Abstract
Objectives
The purpose of this study was to analyze the role of C-reactive protein/albumin ratio (CRP/ALB) in the diagnosis of complicated appendicitis in adults.
Methods
A retrospective analysis of 202 patients with acute appendicitis admitted to the Emergency Department of Weifang People’s Hospital between January 2021 and December 2022 was conducted. Patients were classified into complicated appendicitis group (CA) and non-complicated appendicitis group (NCA) based on postoperative pathological diagnosis, and the two groups were compared in terms of preoperative age, gender, white blood cell count (WBCC), C-reactive protein/albumin ratio (CRP/ALB), serum sodium (Na), and fibrinogen (FIB).
Results
The 202 cases of acute appendicitis in this study, 36.6 % (n=74) were CA. Multivariate logistic regression analysis showed that CPR/ALB (p≤0.001), FIB (p<0.001), and Na (p=0.011) were risk factors for complicated appendicitis. The results of receiver operating characteristic (ROC) analysis, conducted to evaluate the role of CRP/ALB, Na, and FIB in detecting CA, showed that the area under the curve (AUC) of CRP/ALB was 0.871, which was higher than that of FIB and Na. CRP/ALB ratio ≥1.04 was an important indicator for predicting complicated appendicitis, with a sensitivity of 78.2 % and specificity of 84.7 %.
Conclusions
CRP/ALB ratio can serve as a good indicator for predicting complicated appendicitis.
Introduction
Acute appendicitis (AA) is one of the most common acute abdominal emergencies in general surgery [1]. As a frequently encountered acute abdominal symptom, the lifetime risk of AA in men and women is 8.6 and 6.9 %, respectively [2]. According to the pathological type, AA can be classified into two categories: non-complicated appendicitis (NCA) and complicated appendicitis (CA), where NCA includes acute simple and suppurative appendicitis, while CA involves appendiceal necrosis, perforation or periappendiceal abscess [3]. About 3.8–5.0 % of AA patients develop into CA due to delayed treatment, rapid progression of disease or ineffective anti-infective treatment, resulting in severe intra-abdominal infection [4]. Complications related to appendectomy, prolonged hospitalization and secondary surgery are suggested to be associated with acute CA [5]. Although surgical treatment is effective for CA, it may lead to postoperative complications such as adhesive ileus, hemorrhage, and fecal leakage. With the development of digestive endoscopy, endoscopic retrograde appendicitis treatment (ERAT) can be a choice for NCA patients. ERAT has advantages over appendectomy, including no skin incision, organ preservation, reduced postoperative pain, early oral intake, faster recovery, fewer postoperative complications and shorter hospitalization [6]. However, how to accurately and early identify acute CA and NCA is a major challenge. Clinical presentation, Alvarado score and ultrasonography can be helpful for diagnosing AA, but it is difficult to determine the type of appendicitis. In about half of the patients, ultrasonography may fail to detect the appendix clearly, and computed tomography (CT) is limited by radiation and high cost [7]. Therefore, various common inflammatory markers, such as white blood cell count, neutrophil count and mean platelet volume, have been used to predict acute perforated appendicitis due to their simplicity and feasibility [8, 9]. The C-reactive protein/albumin ratio (CRP/ALB) is a novel inflammation-based prognostic score that is related to the severity of inflammation [10]. Previous reports [11, 12] have shown that CRP/ALB is a marker for predicting the surgical mortality of necrotizing enterocolitis in newborns and the prognosis of septicemia in children. CRP/ALB is related to the disease progression of various infectious diseases and has been widely applied in prognostic prediction of diseases such as pancreatic tumors, colon cancer, rectal cancer [13], [14], [15]. Hyponatremia is a common electrolyte disturbance, and studies have shown that it is associated with increased incidence and mortality in the perioperative period [16]. In inflammatory cases, the occurrence of hyponatremia may involve the process of inflammatory cytokines and antidiuretic hormone (ADH) secretion. Inflammation leads to an increase in interleukin (IL)-1b and IL-6 levels, which stimulate ADH release, ultimately resulting in hyponatremia [17, 18]. According to some studies, an elevated level of fibrinogen (FIB) is associated with the severity of acute appendicitis [19]. To further investigate the predictive value of CRP/ALB ratio, serum Na and FIB for CA, we conducted the following study.
