A review of the studies investigating the effects of noise exposure on humans from 2017 to 2022: Trends and knowledge gaps
-
Mohammad Javad SheikhMozafari
Abstract
Background
Due to rapid urbanization and industrialization, noise pollution has become a growing global concern, with significant impacts on occupational and environmental health. Unlike earlier times when it received limited attention, its importance has increased due to mounting evidence of its health effects. Research on noise pollution highlights its consequences and helps identify gaps that require further exploration. This systematic review aims to compile and categorize the health effects associated with various sources of noise pollution.
Methodology
This review focuses on studies published from 2017 to 2022 examining the impact of noise on human health. Eligible studies were identified through comprehensive searches on PubMed and Web of Science.
Results
Out of 1,042 studies retrieved, 287 met the inclusion criteria. The health effects of noise were categorized into auditory effects (e.g., hearing loss), non-auditory effects (e.g., psychological and physiological impacts), and other effects (e.g. immune dysfunction and DNA damage).
Conclusions
While substantial research highlights the adverse effects of noise, future studies should explore its emerging impacts, especially on occupational and environmental health, such as links to cancer and genetic damage, to address existing research gaps and provide a broader understanding of its implications.
1 Introduction
Noise pollution has become a significant concern for various groups, among them acoustic experts, epidemiologists, and urban residents [1,2]. The pervasive and unwanted presence of noise has severe physical and psychological effects on human health [3,4]. The World Health Organization (WHO) ranks noise as the second most harmful environmental factor in Western Europe and a leading cause of health issues [5,6]. Rapid urbanization and industrialization have exacerbated noise pollution to hazardous levels [7]. The harmful effects of noise on both the general public and workers are substantial [8], and these negative impacts are intensifying. If not managed, they could lead to serious consequences [9]. Initially, research focused on the impact of occupational noise, primarily causing noise-induced hearing loss (NIHL). However, studies have expanded to include various noise sources and their detrimental effects beyond hearing loss. The sources of noise pollution include but are not limited to, occupational noise, traffic noise from automobiles, planes, trains, wind turbines, community noise, ambient noise, environmental noise, and so on [10,11,12,13,14,15]. The adverse effects of noise on the public and workers include noise annoyance [16], sleep disorders [17], hearing damage [18,19,20], cardiovascular problems [21,22,23], noise sensitivity [24], mental disorders [25], metabolic disorders [26], decreased concentration [27] increased blood pressure, [24] increased diabetes, [28] increased cholesterol and triglycerides [29], and impaired immune system [30,31]. It is estimated that 10% of the US population is at a heightened risk of NIHL, with 16% exposed to occupational noise as reported [32]. According to estimates, 10% of the U.S. population is at significant risk of NIHL, with 16% of them likely to be exposed to hazardous occupational noise [32]. A recent study reported that approximately 56 million people, or 54% of the European Union’s population, live in areas where annual road traffic noise averages over 55 decibels, posing a significant health risk. Moreover, around 45,000 disability-adjusted life years (DALYs) are lost annually in high-income Western European countries due to environmental noise, primarily affecting children aged 7–19 years [33]. According to a recent study, workers exposed to occupational noise exceeding 90 decibels for 8 h each day displayed a significantly higher diastolic blood pressure compared to individuals exposed to noise levels lower than 90 dB [24]. Zaresakhvidi’s research indicated that a 5 dB increase in road traffic noise heightened the risk of developing diabetes by 17% [34]. Hammer’s investigation revealed that in 2013, over 104 million people in the United States were exposed to noise levels exceeding 70 dB annually, which increases the risk of NIHL, heart disease, and other health issues [35]. A European study reported that environmental noise caused significant sleep disturbances, leading to an annual loss of 900,000 DALYs [36]. Hahad’s study found that road traffic noise alone accounted for 18,000 premature deaths, 1.7 million cases of hypertension, and 80,000 hospital admissions annually in Europe [37]. Numerous other research studies have highlighted similar negative impacts of various sound sources on human health [24,38,39,40,41,42].
Acquiring substantial information from studies on the health impacts of noise is essential for a deeper understanding of the effects of human exposure to noise. Furthermore, to the best of our knowledge, no comprehensive examination has yet explored all potential health effects arising from diverse noise sources. Therefore, this research aims to gather and classify the health effects of noise from various perspectives (auditory and non-auditory effects). Another goal of this study is to investigate the trajectory and characteristics of both field and experimental research to identify the strengths and weaknesses of existing studies and address research gaps in current knowledge. The final objective is to provide an overview of research efforts and approaches that could inform future research needs and areas of study. This research is expected to lay the groundwork for more extensive investigations into the health impacts of noise, particularly in areas where relevant studies are limited or insufficient information is available.
2 Material and methods
2.1 Study period and databases used for article search
This systematic review examined the studies conducted about noise effects on humans during 6 years (2017–2022) according to PRISMA [43]. The search for eligible studies was performed using PubMed and Web of Science, which provided comprehensive coverage of the topic by including all relevant and significant studies.
2.2 Search keywords in the database
Since this study follows the PRISMA guideline, a specific search strategy was applied to each of the databases, Web of Science and PubMed.
Web of Science Search Strategy:
TI = (“occupational noise” OR “ambient noise” OR “transportation noise” OR “traffic noise”) AND (“Oxidative stress” OR “cardiovascular disease” OR “Sleep Disorders”)
PubMed Search Strategy:
((“occupational noise”[tiab] OR “ambient noise”[tiab] OR “transportation noise”[tiab]) AND (“Oxidative stress”[tiab] OR “cardiovascular disease”[tiab] OR “Sleep Disorders”[tiab])) For the full list of keywords used in the search strategy, refer to Table 1.
Search strategy keywords used for noise types and health outcomes
| Keyword group | Keywords |
|---|---|
| Noise types | Occupational noise, Outdoor noise, Ambient noise, Environmental noise, Railway noise, Railroad noise, Aircraft noise, Airport noise, Construction site noise, Airplane noise, Traffic noise, Highway noise, Road traffic noise, Rail traffic noise, Transportation noise |
| Health outcomes | Oxidative stress, NIHL, Tinnitus, temporary threshold shift, Permanent threshold shift, Hyperacusis, Hearing impairment, Cardiovascular disease, Heart disease, Heart failure, Hypertension, Ischaemic heart disease, Stroke, Myocardial infarction, Myocardial ischemia, Atherosclerosis, Coronary heart disease, Annoyance, Sensitivity, Cognitive dysfunction, Cognitive impairment, Reading comprehension, Stress, Anxiety, Depression, Sleep disorders, Sleep disturbance, Sleep quality, Sleep problems, Insomnia, Sleep apnea, Sleep-wake disorders, Sleep deprivation, Sleep hygiene, Dyssomnias, Parasomnias |
Figure 1 shows the flowchart of the review process of obtained studies.
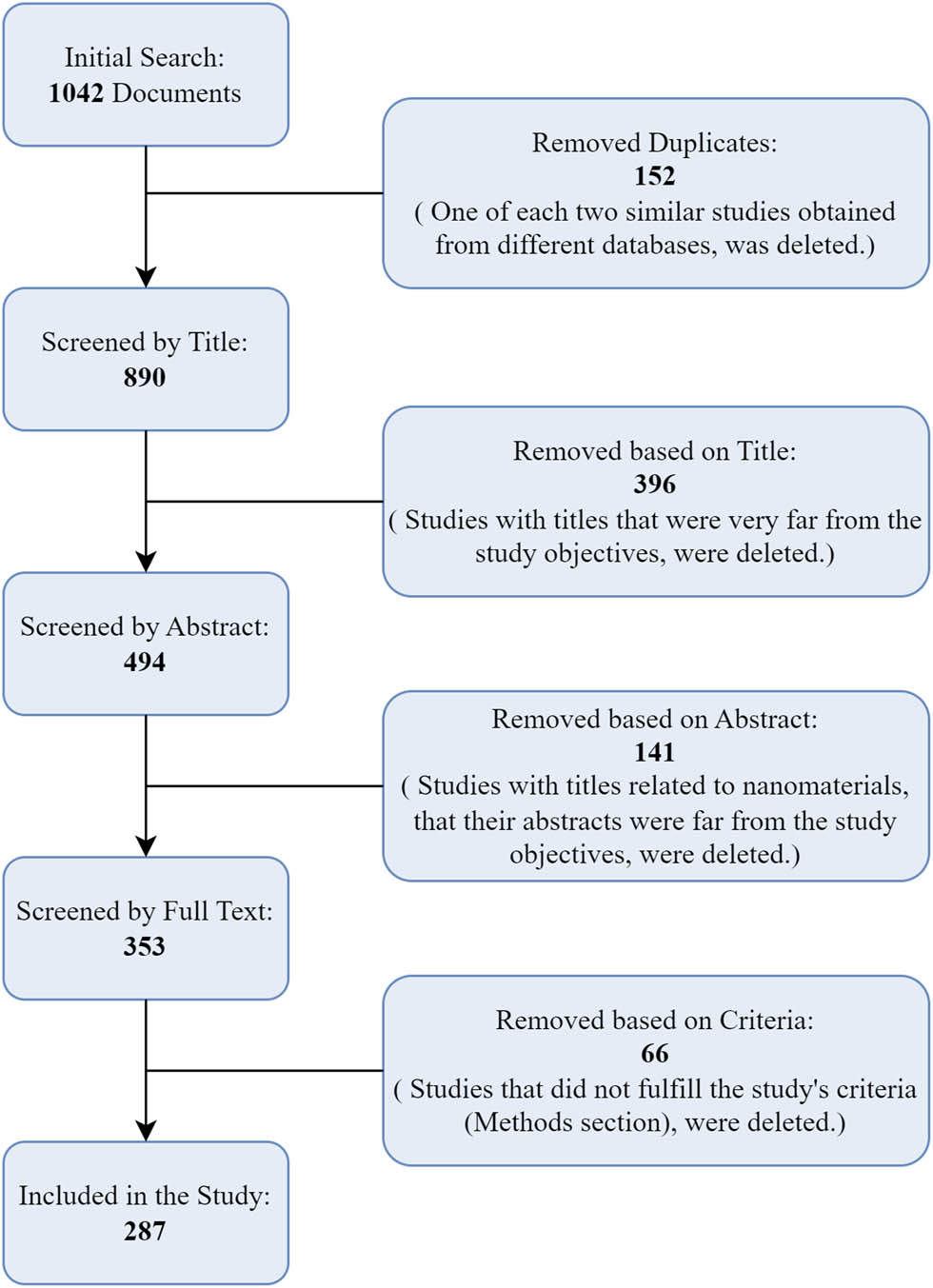
Flow diagram of the systematic review.
2.3 Inclusion and exclusion criteria
Studies meeting the following criteria were included in this review: the study was original, published in English, conducted on humans, examined noise as at least one of the stressors, and demonstrated a significant correlation between noise and the investigated effects. Animal and cellular studies, as well as studies where the relationship between noise and its effects was not statistically significant, were excluded.
After identifying the primary studies, additional steps were taken to ensure comprehensive results. The “related articles” and “citations” features in Google Scholar and ResearchGate were used as supplementary tools to identify and receive potentially relevant studies, particularly when the journals were not open access to direct access to the full text of the articles. In this review, data extraction was performed independently by two of our authors using a standardized table. Extracted data included the study title, authors, publication year, study type, noise type, type of effects investigated, and journal details. A third author compared the two sets of extracted data and resolved any discrepancies by referring to the original article.
Figure 1 illustrates the systematic process used for selecting studies for the research.
3 Results
3.1 Reviewed studies
An initial search using research keywords yielded 1,042 articles published between 2017 and 2022. After eliminating 152 duplicate studies, an initial title review excluded 396 irrelevant studies. Then, the abstract review excluded another 141 studies. Further in the full-text review phase, 66 documents were removed, ultimately leaving 287 studies for analysis. The cumulative frequency of these included studies, categorized by the year of publication, is illustrated in Figure 2.
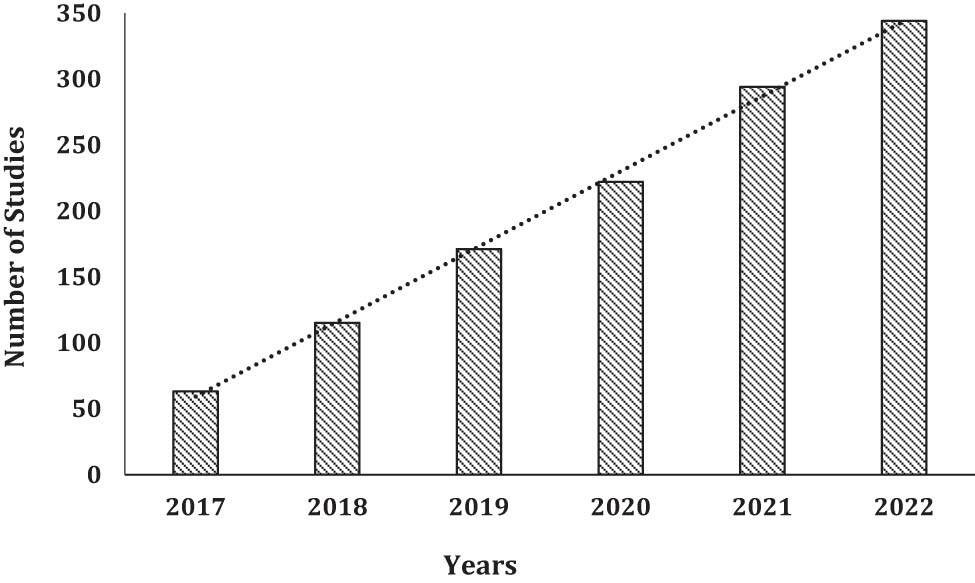
The number of studies conducted each year from 2017 to 2022.
According to Figure 3, studies on noise effects have been conducted globally across 44 countries. Denmark and China have had the highest number of studies in this area. Generally, European countries have made greater contributions to the studies.

Geographical distribution of studies.
The distribution of study types analyzed has been depicted in Figure 4. This review encompassed a diverse range of studies, with the majority comprising cross-sectional (158 studies) and cohort (82 studies) designs.
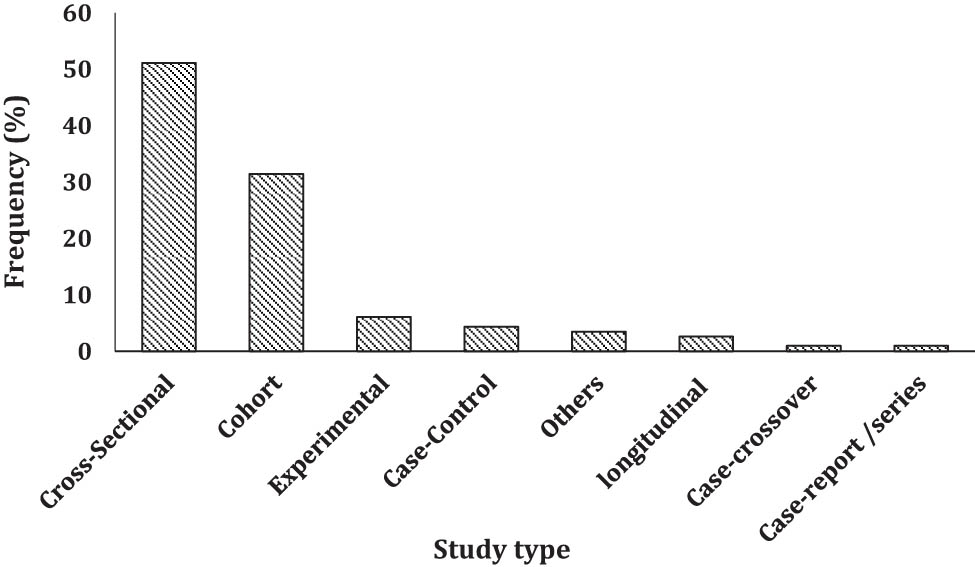
Frequency distribution of study types.
As illustrated in Figure 4, the purpose of this figure is to present the distribution of studies reviewed in this research based on their study design. It highlights that the majority of the reviewed studies are cross-sectional, emphasizing the prevalence of this type of study among the articles analyzed.
3.2 Noise effects on human health
Noise effects can be broadly categorized into three primary types: auditory effects, non-auditory effects, and other adverse effects as explained in other studies too [44]. Auditory effects primarily include hearing loss and hearing damage. Non-auditory effects encompass the psychological and physiological impacts of noise exposure. The category of other adverse effects includes diseases, disorders, and other harmful consequences of noise exposure. Table 2 illustrates the frequency distribution of studies across these categories of noise effects. It shows that, within auditory effects, hearing loss has been more extensively researched compared to hearing damage. Likewise, among non-auditory effects, psychological impacts have received the most research focus. Overall, non-auditory effects constitute the largest body of research.
Classification of the health effects of noise and frequency distribution of the studies conducted in each category (2017–2022)
| Category | Noise effects | Study number | Frequency (%) |
|---|---|---|---|
| Auditory | Hearing loss | 47 | 16.38 |
| Hearing damage | 18 | 6.27 | |
| Non-auditory | Psychological | 114 | 39.72 |
| Physiological | 92 | 32.06 | |
| Other effects | 16 | 5.57 | |
3.3 Auditory effects of noise
Table 3 summarizes research on the auditory effects of noise exposure. The data indicate that sound sources producing pressure levels between 70 and 104 dB can cause hearing impairment, while sources with pressure levels ranging from 45 to 120 dB, covering a broader spectrum, may lead to hearing damage. Additionally, various sources of noise, including occupational noise, traffic from roads, air and rail transportation, environmental noise, and sounds from laboratory and musical instruments, have been identified as contributors to auditory effects.
Studies evaluating the auditory effects of noise
| Auditory effects | Sound source | Noise characteristic | References | |
|---|---|---|---|---|
| Hearing loss | Occupational noise, Traffic noise, aircraft noise, Amusement Tools noise in parkas, surgical tools noise, music, ambient noise, rail noise | 70–104 dB, 3–6 kHz | [16,39,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89] | |
| Auditory system damage | Tinnitus | Occupational noise, musical instruments noise, road traffic noise | 70–120 dB, 0.5–6 kHz | [46,72,81,90,91,92,93,94,95,96] |
| Hearing Fatigue | rail noise | — | [71] | |
| Hyperacusis | Occupational noise, traffic noise (road and air, hospital noise, laboratory noise, leisure noise, ambient noise | 45–125 dB | [97,98,99,100,101,102,103,104] | |
| Cochlea Damage | Occupational noise | 95 dB | [105] | |
| Saccule Damage | Occupational noise | 95 dB, 4 kHz | [105] | |
| Vestibular Damage | Occupational noise | 85 dB, 4 kHz | [105,106] | |
3.4 Psychological effects of noise
The reviewed studies categorize the psychological effects of noise into several subgroups: sleep disorders, noise annoyance, mental health, cognitive disorders, and sleep quality. This classification is summarized in Table 4. Of the 100 studies analyzed, the majority focused on sleep disorders and noise annoyance. These two aspects are notably prominent among the psychological effects reported, particularly when sound pressure levels ranged from 16 to 85 dB.
