Abstract
Context
There is currently no clinical research investigating the effect of osteopathic manipulation on the milk supply of lactating patients. Herbal and prescription galactagogues are limited and have the potential for serious side effects.
Objectives
The objective of this study was to determine whether osteopathic manipulative treatment (OMT) can increase milk supply in lactating people with low milk supply (hypogalactia).
Methods
The patients presented in this series participated in an Institutional Review Board (IRB)-approved prospective pilot study. All participants were aged 18–40 years old and 2–28 weeks postpartum with the desire to exclusively breastfeed with infants who weighed at least 2,500 g at birth. At 1 h, the measured milk production was <1 oz expressed through a hospital-grade pump. Participants were ineligible if they were utilizing prescription galactagogues or had a contraindication to OMT. They were treated with an OMT protocol plus ad lib OMT once a week for 4 weeks. The study was suspended and ultimately closed due to the SARS-CoV-2 pandemic.
Results
All three participants demonstrated an increase in milk production from baseline at each visit. Given the small number of participants, these results are not statistically significant. Power analysis calculated a need for 10 subjects. Therefore, these patients are presented as a case series.
Conclusions
These results show promise for the use of osteopathic manipulation to increase human milk production. A study with a larger number of participants is needed.
Human milk is the perfect infant food, and the majority of women in the United States initiate breastfeeding at birth [1]. However, only a small percentage meet the recommendation for exclusive breastfeeding to 6 months of age [1], [2], [3], [4]. Concerns about inadequate milk supply, perceived insufficient infant weight gain, and difficulty with breastfeeding are among the most commonly cited reasons for earlier-than-intended cessation of breastfeeding [5]. Osteopathic manipulative treatment (OMT), as outlined by Andrew Taylor Still, MD, DO, is described to optimize bodily function through the normalization of structure [6]. Because producing sufficient milk supply to adequately nourish one’s infant should be the biological norm, the investigators hypothesized that utilizing osteopathic manipulation to normalize structure and function could increase milk supply when inadequate.
There appear to be just two references in the osteopathic literature regarding the use of OMT to affect milk supply. Still wrote that there are no issues regarding a shortage in milk supply “where all ribs, vertebrae, and the clavicles are in normal adjustment.” [7] Many decades later, Keller [8] mentioned that treating thoracic vertebrae will help patients “short of breast milk.”
There is no prior research on the use of osteopathic manipulative treatment (OMT) for the purpose of increasing human milk quantity. Other manual medicine practices have demonstrated an increase in milk supply including acupuncture [9], back and breast massage [10], 11], and reflexology [12].
Reported herbal galactagogues include anise, basil, blessed thistle, dandelion, fennel seeds, fenugreek, goat’s rue, marshmallow, moringa leaf, milk thistle, millet, oats, seaweed, shatavari, and torbangun [13]. Despite their use across many cultures, there is little scientific evidence regarding their safety or efficacy [13]. Prescription galactagogues include: domperidone and metoclopramide [13]. Domperidone is commonly utilized worldwide but has a risk for QT prolongation and is not FDA-approved; therefore, it is unavailable in the United States. Metoclopramide is available, but it carries the risk of tardive dyskinesia and drug-induced Parkinsonism and is therefore not recommended for long-term use [13], 14]. Both of these medications increase prolactin, yet it is not known if some or all patients with low milk supply have low levels of prolactin [13], 15].
This authors of this paper initiated this study to determine if OMT could increase milk supply in lactating parents with low milk supply (hypogalactia). This phenomenon had been noted to occur in their practice, and the study was developed to attempt to quantify the effect in a scientific manner.
Methods
The patients reported participated in the Osteopathic Manipulation to Increase Lactation Quantity (OMILQ) Study (ClinicalTrials.gov number NCT03875794) from January 2019 to March 2020. Five subjects were recruited, and three met the inclusion criteria and completed the study prior to the trial being suspended due to the emergence of the SARS-CoV-2 pandemic. The co-investigators both left the sponsoring institution while the trial was suspended, and it was closed as incomplete. The patients in this case series are the three subjects that completed the study. Prior to participation, all subjects signed written informed consent in the presence of a study doctor.
