Abstract
Objectives
In the UK one in 250 pregnancies end in stillbirth. Abnormal placental villous maturation, commonly associated with gestational diabetes, is a risk factor for stillbirth. Histopathology reports of placental distal villous immaturity (DVI) are reported disproportionately in placentas from otherwise unexplained stillbirths in women without formal diagnosis of diabetes but with either clinical characteristics or risk factors for diabetes. This study aims to establish maternal factors associated with DVI in relation to stillbirth.
Methods
Placental histopathology reports were reviewed for all pregnant women delivering at University College London Hospital between July 2018 to March 2020. Maternal characteristics and birth outcomes of those with DVI were compared to those with other placental lesions or abnormal villous maturation.
Results
Of the 752 placental histopathology reports reviewed, 11 (1.5%) were reported as diagnostic of DVI. Eighty cases were sampled for clinical record analysis. All women with DVI had normal PAPP-A (>0.4 MoM), normal uterine artery Doppler studies (UtA-PI) and were normotensive throughout pregnancy. Nearly one in five babies (2/11, 18.5%) with DVI were stillborn and 70% had at least one high glucose test result in pregnancy despite no formal diagnosis of diabetes.
Conclusions
These findings suggest that the mechanism underlying stillbirth in DVI likely relates to glucose dysmetabolism, not sufficient for diagnosis using current criteria for gestational diabetes, resulting in placental dysfunction that is not identifiable before the third trimester. Relying on conventional diabetes tests, foetal macrosomia or growth restriction, may not identify all pregnancies at risk of adverse outcomes from glucose dysmetabolism.
Introduction
Around one in 250 births end in stillbirth in the UK [1]. Gestational diabetes mellitus (GDM) is a risk factor for stillbirth [2] and its prevalence is increasing alongside rising rates of obesity, type 2 diabetes mellitus and advanced maternal age [3, 4]. The potentially lethal consequences of undiagnosed gestational diabetes are well established; women with raised fasting plasma glucose (FPG) levels not diagnosed with GDM have a four-fold increased risk of stillbirth compared to women with normal FPG values (aOR 4.22, 95% CI 1.04–17.02), and to those with a formal diagnosis of GDM (aOR 1.10, 95% CI 0.31–3.91) [5].
Historically, there has been global variation in glucose tolerance test (GTT) diagnostic criteria. In HAPO, 14.3% of women had GDM by three-step IADPSG criteria but not two-step criteria [6]. Studies have shown that women who met IADPSG three-step criteria but who were not diagnosed with GDM based on two-step (e.g. NICE) diagnostic strategies [4], and were therefore not treated, had an increased risk for adverse perinatal outcomes compared with women who do not have GDM but also compared to women who had diagnosed and treated diabetes. Even the WHO criteria have been called into question for not being sensitive enough [7] in identifying women with milder forms of diabetes. The current strategy for diagnosing GDM may be leaving women who are at risk for adverse events without the lifestyle and pharmacological interventions that could improve their pregnancy outcomes [8].
Abnormal placental villous maturation refers to villous morphology with developmentally abnormal features that is not typical of gestational age. A systematic review concluded that women with pre-existing diabetes or GDM have increased frequency of immature villi compared to women with normoglycemia [9]. Diffuse/distal villous immaturity (DVI) is characterised by numerous chorionic villi having centrally placed capillaries, a continuous cytotrophoblast later and decreased vasculosyncytial membranes for gestation [10]. This pathological lesion is typically only reported at histology late in the third trimester [10]. It is hypothesised that foetuses affected by placental DVI have a decreased reserve to withstand stressors such as transient hypoxia in the late stages of pregnancy, thereby increasing their risk of stillbirth [11]. Anecdotally several maternity hospitals have observed a disproportionally high number of placental villous dysmaturity reported in otherwise unexplained stillbirths in women with clinical characteristics or risk factors for diabetes (e.g. foetal macrosomia or high BMI) but without a formal diagnosis of diabetes.