Studies evaluating the psychological effects of noise
| Psychological effects | Sound source | Noise characteristic | References | |
|---|---|---|---|---|
| Sleep disorder | Insomnia, sleep deprivation, sleep quality reduction, sleep irritability | Traffic and transportation noise (road, rail, and air), occupational noise, wind turbine noise, background noise (hospital, neighborhoods), ambient sound, laboratory sounds | 16–85 dB | [12,14,15,24,38,45,48,51,65,66,71,78,94,100,107–158] |
| Obstructive sleep apnea | Occupational noise | — | [51] | |
| Noise annoyance | Acoustic comfort reduction | Random noise, traffic and transportation noise (road, rail, air), construction industry, wind turbine noise, Laboratory sounds, occupational noise | 21.7–85 dB, 40–400 Hz | [29,41,67,97,98,100–102,110,126,129,130,136,137,143,147,150,159–197] |
| Noise disturbance | — | Background noise (neighborhood), traffic noise | — | [198] |
| Mental health | Depression | Occupational noise, traffic and transportation noise (road, rail and air), random noise * | 35.2–88 dB | [45,100,149,183,199,200] |
| Stress and anxiety | Random noise *, road, and transportation noise | 35.2–55 dB | [45,100,132,149,183] | |
| General mental health | Road traffic and airway noise | 46.3–86.3 dB | [24,39,98,99,133,201–205] | |
| Cognitive impairment | Decreased attention | Road traffic and occupational noise | 55 dB | [128,206,207] |
| Decreased concentration | Background noise | [27,198] | ||
| Memory impact | Laboratory noise and road traffic | 34.7–52.1 dB | [101,208] | |
| cognitive function reduction | Laboratory noise and road traffic | 35–65 dB | [124,161,209,210] | |
*Those noises mentioned sporadically in the studies but without being classified into specific categories.
When assessing the physiological effects of noise, researchers have examined its impact on various human organs, as detailed in Table 5. The findings indicate that the cardiovascular system is most prominently affected by noise, with numerous studies focusing on this area. Additionally, research has investigated the effects of noise on other bodily systems, including the immune, nervous, reproductive, urinary, and endocrine systems, and has confirmed negative impacts on these organs. Recent studies have also explored the potential effects of noise, particularly industrial noise levels ranging from 80 to 97 dB, on DNA and biomarkers of oxidative stress.
Studies evaluating the physiological effects of noise
| Physiological effects | Sound sources | Noise characteristic | References | |
|---|---|---|---|---|
| Cell damage | DNA damage | Occupational noise | 80.2–96.7 dB | [160] |
| Oxidative stress | Occupational noise | 80.2–96.7 dB | [160,211,212] | |
| Hormones secretion | Cortisol | Traffic and transportation noise (road, rail and air), hospital noise | 45–76.8 dB | [38,39] |
| Insulin | Traffic noise (road and rail) | 45 dB | [26] | |
| Cardiovascular system | Increased systolic and diastolic blood pressure | Occupational noise, traffic noise (road, rail and air, random noise* | 38–102 dB | [10,21,68,69,71,97,108,126,135,142,143,155,157,160,163,213–250] |
| Arterial and coronary occlusion | Occupational noise, traffic noise (road, rail and air) | 30–85 dB | [42,95,130,251–256] | |
| Aorta Calcification | Road traffic and occupational noise | — | [257,258] | |
| Atherothrombosis | Random noise* | — | [240] | |
| Arterial inflammation | Road traffic and random noise* | — | [254,259] | |
| — | Traffic noise (road, rail and air), wind turbine noise | 40–64 dB | [10,151,236,237,260–264] | |
| Cardio-cerebrovascular | Ambient noise, vehicle noise, | 61.7 dB | [141,235,262] | |
| Fast Heart Rate | Airport noise, random noise*, road traffic noise, wind turbine noise | 31 dB | [21,94,142,242] | |
| Cardiovascular system faults | Road traffic noise, air way noise | 58.3 dB | [253,265,266] | |
| Atrial fibrillation | Traffic noise (road, rail and airway), industrial noise, construction, and random noise* | [99,104,267] | ||
| Myocardial infarction | Wind turbine noise, traffic noise (road, rail, and air), random noise* | 25–79 dB | [103,114,134,237,260,262,268–275] | |
| Stroke | Road traffic noise, occupational noise, rail noise random noise* | 44–79 dB | [65,75,254,276–278] | |
| Cardiovascular mortality | Road, rail, airway noise | 45–60 dB | [252,279,280] | |
| Ischemic heart disease | Road, rail, airway noise, vehicle noise | 24–75 dB | [16,78,95,103,109,141,163,208,262,263,281–285] | |
| Glycated hemoglobin | Road traffic noise | 55–65 dB | [214] | |
| Congestive heart failure | Road traffic noise | 50–56.3 dB | [134] | |
| Increased cholesterol and triglycerides | Road traffic noise | 55–65 dB | [190,214,241] | |
| Immune system | Immune system failure | Road traffic noise | — | [286] |
| Nervous system | Nervous system failure | Occupational noise | 85 dB | [287] |
| Stroke | Road, rail, airway noise, occupational noise | 30–85 dB | [75,147,251,252,277,281,288,289] | |
| Reproductive system and pregnancy | Time of getting pregnant | Road traffic noise | 55 dB | [290] |
| Blood pressure disorders caused by pregnancy | Road Traffic noise, random noise* | 65 dB | [291,292] | |
| Kidney and urinary tract | Renal hemodynamic disorder, decreased glomerular filtration rate | Airplane noise | 80 dB | [293,294] |
*Those noises mentioned sporadically in the studies but without being classified into specific categories.
3.5 Other noise effects
A comprehensive review of the literature indicates that noise impacts extend beyond auditory and non-auditory effects. Specifically, noise can exacerbate existing diseases and disorders and negatively affect overall health and performance. In our study, we have systematically categorized and analyzed these broader impacts, which are presented in the other effects section of our findings. Due to their complex and non-physiological nature, classifying these impacts can be challenging. Commonly observed conditions in this category include but are not limited to, the aggravation of asthma, disturbances in glucose metabolism, and obesity. Additionally, this category encompasses the potential role of noise in the development and progression of cancer. While establishing a direct causal link between noise exposure and cancer remains difficult, some studies have highlighted noise’s involvement in the development of specific cancers, particularly breast and colon cancer. Traffic noise from sources such as air, rail, and road has been identified as a significant contributor to these health outcomes (Table 6).
Studies evaluating side effects of noise
| Other effect | Sound sources | Noise characteristic | References | |
|---|---|---|---|---|
| Cancer | Prevalence/incidence of breast cancer | Traffic noise (road, rail, and airway) | 35–60 dB | [11,253,285,295] |
| Colon cancer | Road traffic noise | 57 dB | [296] | |
| Asthma | Exacerbation of asthma | Traffic noise (road, rail, and airway) | 56 dB | [40] |
| Diabetes | Glucose metabolism disorder | Traffic noise (road, rail, and airway) | 30–63 dB | [26,245,297–302] |
| Obesity | Increased cholesterol | Occupational health | 85 dB | [10,29,160] |
| Increased triglycerides | Road traffic noise, occupational health | 55–85 dB | [29,160,214] | |
| Obesity prevalence | Traffic noise (road, rail, and airway), Random noise* | 30–89 dB | [242,303–306] | |
| Increased Body mass index | Road traffic noise | 55–56.2 dB | [307,308] | |
| Headache | Traffic noise, background noise (neighborhood) | 53.7 dB | [117,198] | |
| Metabolic syndrome | Occupational health | 85–100 dB | [309] | |
| Serum pristine level | Random noise* | 85.98 dB | [70] | |
| Performance And Productivity | Educational achievements reduction | Community noise and Random noise* | 65 dB | [13,310] |
| Life quality | Life quality reduction | Traffic noise (road, rail, and airway) and airport noise | 30–65 dB | [144,145,311] |
*Those noises mentioned sporadically in the studies but without being classified into specific categories.
In Table 7, the noise exposure effects are presented by the type of sound sources. It is worth noting that this table includes only the sources that caused the most significant effects.
Noise exposure effects by the type of sound sources
| Occupational noise | Hearing Loss, Tinnitus, Hyperacusis, Cochlea Damage, Saccule Damage, Vestibular Damage, Insomnia, sleep deprivation, sleep quality reduction, sleep irritability, obstructive sleep apnea, Noise Annoyance, depression, decreased attention, DNA damage, Oxidative stress, Increased systolic and diastolic blood pressure, Arterial and coronary occlusion, aorta Calcification, stroke, Nervous system failure, brain stroke, Increased cholesterol, Increased triglycerides, Metabolic syndrome |
| Transportation noise | Hearing Loss, Tinnitus, Hearing Fatigue, Hyperacusis, Insomnia, sleep deprivation, sleep quality reduction, sleep irritability, Noise Annoyance, Noise Disturbance, depression, Stress and anxiety, General mental health, Decreased attention, Memory impact, cognitive function reduction, Cortisol disorder, Insulin, Increased systolic and diastolic blood pressure, Arterial and coronary occlusion, aorta Calcification, arterial inflammation, Fast Heart Rate, Cardiovascular system faults, Atrial fibrillation, Myocardial infarction, stroke, Cardiovascular mortality, ischemic heart disease, Glycated hemoglobin, Congestive heart failure, Increased cholesterol, triglycerides Immune system failure, brain stroke, time of getting pregnant, Blood pressure disorders caused by pregnancy, Renal hemodynamic disorder, decreased glomerular filtration rate, Prevalence/incidence of breast cancer, Colon cancer, Exacerbation of asthma, Glucose metabolism disorder, Increased triglycerides, Obesity prevalence, Increased Body mass index, Headache, Life quality reduction, cardio-cerebrovascular |
| Environmental noise | Hearing Loss, Insomnia, sleep deprivation, sleep quality reduction, sleep irritability, Noise Annoyance, Noise Disturbance, and depression. Stress and anxiety, Decreased concentration, increased systolic and diastolic blood pressure, Atherothrombosis, arterial inflammation, cardio-cerebrovascular, Fast Heart Rate, Atrial fibrillation, Myocardial infarction, stroke, Blood pressure disorders caused by pregnancy, Obesity prevalence, Headache, Serum pristine level, educational achievements reduction |
| laboratory noise | Hyperacusis, Insomnia, sleep deprivation, sleep quality reduction, sleep irritability, Noise Annoyance, Memory impact, cognitive function reduction |
4 Discussion
This study reviews research published over the past 6 years (2017–2022) on the impact of noise – both occupational and non-occupational – on human health. While noise has long been a significant concern in workplace settings, its effects are now recognized beyond occupational environments. The WHO has identified noise pollution as the second most critical environmental health factor, following air pollution [228]. This assertion is supported by numerous studies documenting the disease burden and mortality associated with noise exposure [312–314]. Consequently, extensive research has been conducted to investigate the health effects of noise. Our review indicates that, within the specified period, 287 studies have been dedicated to examining the impact of noise on various bodily systems and organs. Analysis of the temporal distribution of the studies reveals that between 40 and 60 studies on the effects of noise on human health have been conducted annually (Figure 2). This consistent research output underscores the significance of noise as a stressor and may reflect ongoing challenges in fully concluding studies on its various impacts. Additionally, the increasing recognition of novel effects associated with noise may drive further research efforts aimed at confirming or refuting these connections. Consequently, it is anticipated that the trend of high research activity in this area will persist in the coming years. From a geographical perspective, research on occupational and environmental noise exposure has predominantly been conducted in Europe and Asia (Figure 3). However, there are notable differences in the focus and nature of these studies across various countries and continents. European nations, with their higher levels of welfare and a strong emphasis on workers’ rights and healthcare, enforce stringent regulations concerning hazardous workplace elements, including loud noise exposure. Consequently, research in these countries has expanded beyond occupational noise to include environmental noise [315], as occupational noise levels have generally been reduced to acceptable thresholds or sufficient data has been gathered. In Europe, considerable attention is given to traffic, aircraft, and train noise, as well as other everyday environmental noise, with a strong focus on assessing the associated disease burden and mortality.
In contrast, research in Asia, particularly in East Asian countries such as China, South Korea, Taiwan, and Japan, differs in both scope and focus from studies in West Asia and Africa. While the volume of studies in Eastern Asia is higher, these studies, similar to their European counterparts, often focus on environmental noise exposure. Conversely, research in West Asian, African, and Middle Eastern countries has largely concentrated on occupational noise exposure [316]. An analysis of study types conducted over a specific period reveals that more than 50% of the studies were cross-sectional, with cohort studies being the second most common type. Figure 4 illustrates the distribution of these study types. Cross-sectional studies, due to their low cost and relatively quick execution, are suitable for investigating potential effects among individuals. However, such studies cannot definitively establish causal relationships between effects and noise exposure. In contrast, cohort studies are generally more effective for this purpose.
The review of noise-related studies indicates an increase in both the number and scope of research, highlighting the relationship between noise exposure and various outcomes. However, there is considerable heterogeneity among these studies regarding the number of participants exposed to noise – ranging from millions to smaller groups – and the duration of exposure, which varies from several months to several years. Although this variability in environmental, cultural, racial, and religious contexts can be advantageous in certain respects, it may also complicate comparisons and affect the consistency of study results [317].
In a broad classification, the effects of noise exposure can be divided into two primary categories: auditory and non-auditory effects. Auditory effects refer to the impacts of noise on the human auditory system, which can lead to temporary or permanent hearing impairment. Historically, research on auditory effects has concentrated on high sound pressure levels, particularly within occupational settings. Recently, however, there has been a growing body of research investigating the auditory effects of environmental noise. Additionally, there is increasing concern about the impact of different types of noise, such as Gaussian noise, on hearing in occupational environments [318].
Our analysis indicates that over 53 studies have investigated the adverse effects of noise exposure on hearing within the specified period. Among these, some studies focused on occupational and non-occupational settings. Potential auditory effects of noise exposure include hearing loss, tinnitus, fatigue, and physical trauma to the auditory system (as summarized in Table 2).
Non-auditory effects encompass a broader range of impacts associated with noise exposure, and the number of studies exploring these effects continues to grow. These effects can be categorized into psychological effects (such as sleep disorders, noise annoyance, cognitive disorders, depression, stress and anxiety, and general mental health), physiological disorders (including cardiovascular issues, cellular damage, gland and hormonal disturbances, immune system problems, nervous system disorders, reproductive issues, and kidney and urinary tract disorders), and other adverse effects (such as cancer, asthma, diabetes, obesity, headaches, metabolic syndrome, and reduced quality of life) (Tables 3, 4, and 5). The findings of this study reveal that non-auditory effects, particularly cancer and physiological anomalies, have received significant attention from researchers in recent years. Despite the valuable insights provided by existing studies on the health impacts of noise, there remain unresolved gaps that require further investigation. The following section will discuss critical information and research gaps related to this topic.
Regarding the study and research gaps, one of the most notable gaps in research on the health effects of noise lies in the methodologies and study designs employed within this field. The variability in research methods – such as differences in statistical populations, types of noise sources, settings (occupational versus non-occupational), study designs, periods, duration of evaluations, intervention strategies, and research variables – has created challenges in comparing results, analyzing complex statistics, and drawing coherent conclusions. As a result, adverse effects and statistical relationships associated with noise exposure have often been attributed to either environmental or occupational factors.
Moreover, the lack of methodological diversity and limited evidence specific to individual cases has further compromised the certainty of findings in noise health research and has impeded researchers from establishing definitive health outcomes. For instance, despite substantial evidence linking noise exposure to cardiovascular disorders, methodological inconsistencies among studies indicate a need for additional research in some areas. Another significant gap is related to gender differences. Many of the reviewed studies have not investigated how gender influences cardiovascular risks and blood pressure changes, leaving the impact of gender on these health risks poorly understood [25]. Research on the impact of occupational noise exposure on blood pressure has yielded inconsistent results. Some studies have found a significant correlation between noise exposure and increased blood pressure, while others have not observed such an association. This inconsistency highlights the need for extensive cohort and case–control studies to further investigate this issue. Notably, none of the studies exploring the relationship between noise exposure and blood pressure elevation have assessed 24-h blood pressure monitoring, a factor that could introduce potential bias and uncertainty in the results [319]. Similarly, research into the effects of noise on the immune system reveals a critical gap: there are far fewer human studies compared to animal studies. Generalizing findings from animal research to humans is often challenging. Therefore, advancing to more comprehensive human studies or developing methods to more accurately translate animal model results to human contexts could help bridge existing information gaps in this field. Despite growing interest, few studies have investigated the effects of noise on the human immune system. The limitations of these studies include inadequate consideration of exposure duration and sound frequency, reliance on constant sound intensity, and the omission of various immunological markers. Given this context, there is a pressing need for more clinical and experimental studies to elucidate both the direct and indirect effects of noise on the human immune system [31]. As previously noted, establishing the relationship between noise exposure and non-auditory health effects is complex. This complexity arises from the necessity of conducting thorough and well-designed studies that require high levels of expertise and scientific rigor for selecting appropriate methodologies, analyzing data, measuring correlations, and interpreting results. Moreover, the reversibility or permanence of non-auditory effects resulting from noise exposure remains unclear. Addressing this gap involves identifying which non-auditory effects are reversible upon cessation of noise exposure, determining the permanence of specific effects, and establishing the time frame required for the reversal of these health effects [320].
