Priorities, actions and risks in the COVID-19 pandemic: a flash SoMe survey among surgical oncologists
-
Delia Cortés-Guiral
, Olivia Sgarbura
, Mohammad Alyami
Abstract
Objectives
Corona virus-induced disease 19 (COVID-19) pandemic has globally affected the surgical treatment of cancer patients and has challenged the ethical principles of surgical oncologists around the world. Not only treatment but also diagnosis and follow-up have been disrupted.
Methods
An online survey was sent through Twitter and by the surgical societies worldwide. The survey consisted of 29 closed-ended questions and was conducted over a period of 24 days beginning in March 26, 2020.
Results
Overall, 394 surgical oncologists from 41 different countries answered the questionnaire. The predominant guiding principle was “saving lives” 240 (62%), and the different aspects of lock-down found hence large support (mean 7.1–9.3 out of 10). Shut-down of elective surgery and modification of cancer care found a mean support of 7.0 ± 3.0 and 5.8 ± 3.1, respectively. Modification of cancer care longer than two weeks was considered unacceptable to 114 (29%) responders. Hundred and fifty six (40%) and 138 (36%) expect “return to normal” beyond six months for surgical practice and cancer care, respectively.
Conclusions
Surgical oncologists show strong and long-lasting support for lock-down measures aiming to save lives. The impact of the pandemic on surgical oncology is perceived controversially, but the majority was forced already now to accept what is inacceptable for many of their colleagues.
Introduction
Corona virus-induced disease 19 (COVID-19) pandemic changed our professional and private lives [1], [2], [3] since a brief report to WHO China of few cases of respiratory pneumonia of unknown origin at the end of December 2019 [4] turned into a declaration of Public Health Emergency of International Concern (PHEIC) on January 30 [5]. Radical measures needed to be taken in most countries to contain infectious spread and to increase or shift resources from most domains to emergency units and intensive care aiming to avoid to increase the surge capacity of health care systems and to minimize the number of avoidable COVID-19 deaths [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16].
The general principle of patient care “primum not nocere” was challenged in COVID-19 times, as some of these measures required to limit surgical service and to delay or modify cancer care with yet unknown consequences for the concerned patients [17], [18], [19], [20], [21].
The aim of this survey was to study the surgical oncologist’s view on priorities, risks and measures during the COVID-19 pandemic with special focus on the impact on surgical oncology.
Materials and methods
The present study is a flash survey among surgical oncologists diffused by Social Media (SoMe). The questionnaire consisted of 27 closed-ended questions on demographics (n=5), (A) guiding principles (n=2), (B) measures of containment (n=10), (C) shifting of resources, current management (n=6) and (D) perspective (n=4) (Supplementary Material, Appendix p 1). The intuitive online questionnaire (Google Docs® application, 2012, Mountain View, California, USA) could be answered from any connected device (mobile phone, personal computer, tablet and laptop) and took a median of 7 min to be completed.
The survey was launched online on March 26, 2020 while the pandemic spread exponentially [22], [23], [24] and was closed on April 19, when death tolls peaked in the United States [25], [26], [27]. Twitter is the most engaged social media application for physicians around the world [28, 29] and was therefore chosen as platform to launch the survey. The survey was diffused through the SoMe4Peritoneum account @SPeritoneum, SoMe4Surgery @me4_so and SoMe4HPB @hpb_so (Twitter official accounts from SoMe4Surgery communities specifically focused on surgical oncology and peritoneal surface malignancies) and the private account of one of the surgical oncologists in charge of this community (@DeliaCortesGuir). Concurrently the survey was endorsed and distributed by the following surgical societies: ACS (American College of Surgeons), ESSO (European Society of Surgical Oncology), JSCO (Japan Society Clinical Oncology), RENAPE (French Registry for Rare Peritoneal Tumors), SEOQ (Sociedad Española de Oncología Quirúrgica) and SSCRS (Saudi Society of Colon and Rectal Surgery).