Additional placental histopathological lesions are also reported in women with diabetes in pregnancy [12]. Accelerated villous maturation (AVM) and distal villous hypoplasia (DVH) are associated with maternal vascular malperfusion (MVM) lesions, which represent hypoxic ischaemic damage to the placenta. Foetal thrombotic lesions, including foetal vascular malperfusion (FVM), have also been reported more frequently in placentas of women with diabetes in pregnancies [10, 13].
Current literature demonstrates the link between diabetes and abnormal villous maturity and that puts women at increased risk of stillbirth [14]. However, less is known about the women with DVI without a formal diagnosis of diabetes mellitus. Women with dysregulated glucose metabolism may be underdiagnosed and suffer adverse outcomes as a result. The primary objective of this study is to establish maternal factors related to abnormal villous maturation. Specifically, we compared maternal characteristics and pregnancy outcomes of women with abnormal placental maturation including DVI to other common placental findings such as AVM, DVH, MVM and FVM to determine when in pregnancy this placental dysfunction related to DVI is likely to be identified.
Materials and methods
This was a retrospective case control study investigating clinical factors relating to DVI. Ethics Committee approval was not required as the data were collected as part of the service and no identifiable data were included.
We reviewed all 752 placental histopathology reports and pregnancy outcomes for women delivering at University College London Hospital (UCLH) who had placentas submitted for histological examination between July 2018 and March 2020.
Any histopathology report with mention of AVM or DVH was included in the dataset. Any other abnormalities associated with AVM, MVM and FVM were also included. These included descriptions of small straight villi, hypoplastic villi, villous oedema, avascular villi, fibrin thrombi, intervillous thrombus, intervillous or perivillous fibrin deposition, increase in syncytial knot formation, areas of infarction, a macroscopically small placenta. Cases with foetal abnormality, villitis or chorioamnionitis alone were excluded.
We identified 237 cases of abnormal placental villous histology. Lesions were grouped into categories (Table 1) compliant with the Amsterdam Placental Workshop Group Consensus Statement [10] but with effort to isolate abnormalities relevant to glucose dysmetabolism alone from those associated with pre-eclampsia superimposed on gestational diabetes.
Histopathological groups and characteristics.
| Group | Lesions present | Age >40 years | BMI >30 kg/m2 | Chronic hypertension | PCOS | Group total |
|---|---|---|---|---|---|---|
| A | A1 = Accelerated maturation | 5/12 (41.7%) | 1/12 (8.3%) | 1/12 (8.3%) | 0/12 | n=12 |
| A2 = Distal villous immaturity | 1/11 (9.1%) | 2/10 (20.0%) | 0/11 | 0/10 | n=11 | |
| B | B1 = FVM | 2/11 (16.7%) | 1/9 (11.1%) | 0/11 | 0/11 | n=11 |
| B2 = Villous oedemaa | 0/7 | 0/7 | 0/7 | 0/7 | n=7 | |
| C | A combination of features of both abnormal villous maturation and MVM | 4/20 (20.0%) | 3/18 (16.7%) | 1/20 (5.0%) | 1/20 (5.0%) | n=20 |
| D | MVM alone | 5/19 (26.3%) | 2/19 (10.5%) | 2/19 (10.5%) | 2/19 (10.5%) | n=19 |
-
aCases were not included in group B if there was another justification for villous oedema, such as chorioamnionitis or villitis. Denominators reflect unavailable data (e.g. pre-pregnancy BMI not found in medical records if booking appointment not at UCLH). FVM, foetal vascular malperfusion; MVM, maternal vascular malperfusion; PCOS, polycystic ovarian syndrome.
Clinical records were accessed on Epic™ and ViewPoint™ electronic health record databases through linkage of hospital number or name and date of birth. All patients according to the local protocol had a random blood glucose (BG) in the first trimester, a glucose challenge test (GCT) in the late second trimester and a third trimester 2 h GTT with 75 g dependent on risk factors. Women with foetal macrosomia had home blood glucose monitoring (HBGM).
