Comparison of student perception and performance between case-based learning and lecture-based learning in a clinical laboratory immunology course
-
Xingming Ma
, Yanping Luo
Abstract
Background:
Case-based learning (CBL), an educational method of problem-based learning, provides students with a venue to relate content learned in the classroom to performance in professional practice. This study compared CBL in the teaching of a clinical laboratory immunology (CLI) course to lecture-based learning (LBL), and evaluated the effect on students regarding the CBL.
Methods:
Data were collected from senior students (n=85; 46% males, 54% females) at Lanzhou University in China. The students were divided into two groups, one group was offered CBL, while the other LBL as a teaching instrument. After intervention, perceptions of both the groups about their respective teaching method were evaluated using questionnaires, the resulting scores were compared to those obtained in the LBL group.
Results:
The CBL group showed significantly better scores in course examination (p<0.05) as compared to the LBL group. Seventy-seven (90.6%) students in the CBL group opined that CBL improved their learning and clinical problem-solving skills. CBL also provided them with better understanding (90.6%) and preparation for examinations (90.6%). CBL group improved markedly in comparison to the LBL group with regard to learning motivation (p=0.040), clinical reasoning ability (p=0.023) and clinical problem-solving ability (p=0.022).
Conclusions:
Our findings demonstrate that CBL is a more effective teaching strategy as compared to LBL in a CLI course. Consequently, the implementation of CBL in teaching a CLI course helps students to improve their learning motivation, problem solving abilities and mastery of knowledge.
Introduction
According to Bloom’s cognitive taxonomy, higher orders of learning, above those of knowledge and comprehension, are crucial for clinical medicine training in medical education [1]. Clinical laboratory immunology (CLI), one of the major courses for medical students, is the study of application of immunological technology in clinical laboratory science [2]. For many years, the conventional (didactic lecture) teaching style, teacher-centered instruction has been dominant in higher education in China. In a traditional classroom, students become passive learners, or rather just recipients of teachers’ knowledge [3], [4]. Over the past few decades, attention has been paid to promoting active learning by adopting interactive student-centred approaches in undergraduate medical education, including problem-based learning (PBL) and case-based learning (CBL) [5], [6], [7].
PBL is an educational approach that is being implemented differently in different medical schools. PBL was first introduced by the McMasters University Medical School in Hamilton, Ontario, Canada in late 1960s by Howard Barrows and his colleagues as an educational format centered around the discussion and learning that emanates from a clinical based problem [8]. CBL, an educational method of PBL, provides students with a venue to relate content learned in the classroom to performance in professional practice [9], [10]. This process can be initiated as students solve problems that are posed in simulated real-life situations. CBL, an active learning process, helps learners be pro-active for their own study with the help from their peers, [6], [7], [9], [10]. As a result, teachers become facilitators, and students are far more independent and will learn from their own experience [11].
CBL is also a constructive learning paradigm, in which learners select and transform information, construct ideas, and make decisions based on their current or past knowledge [12], [13]. A case, as a trigger to initiate the learning, is generally written as a problem that provides the student with the history or background of a patient and the clinical situation of the patient including information such as vital signs, symptoms, and laboratory results [11]. In CBL, classroom instructors help students to solve diverse case-based problems that may occur in real-world situations, moving from abstract knowledge to practical applications [13], [14].
In our institute, the CLI course is mainly taught by means of didactic lectures including tutorials, and practical classes which mainly result in teacher-centered, unidirectional learning. The objectives of this study were to find the benefits of CBL in the teaching of the CLI course as compared to didactic lectures, and to evaluate the perceptions of participating students regarding CBL. The hypothesis was that students would have a positive attitude towards this course in response to the new instructional design we introduced.
Materials and methods
Course information
The CLI course, approximately 18 weeks’ duration, was offered during the autumn semester in each academic year at Lanzhou University. Both CBL and traditional lecture-based learning (LBL) education were conducted by the same group of teachers from the Department of Immunology, School of Basic Medical Sciences, Lanzhou University. Every teacher taught the same curriculum contents in both groups. A weekly schedule in the CLI course included 4 h of didactic lectures (total 72 h) and one laboratory session (total 54 h) of 3 h duration.