Materials and methods
A retrospective analysis was conducted using a sample of patients aged 18 years and above who underwent appendectomy at the Emergency and General Surgery Department of Weifang People’s Hospital between January 2021 and December 2022, all of whom were diagnosed with acute appendicitis.
Inclusion criteria were as follows: (1) age of 18 years or above, (2) previous appendectomy at our hospital, (3) pathologically confirmed acute appendicitis, and (4) approved by the hospital’s Ethics Committee.
Patients who underwent elective surgery or those with infectious diseases, malignant tumors, liver or kidney disease, chronic inflammatory diseases, and hematologic disorders were excluded from the study. Additionally, participants who underwent appendectomy for other reasons (such as malignant tumors) but were pathologically confirmed not to have acute appendicitis were also excluded. The surgical procedures included open or laparoscopic surgery, and postoperative specimens were examined by the pathology department of Weifang People’s Hospital. All patient data were obtained from the hospital’s electronic medical record system.
Laboratory parameters (white blood cell count, serum sodium, fibrinogen, and C-reactive protein/albumin ratio), age, gender, and pathological classification of acute appendicitis were collected. Based on the postoperative pathological examination results of acute appendicitis, gangrenous/perforated appendicitis was classified as complicated appendicitis, while simple and suppurative appendicitis were classified as uncomplicated appendicitis.
Statistical methods
All data were organized and stored in an electronic database (Microsoft Excel) and analyzed using SPSS 25.0. The curve graphs were plotted utilizing GraphPad Prism 9.5. Quantitative variables were reported as mean ± standard deviation or median, interquartile range, while categorical variables were presented as counts and percentages. The Student’s t-test and Mann-Whitney U test were used for continuous data analysis, and the Pearson chi-square test was used for categorical variables. Multiple logistic regression analysis was conducted to identify independent factors associated with complex appendicitis. ROC curve analysis and the area under the curve (AUC) were used to identify independent predictors of complex appendicitis and determine the optimal cut-off point for diagnosing complex appendicitis. A p-value of <0.05, a 95 % confidence interval (95 % CI), and a 5 % margin of error were considered statistically significant.
Results
During the study period, a total of 236 patients who underwent appendectomy were collected. Based on the inclusion and exclusion criteria, 202 patients were finally included in the study, among whom 130 (64.4 %) were male and 72 (35.6 %) were female. Of the 202 patients, data showed that 74 (36.6 %) were found to have complicated appendicitis (CA), while the remaining 128 (63.4 %) had non-complicated appendicitis (NCA). The mean age of the 202 patients was 43 (31;57). When the patients were assessed separately, the mean age of CA and NCA patients were 46.5 (33.75;59.75) and 39.5 (30;57) (p=0.303). The mean serum Na level of CA patients was lower than that of NCA patients, and the mean levels of FIB and CPR/ALB were significantly higher in the CA group than in the NCA group (Table 1).
General data comparison between the NCA group and CA group (
| NCA n=128 | CA n=74 | p-Value | |
|---|---|---|---|
| Age | 39.5 (30;57) | 46.5 (33.75;59.75) | 0.303 |
| Gendera | |||
| Male | 77 (60.2 %) | 53 (71.6 %) | 0.001 |
| Female | 51 (39.8 %) | 21 (28.4 %) | |
| WBCC, ×109/L | 11.49 ± 3.68 | 12.92 ± 4.31 | 0.034 |
| FIB, g/L | 3.67 ± 0.96 | 4.82 ± 1.27 | <0.001 |
| CRP/ALB | 0.25 (0.06;0.67) | 2.55 (1.39;4.05) | <0.001 |
| Na, mEq/L | 138.99 ± 2.89 | 136.35 ± 4.13 | <0.001 |
-
aCount and percentage; WBCC, white blood cell count; FIB, fibrinogen; CRP/ALB, C-reactive protein/albumin; Na, serum sodium.
Multivariable logistic regression analysis was performed using two statistically significant variables between groups of NCA=0 and CA=1 patients as independent variables, with the type of acute appendicitis as the dependent variable. The analysis revealed that CPR/ALB (p<0.001), FIB (p<0.001), and serum Na (p=0.011) were independent risk factors for CA (Table 2).