A significant gap in the methodology of assessing the health impacts of noise pertains to the characteristics of sound sources that have captured researchers’ attention. This issue deserves a separate and detailed examination due to its importance. While most research on noise effects has focused on sound pressure levels, other critical factors, such as sound frequency and Gaussian distribution, have received less attention. Sound pressure levels are commonly used to assess occupational noise exposure, with higher levels regarded as hazardous. However, recent studies emphasize the importance of frequency and Gaussian distribution in shaping auditory outcomes. The influence of Gaussian distribution on auditory impairment remains under-researched, and its significance compared to sound pressure levels is not yet fully understood [321]. Consequently, there is ongoing uncertainty about whether lower sound pressure levels might still pose auditory risks due to their Gaussian or non-Gaussian properties. This issue extends to non-occupational noise research as well. In studies evaluating the effects of environmental noise, various methodologies are employed, including the use of average sound pressure level, maximum sound pressure level, or maximum nighttime sound level as indicators. Consequently, the question of whether Gaussian or non-Gaussian characteristics of noise should be considered remains a critical concern across both occupational and non-occupational noise research. The lack of clarity regarding the appropriate exposure index complicates the attribution of many observed effects to environmental noise. For instance, the potential link between aircraft noise and stroke remains uncertain. This uncertainty arises because many studies rely solely on average noise levels for assessment, which some researchers argue is insufficient [322]. In addition to gaps related to noise characteristics, there are significant deficiencies in studies focusing on the effects of different sound sources. While there has been substantial research on occupational, environmental, and traffic noise, less attention has been given to other sources such as anthropogenic noise and the associated physiological and demographic responses. Anthropogenic noise is likely to affect various biological systems, ranging from cellular processes to broader population dynamics [323], in other words, anthropogenic (Human-made) noise has the potential to interfere with processes, on scales – from the microscopic level of cells to broader ecological systems – impacting everything from the behavior of individual cells to the interactions among species in ecosystems, as a whole. A notable gap is the lack of comprehensive, long-term experimental studies on both the duration of exposure and the subsequent post-exposure effects. Long-term studies are crucial as short-term assessments may provide misleading or inaccurate results. Moreover, there is a concerning lack of research comparing the effects of different types of sounds and noise levels on human health [323,324].
An examination of the literature on the health implications of noise reveals a focus on both the direct and indirect effects of noise exposure. These indirect effects are often referred to as secondary effects of noise, the effects of the second stage of noise exposure, or the effects caused by noise effects. These terms encompass outcomes such as noise annoyance, tinnitus, and noise sensitivity. Despite the considerable body of research on these phenomena, there remains ambiguity about whether they are direct consequences of noise exposure or if they are exacerbated by the presence of noise. Moreover, secondary effects can further impact human health, manifesting as relationships between noise annoyance and elevated blood pressure, noise annoyance and stress, anxiety, and sleep disorders, tinnitus and depressive symptoms, noise sensitivity and reduced quality of life, and noise sensitivity with mental health disorders. Additionally, the interplay between noise sensitivity, cortisol secretion, and immune system responses is a critical area of concern.
Identifying these secondary effects and delineating them clearly from primary noise-induced effects constitutes a significant research gap that warrants further investigation. Although numerous studies address these topics, they often fall short of exploring all established effects of noise exposure comprehensively. This limitation hinders effective comparison and conclusive interpretation. Consequently, future research should focus on the secondary effects of noise. For example, the mental and psychological impacts of noise exposure remain poorly understood. The complex relationships among mental disorders, genetic differences, environmental factors, and social influences, as well as the mechanisms underlying these conditions, are still unclear. It remains uncertain whether these disorders are primary effects of noise or secondary effects, such as noise sensitivity and irritation [325]. Further investigation is needed into the relationship between cerebrocardiovascular disorders, mental health issues, and noise exposure [326]. The association between an individual’s mental well-being and the level of noise annoyance remains unclear, particularly regarding its connection to psychological conditions such as depression and anxiety [327]. Additionally, there is concern regarding the impact of noise on performance and productivity. Some studies suggest that noise exposure can impair memory and reduce mental productivity, particularly during tasks requiring sustained visual focus. However, the evidence regarding the impact of occupational noise on workplace productivity is inconclusive [328]. The relationship between sound pressure levels and job productivity lacks definitive proof, and studies have reported inconsistent findings. This issue also extends to non-occupational noise, highlighting the need for further research in this area.
Despite advancements in diagnosing and treating noise-induced hearing disorders, several gaps remain in this field. One notable gap is the need for further investigation into the causes of tinnitus. While tinnitus is commonly assumed to originate from auditory sources, this assumption may not always hold true [329]. It is essential to explore potential non-auditory causes of tinnitus as well. Additionally, there is a need for research into the prevalence of tinnitus among non-adult populations and its correlations with factors such as gender, race, weather, and seasons. Most studies to date have focused on hearing impairment and related sound sources in the context of non-occupational noise, but occupational noise can also contribute to or exacerbate this condition [330]. Therefore, it would be prudent to include this disorder in future research involving employees exposed to occupational noise.
One important consideration is that organizations dedicated to addressing auditory health issues often develop and disseminate guidelines and legal documents based on existing research findings. These guidelines are typically intended for adherence by individuals and groups. However, due to the slow pace at which organizations can update their protocols in response to rapidly advancing research, these documents may not always reflect the most current findings. For instance, while the WHO and some other studies have stated that airplane noise is more disruptive than road or rail traffic noise [331–333], some experimental studies suggest that airplane noise might have a lesser impact on physiological sleep compared to the other two sources [334]. Therefore, further research is needed to evaluate the relative effects of different types of transportation noise on well-being, and guidelines should be revised to incorporate the latest evidence. Numerous research efforts have been dedicated to examining the effects of noise exposure in conjunction with other stressors in workplace environments. Despite the substantial evidence already available, investigations in this area are ongoing. However, there is a notable lack of comprehensive data regarding the simultaneous exposure to environmental stressors such as heat, air pollutants, and light, alongside environmental noise. To address this knowledge gap, further research is required to explore the combined effects of these environmental stressors. Another significant research gap in understanding the health effects of noise pertains to oxidative stress and the generation of free radicals. This indicates that more research is needed to understand how noise exposure might contribute to oxidative stress and the creation of free radicals, which could have serious health implications, such as increasing the risk of chronic diseases, cardiovascular problems, or even cancer. Reactive oxygen species (ROS), which are byproducts of cellular respiration, play a crucial role in various cellular processes when present at normal levels. However, excessive ROS can lead to oxidative damage to DNA, lipids, and proteins, ultimately resulting in cell death. Several studies have demonstrated that exposure to unsafe noise levels increases ROS production in the cochlea, leading to cellular damage in this area [335]. While the involvement of ROS in the exacerbation of NIHL is well-documented, the mechanisms by which these free radicals are generated through occupational noise and their potential generation through non-occupational noise remain unclear. Further research is needed to elucidate these processes and their implications for both types of noise exposure.
The health impacts of noise on human beings have often overlooked the role of genetics, which is a crucial aspect of this issue. Although some studies have investigated gene polymorphisms that might heighten susceptibility to hearing loss [336,337], the full extent of this genetic relationship remains unclear. Identifying specific genes that predispose individuals to adverse effects from noise exposure could substantially mitigate the incidence of noise-induced disorders and diseases. This approach could be integrated into pre-employment screenings or periodic health assessments, particularly for conditions like NIHL. Insights gained from such genetic research could also advance personalized medicine by tailoring preventative measures and treatments to individual genetic profiles.
Biomarkers are becoming increasingly relevant in assessing the health impacts of noise exposure. Despite the limited number of biomarkers available for evaluating auditory health, research efforts, such as those by Parham et al., have explored the potential of prestin protein biomarkers for indicating hearing loss. Their findings suggest that prestin levels in the bloodstream could serve as an alternative biomarker for NIHL. This research highlights the potential for developing more specific biomarkers to investigate the effects of noise exposure on human health, addressing existing gaps in the field. Additionally, the relationship between noise exposure and cancer warrants further examination. Although some studies have suggested a possible link between noise exposure and an increased risk of certain cancers, conclusive evidence is lacking. Thus, additional epidemiological research is needed to clarify the fundamental and biological mechanisms through which noise exposure may contribute to cancer development, especially in occupational settings [338,339].
In summary, future research should place special emphasis on the following areas:
First, standardizing methodologies and study designs is crucial for enabling more consistent comparisons and reliable conclusions across studies. This should include addressing the variability in statistical populations, noise sources, and research variables. Secondly, it is important to investigate the gender-specific impacts of noise, particularly on cardiovascular health and blood pressure, as these effects are currently underexplored. Additionally, research on the impact of noise on the human immune system, especially through more comprehensive human studies, is needed to bridge the gap between animal models and human health outcomes. Lastly, further investigation into the impact of noise characteristics, such as Gaussian distribution and frequency, on auditory and non-auditory health outcomes is warranted, particularly given the current focus on sound pressure levels alone. These areas offer substantial opportunities to advance our understanding of noise-related health risks.
5 Conclusion
In conclusion, this investigation underscores the varied consequences of noise exposure, which can be categorized into three key areas. First, established effects such as hearing impairment, oxidative stress, and elevated blood pressure should continue to be addressed through mitigation efforts, while exploring less understood secondary impacts. Second, for effects with ambiguous links – like memory impairment and nervous disorders – future research should prioritize cohort studies to provide clearer evidence, rather than relying on cross-sectional or laboratory approaches. Finally, emerging associations with conditions such as cancer and diabetes call for preliminary laboratory and cross-sectional research to build foundational evidence, followed by cohort studies for more definitive conclusions. Addressing these areas will advance our understanding of noise exposure’s health impacts and support more effective mitigation strategies.
Acknowledgements
We would like to thank those who helped us in conducting this research.
-
Funding information: The authors state no funding involved.
-
Author contributions: Mohammad Javad SheikhMozafari: investigation, methodology, writing – original draft, review, and editing. Mohammad Reza Monazzam Esmaeelpour: conceptualization, project administration, writing – review and editing. Soqrat Omari Shekaftik: investigation, writing – original draft, writing – review. Jamal Biganeh: investigation, methodology, writing – original draft. Fatameh Fasih Ramandi: methodology, formal analysis.
-
Conflict of interest: The authors state no conflict of interest.
-
Disclosure statement: No potential conflict of interest was reported by the author(s).
-
Ethics approval and consent to participate: Not applicable.
-
Data availability statement: The data sets used and/or analyzed in this study are given, and more details are available from the corresponding authors at reasonable request.
References
[1] Mohammad Alizadeh P, Ahmadi O, Shekoohiyan S, Sheikhmozafari MJ. Comprehensive analysis of acoustic properties of cellulose nano fibers absorbers: experimental and FEM-based mathematical modeling evaluation. Int J Environ Sci Technol. 2025;22:953–68. 10.1007/s13762-024-05849-5.Search in Google Scholar
[2] Hashemi Z, Asadi N, Sadeghian M, Putra A, Ahmadi S, Alidosti M, et al. Optimization and Comparative Analysis of micro-perforated panel sound absorbers: A study on structures and performance enhancement. Measurement. 2024;236:115123.10.1016/j.measurement.2024.115123Search in Google Scholar
[3] Sheikhmozafari MJ, Mohammad Alizadeh P, Ahmadi O, Mazloomi B. Assessment of noise effect on employee comfort in an open-plan office: validation of an assessment questionnaire. J Occup Health Epidemiol. 2021;10(3):193–203.10.52547/johe.10.3.193Search in Google Scholar
[4] Sheikhmozafari MJ, Ahmadi O. Reliability and validity assessment of the persian version of the noise exposure questionnaire (NEQ): An NIHL predictor tool. J Occup Health Epidemiol. 2022;11(3):209–22.10.61186/johe.11.3.209Search in Google Scholar
[5] Peris E, Fenech B. Associations and effect modification between transportation noise, self-reported response to noise and the wider determinants of health: A narrative synthesis of the literature. Sci Total Environ. 2020;748:141040.10.1016/j.scitotenv.2020.141040Search in Google Scholar PubMed
[6] Hemmati N, Sheikhmozafari M, Taban E, Tajik L, Faridan M. Pistachio shell waste as a sustainable sound absorber: an experimental and empirical investigation. Int J Environ Sci Technol. 2024;21(5):4867–80.10.1007/s13762-023-05413-7Search in Google Scholar
[7] Hemmati N, Mirzaei R, Soltani P, Berardi U, Mozafari MJS, Edalat H, et al. Acoustic and thermal performance of wood strands-rock wool-cement composite boards as eco-friendly construction materials. Constr Build Mater. 2024;445:137935.10.1016/j.conbuildmat.2024.137935Search in Google Scholar
[8] Organization WH. Environmental noise guidelines for the European region: World Health Organization. Regional Office for Europe; 2018.Search in Google Scholar
[9] Farooqi ZUR, Sabir M, Latif J, Aslam Z, Ahmad HR, Ahmad I, et al. Assessment of noise pollution and its effects on human health in industrial hub of Pakistan. Environ Sci Pollut Res. 2020;27(3):2819–28.10.1007/s11356-019-07105-7Search in Google Scholar PubMed
[10] Kerns E, Masterson EA, Themann CL, Calvert GM. Cardiovascular conditions, hearing difficulty, and occupational noise exposure within US industries and occupations. Am J Ind Med. 2018;61(6):477–91.10.1002/ajim.22833Search in Google Scholar PubMed PubMed Central
[11] Hegewald J, Schubert M, Wagner M, Dröge P, Prote U, Swart E, et al. Breast cancer and exposure to aircraft, road, and railway-noise: a case-control study based on health insurance records. Scand J Work Env Health. 2017;43(6):509–18.10.5271/sjweh.3665Search in Google Scholar PubMed
[12] Ishitake T. Wind turbine noise and health effects. Nihon Eiseigaku Zasshi. 2018;73(3):298–304.10.1265/jjh.73.298Search in Google Scholar PubMed