Plain descriptive statistics were used to present the results of the current survey and the frequencies were reported as raw numbers and percentages. Median and mean values were calculated for discrete and continuous variables, respectively. Data analysis was performed with IBM© SPSS® Statistics Subscription (IBM Inc., Armonk, NY, USA). Discrete variables were compared with Wilcoxon test, categorical variables were compared with χ2-test and correlations were performed with Pearson and Spearman tests. A two-sided alpha of 0.05 was used to indicate statistical significance.
Results
In the 24 day time period, 394 surgical oncologists from 41 different countries answered the questionnaire. Complete demographics are provided as Supplementary Material, Appendix p. 6. Briefly, 268 (68%) responders worked in academic institutions or dedicated cancer centers. Most responders were consultants 297 (76%) and had at least one subspecialty 334 (85%).
Guiding principles
Figure 1 displays the wide variation of priorities among surgical oncologists concerning pertinent guiding principles. As a pattern, three different levels of priority aims could be identified: 1. Saving lives, 2. Saving life-years, protection of health care system and workers, 3. Maintaining normal life and limit economic consequences. Of note, two-thirds acknowledged that these declared priorities were likely to change in the future course of the pandemic.
Measures of containment
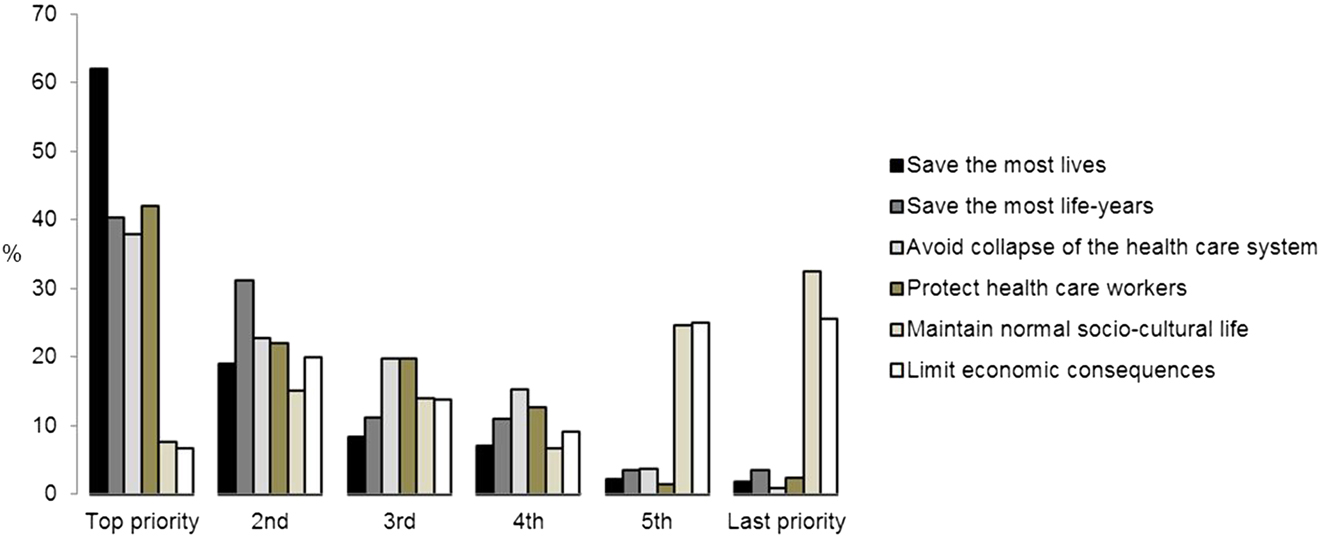
Guiding principles during COVID-19 pandemic.
Schematic representation of guiding principles during COVID-19 pandemic ranked by priority.
Restrictive measures found variable support by the responders and were considered inevitable by 298 (76%) panelists for canceling of large public events, 244 (62%) for limitation of travel, 221 (56%) for closure of schools, 140 (36%) for lock-down and 107 (28%) for handy-tracking. Mean support for these measures of containment is displayed in Figure 2. A variable majority (55–76%) supported all of these measures for “as long as necessary”.