For the purpose of this study, we considered borderline high values for glucose testing to be ‘abnormal’: indicative of potential glucose dysmetabolism. Booking glucose was considered ‘abnormal’ at >5.0 mmol/L, and >7.0 mmol/L was the threshold for GCT. GTT values were considered to be high if 60 min BG was >10 mmol/L and 120 min BG was >7.0 mmol/L. Risk factors for diabetes evaluated in the clinical records were maternal age >40 years, BMI >30, pre-pregnancy polycystic ovary syndrome (PCOS), a first degree relative with diabetes, previous macrosomic baby or previous stillbirth.
Maternal demographics and pregnancy outcomes were recorded, including maternal comorbidities, gestational diabetes, hypertensive disease, antenatal scan findings and birth outcomes. Maternal characteristics and pregnancy outcomes were compared between groups using Fisher’s exact test (Figure 1).
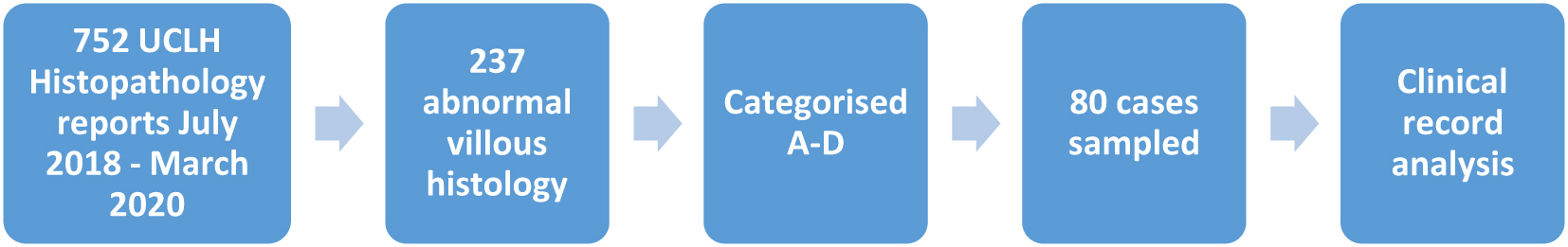
Flow chart showing how samples were derived.
Results
A total of 80 cases were included in the study. Indications for histopathology varied; groups and ranged from obstetric history (adverse outcome, molar pregnancy) to unexpected poor neonatal condition. Group A included placental histopathology with abnormal villous maturation (n=23) and was separated into A1, AVM or villous hypoplasia (n=12) and A2, DVI (n=11). So that all groups would have similar number of cases, the 23 cases of villous maturation were matched to 18 cases (group B), 20 cases (group C) and 19 cases (group D) for clinical record analysis.
Group B (n=18) included cases with abnormal villous histology but with no direct mention of delayed or accelerated maturation. Two cases were excluded as there was coexistent villous oedema and severe chorioamnionitis. This group was further split into two groups; B1 (n=11) included cases with FVM and descriptions of segmental avascular villi or thrombosis. B2 (n=7) included reports of villous oedema, a non-specific finding.
Cases in group C (n=20) show a combination of features of both abnormal villous maturation and MVM. That is, mention of either A or B lesions plus a mention MVM or findings associated with MVM such as increased syncytial knot formation, intervillous thrombus, infarction, perivillous fibrin or fibrin thrombi.
Group D (n=19) includes findings suggestive of MVM but no factors mentioned suggestive of otherwise abnormal villous maturation.
There were no cases of pre-existing diabetes. PCOS was found only in cases with MVM (groups C and D) in this study. Advanced maternal age >40 and hypertensive conditions were most prevalent in groups A1, C and D compared to group A2 and B1 (Table 1). DVI (group A2) was associated with numerically higher rates of stillbirth (n=2/11, 18.2%) and maternal BMI >30 (n=2/10, 20%), compared to other groups (Table 2). None of the mothers to babies that were stillborn with DVI were >40 years old, none had pre-existing diabetes, none had chronic hypertension (Table 1).