Multivariate logistic regression analysis.
| β | Standard error | p-Value | OR | OR 95 % CI | |
|---|---|---|---|---|---|
| Na | −0.172 | 0.068 | 0.011 | 0.842 | 0.738–0.962 |
| FIB | 1.063 | 0.693 | <0.001 | 2.894 | 1.799–4.658 |
| CRP/ALB | 1.212 | 0.227 | <0.001 | 3.361 | 2.156–5.241 |
-
Na, serum sodium; FIB, fibrinogen; CRP/ALB, C-reactive protein/albumin.
The present study performed ROC curve analysis to determine the diagnostic value of CRP/ALB, FIB, and serum Na in CA. The AUC of CRP/ALB was 0.871, with a critical value of 1.04, sensitivity of 78.2 %, and specificity of 84.7 % (p≤0.001, [95 % CI, 0.816–0.925]). FIB yielded an AUC of 76.6 %, with a critical value of 4.03 g/L, sensitivity of 73.1 %, and specificity of 71.0 % (p<0.0001, [95 % CI, 0.700–0.832]). The AUC of serum Na was 68.0 %, with a critical value of 135 mEq/L, sensitivity of 40.0 %, and specificity of 90.3 % (p≤0.001, [95 % CI, 0.602–0.759]). CRP yielded an AUC of 0.867, with a critical value of 81.55 mg/L, sensitivity of 67.9 %, and specificity of 94.4 % (p≤0.001, [95 % CI, 0.813–0.922]) (Table 3, Figure 1).
ROC results summarized by AUC.
| AUC | Standard error | p-Value | 95 % CI | |
|---|---|---|---|---|
| Na | 0.68 | 0.037 | <0.001 | 0.602–0.759 |
| FIB | 0.766 | 0.034 | <0.001 | 0.700–0.832 |
| CRP/ALB | 0.871 | 0.028 | <0.001 | 0.816–0.925 |
-
Na, serum sodium; FIB, fibrinogen; CRP/ALB, C-reactive protein/albumin.
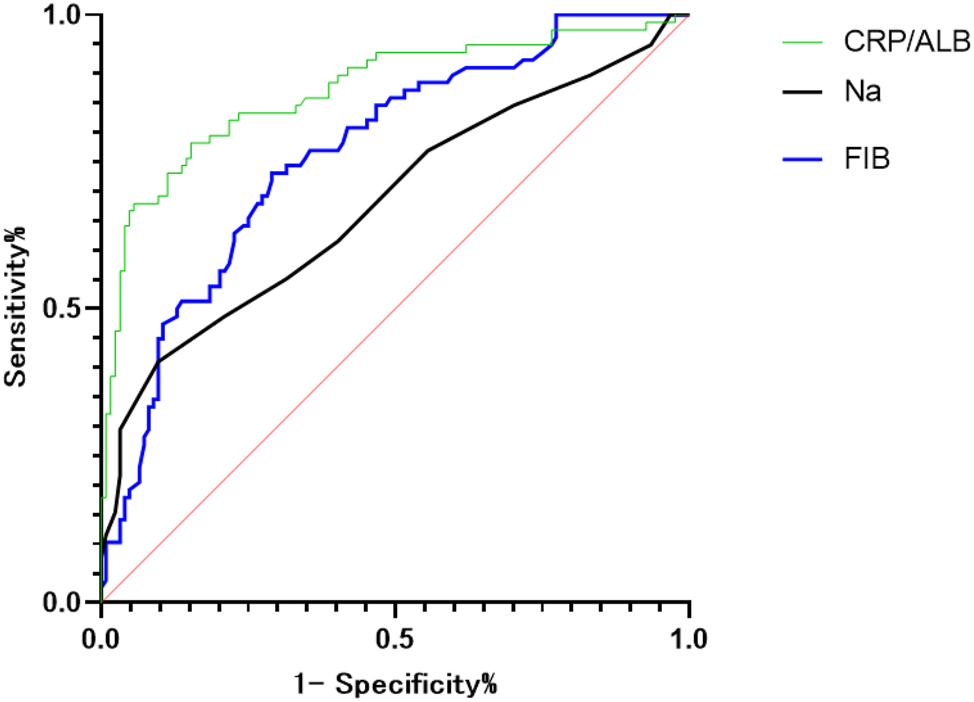
ROC curves.