Shifting resources
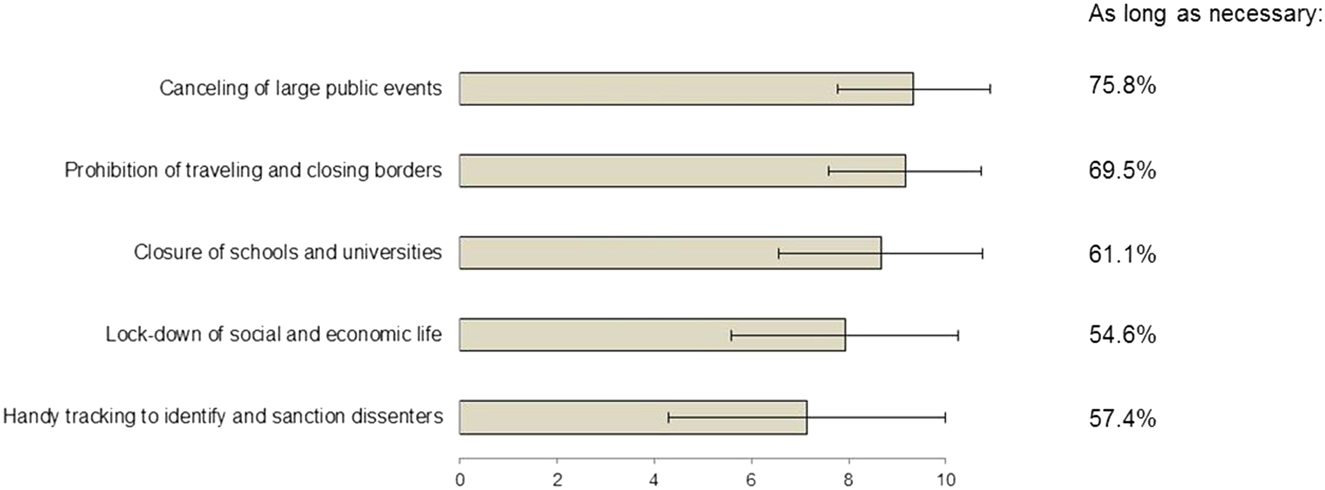
Measures of containment during COVID-19 pandemic: support and acceptable duration.
Support for measures of containment during COVID-19 pandemic rated from 0 (no support) to 10 (total support). Displayed are means and standard deviation. The majority of responders supported containment as long as necessary, as indicated by percentages for each containment measure.
Large heterogeneity was encountered with regards to the shutdown of elective surgery program (mean support 7.0 ± 3.0) and modification of cancer care (Figure 3A, B). The latter found little support by surgical oncologists (mean support 5.8 ± 3.1). Interestingly 114 (29%) of responders judged modification of cancer care to be inacceptable at all or for >two weeks, while 115 (29%) could accept this profound paradigm shift for “as long as necessary”. Further, 258 (66%) declared to have changed their strategy already as detailed in Figure 4.