Study participants
A total of 85 senior students were enrolled in the CLI course during the autumn semester in 2012 year group (n=44), and in 2013 year group (n=41), respectively. All the students in each year were divided into two groups by sortition. One group was offered CBL, while the other was offered LBL as the teaching instrument. In the mid semester, the students undertook the first exam and then had to cross over from CBL to LBL (Figure 1). All participants were enrolled in a mandatory CLI course, which was delivered through traditional LBL and CBL. Moreover, participants who completed the questionnaire survey also filled out an informed consent form agreeing to participate in the study. Students in CBL group were briefed on the study purpose and process, and without any adverse effect on this course grade.
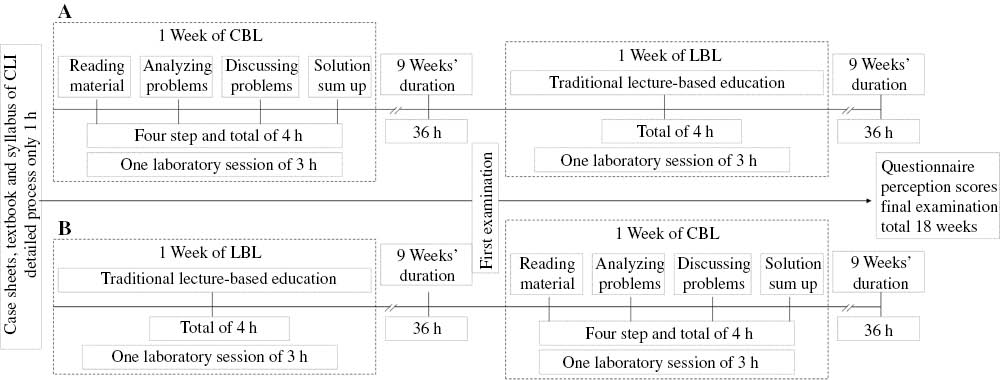
A weekly schedule and curriculum designing in the CLI course.
(A) Schedule of the CBL group. (B) Schedule the LBL group. CLI, clinical laboratory immunology course.
Ethical considerations
Before the study, approval was obtained from the Curriculum Development Committee and Ethics Committee at School of Basic Medical Sciences, Lanzhou University in China.
Curriculum designing and management
According to the syllabus of the CLI course, a total 35 different case sheets with a history and relevant information was designed by a committee of three professors of immunology, a chief physician of hematology and a chief physician of rheumatology from Lanzhou University. For a case, the five leading-problems were determined by the committee to be important in the education of those studying CLI science.
At the beginning of the CBL, a facilitator briefed the students about how CBL worked for 1 h. The CBL group was then further divided into five subgroups for thorough discussion. CBL lasted a total of 4 h which included reading the material, discussion and summarization, and during this time, the team facilitator adjusted the time and direction of the discussion in order to ensure smoothness and to avoid deviation from the given topic. In this manner, the program was conducted over four sessions, one per week, 1 h per session (Figure 1).
In the first step, CBL students were given the cases and were asked to analyze the five leading problems. In the second step, each individual student was asked to provide a detailed plan for solving problems. In the third step, based on the individually collected solution plans, data were collected. Through discussions, students were encouraged to compare and analyze the source of the problems, and to draw various conclusions based on the proposed/discussed solutions. The role of the facilitator was to help students focus on learning objectives and ensure group dynamics. In the last step, based on the results and data gathered from the aforementioned discussions, the most appropriate solutions to the problems were proposed via the facilitator.
In the LBL group, the students firstly received the reading material including case sheets, textbook and syllabus of the CLI course. Then, the topics of each chapter were taught through the traditional didactic lecture mode given by the instructors for 4 h each week. Students had opportunities to ask questions and use reference books and teaching materials, and these were also used by the CBL group. Finally, the teachers answered students’ questions and repeated any points that had not been fully understood.
Evaluation methods
A cross sectional survey was conducted among the students using a questionnaire in order to assess the students’ perceptions of CBL. These included items regarding CBL and how it linked to their learning, analytical and problem-solving abilities. The student responses were in the yes/no pattern.