[13] Onchang R, Hawker DW. Community noise exposure and annoyance, activity interference, and academic achievement among university students. Noise Health. 2018;20(94):69–76.Search in Google Scholar
[14] Bevan R, Grantham-Hill S, Bowen R, Clayton E, Grice H, Venditti HC, et al. Sleep quality and noise: comparisons between hospital and home settings. Arch Dis Child. 2019;104(2):147–51.10.1136/archdischild-2018-315168Search in Google Scholar PubMed
[15] Rudolph KE, Shev A, Paksarian D, Merikangas KR, Mennitt DJ, James P, et al. Environmental noise and sleep and mental health outcomes in a nationally representative sample of urban US adolescents. Env Epidemiol. 2019;3(4):e056.10.1097/EE9.0000000000000056Search in Google Scholar PubMed PubMed Central
[16] Stansfeld S, Clark C, Smuk M, Gallacher J, Babisch W. Road traffic noise, noise sensitivity, noise annoyance, psychological and physical health and mortality. Env Health. 2021;20(1):32.10.1186/s12940-021-00720-3Search in Google Scholar PubMed PubMed Central
[17] Smith MG, Cordoza M, Basner M. Environmental noise and effects on sleep: an update to the WHO systematic review and meta-analysis. Environ health Perspect. 2022;130(7):076001.10.1289/EHP10197Search in Google Scholar PubMed PubMed Central
[18] Paciello F, Pisani A, Rinaudo M, Cocco S, Paludetti G, Fetoni AR, et al. Noise-induced auditory damage affects hippocampus causing memory deficits in a model of early age-related hearing loss. Neurobiol Dis. 2023;178:106024.10.1016/j.nbd.2023.106024Search in Google Scholar PubMed
[19] Mayes JL. Urban noise levels are high enough to damage auditory sensorineural health. Cities & Health. 2021;5(1–2):96–102.10.1080/23748834.2019.1577204Search in Google Scholar
[20] Natarajan N, Batts S, Stankovic KM. Noise-induced hearing loss. J Clin Med. 2023;12(6):2347.10.3390/jcm12062347Search in Google Scholar PubMed PubMed Central
[21] Nassur AM, Léger D, Lefèvre M, Elbaz M, Mietlicki F, Nguyen P, et al. Effects of aircraft noise exposure on heart rate during sleep in the population living near airports. Int J Env Res Public Health. 2019;16(2):269.10.3390/ijerph16020269Search in Google Scholar PubMed PubMed Central
[22] Zaman M, Muslim M, Jehangir A. Environmental noise-induced cardiovascular, metabolic and mental health disorders: a brief review. Environ Sci Pollut Res. 2022;29(51):76485–500.10.1007/s11356-022-22351-ySearch in Google Scholar PubMed
[23] Sivakumaran K, Ritonja JA, Waseem H, AlShenaibar L, Morgan E, Ahmadi SA, et al. Impact of noise exposure on risk of developing stress-related health effects related to the cardiovascular system: A systematic review and meta-analysis. Noise Health. 2022;24(114):107–29.10.4103/nah.nah_83_21Search in Google Scholar PubMed PubMed Central
[24] Petri D, Licitra G, Vigotti MA, Fredianelli L. Effects of exposure to road, railway, airport and recreational noise on blood pressure and hypertension. Int J Environ Res Public Health. 2021;18(17):9145.10.3390/ijerph18179145Search in Google Scholar PubMed PubMed Central
[25] Hegewald J, Schubert M, Freiberg A, Romero Starke K, Augustin F, Riedel-Heller SG, et al. Traffic noise and mental health: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(17):6175.10.3390/ijerph17176175Search in Google Scholar PubMed PubMed Central
[26] Thiesse L, Rudzik F, Spiegel K, Leproult R, Pieren R, Wunderli JM, et al. Adverse impact of nocturnal transportation noise on glucose regulation in healthy young adults: Effect of different noise scenarios. Env Int. 2018;121(Pt 1):1011–23.10.1016/j.envint.2018.05.036Search in Google Scholar PubMed
[27] Yan G, Meng Z, Liu N, He L, Paterson KB. Effects of irrelevant background speech on eye movements during reading. Q J Exp Psychol (Hove). 2018;71(6):1270–5.10.1080/17470218.2017.1339718Search in Google Scholar PubMed
[28] Kacem I, Kahloul M, Maoua M, Hafsia M, Brahem A, Limam M, et al. Occupational noise exposure and diabetes risk. J Environ Public Health. 2021;2021(1):1804616.10.1155/2021/1804616Search in Google Scholar PubMed PubMed Central
[29] Abbasi M, Nassiri P, Poshti RJT, Taghavi SM, Aarabi S, Madvari RF, et al. Investigation the relationship between occupational noise exposure and noise annoyance with blood pressure, serum cholesterol and triglyceride levels among workers of a textile industry. J Health Saf Work. 2018;8(3):223.Search in Google Scholar
[30] Yang Y, Zhang E, Zhang J, Chen S, Yu G, Liu X, et al. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in China: A meta-analysis. Medicine. 2018;97(30):e11720.10.1097/MD.0000000000011720Search in Google Scholar PubMed PubMed Central
[31] Abouee-Mehrizi A, Rasoulzadeh Y, Kazemi T, Mesgari-Abbasi M. Inflammatory and immunological changes caused by noise exposure: A systematic review. J Environ Sci Health, Part C. 2022;38(1):61–90.10.1080/26896583.2020.1715713Search in Google Scholar PubMed
[32] Ileperuma D, Arachchige IR. Hearing status and noise exposure levels of workers at a laundry plant in Sri Lanka. Audiol Speech Res. 2022;18(2):95–101.10.21848/asr.220004Search in Google Scholar
[33] Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383(9925):1325–32.10.1016/S0140-6736(13)61613-XSearch in Google Scholar PubMed PubMed Central
[34] Sakhvidi MJZ, Sakhvidi FZ, Mehrparvar AH, Foraster M, Dadvand P. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ Res. 2018;166:647–57.10.1016/j.envres.2018.05.011Search in Google Scholar PubMed
[35] Hammer MS, Swinburn TK, Neitzel RL. Environmental noise pollution in the United States: developing an effective public health response. Environ Health Perspect. 2014;122(2):115–9.10.1289/ehp.1307272Search in Google Scholar PubMed PubMed Central
[36] Smith MG, Ögren M, Thorsson P, Hussain-Alkhateeb L, Pedersen E, Forssén J, et al. A laboratory study on the effects of wind turbine noise on sleep: results of the polysomnographic WiTNES study. Sleep. 2020;43(9):zsaa046.10.1093/sleep/zsaa046Search in Google Scholar PubMed PubMed Central
[37] Hahad O, Kröller-Schön S, Daiber A, Münzel T. The cardiovascular effects of noise. Dtsch Ärzteblatt Int. 2019;116(14):245.10.3238/arztebl.2019.0245Search in Google Scholar PubMed PubMed Central
[38] Lin CY, Tsai PJ, Lin KY, Chen CY, Chung LH, Wu JL, et al. Will daytime occupational noise exposures induce nighttime sleep disturbance? Sleep Med. 2018;50:87–96.10.1016/j.sleep.2018.05.025Search in Google Scholar PubMed
[39] Thiesse L, Rudzik F, Kraemer JF, Spiegel K, Leproult R, Wessel N, et al. Transportation noise impairs cardiovascular function without altering sleep: The importance of autonomic arousals. Env Res. 2020;182:109086.10.1016/j.envres.2019.109086Search in Google Scholar PubMed
[40] Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Pieren R, et al. Transportation noise exposure, noise annoyance and respiratory health in adults: A repeated-measures study. Env Int. 2018;121(Pt 1):741–50.10.1016/j.envint.2018.10.006Search in Google Scholar PubMed
[41] Okokon EO, Yli-Tuomi T, Turunen AW, Tiittanen P, Juutilainen J, Lanki T. Traffic noise, noise annoyance and psychotropic medication use. Env Int. 2018;119:287–94.10.1016/j.envint.2018.06.034Search in Google Scholar PubMed
[42] Rojek M, Rajzer MW, Wojciechowska W, Drożdż T, Skalski P, Pizoń T, et al. Relationship among long-term aircraft noise exposure, blood pressure profile, and arterial stiffness. J Hypertens. 2019;37(7):1350–8.10.1097/HJH.0000000000002060Search in Google Scholar PubMed
[43] Selçuk AA. A guide for systematic reviews: PRISMA. Turkish Arch Otorhinolaryngology. 2019;57(1):57.10.5152/tao.2019.4058Search in Google Scholar PubMed PubMed Central
[44] Manohare M, Rajasekar E, Parida M, Vij S. Bibliometric analysis and review of auditory and non-auditory health impact due to road traffic noise exposure. Noise Mapp. 2022;9(1):67–88.10.1515/noise-2022-0005Search in Google Scholar
[45] Demirtas H, Saygun M, Muluk NB. Is there a relationship between occupational noise and hearing levels, sleep quality, and QoL of the factory workers? Neurol Sci. 2022;43(2):1015–23.10.1007/s10072-021-05458-xSearch in Google Scholar PubMed
[46] Staudt AM, Whitworth KW, Chien LC, Whitehead LW, de Porras DGR. Association of organic solvents and occupational noise on hearing loss and tinnitus among adults in the US, 1999–2004. Int Arch Occup Environ Health. 2019;92(3):403–13.10.1007/s00420-019-01419-2Search in Google Scholar PubMed PubMed Central
[47] Al-Rawi NH, Al Nuaimi AS, Sadiqi A, Azaiah E, Ezzeddine D, Ghunaim Q, et al. Occupational noise-induced hearing loss among dental professionals. Quintessence Int. 2019;50(3):245–50.Search in Google Scholar
[48] Buqammaz M, Gasana J, Alahmad B, Shebl M, Albloushi D. Occupational noise-induced hearing loss among migrant workers in Kuwait. Int J Environ Res Public Health. 2021;18(10):5295.10.3390/ijerph18105295Search in Google Scholar PubMed PubMed Central
[49] Erol I. Investigation of occupational noise-induced hearing loss of underground coal mines. Min Metall Explor. 2022;39(3):1045–60.10.1007/s42461-022-00585-1Search in Google Scholar
[50] Bandyopadhyay A, Ghosal R, Dasgupta P, Mukherjee A. Assessment of occupational noise generation and associated noise-induced hearing loss among employees of a black tea processing factory in Darjeeling District, India. IndianJ Occup Environ Med. 2022;26(3):183–8.10.4103/ijoem.ijoem_356_21Search in Google Scholar PubMed PubMed Central
[51] Cho S, Park WJ, Ahn JS, Lim DY, Kim SH, Moon JD. Obstructive sleep apnea risk and hearing impairment among occupational noise-exposed male workers. Arch Environ Occup Health. 2022.10.1080/19338244.2022.2094306Search in Google Scholar PubMed
[52] Frederiksen TW, Ramlau-Hansen CH, Stokholm ZA, Grynderup MB, Hansen AM, Kristiansen J, et al. Noise-induced hearing loss - A preventable disease? Results of a 10-year longitudinal study of workers exposed to occupational noise. Noise Health. 2017;19(87):103–11.Search in Google Scholar
[53] Thai T, Kucera P, Bernatik A. Noise pollution and its correlations with occupational noise-induced hearing loss in cement plants in Vietnam. Int J Environ Res Public Health. 2021;18(8):4229.10.3390/ijerph18084229Search in Google Scholar PubMed PubMed Central
[54] Gilbertson LR, Thies LE, Vosburgh DJ. Noise levels of amusement ride operators. J Occup Env Hyg. 2017;14(4):237–42.10.1080/15459624.2016.1250007Search in Google Scholar PubMed
[55] Liu QC, Duo CH, Wang Z, Yan K, Zhang J, Xiong W, et al. Analysis on occupational noise-induced hearing loss of different type workers in underground mining. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2017;35(11):852–4.Search in Google Scholar
[56] Sriopas A, Chapman RS, Sutammasa S, Siriwong W. Occupational noise-induced hearing loss in auto part factory workers in welding units in Thailand. J Occup Health. 2017;59(1):55–62.10.1539/joh.15-0291-OASearch in Google Scholar PubMed PubMed Central
[57] Yu SF, Chen GS, Jiao J, Gu GZ, Zhang HL, Wang XM, et al. A cohort study on occupational noise induced hearing loss in workers at an iron and steel plant. Zhonghua Yu Fang Yi Xue Za Zhi. 2017;51(1):13–9.Search in Google Scholar
[58] Almaayeh M, Al-Musa A, Khader YS. Prevalence of noise induced hearing loss among Jordanian industrial workers and its associated factors. Work. 2018;61(2):267–71.10.3233/WOR-182797Search in Google Scholar PubMed
[59] Sturman CJ, Frampton CM, Ten Cate WJF. Hearing loss asymmetry due to chronic occupational noise exposure. Otol Neurotol. 2018;39(8):e627–e34.10.1097/MAO.0000000000001908Search in Google Scholar PubMed
[60] Vaisbuch Y, Alyono JC, Kandathil C, Wu SH, Fitzgerald MB, Jackler RK. Occupational noise exposure and risk for noise-induced hearing loss due to temporal bone drilling. Otol Neurotol. 2018;39(6):693–9.10.1097/MAO.0000000000001851Search in Google Scholar PubMed
[61] Fredriksson S, Kim JL, Torén K, Magnusson L, Kähäri K, Söderberg M, et al. Working in preschool increases the risk of hearing-related symptoms: a cohort study among Swedish women. Int Arch Occup Env Health. 2019;92(8):1179–90.10.1007/s00420-019-01453-0Search in Google Scholar PubMed PubMed Central
[62] Siegel MG. The risk of noise-induced hearing loss performing knee replacement surgery. Noise Health. 2019;21(102):183–8.Search in Google Scholar
[63] Thepaksorn P, Koizumi A, Harada K, Siriwong W, Neitzel RL. Occupational noise exposure and hearing defects among sawmill workers in the south of Thailand. Int J Occup Saf Erg. 2019;25(3):458–66.10.1080/10803548.2017.1394710Search in Google Scholar PubMed
[64] Kerdonfag P, Wadwongtham W, Taneepanichskul S. Hearing threshold levels among steel industry workers in Samut Prakan, Thailand. Risk Manag Healthc Policy. 2019;12:57–66.10.2147/RMHP.S166042Search in Google Scholar PubMed PubMed Central
[65] Cole-Hunter T, So R, Amini H, Backalarz C, Brandt J, Bräuner EV, et al. Long-term exposure to road traffic noise and all-cause and cause-specific mortality: a Danish Nurse Cohort study. Sci Total Env. 2022;820:153057.10.1016/j.scitotenv.2022.153057Search in Google Scholar PubMed
[66] Danioth L, Brotschi G, Croy I, Friedrich H, Caversaccio MD, Negoias S. Multisensory environmental sensitivity in patients with chronic tinnitus. J Psychosom Res. 2020;135:110155.10.1016/j.jpsychores.2020.110155Search in Google Scholar PubMed
[67] Hahad O, Beutel M, Michal M, Schulz A, Pfeiffer N, Gianicolo E, et al. Noise annoyance in the German general population: Prevalence and determinants in the Gutenberg Health Study. Herz. 2022;47(3):265–79.10.1007/s00059-021-05060-zSearch in Google Scholar PubMed PubMed Central
[68] Kim CS, Grady ST, Hart JE, Laden F, VoPham T, Nguyen DD, et al. Long-term aircraft noise exposure and risk of hypertension in the Nurses’ Health Studies. Env Res. 2022;207:112195.10.1016/j.envres.2021.112195Search in Google Scholar PubMed PubMed Central
[69] Kourieh A, Giorgis-Allemand L, Bouaoun L, Lefevre M, Champelovier P, Lambert J, et al. Incident hypertension in relation to aircraft noise exposure: results of the DEBATS longitudinal study in France. Occup Environ Med. 2022;79(4):268–76.10.1136/oemed-2021-107921Search in Google Scholar PubMed
[70] Parker A, Parham K, Skoe E. Noise exposure levels predict blood levels of the inner ear protein prestin. Sci Rep. 2022;12(1):1154.10.1038/s41598-022-05131-zSearch in Google Scholar PubMed PubMed Central
[71] Sahu P, Galhotra A, Raj U, Ranjan RV. A study of self-reported health problems of the people living near railway tracks in Raipur city. J Family Med Prim Care. 2020;9(2):740–4.10.4103/jfmpc.jfmpc_1029_19Search in Google Scholar PubMed PubMed Central
[72] Silva BG, Gonzaga D, Rocha CH, Gomes RF, Moreira RR, Bistafa SR, et al. Noise exposure, headsets, and auditory and nonauditory symptoms in call center operators. Am J Audiol. 2022;31(1):112–25.10.1044/2021_AJA-21-00088Search in Google Scholar PubMed
[73] So R, Jørgensen JT, Lim YH, Mehta AJ, Amini H, Mortensen LH, et al. Long-term exposure to low levels of air pollution and mortality adjusting for road traffic noise: A Danish Nurse Cohort study. Env Int. 2020;143:105983.10.1016/j.envint.2020.105983Search in Google Scholar PubMed
[74] Song C, Li H, Ma H, Han T, Wu J. Effects of noise type and noise sensitivity on working memory and noise annoyance. Noise Health. 2022;24(114):173–81.10.4103/nah.nah_6_22Search in Google Scholar PubMed PubMed Central
[75] Sorensen M, Poulsen AH, Hvidtfeldt UA, Munzel T, Thacher JD, Ketzel M, et al. Transportation noise and risk of stroke: a nationwide prospective cohort study covering Denmark. Int J Epidemiol. 2021;50(4):1147–56.10.1093/ije/dyab024Search in Google Scholar PubMed
[76] Sørensen M, Poulsen AH, Kroman N, Hvidtfeldt UA, Thacher JD, Roswall N, et al. Road and railway noise and risk for breast cancer: A nationwide study covering Denmark. Env Res. 2021;195:110739.10.1016/j.envres.2021.110739Search in Google Scholar PubMed
[77] Su Y, Qin Z, Wang C, Wang H, Li C, Zhang X, et al. Relationship between occupational noise exposure and hypertension in male steel workers. Wei Sheng Yan Jiu. 2020;49(3):403–8.Search in Google Scholar
[78] Tagusari J, Matsui T. Estimation of health risk posed by road traffic noise in Japan based on the environmental noise guidelines for the European region. Nihon Eiseigaku Zasshi. Japanese J Hyg. 2021;76(0). 10.1265/jjh.19014.Search in Google Scholar PubMed
[79] Takihata S, Mizutari K, Morita I, Matsuo H, Nakayama A, Shimizu S, et al. The influence of a noisy environment on hearing impairment and tinnitus: The hearing outcomes of 50-year-old male Japan ground self-defense force personnel. Auris Nasus Larynx. 2020;47(6):931–7.10.1016/j.anl.2020.05.010Search in Google Scholar PubMed
[80] Tripathy DP, Rao DS. Occupational noise-induced hearing loss of workers in a bauxite mine in India. Noise Control Eng J. 2017;65(3):224–33.10.3397/1/376440Search in Google Scholar
[81] Wang TC, Chang TY, Tyler RS, Hwang BF, Chen YH, Wu CM, et al. Association between exposure to road traffic noise and hearing impairment: a case-control study. J Env Health Sci Eng. 2021;19(2):1483–9.10.1007/s40201-021-00704-ySearch in Google Scholar PubMed PubMed Central
[82] Worede EA, Yalew WW, Wami SD. Self reported hearing impairments and associated risk factors among metal and woodwork workers in Gondar Town, North West Ethiopia. Env Health Insights. 2022;16:11786302221084868.10.1177/11786302221084868Search in Google Scholar PubMed PubMed Central
[83] Wouters NL, Kaanen CI, den Ouden PJ, Schilthuis H, Böhringer S, Sorgdrager B, et al. Noise exposure and hearing loss among brewery workers in Lagos, Nigeria. Int J Env Res Public Health. 2020;17(8):2880.10.3390/ijerph17082880Search in Google Scholar PubMed PubMed Central