Perspectives
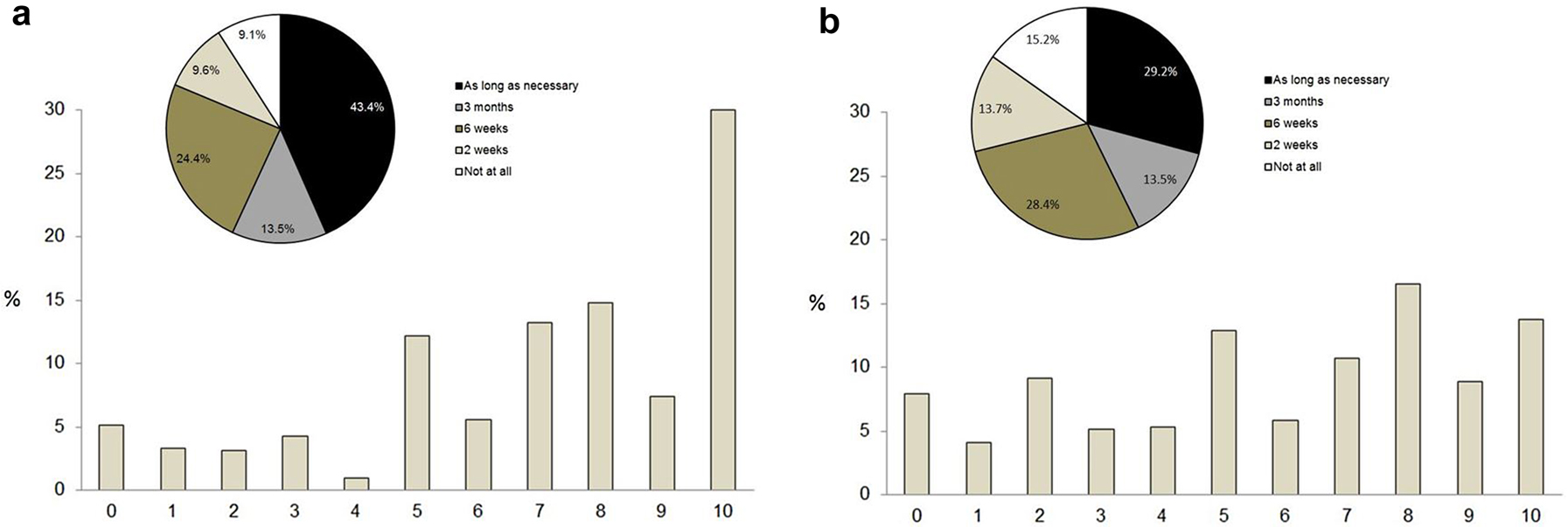
Acceptance of shifting of resources during COVID-19 pandemic.
(A) Shut-down of elective surgery program. (B) Deferring or modification of cancer care. Acceptance of shifting of resources for (A) shut-down of elective surgery program and (B) deferring or modification of cancer care rated from 0 (no support) to 10 (total support). Pie charts represent acceptable time lines for shifting of resources.
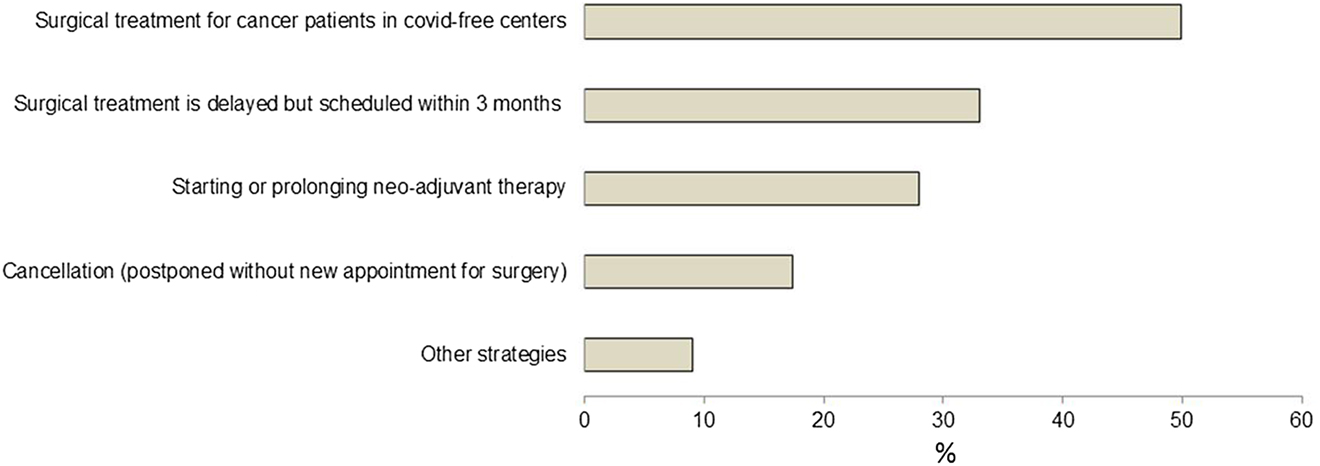
Changes in management of cancer patients during the COVID-19 pandemic.
Estimated duration until “return to normal” for surgical practice, cancer care, medical meetings and social life are summarized in Table 1. Of note, return to normal surgical practice and cancer care was not expected to occur before six months of time by 156 (40%) and 138 (36%) of the surveyed surgical oncologists, respectively.
