An international survey on the geographical differences in practice patterns and training of endoscopic ultrasound
-
Tobias Kleemann
Abstract
Background and Objectives
Recently, a series of publications discuss what kind of clinical and technical information is important to know before performing endoscopic ultrasound (EUS) examinations. This paper aims to investigate variations in the performance of EUS examinations in different countries worldwide to present views and experiences on the use of pre-EUS investigations.
Methods
In a multinational and multidisciplinary survey, more than 100 practicing EUS endoscopists were surveyed by a questionnaire asking for their level of education and training, their experience in diagnostic and therapeutic procedures, preferred technical use and procedural steps before EUS examination. Substantial geographic variation not only in the level of training and mandatory imaging prior to EUS, but consequently also in the standards and practice of EUS examinations and advanced EUS guided therapeutic procedures were observed. The participants’ preferences regarding technical use and procedural steps prior to EUS examinations were assessed according to their level of education and training experience.
Results
Transabdominal ultrasound (TUS) is performed prior to EUS by the EUS endoscopists themselves in most European countries but not in North and South Americas where non-invasive pre-EUS imaging is delegated to other specialties such as radiology. Different training backgrounds, cultural beliefs, infrastructures, available equipment and access to training programs have a strong impact on the EUS workforce and EUS procedural practice across the continents.
Conclusions
The study results suggest existence of relevant geographical differences that reflect not only the different levels of education in different settings but also differences regarding technical standards for the performance of EUS and TUS examinations worldwide.
Introduction
Endoscopic ultrasound (EUS) has been introduced more than forty years ago and is often referred to as the most advanced endoscopic procedure.[1] The role and practical use of EUS varies in different countries, scientific, and cultural contexts. We recently initiated and published a series of papers on how to perform endoscopic ultrasound and discussed “controversies in endoscopic ultrasound”.[2, 3, 4, 5, 6, 7] This series of papers inspired us to study the variation of current practices of EUS in different settings and cultures. Practicing EUS endoscopists and opinion leaders in EUS from various regions across the world were not only invited to answer a questionnaire but also to contribute to this review and to discuss their standards of practice with regards to currently available evidence and according to personal preferences.
The aim of this paper is to present and discuss survey data on the worldwide current practice of EUS, allowing readers to evaluate their own pre-EUS procedures and to stimulate further discussion.
Material and methods
EUS endoscopists from various regions across the world were invited to answer a survey. The questionnaire included epidemiological data about age, country of origin, specialty and research activity of each of the interviewed endoscopists. Furthermore, respondents’ educational level regarding transabdominal ultrasound (TUS) and EUS, their preferred imaging and interventional techniques, and standardized procedures before interventions were asked. The structure of the survey and the description of all participants is explained in detail below. To increase the response rate, EUS endoscopists were approached personally by e-mail. In some cases, various national gastroenterology societies were contacted by e-mail to get in touch with their members who could then participate in our survey.
Participants
Epidemiology: Epidemiological data that the respondents were asked included the following:
Name
Age
Gender
Country
Profession (surgeon, gastroenterologist)
Research activity (publications in TUS and EUS)
Education: Educational data that the respondents were asked included:
Level of education according to German, Austrian, and Swiss Societies for Ultrasound in Medicine (DEGUM, ÖGUM, SGUM) in TUS combined in the European Federation of Societies in Ultrasound in Medicine and Biology (EFSUMB) levels of education
Years performing TUS, EUS, endorectal ultrasound (ERUS), and/or endobronchial ultrasound (EBUS)
Imaging techniques used: The following questions were asked:
Frequency of TUS prior to EUS
Frequency of esophagogastroduodenoscopy (EGD) prior to EUS
TUS performed by respondents
Screen orientation of TUS and EUS
Use of radial and/or longitudinal EUS (%)
Use of ultrasound miniprobes
Use of EUS elastography (frequency)
Use of contrast enhanced endoscopic ultrasound (CE-EUS) (frequency)
Interventional techniques used: The participants were asked whether they apply the following interventional techniques:
EUS guided rendezvous via common bile duct (CBD) (transduodenal or transgastric)
EUS guided retrograde drainage of CBD into duodenum
EUS guided rendezvous via stomach (left liver lobe, LLL)
EUS guided antegrade bile duct drainage via left liver lobe
EUS guided pancreatic duct access
EUS guided cholecystostomy
EUS guided enteral access, anastomosis
EUS guided fiducial placement
EUS guided ablative therapy (ethanol, RFA)
Standardized procedures
The following questions were asked:
Requirement of coagulation tests before EUS guided sampling (%)
Stop antiplatelets prior to EUS guided sampling?
Antibiotic prophylaxis mandatory before EUS guided sampling?
Is there a difference regarding informed consent for EGD and diagnostic EUS?
Statistical analysis of the data
Continuous data were checked for normal distribution using Shapiro-Wilk test and are shown as mean (minimum value - maximum value), due to small sample size and/or lack of normal distribution. Differences between groups were compared by using Mann-Whitney U-test. All categorical data were assessed by Fisher's exact test and expressed as number (percentage). All analyses were carried out using SPSS-Statistics for Windows Version 24.0.0 (Armonk, NY, IBM Corp, USA). The map in figure 2 was created using Excel 2021 (Redmond, WA, Microsoft Corporation, USA).
Results
Epidemiologic data
Geographical area, age, gender, and clinical specialty: In total, around 250 endoscopists from around the world were asked to participate in our survey. About 165 EUS-performing endoscopists (153 gastroenterologists and 12 surgeons) replied resulting in a response rate of 67%. The age ranged between 31 and 67 years with an average age of 48.9 years. The majority of respondents were male (143 male, 22 female). The distribution of age, gender, and clinical specialty is shown in Table 1 according to geographical origin. Besides the mean values of age, the minimum and maximum values are shown as range in brackets.
Distribution of respondents according to geographical area, age and gender
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 165 | 5 | 67 | 79 | 11 | 3 |
| Age | ||||||
| Years (min-max) | 48.9 (31–67) | 46.4 (37–59) | 48.4 (32–67) | 49.7 (31–67) | 49.1 (35–62) | 43.3 (34–57) |
| Sex (%) | ||||||
| Male | 86.7 | 100.0 | 85.1 | 86.1 | 90.9 | 100.0 |
| Female | 13.3 | 0.0 | 14.9 | 13.9 | 9.1 | 0.0 |
| Specialty (%) | ||||||
| Gastroenterologist | 92.7 | 80.0 | 97.0 | 91.1 | 100.0 | 33.3 |
| Surgeon | 7.3 | 20.0 | 3.0 | 8.9 | 0.0 | 66.7 |
Country of origin: The majority of endoscopists (n = 79) came from Europe (47.9%) followed by 67 respondents from Asia (40.6%), 14 respondents from North and South America (8.5%) and 5 respondents from Africa (3.0%) (Figure 1). Within Europe, the majority of respondents came from Germany (35), followed by Italy (14), the United Kingdom (7), Spain (4), Poland (3), Switzerland (3), Denmark (3), Norway (2), Portugal (2), Greece (2), Croatia (1), France (1), Hungary (1) and Romania (1) (Figure 2).
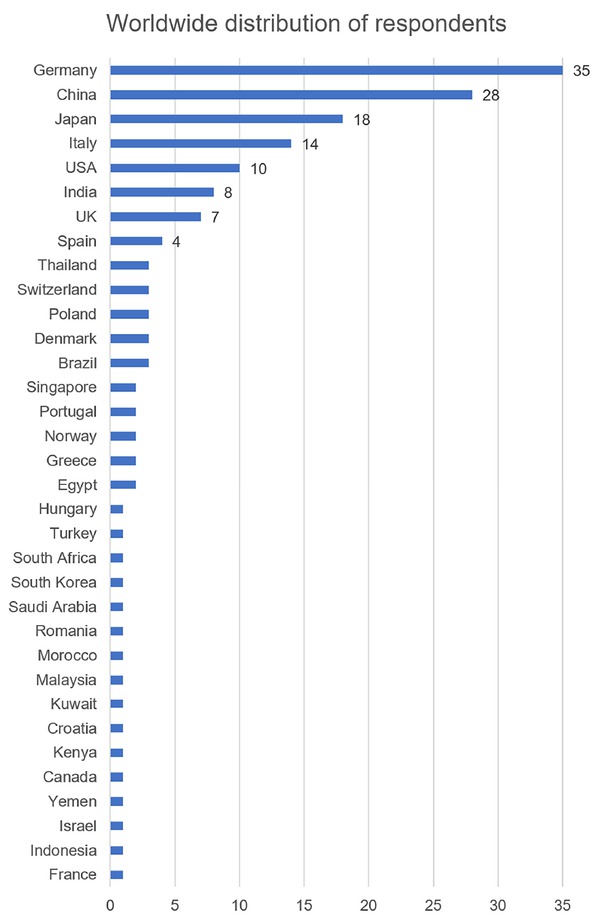
Worldwide distribution of respondents.