Capability perceptions on CBL and LBL were recorded using a separate questionnaire in which responses were graded on Likert scale from strongly agree to strongly disagree according to the syllabus of the course. Students scored statements according to their perceptions from 1 (strongly disagree) to 5 (strongly agree), and total perception scores were calculated in Table 3. Besides assessing their level of responses with overall planning and conduct of CBL, it also rated the impact of CBL on student learning of the CLI course subject matter.
In order to assess the academic performance of students in the mastery of knowledge of the CLI course after CBL and conventional LBL lectures, we compared the average scores obtained by the two group students in course examinations. In the mid semester and at end of the course, the students undertook the same first and last examination with 100 multiple choice questions, respectively.
Statistical analysis
The test scores of the groups were compared by paired T-tests and the percentages of highest scores (marks≥80) of the groups were compared by the Pearson’s χ2-test through SPSS 19.0 for Windows software (SPSS, Inc., Chicago, IL, USA). Statistical significance was defined as p<0.05.
Results
In a total of 85 students, there were no differences in gender proportion or mean age between the groups in Table 1 (p>0.05). Among the 85 students who participated in the survey, 81 (95.3%) students believed that the case scenarios were appropriate for the lecture topics, and 77 (90.6%) students agreed that CBL helped their learning skills, clinical problem-solving skills, understanding the difficult contents, and preparing for examinations. There were also 66 (77.6%) participants who thought that CBL contributed to understanding the CLI course learning objectives (Table 2).
The gender and age characteristics of students.
| Class | Gender | Age/year (mean±SD) | |
|---|---|---|---|
| Male (%) | Female (%) | ||
| 2012 | 20 (44.4) | 25 (55.6) | 22.3±1.36 |
| 2013 | 19 (46.3) | 21 (52.7) | 22.2±1.41 |
The CLI students’ questionnaire on case-based learning and participants’ responses (n=85).
| Question/statement | Responses (yes in %) | ||
|---|---|---|---|
| In 2012 n=44 | In 2013 n=41 | Total n=85 | |
| Case scenarios were appropriate for the lecture topics | 42 (95.5) | 39 (95.1) | 81 (95.3) |
| Five leading-problems were appropriate for the case | 40 (93.2) | 35 (85.4) | 75 (88.2) |
| CBL was an effective learning tool for me | 36 (81.8) | 39 (95.1) | 75 (88.2) |
| CBL sessions helped me learning CLIa | 38 (86.4) | 37 (90.2) | 75 (88.2) |
| The reference materials for CBL were useful/adequate | 36 (81.8) | 39 (95.1) | 75 (88.2) |
| CBL improved my learning skills | 40 (91.7) | 37 (90.2) | 77 (90.6) |
| CBL improved my independent learning skills | 38 (86.4) | 33 (80.5) | 71 (83.5) |
| CBL improved my analytical skills | 38 (86.4) | 37 (90.2) | 75 (88.2) |
| CBL improved my communication skills | 36 (81.8) | 35 (85.4) | 71 (83.5) |
| CBL improved my clinical problem-solving skills | 38 (86.4) | 39 (95.1) | 77 (90.6) |
| Student discussion addresses the lecture objectives | 38 (86.4) | 35 (85.4) | 73 (85.9) |
| CBL helped me generating questions for further investigation the problems in the case | 38 (86.4) | 35 (85.4) | 73 (85.9) |
| CBL helped me understanding the course objectives | 33 (75.0) | 33 (80.5) | 66 (77.6) |
| CBL improved my ability to retain information | 34 (77.3) | 31 (75.6) | 65 (76.5) |
| CBL improved my ability to work within a team | 34 (77.3) | 37 (90.2) | 71 (83.5) |
| CBL allowed me to help other students in my group understand difficult cases | 38 (86.4) | 39 (95.1) | 77 (90.6) |
| CBL helped me better understand the difficult contents in this course | 38 (86.4) | 39 (95.1) | 77 (90.6) |
| CBL helped me prepare for exams | 40 (93.2) | 37 (90.2) | 77 (90.6) |
| The faculty present during CBL facilitated the whole process | 36 (81.8) | 35 (85.4) | 71 (83.5) |
| Time allowed for case discussion was sufficient | 36 (81.8) | 37 (90.2) | 73 (85.9) |
aCLI, clinical laboratory immunology course.