Discussion
The treatment of acute appendicitis has evolved significantly in recent years, with clinicians having access to a wider range of treatment options. Recent research suggests that most cases of acute uncomplicated appendicitis can be treated using an antibiotic-first approach [20, 21]. Antibiotic therapy alone has been shown to offer several advantages for patients, including avoiding surgical scars, postoperative pain, and a quicker recovery [22]. With the development of digestive endoscopy, less invasive procedures, such as endoscopic retrograde appendicitis therapy (ERAT), have become safe and effective options for the treatment of non-complicated appendicitis. Liu et al. conducted a multicenter retrospective study that analyzed the efficacy and safety of ERAT on treating non-complicated appendicitis in 33 patients, of which 32 experienced immediate relief of abdominal pain [23]. Research has shown that the appendix serves as not only a lymphatic organ with immune function but also as a site for immune replication and regeneration and secretes various digestive enzymes and gastrointestinal hormones. Furthermore, it helps maintain a balance of the intestinal microbiota and reduces the risk of colorectal cancer [24, 25]. For patients with non-complicated appendicitis, a combination of antibiotic and ERAT therapy provides more benefits to long-term quality of life and aligns with patients’ cosmetic requirements. For complicated appendicitis, traditional surgical intervention remains the primary option. However, research has shown that there is a high negative-appendectomy rate of more than 15 % [26]. As such, prompt identification of the type of acute appendicitis is particularly important for selecting the appropriate treatment strategy.
CRP/ALB is considered as a relevant biological marker reflecting microvascular permeability [27]. Several studies have shown that the CRP/ALB ratio can indicate the degree of inflammation and prognosis of inflammatory bowel disease and pancreatitis [28], [29], [30], but there is no report on using CRP/ALB as a diagnostic marker for adult complicated appendicitis. Hu et al. demonstrated that CRP/ALB is a reliable biomarker for complicated appendicitis in children, and patients with a CRP/ALB ratio ≥1.39 are more likely to suffer from complicated appendicitis [31]. Serum Na and FIB, as simple, inexpensive and widely used laboratory tests, have been reported to be helpful in determining the diagnosis of necrotizing soft tissue infections and predicting the mortality of these patients with low serum sodium [32]. Preoperative hyponatremia has been shown to be associated with an increase in perioperative morbidity and mortality [16], and it was found to be an important potential indicator for predicting rectal anastomotic leakage in the report of Alsaleh et al. [33] Acute appendicitis is usually associated with systemic inflammatory response, often leading to coagulation activation, and FIB, as an indicator of pro-inflammatory state, increases several times and acts as a regulator in several pathological conditions such as inflammation after infection or injury, tissue repair or disease-related endothelial damage [34, 35].
In this study, a multiple logistic regression analysis revealed that CPR/ALB, FIB, and Na were independent risk factors for CA. Different cut-off values for CRP/ALB, FIB, and Na levels were established as predictive factors for CA in ROC analysis. CPR/ALB, as a novel inflammatory marker, demonstrated good diagnostic efficacy for CA when the ratio exceeded 1.04. There was no significant difference between using the commonly used cut-off values for low sodium and high fibrinogen levels and the cut-off values identified in this study. We believe that using the widely adopted cut-off values would facilitate the implementation of routine clinical practice. However, the use of cut-off values derived from ROC analysis enhanced the sensitivity and accuracy of CA diagnosis.
Our study has some limitations. Firstly, as our data was retrospectively collected, it only includes patients who underwent appendectomy and does not investigate patients who received conservative treatment. Additionally, this was a small sample, single-center study. Therefore, further validation is required through large-scale prospective studies with multiple centers. Furthermore, potential confounding factors of cases occurring during the COVID-19 pandemic, such as reduced number of patients receiving surgical treatment, may have artificially lowered our number of complication-free cases.
Conclusions
This study aimed to identify predictive factors and indicators of complicated appendicitis through a retrospective analysis. In the adult population, statistically significant results were found indicating that patients with acute appendicitis who have a CRP/ALB ratio ≥1.04, hyponatremia, or hyperfibrinogenemia are more likely to develop complicated appendicitis. Additionally, by combining clinical symptoms and other diagnostic aids, clinicians can accurately diagnose complicated appendicitis. In conclusion, our study highlights the predictive value of CRP/ALB in complicated appendicitis.