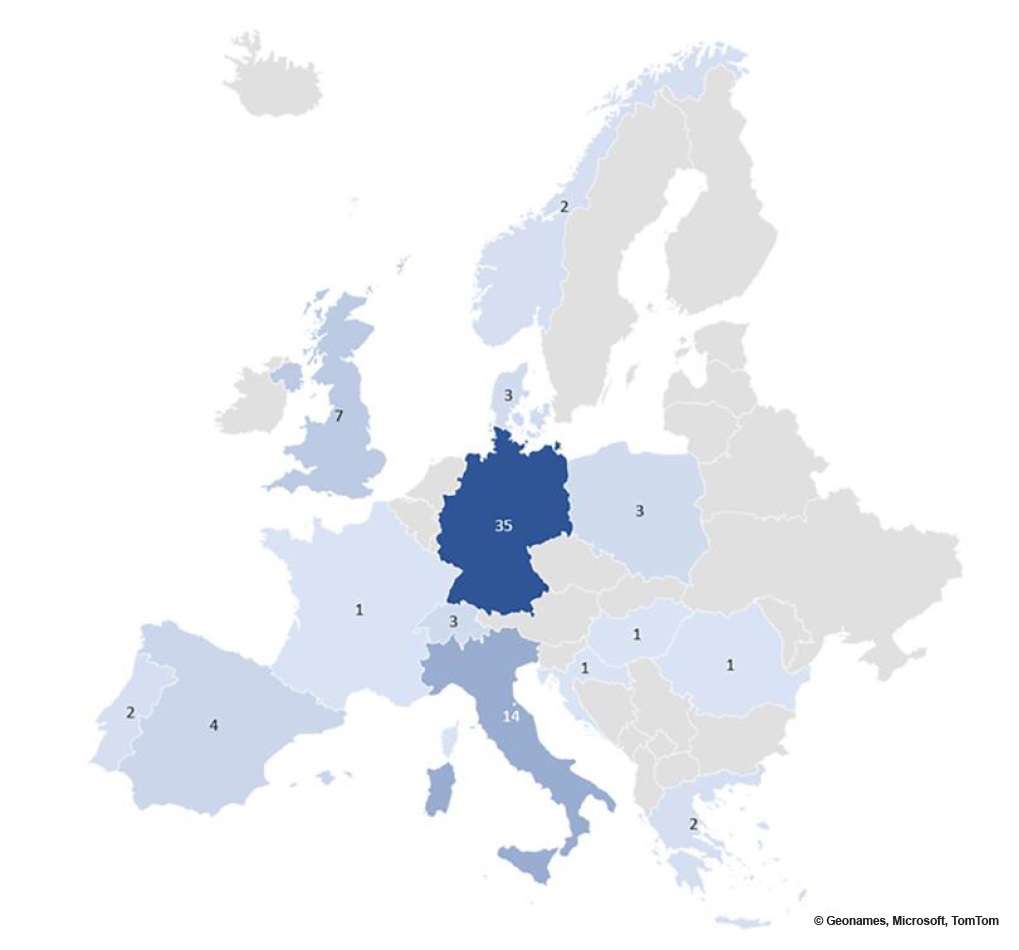
European distribution of respondents.
Research activity
We interviewed the respondents about their previous scientific work and asked about the respondent’s number of publications. The majority of respondents published ≤ 20 articles, the majority of these publications related to EUS compared with TUS. In addition, the majority of respondents who published TUS papers came from Europe followed by Asia, while respondents from Africa and North- and South America published ≤ 3 TUS papers. Respondents who published EUS papers were similarly distributed in percentage between Europe, Asia and North America, followed by South America. In contrast, respondents from Africa had published rarely (Figure 3 and Figure 4).
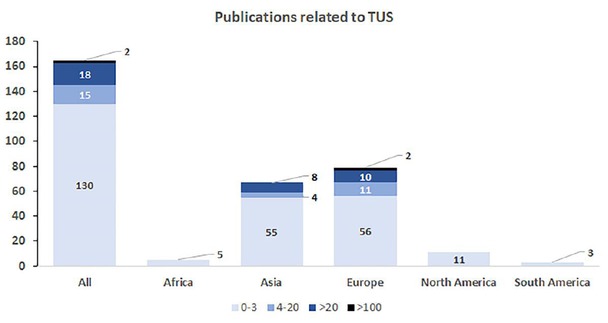
Number of publications in transabdominal ultrasound by respondents.
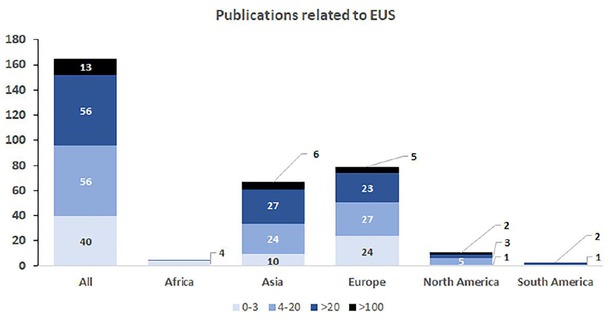
Number of publications in endoscopic ultrasound by respondents.
Education
Educational level in transabdominal ultrasound according to qualification: The majority of the EUS practicing specialists claimed to have advanced knowledge of TUS. However, most respondents had less than 5 years of practical experience with TUS. The majority of all participants (56.4%) responded to have been educated in TUS with an average experience of 11.6 years. The minimum and maximum years of experience are shown in brackets. It is important to mention that the majority of respondents trained in TUS are based in Europe (63 of 79 European respondents, 79.7%). They had an average experience in TUS of 15.3 years, followed by their colleagues in Asia (46.3%) with an average experience of 9.7 years. Respondents from Africa (40%), however, had an average experience of 9.2 years. Respondents from North and South American declared to have no educational experience in TUS (Table 2). Figure 5 shows the Level of Education that respondents stated according to the guidelines of the EFSUMB.[8]
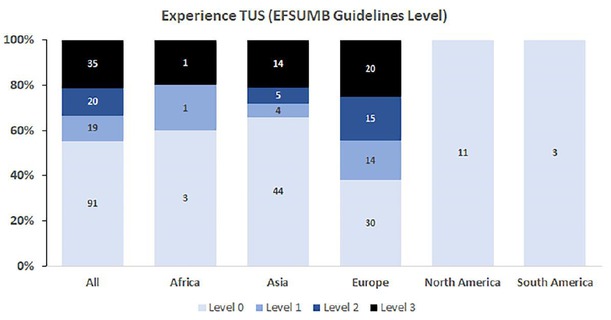
Experience in transabdominal ultrasound for all respondents according to the EFSUMB Guidelines Level 1–3.
Expertise of respondents in transabdominal ultrasound
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 165 | 5 | 67 | 79 | 11 | 3 |
| TUS | ||||||
| Educated in TUS | 56.4% | 40.0% | 46.3% | 79.7% | 0.0% | 0.0% |
| Experience in years (min-max) | 11.6 (0–37) | 9.2 (0–32) | 9.7 (0–35) | 15.3 (0–37) | 0.0 | 0.0 |
TUS: transabdominal ultrasound.
Performance of transabdominal ultrasound, endoscopic ultrasound, endorectal ultrasound and endobronchial ultrasound: Interestingly, the specialists’ experience in performing TUS correlates with their experience in performing EUS considering experience up to 10, 20 and 30 years. A narrow majority of the EUS examiners (55%) also perform TUS. Figure 6 shows the performance of TUS by the respondents. Geographically, mostly European EUS examiners perform TUS themselves as well, followed by African and Asian examiners. Interestingly, none of the respondents from North- and South America performed TUS.
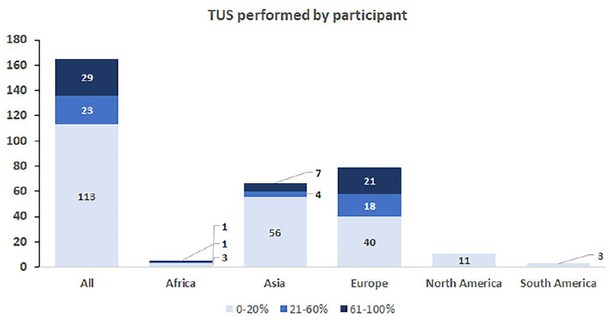
Overview of the performance of transabdominal ultrasound.
While the simultaneous performance of TUS for EUS endoscopists is quite common, the use of ERUS and EBUS ultrasound is less frequent. The questionnaire evaluated the performance of ERUS and EBUS including the time of performance in years. ERUS is used by a majority of the respondents (69.3%) within a mean timeframe of around 10.5 years of experience. EBUS is only used by a minority of the respondents (8.5%) with a mean timeframe of around 0.6 years of experience. While the use of ERUS is quite high in Europe (74%), Africa (80%) and Asia (59.7%), all participants in North America (100%) use ERUS whereas respondents in South America use ERUS only in 33.3%. The mean experience in ERUS was high in Europe (12.6 years) and North America (15.9 years) followed by Asia (7.8 years), Africa (6.4 years) and finally South America (3 years). Considering EBUS experience, it is worthwhile to note that EBUS is used by only a few EUS endoscopists. Participants from South America seem to have the most usage experience with a mean of 3.7 years followed by Europe with 1 year of mean EBUS usage experience. The overall mean EBUS usage experience of participants of the survey lies at about 0.6 years with the minimum and maximum values ranging from 0 to 13 years of experience (Table 3).
Use of endorectal ultrasound and endobronchial ultrasound by respondents
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 165 | 5 | 67 | 79 | 11 | 3 |
| Respondents performing ERUS (%) | 69.3 | 80.0 | 59.7 | 74.0 | 100.0 | 33.3 |
| ERUS experience in years (Range) | 10.5 (0–30) | 6.4 (0–20) | 7.8 (0–30) | 12.6 (0–30) | 15.9 (4–30) | 3.0 (0–9) |
| ERUS/EUS (%) (Range) | 7.2 (0–85) | 3.8 (0–10) | 5.7 (0–85) | 8.4 (0–50) | 10.5 (5–30) | 1.7 (0–5) |
| Respondents performing EBUS (%) | 8.5 | 0.0 | 1.5 | 15.2 | 0.0 | 33.3 |
| EBUS experience in years (Range) | 0.6 (0–13) | 0.0 | 0.1 (0-8) | 1.0 (0–13) | 0.0 | 3.7 (0–11) |
ERUS: endorectal ultrasound; EBUS: endobronchial ultrasound.
Imaging techniques
TUS prior to EUS: The questionnaire asked about the frequency of performing TUS prior to EUS. Figure 12 shows the geographical distribution of TUS performance prior to EUS. Around half of respondents (50.9%) perform TUS prior to EUS in more than 60% of examinations while a minority (40%) of colleagues is using TUS prior to EUS in less than 20% of examinations (Figure 7).
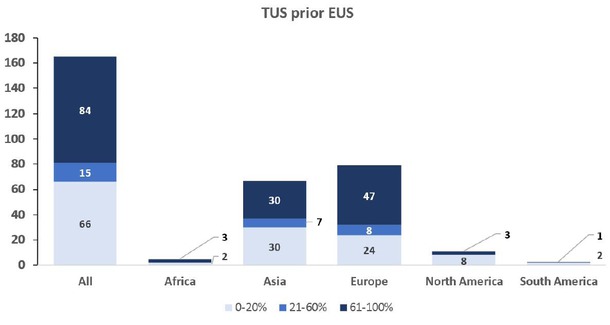
Frequency of performing transabdominal ultrasound prior to endoscopic ultrasound.