Intercultural variations
Estimated duration of COVID-19 crisis: “Back to normal”.
| Normality in … | Six weeks | Three months | Six months | One year + |
|---|---|---|---|---|
| Surgical practice | 24% | 37% | 28% | 12% |
| Cancer care | 28% | 37% | 25% | 11% |
| Meetings | 7% | 21% | 46% | 26% |
| Social life | 8% | 31% | 37% | 24% |
Highest proportion is displayed in bold.
The results of the main group of respondents (Japan) were compared to the rest of the participants. Of note, a significantly lower rate of surgeons needed to change their strategies of cancer care (31 vs. 88%, p<0.0001) but a similar number estimated that they might change their priorities in the future (62 vs. 70% in the rest of the group, p = not significant [NS]). The ranking of priorities was similar in the two populations. Global support for the measures of containment was significantly lower in the Japanese population (8 vs. 9.2, p<0.0001) and the difference was confirmed for every category.
Support for deferring cancer care was significantly lower than for all other measures of containment in the entire population (5.8 vs 8.7; p<0.0001). The support was lower in the Japanese subgroup than in the rest of the respondents (5.3 vs 6.3; p<0.0001).
Discussion
The present flash survey depicts the current view of surgical oncologists on priorities, measures and their impact on surgical care. The top priority guiding principle “to safe lives” leads currently to wide acceptance of restrictive measures despite the perceived negative impact on cancer care. While there is reluctance to delay or modify surgical oncology, this change has widely taken place already and it is expected to last for at least six months.
Fair allocation of resources in situation of scarcity has been long discussed in different contexts [30, 31] and it is nowadays accepted that the four leading principles are: maximizing benefits of scarce resources, treating people equally, promoting and rewarding instrumental value and giving priority to the worst off. In this survey, “saving most lives” came up as a top priority for most respondents while “saving most life-years” appeared more frequently in the second position but was almost as frequently cited as the third or even fourth priority. These two principles are considered as the equivalent of a consensus in bioethics [30], [31], [32] and, although some heterogeneity was noted, surgical oncologists recognized them as such.
Although the support of surgical oncologists for different containment measures was variable, cancelation of public events, limitations of travel and closure of schools obtained a moderate to large consensus (more than 60%) just as a similar rate was encountered in support of these measures “as long as necessary”. These results are consistent with the fact that surgical oncologists are caregivers placing healthcare in the top of the societal prime concern, particularly in pandemic context. Given the large range of nationalities of the respondents of these surveys and the share of 38% of Japanese oncologists, these results imply that professional focus outreaches the cultural specificity in this issue. Since the first report indicating a significantly higher rate of COVID-19 infections in cancer patients [20], several national and international guidelines proposed recommendations concerning the potential deferral mechanisms in cancer care and targeted pathologies [33], [34], [35], [36]. In the light of these recommendations, some authors [37, 38] analyzed big data in a tentative to calculate a safe postponement period that turned out to be a median of three weeks since specialist consultation and six weeks since diagnosis for cancers treated with surgery first. In the present survey, two-thirds of the respondents acknowledge to have changed their cancer care strategies during the COVID-19 pandemic. The acceptable deferring period for cancer care was the item with the highest heterogeneity in this study. Of note, one third of the respondents considered that deferral was unacceptable or acceptable for a maximum of two weeks while another third accepted it for “as long as necessary”. These results are highly suggestive of a potential conflict faced by surgical oncologists during the present sanitary situations as the traditional pressure put on cancer care systems to be highly responsive in the management of the disease collides with present ambiguous recommendations from scientific societies and scant evidence-based data.
Even in normal times, rationing of the resources and, potentially, of healthcare is unavoidable [39]. However, it has been showed before that practitioners, including ICU practitioners that are exposed to that selection on a regular basis, are not always aware of the choices they are making [39]. Furthermore, the individual physician should not be faced with the terrible task of performing the selection in isolation [30]. The current situation is sometimes exposing the surgical oncologists to making that choice on their own or together with their colleagues in local multidisciplinary tumor boards which questions their preparation to facing bioethical dilemmas.
