Abstract
Objectives
Transvaginal cervical cerclage is a common intervention to prevent preterm birth in high-risk patients. This study aimed to compare McDonald and Shirodkar cerclage techniques in preventing preterm birth among patients with obesity, a group at increased risk for adverse pregnancy outcomes.
Methods
This was a retrospective study of singleton pregnancies complicated by pre-pregnancy obesity (BMI≥30 kg/m2) and transvaginal cerclage placement between 2018 and 2023 within a large health system in New York. The primary exposure was type of cerclage, McDonald or Shirodkar. Primary outcomes were preterm birth <37 weeks and <34 weeks. Secondary outcomes were spontaneous preterm birth <37 and <34 weeks, and gestational age at delivery. Subgroup analyses were performed by cerclage indication (history-, ultrasound-, or exam-indicated). Multivariate logistic regression and linear mixed model analyses were utilized to evaluate these outcomes while controlling for potential confounders.
Results
Of 495 patients included, 375 (76 %) underwent McDonald and 120 (24 %) underwent Shirodkar cerclage. In adjusted and unadjusted analyses, there was no significant difference in preterm birth at <37 or <34 weeks (p=0.98 and p=0.30 respectively) or spontaneous preterm birth at <37 or <34 weeks (p=0.75 and p=0.36) between the groups. There was no significant difference in mean gestational age at delivery (36.4 ± 4.3 vs. 35.9 ± 4.7 weeks, p=0.50). Subgroup analyses confirmed similar findings across cerclage indications, though with a benefit for the McDonald technique for ultrasound-indicated cerclages (36.6 ± 4.2 vs. 35.0 ± 5.1 weeks, p=0.02).
Conclusions
McDonald and Shirodkar cerclages are equally effective in prolonging pregnancy in patients with obesity.
Introduction
Transvaginal cervical cerclage is a well-established intervention in obstetrics, aimed at reducing preterm birth among patients with an elevated risk of cervical insufficiency. While the McDonald and Shirodkar techniques remain the two predominant approaches for this procedure, the choice between them is often dictated by provider preference and surgical complexity. The McDonald technique involves placing a purse-string suture circumferentially around the cervix, just distal to the vesico-cervical junction [1], 2]. The Shirodkar technique involves placement of this suture more cephalad, at the level of the internal cervical os, by first dissecting the bladder and rectum off the cervix [2], 3].
Several studies have compared the efficacy of the Shirodkar and McDonald techniques for history-, ultrasound-, and exam-indicated cerclages [2], [4], [5], [6], [7], [8], [9], [10], [11]. Overall, these studies have not demonstrated significant differences in their effectiveness for preventing spontaneous preterm birth. Limited evidence has directly compared the efficacy of these two techniques in specific patient populations, such as those with obesity. A recent study suggested that the Shirodkar technique may offer advantages in maintaining gestational length among patients with obesity, possibly due to its placement closer to the internal cervical os [12].
Obesity, defined as a body mass index (BMI) of 30 kg/m2 or greater, is a well-established risk factor for adverse pregnancy outcomes [13], 14] yet its impact on cerclage efficacy remains underexplored. The prevalence of obesity in pregnancy is increasing; in 2020, 29.5 % of live births in the United States were to mothers with a pre-pregnancy BMI of 30 kg/m2 or greater, and 26.7 % were in the overweight range with a BMI of 25 kg/m2 or greater [15]. Prior studies have shown mixed findings regarding the impact of obesity on preterm birth risk, both for patients with and without a cerclage [14], [16], [17], [18], [19], [20], [21], [22], [23]. While prior analyses comparing McDonald and Shirodkar techniques have reported similar outcomes in the general obstetric population, the potential benefit of the Shirodkar’s more proximal placement in mitigating cervical insufficiency in patients with obesity warrants focused investigation.
This study aims to evaluate the comparative effectiveness of McDonald vs. Shirodkar cervical cerclage in patients with obesity. By clarifying the impact of cerclage type on gestational age at delivery and preterm birth risk in this high-risk population, our findings can advance evidence-based pregnancy management and inform best practices to optimize maternal and neonatal outcomes.