Diagnosis of gestational diabetes, macrosomia, abnormal lacentation and outcome of pregnancies in each group.
| Group | Diabetes | Placental dysfunction | Stillbirth | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lesion | Any formally abnormal glucose reading | Any abnormal glucose reading | Glucose normal but risk factors for diabetes | Formal diagnosis of GDM | Macrosomia | Uterine artery Doppler total PI >2.5b | PAPP-A <0.4c | PET | FGR | ||
| A | A1 = Accelerated maturation (n=12) | 3/12 (25.0%) | 6/12 (50.0%) | 4/6 (66.7%) | 2/12 (16.7%) | 0/12 | 3/6 (50.0%) | 1/7 (14.3%) | 1/11 (9.1%) | 6/11 (54.5%) | 0/12 |
| A2 = Distal villous immaturity (n=11) | 5/10 (50.0%) | 7/10 (70.0%) | 1/3 (30%) | 0/10 | 3/10 (30.0%) | 0/9 | 0/7 | 0/11 | 2/10 (20%) | 2/11 (18.2%) | |
| B | B1 = FVM (n=11) | 4/10 (40.0%) | 5/10 (50.0%) | 2/5 (40.0%) | 0/11 | 1/11 (9.1%) | 5/9 (55.6%) | 0/7 | 0/10 | 1/10 (41.2%) | 0/11 |
| B2 = Villous oedema (n=7) | 2/7 (28.6%) | 2/7 (28.6%) | 1/5 (20.0%) | 1/6 (16.7) | 0/7 | 4/5 (80.0%) | 0/4 | 1/6 (16.7%) | 5/5 (100%) | 0/7 | |
| C | Combined dysmaturity and MVM (n=20) | 4/17 (23.5%) | 7/17 (41.2%) | 4/10 (40.0%) | 2/19 (10.5%) | 1/19 (5.3%) | 15/20 (75.0%) | 5/15 (33.3%) | 12/19 (63.2%) | 14/19 (73.7%) | 1/20 (5%) |
| D | MVM alone (n=19) | 2/18 (11.1%) | 5/18 (27.8%) | 6/13 (46.2%) | 1/19 (5.3%) | 0/16 | 8/14 (57.1%) | 1/12 (8.3%) | 5/17 (29.4%) | 5/15 (33.3%) | 2/19 (10.5%) |
-
Denominators reflect unavailable data (e.g. PAPP-A not performed). GDM, gestational diabetes mellitus; PET, pre-eclampsia; FGR, foetal growth restriction; FVM, foetal vascular malperfusion; MVM, maternal vascular malperfusion. bp<0.001 A2 vs. other groups, cp<0.05 A2 and B vs. other groups.
All (100%) women with DVI and FVM had normal first trimester pregnancy associated plasma protein-A (PAPP-A) levels (>0.4 MoM), a proportion significantly higher for DVI and FVM than all other groups. All (100%) women with DVI had normal uterine artery Doppler studies, a proportion significantly higher for DVI than all other groups. In contrast, 55.6% (5/9) of the women with FVM (another histopathology possibly associated with undiagnosed diabetes) had abnormal uterine artery Doppler pulsatility index (PI) by UCLH criteria (total bilateral >2.5). No woman with DVI had pregnancy induced hypertension.
A total of 63.2% (12/19) of those with combined abnormal villous maturation and MVM (group C) showed pre-eclampsia and 73.7% (14/19) had FGR, whereas those with MVM alone (group D) showed 29.4% (5/17) and 33.3% (5/15) of pre-eclampsia and FGR respectively.