To be eligible for inclusion, potential participants had to be between the ages of 18 and 40 years old, be between 2 and 28 weeks postpartum, and have the desire to exclusively breastfeed. The infant’s birth weight was to be at least 2,500 g. If they were providing human milk to more than one child, the children must be the same age, i.e., twins, as opposed to an infant and a toddler. The mother’s milk production measured after a 1-h waiting period in the study office was to be <1 oz per infant.
Participants were ineligible if they were utilizing prescriptive galactagogues: domperidone or metoclopramide [13]. Subjects with a history of breast surgery or insufficient glandular tissue were excluded as well because these are known intramammary structural reasons for low milk supply [13]. Participants with current malignancy, pulmonary embolism, deep vein thrombosis, or a medical condition resulting in increased intracranial pressure were excluded, because these are relative contraindications to the osteopathic manipulation techniques that were likely to be utilized [16].
For each milk expression required by the study, participants expressed milk in the study office with the same study supplied Medela Symphony® double breast pump for 15 min or until milk stopped flowing within 15 min. Participants were fitted with appropriately sized pump-flanges and oriented to the pump settings by the study physician. All additional single-user pumping parts were supplied and utilized only by the assigned participant for each of their milk expressions. Subjects were provided with a pumping bra for convenience, if desired. Milk was collected in clean bottles attached to the pump and then weighed on a scientific scale. All expressed milk was taken home by the subject at the conclusion of each visit.
All study visits occurred between 13:00 and 17:00. Once the subject completed their initial milk expression, a 1-h timer was started and they were assessed for somatic dysfunction and treated with OMT. Treatments typically took between 10 and 15 min.
Participants were treated once a week for 4 weeks with a protocol. The protocol advised the treatment of the following structures if somatic dysfunction was present: reciprocal tension membrane balanced membranous tension, venous sinus drainage, clavicle balanced ligamentous tension, direct thoracic inlet release, pectoral traction, Cooper’s ligaments and breast myofascial release, T3-T5 balanced ligamentous tension, rib 1 Still technique, ribs 2–6 balanced ligamentous tension, abdominal diaphragm ligamentous articular strain, and modified pedal pump. Additionally, the neuromusculoskeletal medicine (NMM) board-certified study doctors (EC and AO) treated other somatic dysfunctions that they identified as needing treatment.