Materials and methods
Study population
This was a retrospective cohort study of all singleton pregnancies complicated by obesity (BMI ≥30 kg/m2) and transvaginal cerclage placement between January 2018 and December 2023 at seven hospitals within a large academic health system in New York. These facilities provide care to a diverse patient population from both urban and suburban areas, representing a wide range of socioeconomic backgrounds. Patients were excluded if they had multiple gestations, transabdominal cerclages, other contraindications to vaginal cerclage placement, and if primary exposure or delivery outcome data was unavailable.
Data collection
Clinical and demographic data were obtained from the inpatient electronic medical record (EMR) system (Sunrise Clinical Manager, Allscripts Corp., Chicago, IL). Baseline demographic data included maternal age, self-identified race and ethnicity, and insurance status. Clinical data included BMI, parity, history of preterm birth, medical comorbidities, gestational age at delivery, and details of cerclage including type, indication, and gestational age at placement.
Exposures
The primary exposure was the type of cervical cerclage, McDonald or Shirodkar. The McDonald cerclage involved a purse-string suture placed distal to the vesicocervical junction, while the Shirodkar technique required a more cephalad placement with dissection of the bladder and rectum off the cervix.
Outcomes
The primary outcomes evaluated were preterm birth at <37 and <34 weeks of gestational age. The secondary outcomes evaluated were spontaneous preterm birth at <37 and <34 weeks, as well as gestational age at delivery, a continuous variable.
Statistical analysis
Descriptive statistics were used to characterize the study population, with categorical variables presented as frequencies and percentages and continuous variables as means with standard deviations. These characteristics were analyzed using chi-square or t-tests for categorical and continuous variables respectively. Outcomes of preterm birth and spontaneous preterm birth at <37 weeks and <34 weeks of gestation were analyzed using multivariate logistic regression to account for potential confounders, including cerclage indication, nulliparity, maternal age, BMI, history of preterm birth, and race and ethnicity group. Gestational age at delivery was analyzed using linear mixed model regression analysis, using the same adjustments as the primary analysis. Subgroup analyses were conducted based on cerclage indications (history-, ultrasound-, or exam-indicated), with additional adjustment for very short cervix (<1 cm) in the ultrasound-indicated cerclage subgroup.
There was no missing data for any of the primary or secondary outcomes, as patients were excluded from the study if this data was unavailable. For the independent variables, the only missing data were gestational ages at cerclage placement in two patients. As this represented only 0.4 % of the study population, no imputation of missing data was performed, and only available data was used in the analysis.
Statistical significance was defined as p<0.05, and all analyses were performed using R version 4.3.1. The Institutional Review Board approved this study as minimal-risk research using data collected for routine clinical practice and waived the requirement for informed consent.
Results
Out of 1,320 patients who received a cerclage between 2018 and 2023, 495 patients with obesity and singleton pregnancies who underwent transvaginal cervical cerclage were included for analysis. Patients were excluded for abdominal cerclage (n=22), multiple gestations (n=22), and missing primary exposure (n=111) or outcome data (n=409, 82 % McDonald and 18 % Shirodkar cerclages). Of the remainder, those with obesity were included in the study. Among these 495 included patients, 375 (76 %) received a McDonald cerclage, and 120 (24 %) received a Shirodkar cerclage. The study population included patients with history-indicated (n=160, 32.3 %), ultrasound-indicated (n=223, 45.1 %), and exam-indicated (n=112, 22.6 %) cerclages. Baseline characteristics of the study population are shown in Table 1 including maternal age, BMI, insurance status, race and ethnicity, nulliparity, and gestational age at cerclage placement, which were similar between the McDonald and Shirodkar groups. Progesterone use and history of preterm birth were also similar between the groups. There were significant differences noted in cerclage indication, with an increased frequency of Shirodkar cerclages in the ultrasound-indicated group compared to other indications (p=0.003).