Of those with AVM (A1) and DVI (A2), 83% (10/12) and 80% (8/10) respectively had at least one abnormal glucose test result or risk factor for diabetes. Substantially more women with disorders of villous maturation had at least one abnormal glucose test result (random glucose or GCT) compared to other groups (70%, 7/10, in group A2 vs. 28.6%, 41.2%, 27.8% in groups B2, C, D respectively), despite no formal diagnosis of diabetes (normal GTT/HMGM). Of the seven women with DVI (A2) with an abnormal glucose test result, 3/7 had an abnormal GCT, 3/7 had abnormal booking/random BG reading and 1/7 had an abnormal 2 h GTT.
DVI was also associated with significantly higher rates of macrosomia than all other groups (30% in A2 vs. 0%, 9.1%, 0%, 5.3% and 0% in groups A1, B1, B2, C and D respectively). Half (5/10, 50%) of their babies were normal weight, 3/10 had macrosomia and 2/10 were growth restricted.
Discussion
The results suggest that women with abnormal villous maturation may have dysregulated glucose metabolism which is not currently diagnosed antenatally. Moreover, women with DVI do not show signs of placental dysfunction in the first (PAPP-A) or second (uterine artery PI) trimester, whereas conversely women with FVM, another histopathology possibly associated with undiagnosed diabetes, tend to have abnormal uterine artery PI despite normal PAPP-A. Women with dysregulated glucose metabolism may be undetected using current criteria for detection of diabetes and screening for placental dysfunction and suffer adverse outcomes as a result.
This was a retrospective review of clinical reports meaning that the reporting pathologists were unblinded to the clinical history which may have introduced bias. The study was also small and in a single centre; future larger multicentre studies should be blinded to indication for placental examination. However, a strength of the study is that all women at the unit routinely have both PAPP-A and uterine artery PI measured in the first and second trimester respectively; missing data reflect women with care partially delivered elsewhere. This enabled us to study patterns in these two markers preceding the various histopathological patterns.
Pregnancies with abnormal villous maturation such as DVI appear to start with normal placentation, but with villous changes occurring in the third trimester, possibly as a result of glucose dysmetabolism not sufficient for diagnosis with current diabetes criteria. Women with FVM and other isolated villous abnormalities seem to develop placental dysfunction earlier, in the second trimester. We provide preliminary evidence to support the hypothesis that DVI occurs in association with glucose dysmetabolism (insufficient for diagnosis with current diabetes criteria), as higher BMI, BG readings at early screening tests, macrosomia and stillbirth rates, were observed in the DVI group compared to pregnancies with other placental pathologies. Conversely, characteristics typically associated with ischaemic placental insufficiency including advanced maternal age >40 years and hypertensive disease, were not prevalent in the DVI group. There appears to be much higher levels of pre-eclampsia and foetal growth restriction when both abnormal villous maturation and MVM (group C) placental lesions are present, compared to MVM alone (group D).
Our analysis of placental pathology in association with maternal characteristics and birth outcomes enables us to broadly categorise women two categories; those with placental dysfunction primarily related impaired placentation and MVM and those with dysfunction primarily related to abnormal maturation and glucose metabolism. Since diabetes mellitus may also be associated with pre-eclampsia, placentas may have features of more than one histopathological pattern, making sufficiently powered research difficult. FVM appears to be an example of complex underlying pathophysiology and may in part result from multiple different insults leading to signs of FVM in stillbirths, such as viral infections and umbilical cord variations [15], or mild thrombophilias, particularly when combined with undiagnosed diabetes affecting red cell deformability. The potentially severe consequences of fetal vascular malperfusion have recently been highlighted by Gardella et al. including an increased risk of severe neurodevelopmental impairment at two years of age in pregnancies complicated by early (<34 weeks) fetal growth restriction [16]. Yet, the relative contribution of glucose dysmetabolism, umbilical cord abnormalities and other pathologies to the pathogenesis of FVM remains unknown.