The average sums of the perception scores in the CBL and LBL groups were 43.82±5.59 and 42.31±5.51 in Table 3, respectively, which showed no significant difference in students’ capability perceptions with the educational method between the CBL group and the LBL group (t=1.770, p=0.079). There were significantly different perception scores in the learning motivation (t=2.091, p=0.040), clinical reasoning ability (t=2.310, p=0.023), clinical problem-solving ability (t=2.337, p=0.022) and preparing for exams (t=2.043, p=0.044) between the groups (Table 3).
Capability perception scores in both groups (mean±SD) (n=85).
| Question/statement | CBL group | LBL group | t (p) |
|---|---|---|---|
| Increase study interest in CLIa | 4.44±0.91 | 4.20±0.98 | 1.678 (p=0.095) |
| Help to understand basic concepts | 4.42±1.13 | 4.10±1.00 | 0.739 (p=0.461) |
| Increase learning motivation | 4.56±0.80 | 4.15±0.96 | 2.090 (p=0.040)b |
| Enhance clinical reasoning ability | 4.47±0.83 | 4.10±1.05 | 2.311 (p=0.023)b |
| Extent more related knowledge | 4.24±0.88 | 4.30±0.85 | –0.418 (p=0.676) |
| Enhance clinical problem-solving ability | 4.56±0.72 | 4.10±1.05 | 2.337 (p=0.022)b |
| Improve peer interaction | 4.15±0.89 | 4.25±0.83 | –0.497 (p=0.620) |
| Help to prepare for exams | 4.47±0.89 | 4.05±0.97 | 2.043 (p=0.044)b |
| Promote self-learning skills | 4.33±0.82 | 4.20±0.90 | 0.708 (p=0.481) |
| Time allotted was appropriate | 4.26±0.80 | 4.32±0.88 | –0.317 (p=0.752) |
| Sum of perception scores (5×10=50) | 43.82±5.59 | 42.31±5.51 | 1.770 (p=0.079) |
Students scored statements according to their perceptions from 1 (strongly disagree) to 5 (strongly agree), and total perception scores were calculated. This data shown the CBL approach would help students improve their learning motivation, clinical problem-solving abilities, as well as help them in long-term retention of knowledge, which in turn helped them in performing better in their examination. aCLI, clinical laboratory immunology course. bp<0.05.
The majority of students (83.5%) believed that CBL contributed to improving their communication skills and ability to work as part of a team (Table 2). Compared with peer interaction perception scores in both groups there was a higher perception score in improving peer interaction in CBL group (4.25±0.83) than those in LBL group (4.15±0.89) (Table 3). However, there were no significant different perception score in both groups on improving peer interaction (t=–0.497, p=0.620).
The course test scores of the CBL group (81.20±5.17, range 60–96) were significantly higher (p=0.001) than those of the LBL group (76.67±7.17, range: 60–95) (Figure 2A). Fifty-four students (54/85=61%) achieved test scores higher than 80 in the CBL group, whilst this was the case for 23 students (23/85=28%) in the LBL group. The percentage of high test score (marks≥80) was significantly higher (p=0.001) in the CBL group than in the LBL group (Figure 2B).
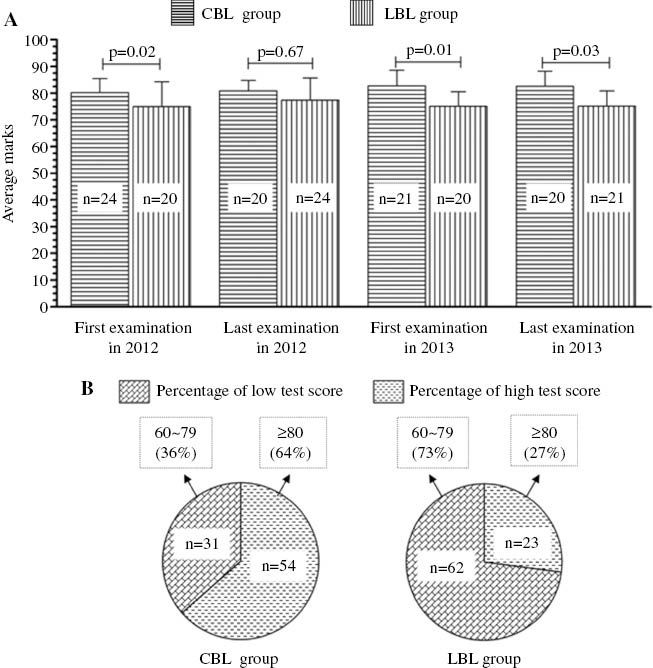
Comparison of clinical laboratory science students’ scores.