Baseline characteristics.
| Characteristic | Full cohort (n=495) | McDonald (n=375) | Shirodkar (n=120) | p-Value |
|---|---|---|---|---|
| Maternal age, years | 33.6 ± 4.8 | 33.6 ± 4.9 | 33.6 ± 4.3 | 0.97 |
| BMI, kg/m2 | 37.4 ± 14.2 | 37.8 ± 16.1 | 36.3 ± 4.3 | 0.33 |
| Race and ethnicity | 0.06 | |||
| Non-Hispanic White | 68 (13.7) | 54 (14.4) | 14 (11.7) | |
| Non-Hispanic Black | 226 (45.7) | 166 (44.3) | 60 (50.0) | |
| Hispanic | 98 (19.8) | 84 (22.4) | 14 (11.7) | |
| Asian or Pacific Islander | 40 (8.1) | 25 (6.7) | 15 (12.5) | |
| Other or multiracial | 46 (9.3) | 34 (9.1) | 12 (10.0) | |
| Unknown or declined | 17 (3.4) | 12 (3.2) | 5 (4.2) | |
| Public health insurance | 226 (45.7) | 163 (43.5) | 63 (52.5) | 0.08 |
| Nulliparous | 216 (43.6) | 15 (41.3) | 61 (50.8) | 0.07 |
| History of preterm birth | 180 (36.4) | 145 (38.7) | 35 (29.2) | 0.06 |
| Pre-gestational diabetes | 26 (5.3) | 14 (3.7) | 12 (10.0) | 0.007 |
| Chronic hypertension | 57 (11.5) | 36 (9.6) | 21 (17.5) | 0.02 |
| Progesterone use | 139 (28.1) | 101 (26.9) | 38 (31.7) | 0.32 |
| Cerclage indication | 0.003 | |||
| History | 160 (32.3) | 130 (34.7) | 30 (25.0) | |
| Ultrasound | 223 (45.1) | 153 (40.8) | 70 (58.3) | |
| Exam | 112 (22.6) | 92 (24.5) | 20 (16.7) | |
| Gestational age at cerclage placement, weeksa | 17.0 ± 3.5 | 17.0 ± 3.5 | 17.2 ± 3.3 | 0.64 |
-
Data are presented as number (percentage) or mean±standard deviation. BMI, body mass index. aData missing in 2 cases (0.4 %), means are calculated based on cases with non-missing data.
There were no significant differences between the McDonald and Shirodkar groups in the adjusted or unadjusted analyses for the outcomes of preterm birth at <37 weeks (p=0.98) or at <34 weeks (p=0.30) (Table 2). There were also no significant differences in the outcomes of spontaneous preterm birth at <37 weeks (p=0.75) or at <34 weeks (p=0.36) (Table 3). Gestational age at delivery also did not differ significantly between the groups in both the unadjusted and adjusted analyses (Table 4). The mean gestational age at delivery was 36.4 ± 4.3 weeks for the McDonald group and 35.9 ± 4.7 weeks for the Shirodkar group (p=0.50). Subgroup analyses by cerclage indication (history-, ultrasound-, or exam-indicated) also revealed no significant difference in gestational age at delivery between the two techniques, except for ultrasound-indicated cerclages which favored the McDonald technique (36.6 ± 4.2 weeks vs. 35.0 ± 5.1 weeks, p=0.02) (Figure 1).
Multivariate logistic regression model for preterm birth <37 and <34 weeks.