Frequency of esophagogastroduodenoscopy performed prior to endoscopic ultrasound. It is shown how often (percentage) esophagogastroduodenoscopy is performed prior to endoscopic ultrasound.
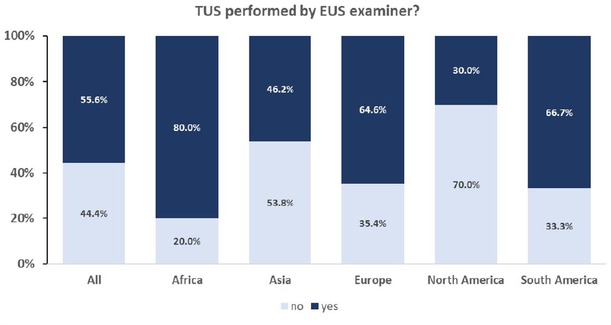
The figure shows respondent’s opinion about whether transabdominal ultrasound should be performed by the same examiner as endoscopic ultrasound.
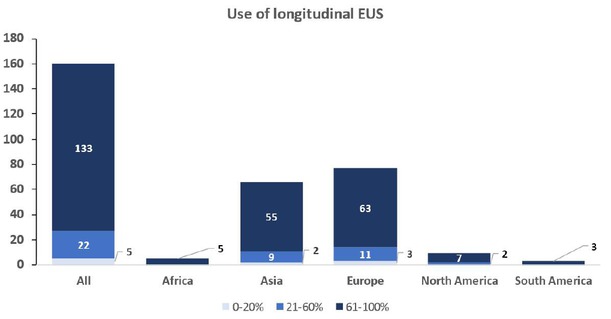
Overview of the use of longitudinal endoscopic ultrasound.
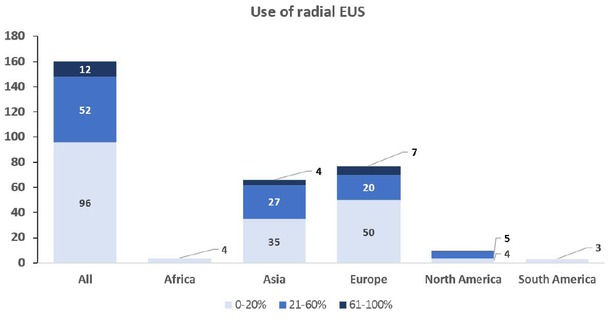
Overview of the use of radial endoscopic ultrasound.
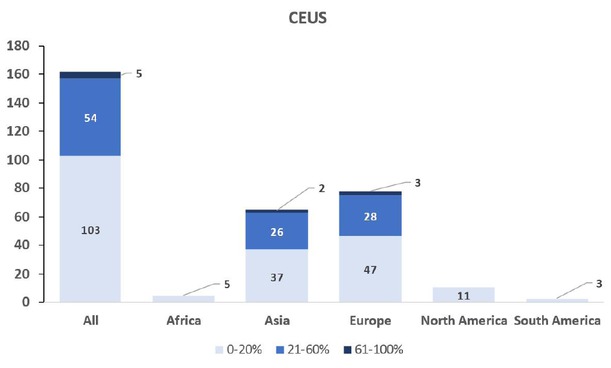
Frequency of use of contrast enhanced endoscopic ultrasound.
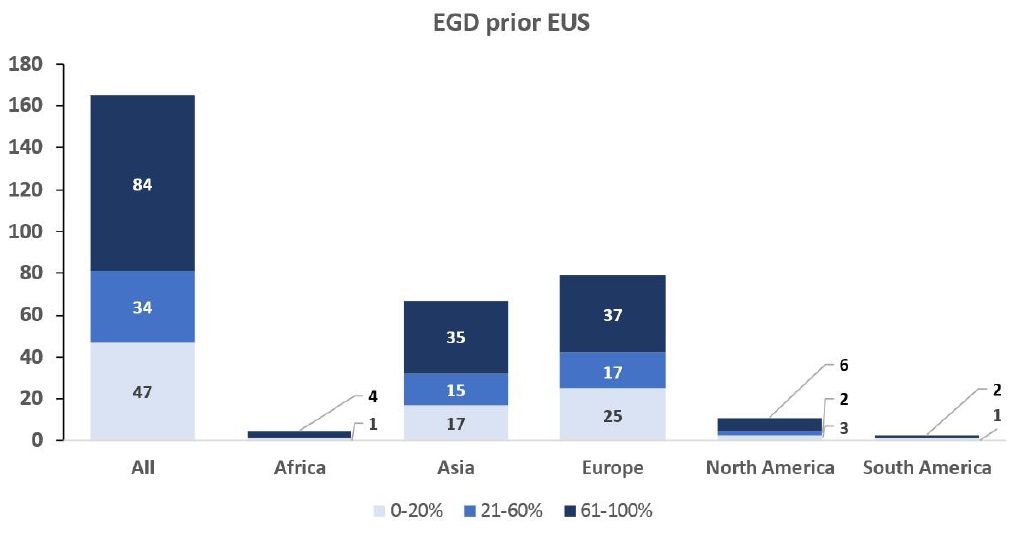
Esophagogastroduodenoscopy prior to endoscopic ultrasound: An EGD prior to EUS was performed by the majority (59.4%) of endosonographers who responded to this survey. Most African (80%) and most of the South American (70%) investigators include an EGD prior to EUS. European, Asian and North American respondents performed an EGD prior to EUS with a comparable frequency of 55.6%, 61.1 and 63.6% (Table 4).
Mean frequency of respondents performing esophagogastroduodenoscopy prior to endoscopic ultrasound
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 165 | 5 | 67 | 79 | 11 | 3 |
| Respondents performing EGD prior EUS (%) (range) | 59.4 (0–100) | 80.0 (0–100) | 61.1 (0–100) | 55.6 (0–100) | 63.6 (0–100) | 70.0 (10–100) |
EGD: esophagogastroduodenoscopy; EUS endoscopic ultrasound.
Figure 8 shows in detail that most of the respondents (n = 84) performed EGD prior to EUS in more than 60% of their EUS cases, while a subgroup performed EGD with a frequency of 20-60% of cases (n = 34). Only one fourth of the respondents (n = 47) used EGD prior to EUS in less than 20% of the cases.
Transabdominal ultrasound performance by same operator as endoscopic ultrasound: The majority of the interviewed specialists perform TUS personally. The survey could not clarify which medical professional performs TUS if this was not done by the EUS specialists themselves. Nevertheless, the majority of respondents stated that TUS should be performed by the same examiner as EUS. Most European examiners perform TUS by themselves, while American examiners do not perform TUS on their own, whereas African and Asian Examiners rarely perform TUS (Figure 6 and Figure 9).
Screen orientation of transabdominal ultrasound and endoscopic ultrasound: For TUS, the majority of respondents work with a left cranial orientation (76.5%), whereas for EUS, right cranial and left cranial screen orientation are preferred with nearly equal frequency (54.1% vs. 45.9%). The use of left cranial orientation in TUS is dominant in Asia (83.9%), Europe (78%) and Africa (75%), while respondents from North- and South America only use a right cranial orientation on TUS (100%). In EUS, the right cranial orientation dominates in North America (82.8%), South America (66.7%) and Africa (60.0%). The left cranial orientation dominates in Asia (60.9%) and in Europe (55.3%) (Table 5).
Screen orientations used for transabdominal ultrasound and endoscopic ultrasound
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 98 | 4 | 31 | 59 | 2 | 2 |
| TUS | ||||||
| Screen orientation (%) | ||||||
| Left cranial | 76.5 | 75.0 | 83.9 | 78.0 | 0.0 | 0.0 |
| Right cranial | 23.5 | 25.0 | 16.1 | 22.0 | 100.0 | 100.0 |
| Participants (n) | 159 | 5 | 64 | 76 | 11 | 3 |
| EUS | ||||||
| Screen orientation (%) | ||||||
| Left cranial | 54.1 | 40.0 | 60.9 | 55.3 | 18.2 | 33.3 |
| Right cranial | 45.9 | 60.0 | 39.1 | 44.7 | 82.8 | 66.7 |
EUS: endoscopic ultrasound; TUS: transabdominal ultrasound.
Use of radial and longitudinal EUS: Regarding the use of radial and longitudinal EUS, our study revealed that the majority of the interviewed specialists prefer to use longitudinal to radial EUS. Figures 11 and 12 show the frequency of use of radial and longitudinal EUS scanners, as specified by percentage of use and also by its geographical distribution.
Endoscopic ultrasound with miniprobes: Table 6 shows that 50.3% of respondents use miniprobes during endoscopic procedures. However, the geographical distribution shows that in Asia (84.8%) and North America (54.5%) most respondents use miniprobes, while respondents from Europe use them less frequently (25.6%). Respondents from Africa (0%) and South America (0%) do not use miniprobes at all which might be a cost issue as that requires additional cost to standard linear or radial EUS.
Endoscopic ultrasound with miniprobes
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 163 | 5 | 66 | 78 | 11 | 3 |
| Use of miniprobes (%) | 50.3 | 0.0 | 84.8 | 25.6 | 54.5 | 0.0 |
Use of endoscopic ultrasound elastography and contrast enhanced endoscopic ultrasound: EUS elastography was regularly used by more than two thirds of the respondents with wide variance between different respondents. Elastography is mostly used in Asia (76.5%), Europe (73.4%), and Africa (50%), while examiners in North America (22.2%) and South America (33.3%) use elastography less frequently. 78.7% of respondents affirmed the use of CE-EUS, whereby geographical distribution shows that only participants from Europe (92.4%) and Asia (83.3%) frequently use CE-EUS (Table 7 and Figures 12 and Figure 13).
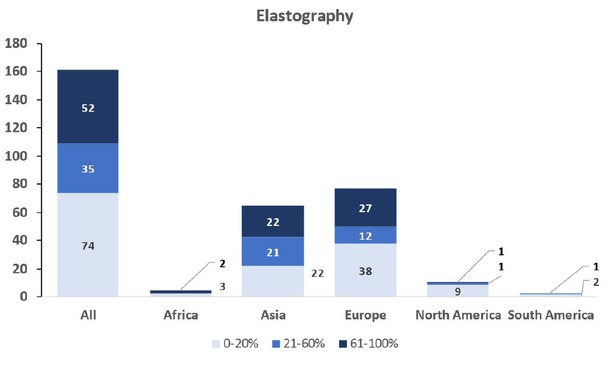
Frequency of endoscopic ultrasound elastography use.