-
Research ethics: This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: Xin Zhao and Jun Li wrote the main manuscript text and Jian Yang and Xin Zhao prepared figure and table. Jun Li reviewed and proofread this article. The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Krzyzak, M, Mulrooney, SM. Acute appendicitis review: background, epidemiology, diagnosis, and treatment. Cureus 2020;12:e8562. https://doi.org/10.7759/cureus.8562.Search in Google Scholar PubMed PubMed Central
2. Baird, DLH, Simillis, C, Kontovounisios, C, Rasheed, S, Tekkis, PP. Acute appendicitis. BMJ 2017;357:j1703. https://doi.org/10.1136/bmj.j1703.Search in Google Scholar PubMed
3. Bhangu, A, Søreide, K, Di Saverio, S, Assarsson, JH, Drake, FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 2015;386:1278–87. https://doi.org/10.1016/s0140-6736(15)00275-5.Search in Google Scholar
4. Hansson, LE, Laurell, H, Gunnarsson, U. Impact of time in the development of acute appendicitis. Dig Surg 2008;25:394–9. https://doi.org/10.1159/000180451.Search in Google Scholar PubMed
5. Willis, ZI, Duggan, EM, Bucher, BT, Pietsch, JB, Milovancev, M, Wharton, W, et al.. Effect of a clinical practice guideline for pediatric complicated appendicitis. JAMA Surg 2016;151:e160194. https://doi.org/10.1001/jamasurg.2016.0194.Search in Google Scholar PubMed PubMed Central
6. Liu, BR, Kong, LJ, Ullah, S, Xiao, M, Sun, XZ, Zhang, JY, et al.. Endoscopic retrograde appendicitis therapy (ERAT) vs appendectomy for acute uncomplicated appendicitis: a prospective multicenter randomized clinical trial. J Dig Dis 2022;23:636–41. https://doi.org/10.1016/j.gie.2022.04.591.Search in Google Scholar
7. Acharya, A, Markar, SR, Ni, M, Hanna, GB. Biomarkers of acute appendicitis: systematic review and cost-benefit trade-off analysis. Surg Endosc 2017;31:1022–31. https://doi.org/10.1007/s00464-016-5109-1.Search in Google Scholar PubMed PubMed Central
8. Shafi, SM, Afsheen, M, Reshi, FA. Total leucocyte count, C-reactive protein and neutrophil count: diagnostic aid in acute appendicitis. Saudi J Gastroenterol 2009;15:117–20. https://doi.org/10.4103/1319-3767.48969.Search in Google Scholar PubMed PubMed Central
9. Albayrak, Y, Albayrak, A, Albayrak, F, Yildirim, R, Aylu, B, Uyanik, A, et al.. Mean platelet volume: a new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb Hemost 2011;17:362–6. https://doi.org/10.1177/1076029610364520.Search in Google Scholar PubMed
10. Ni, XF, Wu, J, Ji, M, Shao, YJ, Xu, B, Jiang, JT, et al.. Effect of C-reactive protein/albumin ratio on prognosis in advanced non-small-cell lung cancer. Asia Pac J Clin Oncol 2018;14:402–9. https://doi.org/10.1111/ajco.13055.Search in Google Scholar PubMed
11. Mohd Amin, AT, Zaki, RA, Friedmacher, F, Sharif, SP. C-reactive protein/albumin ratio is a prognostic indicator for predicting surgical intervention and mortality in neonates with necrotizing enterocolitis. Pediatr Surg Int 2021;37:881–6. https://doi.org/10.1007/s00383-021-04879-1.Search in Google Scholar PubMed PubMed Central
12. Wang, QY, Lu, F, Li, AM. The clinical value of high mobility group box-1 and CRP/Alb ratio in the diagnosis and evaluation of sepsis in children. Eur Rev Med Pharmacol Sci 2022;26:6361–6. https://doi.org/10.26355/eurrev_202209_29662.Search in Google Scholar PubMed
13. Fu, YJ, Li, KZ, Bai, JH, Liang, ZQ. C-reactive protein/albumin ratio is a prognostic indicator in Asians with pancreatic cancers: a meta-analysis. Medicine 2019;98:e18219. https://doi.org/10.1097/md.0000000000018219.Search in Google Scholar