In the present flash survey, two-thirds of the respondents admitted that they might change priorities during this sanitary situation and more than a third did not think that a return to normality would happen before six months. These results are in contrast with the reduced acceptability of the cancer care deferral, but they show that, in spite of the lack of explicit knowledge, surgical oncologists remain highly adaptable to change. In Megginson’s words “According to Darwin’s Origin of Species, it is not the most intellectual of the species that survives; it is not the strongest that survives; but the species that survives is the one that is able best to adapt and adjust to the changing environment in which it finds itself ” [40].
The present survey benefitted from a high rate of Japanese respondents. Their availability to complete the survey is probably linked to the high influence of JSCO. Several high-quality Western organizations supported this survey but their area of influence is probably more heterogenous. The earlier phase in the management of COVID-19 at the time of the survey and the significantly lower percentage of Japanese surgical oncologists that had to alter cancer care explain lower acceptance of containment measures but probably should not be considered as the sole influencing factor as other cultural and social confounding variable were not taken into consideration by the present survey.
This flash survey can only picture the current situation. Attitudes of responders are likely to change during the pandemic as two-thirds of them confirmed. The surveyed sample of surgical oncologists was not specifically selected (biased) but is not representative neither due to the voluntary character. Response for most of the questions depended on many factors such as country of origin, setting, experienced phase of the pandemic, timing of response to the survey, but also general attitude, personality and values of the responders.
Conclusions
Surgical oncologists have widely embraced the consequences of prioritizing the principle of “maximizing the benefits”, and strong and long-lasting support for lock-down measures aiming to save lives as top guiding principle. The pandemic forced surgical oncologist to accept the inacceptable, namely to modify best cancer care, probably for a prolonged period. To solve this dilemma, alternative strategies need not only to be developed but also to be monitored carefully to guarantee equipoise.
Acknowledgments
The authors thank ACS (American College of Surgeons), ESSO (European Society of Surgical Oncology) , JSCO (Japanese Society of Clinical Oncology), RENAPE (French Registry for Rare Peritoneal Tumors), SEOQ (Spanish Society of Surgical Oncology) and SSCRS (Saudi Society of Colon and Rectal Surgery) for their invaluable contribution and support spreading disinterestedly this survey among their affiliates.
Research funding: None declared.
Author contributions: DCG, OS, MA and MH developed the idea. All authors drafted the survey, the article and prepared the tables and figures. All authors substantially revised the manuscript. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Competing interests: Authors state no conflict of interest.
Informed consent: Informed consent was obtained from all individuals included in this study
Ethical approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as revised in 2013), and has been approved by the authors’ Institutional Review.
References
1. Verity, R, Okell, LC, Dorigatti, I, Winskill, P, Whittaker, C, Imai, N, et al.. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020;20:669–77. https://doi.org/10.1016/s1473-3099(20)30243-7.Search in Google Scholar
2. Martin Reeves, PC-S, Whitaker, K, Abraham, M. Post-COVID era. Boston, MA: BCG Henderson Institute; 2020.Search in Google Scholar
3. Nimmo, B. Business continuity in a COVID-19 world. London, UK: KPMG International Limited (KPMG International); 2020.Search in Google Scholar
4. Organization. WH. Corona virus disease 2019 (COVID-19): situation report-1; 2020. 20200121-sitrep-1-2019-ncov.pdf (who.int).Search in Google Scholar
5. Organization, World Health. Corona virus disease 2019 (COVID-19): situation report-11. Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.Search in Google Scholar