Use of endoscopic ultrasound elastography and contrast enhanced endoscopic ultrasound
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 164 | 5 | 66 | 79 | 11 | 3 |
| Usage of CE-EUS (%) | 78.7 | 0.0 | 83.3 | 92.4 | 9.1 | 0.0 |
| Elastography (%) | 72.6 | 60.0 | 81.8 | 73.4 | 27.3 | 33.3 |
CE-EUS: contrast enhanced endoscopic ultrasound.
EUS guided interventional techniques
The questionnaire also evaluated the preferred access techniques for EUS guided biliary drainage procedures (Figure 14 and Figure 15).
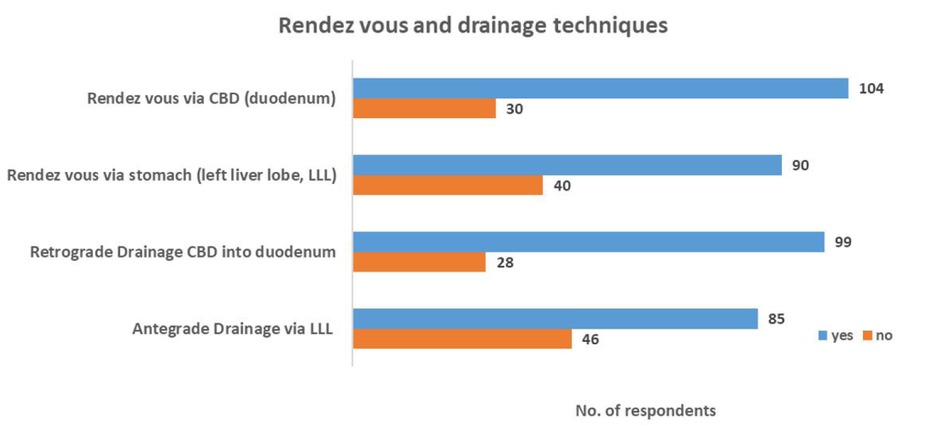
Use of endoscopic ultrasound guided biliary drainage techniques.
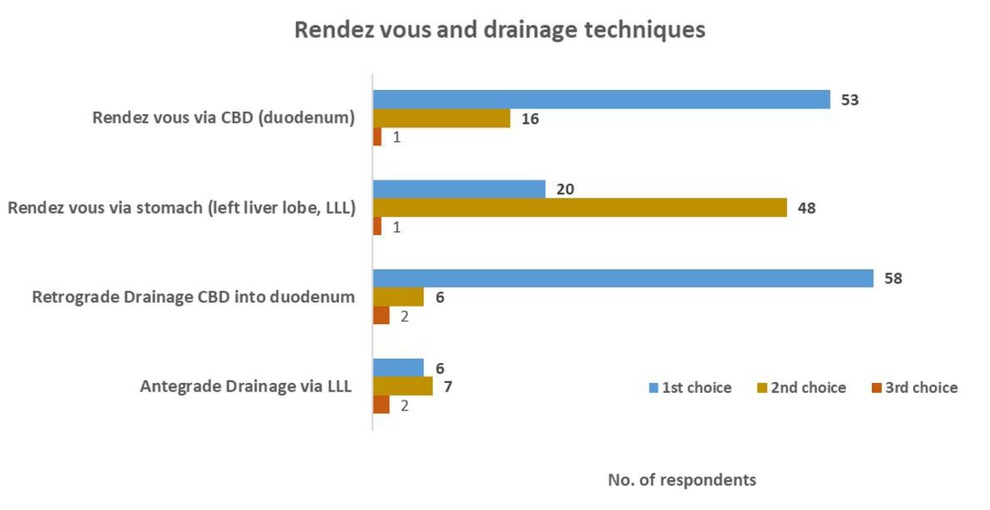
Use of different biliary drainage techniques according to 1st, 2nd, or 3rd choice.
Sixty-three percent of respondents (n = 104/165) practice EUS guided biliary drainage techniques. The rendez vous route via the CBD (duodenum) is the first choice of fifty-one percent (n = 53/104) of endosonographers who practice EUS guided biliary drainage as their preferred technique.
Retrograde drainage of CBD into the duodenum was identified as the second frequent technique used by sixty percent of respondents (n = 99), mostly mentioned as first choice (n = 58). Although the rendez vous technique via the stomach (left liver lobe, LLL) is mostly used as a second choice by the respondents (n = 48), this technique reached only the third place of all reviewed performance techniques used by respondents (n = 90). Antegrade drainage via the left liver lobe is only used by thirty-eight percent of respondents (n = 85) and mostly applied as second choice (n = 7).
Table 8 gives an overview on the usage of various EUS guided interventional techniques. Due to the low participation rate of North America, South America and Africa, the results are prone to selection bias. Out of all respondents, EUS guided pancreatic ductal access was mentioned to be the most frequently used EUS application followed by EUS-guided cholecystostomy. Special EUS-guided interventions like EUS-guided enteral access, EUS-guided placement of fiducial markers and EUS-guided ablative therapy are performed only by a minority of all respondents. Nevertheless, these interventions are frequently used in Asia and North America.
Percentage use of some emerging or not universally practiced endoscopic ultrasound guided interventional techniques
| All | Africa | Asia | Europe | North America | South America | |
|---|---|---|---|---|---|---|
| Participants (n) | 165 | 5 | 67 | 79 | 11 | 3 |
| EUS-applications (%) | ||||||
| EUS guided pancreatic ductal access | 46.7 | 20.0 | 61.2 | 36.7 | 54.5 | 0.0 |
| EUS guided cholecystostomy | 41.2 | 0.0 | 61.2 | 26.6 | 54.5 | 0.0 |
| EUS guided enteral access, anastomosis | 29.7 | 0.0 | 46.3 | 16.5 | 45.5 | 0.0 |
| EUS guided fiducial placement | 21.8 | 0.0 | 26.9 | 11.4 | 81.8 | 0.0 |
| EUS guided ablative therapy | 29.7 | 40.0 | 44.8 | 13.9 | 54.5 | 0.0 |
EUS: endoscopic ultrasound.
Standardized procedures
In the following part, we focus on peri-procedural protocols which have been asked for in the survey like e.g., mandatory coagulation tests before EUS guided interventions, the discontinuation of anti-platelets therapy, the prophylactic administration of antibiotics, and finally the use of miniprobes during EUS examinations.
Mandatory coagulation tests before endoscopic ultrasound guided sampling: Figure 16 shows that the majority of respondents check coagulation tests routinely before EUS-guided sampling.
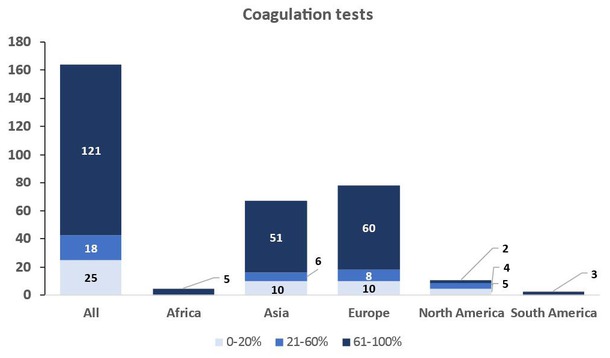
Frequency of performing coagulation tests prior to endoscopic ultrasound guided sampling.
Discontinuation of antiplatelet medications prior to endoscopic ultrasound guided sampling and other interventions: Another point of interest was the discontinuation of antiplatelet medications prior to EUS guided interventions. Figure 17 shows that 4.3% of respondents never stop antiplatelets, whereas 26.8% stop all antiplatelets including acetylsalicylic acid (ASA) and further 6.1% only stop non-ASA antiplatelet agents for any intervention. The majority of respondents decide whether to stop antiplatelet agents depending on the clinical indication for antiplatelet treatment (62.2%) and individual risk assessment (e.g., for stroke, coronary disease, stents etc.), or in case of a cystic lesion that is scheduled for biopsy (0.6%).
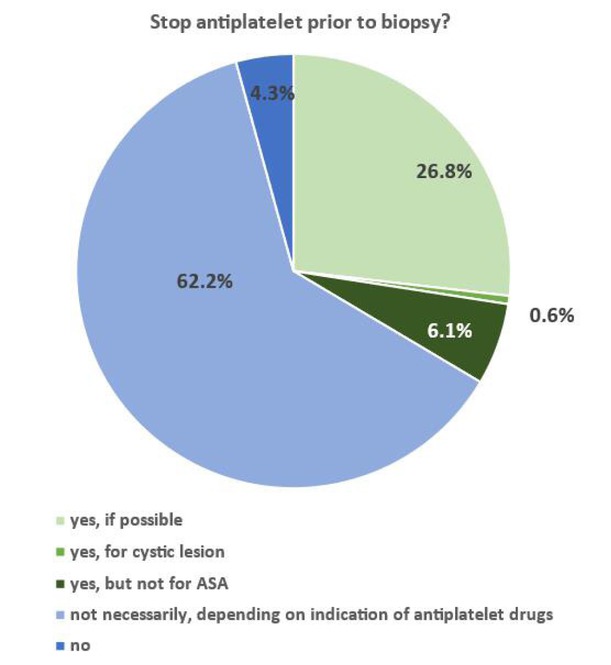
Discontinuation of antiplatelet therapy prior to endoscopic ultrasound guided sampling.
Antibiotic prophylaxis before endoscopic ultrasound guided sampling? Evaluating the respondents’ answers, antibiotic prophylaxis is considered necessary by the respondents prior to fine-needle puncture of cystic lesions, abscesses, pseudocysts and coeliac block maneuvers. Only 6 respondents (3.9%) always use antibiotic prophylaxis, whereas 18 respondents (11.0%) do not use any antibiotic prophylaxis prior to EUS guided interventions (Figure 19).
Should informed consent for endoscopic ultrasound differ from that for esophagogastroduodenoscopy? The question whether informed consent for diagnostic EUS should differ from that used for EGD was agreed by 91.4% of the respondents while only 8.6% of the respondents did not agree with this proposal.