(A) Average marks. (B) The percentage of high test score (marks≥80) on CBL group (n=85) and LBL group (n=85) for the CLI course examinations (mean±SD).
Discussion
For the students of clinical laboratory science, it is very important to apply laboratory immunology knowledge into clinical practice [2]. Learning through CBL helps students to build on prior knowledge, integrate knowledge, and consider an application to future situations. While it is widely agreed upon that problem solving skills are essential in the practice of medicine, there is a wide spread skepticism to transform educational strategies in this direction [11], [15]. There are very few medical schools in China who have whole-heartedly embraced these approaches. Though we met the challenge of a traditional curricular framework, the CBL educational approach was first introduced in the CLI course for clinical laboratory science students in Lanzhou University, and the benefits of CBL in the teaching of this course were evaluated in 2012 and 2013.
Most of previous studies reported that CBL is a powerful educational strategy which improves students’ problem-solving abilities, independent learning skills and their ability to prepare for examinations [16], [17], [18], [19]. The findings of the current investigation are consistent with previous studies which examined the impact of CBL for clinical laboratory science students in the CLI course. Our study showed that 88.2% of students agreed that CBL provides a self-directed learning approach and helped them to learn the CLI course. CBL provides students with the opportunity to ask important analytical questions, consider various responses, and argue for or against various situations [13], [20], [21]. Our study data shows that 90.6% of students stated that CBL improved their clinical problem-solving skills, learning skills and helped them to better prepare for examinations, as well as improved their understanding of the subject matter and helped them to develop their clinical thinking in making their own diagnosis. As CBL focuses on real-life case problems, it is a potentially powerful method for training students’ ability in the CLI course. The cases presented using CBL enabled students to integrate and apply their developing clinical knowledge, as well as to reflect on complex situations, as opposed to performing clearly defined, predetermined tasks [20]. In addition, CBL encourages students to actively create their own knowledge and independently develop solutions, rather than refer to the knowledge imparted to them by educators or textbooks for problem solving [20]. This would promote the motivation to learn and help in their mastery of knowledge of the CLI course.
Although, CBL has been documented in the past as an effective teaching method to enhance the capability of medical students [16], [17], [18], [19], [22], few studies have been carried out to evaluate the effectiveness of CBL in the CLI course for clinical laboratory science students in China. The present study is the first step in curriculum innovation in the CLI course. To fully appreciate CBL, prospective follow-up studies are needed to monitor students’ progress. The present study only surveyed the students’ perceptions of CBL and LBL education. As compared to the LBL group, there was a significant increase of perception score in learning motivation (p=0.040), clinical reasoning ability (p=0.023), clinical problem-solving ability (p=0.022) and preparing for exams (p=0.044) in the CBL group. Our study data shows the CBL approach would help clinical laboratory science students improve their learning motivation, and problem solving abilities, as well as help them in the long-term retention of the CLI knowledge in the study, which in turn helped them to preform better in their examination. Therefore, the introduction of the CBL educational strategy would not only help the students gain requisite knowledge in the CLI course but also enhance their analytic and problem-solving skills.
Several limitations pertaining to this study must be considered when interpreting the findings. First, this study is limited in the sample size. Only 85 students were involved in this study from Lanzhou university during 2 years. This may not fully allow for generalizing the findings to the general population of clinical laboratory science students. Second, the instrument utilized to assess students’ perceptions was only designed to be administered on a single occasion at the end of this course, rather than assessing students’ perceptions on each separate unit and comparing the results. A multi-stage assessment of changes in student perceptions would have been more reliable for measuring student attitudes towards course restructuring. The final limitation was that we did not consider the student’s attitude in the current course and learning styles such as interactive or passive.
Conclusions
This pilot study was the first step of curriculum innovation in the CLI course. The overall positive response from the students confirms that CBL is a more effective teaching strategy and educational mode as compared to LBL in the CLI course.