14. Haruki, K, Shiba, H, Shirai, Y, Horiuchi, T, Iwase, R, Fujiwara, Y, et al.. The C-reactive protein to albumin ratio predicts long-term outcomes in patients with pancreatic cancer after pancreatic resection. World J Surg 2016;40:2254–60. https://doi.org/10.1007/s00268-016-3491-4.Search in Google Scholar PubMed
15. Shibutani, M, Maeda, K, Nagahara, H, Iseki, Y, Ikeya, T, Hirakawa, K. Prognostic significance of the preoperative ratio of C-reactive protein to albumin in patients with colorectal cancer. Anticancer Res 2016;36:995–1001.Search in Google Scholar
16. Leung, AA, McAlister, FA, Rogers, SOJr, Pazo, V, Wright, A, Bates, DW. Preoperative hyponatremia and perioperative complications. Arch Intern Med 2012;172:1474–81. https://doi.org/10.1001/archinternmed.2012.3992.Search in Google Scholar PubMed
17. Park, SJ, Shin, JI. Inflammation and hyponatremia: an underrecognized condition? Korean J Pediatr 2013;56:519–22. https://doi.org/10.3345/kjp.2013.56.12.519.Search in Google Scholar PubMed PubMed Central
18. Swart, RM, Hoorn, EJ, Betjes, MG, Zietse, R. Hyponatremia and inflammation: the emerging role of interleukin-6 in osmoregulation. Nephron Physiol 2011;118:45–51. https://doi.org/10.1159/000322238.Search in Google Scholar PubMed
19. Li, J, Liu, Y, Yin, W, Zhang, C, Huang, J, Liao, C, et al.. Alterations of the preoperative coagulation profile in patients with acute appendicitis. Clin Chem Lab Med 2011;49:1333–9. https://doi.org/10.1515/cclm.2011.214.Search in Google Scholar
20. Podda, M, Gerardi, C, Cillara, N, Fearnhead, N, Gomes, CA, Birindelli, A, et al.. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg 2019;270:1028–40. https://doi.org/10.1097/sla.0000000000003225.Search in Google Scholar PubMed
21. O’Leary, DP, Walsh, SM, Bolger, J, Baban, C, Humphreys, H, O’Grady, S, et al.. A randomized clinical trial evaluating the efficacy and quality of life of antibiotic-only treatment of acute uncomplicated appendicitis: results of the COMMA trial. Ann Surg 2021;274:240–7. https://doi.org/10.1097/sla.0000000000004785.Search in Google Scholar PubMed
22. Flum, DR. Clinical practice. Acute appendicitis--appendectomy or the “antibiotics first” strategy. N Engl J Med 2015;372:1937–43. https://doi.org/10.1056/nejmcp1215006.Search in Google Scholar
23. Liu, BR, Ma, X, Feng, J, Yang, Z, Qu, B, Feng, ZT, et al.. Endoscopic retrograde appendicitis therapy (ERAT): a multicenter retrospective study in China. Surg Endosc 2015;29:905–9. https://doi.org/10.1007/s00464-014-3750-0.Search in Google Scholar PubMed
24. Kooij, IA, Sahami, S, Meijer, SL, Buskens, CJ, Te Velde, AA. The immunology of the vermiform appendix: a review of the literature. Clin Exp Immunol 2016;186:1–9. https://doi.org/10.1111/cei.12821.Search in Google Scholar PubMed PubMed Central
25. Randal Bollinger, R, Barbas, AS, Bush, EL, Lin, SS, Parker, W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol 2007;249:826–31. https://doi.org/10.1016/j.jtbi.2007.08.032.Search in Google Scholar PubMed
26. Park, JS, Jeong, JH, Lee, JI, Lee, JH, Park, JK, Moon, HJ. Accuracies of diagnostic methods for acute appendicitis. Am Surg 2013;79:101–6. https://doi.org/10.1177/000313481307900138.Search in Google Scholar
27. Cordemans, C, De Laet, I, Van Regenmortel, N, Schoonheydt, K, Dits, H, Huber, W, et al.. Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak, and fluid balance. Ann Intensive Care 2012;2:1–12. https://doi.org/10.1186/2110-5820-2-s1-s1.Search in Google Scholar PubMed PubMed Central
28. Lewis, JD. The utility of biomarkers in the diagnosis and therapy of inflammatory bowel disease. Gastroenterology 2011;140:1817–26. https://doi.org/10.1053/j.gastro.2010.11.058.Search in Google Scholar PubMed PubMed Central