Diabetes mellitus represents a disease spectrum [7] and the study results suggest that relying on conventional diabetes tests, fetal macrosomia or growth restriction may not identify all pregnancies at risk of stillbirth from glucose dysmetabolism. Moreover, models of stillbirth prevention focussing on PAPP-A and uterine artery PI, as well as maternal age, considered to be amongst the best prognostic markers alongside placental growth factor (PlGF) [17] might miss every single case at risk of DVI. Prevention of harm could instead involve testing for dysmetabolism with more sensitive criteria, and novel approaches including antenatal micro-imaging of the placenta. The human placenta project strives to develop new technologies for the real-time assessment of placental development and interventions to prevent abnormal placental development [18].
The need for progress is urgent. Whilst otherwise ‘unexplained’ stillbirths may occur in women with markers of diabetes associated with placental DVI or FVM, identification and treatment of glucose dysmetabolism with carbohydrate restriction and if necessary, insulin may reduce both the incidence and the severity of FVM [19]. It remains uncertain whether early diagnosis and treatment might ameliorate DVI progression. In the meantime, all women in pregnancy should be supported and encouraged to have a healthy lifestyle including exercise [20].
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interest: Authors state no conflict of interest.
-
Informed consent: Not applicable.
-
Ethical approval: Not applicable. Ethics Committee approval was not required as the data were collected as part of the service and no identifiable data were included.
References
1. ONS. Vital statistics in the UK: births, deaths and marriages - 2018 update. London, England: Office of National Statistics; 2018.Search in Google Scholar
2. Schmidt, M, Duncan, B, Reichelt, A, Branchtein, L, Matos, M, Costa e Forti, A, et al.. Gestational diabetes mellitus diagnosed with a 2-h 75-g oral glucose tolerance test and adverse pregnancy outcomes. Diabetes Care 2001;24:1151–5. https://doi.org/10.2337/diacare.24.7.1151.Search in Google Scholar PubMed
3. Ferrara, A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care 2007;30:S141–6. https://doi.org/10.2337/dc07-s206.Search in Google Scholar PubMed
4. National Institute for Health and Care Excellence. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. Available from: nice.org.uk/guidance/ng3 [Accessed 9 Jun 2020].Search in Google Scholar
5. Stacey, T, Tennant, PWG, McCowan, LME, Mitchell, EA, Budd, J, Li, M, et al.. Gestational diabetes and the risk of late stillbirth: a case–control study from England, UK. Br J Obstet Gynaecol 2019;126:973–82. https://doi.org/10.1111/1471-0528.15659.Search in Google Scholar PubMed
6. Waters, TP, Dyer, AR, Scholtens, DM, Dooley, SL, Herer, E, Lowe, LP, et al.. HAPO Cooperative Study Research Group. Maternal and neonatal morbidity for women who would Be added to the diagnosis of GDM using IADPSG criteria: a secondary analysis of the hyperglycemia and adverse pregnancy outcome study. Diabetes Care 2016;39:2204–10. https://doi.org/10.2337/dc16-1194.Search in Google Scholar PubMed PubMed Central
7. Hezelgrave, N, Rajasingham, D, Shennan, A, Torloni, M. Mild gestational diabetes: towards a redefined threshold? Expet Rev Endocrinol Metabol 2012;7:669–76. https://doi.org/10.1586/eem.12.59.Search in Google Scholar PubMed
8. Shah, BR, Sharifi, F. Perinatal outcomes for untreated women with gestational diabetes by IADPSG criteria: a population-based study. Br J Obstet Gynaecol 2020;127:116–22. https://doi.org/10.1111/1471-0528.15964.Search in Google Scholar PubMed
9. Huynh, J, Dawson, D, Roberts, D, Bentley-Lewis, R. A systematic review of placental pathology in maternal diabetes mellitus. Placenta 2015;36:101–14. https://doi.org/10.1016/j.placenta.2014.11.021.Search in Google Scholar PubMed PubMed Central
10. Khong, T, Mooney, E, Ariel, I, Balmus, N, Boyd, T, Brundler, M, et al.. Sampling and definitions of placental lesions: Amsterdam placental Workshop group consensus statement. Arch Pathol Lab Med 2016;140:698–713. https://doi.org/10.5858/arpa.2015-0225-cc.Search in Google Scholar PubMed
11. Redline, R. Distal villous immaturity. Diagn Histopathol 2012;18:189–94. https://doi.org/10.1016/j.mpdhp.2012.02.002.Search in Google Scholar