| Preterm birth | ||||
|---|---|---|---|---|
| <37 Weeks | <34 Weeks | |||
| Characteristic | aOR (95 % CI) | p-Value | aOR (95 % CI) | p-Value |
| Cerclage type | ||||
| McDonald | Reference | Reference | ||
| Shirodkar | 1.0 (0.64–1.57) | 0.98 | 1.34 (0.77–2.29) | 0.30 |
| Cerclage indication | ||||
| History | Reference | Reference | ||
| Ultrasound | 0.87 (0.55–1.37) | 0.55 | 1.23 (0.68–2.27) | 0.50 |
| Exam | 1.23 (0.72–2.10) | 0.44 | 1.32 (0.66–2.66) | 0.43 |
| Nulliparity | 1.64 (1.08–2.51) | 0.02 | 1.24 (0.73–2.1) | 0.43 |
| History of preterm birth | 1.14 (0.74–1.77) | 0.55 | 0.55 (0.3–0.98) | 0.05 |
| BMI≥40 kg/m2 | 1.12 (0.72–1.73) | 0.61 | 1.30 (0.75–2.20) | 0.34 |
| Age≥35 years | 1.13 (0.77–1.65) | 0.54 | 0.86 (0.53–1.39) | 0.53 |
| Race and ethnicity | ||||
| Non-Hispanic White | Reference | Reference | ||
| Non-Hispanic Black | 1.32 (0.74–2.39) | 0.35 | 1.14 (0.58–2.37) | 0.71 |
| Hispanic | 1.22 (0.63–2.40) | 0.56 | 0.97 (0.43–2.26) | 0.95 |
| Asian or Pacific Islander | 0.93 (0.39–2.18) | 0.87 | 0.47 (0.12–1.47) | 0.22 |
| Other or multiracial | 1.06 (0.47–2.38) | 0.88 | 0.65 (0.21–1.84) | 0.44 |
| Unknown or declined | 0.63 (0.16–2.05) | 0.47 | 0.25 (0.01–1.42) | 0.20 |
-
CI, confidence interval; aOR, adjusted odds ratio; BMI, body mass index.
Multivariate logistic regression model for spontaneous preterm birth <37 and <34 weeks.
| Spontaneous preterm birth | ||||
|---|---|---|---|---|
| <37 Weeks | <34 Weeks | |||
| Characteristic | aOR (95 % CI) | p-Value | aOR (95 % CI) | p-Value |
| Cerclage type | ||||
| McDonald | Reference | Reference | ||
| Shirodkar | 1.09 (0.65–1.79) | 0.75 | 1.32 (0.71–2.39) | 0.36 |
| Cerclage indication | ||||
| History | Reference | Reference | ||
| Ultrasound | 1.25 (0.72–2.19) | 0.43 | 1.37 (0.68–2.87) | 0.39 |
| Exam | 2.33 (1.28–4.31) | 0.006 | 2.01 (0.93–4.47) | 0.08 |
| Nulliparity | 1.63 (1.02–2.63) | 0.04 | 1.51 (0.84–2.73) | 0.17 |
| History of preterm birth | 0.77 (0.46–1.29) | 0.33 | 0.39 (0.18–0.78) | 0.01 |
| BMI≥40 kg/m2 | 0.87 (0.52–1.44) | 0.60 | 1.04 (0.55–1.90) | 0.90 |
| Age≥35 years | 1.11 (0.72–1.71) | 0.65 | 0.97 (0.56–1.67) | 0.92 |
| Race and ethnicity | ||||
| Non-Hispanic White | Reference | Reference | ||
| Non-Hispanic Black | 1.33 (0.79–2.66) | 0.40 | 0.96 (0.47–2.08) | 0.92 |
| Hispanic | 1.25 (0.59–2.74) | 0.57 | 0.81 (0.33–2.01) | 0.65 |
| Asian or Pacific Islander | 0.88 (0.32–2.33) | 0.80 | 0.24 (0.03–0.0.95) | 0.07 |
| Other or multiracial | 1.15 (0.45–2.84) | 0.77 | 0.58 (0.17–1.74) | 0.35 |
| Unknown or declined | 0.24 (0.01–1.39) | 0.19 | 0.29 (0.02–1.73) | 0.26 |
-
CI, confidence interval; aOR, adjusted odds ratio; BMI, body mass index.