Acknowledgments
We thank Dr. Jinyu Shan of the University of Leicester, UK, for assistance in editing the language.
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission. Xingming Ma conception and design of research; Yanping Luo, Jingqiu Wang, Lifeng Zhang, Yaling Liang, Yufeng wu, Hongjuan Yu and Mingqiang Cao performed experiments; Xingming Ma, Yanping Lu, Jingqiu Wang and Lifeng Zhang analyzed data; Xingming Ma, Yanping Lu and Jingqiu Wang drafted manuscript.
Research funding: This work was supported by the Teaching Research Project of Lanzhou University in China (201125).
Employment or leadership: None declared.
Honorarium: None declared.
Competing interests: The funding organization(s) played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
References
1. Robert ED, Adam MP. Use of case-based learning in a clinical pharmacokinetics course. Am J Pharm Educ 2008;72:29.10.5688/aj720229Search in Google Scholar PubMed PubMed Central
2. Lanlan W, Huaxi X. Clinical laboratory immunology, 5th ed. Beijing: People’s Medical Publishing House, 2013:2–11.Search in Google Scholar
3. Ghosh S. Combination of didactic lectures and case-oriented problem-solving tutorials toward better learning: perceptions of students from a conventional medical curriculum. Adv Physiol Educ 2007;31:193–7.10.1152/advan.00040.2006Search in Google Scholar PubMed
4. Meier S, Hoode R, Meier R. Problem-solving: teacher’s perceptions, content area models and interdisciplinary connection. Sch Sci Math 1996;96:230–7.10.1111/j.1949-8594.1996.tb10234.xSearch in Google Scholar
5. Husain A. Problem-based learning: a current model of education. Oman Med J 2011;26:294–5.10.5001/omj.2011.74Search in Google Scholar PubMed PubMed Central
6. Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med 2007;82: 74–82.10.1097/01.ACM.0000249963.93776.aaSearch in Google Scholar PubMed
7. Yasin IT. The Impact of small group case-based learning on traditional pharmacology teaching. Sultan Qaboos Univ Med J 2013;13:115–20.10.12816/0003204Search in Google Scholar PubMed PubMed Central
8. Puja D, Nirmal AP. Case based methodology: a method to enhance the learning of physiological basis of cardiovascular and respiratory system to undergraduate medical students. Am J Educ Res 2013;1:425–9.10.12691/education-1-10-3Search in Google Scholar
9. Armbruster P, Patel M, Johnson E, Weiss M. Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology. CBE-Life Sci Educ 2009;8:203–13.10.1187/cbe.09-03-0025Search in Google Scholar PubMed PubMed Central
10. Chan WP, Hsu CY, Hong CY. Innovative “case-based integrated teaching” in an undergraduate medical curriculum: development and teachers’ and students’ responses. Ann Acad Med Singapore 2008;37:952–6.10.47102/annals-acadmedsg.V37N11p952Search in Google Scholar
11. Ciraj AM, Vinod P, Ramnarayan K. Enhancing active learning in microbiology through case based learning: experiences from an Indian medical school. Indian J Pathol Microbiol 2010;53:729–33.10.4103/0377-4929.72058Search in Google Scholar PubMed
12. Brandon AF, All AC. Constructivism theory analysis and application to curricula. Nurs Educ 2010;31:89–92.Search in Google Scholar
13. Moon-Sook Y, Hyung-Ran P. Effects of case-based learning on communication skills, problem-solving ability, and learning motivation in nursing students. Nurs Health Sci 2015;17:166–72.10.1111/nhs.12151Search in Google Scholar PubMed
14. Srisawasdi N. Fostering pre-service STEM teachers’ technological pedagogical content knowledge: a lesson learned from case-based learning approach. J Korean Assoc Sci Educ 2012;32:1356–66.10.14697/jkase.2012.32.8.1356Search in Google Scholar
15. Wojtczak A, Roy SM. Minimum essential requirements and standards in medical education. Med Teach 2000;22:555–9.10.1080/01421590050175514Search in Google Scholar PubMed
16. Blewett EL, Kisamore JL. Evaluation of an interactive, case-based review session in teaching medical microbiology. BMC Med Educ 2009;9:56.10.1186/1472-6920-9-56Search in Google Scholar PubMed PubMed Central