6. Aminian, A, Safari, S, Razeghian-Jahromi, A, Ghorbani, M, Delaney, CP. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg 2020;272:e27-9. https://doi.org/10.1097/SLA.0000000000003925.Search in Google Scholar
7. Chopra, V, Toner, E, Waldhorn, R, Washer, L. How should US hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med 2020;172:621–3. https://doi.org/10.7326/M20-0907.Search in Google Scholar
8. Desai, A, Sachdeva, S, Parekh, T, Desai, R. COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Global Oncol 2020;6:557–9. https://doi.org/10.1200/go.20.00097.Search in Google Scholar
9. Fong, MW, Gao, H, Wong, JY, Xiao, J, Shiu, EY, Ryu, S, et al.. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerg Infect Dis 2020;26:976–84. https://doi.org/10.3201/eid2605.190995.Search in Google Scholar
10. Heymann, DL, Shindo, N. COVID-19: what is next for public health? Lancet 2020;395:542–5. https://doi.org/10.1016/s0140-6736(20)30374-3.Search in Google Scholar
11. Leung, K, Wu, JT, Liu, D, Leung, GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet 2020;395:1382–93. https://doi.org/10.1016/S0140-6736(20)30746-7.Search in Google Scholar
12. Lewnard, JA, Lo, NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis 2020;20:631–3. https://doi.org/10.1016/S1473-3099(20)30190-0.Search in Google Scholar
13. Matrajt, L, Leung, T. Evaluating the effectiveness of social distancing interventions against COVID-19. Emerg Infect Dis 2020;26:1740–8. https://doi.org/10.1101/2020.03.27.20044891.Search in Google Scholar
14. McCall, B. COVID-19 and artificial intelligence: protecting health-care workers and curbing the spread. Lancet Digit Health 2020;2:e166–7. https://doi.org/10.1016/s2589-7500(20)30054-6.Search in Google Scholar
15. Munster, VJ, Koopmans, M, van Doremalen, N, van Riel, D, de Wit, E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med 2020;382:692–4. https://doi.org/10.1056/nejmp2000929.Search in Google Scholar
16. Surgeons ACo. COVID-19 and surgery. Resources for the surgical community.Search in Google Scholar
17. Burki, TK. Cancer care in the time of COVID-19. Lancet Oncol 2020;8:644–6. doi:https://doi.org/10.1016/s2213-2600(20)30508-7.Search in Google Scholar
18. Glehen, O, Kepenekian, V, Bouché, O, Gladieff, L, Honore, C. Treatment of primary and metastatic peritoneal tumors in the Covid-19 pandemic. J Visc Surg 2020;157:S25-31. https://doi.org/10.1016/j.jviscsurg.2020.04.013.Search in Google Scholar
19. Lambertini, M, Toss, A, Passaro, A, Criscitiello, C, Cremolini, C, Cardone, C, et al.. Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: young oncologists’ perspective. London, UK: BMJ Publishing Group Limited; 2020.10.1136/esmoopen-2020-000759Search in Google Scholar
20. Liang, W, Guan, W, Chen, R, Wang, W, Li, J, Xu, K, et al.. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335–7. https://doi.org/10.1016/s1470-2045(20)30096-6.Search in Google Scholar
21. ESSO (European Society of Surgical Oncology). Statement on COVID-19. Advice for surgical oncologists on cancer service provision 2020. https://www.essoweb.org/news/esso-statement-covid-19.Search in Google Scholar
22. Gerstenhaber, F, Grossman, J, Lubezky, N, Itzkowitz, E, Nachmany, I, Sever, R, et al.. Pancreaticoduodenectomy in elderly adults: is it justified in terms of mortality, long-term morbidity, and quality of life?. J Am Geriatr Soc 2013;61:1351–7. https://doi.org/10.1111/jgs.12360.Search in Google Scholar
23. Ministero de la Salute IMoH. Available from: http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=english&id=5367&area=nuovoCoronavirus&menu=vuoto.Search in Google Scholar
24. Health SMo. Daily report from Spanish ministry of health. Available from: https://covid19.isciii.es/.Search in Google Scholar
25. Control CfD. Cases in U.S. Center for Disease Control [Accessed 19 April 2020].Search in Google Scholar
26. Partners, GHE. Daily COVID-19 global case summary report. GE Healthcare Command Centers; 2020.Search in Google Scholar
27. COVID-19 projections. Institute for Healthcare Metrics and Evaluation; 2020.Search in Google Scholar
28. Gallo, G, Sturiale, A, De Simone, V, Mayol, J. Epistemic networks on twitter: a new way to learn. J Invest Surg 2019;1–9. https://doi.org/10.1080/08941939.2019.1656787.Search in Google Scholar