Birth outcomes by cerclage type.
| Outcome | McDonald (n=375) | Shirodkar (n=120) | aOR or aMD (95 % CI) | p-Value |
|---|---|---|---|---|
| Preterm birth | ||||
| <37 weeks | 133 (35.5) | 42 (35.0) | 1.0 (0.64–1.57) | 0.98 |
| <34 weeks | 61 (16.3) | 25 (20.8) | 1.34 (0.77–2.29) | 0.30 |
| Spontaneous preterm birth | ||||
| <37 weeks | 87 (23.2) | 30 (25.0) | 1.09 (0.65–1.79) | 0.75 |
| <34 weeks | 48 (12.8) | 20 (16.7) | 1.32 (0.71–2.39) | 0.36 |
| Gestational age at delivery | 36.4 ± 4.3 | 35.9 ± 4.7 | −0.31 (−1.23–0.60) | 0.50 |
-
Data are presented as number (percentage) or mean±standard deviation. CI, confidence interval; aMD, adjusted mean difference; aOR, adjusted odds ratio.
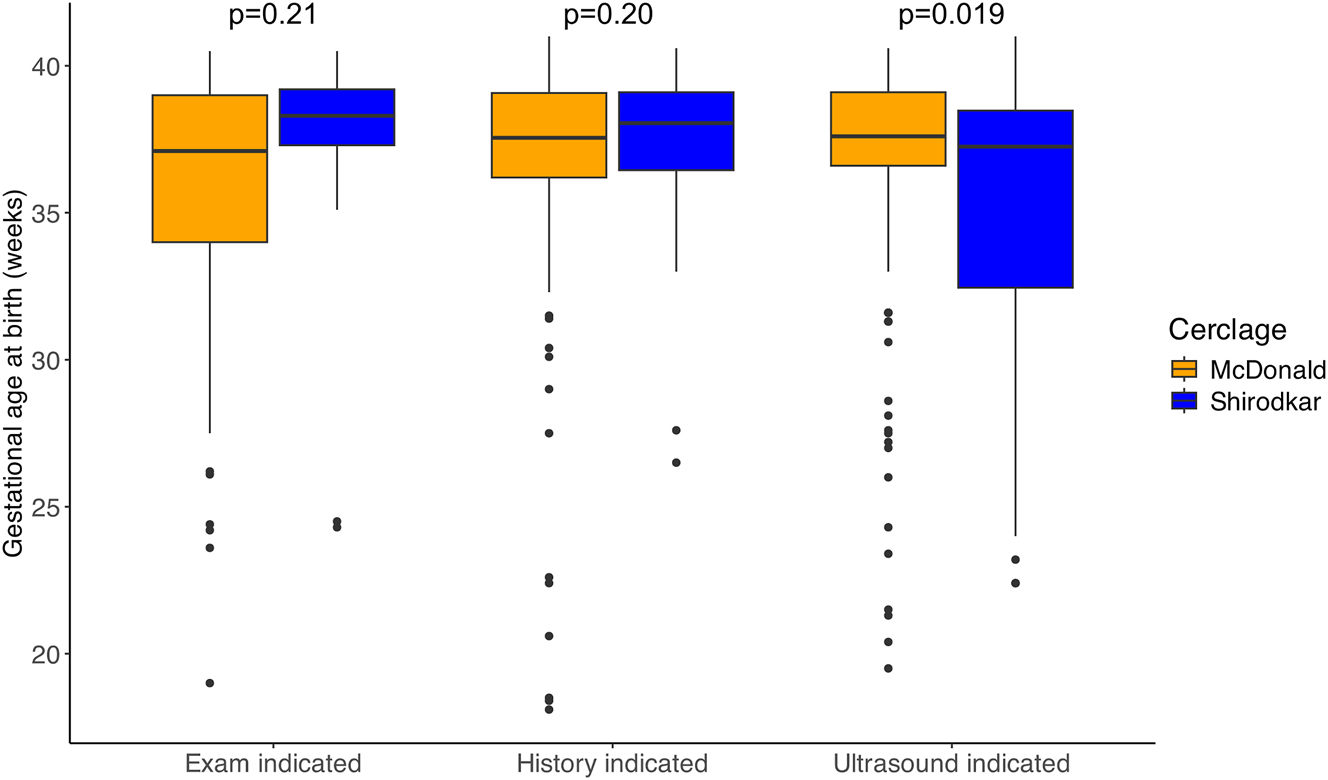
Subgroup analysis of gestational age at birth by cerclage indication and cerclage type.