Patient cases
Patient #1
The first patient was 29 years old and was 2 weeks and 3 days postpartum. She had delivered an infant weighing 2,580 g at 37 weeks gestation via Cesarian section after failing induction of labor due to preeclampsia. Risk factors for breastfeeding difficulty included: early-term gestation, Cesarian section, preeclampsia, and primiparous status. She had no other relevant medication history or abnormal physical examination findings. After four treatments (Table 1), she had a 350 % increase in milk production from the initial visit to the final visit (Figure 1).
Regions of treatment and technique utilized.
| Region | Week 1 | Week 2 | Week 3 | Week 4 | |
|---|---|---|---|---|---|
| Subject 1 | Head | OCMM | OCMM | OCMM | OCMM |
| Cervical | FPR, BLT | BLT, soft tissue | |||
| Thoracic | MFR, BLT | MFR, BLT | MFR, BLT | BLT, HVLA | |
| Ribs | Still, BLT, HVLA | Still, BLT | Still, BLT | Still, BLT, HVLA | |
| Lumbar | |||||
| Sacrum | Still | ||||
| Pelvis | Still | Still | Still | ||
| Upper extremity | Pec traction, BLT | Pec traction, BLT | Pec traction, BLT | Pec traction, BLT | |
| Lower extremity | |||||
| Viscera/lymphatics | LAS, MFR, pedal pump, visceral | LAS, MFR, pedal pump | LAS, MFR, pedal pump, | LAS, MFR, pedal pump, | |
| Subject 2 | Head | OCMM | OCMM | OCMM | OCMM |
| Cervical | MFR | MFR | MFR | ||
| Thoracic | BLT, MFR | BLT, MFR | BLT, MFR | BLT, MFR | |
| Ribs | Still, BLT | BLT | Still, BLT | Still, BLT | |
| Lumbar | Still | Still | Still | ||
| Sacrum | OCM | Still | Still | ||
| Pelvis | Still | Still | Still | MFR | |
| Upper extremity | Pec traction, BLT | Pec traction, BLT | Pec traction, BLT | Pec traction, BLT | |
| Lower extremity | MFR | ||||
| Viscera/lymphatics | LAS, MFR, pedal pump, visceral | LAS, MFR, visceral | MFR | LAS, MFR, pedal pump, visceral | |
| Subject 3 | Head | OCMM | OCMM | OCMM | OCMM |
| Cervical | MFR | BLT, MFR | BLT | MFR | |
| Thoracic | MFR, BLT | BLT, HVLA | BLT | Mlt, MFR | |
| Ribs | BLT, MFR | Still, BLT, HVLA | Still | BLT | |
| Lumbar | Still | Still | Still | ||
| Sacrum | Still | Still, BLT | Still | ||
| Pelvis | Still | Still | |||
| Upper extremity | Pec traction, BLT | Pec traction | Pec traction | Pec traction, BLT | |
| Lower extremity | |||||
| Viscera/lymphatics | LAS, MFR | LAS, pedal pump | MFR, pedal pump | LAS |
-
BLT, balanced ligamentous tension; FPR, facilitated positional release; HVLA, high velocity, low amplitude; LAS, ligamentous articular strain; MFR, myofascial release; OCMM, osteopathic cranial manipulative medicine; Pec traction, pectoral traction; Pedal pump, modified pedal lymphatic technique; Still, Still technique; Visceral, Barral style visceral technique.
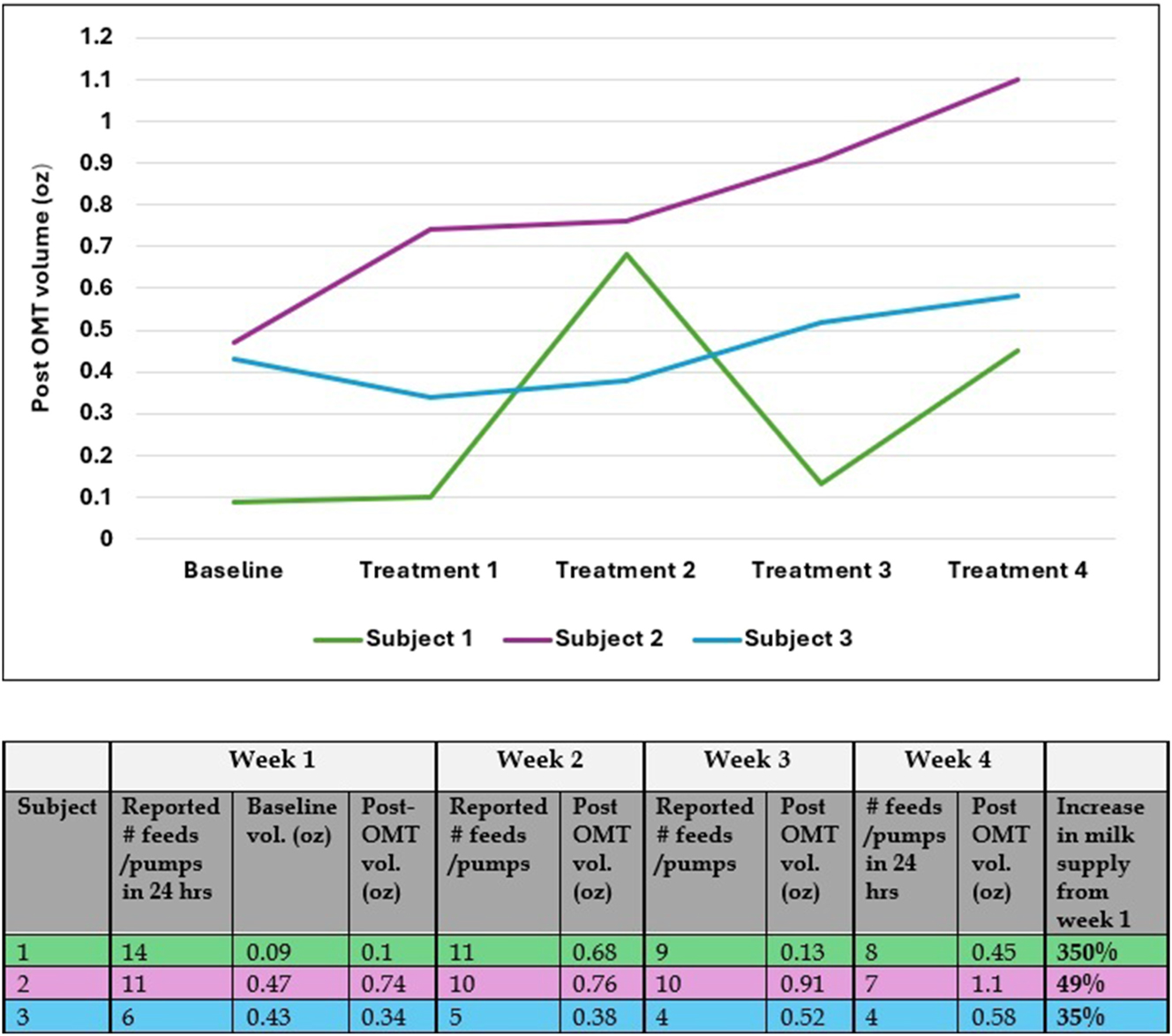
Measured milk volumes.