Discussion
Our survey completed by EUS endoscopists from all continents reveals epidemiological and educational differences, but also differences in preparations which are deemed to be mandatory prior to EUS. Endoscopic techniques and echoendoscope preferences varied with the geographical location of the EUS endoscopists. These notable variations in EUS practice might be due to different education or working conditions around the world. In the discussion below we would like to discuss the worldwide differences and sociocultural influences that the survey could reveal.
Epidemiology
Out of 165 respondents of the survey, the majority came from Europe (n = 79) and Asia (n = 67). Due to the low number of respondents from North America (n = 11), Africa (n = 4) and South America (n = 3), results from these countries should be interpreted with great caution, while those from Europe and Asia are solid and reliable. Most of the respondents were gastroenterologists whereas in South America the majority were surgeons. With 86.7%, a large majority of respondents were males with a mean age of 48.9 years. No women from Africa or South America took part in our survey.
Our results suggest that, as reported for gastroenterology and surgery as a whole, in most countries endoscopic ultrasound as the “supreme discipline” of gastrointestinal endoscopy is still male-dominated. Physician Data Reports from the USA show a slow increase of female representation in gastroenterology workforce from 11% in 2007 to 19.7% in 2021. At the same time (2021), female representation over all specialties was 37.1% in the USA.[9] In 1997, in the USA women represented only 16% of gastrointestinal fellows.[10] Over a 10-year period from 2009-2019, female representation in GI fellowship positions increased to 33.6%.[11] Similar data are available from Europe. According to data from Healthcare-in-europe.com in 1996, for example, only about 12 percent of gastroenterologists in Germany were women. By 2011, that figure had risen to 22 percent. After training as gastroenterologist, the majority of the job spectrum of many gastroenterologists includes the performance of gastroscopies and colonoscopies.[12] The therapeutic EUS-guided interventions addressed in our survey require a far advanced training level and endoscopic skills that may not be reached in a few years. To become confident in EUS guided interventions, a long training phase and experience is needed. Therefore, women are underrepresented in advanced endoscopy including EUS. For example, in 2019 women represented only 14.0 % of all current advanced endoscopy fellows in the USA.[13] Barriers for women to achieve expertise in EUS and interventional endoscopy are also reported from Italy[14] and India.[15] These barriers include implicit gender bias, lack of flexibility in the training programs with regard to family planning and family obligations (e.g., part-time work options, maternity leave, hours and call), exposure to fluoroscopy during childbearing age, lack of ergonomic equipment, and lack of female program directors and educators.[11,16, 17, 18, 19, 20] Patriarchal structures in some regions and poor self-advocacy still appear to hinder women to enter advanced endoscopy training programs.[21] Ambitious young women may possibly become discouraged by prejudiced conservative male leaders who take their own way of thinking as a pretext to hinder women in their commitment.
Hence, the question of equal opportunities for women in terms of schooling, training and professional development in EUS and other advanced endoscopy techniques arises. In different regions of the world, the gap in education levels varies for men and women.
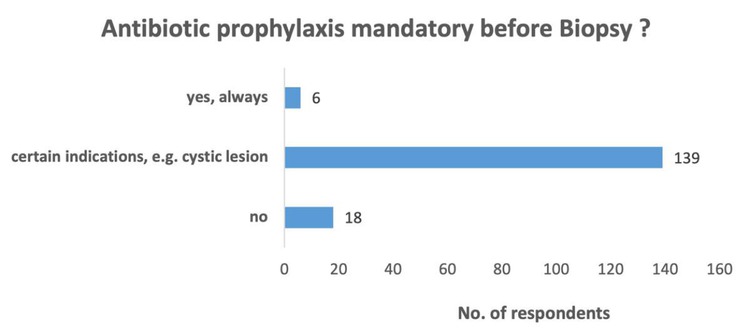
Antibiotic prophylaxis before endoscopic ultrasound guided sampling.
The recently created international organization called “Women In Endoscopy” (womeninendo.org) has the mission to champion the advancement of women through education, professional growth and leadership development. This global organization is a welcome move to address the inequities and challenges that women may uniquely face in their endoscopy careers.
Considering research activities, we found that the majority of respondents had published less than 20 articles, whereas more research work has been published about EUS issues than about TUS topics. Particularly in Africa, North- and South America, there have been no publications about TUS, which underlines the fact that in some societies, TUS is not part of the daily clinical workload of endoscopists. EUS, for example, is carried out by gastroenterologists in Anglo-American countries where TUS is most frequently performed by radiologists or physician assistants who have not been addressed in our survey. In Europe and Asia, many EUS examiners apply TUS themselves, which explains why clinical research work including TUS studies are more frequently published by gastroenterologists and surgeons. Publications of EUS papers were distributed similarly worldwide, although respondents from Africa published less than their colleagues abroad. Nevertheless, since the response rate in Africa was quite low (n = 4), these results cannot be generalized. On the other hand, research activities are mostly possible at University institutions due to less access to research facilities and requirements in rural hospitals, when compared to Europe, Asia and America.
Education
Educational level in transabdominal ultrasound according to qualification: Although the majority of EUS examiners reported to be educated in transabdominal ultrasound (TUS), the mean experience in performing TUS by the respondents has been 11.6 years. Furthermore, respondents from North- and South America mentioned no training in TUS. In the Americas, TUS is the domain of radiology and mainly performed by radiology technicians and radiologists. The relatively high proportion of TUS education in Europe is due to the fact that TUS is embedded in the training curricula for gastroenterologists in most European countries except the UK. The low educational level in TUS in Africa and Asia may be due to lower responder rates and the lack of TUS facilities. Nevertheless, it is quite obvious that European examiners have a high rate of TUS experience which could be measured by the years of performance in TUS. In contrast, the TUS performance rate in other countries was very low or zero. This might also underline that almost all European EUS examiners are educated and still practicing users of TUS while in other countries TUS or TUS might be done by other specialists like radiologists or radiology technicians/assistants.
While the simultaneous performance of TUS for EUS endoscopists is quite common, use of ERUS and EBUS ultrasound is less frequent. While ERUS is used by most of the respondents, EBUS is not used that much. One reason for the lower use of EBUS might be that respondents mostly had a clinical background in gastroenterology whereas EBUS is more used in the clinical background of pneumologists.
Imaging techniques used
Frequency of transabdominal ultrasound prior to endoscopic ultrasound (performed by respondents): When we considered the frequency of TUS performance prior to EUS, again the examiners from North and South America have mentioned that they do not perform TUS before the EUS. The reason might be again the delegation of TUS to other specialties like radiologists or physician assistants, radiographers. Patients are referred for endosonography through a variety of pathways. In the optimal case, the patient is under the care of the gastroenterologist who makes the management decisions such as the indications for various examinations, who performs the TUS and decides to perform EUS on the basis of his or her own results and available radiological findings. The majority of the respondents stated that TUS should be performed by the same examiner as EUS and we found that the slim majority of the interviewed specialists (55%) are performing TUS themselves, too. The reason of the quite high frequency of TUS prior to EUS in Europe might be the routine diagnostic pathway that the majority of patients start with a TUS as basic imaging followed by CT- and MRI- Scans and then EUS if abnormalities are detected, worthwhile to be investigated further. Due to the high acquisition costs, usually only hospitals have endosonography equipment and workstations. Patients are often referred by their general practitioners in the case of unclear complaints and findings or on the recommendation of radiologists to clarify unclear CT or MRI findings. Sometimes radiological imaging with other indications (cardio-MR, spine, kidney) reveals findings that are then directly referred to EUS for clarification. In some patients with complete imaging, one must occasionally have doubts about the image quality. The experienced examiner would perform a high quality TUS in such a situation. In daily practice, however, some outpatient examiners feel that their honor and qualifications have been violated and prefer instead to use all diagnostic possibilities to the full.
The clinical routine is usually so tense that it is not possible to repeat a sonography in this patient group, especially if the EUS workstation and high-end ultrasound are located in different rooms or even buildings. Geographical distribution discovered that mostly European examiners are using TUS while American examiners are not performing TUS themselves and African and Asian examiners only sometimes although Africa also has a quite high frequency of TUS prior to EUS which might be due to the availability of TUS next to the EUS examiners and possibly the difficult access to cross-sectional imaging methods. Nevertheless, the low rate of responders might distort the result here.
Frequency of esophagogastroduodenoscopy prior to endoscopic ultrasound: The survey revealed that the majority of the respondents are performing an EGD prior to EUS. Geographically almost all respondents in Africa and South America are following this approach, possibly because EGD might be an easy and fast method to detect unclear lesions that require further investigation with EUS. Alternatively, the EUS examiner might want to exclude strictures and pouches by EGD to avoid potential perforations with the stiffer, larger caliber and, in case of using longitudinal EUS, side viewing echoendoscope during EUS.
The observed difference might also reflect a variation in diagnostic workload in EUS practice whether mainly hepatobiliopancreatic indications, gastrointestinal tumour staging or assessment of subepithelial lesions is needed. In particular, if an EGD has already been carried out recently in advance by the same endoscopist, this does not have to be repeated. On the other hand if the EGD was performed by another physician who referred the patient to the EUS specialist, he or she may prefer to perform their own EGD first to confirm luminal findings especially in the case of luminal GI tumor staging and subepithelial lesions. Many experienced endoscopists ask the patient about dysphagia and perform an EGD only if patients have difficulty swallowing. Otherwise, especially for pancreatobiliary indications, many endosonographers may directly pass the EUS scope into the patient without an EGD. There certainly is a variability in practice based on indication of the procedure, whether prior EGD was done by the same physician and physician preference. The experienced endosonographer is probably more likely to see (or feel) resistance in the esophagus, recognize wall thickenings, diverticula, stenoses and angulations; which may be reason to abort the EUS and switch to an EGD procedure, if not done already. For the experienced physician, it is usually possible to safely advance an EUS device into the stomach and then pass the pylorus and bulb duodenal junction under endoscopic vision. However rare, perforations have been reported to occur in the pharynx or bulbo-duodenal junction during EUS. This is due to the stiff and slightly higher caliber distal end of the echoendoscope. There is a slightly increased risk of perforation in the area of angulations such as in the hypopharynx, but especially at the junction between the duodenal bulb and extra bulbar duodenum. This concerns the longitudinal probes with the additional limited endoscopic view due to the altered optical viewing axis. Extra care should be taken while navigating these regions.[22]
Screen orientation of transabdominal ultrasound and longitudinal endoscopic ultrasound: Looking at the preferred screen orientation of TUS and EUS, the majority of TUS examiners use a left cranial orientation (76.5%). Even in EUS, a left cranial orientation (54.9%) is dominating. Considering the geographical distribution, the use of TUS left cranial orientation is frequently seen in Asia (83.9%), Europe (78%) and Africa (75%) while colleagues from North- and South-America preferentially used a right cranial orientation for TUS (100%) and EUS (North America 82.8% and South America 66.7%). Furthermore, respondents from Europe (except from UK) are using more frequently a left cranial orientation in TUS (78%) and EUS (55.3%). The reason for this might be due to different TUS and EUS systems that have not been addressed by the survey and need further investigation. Standardization would be desirable. However, even experienced examiners work with the marking on the left in the TUS and on the right in the EUS. However, most commercially available ultrasound processors allow to switch the screen orientation and it is likely based on national conventions as well as how the endoscopists learned EUS initially.