Discussion
This study evaluated the comparative effectiveness of McDonald and Shirodkar cervical cerclage techniques in patients with obesity. Both techniques demonstrated similar efficacy in prolonging pregnancy, with no significant difference in gestational age at delivery, preterm birth, or spontaneous preterm birth at <37 or 34 weeks. Subgroup analyses by cerclage indication (history-, ultrasound-, or exam-indicated) confirmed these findings, with no difference for history- and exam-indicated cerclages, and greater pregnancy prolongation with the McDonald technique for ultrasound-indicated cerclages.
Prior research comparing McDonald and Shirodkar techniques has generally found comparable efficacy in the prevention of preterm birth across different patient populations [4], [5], [6], [7], [8], [9], [10], [11]. However, the effect of obesity on cerclage efficacy remains underexplored. Nguyen et al. conducted a large retrospective study using California birth data to assess the impact of maternal obesity on preterm delivery in patients with cervical cerclage [16]. Although cerclage type and indication were not evaluated, the study found that obesity did not increase the risk of spontaneous preterm delivery but was linked to higher overall preterm delivery rates, likely due to medical indications. The findings suggest cerclage effectively prevents spontaneous preterm delivery across BMI groups, but obese patients may face increased overall risk from other complications. A retrospective study by Figueroa et al. specifically investigated the interaction between maternal BMI and cerclage type on pregnancy duration [12]. The authors analyzed 95 women receiving McDonald or Shirodkar cerclage at a single institution over approximately 6 years. Shirodkar cerclage extended pregnancy compared to McDonald (36.7 vs. 33.9 weeks; p=0.02), with the greatest effect in obese women (32.6 vs. 28.8 weeks; p<0.01). No differences were seen in normal or overweight women (p=0.63). While these findings suggest that the Shirodkar technique may benefit obese patients, our much larger study found no BMI-related differences in cerclage efficacy, except improved pregnancy prolongation for the McDonald technique for ultrasound-indicated cerclages. Discrepancies may reflect population differences or unmeasured factors, highlighting the need for further research on BMI, cervical anatomy, and cerclage outcomes.
Given the similar efficacy of McDonald and Shirodkar cerclages in this study, the choice of technique in patients with obesity should consider other factors, such as surgeon familiarity, procedural difficulty, and the patient’s specific anatomy. In addition, rates of complications such as bladder injury and need for regional anesthesia for cerclage removal may be higher in Shirodkar compared to McDonald cerclages. Concern about more complications with equivalent benefit may lead providers to favor the McDonald technique. Overall, care can be individualized to consider all of these factors, and this flexibility in clinical decision-making may help optimize outcomes without sacrificing efficacy. Our findings suggest that providers can prioritize patient-centered care and surgical efficiency when determining the appropriate technique for cerclage placement in patients with obesity.
Future research should focus on clarifying the interaction between obesity, cervical anatomy, and cerclage efficacy. While this study found no difference in outcomes between McDonald and Shirodkar cerclages in obese patients, conflicting findings in prior studies highlight the need to explore factors such as cervical length, suture material, and degree of dilation at placement. Investigating the biomechanical impact of cerclage techniques in the context of increased intra-abdominal pressure could provide valuable insights, particularly for obese patients who may experience higher cervical stress. Subgroup analyses, including patients with prior cervical surgery or mid-trimester loss, may help identify those who derive greater benefit from Shirodkar cerclage. Advanced imaging and computational modeling can further elucidate how cerclage placement affects cervical tissue integrity. Additionally, studies assessing long-term maternal and neonatal outcomes will help refine patient selection and optimize management strategies for cervical insufficiency in this high-risk population.