Patient #2
The second patient was 37 years old and was 2 weeks postpartum. She delivered an infant weighing 2,721 g at 36 weeks through spontaneous vaginal delivery. Risk factors for difficulty breastfeeding included: advanced maternal age, late-preterm gestation, obesity, and primiparous status. She had no other relevant medication history or abnormal physical examination findings. After four treatments (Table 1), she had a 49 % increase in milk production from the initial visit to the final visit (Figure 1).
Patient #3
The third patient was 37 years old and was 3 weeks and 6 days postpartum. She delivered an infant weighing 2,551 g at 36 weeks and 5 days through Cesarean section. The reason for the Cesarean section was unfortunately not noted. Risk factors for difficulty breastfeeding included: advanced maternal age, late-preterm gestation, and primiparous status. She had no other relevant medication history or abnormal physical examination findings. After four treatments (Table 1), she had a 35 % increase in milk production from the initial visit to the final visit (Figure 1).
None of the participants experienced any adverse events or treatment complications after OMT.
Discussion
This small series of patients demonstrated an increase in milk supply from baseline in all three subjects after four weekly treatments with OMT. There is no prior research investigating the use of OMT to increase human milk production. Other manual medicine modalities, including acupuncture, back and breast massage, and reflexology, have been shown to increase human milk production [9], [10], [11], [12]. In addition to being insufficiently powered, there are multiple limitations to this study.
The method of milk measurement in this case series is imperfect. In studies seeking to quantify milk volume, several methods have been employed including: pre- and postdirect breastfeeding infant weights plus measurement of expressed milk volume over 24 h and computer-based pre- and postexpression of milk breast volume measurement [17], 18]. These methods were specifically not utilized because they rely on the infant to be a good extractor of milk. As poor infant feeding is itself a risk factor for low milk supply, methods relying on infant extraction were deemed undesirable [13]. Therefore, expression with a hospital-grade pump was selected, although admittedly there are some people who do not respond well to an electric pump [13]. Additionally, a lengthier assessment of milk production would be beneficial, such as over 24 h or several days, because the measurements in this study were single points in time.
The decision was made to enroll subjects starting at 2 weeks postpartum because full milk supply can be reached by day 14, although milk volume can increase from day 14 to 28 with increased milk extraction [19], 20]. Additionally, the classic definition of low milk supply in the lactation community is insufficient milk to allow expected infant growth on the World Health Organization (WHO) standards growth chart [21]. The American Academy of Pediatrics (AAP) guidelines indicate that breastfed infants should be back to their birth weight by 10–14 days old [22]. Therefore, it is largely presumed that the majority of breastfed infants who have not achieved this weight gain are likely either not extracting milk well or there is insufficient milk available [21]. Additionally, it is more common to have hyperlactation in the initial postpartum weeks as milk production is hormonally driven and then milk supply downregulates in galactopoesis (formerly known as lactogenesis III) to match infant demand [21], 23].