[84] Wu J, Wang F, Wang DM, Dai XY, Yi GL, Chen ZL. Investigation of occupational noise exposure and hearing loss among automobile manufacturing workers. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2021;39(8):593–7.Search in Google Scholar
[85] Yang S, Hu SQ, Huang W, Zhu XH, Sun K, Wang X. Analysis of hearing surveillance of noise-exposed workers in Zhuzhou city. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(3):227–31.Search in Google Scholar
[86] Albizu EJ, de Oliveira Gonçalves CG, de Lacerda ABM, Zeigelboim BS, Marques JM. Noise exposure and effects on hearing in Brazilian fishermen. Work. 2020;65(4):881–9.10.3233/WOR-203139Search in Google Scholar PubMed
[87] Michaud DS, Marro L, McNamee JP. High frequency hearing impairment and cardiovascular disease in Canada: Results from the Canadian Health Measures Survey. J Acoust Soc Am. 2021;150(2):1001.10.1121/10.0005589Search in Google Scholar PubMed
[88] Rahman A, Tuah NAA, Win KN, Lai ASC. A survey of noise-induced auditory symptoms in manufacturing workers in Brunei Darussalam. Int J Occup Saf Erg. 2022;28(2):1183–8.10.1080/10803548.2021.1876969Search in Google Scholar PubMed
[89] Feder K, Michaud D, McNamee J, Fitzpatrick E, Davies H, Leroux T. Prevalence of hazardous occupational noise exposure, hearing loss, and hearing protection usage among a representative sample of working canadians. J Occup Env Med. 2017;59(1):92–113.10.1097/JOM.0000000000000920Search in Google Scholar PubMed PubMed Central
[90] Boger ME, Sampaio ALL, de Oliveira CACP. Analysis of hearing and tinnitus in workers exposed to occupational noise. Int Tinnitus J. 2016;20(2):88–92.10.5935/0946-5448.20160017Search in Google Scholar PubMed
[91] Frederiksen TW, Ramlau-Hansen CH, Stokholm ZA, Grynderup MB, Hansen AM, Lund SP, et al. Occupational noise exposure, psychosocial working conditions and the risk of tinnitus. Int Arch Occup Environ Health. 2017;90(2):217–25.10.1007/s00420-016-1189-4Search in Google Scholar PubMed
[92] Marchiori LLM, Dias ACM, Gonçalvez AS, Poly-Frederico RC, Doi MY. Association between polymorphism of tumor necrosis factor alpha (tnfα) in the region -308 g/a with tinnitus in the elderly with a history of occupational noise exposure. Noise Health. 2018;20(93):37–41.Search in Google Scholar
[93] Couth S, Mazlan N, Moore DR, Munro KJ, Dawes P. Hearing difficulties and tinnitus in construction, agricultural, music, and finance industries: contributions of demographic, health, and lifestyle factors. Trends Hear. 2019;23:2331216519885571.10.1177/2331216519885571Search in Google Scholar PubMed PubMed Central
[94] Blume C, Schoch SF, Vienneau D, Roosli M, Kohler M, Moeller A, et al. Association of transportation noise with sleep during the first year of life: A longitudinal study. Environ Res. 2022;203:111776.10.1016/j.envres.2021.111776Search in Google Scholar PubMed
[95] Thacher JD, Poulsen AH, Raaschou-Nielsen O, Hvidtfeldt UA, Brandt J, Christensen JH, et al. Exposure to transportation noise and risk for cardiovascular disease in a nationwide cohort study from Denmark. Environ Res. 2022;211:113106.10.1016/j.envres.2022.113106Search in Google Scholar PubMed
[96] Thacher JD, Poulsen AH, Roswall N, Hvidtfeldt U, Raaschou-Nielsen O, Jensen SS, et al. Road traffic noise exposure and filled prescriptions for antihypertensive medication: A Danish cohort study. Env Health Perspect. 2020;128(5):57004.10.1289/EHP6273Search in Google Scholar PubMed PubMed Central
[97] Fredriksson S, Hussain-Alkhateeb L, Toren K, Sjostrom M, Selander J, Gustavsson P, et al. The impact of occupational noise exposure on hyperacusis: a longitudinal population study of female workers in Sweden. Ear Hearing. 2022;43(4):1366–77.10.1097/AUD.0000000000001194Search in Google Scholar PubMed PubMed Central
[98] Alkhalawi E, Orban E, Schramm S, Katsarava Z, Hoffmann B, Moebus S. Residential traffic noise exposure and headaches: Results from the population-based heinz nixdorf recall study. Noise Health. 2021;23(108):1–10.10.4103/nah.NAH_1_20Search in Google Scholar PubMed PubMed Central
[99] Andersson EM, Ögren M, Molnár P, Segersson D, Rosengren A, Stockfelt L. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Env Res. 2020;185:109446.10.1016/j.envres.2020.109446Search in Google Scholar PubMed
[100] Dunbar C, Catcheside P, Lechat B, Hansen K, Zajamsek B, Liebich T, et al. EEG power spectral responses to wind farm compared with road traffic noise during sleep: A laboratory study. J Sleep Res. 2022;31(3):e13517.10.1111/jsr.13517Search in Google Scholar PubMed
[101] Escobar-Castro DI, Vivas-Cortés MJ, Espinosa-Cepeda CP, Zamora-Romero AM, Peñuela-Epalza ME. Hearing loss symptoms and leisure noise exposure in university students in Barranquilla. Colomb Codas. 2021;34(1):e20200379.10.1590/2317-1782/20212020379Search in Google Scholar PubMed PubMed Central
[102] Filova A, Jurkovicova J, Hirosova K, Vondrova D, Filova B, Samohyl M, et al. Social noise exposure in a sample of Slovak university students. Int J Env Res Public Health. 2020;17(1):324.10.3390/ijerph17010324Search in Google Scholar PubMed PubMed Central
[103] Thacher JD, Hvidtfeldt UA, Poulsen AH, Raaschou-Nielsen O, Ketzel M, Brandt J, et al. Long-term residential road traffic noise and mortality in a Danish cohort. Env Res. 2020;187:109633.10.1016/j.envres.2020.109633Search in Google Scholar PubMed
[104] Thacher JD, Poulsen AH, Hvidtfeldt UA, Raaschou-Nielsen O, Ketzel M, Jensen SS, et al. Long-term exposure to transportation noise and risk for atrial fibrillation: A Danish nationwide cohort study. Env Res. 2022;207:112167.10.1016/j.envres.2021.112167Search in Google Scholar PubMed
[105] Abd El-Salam NM, Ismail EI, El-Sharabasy AE. Evaluation of cervical vestibular evoked myogenic potential in subjects with chronic noise exposure. J Int Adv Otol. 2017;13(3):358–62.10.5152/iao.2017.4214Search in Google Scholar PubMed
[106] Yilmaz N, Ila K, Soylemez E, Ozdek A. Evaluation of vestibular system with vHIT in industrial workers with noise-induced hearing loss. Eur Arch Otorhinolaryngol. 2018;275(11):2659–65.10.1007/s00405-018-5125-ySearch in Google Scholar PubMed
[107] Evandt J, Oftedal B, Hjertager Krog N, Nafstad P, Schwarze PE, Marit Aasvang G. A population-based study on nighttime road traffic noise and insomnia. Sleep. 2017;40(2):zsw055.10.1093/sleep/zsw055Search in Google Scholar PubMed
[108] Evandt J, Oftedal B, Krog NH, Skurtveit S, Nafstad P, Schwarze PE, et al. Road traffic noise and registry based use of sleep medication. Environ Health. 2017;16.10.1186/s12940-017-0330-5Search in Google Scholar PubMed PubMed Central
[109] Wang DM, Li WZ, Xiao Y, Feng XB, Liu W, Chen WH. Association between occupational noise exposure and the risk of cardiovascular diseases. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2022;40(3):183–7.Search in Google Scholar
[110] Gilani TA, Mir MS. A study on road traffic noise exposure and prevalence of insomnia. Environ Sci Pollut Res. 2022;29(27):41065–80.10.1007/s11356-021-18291-8Search in Google Scholar PubMed
[111] Myllyntausta S, Virkkala J, Salo P, Varjo J, Rekola L, Hongisto V. Effect of the frequency spectrum of road traffic noise on sleep: A polysomnographic study. J Acoustical Soc Am. 2020;147(4):2139–49.10.1121/10.0000985Search in Google Scholar PubMed
[112] Weyde KV, Krog NH, Oftedal B, Evandt J, Magnus P, Øverland S, et al. Nocturnal road traffic noise exposure and children’s sleep duration and sleep problems. Int J Env Res Public Health. 2017;14(5):491.10.3390/ijerph14050491Search in Google Scholar PubMed PubMed Central
[113] Azadboni ZD, Talarposhti RJ, Ghaljahi M, Mehri A, Aarabi S, Poursadeghiyan M, et al. Effect of occupational noise exposure on sleep among workers of textile industry. J Clin Diagn Res. 2018;12(3):LC18–21.10.7860/JCDR/2018/26084.11334Search in Google Scholar
[114] Bartels S, Ogren M, Kim JL, Fredriksson S, Waye KP. The impact of nocturnal road traffic noise, bedroom window orientation, and work-related stress on subjective sleep quality: results of a cross-sectional study among working women. Int Arch Occup Environ Health. 2021;94(7):1523–36.10.1007/s00420-021-01696-wSearch in Google Scholar PubMed PubMed Central
[115] Casario K, Howard K, Smith MG, Rocha S, White M, Basner M. The effects of nocturnal aircraft noise on self-reported sleep. Sleep. 2020;43:A73–4.10.1093/sleep/zsaa056.185Search in Google Scholar
[116] Elmenhorst EM, Griefahn B, Rolny V, Basner M. Comparing the effects of road, railway, and aircraft noise on sleep: exposure-response relationships from pooled data of three laboratory studies. Int J Environ Res Public Health. 2019;16(6):1073.10.3390/ijerph16061073Search in Google Scholar PubMed PubMed Central
[117] Li DK, Wang LL, Yang YP, Hu YH, Wang YJ, Tian YH, et al. Associations of long-term exposure to ambient air pollution and road traffic noise with sleep health in UK Biobank. J Affect Disord. 2022;310:1–9.10.1016/j.jad.2022.04.136Search in Google Scholar PubMed
[118] McGuire S, Witte M, Kallarackal A, Basner M. Pilot study examining the effects of aircraft noise on sleep in communities near philadelphia international airport. Sleep. 2017;40:A60–A1.10.1093/sleepj/zsx050.161Search in Google Scholar
[119] Moroe NF. Occupational noise-induced hearing loss in the mining sector of South Africa: Perspectives of occupational health practitioners on how mineworkers are trained. South Afr J Commun Disord. 2020;67(2):1–6.10.4102/sajcd.v67i2.676Search in Google Scholar PubMed PubMed Central
[120] Nassur AM, Leger D, Lefevre M, Elbaz M, Mietlicki F, Nguyen P, et al. The impact of aircraft noise exposure on objective parameters of sleep quality: results of the DEBATS study in France. Sleep Med. 2019;54:70–7.10.1016/j.sleep.2018.10.013Search in Google Scholar PubMed
[121] Nassur AM, Lefevre M, Laumon B, Leger D, Evrard AS. Aircraft noise exposure and subjective sleep quality: the results of the DEBATS study in france. Behav Sleep Med. 2019;17(4):502–13.10.1080/15402002.2017.1409224Search in Google Scholar PubMed
[122] Smith MG, Younes M, Aeschbach D, Muller U, Basner M. Planes, trains and automobiles: Traffic noise and its impact on sleep depth measured by odds ratio product. Sleep. 2019;42:A54.10.1093/sleep/zsz067.130Search in Google Scholar
[123] Teoh T, Olson C. Effects of ambient noise on sleep in New York City. J Transp Health. 2018;9:S44.10.1016/j.jth.2018.05.027Search in Google Scholar
[124] Zhang L, Ma H. The effects of environmental noise on children?s cognitive performance and annoyance. Appl Acoust. 2022;198:108995.10.1016/j.apacoust.2022.108995Search in Google Scholar
[125] Rudzik F, Thiesse L, Pieren R, Wunderli JM, Brink M, Foraster M, et al. Sleep spindle characteristics and arousability from nighttime transportation noise exposure in healthy young and older individuals. Sleep. 2018;41(7):zsy077.10.1093/sleep/zsy077Search in Google Scholar PubMed
[126] Eriksson C, Bodin T, Selander J. Burden of disease from road traffic and railway noise–a quantification of healthy life years lost in Sweden. Scand J Work Environ Health. 2017;43(6):519–25.10.5271/sjweh.3653Search in Google Scholar PubMed
[127] Lim HM, Kang W, Park WJ, Jang KH, Ann JS, Moon JD. Insomnia and hearing impairment among occupational noise exposed male workers. Ann Occup Env Med. 2017;29:36.10.1186/s40557-017-0195-7Search in Google Scholar PubMed PubMed Central
[128] Skrzypek M, Kowalska M, Czech EM, Niewiadomska E, Zejda JE. Impact of road traffic noise on sleep disturbances and attention disorders amongst school children living in Upper Silesian Industrial Zone, Poland. Int J Occup Med Env Health. 2017;30(3):511–20.10.13075/ijomeh.1896.00823Search in Google Scholar PubMed
[129] Carugno M, Imbrogno P, Zucchi A, Ciampichini R, Tereanu C, Sampietro G, et al. Effects of aircraft noise on annoyance, sleep disorders, and blood pressure among adult residents near the Orio al Serio International Airport (BGY), Italy. Med Lav. 2018;109(4):253–63.10.23749/mdl.v109i4.7271Search in Google Scholar PubMed PubMed Central
[130] Dzhambov AM, Markevych I, Tilov B, Arabadzhiev Z, Stoyanov D, Gatseva P, et al. Pathways linking residential noise and air pollution to mental ill-health in young adults. Env Res. 2018;166:458–65.10.1016/j.envres.2018.06.031Search in Google Scholar PubMed
[131] Basner M, Witte M, McGuire S. Aircraft noise effects on sleep-results of a pilot study near Philadelphia International Airport. Int J Env Res Public Health. 2019;16(17):3178.10.3390/ijerph16173178Search in Google Scholar PubMed PubMed Central
[132] Jensen HAR, Rasmussen B, Ekholm O. Neighbour noise annoyance is associated with various mental and physical health symptoms: results from a nationwide study among individuals living in multi-storey housing. BMC Public Health. 2019;19(1):1508.10.1186/s12889-019-7893-8Search in Google Scholar PubMed PubMed Central
[133] Asghari M. Tinnitus characteristics at high-and low-risk occupations from occupational noise exposure standpoint. Int Tinnitus J. 2021;25(1):87–93.10.5935/0946-5448.20210016Search in Google Scholar PubMed
[134] Bai L, Shin S, Oiamo TH, Burnett RT, Weichenthal S, Jerrett M, et al. Exposure to road traffic noise and incidence of acute myocardial infarction and congestive heart failure: a population-based cohort study in Toronto, Canada. Environ Health Perspect. 2020;128(8):087001.10.1289/EHP5809Search in Google Scholar PubMed PubMed Central
[135] Baudin C, Lefèvre M, Babisch W, Cadum E, Champelovier P, Dimakopoulou K, et al. The role of aircraft noise annoyance and noise sensitivity in the association between aircraft noise levels and hypertension risk: Results of a pooled analysis from seven European countries. Env Res. 2020;191:110179.10.1016/j.envres.2020.110179Search in Google Scholar PubMed
[136] Baudin C, Lefevre M, Champelovier P, Lambert J, Laumon B, Evrard AS. Self-rated health status in relation to aircraft noise exposure, noise annoyance or noise sensitivity: the results of a cross-sectional study in France. BMC Public Health. 2021;21(1):1–11.10.1186/s12889-020-10138-0Search in Google Scholar PubMed PubMed Central
[137] Biel R, Danieli C, Shekarrizfard M, Minet L, Abrahamowicz M, Baumgartner J, et al. Acute cardiovascular health effects in a panel study of personal exposure to traffic-related air pollutants and noise in Toronto, Canada. Sci Rep. 2020;10(1):16703.10.1038/s41598-020-73412-6Search in Google Scholar PubMed PubMed Central
[138] Bosch A, Kannenkeril D, Jung S, Striepe K, Karg MV, Ott C, et al. The influence of aircraft noise exposure on the systemic and renal haemodynamics. Eur J Prev Cardiol. 2022;29(1):116–24.10.1093/eurjpc/zwaa036Search in Google Scholar PubMed
[139] Burns-O’Connell G, Stockdale D, Cassidy O, Knowles V, Hoare DJ. Surrounded by sound: The impact of tinnitus on musicians. Int J Env Res Public Health. 2021;18(17):9036.10.3390/ijerph18179036Search in Google Scholar PubMed PubMed Central
[140] Bustaffa E, Curzio O, Donzelli G, Gorini F, Linzalone N, Redini M, et al. Risk associations between vehicular traffic noise exposure and cardiovascular diseases: a residential retrospective cohort study. Int J Env Res Public Health. 2022;19(16):10034.10.3390/ijerph191610034Search in Google Scholar PubMed PubMed Central
[141] Cai C, Xu Y, Wang Y, Wang Q, Liu L. Experimental study on the effect of urban road traffic noise on heart rate variability of noise-sensitive people. Front Psychol. 2021;12:749224.10.3389/fpsyg.2021.749224Search in Google Scholar PubMed PubMed Central
[142] Cai Y, Zijlema WL, Sørgjerd EP, Doiron D, de Hoogh K, Hodgson S, et al. Impact of road traffic noise on obesity measures: Observational study of three European cohorts. Env Res. 2020;191:110013.10.1016/j.envres.2020.110013Search in Google Scholar PubMed
[143] Carneiro Muniz CMD, da Silva SFS, Façanha RC, Bassi-Dibai D, Silva FB, Felipe IMA, et al. Audiological and noise exposure findings among members of a Brazilian folklore music group. Work. 2021;68(1):235–41.10.3233/WOR-203370Search in Google Scholar PubMed
[144] Cerletti P, Eze IC, Schaffner E, Foraster M, Viennau D, Cajochen C, et al. The independent association of source-specific transportation noise exposure, noise annoyance and noise sensitivity with health-related quality of life. Environ Int. 2020;143:105960.10.1016/j.envint.2020.105960Search in Google Scholar PubMed
[145] Chang TY, Wu YY, Wang VS, Bao BY, Liu CS. Short-term exposure to noise on stroke volume and left ventricular contractility: A repeated-measure study. Env Pollut. 2020;263(Pt A):114670.10.1016/j.envpol.2020.114670Search in Google Scholar PubMed
[146] Chere B, Kirkham N. The negative impact of noise on adolescents’ executive function: an online study in the context of home-learning during a pandemic. Front Psychol. 2021;12:715301.10.3389/fpsyg.2021.715301Search in Google Scholar PubMed PubMed Central
[147] Cole-Hunter T, Dehlendorff C, Amini H, Mehta A, Lim YH, Jorgensen JT, et al. Long-term exposure to road traffic noise and stroke incidence: a Danish Nurse Cohort study. Environ Health. 2021;20(1):115.10.1186/s12940-021-00802-2Search in Google Scholar PubMed PubMed Central
[148] Dierickx M, Verschraegen S, Wierinck E, Willems G, van Wieringen A. Noise disturbance and potential hearing loss due to exposure of dental equipment in Flemish Dentists. Int J Env Res Public Health. 2021;18(11):5617.10.3390/ijerph18115617Search in Google Scholar PubMed PubMed Central