Use of radial and longitudinal endoscopic ultrasound: The majority of the respondents prefer using longitudinal over radial EUS which is also seen after adjusting geographical distribution. The reason may be the fact of higher acquisition costs for purchasing both, radial and longitudinal equipment.[23,24] A radial equipment can only be used for diagnostic reasons but not for taking biopsies or therapeutic interventions. Therefore, some institutions may prefer to acquire only longitudinal endoscopes as they are more versatile allowing diagnostic staging but also interventions and histological investigations by taking biopsies. This is useful because the majority of EUS indications are related to oncological patients and therefore it is always favorable to have the option for performing EUS guided sampling. Furthermore, longitudinal echoendoscopes have a higher spatial resolution, which may be crucial e.g., for pancreatic indications where there is evidence that longitudinal echoendoscopes are able to detect even very small lesions. In addition, detection of submucosal invasion in early cancer may be another advantage of longitudinal EUS.[25, 26, 27, 28] However, it should be taken into account that it is not completely possible to rotate the longitudinal probe in the gastric antrum to the major position. The major antrum cannot be viewed satisfactorily with the longitudinal probe. It is much more comfortable to T-stage tumors in the stomach and esophagus with the radial probe. For staging of rectal cancer, the flexible radial probe can be used excellently. It is therefore advisable and even necessary to also have a radial probe available. Furthermore, a learning curve is necessary for each technique.[29, 30, 31] Hence, training of only longitudinal EUS would be a faster approach for the examiner in performing diagnostic and therapeutic endoscopic ultrasound, too.[31]
Use of miniprobes: Most respondents do not regularly use miniprobes.[32] The use of balloon miniprobes in the bronchial system has been mostly replaced by EBUS. Earlier expectations placed on the mini-probes in the staging of early gastro-intestinal carcinomas have not been fulfilled. Regarding the biliary system, many clinical questions are answered by EUS, MRCP and modular cholangioscopy with the option to biopsy.[33, 34, 35] Nevertheless, in Asia and North America the majority of respondents are using miniprobes, although the delicate and fragile miniprobe systems may be too expensive and add only limited diagnostic benefit when compared to normal EUS staging. Because of these limitations, respondents from Europe may rarely use miniprobes and respondents from Africa and South America may never use them.
Use of endoscopic ultrasound elastography and contrast enhanced endoscopic ultrasound: We found that EUS elastography and CE-EUS were used by a majority of respondents (72.6% and 78.7%, respectively), although a geographical disparity is evident for both modalities. EUS elastography is used by the majority of respondents in Asia (81.8%), Europe (73.4%), and Africa (60%), but to a lesser extent in North America (27.3%) and South America (33.3%). The differences in utilization are even more pronounced for CE-EUS with only participants from Europe (92.4%) and Asia (83.3%) frequently using CE-EUS. Both techniques are considered advanced multiparametric ultrasound technologies, in particular CE-EUS was primarily developed for TUS. It is therefore not surprising that the geographical differences in the frequency of use of EUS elastography and CE-EUS coincide with those of TUS in general and the fact that TUS is frequently performed by radiologists or sonographers in North- and South America. One additional reason for non-using CE-EUS may be the high price of the ultrasound contrast agent and, for some regions, no availability of any ultrasound contrast agent before 2016.
Provision and performance of endoscopic ultrasound techniques
Interventional techniques used: The questionnaire evaluated the preferred use of different access techniques of endoscopic ultrasound for biliary drainage procedures. Due to a quite high respondents’ rate, the results seem to be reliable. Assuming a high expertise in ERCP in all respondents it seems understandable that the majority of respondents prefer “rendez vous techniques” via the CBD (duodenum), or retrograde drainage of the CBD into duodenum. This may be due to the normal endoscopic technique similar to ERCP where the switch to ERCP technique allows to insert the stent into the CBD; this may be the fastest and easiest way for biliary drainage when access to the CBD had been achieved. Rendez vous via the stomach (left liver lobe) and antegrade drainage via the left liver lobe have not been the first choice for drainage of the biliary system. Possible reasons include be the above-mentioned easier access methods to the CBD via duodenum due to similar investigation method compared with ERCP, and/or published higher serious adverse event rates for the hepatic access route.[36, 37, 38, 39]
In detail, we asked for less common EUS guided applications such as EUS guided pancreatic ductal access, EUS guided cholecystostomy, EUS guided enteral access, EUS guided fiducial marker placement and EUS guided ablative therapy. Respondents from North America practice these techniques most frequently, but due to the low number no comparison can be made. Acknowledging that high expertise in EUS and interventional endoscopy is needed to perform these interventions, lack of available expertise may lead to transfer these patients for alternative interventions to radiologists (e.g., CT guided cholecystostomy or ablative therapy, duodenal stenting) or to surgeons (e.g., gastroenterostomy). Due to the low response rate from Africa, the results are not generalizable to the whole continent.
Standardized procedures
In our survey we focused on procedural protocols such as the requirement of coagulation tests before EUS guided interventions, discontinuation of anti-coagulation therapy, prophylaxis with antibiotics and finally the use of miniprobes during EUS examinations. The majority of respondents declared to stop antiplatelets prior to EUS guided sampling which most frequently depended on the clinical indication of the endoscopic intervention and the individual antiplatelet agent used. We assume that some respondents base their decision on International or National guidelines whereas others rely on their clinical experience and consensus decisions together with other clinical specialties.[40, 41, 42, 43, 44, 45] Guidelines classify EUS guided sampling and other interventions as high risk procedure of bleeding and thus recommend to stop non-ASA antiplatelets, when possible.[46, 47, 48] In addition, the Guideline of the European Society for Gastrointestinal Endoscopy (ESGE) on EUS guided sampling suggests: “The need for bridging therapy with low molecular weight heparin or switching to acetylsalicylic acid should be determined on the basis of the underlying indication for antithrombotic therapy and the risk for thromboembolic events. EUS-guided sampling can be performed in patients on low dose acetylsalicylic acid therapy”.[49] Hence, further investigation is needed to clarify the reasons for respondents’ decision to stop or continue anticoagulation when biopsies are taken.
Considering antibiotic prophylaxis prior to EUS-guided fine-needle sampling, 139 respondents (85%) mentioned to follow guidelines, especially prior to fine-needle puncture of cystic lesions, abscesses, pseudocysts and coeliac block maneuvers, which is in keeping with earlier clinical guidelines. Recent studies suggest that antibiotic prophylaxis may not be necessary, not even prior to EUS guided fine-needle aspiration (FNA) of pancreatic cysts.[50,51] However, due to the lack of definitive studies on this topic, EFSUMB, ESGE and the American Society for Gastrointestinal Endoscopy (ASGE) currently recommend antibiotic prophylaxis.[46,47,49,52,53] In a multicenter study by Colán-Hernández et al of patients undergoing EUS guided FNA for pancreatic cyst examination, the risk of infection was low. The incidence of infection did not differ significantly with or without ciprofloxacin prophylaxis. The only case of FNA-related infection (0.44%) occurred in a patient in the placebo group (0.87%).[51] Facciorusso’s meta-analysis also assessed that prophylactic antibiotics do not significantly reduce the risk of infection after EUS guided FNA of pancreatic cystic lesions, and the routine use of prophylactic antibiotics should therefore be questioned.[50,54] In contrast, Troncone et al are critical of generally not using antibiotic prophylaxis under special circumstances. In particular, there is a higher risk when using the 19 G needle on cystic pancreatic lesions for through-the-needle micro forceps biopsy (EUS-TTNB) and needle-based confocal laser endomicroscopy (EUS-nCLE). Further definitive studies are needed.[55]
Is there a difference in informed consent for esophagogastroduodenoscopy and diagnostic endoscopic ultrasound?
The majority of respondents agreed that the content of informed consent to EGD and diagnostic EUS should be different. Since complication rates of EUS are reported to be higher than for diagnostic EGD, the consenting process for both investigations should be specified in a different manner and form.[56]
Limitations
Response bias is a significant concern in survey research as it can influence the reliability and generalizability of the findings. In this study, lower response rates from regions such as North America and Africa have been identified, which could skew the results and limit the applicability of the conclusions. It is crucial to acknowledge this limitation to provide transparency and context for the interpretation of the results. To clarify the limitations in our study, we have listed the results overall [all] and divided by continent separately by identifying the participants [n] in the tables shown above. These can be derived directly from the graphics. To improve the quality and impact of future studies, broader participation should be encouraged across all regions by implementing targeted outreach efforts like e.g., incentives for participation such as access to study findings, professional development opportunities or even monetary rewards. Furthermore, enhanced communication like engagement with professional societies, regional conferences and local experts could improve participation in underrepresented regions like Africa and South America. Finally, language and cultural adaptations may help addressing response bias by ensuring that the survey is available in multiple languages and culturally adapted. A further limitation of this survey study relates to causal explanations for different approaches, preferences and frequencies of use. In the discussion, we have tried to explain these differences indirectly and using published data. On this basis, further surveys should attempt to use specific questions to identify historical and health economic causes and causes associated with different organizational forms of healthcare systems.
Conclusion
Our study results suggest existence of relevant geographical differences that reflect not only the different levels of education in different settings but also differences regarding technical standards for the performance of EUS and TUS examinations worldwide.