12. Scifres, C, Parks, W, Feghali, M, Caritis, S, Catov, J. Placental maternal vascular malperfusion and adverse pregnancy outcomes in gestational diabetes mellitus. Placenta 2017;49:10–5. https://doi.org/10.1016/j.placenta.2016.11.004.Search in Google Scholar PubMed
13. Redline, RW, Ravishankar, S. Fetal vascular malperfusion, an update. APMIS 2018;126:561–9. https://doi.org/10.1111/apm.12849.Search in Google Scholar PubMed
14. Stallmach, T, Hebisch, G, Meier, K, Dudenhausen, J, Vogel, M. Rescue by birth: defective placental maturation and late fetal mortality. Obstet Gynecol 2001;97:505–9. https://doi.org/10.1097/00006250-200104000-00005.Search in Google Scholar
15. Ptacek, I, Sebire, NJ, Man, JA, Brownbill, P, Heazell, AE. Systematic review of placental pathology reported in association with stillbirth. Placenta 2014;35:552–62. https://doi.org/10.1016/j.placenta.2014.05.011.Search in Google Scholar PubMed
16. Gardella, B, Dominoni, M, Caporali, C, Cesari, S, Fiandrino, G, Longo, S, et al.. Placental features of fetal vascular malperfusion and infant neurodevelopmental outcomes at two years of age in severe fetal growth restriction. Am J Obstet Gynecol 2021;225:413.e1–11. https://doi.org/10.1016/j.ajog.2021.03.037.Search in Google Scholar PubMed
17. Townsend, R, Sileo, FG, Allotey, J, Dodds, J, Heazell, A, Jorgensen, L, et al.. Prediction of stillbirth: an umbrella review of evaluation of prognostic variables. Br J Obstet Gynaecol 2021;128:238–50. https://doi.org/10.1111/1471-0528.16510.Search in Google Scholar PubMed
18. Weignberg, D. Human placenta project [Internet]. Available from: https://www.nichd.nih.gov/; https://www.nichd.nih.gov/research/supported/HPP/default [Accessed 11 Jun 2020].Search in Google Scholar
19. Barda, G, Bar, J, Mashavi, M, Schreiber, L, Shargorodsky, M. Insulin treatment is associated with improved fetal placental vascular circulation in obese and non-obese women with gestational diabetes mellitus. Front Endocrinol 2019;10:84. https://doi.org/10.3389/fendo.2019.00084.Search in Google Scholar PubMed PubMed Central
20. Hassan, A, Meah, VL, Davies, GA, Davenport, MH, Siassakos, D. Modify, don’t stop! Time to reconsider the ‘relative’ and ‘absolute’ contraindications to physical activity in pregnancy: an opinion piece. Br J Obstet Gynaecol 2022;129:331–5. https://doi.org/10.1111/1471-0528.16879.Search in Google Scholar PubMed
© 2022 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Editorials
- Preventing stillbirth: risk factors, case reviews, care pathways
- Managing stillbirth: taking care to investigate the cause and provide care for bereaved families
- Epidemiology and Risk Factors
- Spatial dynamics of fetal mortality and the relationship with social vulnerability
- Stillbirth occurrence during COVID-19 pandemic: a population-based prospective study
- The effect of the Covid pandemic and lockdown on stillbirth rates in a South Indian perinatal centre
- Stillbirths preceded by reduced fetal movements are more frequently associated with placental insufficiency: a retrospective cohort study
- The prevalence of and risk factors for stillbirths in women with severe preeclampsia in a high-burden setting at Mpilo Central Hospital, Bulawayo, Zimbabwe
- Surveillance and Prevention
- Perinatal mortality audits and reporting of perinatal deaths: systematic review of outcomes and barriers
- Stillbirth diagnosis and classification: comparison of ReCoDe and ICD-PM systems
- Facility-based stillbirth surveillance review and response: an initiative towards reducing stillbirths in a tertiary care hospital of India
- Impact of introduction of the growth assessment protocol in a South Indian tertiary hospital on SGA detection, stillbirth rate and neonatal outcome
- Evaluating the Growth Assessment Protocol for stillbirth prevention: progress and challenges
- Prospective risk of stillbirth according to fetal size at term
- Understanding the Pathology of Stillbirth
- Placental findings in singleton stillbirths: a case-control study from a tertiary-care center in India
- Abnormal placental villous maturity and dysregulated glucose metabolism: implications for stillbirth prevention
- Comparison of prenatal central nervous system abnormalities with postmortem findings in fetuses following termination of pregnancy and clinical utility of postmortem examination
- Cardiac ion channels associated with unexplained stillbirth – an immunohistochemical study
- Viral infections in stillbirth: a contribution underestimated in Mexico?