Once mature milk production is achieved generally starting around postpartum day 9 (galactopoesis), milk production shifts from an endocrine process to an autocrine process reliant primarily on supply and demand [21]. One of the keys to maintaining full milk supply is sufficient and frequent milk extraction [13]. The number of times that milk needs to be removed from the breasts to maintain the needed milk supply varies from person to person, depending on breast storage capacity, but averages 8–12 times per day [24]. Among the patients treated, only the first maintained what was likely sufficient breastfeeding frequency to support full milk production by the fourth week of the study. She also started with the lowest volume at baseline and had the most significant increase in milk quantity. This demonstrates that OMT may be able to optimize the normal biological function of the body, but OMT cannot overcome otherwise suboptimal feeding practices.
The proposed mechanism for osteopathic manipulation to increase milk supply is through increased blood supply to the breast, increased lymphatic drainage, and decreased viscerosomatic reflexes. This pilot study was designed to follow a flexible protocol in that specific common somatic dysfunctions were treated, when possible, with a predetermined technique. This was done in an attempt to make the outcome replicable. Both physicians treating the patients are board-certified in NMM and utilized their clinical judgment to diagnose and treat somatic dysfunctions. This preserves the true spirit of osteopathy by treating the individual and is a strength of the study.
There are multiple options for a future trial with a larger sample size. Because the lack of a control group is a limitation, a crossover control with a waiting period could be considered. Another option would be to compare a standard of care group receiving lactation counseling from an International Board-Certified Lactation Consultant (IBCLC) to a group receiving this same counseling in addition to OMT.
Conclusions
Although the sample size of this case series is small, there is no other record in the literature investigating the use of OMT to improve milk supply in patients with hypogalactia. These cases indicate that there is an application for osteopathic manipulation in supporting the breastfeeding dyad that would benefit from a larger clinical trial.
Acknowledgments
The authors would like to thank Xiawei Zhong, DO (ONMM3 Residency Faculty at AdventHealth East Orlando) for her assistance in record review and data compilation.
-
Research ethics: This study was approved by Florida Hospital (now AdventHealth) Institutional Review Board (#1174025). ClinicalTrials.gov registry: #NCT03875794.
-
Informed consent: All participants in this study provided written informed consent prior to participation.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: Dr. Conaway has received speaker honoraria from the American Academy of Osteopathy, the Florida Osteopathic Medical Association, the South Carolina Osteopathic Medical Society, Osteopathic Physicians and Surgeons of California, and Osteopathy’s Promise to Children. She also received a single consultation fee from Willow Breast Pumps in 2022. Dr. O’Donnell has received speaker honoraria from the Florida Osteopathic Medical Association.
-
Data availability: All relevant data are available from the corresponding author upon reasonable request.
References
1. Centers for Disease Control and Prevention. Breastfeeding report card. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/data/reportcard.htm [Accessed 31 August 2022].Suche in Google Scholar
2. World Health Organization. Breastfeeding. World Health Organization; 2021. Available from: https://www.who.int/health-topics/breastfeeding#tab=tab_2.Suche in Google Scholar
3. Centers For Disease Control and Prevention. Recommendations and benefits. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/nutrition/infantandtoddlernutrition/breastfeeding/recommendationsbenefits.html.Suche in Google Scholar
4. Meek, JY, Noble, L. Section on breastfeeding. Policy statement: breastfeeding and the use of human milk. Pediatrics 2022;150. https://doi.org/10.1542/peds.2022-057988.Suche in Google Scholar PubMed
5. Odom, EC, Li, R, Scanlon, KS, Perrine, CG, Grummer-Strawn, L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726–32. https://doi.org/10.1542/peds.2012-1295.Suche in Google Scholar PubMed PubMed Central