[149] Ebben MR, Yan P, Krieger AC. The effects of white noise on sleep and duration in individuals living in a high noise environment in New York City. Sleep Med. 2021;83:256–9.10.1016/j.sleep.2021.03.031Search in Google Scholar PubMed
[150] Veber T, Tamm T, Ründva M, Kriit HK, Pyko A, Orru H. Health impact assessment of transportation noise in two Estonian cities. Env Res. 2022;204(Pt C):112319.10.1016/j.envres.2021.112319Search in Google Scholar PubMed
[151] Wang SS, Glied S, Williams S, Will B, Muennig PA. Impact of aeroplane noise on mental and physical health: a quasi-experimental analysis. BMJ Open. 2022;12(5):e057209.10.1136/bmjopen-2021-057209Search in Google Scholar PubMed PubMed Central
[152] Amoatey P, Al-Harthy I, Al-Jabri K, Al-Mamun A, Baawain MS, Al-Mayahi A. Impact of COVID-19 pandemic on aircraft noise levels, annoyance, and health effects in an urban area in Oman. Env Sci Pollut Res Int. 2022;29(16):23407–18.10.1007/s11356-021-17514-2Search in Google Scholar PubMed PubMed Central
[153] Lin YT, Chen TW, Chang YC, Chen ML, Hwang BF. Relationship between time-varying exposure to occupational noise and incident hypertension: A prospective cohort study. Int J Hyg Env Health. 2020;226:113487.10.1016/j.ijheh.2020.113487Search in Google Scholar PubMed
[154] Nari F, Kim YK, Kang SH, Park EC, Jang SI. Association between Occupational Noise and Vibration Exposure and Insomnia among Workers in Korea. Life (Basel). 2020;10(4):46.10.3390/life10040046Search in Google Scholar PubMed PubMed Central
[155] Nguyen TL, Trieu BL, Hiraguri Y, Morinaga M, Morihara T, Yano T. Effects of changes in acoustic and non-acoustic factors on public health and reactions: Follow-up surveys in the vicinity of the Hanoi Noi Bai International Airport. Int J Env Res Public Health. 2020;17(7):2597.10.3390/ijerph17072597Search in Google Scholar PubMed PubMed Central
[156] Peltz JS. The day-to-day impact of nighttime noise disturbances on college students’ psychological functioning. J Am Coll Health. 2022;70(7):2061–9.10.1080/07448481.2020.1842422Search in Google Scholar PubMed
[157] Rojek M, Wojciechowska W, Januszewicz A, Czarnecka D, Skalski P, Rajzer M. The relation of nocturnal exposure to aircraft noise and aircraft noise-induced insomnia with blood pressure. Pol Arch Intern Med. 2021;131(1):33–41.10.20452/pamw.15716Search in Google Scholar PubMed
[158] Roswall N, Poulsen AH, Thacher JD, Hvidtfeldt UA, Raaschou-Nielsen O, Jensen SS, et al. Nighttime road traffic noise exposure at the least and most exposed façades and sleep medication prescription redemption-a Danish cohort study. Sleep. 2020;43(8):zsaa029.10.1093/sleep/zsaa029Search in Google Scholar PubMed
[159] Liu Y, Xia B, Cui C, Skitmore M. Community response to construction noise in three central cities of Zhejiang province, China. Env Pollut. 2017;230:1009–17.10.1016/j.envpol.2017.07.058Search in Google Scholar PubMed
[160] Bagheri Hosseinabadi M, Khanjani N, Münzel T, Daiber A, Yaghmorloo M. Chronic occupational noise exposure: Effects on DNA damage, blood pressure, and serum biochemistry. Mutat Res Genet Toxicol Env Mutagen. 2019;841:17–22.10.1016/j.mrgentox.2019.04.006Search in Google Scholar PubMed
[161] Fuks KB, Wigmann C, Altug H, Schikowski T. Road Traffic Noise at the Residence, Annoyance, and Cognitive Function in Elderly Women. Int J Environ Res Public Health. 2019;16(10):1790.10.3390/ijerph16101790Search in Google Scholar PubMed PubMed Central
[162] Gille LA, Marquis-Favre C, Lam KC. Partial and total annoyance due to road traffic noise combined with aircraft or railway noise: Structural equation analysis. Int J Environ Res Public Health. 2017;14(12):1478.10.3390/ijerph14121478Search in Google Scholar PubMed PubMed Central
[163] Khomenko S, Cirach M, Barrera-Gómez J, Pereira-Barboza E, Iungman T, Mueller N, et al. Impact of road traffic noise on annoyance and preventable mortality in European cities: A health impact assessment. Env Int. 2022;162:107160.10.1016/j.envint.2022.107160Search in Google Scholar PubMed
[164] Bartels S, Rooney D, Muller U. Assessing aircraft noise-induced annoyance around a major German airport and its predictors via telephone survey - The COSMA study. Transp Res Part D-Transp Environ. 2018;59:246–58.10.1016/j.trd.2018.01.015Search in Google Scholar
[165] Brink M, Schaffer B, Vienneau D, Foraster M, Pieren R, Eze IC, et al. A survey on exposure-response relationships for road, rail, and aircraft noise annoyance: Differences between continuous and intermittent noise. Environ Int. 2019;125:277–90.10.1016/j.envint.2019.01.043Search in Google Scholar PubMed
[166] Janson E, Johannessen A, Holm M, Franklin K, Holst GJ, Gislason T, et al. Insomnia associated with traffic noise and proximity to traffic-a cross-sectional study of the Respiratory Health in Northern Europe III population. J Clin Sleep Med. 2020;16(4):545–52.10.5664/jcsm.8274Search in Google Scholar PubMed PubMed Central
[167] Monazzam MR, Zakerian SA, Kazemi Z, Ebrahimi MH, Ghaljahi M, Mehri A, et al. Investigation of occupational noise annoyance in a wind turbine power plant. J Low Freq Noise Vib Act Control. 2019;38(2):798–807.10.1177/1461348418769162Search in Google Scholar
[168] Ogren M, Gidlof-Gunnarsson A, Smith M, Gustavsson S, Waye KP. Comparison of Annoyance from Railway Noise and Railway Vibration. Int J Environ Res Public Health. 2017;14(7):805.10.3390/ijerph14070805Search in Google Scholar PubMed PubMed Central
[169] Park HK. Indoor noise annoyance due to transportation noise. J Asian Archit Build Eng. 2018;17(1):149–55.10.3130/jaabe.17.149Search in Google Scholar
[170] Preisendorfer P, Liebe U, Enzler HB, Diekmann A. Annoyance due to residential road traffic and aircraft noise: Empirical evidence from two European cities. Environ Res. 2022;206:112269.10.1016/j.envres.2021.112269Search in Google Scholar PubMed
[171] Quehl J, Muller U, Mendolia F. Short-term annoyance from nocturnal aircraft noise exposure: results of the NORAH and STRAIN sleep studies. Int Arch Occup Environ Health. 2017;90(8):765–78.10.1007/s00420-017-1238-7Search in Google Scholar PubMed
[172] Tinnam P, Yodpijit N, Jongprasithporn M, Junsupasen S. Assessment of environmental noise annoyance: A case study of industrial noise in Thailand. 2021 IEEE International Conference on Industrial Engineering and Engineering Management (IEEM). IEEE; 2021. p. 1412–6.10.1109/IEEM50564.2021.9672800Search in Google Scholar
[173] Zamorano-Gonzalez B, Pena-Cardenas F, Velazquez-Narvaez Y, Parra-Sierra V, Vargas-Martinez JI, Monreal-Aranda O, et al. Traffic noise annoyance in the population of North Mexico: Case study on the daytime period in the city of Matamoros. Front Psychol. 2021;12:657428.10.3389/fpsyg.2021.657428Search in Google Scholar PubMed PubMed Central
[174] Brännström KJ, Johansson E, Vigertsson D, Morris DJ, Sahlén B, Lyberg-Åhlander V. How children perceive the acoustic environment of their school. Noise Health. 2017;19(87):84.Search in Google Scholar
[175] Sung JH, Lee J, Jeong KS, Lee S, Lee C, Jo MW, et al. Influence of transportation noise and noise sensitivity on annoyance: A cross-sectional study in South Korea. Int J Env Res Public Health. 2017;14(3):322.10.3390/ijerph14030322Search in Google Scholar PubMed PubMed Central
[176] Yokoshima S, Morihara T, Sato T, Yano T. Combined effects of high-speed railway noise and ground vibrations on annoyance. Int J Env Res Public Health. 2017;14(8):845.10.3390/ijerph14080845Search in Google Scholar PubMed PubMed Central
[177] Baudin C, Lefèvre M, Champelovier P, Lambert J, Laumon B, Evrard AS. Aircraft noise and psychological ill-health: the results of a cross-sectional study in France. Int J Env Res Public Health. 2018;15(8):1642.10.3390/ijerph15081642Search in Google Scholar PubMed PubMed Central
[178] Nguyen TL, Nguyen TL, Morinaga M, Yokoshima S, Yano T, Sato T, et al. Community response to a step change in the aircraft noise exposure around Hanoi Noi Bai International Airport. J Acoust Soc Am. 2018;143(5):2901.10.1121/1.5037567Search in Google Scholar PubMed
[179] Schäffer B, Pieren R, Schlittmeier SJ, Brink M. Effects of different spectral shapes and amplitude modulation of broadband noise on annoyance reactions in a controlled listening experiment. Int J Env Res Public Health. 2018;15(5):1029.10.3390/ijerph15051029Search in Google Scholar PubMed PubMed Central
[180] Wallas A, Eriksson C, Gruzieva O, Lind T, Pyko A, Sjöström M, et al. Road traffic noise and determinants of saliva cortisol levels among adolescents. Int J Hyg Env Health. 2018;221(2):276–82.10.1016/j.ijheh.2017.11.003Search in Google Scholar PubMed
[181] Taghipour A, Pieren R, Schäffer B. Short-term annoyance reactions to civil helicopter and propeller-driven aircraft noise: A laboratory experiment. J Acoust Soc Am. 2019;145(2):956.10.1121/1.5090500Search in Google Scholar PubMed
[182] Paiva KM, Cardoso MRA, Zannin PHT. Exposure to road traffic noise: Annoyance, perception and associated factors among Brazil’s adult population. Sci Total Env. 2019;650(Pt 1):978–86.10.1016/j.scitotenv.2018.09.041Search in Google Scholar PubMed
[183] Farooqi ZUR, Ahmad I, Zeeshan N, Ilić P, Imran M, Saeed MF. Urban noise assessment and its nonauditory health effects on the residents of Chiniot and Jhang, Punjab, Pakistan. Env Sci Pollut Res Int. 2021;28(39):54909–21.10.1007/s11356-021-14340-4Search in Google Scholar PubMed
[184] Faulkner JP, Murphy E. Estimating the harmful effects of environmental transport noise: An EU study. Sci Total Env. 2022;811:152313.10.1016/j.scitotenv.2021.152313Search in Google Scholar PubMed
[185] Gabinet NM, Portnov BA. Assessing the impacts of ALAN and noise proxies on sleep duration and quality: evidence from a nation-wide survey in Israel. Chronobiol Int. 2021;38(5):638–58.10.1080/07420528.2021.1886111Search in Google Scholar PubMed
[186] Gilani TA, Mir MS. Association of road traffic noise exposure and prevalence of coronary artery disease: A cross-sectional study in North India. Environ Sci Pollut Res. 2021;28(38):53458–77.10.1007/s11356-021-14582-2Search in Google Scholar PubMed PubMed Central
[187] Gilani TA, Mir MS. A study on the assessment of traffic noise induced annoyance and awareness levels about the potential health effects among residents living around a noise-sensitive area. Env Sci Pollut Res Int. 2021;28(44):63045–64.10.1007/s11356-021-15208-3Search in Google Scholar PubMed PubMed Central
[188] Glaubitz L, Stumme J, Lucht S, Moebus S, Schramm S, Jockwitz C, et al. Association between long-term air pollution, chronic traffic noise, and resting-state functional connectivity in the 1000BRAINS study. Env Health Perspect. 2022;130(9):97007.10.1289/EHP9737Search in Google Scholar PubMed PubMed Central
[189] González DM, Morillas JMB, Rey-Gozalo G. Effects of noise on pedestrians in urban environments where road traffic is the main source of sound. Sci Total Env. 2022;857:159406.10.1016/j.scitotenv.2022.159406Search in Google Scholar PubMed
[190] Hahad O, Wild PS, Prochaska JH, Schulz A, Lackner KJ, Pfeiffer N, et al. Midregional pro atrial natriuretic peptide: a novel important biomarker for noise annoyance-induced cardiovascular morbidity and mortality? Clin Res Cardiol. 2021;110(1):29–39.10.1007/s00392-020-01645-6Search in Google Scholar PubMed PubMed Central
[191] Hanibuchi T, Nakaya T, Kitajima T, Yatsuya H. Associations of insomnia with noise annoyance and neighborhood environments: A nationwide cross-sectional study in Japan. Prev Med Rep. 2021;23:101416.10.1016/j.pmedr.2021.101416Search in Google Scholar PubMed PubMed Central
[192] Jafari Z, Copps T, Hole G, Nyatepe-Coo F, Kolb BE, Mohajerani MH. Tinnitus, sound intolerance, and mental health: the role of long-term occupational noise exposure. Eur Arch Otorhinolaryngol. 2022;279(11):5161–70.10.1007/s00405-022-07362-2Search in Google Scholar PubMed
[193] Weidenfeld S, Sanok S, Fimmers R, Puth MT, Aeschbach D, Elmenhorst EM. Short-term annoyance due to night-time road, railway, and air traffic noise: role of the noise source, the acoustical metric, and non-acoustical factors. Int J Env Res Public Health. 2021;18(9):4647.10.3390/ijerph18094647Search in Google Scholar PubMed PubMed Central
[194] Wolf K, Kraus U, Dzolan M, Bolte G, Lakes T, Schikowski T, et al. Nighttime transportation noise annoyance in Germany: personal and regional differences in the German National Cohort Study. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2020;63(3):332–43.10.1007/s00103-020-03094-ySearch in Google Scholar PubMed
[195] Yokoshima S, Morinaga M, Tsujimura S, Shimoyama K, Morihara T. Representative exposure-annoyance relationships due to transportation noises in Japan. Int J Env Res Public Health. 2021;18(20):10935.10.3390/ijerph182010935Search in Google Scholar PubMed PubMed Central
[196] Yonemura M, Lee H, Sakamoto S. Subjective evaluation on the annoyance of environmental noise containing low-frequency tonal components. Int J Env Res Public Health. 2021;18(13):7127.10.3390/ijerph18137127Search in Google Scholar PubMed PubMed Central
[197] Amoatey P, Omidvarbona H, Baawain MS, Al-Mayahi A, Al-Mamun A, Al-Harthy I. Exposure assessment to road traffic noise levels and health effects in an arid urban area. Env Sci Pollut Res Int. 2020;27(28):35051–64.10.1007/s11356-020-09785-ySearch in Google Scholar PubMed
[198] Wang J, Norbäck D. Home environment and noise disturbance in a national sample of multi-family buildings in Sweden-associations with medical symptoms. BMC Public Health. 2021;21(1):1989.10.1186/s12889-021-12069-wSearch in Google Scholar PubMed PubMed Central
[199] Eze IC, Foraster M, Schaffner E, Vienneau D, Pieren R, Imboden M, et al. Incidence of depression in relation to transportation noise exposure and noise annoyance in the SAPALDIA study. Environ Int. 2020;144:106014.10.1016/j.envint.2020.106014Search in Google Scholar PubMed
[200] Deng XF, Shi GQ, Guo LL, Zhu CA, Chen YJ. Analysis on risk factors of depressive symptoms in occupational noise-induced hearing loss patients: a cross-sectional study. Noise Health. 2019;21(98):17–24.10.4103/nah.NAH_16_18Search in Google Scholar PubMed PubMed Central
[201] Dzhambov A, Tilov B, Markevych I, Dimitrova D. Residential road traffic noise and general mental health in youth: The role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Env Int. 2017;109:1–9.10.1016/j.envint.2017.09.009Search in Google Scholar PubMed
[202] Jensen HAR, Rasmussen B, Ekholm O. Neighbour and traffic noise annoyance: a nationwide study of associated mental health and perceived stress. Eur J Public Health. 2018;28(6):1050–5.10.1093/eurpub/cky091Search in Google Scholar PubMed
[203] Amoatey P, Al-Harthy I, Al-Mushaifari MA, Al-Jabri K, Al-Mamun A. Effect of ambient noise on indoor environments in a health care facility in Oman. Env Sci Pollut Res Int. 2022;29(10):15081–97.10.1007/s11356-021-16875-ySearch in Google Scholar PubMed
[204] Monazzam MR, Shamsipour M, Zaredar N, Bayat R. Evaluation of the relationship between psychological distress and sleep problems with annoyance caused by exposure to environmental noise in the adult population of Tehran Metropolitan City, Iran. J Env Health Sci Eng. 2022;20(1):1–10.10.1007/s40201-021-00703-zSearch in Google Scholar PubMed PubMed Central
[205] Nazneen S, Raza A, Khan S. Assessment of noise pollution and associated subjective health complaints and psychological symptoms: analysis through structure equation model. Env Sci Pollut Res Int. 2020;27(17):21570–80.10.1007/s11356-020-08655-xSearch in Google Scholar PubMed
[206] Weyde KV, Krog NH, Oftedal B, Magnus P, Øverland S, Stansfeld S, et al. Road traffic noise and children’s inattention. Environ Health. 2017;16(1):1–14.10.1186/s12940-017-0337-ySearch in Google Scholar PubMed PubMed Central
[207] Monteiro R, Tomé D, Neves P, Silva D, Rodrigues MA. The interactive effect of occupational noise on attention and short-term memory: A pilot study. Noise Health. 2018;20(96):190–8.Search in Google Scholar
[208] Eriksson HP, Söderberg M, Neitzel RL, Torén K, Andersson E. Cardiovascular mortality in a Swedish cohort of female industrial workers exposed to noise and shift work. Int Arch Occup Env Health. 2021;94(2):285–93.10.1007/s00420-020-01574-xSearch in Google Scholar PubMed PubMed Central
[209] Yu Y, Haan M, Paul KC, Mayeda ER, Jerrett M, Wu J, et al. Metabolic dysfunction modifies the influence of traffic-related air pollution and noise exposure on late-life dementia and cognitive impairment: A cohort study of older Mexican-Americans. Env Epidemiol. 2020;4(6):e122.10.1097/EE9.0000000000000122Search in Google Scholar PubMed PubMed Central
[210] Mac Domhnaill C, Douglas O, Lyons S, Murphy E, Nolan A. Road traffic noise and cognitive function in older adults: a cross-sectional investigation of The Irish Longitudinal Study on Ageing. BMC Public Health. 2021;21(1):1814.10.1186/s12889-021-11853-ySearch in Google Scholar PubMed PubMed Central
[211] Khavanin A, Khajehnasiri F, Shahhoseini S. The effects of occupational noise pollution and shift work on oxidative stress markers in cement workers, Iran. Pollution. 2022;8(1):105–15.Search in Google Scholar
[212] Mirmohammadi S, Khanjani N, Nazarkhani F, Abediankenari S, Yazdani J, Tilaki RAD. The effect of noise and dust exposure on oxidative stress among livestock and poultry feed industry workers. Toxicol Ind Health. 2020;36(11):908–15.10.1177/0748233720962253Search in Google Scholar PubMed
[213] Dzhambov AM, Tokmakova MP, Gatseva PD, Zdravkov NG, Gencheva DG, Ivanova NG, et al. Community noise exposure and its effect on blood pressure and renal function in patients with hypertension and cardiovascular disease. Folia Med (Plovdiv). 2017;59(3):344–56.10.1515/folmed-2017-0045Search in Google Scholar PubMed