A key strength of this study is its large cohort size, which allowed for robust statistical analyses and subgroup evaluations. Additionally, the inclusion of a diverse patient population enhances the generalizability of the findings. However, the retrospective design introduces potential biases, including unmeasured clinical factors and other confounders that may have influenced the choice of cerclage technique. Data on physician experience, suture material, suture number, and concomitant progesterone use were not collected and thus could not be included in this analysis. The absence of data on secondary outcomes, such as cerclage-associated complications, limits the comprehensiveness of the analysis. Future studies should address these limitations by incorporating prospective designs and broader outcome measures.
Conclusions
Both McDonald and Shirodkar cerclages are effective in prolonging pregnancy in patients with obesity, with no significant difference in gestational age at delivery between techniques. These findings support the use of either method based on procedural considerations and provider expertise, offering flexibility in managing a high-risk population. Further research is needed to confirm these results and explore additional factors that may influence cerclage outcomes.
Acknowledgments
Research findings were presented at the Society for Maternal-Fetal Medicine Annual Pregnancy Meeting in Denver, CO in January 2025.
-
Research ethics: The Northwell Health Institutional Review Board approved this study on 5/31/2024, IRB reference number 24-0245. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The participants of this study did not give written consent for their data to be shared publicly, so supporting data is not available.
References
1. McDonald, IA. Suture of the cervix for inevitable miscarriage. J Obstet Gynaecol Br Emp 1957;64:346–50. https://doi.org/10.1111/j.1471-0528.1957.tb02650.x.Suche in Google Scholar PubMed
2. Berghella, V, Ludmir, J, Simonazzi, G, Owen, J. Transvaginal cervical cerclage: evidence for perioperative management strategies. Am J Obstet Gynecol 2013;209:181–92. https://doi.org/10.1016/j.ajog.2013.02.020.Suche in Google Scholar PubMed
3. Shirodkar, V. A new method of operative treatment for habitual abortions in the second trimester of pregnancy. Antiseptic 1955;52:299–300.Suche in Google Scholar
4. Peters, W3rd, Thiagarajah, S, Harbert, GJ. Cervical cerclage: twenty years’ experience. South Med J 1979;72:933–7. https://doi.org/10.1097/00007611-197908000-00010.Suche in Google Scholar PubMed
5. Cardwell, MS. Cervical cerclage: a ten-year review in a large hospital. South Med J 1988;8:15–9. https://doi.org/10.1097/00007611-198801000-00004.Suche in Google Scholar PubMed
6. Otsuki, K, Nakai, A, Matsuda, Y, Shinozuka, N, Kawabata, I, Makino, Y, et al.. Randomized trial of ultrasound-indicated cerclage in singleton women without lower genital tract inflammation. J Obstet Gynaecol Res 2016;42:148–57. https://doi.org/10.1111/jog.12880.Suche in Google Scholar PubMed
7. Basbug, A, Bayrak, M, Doğan, O, Ellibeş Kaya, A, Goynumer, G. McDonald versus modified Shirodkar rescue cerclage in women with prolapsed fetal membranes. J Matern Fetal Neonatal Med 2020;33:1075–9. https://doi.org/10.1080/14767058.2018.1514378.Suche in Google Scholar PubMed
8. Harger, HH. Comparison of success and morbidity in cervical cerclage procedures. Obstet Gynecol 1980;56:543–8.Suche in Google Scholar
9. Rozenberg, P, Sénat, MV, Gillet, A, Ville, Y. Comparison of two methods of cervical cerclage by ultrasound cervical measurement. J Matern Fetal Neonatal Med 2003;13:314–7. https://doi.org/10.1080/jmf.13.5.314.317.Suche in Google Scholar PubMed