TUS is performed prior to EUS by the EUS endoscopists themselves in most European countries but not in North and South Americas where non-invasive pre-EUS imaging is delegated to other specialties such as radiology. Different training backgrounds, cultural beliefs, infrastructures, available equipment and access to training programs have a strong impact on the EUS workforce and EUS procedural practice across the continents. Global standardization of EUS training and EUS procedural protocols will facilitate international recognition of qualifications, improve safety of the interventions and enable international multi-center research activity to produce the evidence we need to advance EUS practice further.
The shortfall of this study was the low response rate from countries outside Europe and Asia. Therefore, large-scale generalizations across the globe may not be accurate. However, this study does provide a “snap shot” of EUS practice patterns across Europe and Asia as well as how it may differ from practices in other parts of the world. To enhance the validity and credibility, future research to understand the global landscape of EUS practice patterns and training differences among gastroenterologists should seek to achieve greater representativeness through targeted network utilization and outreach efforts, and better capture causalities through specific questions.
Funding statement: None.
Acknowledgements
None.
-
Author Contributions
CFD: Conceptualization; TK, RF and CFD: Writing—Original draft preparation; All authors: Writing—Reviewing and Editing; CFD, TK: Conceptualization, Supervision; CFD and TK: Supervision, Project administration.
-
Ethical Approval
Not applicable.
-
Informed Consent
Not applicable.
-
Conflict of Interest
None declared.
-
Use of Large Language Models, AI and Machine Learning Tools
None declared.
-
Data Availability Statement
No additional data is available.
References
1 Dietrich CF. Endosonography as theme of this issue--update of endoscopic ultrasound techniques. Z Gastroenterol 2008;46:553-554.10.1055/s-2008-1027506Suche in Google Scholar PubMed
2 Dietrich CF, Lucius C, Nielsen MB, Burmester E, Westerway SC, Chu CY, et al. The ultrasound use of simulators, current view, and perspectives: Requirements and technical aspects (WFUMB state of the art paper). Endosc Ultrasound 2023;12:38-49.10.4103/EUS-D-22-00197Suche in Google Scholar PubMed PubMed Central
3 Dietrich CF, Arcidiacono PG, Braden B, Burmeister S, Carrara S, Cui X, et al. What should be known prior to performing EUS exams? (Part II). Endosc Ultrasound 2019;8:360-369.10.4103/eus.eus_57_19Suche in Google Scholar PubMed PubMed Central
4 Braden B, Hocke M, Selvaraj E, Kaushal K, Möller K, Ignee A, et al. Mishaps with EUS-guided lumen-apposing metal stents in therapeutic pancreatic EUS: Management and prevention. Endosc Ultrasound 2023;12:393-401.10.1097/eus.0000000000000018Suche in Google Scholar PubMed PubMed Central
5 Möller K, Braden B, Jenssen C, Ignee A, Cui XW, Yamashita Y, et al. Intraductal papillary neoplasms of the bile ducts-what can be seen with ultrasound? Endosc Ultrasound 2023;12:445-455.10.1097/eus.0000000000000040Suche in Google Scholar PubMed PubMed Central
6 Lucius C, Nielsen MB, Blaivas M, Burmester E, Westerway SC, Chu CY, et al. The use of simulation in medical ultrasound: Current perspectives on applications and practical implementation (WFUMB state-of-the-art paper). Endosc Ultrasound 2023;12:311-318.10.1097/eus.0000000000000022Suche in Google Scholar PubMed PubMed Central
7 Saftoiu A, Napoleon B, Arcidiacono PG, Braden B, Burmeister S, Car-rara S, et al. Do we need contrast agents for EUS? Endosc Ultrasound 2020;9:361-368.10.4103/eus.eus_20_20Suche in Google Scholar PubMed PubMed Central
8 Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, et al. EFSUMB recommendations and guidelines for gastrointestinal ultrasound. Ultraschall Med 2017;38:273-284.10.1055/s-0042-115410Suche in Google Scholar PubMed
9 Association of American Medical Colleges. 2020 Physicians specialty data report. Washington, DC, January 2021. Available at: http://resource.nlm.nih.gov/101778485. Accessed on 2024-02-15.Suche in Google Scholar
10 Hecht G. Women in gastroenterology: exciting times and trends. Gas-troenterology 2008;134:913-914.10.1053/j.gastro.2008.01.026Suche in Google Scholar PubMed
11 Starkey M, Daboul J, Lang J, Hart B, Ekwenna O. Trends in female representation in gastroenterology fellowships in the United States. Ann Gastroenterol 2022;35:577-583.10.20524/aog.2022.0747Suche in Google Scholar PubMed PubMed Central
12 Koo P, Yung V, Dutta A, Sarkar S. Choosing a Career in Advanced Endoscopy or General Gastroenterology. Dig Dis Sci 2017;62:1409-1411.10.1007/s10620-017-4575-1Suche in Google Scholar PubMed
13 Yu JX, Berzin TM, Enestvedt B, Anderson MA, Popov VB, Thompson CC, Schulman AR. Gender disparities in advanced endoscopy fellowship. Endosc Int Open 2021;9:E338-E342.10.1055/a-1311-0899Suche in Google Scholar PubMed PubMed Central
14 Venezia L, Labarile N, Maselli R, Benedetti A, Annibale B, Parodi MC, et al. Women in Gastroenterology: What Is the Current Situation? Results of an Italian National Survey. Dig Dis Sci 2024;69:1990-1995.10.1007/s10620-024-08407-8Suche in Google Scholar PubMed PubMed Central
15 Gahra AK, Mathur S, Banerjee R, Patil P, Van Hooft JE, Kamani L, et al. Challenges in the uptake of advanced endoscopy among women gastroenterologists: A survey. Indian J Gastroenterol 2024 May 20. Epub ahead of print.10.1007/s12664-024-01599-xSuche in Google Scholar PubMed
16 Fritze-Buttner F, Schlosser K, Prediger S. Zentralbl Chir 2019;144:329332.10.1055/a-0758-1999Suche in Google Scholar PubMed
17 Fritze-Buttner F, Toth B, Buhren A, Schlosser K, Schierholz S, Rumpel B, et al. Surgery during pregnancy - results of a German questionnaire. Innov Surg Sci 2020;5:21-26.10.1515/iss-2020-0025Suche in Google Scholar PubMed PubMed Central
18 Siddiqui UD, van Hooft JE, Sethi A. Gender disparities in advanced endoscopy fellowship: Women in Endoscopy (WIE) perspective. Endosc Int Open 2021;9:E505-E506.10.1055/a-1339-1432Suche in Google Scholar PubMed PubMed Central
19 Rabinowitz LG, Grinspan LT, Williams KE, Zylberberg HM, David Y, Kumta NA, et al. Gender dynamics in education and practice of gastro-enterology. Gastrointest Endosc 2021;93:1047-1056 e1045.10.1016/j.gie.2020.08.022Suche in Google Scholar PubMed
20 Rabinowitz LG, Grinspan LT, Zylberberg HM, Dixon R, David YN, Aroniadis OC, et al. Survey Finds Gender Disparities Impact Both Women Mentors and Mentees in Gastroenterology. Am J Gastroenterol 2021;116:1876-1884.10.14309/ajg.0000000000001341Suche in Google Scholar PubMed
21 Rembacken BJ, Dixon S, Albuquerque A, Fairbrass K, Pana M. Barriers and bias standing in the way of female trainees wanting to learn advanced endoscopy. United European Gastroenterol J 2019;7:1141-1145.10.1177/2050640619877603Suche in Google Scholar PubMed PubMed Central
22 Mizuide M, Ryozawa S, Fujita A, Ogawa T, Katsuda H, Suzuki M, et al. Complications of endoscopic ultrasound-guided fine needle aspiration: a narrative review. Diagnostics (Basel) 2020;10.10.3390/diagnostics10110964Suche in Google Scholar PubMed PubMed Central
23 Committee AT, Murad FM, Komanduri S, Abu Dayyeh BK, Chauhan SS, Enestvedt BK, Fujii-Lau LL, et al. Echoendoscopes. Gastrointest Endosc 2015;82:189-202.10.1016/j.gie.2015.02.017Suche in Google Scholar PubMed
24 Faigel DO. Economic realities of EUS in an academic practice. Gastro-intest Endosc 2007;65:287-289.10.1016/j.gie.2006.06.045Suche in Google Scholar PubMed
25 Kaneko M, Katanuma A, Maguchi H, Takahashi K, Osanai M, Yane K, et al. Prospective, randomized, comparative study of delineation capability of radial scanning and curved linear array endoscopic ultrasound for the pancreaticobiliary region. Endosc Int Open 2014;2:E160-E170.10.1055/s-0034-1377384Suche in Google Scholar PubMed PubMed Central
26 Lan Z, Hu H, Mandip R, Zhu W, Guo W, Wen J, et al. Linear-array endoscopic ultrasound improves the accuracy of preoperative submucosal invasion prediction in suspected early gastric cancer compared with radial endoscopic ultrasound: A prospective cohort study. J Gastroenterol Hepatol 2020;35:118-123.10.1111/jgh.14819Suche in Google Scholar PubMed
27 Lan Z, Sun K, Luo Y, Hu H, Zhu W, Guo W, et al. Linear-array EUS improves the accuracy of predicting deep submucosal invasion in non-pedunculated rectal polyps compared with radial EUS: a prospective observational study. Surg Endosc 2021;35:1734-1740.10.1007/s00464-020-07566-9Suche in Google Scholar PubMed
28 Shin EJ, Topazian M, Goggins MG, Syngal S, Saltzman JR, Lee JH, et al. Linear-array EUS improves detection of pancreatic lesions in high-risk individuals: a randomized tandem study. Gastrointest Endosc 2015;82:812-818.10.1016/j.gie.2015.02.028Suche in Google Scholar PubMed PubMed Central
29 Wani S, Keswani R, Hall M, Han S, Ali MA, Brauer B, et al. A prospective multicenter study evaluating learning curves and competence in endoscopic ultrasound and endoscopic retrograde cholangiopancreatography among advanced endoscopy trainees: the rapid assessment of trainee endoscopy skills study. Clin Gastroenterol Hepatol 2017;15:1758-1767 e1711.Suche in Google Scholar