29. Qin, G, Tu, J, Liu, L, Luo, L, Wu, J, Tao, L, et al.. Serum albumin and C-reactive protein/albumin ratio are useful biomarkers of crohn’s disease activity. Med Sci Mon Int Med J Exp Clin Res 2016;22:4393–400. https://doi.org/10.12659/msm.897460.Search in Google Scholar PubMed
30. Wang, X, Cui, Z, Li, H, Saleen, AF, Zhang, D, Miao, B, et al.. Nosocomial mortality and early prediction of patients with severe acute pancreatitis. J Gastroenterol Hepatol 2010;25:1386–93. https://doi.org/10.1111/j.1440-1746.2010.06376.x.Search in Google Scholar PubMed
31. Hou, J, Feng, W, Liu, W, Hou, J, Die, X, Sun, J, et al.. The use of the ratio of C-reactive protein to albumin for the diagnosis of complicated appendicitis in children. Am J Emerg Med 2022;52:148–54. https://doi.org/10.1016/j.ajem.2021.12.007.Search in Google Scholar PubMed
32. Yaghoubian, A, de Virgilio, C, Dauphine, C, Lewis, RJ, Lin, M. Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Arch Surg 2007;142:840–6. https://doi.org/10.1001/archsurg.142.9.840.Search in Google Scholar PubMed
33. Alsaleh, A, Pellino, G, Christodoulides, N, Malietzis, G, Kontovounisios, C. Hyponatremia could identify patients with intrabdominal sepsis and anastomotic leak after colorectal surgery: a systematic review of the literature. Updates Surg 2019;71:17–20. https://doi.org/10.1007/s13304-019-00627-2.Search in Google Scholar PubMed
34. Davalos, D, Akassoglou, K. Fibrinogen as a key regulator of inflammation in disease. Semin Immunopathol 2012;34:43–62. https://doi.org/10.1007/s00281-011-0290-8.Search in Google Scholar PubMed
35. Feng, S, Wu, P, Chen, X. Hyperfibrinogenemia in appendicitis: a new predictor of perforation in children. Pediatr Surg Int 2014;30:1143–7. https://doi.org/10.1007/s00383-014-3585-8.Search in Google Scholar PubMed
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Diagnostic accuracy of stool sample-based PCR in detecting Helicobacter pylori infection: a meta-analysis
- Original Articles
- Assessment of antibody titer and side effects after fourth doses of COVID-19 mRNA vaccination in 38 healthy volunteers
- The predictive value of the C-reactive protein/albumin ratio in adult patients with complicated appendicitis
- A novel multimodal approach for the assessment of phlebotomy performance in nurses
- A new approach to the interpretation of B-type natriuretic peptide concentration in children with congenital heart disease
- Bilirubin is a superior biomarker for hepatocellular carcinoma diagnosis and for differential diagnosis of benign liver disease
- Congress Abstracts
- German Congress of Laboratory Medicine: 18th Annual Congress of the DGKL and 5th Symposium of the Biomedical Analytics of the DVTA e. V.
Articles in the same Issue
- Frontmatter
- Review
- Diagnostic accuracy of stool sample-based PCR in detecting Helicobacter pylori infection: a meta-analysis
- Original Articles
- Assessment of antibody titer and side effects after fourth doses of COVID-19 mRNA vaccination in 38 healthy volunteers
- The predictive value of the C-reactive protein/albumin ratio in adult patients with complicated appendicitis
- A novel multimodal approach for the assessment of phlebotomy performance in nurses
- A new approach to the interpretation of B-type natriuretic peptide concentration in children with congenital heart disease
- Bilirubin is a superior biomarker for hepatocellular carcinoma diagnosis and for differential diagnosis of benign liver disease
- Congress Abstracts
- German Congress of Laboratory Medicine: 18th Annual Congress of the DGKL and 5th Symposium of the Biomedical Analytics of the DVTA e. V.