10. Robertson, P, Chaithongwongwatthana, S, Daly, S, Pereira, L, Rasanen, J, Cotter, A, et al.. McDonald vs. Shirodkar: outcomes in the expectant management compared to physical exam-indicated cerclage (EM-PEC) international cohort study. Am J Obstet Gynecol 2006;195:S25. https://doi.org/10.1016/j.ajog.2006.10.064.Suche in Google Scholar
11. Odibo, AO, Berghella, V, To, MS, Rust, OA, Althuisius, SM, Nicolaides, KH. Shirodkar versus McDonald cerclage for the prevention of preterm birth in women with short cervical length. Am J Perinatol 2007;24:55–60. https://doi.org/10.1055/s-2006-958165.Suche in Google Scholar PubMed
12. Figueroa, R, Crowell, R, Martinez, A, Morgan, M, Wakefield, D. McDonald versus Shirodkar cervical cerclage for the prevention of preterm birth: impact of body mass index. J Matern Fetal Neonatal Med 2019;32:3408–14. https://doi.org/10.1080/14767058.2018.1465037.Suche in Google Scholar PubMed
13. Obesity in Pregnancy: ACOG Practice Bulletin, Number 230. Obstet Gynecol 2021;6:e128–44.10.1097/AOG.0000000000004395Suche in Google Scholar PubMed
14. Khan, S, Baranco, N, Wojtowycz, M, Parker, P, Mastrogiannis, DS. Maternal super obesity is increasing and is associated with an increased risk of pregnancy complications—a call for concern. J Matern Fetal Neonatal Med 2024;37. https://doi.org/10.1080/14767058.2024.2396071.Suche in Google Scholar PubMed
15. Creanga, AA, Catalano, PM, Bateman, BT. Obesity in pregnancy. N Engl J Med 2022;387:248–59. https://doi.org/10.1056/nejmra1801040.Suche in Google Scholar
16. Nguyen, HY, Park, B, Rossi, J, Tse, B, Cryer, A, Yao, R. Impact of maternal obesity on preterm delivery in patients with cervical cerclage. AJOG Global Rep 2023;3. https://doi.org/10.1016/j.xagr.2023.100211.Suche in Google Scholar PubMed PubMed Central
17. Poggi, SH, Vyas, NA, Pezzullo, JC, Landy, HJ, Ghidini, A. Does increasing body mass index affect cerclage efficacy. J Perinatol 2012;32:777–9. https://doi.org/10.1038/jp.2011.198.Suche in Google Scholar PubMed
18. Lynch, AM, Hart, JE, Agwu, OC, Fisher, BM, West, NA, Gibbs, RS. Association of extremes of prepregnancy BMI with the clinical presentations of preterm birth. Am J Obstet Gynecol 2014;210:428.e1–428.e9. https://doi.org/10.1016/j.ajog.2013.12.011.Suche in Google Scholar PubMed
19. Hendler, I, Goldenberg, RL, Mercer, BM, Iams, JD, Meis, PJ, Moawad, AH, et al.. The Preterm Prediction study: association between maternal body mass index and spontaneous and indicated preterm birth. Am J Obstet Gynecol 2005;192:882–6.10.1016/j.ajog.2004.09.021Suche in Google Scholar PubMed
20. Lee, KN, Yun, S, Park, SY, Kim, K, Lee, KY, Lee, JJ, et al.. Factors associated with spontaneous preterm birth after ultrasound-indicated cerclage. J Personalized Med 2023;13. https://doi.org/10.3390/jpm13121678.Suche in Google Scholar PubMed PubMed Central
21. Sawadogo, W, Tsegaye, M, Gizaw, A, Newland, H, Adera, T. Maternal pre-pregnancy body mass index and risk of preterm birth: the role of weight gain during pregnancy, race and ethnicity. Am J Perinatol 2024. https://doi.org/10.1055/a-2494-2080.Suche in Google Scholar PubMed
22. Farinelli, CK, Wing, DA, Szychowski, JM, Owen, J, Hankins, G, Iams, JD, et al.. Association between body mass index and pregnancy outcome in a randomized trial of cerclage for short cervix. Ultrasound Obstet Gynecol 2012;40:669–73. https://doi.org/10.1002/uog.11170.Suche in Google Scholar
23. Yalvac, S, Esin, S, Kocak, O, Yirci, B, Kandemir, O. Effect of body mass index on latency periods after history-indicated cervical cerclage. Aust N Z J Obstet Gynaecol 2014;54:121–5. https://doi.org/10.1111/ajo.12185.Suche in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