6. Still, AT. Philosophy and mechanical principles of osteopathy. Kansas City, MO: Hudson-Kimberly Pub Co; 1902.Suche in Google Scholar
7. Still, AT. Osteopathy, research and practice. Kirksville, MO: A.T. Still; 1910.Suche in Google Scholar
8. Keller, JA. Osteopathic medicine. AAO J; Fall 1993. Available from: https://ostemeddr.contentdm.oclc.org/digital/collection/myfirst/id/9875/rec/1.Suche in Google Scholar
9. Bao, QN, Yin, ZH, Zhou, YF, Li, YQ, Zhang, XY, Xia, MZ, et al.. Efficacy and safety of acupuncture for postpartum hypogalactia: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2024;19:e0303948. https://doi.org/10.1371/journal.pone.0303948.Suche in Google Scholar PubMed PubMed Central
10. Erci̇Yas, ŞK, Kavlak, O. The effect of back and breast massage on the amount of milk and anxiety level of mothers with preterm birth: a randomized controlled study. J Neonatal Nurs 2023;30:251–7. https://doi.org/10.1016/j.jnn.2023.10.003.Suche in Google Scholar
11. Katmini, K, Sholichah, NM. Lactation massage for increasing breast milk production in postpartum mothers. J Qual Publ Health 2020;4:104–13. https://doi.org/10.30994/jqph.v4i1.168.Suche in Google Scholar
12. Mohammadpour, A, Valiani, M, Sadeghnia, A, Talakoub, S. Investigating the effect of reflexology on the breast milk volume of preterm infants’ mothers. Iran J Nurs Midwifery Res 2018;23:371–5. https://doi.org/10.4103/ijnmr.IJNMR_175_16.Suche in Google Scholar PubMed PubMed Central
13. Brodribb, W. ABM clinical protocol #9: use of galactogogues in initiating or augmenting maternal milk production, second revision 2018. Breastfeed Med 2018;13:307–14. https://doi.org/10.1089/bfm.2018.29092.wjb.Suche in Google Scholar PubMed
14. Alaven Pharmaceutical LLC. Highlights of prescribing information; 2010. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021793s008lbl.pdf.Suche in Google Scholar
15. Geddes, DT, Gridneva, Z, Perrella, SL, Mitoulas, LR, Kent, JC, Stinson, LF, et al.. 25 Years of research in human lactation: from discovery to translation. Nutrients 2021;13:3071. https://doi.org/10.3390/nu13093071.Suche in Google Scholar PubMed PubMed Central
16. Kuchera, ML. Effectiveness and safety of osteopathic manipulatve treatment. In: Seffinger, DM, editor. Foundations of osteopathic medicine, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2018:1531–42 pp.Suche in Google Scholar
17. Nommsen-Rivers, L, Thompson, A, Riddle, S, Ward, L, Wagner, E, King, E. Feasibility and acceptability of metformin to augment low milk supply: a pilot randomized controlled trial. J Hum Lactation 2019;35:261–71. https://doi.org/10.1177/0890334418819465.Suche in Google Scholar PubMed PubMed Central
18. Daly, SEJ, Kent, JC, Huynh, DQ, Owens, R, Alexander, B, Ng, K, et al.. The determination of short-term breast volume changes and the rate of synthesis of human milk using computerized breast measurement. Exp Physiol 1992;77:79–87. https://doi.org/10.1113/expphysiol.1992.sp003584.Suche in Google Scholar PubMed
19. Saint, L, Smith, M, Hartmann, PE. The yield and nutrient content of colostrum and milk of women from giving birth to 1 month post-partum. Br J Nutr 1984;52:87–95. https://doi.org/10.1079/bjn19840074.Suche in Google Scholar PubMed
20. Perrella, S, Gridneva, Z, Lai, CT, Stinson, L, George, A, Bilston-John, S, et al.. Human milk composition promotes optimal infant growth, development and health. Semin Perinatol 2021;45:151380. https://doi.org/10.1016/j.semperi.2020.151380.Suche in Google Scholar PubMed
21. Wambach, K, Spencer, B. Breastfeeding and human lactation. Burlington, MA: Jones & Bartlett Learning; 2024.Suche in Google Scholar
22. Mcinerny, TK, Adam, HM, Campbell, DE. American Academy of Pediatrics textbook of pediatric care. Itasca, IL: American Academy of Pediatrics; 2017.Suche in Google Scholar
23. Johnson, HM, Eglash, A, Mitchell, KB, Leeper, K, Smillie, CM, Moore-Ostby, L, et al.. ABM clinical protocol #32: management of hyperlactation. Breastfeed Med 2020;15:129–34. https://doi.org/10.1089/bfm.2019.29141.hmj.Suche in Google Scholar PubMed
24. Mohrbacher, N. The magic number and long-term milk production. Clin Lactation 2011;2:15–8. https://doi.org/10.1891/215805311807011827.Suche in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