17. Hirshbein LD, Gay T. Case-based independent study for medical students in emergency psychiatry. Acad Psychiatry 2005;29:96–9.10.1176/appi.ap.29.1.96Search in Google Scholar PubMed
18. Kumar V, Gadbury-Amyot CC. A case-based and team-based learning model in oral and maxillofacial radiology. J Dental Educ 2012;76:330–7.10.1002/j.0022-0337.2012.76.3.tb05262.xSearch in Google Scholar
19. Thurman J, Volet SE, Bolton JR. Collaborative, case-based learning: how do students actually learn from each other? J Vet Med Educ 2009;36:297–304.10.3138/jvme.36.3.297Search in Google Scholar PubMed
20. Mukeshkumar BV, Chinmay JS. Case-based learning in pharmacology: moving from teaching to learning. Int J Appl Basic Med Res 2015;5:S21–3.10.4103/2229-516X.162259Search in Google Scholar PubMed PubMed Central
21. Newble DI, Entwistle NJ. Learning styles and approaches: implications for medical education. Med Educ 1986;20:162–75.10.1111/j.1365-2923.1986.tb01163.xSearch in Google Scholar PubMed
22. Saint DA, Horton D, Yool A, Elliott A. A progressive assessment strategy improves student learning and perceived course quality in undergraduate physiology. Adv Physiol Educ 2015;39:218–22.10.1152/advan.00004.2015Search in Google Scholar PubMed
©2016 Walter de Gruyter GmbH, Berlin/Boston
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Articles in the same Issue
- Frontmatter
- Editorial
- Wechsel in der Schriftleitung: Peter Schuff-Werner übernimmt die Schriftleitung bei der Zeitschrift LaboratoriumsMedizin
- Labormanagement/Laboratory Management / Redaktion: E. Wieland
- Chancen und Risiken von e-Health in der Labormedizin
- Infektiologie und Mikrobiologie (Schwerpunkt Bakteriologie)/ Infectiology and Microbiology (Focus Bacteriology) / Redaktion: P. Ahmad-Nejad/B. Ghebremedhin
- Normal and abnormal vaginal microbiota
- Pädiatrisches Labor/Pediatric Laboratory Medicine / Redaktion: K.P. Kohse
- Association of osteocalcin, insulin resistance and oxidative stress during noncomplicated pregnancy
- Originalarbeiten/Original Articles
- Flow cytometry as an important tool in the diagnosis of immunodeficiencies demonstrated in a patient with ataxia-telangiectasia
- Bias, its minimization or circumvention to simplify internal quality assurance
- Permissible measurement uncertainty in the lower part of measurement intervals
- Efficient use of laboratory resources: pre-screening for urine cultures by automated urinalysis and microscopy to allow exclusion of specimens from culture workflow
- Comparison of student perception and performance between case-based learning and lecture-based learning in a clinical laboratory immunology course
Articles in the same Issue
- Frontmatter
- Editorial
- Wechsel in der Schriftleitung: Peter Schuff-Werner übernimmt die Schriftleitung bei der Zeitschrift LaboratoriumsMedizin
- Labormanagement/Laboratory Management / Redaktion: E. Wieland
- Chancen und Risiken von e-Health in der Labormedizin
- Infektiologie und Mikrobiologie (Schwerpunkt Bakteriologie)/ Infectiology and Microbiology (Focus Bacteriology) / Redaktion: P. Ahmad-Nejad/B. Ghebremedhin
- Normal and abnormal vaginal microbiota
- Pädiatrisches Labor/Pediatric Laboratory Medicine / Redaktion: K.P. Kohse
- Association of osteocalcin, insulin resistance and oxidative stress during noncomplicated pregnancy
- Originalarbeiten/Original Articles
- Flow cytometry as an important tool in the diagnosis of immunodeficiencies demonstrated in a patient with ataxia-telangiectasia
- Bias, its minimization or circumvention to simplify internal quality assurance
- Permissible measurement uncertainty in the lower part of measurement intervals
- Efficient use of laboratory resources: pre-screening for urine cultures by automated urinalysis and microscopy to allow exclusion of specimens from culture workflow
- Comparison of student perception and performance between case-based learning and lecture-based learning in a clinical laboratory immunology course