[214] Kupcikova Z, Fecht D, Ramakrishnan R, Clark C, Cai YS. Road traffic noise and cardiovascular disease risk factors in UK Biobank. Eur Heart J. 2021;42(21):2072–84.10.1093/eurheartj/ehab121Search in Google Scholar PubMed PubMed Central
[215] Bruno R, Faraguna U, Di Pilla M, Di Galante M, Banfi T, Gemignani A, et al. Increased central pressure augmentation is associated with reduced sleep duration in individuals exposed to aircraft noise pollution: The sera-cv study. J Hypertension. 2017;35:E247.10.1097/01.hjh.0000523715.41136.e4Search in Google Scholar
[216] Kim MG, Ahn YS. The relationship between occupational noise exposure and hypertension using nearest age-matching method in South Korea male workers. Cogent Eng. 2021;8(1):1909798.10.1080/23311916.2021.1909798Search in Google Scholar
[217] Lefevre M, Chaumond A, Champelovier P, Allemand LG, Lambert J, Laumon B, et al. Understanding the relationship between air traffic noise exposure and annoyance in populations living near airports in France. Environ Int. 2020;144.Search in Google Scholar
[218] Li WZ, Yi GL, Chen ZL, Wu J, Lu ZX, Liang JJ, et al. Association of occupational noise exposure, bilateral hearing loss with hypertension among Chinese workers. J Hypertens. 2021;39(4):643–50.10.1097/HJH.0000000000002696Search in Google Scholar PubMed
[219] Wu XM, Li CX, Zhang XH, Song YM, Zhao D, Lan YY, et al. The impact of occupational noise on hypertension risk: a case-control study in automobile factory personnel. Front Cardiovasc Med. 2022;9:803695.10.3389/fcvm.2022.803695Search in Google Scholar PubMed PubMed Central
[220] Chen S, Ni Y, Zhang L, Kong L, Lu L, Yang Z, et al. Noise exposure in occupational setting associated with elevated blood pressure in China. BMC Public Health. 2017;17(1):107.10.1186/s12889-017-4050-0Search in Google Scholar PubMed PubMed Central
[221] Evrard AS, Lefèvre M, Champelovier P, Lambert J, Laumon B. Does aircraft noise exposure increase the risk of hypertension in the population living near airports in France? Occup Env Med. 2017;74(2):123–9.10.1136/oemed-2016-103648Search in Google Scholar PubMed
[222] Fuks KB, Weinmayr G, Basagaña X, Gruzieva O, Hampel R, Oftedal B, et al. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur Heart J. 2017;38(13):983–90.10.1093/eurheartj/ehw413Search in Google Scholar PubMed
[223] Halonen JI, Dehbi HM, Hansell AL, Gulliver J, Fecht D, Blangiardo M, et al. Associations of night-time road traffic noise with carotid intima-media thickness and blood pressure: The Whitehall II and SABRE study cohorts. Env Int. 2017;98:54–61.10.1016/j.envint.2016.09.023Search in Google Scholar PubMed
[224] Nserat S, Al-Musa A, Khader YS, Abu Slaih A, Iblan I. Blood pressure of Jordanian workers chronically exposed to noise in industrial plants. Int J Occup Env Med. 2017;8(4):217–23.10.15171/ijoem.2017.1134Search in Google Scholar PubMed PubMed Central
[225] Pitchika A, Hampel R, Wolf K, Kraus U, Cyrys J, Babisch W, et al. Long-term associations of modeled and self-reported measures of exposure to air pollution and noise at residence on prevalent hypertension and blood pressure. Sci Total Env. 2017;593–594:337–46.10.1016/j.scitotenv.2017.03.156Search in Google Scholar PubMed
[226] Tong J, Wang Y, Yuan J, Yang J, Wang Z, Zheng Y, et al. Effect of interaction between noise and A1166C site of AT1R gene polymorphism on essential hypertension in an iron and steel enterprise workers. J Occup Env Med. 2017;59(4):412–6.10.1097/JOM.0000000000000970Search in Google Scholar PubMed PubMed Central
[227] Zeeb H, Hegewald J, Schubert M, Wagner M, Dröge P, Swart E, et al. Traffic noise and hypertension - results from a large case-control study. Env Res. 2017;157:110–7.10.1016/j.envres.2017.05.019Search in Google Scholar PubMed
[228] Cayir A, Barrow TM, Wang H, Liu H, Li C, Ding N, et al. Occupational noise exposure is associated with hypertension in China: Results from project ELEFANT. PLoS One. 2018;13(12):e0209041.10.1371/journal.pone.0209041Search in Google Scholar PubMed PubMed Central
[229] Pyko A, Lind T, Mitkovskaya N, Ögren M, Östenson CG, Wallas A, et al. Transportation noise and incidence of hypertension. Int J Hyg Env Health. 2018;221(8):1133–41.10.1016/j.ijheh.2018.06.005Search in Google Scholar PubMed
[230] Wang D, Zhou M, Li W, Kong W, Wang Z, Guo Y, et al. Occupational noise exposure and hypertension: the Dongfeng-Tongji Cohort Study. J Am Soc Hypertens. 2018;12(2):71–9.e5.10.1016/j.jash.2017.11.001Search in Google Scholar PubMed
[231] Brahem A, Riahi S, Chouchane A, Kacem I, Maalel OE, Maoua M, et al. Impact of occupational noise in the development of arterial hypertension: A survey carried out in a company of electricity production. Ann Cardiol Angeiol (Paris). 2019;68(3):168–74.10.1016/j.ancard.2018.10.008Search in Google Scholar PubMed
[232] Zhou F, Shrestha A, Mai S, Tao Z, Li J, Wang Z, et al. Relationship between occupational noise exposure and hypertension: A cross-sectional study in steel factories. Am J Ind Med. 2019;62(11):961–8.10.1002/ajim.23034Search in Google Scholar PubMed
[233] Kuang D, Yu YY, Tu C. Bilateral high-frequency hearing loss is associated with elevated blood pressure and increased hypertension risk in occupational noise exposed workers. PLoS One. 2019;14(9):e0222135.10.1371/journal.pone.0222135Search in Google Scholar PubMed PubMed Central
[234] Lee PJ, Park SH, Jeong JH, Choung T, Kim KY. Association between transportation noise and blood pressure in adults living in multi-storey residential buildings. Env Int. 2019;132:105101.10.1016/j.envint.2019.105101Search in Google Scholar PubMed
[235] Oh M, Shin K, Kim K, Shin J. Influence of noise exposure on cardiocerebrovascular disease in Korea. Sci Total Env. 2019;651(Pt 2):1867–76.10.1016/j.scitotenv.2018.10.081Search in Google Scholar PubMed
[236] Dimakopoulou K, Koutentakis K, Papageorgiou I, Kasdagli MI, Haralabidis AS, Sourtzi P, et al. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup Env Med. 2017;74(11):830–7.10.1136/oemed-2016-104180Search in Google Scholar PubMed
[237] Yang WT, Wang VS, Chang LT, Chuang KJ, Chuang HC, Liu CS, et al. Road traffic noise, air pollutants, and the prevalence of cardiovascular disease in Taichung, Taiwan. Int J Env Res Public Health. 2018;15(8):1707.10.3390/ijerph15081707Search in Google Scholar PubMed PubMed Central
[238] Khosravipour M, Abdollahzad H, Khosravi F, Rezaei M, Mohammadi Sarableh H, Moradi Z. The association of occupational noises and the prevalence of metabolic syndrome. Ann Work Expo Health. 2020;64(5):514–21.10.1093/annweh/wxaa030Search in Google Scholar PubMed
[239] Khosravipour M, Khosravi F, Ashtarian H, Rezaei M, Moradi Z, Mohammadi Sarableh H. The effects of exposure to different noise frequency patterns on blood pressure components and hypertension. Int Arch Occup Env Health. 2020;93(8):975–82.10.1007/s00420-020-01545-2Search in Google Scholar PubMed
[240] Koczorowski M, Bernard N, Mauny F, Chagué F, Pujol S, Maza M, et al. Environmental noise exposure is associated with atherothrombotic risk. Sci Rep. 2022;12(1):3151.10.1038/s41598-022-06825-0Search in Google Scholar PubMed PubMed Central
[241] Kuo CY, Hung CL, Chen HC, Shih CP, Lu RH, Chen CW, et al. The immediate and long-term impact of military aircraft noise on hearing: a cross-sectional comparison of fighter pilots and ground staff. Int J Env Res Public Health. 2021;18(6):2982.10.3390/ijerph18062982Search in Google Scholar PubMed PubMed Central
[242] Lechat B, Scott H, Decup F, Hansen KL, Micic G, Dunbar C, et al. Environmental noise-induced cardiovascular responses during sleep. Sleep. 2022;45(3):zsab302.10.1093/sleep/zsab302Search in Google Scholar PubMed
[243] Lechner C, Kirisits C, Bose-O’Reill S. Combined annoyance response from railroad and road traffic noise in an alpine valley. Noise Health. 2020;22(104):10–8.Search in Google Scholar
[244] Lechner C, Schnaiter D, Siebert U, Böse-O’Reilly S. Effects of Motorcycle Noise on Annoyance-A Cross-Sectional Study in the Alps. Int J Env Res Public Health. 2020;17(5):1580.10.3390/ijerph17051580Search in Google Scholar PubMed PubMed Central
[245] Lee J, Park J, Lee J, Ahn JH, Sim CS, Kweon K, et al. Effect of noise on sleep and autonomic activity in children according to source. J Korean Med Sci. 2021;36(37):e234.10.3346/jkms.2021.36.e234Search in Google Scholar PubMed PubMed Central
[246] Warembourg C, Nieuwenhuijsen M, Ballester F, de Castro M, Chatzi L, Esplugues A, et al. Urban environment during early-life and blood pressure in young children. Env Int. 2021;146:106174.10.1016/j.envint.2020.106174Search in Google Scholar PubMed
[247] Wojciechowska W, Januszewicz A, Drożdż T, Rojek M, Bączalska J, Terlecki M, et al. Blood pressure and arterial stiffness in association with aircraft noise exposure:long-term observation and potential effect of COVID-19 lockdown. Hypertension. 2022;79(2):325–34.10.1161/HYPERTENSIONAHA.121.17704Search in Google Scholar PubMed PubMed Central
[248] Yaghoubi K, Alimohammadi I, Abolghasemi J, Shirin Shandiz M, Aboutaleb N, Ashtarinezhad A. The effect of occupational noise exposure on systolic blood pressure, diastolic blood pressure and salivary cortisol level among automotive assembly workers. Int J Occup Saf Erg. 2021;27(1):8–13.10.1080/10803548.2018.1510608Search in Google Scholar PubMed
[249] Yun B, Sim J, Jeong I, Lee S, Kim S, Cho A, et al. Does severe subacute noise exposure increase risk of new onset hypertension beyond conventional risk factors? A 30 000 person-years cohort study. J Hypertens. 2022;40(3):588–95.10.1097/HJH.0000000000003052Search in Google Scholar PubMed PubMed Central
[250] Okokon EO, Yli-Tuomi T, Siponen T, Tiittanen P, Turunen AW, Kangas L, et al. Heterogeneous urban exposures and prevalent hypertension in the Helsinki Capital region, Finland. Int J Env Res Public Health. 2021;18(3):1196.10.3390/ijerph18031196Search in Google Scholar PubMed PubMed Central
[251] Eriksson HP, Andersson E, Schioler L, Soderberg M, Sjostrom M, Rosengren A, et al. Longitudinal study of occupational noise exposure and joint effects with job strain and risk for coronary heart disease and stroke in Swedish men. BMJ Open. 2018;8(4):019160.10.1136/bmjopen-2017-019160Search in Google Scholar PubMed PubMed Central
[252] Roca-Barcelo A, Nardocci A, de Aguiar BS, Ribeiro AG, Failla MA, Hansell AL, et al. Risk of cardiovascular mortality, stroke and coronary heart mortality associated with aircraft noise around Congonhas airport, Sao Paulo, Brazil: a small-area study. Environ Health. 2021;20(1):59.10.1186/s12940-021-00746-7Search in Google Scholar PubMed PubMed Central
[253] Lim YH, Jørgensen JT, So R, Cole-Hunter T, Mehta AJ, Amini H, et al. Long-Term exposure to air pollution, road traffic noise, and heart failure incidence: The Danish Nurse Cohort. J Am Heart Assoc. 2021;10(20):e021436.10.1161/JAHA.121.021436Search in Google Scholar PubMed PubMed Central
[254] Osborne MT, Abohashem S, Naddaf N, Abbasi T, Zureigat H, Mezue K, et al. The combined effect of air and transportation noise pollution on atherosclerotic inflammation and risk of cardiovascular disease events. J Nucl Cardiol. 2022;30(2):665–79.10.1007/s12350-022-03003-7Search in Google Scholar PubMed PubMed Central
[255] Wang DM, Xiao Y, Feng XB, Wang B, Li WZ, He MA, et al. Association of occupational noise exposure, bilateral hearing loss with atherosclerotic cardiovascular disease risk in Chinese adults. Int J Hyg Environ Health. 2021;235:113776.10.1016/j.ijheh.2021.113776Search in Google Scholar PubMed
[256] Foraster M, Eze IC, Schaffner E, Vienneau D, Héritier H, Endes S, et al. Exposure to road, railway, and aircraft noise and arterial stiffness in the SAPALDIA study: annual average noise levels and temporal noise characteristics. Env Health Perspect. 2017;125(9):097004.10.1289/EHP1136Search in Google Scholar PubMed PubMed Central
[257] Hoffmann B, Hennig F, Geisel H, Lucht S, Moebus S, Erbel R, et al. Air pollution, traffic noise and development of subclinical atherosclerosis in the Thoracic Aorta. Circulation. 2019;139.10.1161/circ.139.suppl_1.P102Search in Google Scholar
[258] Wang L, Yu M, Zhang S, Li X, Yuan J. Associations of occupational heat stress and noise exposure with carotid atherosclerosis among chinese steelworkers: a cross-sectional survey. Int J Env Res Public Health. 2021;19(1):24.10.3390/ijerph19010024Search in Google Scholar PubMed PubMed Central
[259] Osborne MT, Radfar A, Hassan MZO, Abohashem S, Oberfeld B, Patrich T, et al. A neurobiological mechanism linking transportation noise to cardiovascular disease in humans. Eur Heart J. 2020;41(6):772–82.10.1093/eurheartj/ehz820Search in Google Scholar PubMed PubMed Central
[260] Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol. 2017;32(4):307–15.10.1007/s10654-017-0234-2Search in Google Scholar PubMed
[261] Cai Y, Hansell AL, Blangiardo M, Burton PR, de Hoogh K, Doiron D, et al. Long-term exposure to road traffic noise, ambient air pollution, and cardiovascular risk factors in the HUNT and lifelines cohorts. Eur Heart J. 2017;38(29):2290–6.10.1093/eurheartj/ehx263Search in Google Scholar PubMed PubMed Central
[262] Recio A, Linares C, Banegas JR, Díaz J. Impact of road traffic noise on cause-specific mortality in Madrid (Spain). Sci Total Env. 2017;590–591:171–3.10.1016/j.scitotenv.2017.02.193Search in Google Scholar PubMed
[263] Cai Y, Hodgson S, Blangiardo M, Gulliver J, Morley D, Fecht D, et al. Road traffic noise, air pollution and incident cardiovascular disease: A joint analysis of the HUNT, EPIC-Oxford and UK Biobank cohorts. Env Int. 2018;114:191–201.10.1016/j.envint.2018.02.048Search in Google Scholar PubMed
[264] Poulsen AH, Raaschou-Nielsen O, Peña A, Hahmann AN, Nordsborg RB, Ketzel M, et al. Short-term nighttime wind turbine noise and cardiovascular events: A nationwide case-crossover study from Denmark. Env Int. 2018;114:160–6.10.1016/j.envint.2018.02.030Search in Google Scholar PubMed
[265] Sørensen M, Wendelboe Nielsen O, Sajadieh A, Ketzel M, Tjønneland A, Overvad K, et al. Long-term exposure to road traffic noise and nitrogen dioxide and risk of heart failure: a cohort study. Environ Health Perspect. 2017;125(9):097021.10.1289/EHP1272Search in Google Scholar PubMed PubMed Central
[266] Schmidt FP, Herzog J, Schnorbus B, Ostad MA, Lasetzki L, Hahad O, et al. The impact of aircraft noise on vascular and cardiac function in relation to noise event number: a randomized trial. Cardiovasc Res. 2021;117(5):1382–90.10.1093/cvr/cvaa204Search in Google Scholar PubMed PubMed Central
[267] Hahad O, Beutel M, Gori T, Schulz A, Blettner M, Pfeiffer N, et al. Annoyance to different noise sources is associated with atrial fibrillation in the Gutenberg Health Study. Int J Cardiol. 2018;264:79–84.10.1016/j.ijcard.2018.03.126Search in Google Scholar PubMed
[268] Lim YH, Jorgensen JT, So RN, Cramer J, Amini H, Mehta A, et al. Long-term exposure to road traffic noise and incident myocardial infarction: A Danish Nurse Cohort study. Environ Epidemiol. 2021;5(3):148.10.1097/EE9.0000000000000148Search in Google Scholar PubMed PubMed Central
[269] Moreyra AE, Subramanian K, Mi ZY, Cosgrove NM, Kostis WJ, Ke F, et al. The impact of exposure to transportation noise on the rates of myocardial infarction in New Jersey. J Am Coll Cardiology. 2022;79(9):1148.10.1016/S0735-1097(22)02139-8Search in Google Scholar
[270] Roswall N, Raaschou-Nielsen O, Ketzel M, Gammelmark A, Overvad K, Olsen A, et al. Long-term residential road traffic noise and NO2 exposure in relation to risk of incident myocardial infarction - A Danish cohort study. Environ Res. 2017;156:80–6.10.1016/j.envres.2017.03.019Search in Google Scholar PubMed
[271] Bräuner EV, Jørgensen JT, Duun-Henriksen AK, Backalarz C, Laursen JE, Pedersen TH, et al. Long-term wind turbine noise exposure and incidence of myocardial infarction in the Danish nurse cohort. Env Int. 2018;121(Pt 1):794–802.10.1016/j.envint.2018.10.011Search in Google Scholar PubMed
[272] Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, de Hoogh K, et al. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J. 2019;40(7):598–603.10.1093/eurheartj/ehy650Search in Google Scholar PubMed
[273] Fang Q, Lai X, Yang L, Wang Z, Zhan Y, Zhou L, et al. Hearing loss is associated with increased stroke risk in the Dongfeng-Tongji Cohort. Atherosclerosis. 2019;285:10–6.10.1016/j.atherosclerosis.2019.03.012Search in Google Scholar PubMed
[274] Vivanco-Hidalgo RM, Avellaneda-Gómez C, Dadvand P, Cirach M, Ois Á, Gómez González A, et al. Association of residential air pollution, noise, and greenspace with initial ischemic stroke severity. Environ Res. 2019;179(Pt A):108725.10.1016/j.envres.2019.108725Search in Google Scholar PubMed
[275] Yankoty LI, Gamache P, Plante C, Goudreau S, Blais C, Perron S, et al. Manuscript title: Long-term residential exposure to environmental/transportation noise and the incidence of myocardial infarction. Int J Hyg Environ Health. 2021;232:113666.10.1016/j.ijheh.2020.113666Search in Google Scholar PubMed
[276] Magnoni P, Murtas R, Russo AG. Residential exposure to traffic-borne pollution as a risk factor for acute cardiocerebrovascular events: a population-based retrospective cohort study in a highly urbanized area. Int J Epidemiol. 2021;50(4):1160–71.10.1093/ije/dyab068Search in Google Scholar PubMed PubMed Central
