing spondylitis
- Letter
- A 16-year-old boy with arthritis, rash, and hemoptysis: Beyond “undifferentiated connective tissue disease”?