29. Mayol, J, Otero, J. Breaking international barriers: #ColorectalSurgery is #GlobalSurgery. Clin Colon Rectal Surg 2017;30:277–80. https://doi.org/10.1055/s-0037-1604257.Search in Google Scholar
30. Emanuel, EJ, Persad, G, Upshur, R, Thome, B, Parker, M, Glickman, A, et al.. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020;382:2049–55. https://doi.org/10.1056/NEJMsb2005114.Search in Google Scholar
31. Persad, G, Wertheimer, A, Emanuel, EJ. Principles for allocation of scarce medical interventions. Lancet 2009;373:423–31. https://doi.org/10.1016/s0140-6736(09)60137-9.Search in Google Scholar
32. Biddison, LD, Berkowitz, KA, Courtney, B, De Jong, CM, Devereaux, AV, Kissoon, N, et al.. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e145S–55S. https://doi.org/10.1378/chest.14-0742.Search in Google Scholar
33. Surgeons ACo. ACS guidelines for triage and management of elective cancer surgery cases during the acute and recovery phases of coronavirus disease 2019 (COVID-19) pandemic; 2020.Search in Google Scholar
34. Surgeons SSo. Documentos de posicionamiento y recomendaciones de la AEC en relación con la cirugía y COVID-19 2020. Available from: https://www.aecirujanos.es/Documentos-de-posicionamiento-y-recomendaciones-de-la-AEC-en-relacion-con-la-cirugia-y-COVID19_es_1_152.html.Search in Google Scholar
35. (SAGES) SoAGaES. Sages recommendations regarding surgical management OF colorectal cancer patients during the response to the COVID-19 crisis 2020. Available from: https://www.sages.org/recommendations-surgical-management-colorectal-cancer-covid-19/.Search in Google Scholar
36. Coloproctology ESo. ESCP endorses new recommendations regarding surgical response to COVID-19 crisis 2020. Available from: https://www.escp.eu.com/news/2088-escp-endorses-new-recommendations-regarding-surgical-response-to-covid-19-crisis.Search in Google Scholar
37. Turaga, K, Girotra, S. Are we harming cancer patients by delaying their cancer surgery during the COVID-19 pandemic? Ann Surg 2020. https://doi.org/10.1097/SLA.0000000000003967 [Publish ahead of print].Search in Google Scholar
38. Sud, A, Jones, ME, Broggio, J, Loveday, C, Torr, B, Garrett, A, et al.. Collateral damage: the impact on cancer outcomes of the COVID-19 pandemic. medRxiv 2020; Preprint.10.1101/2020.04.21.20073833Search in Google Scholar
39. Scheunemann, LP, White, DB. The ethics and reality of rationing in medicine. Chest 2011;140:1625–32. https://doi.org/10.1378/chest.11-0622.Search in Google Scholar
40. Megginson, LC. Lessons from Europe for American business. SW Soc Sci Q 1963;44:3–13.Search in Google Scholar
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/pap-2020-0142).
© 2020 Delia Cortés-Guiral et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Mini Review
- Survival and pleurodesis outcome in patients with malignant pleural effusion – a systematic review
- Research Articles
- Priorities, actions and risks in the COVID-19 pandemic: a flash SoMe survey among surgical oncologists
- A review of malignant pleural mesothelioma in a large North East UK pleural centre
- Predictors of morbidity and mortality in patients submitted to cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy for ovarian carcinomatosis: a multicenter study
- Cytokine clearance in serum and peritoneal fluid of patients undergoing damage control surgery with abdominal negative pressure therapy for abdominal sepsis
- Current practice and perceptions of safety protocols for the use of intraperitoneal chemotherapy in the operating room: results of the IP-OR international survey
Articles in the same Issue
- Frontmatter
- Mini Review
- Survival and pleurodesis outcome in patients with malignant pleural effusion – a systematic review
- Research Articles
- Priorities, actions and risks in the COVID-19 pandemic: a flash SoMe survey among surgical oncologists
- A review of malignant pleural mesothelioma in a large North East UK pleural centre
- Predictors of morbidity and mortality in patients submitted to cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy for ovarian carcinomatosis: a multicenter study
- Cytokine clearance in serum and peritoneal fluid of patients undergoing damage control surgery with abdominal negative pressure therapy for abdominal sepsis
- Current practice and perceptions of safety protocols for the use of intraperitoneal chemotherapy in the operating room: results of the IP-OR international survey