30 Hedenstrom P, Sadik R. The assessment of endosonographers in training. World J Clin Cases 2018;6:735-744.10.12998/wjcc.v6.i14.735Suche in Google Scholar PubMed PubMed Central
31 Xu W, Liu Y, Pan P, Guo Y, Wu RP, Yao YZ. Prior radial-scanning endoscopic ultrasonography training did not contribute to subsequent linear-array endoscopic ultrasonography study performance in the stomach of a porcine model. Gut Liver 2015;9:353-357.10.5009/gnl13419Suche in Google Scholar PubMed PubMed Central
32 Seifert H, Fusaroli P, Arcidiacono PG, Braden B, Herth F, Hocke M, et al. Controversies in EUS: Do we need miniprobes? Endosc Ultrasound 2021;10:246-269.10.4103/EUS-D-20-00252Suche in Google Scholar PubMed PubMed Central
33 Tringali A, Lemmers A, Meves V, Terheggen G, Pohl J, Manfredi G, et al. Intraductal biliopancreatic imaging: European Society of Gastrointestinal Endoscopy (ESGE) technology review. Endoscopy 2015;47:739-753.10.1055/s-0034-1392584Suche in Google Scholar PubMed
34 Navaneethan U, Moon JH, Itoi T. Biliary interventions using single-operator cholangioscopy. Dig Endosc 2019;31:517-526.10.1111/den.13361Suche in Google Scholar PubMed
35 Pereira P, Peixoto A, Andrade P, Macedo G. Peroral cholangiopancrea-toscopy with the SpyGlass(R) system: what do we know 10 years later. J Gastrointestin Liver Dis 2017;26:165-170.10.15403/jgld.2014.1121.262.choSuche in Google Scholar PubMed
36 Khan MA, Akbar A, Baron TH, Khan S, Kocak M, Alastal Y, et al. Endoscopic Ultrasound-guided biliary drainage: a systematic review and meta-analysis. Dig Dis Sci 2016;61:684-703.10.1007/s10620-015-3933-0Suche in Google Scholar PubMed
37 Li J, Tang J, Liu F, Fang J. Comparison of Choledochoduodenostomy and Hepaticogastrostomy for EUS-Guided Biliary Drainage: A Meta-Analysis. Front Surg 2022;9:811005.10.3389/fsurg.2022.811005Suche in Google Scholar PubMed PubMed Central
38 Dietrich CF, Bekkali NL, Burmeister S, Dong Y, Everett SM, Hocke M, et al. Controversies in ERCP: Indications and preparation. Endosc Ultrasound 2022;11:186-200.10.4103/EUS-D-21-00106Suche in Google Scholar PubMed PubMed Central
39 Dietrich CF, Bekkali NL, Burmeister S, Dong Y, Everett SM, Hocke M, et al. Controversies in ERCP: Technical aspects. Endosc Ultrasound 2022;11:27-37.10.4103/EUS-D-21-00102Suche in Google Scholar PubMed PubMed Central
40 Gil HI, Ko RE, Lee K, Um SW, Kim H, Jeong BH. Effects of antithrom-botic treatment on bleeding complications of EBUS-TBNA. Medicina (Kaunas) 2021;57.10.3390/medicina57020142Suche in Google Scholar PubMed PubMed Central
41 Inoue T, Okumura F, Sano H, Kobayashi Y, Ishii N, Suzuki Y, et al. Bleeding risk of endoscopic ultrasound-guided fine-needle aspiration in patients undergoing antithrombotic therapy. Dig Endosc 2017;29:91-96.10.1111/den.12687Suche in Google Scholar PubMed
42 Kawakubo K, Yane K, Eto K, Ishiwatari H, Ehira N, Haba S, et al. A prospective multicenter study evaluating bleeding risk after endoscopic ultrasound-guided fine needle aspiration in patients prescribed an-tithrombotic agents. Gut Liver 2018.10.5009/gnl17293Suche in Google Scholar PubMed PubMed Central
43 Sejpal DV, Trindade AJ, Lee C, Miller LS, Benias PC, Inamdar S, et al. Digital cholangioscopy can detect residual biliary stones missed by occlusion cholangiogram in ERCP: a prospective tandem study. Endoscopy international open 2019;7:E608-E614.10.1055/a-0842-6450Suche in Google Scholar PubMed PubMed Central
44 Polmanee P, Hara K, Mizuno N, Hijioka S, Kuwahara T, Okuno N, et al. Outcomes of EUS-FNA in patients receiving antithrombotic therapy. Endosc Int Open 2019;7:E15-E25.10.1055/a-0735-9107Suche in Google Scholar PubMed PubMed Central
45 Hamada T, Yasunaga H, Nakai Y, Isayama H, Horiguchi H, Matsuda S, et al. Severe bleeding and perforation are rare complications of endoscopic ultrasound-guided fine needle aspiration for pancreatic masses: an analysis of 3,090 patients from 212 hospitals. Gut Liver 2014;8:215-218.10.5009/gnl.2014.8.2.215Suche in Google Scholar PubMed PubMed Central
46 Jenssen C, Hocke M, Fusaroli P, Gilja OH, Buscarini E, Havre RF, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part IV - EUS-guided Interventions: General aspects and EUS-guided sampling (Long Version). Ultraschall Med 2016;37:E33-76.10.1055/s-0035-1553785Suche in Google Scholar PubMed
47 Dumonceau JM, Deprez PH, Jenssen C, Iglesias-Garcia J, Larghi A, Van-biervliet G, et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated January 2017. Endoscopy 2017;49:695-714.10.1055/s-0043-109021Suche in Google Scholar PubMed
48 Veitch AM, Vanbiervliet G, Gershlick AH, Boustiere C, Baglin TP, Smith LA, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut 2016;65:374-389.10.1136/gutjnl-2015-311110Suche in Google Scholar PubMed PubMed Central
49 Polkowski M, Jenssen C, Kaye P, Carrara S, Deprez P, Gines A, et al. Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline - March 2017. Endoscopy 2017;49:989-1006.10.1055/s-0043-119219Suche in Google Scholar PubMed
50 Facciorusso A, Mohan BP, Tacelli M, Crino SF, Antonini F, Fantin A, Barresi L. Use of antibiotic prophylaxis is not needed for endoscopic ultrasound-guided fine-needle aspiration of pancreatic cysts: a meta-analysis. Expert Rev Gastroenterol Hepatol 2020;14:999-1005.10.1080/17474124.2020.1797486Suche in Google Scholar PubMed
51 Colan-Hernandez J, Sendino O, Loras C, Pardo A, Gornals JB, Con-cepcion M, et al. Antibiotic prophylaxis is not required for endoscopic ultrasonography-guided fine-needle aspiration of pancreatic cystic lesions, based on a randomized trial. Gastroenterology 2020;158:1642-1649 e1641.10.1053/j.gastro.2020.01.025Suche in Google Scholar PubMed
52 Committee ASoP, Khashab MA, Chithadi KV, Acosta RD, Bruining DH, Chandrasekhara V, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 2015;81:81-89.10.1016/j.gie.2014.08.008Suche in Google Scholar PubMed
53 Dietrich CF, Lorentzen T, Appelbaum L, Buscarini E, Cantisani V, Correas JM, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part III - Abdominal Treatment Procedures (Long Version). Ultraschall Med 2016;37:E1-E32.10.1055/s-0035-1553917Suche in Google Scholar PubMed
54 Facciorusso A, Buccino VR, Sacco R. A meta-analysis confirms that antibiotic prophylaxis is not needed for endoscopic ultrasound-guided fine needle aspiration of pancreatic cysts. Gastroenterology 2021;160:969.10.1053/j.gastro.2020.02.072Suche in Google Scholar PubMed
55 Troncone E, D’Aversa F, Larghi A. Antibiotic prophylaxis for endoscopic ultrasound-guided diagnostic interventions on pancreatic cysts: a never-ending story. Gastroenterology 2021;160:970-971.10.1053/j.gastro.2020.02.073Suche in Google Scholar PubMed
56 Jenssen C, Alvarez-Sanchez MV, Napoleon B, Faiss S. Diagnostic endoscopic ultrasonography: assessment of safety and prevention of complications. World J Gastroenterol 2012;18:4659-4676.10.3748/wjg.v18.i34.4659Suche in Google Scholar PubMed PubMed Central
© 2025 Tobias Kleemann, Robert Freund, Barbara Braden, Michael Hocke, Stephan Hollerbach, Christian Jenssen, Kathleen Möller, Yi Dong, Manoop Singh Bhutani, Masayuki Kitano, Siyu Sun, Abed El-Lehibi, Christoph Frank Dietrich, published by De Gruyter on behalf of the SMP
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Artikel in diesem Heft
- Perspective
- Reperfusion therapy for acute ischemic stroke: Where we are and where to go
- Deciphering peripheral neuroimmune crosstalk for translational therapeutics
- Current applications and future perspectives of artificial intelligence in valvular heart disease
- Review Article
- Targeting regulated cell death: Apoptosis, necroptosis, pyroptosis, ferroptosis, and cuproptosis in anticancer immunity
- Senescent cells as a target for anti-aging interventions: From senolytics to immune therapies
- Original Article
- An international survey on the geographical differences in practice patterns and training of endoscopic ultrasound
- Glymphatic function decline as a mediator of core memory-related brain structures atrophy in aging
- Development of a broadly potent neutralizing antibody targeting Nidogen 1 effectively inhibits cancer growth and metastasis in preclinical tumor models
Artikel in diesem Heft
- Perspective
- Reperfusion therapy for acute ischemic stroke: Where we are and where to go
- Deciphering peripheral neuroimmune crosstalk for translational therapeutics
- Current applications and future perspectives of artificial intelligence in valvular heart disease
- Review Article
- Targeting regulated cell death: Apoptosis, necroptosis, pyroptosis, ferroptosis, and cuproptosis in anticancer immunity
- Senescent cells as a target for anti-aging interventions: From senolytics to immune therapies
- Original Article
- An international survey on the geographical differences in practice patterns and training of endoscopic ultrasound
- Glymphatic function decline as a mediator of core memory-related brain structures atrophy in aging
- Development of a broadly potent neutralizing antibody targeting Nidogen 1 effectively inhibits cancer growth and metastasis in preclinical tumor models