- Audit and Bereavement Care
- Investigation and management of stillbirth: a descriptive review of major guidelines
- Delivery characteristics in pregnancies with stillbirth: a retrospective case-control study from a tertiary teaching hospital
- Perinatal bereavement care during COVID-19 in Australian maternity settings
- Beyond emotional support: predictors of satisfaction and perceived care quality following the death of a baby during pregnancy
- Stillbirth aftercare in a tertiary obstetric center – parents’ experiences
Articles in the same Issue
- Frontmatter
- Editorials
- Preventing stillbirth: risk factors, case reviews, care pathways
- Managing stillbirth: taking care to investigate the cause and provide care for bereaved families
- Epidemiology and Risk Factors
- Spatial dynamics of fetal mortality and the relationship with social vulnerability
- Stillbirth occurrence during COVID-19 pandemic: a population-based prospective study
- The effect of the Covid pandemic and lockdown on stillbirth rates in a South Indian perinatal centre
- Stillbirths preceded by reduced fetal movements are more frequently associated with placental insufficiency: a retrospective cohort study
- The prevalence of and risk factors for stillbirths in women with severe preeclampsia in a high-burden setting at Mpilo Central Hospital, Bulawayo, Zimbabwe
- Surveillance and Prevention
- Perinatal mortality audits and reporting of perinatal deaths: systematic review of outcomes and barriers
- Stillbirth diagnosis and classification: comparison of ReCoDe and ICD-PM systems
- Facility-based stillbirth surveillance review and response: an initiative towards reducing stillbirths in a tertiary care hospital of India
- Impact of introduction of the growth assessment protocol in a South Indian tertiary hospital on SGA detection, stillbirth rate and neonatal outcome
- Evaluating the Growth Assessment Protocol for stillbirth prevention: progress and challenges
- Prospective risk of stillbirth according to fetal size at term
- Understanding the Pathology of Stillbirth
- Placental findings in singleton stillbirths: a case-control study from a tertiary-care center in India
- Abnormal placental villous maturity and dysregulated glucose metabolism: implications for stillbirth prevention
- Comparison of prenatal central nervous system abnormalities with postmortem findings in fetuses following termination of pregnancy and clinical utility of postmortem examination
- Cardiac ion channels associated with unexplained stillbirth – an immunohistochemical study
- Viral infections in stillbirth: a contribution underestimated in Mexico?
- Audit and Bereavement Care
- Investigation and management of stillbirth: a descriptive review of major guidelines
- Delivery characteristics in pregnancies with stillbirth: a retrospective case-control study from a tertiary teaching hospital
- Perinatal bereavement care during COVID-19 in Australian maternity settings
- Beyond emotional support: predictors of satisfaction and perceived care quality following the death of a baby during pregnancy
- Stillbirth aftercare in a tertiary obstetric center – parents’ experiences