[277] Roswall N, Pyko A, Ogren M, Oudin A, Rosengren A, Lager A, et al. Long-term exposure to transportation noise and risk of incident stroke: a pooled study of nine Scandinavian cohorts. Environ Health Perspect. 2021;129(10):107002.10.1289/EHP8949Search in Google Scholar PubMed PubMed Central
[278] Yankoty LI, Gamache P, Plante C, Goudreau S, Blais C, Perron S, et al. Relationships between long-term residential exposure to total environmental noise and stroke incidence. Noise Health. 2022;24(113):33–9.10.4103/nah.nah_34_21Search in Google Scholar PubMed PubMed Central
[279] Saucy A, Schäffer B, Tangermann L, Vienneau D, Wunderli JM, Röösli M. Does night-time aircraft noise trigger mortality? A case-crossover study on 24 886 cardiovascular deaths. Eur Heart J. 2021;42(8):835–43.10.1093/eurheartj/ehaa957Search in Google Scholar PubMed PubMed Central
[280] Vienneau D, Saucy A, Schäffer B, Flückiger B, Tangermann L, Stafoggia M, et al. Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Env Int. 2022;158:106974.10.1016/j.envint.2021.106974Search in Google Scholar PubMed
[281] Pyko A, Andersson N, Eriksson C, de Faire U, Lind T, Mitkovskaya N, et al. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup Env Med. 2019;76(4):201–7.10.1136/oemed-2018-105333Search in Google Scholar PubMed
[282] Okazaki Y, Ito L, Tokai A. Characterizing potential risk triggered by road traffic noise in comparison with typical air pollutants NO(2) and PM(2.5). Env Syst Decis. 2021;41(1):147–62.10.1007/s10669-021-09800-8Search in Google Scholar PubMed PubMed Central
[283] Andersen ZJ, Cramer J, Jørgensen JT, Dehlendorff C, Amini H, Mehta A, et al. Long-term exposure to road traffic noise and air pollution, and incident atrial fibrillation in the Danish Nurse Cohort. Env Health Perspect. 2021;129(8):87002.10.1289/EHP8090Search in Google Scholar PubMed PubMed Central
[284] Michaud DS, Marro L, McNamee JP. Self-reported occupational noise exposure and cardiovascular disease in Canada: Results from the Canadian Health Measures Survey. J Acoust Soc Am. 2021;150(2):990.10.1121/10.0005588Search in Google Scholar PubMed
[285] Tzivian L, Soppa V, Winkler A, Hennig F, Weimar C, Moebus S, et al. The role of depressive symptoms within the association of long-term exposure to indoor and outdoor traffic noise and cognitive function - Results from the Heinz Nixdorf Recall study. Int J Hyg Env Health. 2020;230:113570.10.1016/j.ijheh.2020.113570Search in Google Scholar PubMed
[286] Kim A, Sung JH, Bang JH, Cho SW, Lee J, Sim CS. Effects of self-reported sensitivity and road-traffic noise levels on the immune system. PLoS One. 2017;12(10):e0187084.10.1371/journal.pone.0187084Search in Google Scholar PubMed PubMed Central
[287] Lee S, Lee W, Roh J, Won JU, Yoon JH. Symptoms of nervous system related disorders among workers exposed to occupational noise and vibration in Korea. J Occup Env Med. 2017;59(2):191–7.10.1097/JOM.0000000000000935Search in Google Scholar PubMed
[288] Seidler AL, Hegewald J, Schubert M, Weihofen VM, Wagner M, Droge P, et al. The Effect of aircraft road, and railway traffic noise on stroke - results of a case-control study based on secondary data. Noise Health. 2018;20(95):152–61.10.1016/j.envres.2016.10.017Search in Google Scholar PubMed
[289] Thacher JD, Roswall N, Lissaker C, Aasvang GM, Albin M, Andersson EM, et al. Occupational noise exposure and risk of incident stroke: a pooled study of five Scandinavian cohorts. Occup Environ Med. 2022;79(9):594–601.10.1136/oemed-2021-108053Search in Google Scholar PubMed PubMed Central
[290] Christensen JS, Raaschou-Nielsen O, Ketzel M, Ramlau-Hansen CH, Bech BH, Olsen J, et al. Exposure to residential road traffic noise prior to conception and time to pregnancy. Env Int. 2017;106:48–52.10.1016/j.envint.2017.05.011Search in Google Scholar PubMed
[291] Pedersen M, Halldorsson TI, Olsen SF, Hjortebjerg D, Ketzel M, Grandström C, et al. Impact of road traffic pollution on pre-eclampsia and pregnancy-induced hypertensive disorders. Epidemiology. 2017;28(1):99–106.10.1097/EDE.0000000000000555Search in Google Scholar PubMed PubMed Central
[292] Auger N, Duplaix M, Bilodeau-Bertrand M, Lo E, Smargiassi A. Environmental noise pollution and risk of preeclampsia. Env Pollut. 2018;239:599–606.10.1016/j.envpol.2018.04.060Search in Google Scholar PubMed
[293] Bosch A, Kannenkeril D, Ott C, Harazny JM, Striepe K, Karg MV, et al. The influence of annoyance due to aircraft noise on renal hemodynamic. J Hypertension. 2019;37:E200.10.1097/01.hjh.0000572584.67646.aaSearch in Google Scholar
[294] Shanmugarajah SK, Dilara Wijesinghe MS. Noise level inside Sri Lanka transport board buses and hearing impairment of long- and short-distance bus drivers of Ampara and Batticaloa Districts, Sri Lanka. Indian J Community Med. 2022;47(2):280–4.10.4103/ijcm.ijcm_768_21Search in Google Scholar PubMed PubMed Central
[295] Liebich T, Lack L, Hansen K, Zajamsek B, Micic G, Lechat B, et al. An experimental investigation on the impact of wind turbine noise on polysomnography-measured and sleep diary-determined sleep outcomes. Sleep. 2022;45(8):zsac085.10.1093/sleep/zsac085Search in Google Scholar PubMed
[296] Roswall N, Raaschou-Nielsen O, Ketzel M, Overvad K, Halkjær J, Sørensen M. Modeled traffic noise at the residence and colorectal cancer incidence: a cohort study. Cancer Causes Control. 2017;28(7):745–53.10.1007/s10552-017-0904-0Search in Google Scholar PubMed
[297] Clark C, Sbihi H, Tamburic L, Brauer M, Frank LD, Davies HW. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: a prospective cohort study. Env Health Perspect. 2017;125(8):087025.10.1289/EHP1279Search in Google Scholar PubMed PubMed Central
[298] Thiesse L, Rudzik F, Pieren R, Wunderli JM, Spiegel K, Leproult R, et al. Temporal variation of transportation noise during sleep impacts on glucose metabolism. Sleep. 2017;40:A36.10.1093/sleepj/zsx050.095Search in Google Scholar
[299] Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol. 2017;46(4):1115–25.10.1093/ije/dyx020Search in Google Scholar PubMed PubMed Central
[300] Klompmaker JO, Janssen NAH, Bloemsma LD, Gehring U, Wijga AH, van den Brink C, et al. Associations of combined exposures to surrounding green, air pollution, and road traffic noise with cardiometabolic diseases. Env Health Perspect. 2019;127(8):87003.10.1289/EHP3857Search in Google Scholar PubMed PubMed Central
[301] Michaud DS, Marro L, Denning A, Shackleton S, Toutant N, McNamee JP. A comparison of self-reported health status and perceptual responses toward environmental noise in rural, suburban, and urban regions in Canada. J Acoust Soc Am. 2022;151(3):1532.10.1121/10.0009749Search in Google Scholar PubMed
[302] Shin S, Bai L, Oiamo TH, Burnett RT, Weichenthal S, Jerrett M, et al. Association between road traffic noise and incidence of diabetes mellitus and hypertension in Toronto, Canada: A population-based cohort study. J Am Heart Assoc. 2020;9(6):e013021.10.1161/JAHA.119.013021Search in Google Scholar PubMed PubMed Central
[303] Dzhambov AM, Gatseva PD, Tokmakova MP, Zdravkov NG, Vladeva SV, Gencheva DG, et al. Association between community noise and adiposity in patients with cardiovascular disease. Noise Health. 2017;19(91):270–7.10.4103/nah.NAH_78_16Search in Google Scholar PubMed PubMed Central
[304] Foraster M, Eze IC, Vienneau D, Schaffner E, Jeong A, Héritier H, et al. Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Env Int. 2018;121(Pt 1):879–89.10.1016/j.envint.2018.09.057Search in Google Scholar PubMed
[305] Miao L, Zhang J, Yin L, Pu Y. Hearing loss and hypertension among noise-exposed workers: a pilot study based on baseline data. Int J Env Health Res. 2022;33(8):783–95.10.1080/09603123.2022.2050681Search in Google Scholar PubMed
[306] Quehl J, Bartels S, Fimmers R, Aeschbach D. Effects of nocturnal aircraft noise and non-acoustical factors on short-term annoyance in primary school children. Int J Env Res Public Health. 2021;18(13):6959.10.3390/ijerph18136959Search in Google Scholar PubMed PubMed Central
[307] Weyde KV, Krog NH, Oftedal B, Magnus P, White R, Stansfeld S, et al. A longitudinal study of road traffic noise and body mass index trajectories from birth to 8 years. Epidemiology. 2018;29(5):729–38.10.1097/EDE.0000000000000868Search in Google Scholar PubMed PubMed Central
[308] Cramer J, Therming Jørgensen J, Sørensen M, Backalarz C, Laursen JE, Ketzel M, et al. Road traffic noise and markers of adiposity in the Danish Nurse Cohort: A cross-sectional study. Env Res. 2019;172:502–10.10.1016/j.envres.2019.03.001Search in Google Scholar PubMed
[309] Liang X, Tang X, Liu M, Liang X, Chen L, Chen X, et al. Associations of self-reported residential noise exposure with obesity and hypertension in children and adolescents. Front Pediatr. 2022;10:902868.10.3389/fped.2022.902868Search in Google Scholar PubMed PubMed Central
[310] Massonnié J, Frasseto P, Ng-Knight T, Gilligan-Lee K, Kirkham N, Mareschal D. Children’s effortful control skills, but not their prosocial skills, relate to their reactions to classroom noise. Int J Env Res Public Health. 2022;19(14):8815.10.3390/ijerph19148815Search in Google Scholar PubMed PubMed Central
[311] Welch D, Dirks KN, Shepherd D, McBride D. Health-related quality of life is impacted by proximity to an airport in noise-sensitive people. Noise Health. 2018;20(96):171–7.Search in Google Scholar
[312] Tobollik M, Hintzsche M, Wothge J, Myck T, Plass D. Burden of disease due to traffic noise in Germany. Int J Environ Res Public Health. 2019;16(13):2304.10.3390/ijerph16132304Search in Google Scholar PubMed PubMed Central
[313] Cai Y, Ramakrishnan R, Rahimi K. Long-term exposure to traffic noise and mortality: A systematic review and meta-analysis of epidemiological evidence between 2000 and 2020. Environ Pollut. 2021;269:116222.10.1016/j.envpol.2020.116222Search in Google Scholar PubMed
[314] Shamsipour M, Zaredar N, Monazzam MR, Namvar Z, Mohammadpour S. Burden of diseases attributed to traffic noise in the metropolis of Tehran in 2017. Env Pollut. 2022;301:119042.10.1016/j.envpol.2022.119042Search in Google Scholar PubMed
[315] Miloradović D, Glišović J, Lukić J. Regulations on road vehicle noise – trends and future activities. Mobil Veh Mech. 2017;43:57–72.10.24874/mvm.2017.43.01.05Search in Google Scholar
[316] Bouzir TAK, Berkouk D, Barrigón Morillas JM, Rey-Gozalo G, Montes González D. Noise pollution studies in the arab world: a scientometric analysis and research Agenda. Sustainability. 2024;16(11):4350.10.3390/su16114350Search in Google Scholar
[317] Mucci N, Traversini V, Lorini C, De Sio S, Galea RP, Bonaccorsi G, et al. Urban noise and psychological distress: A systematic review. Int J Environ Res Public Health. 2020;17(18):6621.10.3390/ijerph17186621Search in Google Scholar PubMed PubMed Central
[318] Shi Z, Zhou J, Huang Y, Hu Y, Zhou L, Shao Y, et al. Occupational hearing loss associated with non-Gaussian noise: A systematic review and meta-analysis. Ear Hearing. 2021;42(6):1472.10.1097/AUD.0000000000001060Search in Google Scholar PubMed PubMed Central
[319] Chen F, Fu W, Shi O, Li D, Jiang Q, Wang T, et al. Impact of exposure to noise on the risk of hypertension: A systematic review and meta-analysis of cohort studies. Environ Res. 2021;195:110813.10.1016/j.envres.2021.110813Search in Google Scholar PubMed
[320] Hahad O, Jimenez MTB, Kuntic M, Frenis K, Steven S, Daiber A, et al. Cerebral consequences of environmental noise exposure. Environ Int. 2022;165:107306.10.1016/j.envint.2022.107306Search in Google Scholar PubMed
[321] Zhou J, Shi Z, Zhou L, Hu Y, Zhang M. Occupational noise-induced hearing loss in China: A systematic review and meta-analysis. BMJ Open. 2020;10(9):e039576.10.1136/bmjopen-2020-039576Search in Google Scholar PubMed PubMed Central
[322] Weihofen VM, Hegewald J, Euler U, Schlattmann P, Zeeb H, Seidler A. Aircraft noise and the risk of stroke: a systematic review and meta-analysis. Dtsch Ärzteblatt Int. 2019;116(14):237.10.3238/arztebl.2019.0237Search in Google Scholar PubMed PubMed Central
[323] Jerem P, Mathews F. Trends and knowledge gaps in field research investigating effects of anthropogenic noise. Conserv Biol. 2021;35(1):115–29.10.1111/cobi.13510Search in Google Scholar PubMed
[324] Slabbekoorn H, Dooling RJ, Popper AN, Fay RR. Effects of anthropogenic noise on animals. New York: Springer; 2018.10.1007/978-1-4939-8574-6Search in Google Scholar
[325] Dzhambov AM, Lercher P. Road traffic noise exposure and depression/anxiety: an updated systematic review and meta-analysis. Int J Environ Res Public Health. 2019;16(21):4134.10.3390/ijerph16214134Search in Google Scholar PubMed PubMed Central
[326] Luca M, Guzik T, Luca A. Oxidative stress as a link between cerebrocardiovascular and psychiatric disorders. Egypt: Hindawi; 2020.10.1155/2020/5685317Search in Google Scholar PubMed PubMed Central
[327] Gong X, Fenech B, Blackmore C, Chen Y, Rodgers G, Gulliver J, et al. Association between noise annoyance and mental health outcomes: A systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19(5):2696.10.3390/ijerph19052696Search in Google Scholar PubMed PubMed Central
[328] Mucci N, Traversini V, Lulli LG, Vimercati L, Rapisarda V, Galea RP, et al. Neurobehavioral alterations in occupational noise exposure: a systematic review. Sustainability. 2021;13(21):12224.10.3390/su132112224Search in Google Scholar
[329] Jarach CM, Lugo A, Scala M, van den Brandt PA, Cederroth CR, Odone A, et al. Global prevalence and incidence of tinnitus: A systematic review and meta-analysis. JAMA Neurol. 2022;79(9):888–900.10.1001/jamaneurol.2022.2189Search in Google Scholar PubMed PubMed Central
[330] Mehlum IS, Aarhus L. Occupational noise: A determinant of social inequalities in health. In: Theorell, T. (ed.), Handbook of socioeconomic determinants of occupational health. Handbook series in occupational health sciences. Cham: Springer. 2020. p. 1–15.10.1007/978-3-030-05031-3_2-1.Search in Google Scholar
[331] Helmer R. Guidelines for community noise. London: World Health Organization (WHO); 1999.Search in Google Scholar
[332] Lefèvre M, Chaumond A, Champelovier P, Allemand LG, Lambert J, Laumon B, et al. Understanding the relationship between air traffic noise exposure and annoyance in populations living near airports in France. Environ Int. 2020;144:106058.10.1016/j.envint.2020.106058Search in Google Scholar PubMed
[333] Lee W, Chun C, Kim D, Lee S. Modeling and mapping of combined noise annoyance for aircraft and road traffic based on a partial loudness model. Int J Environ Res Public Health. 2021;18(16):8724.10.3390/ijerph18168724Search in Google Scholar PubMed PubMed Central
[334] Liebich T, Lack L, Hansen K, Zajamšek B, Lovato N, Catcheside P, et al. A systematic review and meta‐analysis of wind turbine noise effects on sleep using validated objective and subjective sleep assessments. J Sleep Res. 2021;30(4):e13228.10.1111/jsr.13228Search in Google Scholar PubMed
[335] Chen K-H, Su S-B, Chen K-T. An overview of occupational noise-induced hearing loss among workers: epidemiology, pathogenesis, and preventive measures. Environ Health Preventive Med. 2020;25(1):1–10.10.1186/s12199-020-00906-0Search in Google Scholar PubMed PubMed Central
[336] Chen XM, Xue XM, Yu N, Guo WW, Yuan SL, Jiang QQ, et al. The role of genetic variants in the susceptibility of noise-induced hearing loss. Front Cell Neurosci. 2022;16:946206.10.3389/fncel.2022.946206Search in Google Scholar PubMed PubMed Central
[337] Gao Y, Wang HY, Guan J, Lan L, Zhao C, Xie LY, et al. Genetic susceptibility study of Chinese sudden sensorineural hearing loss patients with vertigo. Curr Med Sci. 2021;41(4):673–9.10.1007/s11596-021-2422-2Search in Google Scholar PubMed
[338] Parham K, Sohal M, Petremann M, Romanet C, Broussy A, Van Ba CT, et al. Noise-induced trauma produces a temporal pattern of change in blood levels of the outer hair cell biomarker prestin. Hearing Res. 2019;371:98–104.10.1016/j.heares.2018.11.013Search in Google Scholar PubMed
[339] Abbasi M, Yazdanirad S, Dehdarirad H, Hughes D. Noise exposure and the risk of cancer: a comprehensive systematic review. Rev Environ Health. 2023;38(4):713–26.10.1515/reveh-2022-0021Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Article
- Sound event detection by intermittency ratio criterium and source classification by deep learning techniques
- Influence of land cover on noise simulation output – A case study in Malmö, Sweden
- Main design parameters to build acoustic maps by measurements in Uruguay
- Review Article
- A review of the studies investigating the effects of noise exposure on humans from 2017 to 2022: Trends and knowledge gaps
- Letter to the Editor
- Rethinking environmental noise assessment through a noise footprint framework
- Special Issue: Strategic noise mapping in the CNOSSOS-EU era - Part II
- CNOSSOS-EU road surface types: Evaluation of the influence of different national values on noise emissions
Articles in the same Issue
- Research Article
- Sound event detection by intermittency ratio criterium and source classification by deep learning techniques
- Influence of land cover on noise simulation output – A case study in Malmö, Sweden
- Main design parameters to build acoustic maps by measurements in Uruguay
- Review Article
- A review of the studies investigating the effects of noise exposure on humans from 2017 to 2022: Trends and knowledge gaps
- Letter to the Editor
- Rethinking environmental noise assessment through a noise footprint framework
- Special Issue: Strategic noise mapping in the CNOSSOS-EU era - Part II
- CNOSSOS-EU road surface types: Evaluation of the influence of different national values on noise emissions

