Determining the effects of social media engagement on surgery residents within the American College of Osteopathic Surgeons
-
Vincent S. Alexander
, Bebe Eke
, Andrew Greek
, Bracken Burns
Abstract
Context
The widespread adoption of social media has transformed how individuals connect in medicine. This study explores how social media can be utilized as a conduit to connect osteopathic medical students and residents. By examining how these digital connections can support professional development, this study investigates social media’s role as a potential foundation for a mentorship program, fostering guidance, support, and career insights for osteopathic medical students within the surgical field.
Objectives
This study aimed to evaluate the effectiveness of “X” (formerly Twitter) in networking between osteopathic medical students and surgical residents, specifically assessing engagement rates and the potential of social media as a tool for mentorship in the osteopathic surgical community.
Methods
The Accreditation Council on Graduate Medical Education (ACGME)-approved surgical programs that the American College of Osteopathic Surgeons (ACOS) represents were identified online. Doctor of Osteopathic Medicine (DO) residents were identified retrospectively through an online search of publicly available data. Residents and programs were searched through X, and account handles were collected. Residents were contacted through X by direct messaging and subsequently directly commented in the initial ACOS Medical Student Section (ACOS-MSS) message. Descriptive statistics along with the chi-square and Fisher’s exact statistical tests were utilized for demographic and categorical variable analysis, respectively.
Results
There are 1179 DO surgical residents in ACGME programs, with 84.8 % of those being General Surgery residents. Among residents, 75 % of Cardiothoracic (CT) Surgery, 46.4 % of Urology, 28.6 % of Neurosurgery, 17.3 % of General Surgery, and 11.11 % of Plastic Surgery residents have X accounts. Specific surgical subspecialties are more likely to have an X account in comparison to General Surgery, including CT Surgery (odds ratio [OR], 11.13; p=0.02), Urology (OR, 4.13; p<0.0001), and Neurosurgery (OR, 0.842; p=0.047). After multiple attempts, 0 % of Plastic Surgery, 2.9 % of General Surgery, 7.8 % of Urology, 18.8 % of Neurosurgery, and 33.3 % of CT Surgery residents signed up for the mentorship program, totaling 13 residents.
Conclusions
The study reveals low social media engagement via X among osteopathic surgical residents, with notable variation across surgical specialties. This limited engagement suggests exploring and refining social media strategies that foster mentorship connections within the osteopathic surgical community. Future studies should examine other social media platforms and alternative engagement approaches to enhance the reach and impact of mentorship initiatives, ultimately supporting osteopathic medical students as they navigate career paths in surgery.
As of 2023, roughly 7 out of every 10 Americans state that they utilize social media [1]. This pervasive use of social media has transformed numerous fields, including research and education, enabling unprecedented access to collaborative networks. The widened access to research collaboration through social media has led to a paradigm shift in how research is conducted, with an increasing number of research projects examining this effect [2], 3]. The traditional mentorship model in medical education involves face-to-face interactions, formalized mentorship programs, and hierarchical structures. Mentorship is a critical component for medical students and is highly valued early in their medical careers [4]. Strong relationships with mentors seem to impact a student’s decision concerning residency programs, their field of practice, and even their career trajectory [5]. While recent studies have demonstrated a lack of mentorship across all medical schools, osteopathic medical schools may have a stronger deficit [5], 6]. This may be even more exaggerated for those osteopathic medical students pursuing surgery subspecialties [7], 8]. Although there has been an increase in osteopathic students applying to surgical subspecialties, their match rate in all surgical subspecialties remains significantly lower than their allopathic counterparts [9]. Multiple actions to address these discrepancies may include students seeking opportunities in research or showing early interest and dedication in a specific surgical subspecialty. However, the common theme in these factors may be a lack of mentorship to students from osteopathic surgeons and surgical residents who have faced these same barriers [10].
This study is the first of a two-part series that will investigate the utility of utilizing a social media platform, “X” (formerly Twitter), to engage with osteopathic surgery residents. Subsequently, this will be developed to analyze the impact of a pilot resident mentorship program that establishes connections between residents and students who are members of the American College of Osteopathic Surgeons (ACOS). This initial study aims to examine social media’s effects on engaging surgical residents.
Methods
Data collection
Osteopathic residents training in the 2023–2024 academic year from surgical and surgical subspecialties falling under the ACOS were identified retrospectively through a search of publicly available online data. A list of all Accreditation Council on Graduate Medical Education (ACGME)-approved integrated Cardiothoracic (CT) Surgery, General Surgery, integrated Plastic Surgery, Urology, and Neurologic Surgery programs was identified from the ACGME’s website. These ACGME residency programs’ official websites were found online, with the identification of all Allopathic Medicine (MD), Doctor of Osteopathic Medicine (DO), and Bachelor of Medicine, Bachelor of Surgery (MBBS) residents comprising the programs identified. Up-to-date official residency program websites – including 270 out of 360 General Surgery residency programs, 27 out of 33 integrated CT residency programs, 135 out of 151 Urology residencies, 86 out of 87 integrated Plastic Surgery residencies, and 115 out of 117 Neurosurgery residencies – were reviewed. Social media handles were identified for residency programs and their DO residents through X and Google search functions. This was completed from August 2023 to November 2023. Solicitation was tweeted to all accounted DO residents so they could sign up to become mentors through the ACOS Medical Student Section (ACOS-MSS) official X account (Appendix). This was completed in December 2023. Then, those residents who still had not signed up were messaged privately through X to solicit enrollment in the mentorship program if they had not already signed up. Each resident was also directly contacted through a direct tweet. All resident enrollments were recorded and categorized by specialty. Residents were contacted through X by direct messaging and subsequently directly commented in the initial ACOS-MSS message. Once enrolled, the residents were matched with mentees according to their specialties, interests, and goals, creating a structured framework for ongoing mentorship interactions. Engagement in this study was defined across multiple levels: first, whether residents were contactable through X, which depended on their account settings and platform restrictions; second, whether they responded to initial outreach efforts, which indicated their awareness and potential interest in the mentorship program; and finally, whether they ultimately signed up for the program, marking active participation.
Statistical analysis
Descriptive statistics were utilized for demographic analysis. Where appropriate, categorical variables were compared utilizing the chi-square test or Fisher’s exact test. Statistical analysis and generation of graphs were performed utilizing GraphPad Prism version 10.1.2 for Windows (San Diego, CA).
Results
The data analyzed 1,179 DO surgical residents across five specialties (General Surgery, Urology, CT Surgery, Neurosurgery, and Plastic Surgery) that observed the distribution and impact of social media engagement, specifically on X. The highest proportion of X accounts was seen in CT Surgery, in which 75 % of residents (3 out of 4) held accounts, significantly greater than Urology (46.4 %, or 51 out of 110), Neurosurgery (28.6 %, or 16 out of 56), General Surgery (17.3 %, or 173 out of 1,000), and Plastic Surgery (11.1 %, or 1 out of 9) (Figure 1). It is worth noting that the number of residents in Plastic Surgery (9) and CT Surgery (4) with X accounts were notably lower than that of other specialties.
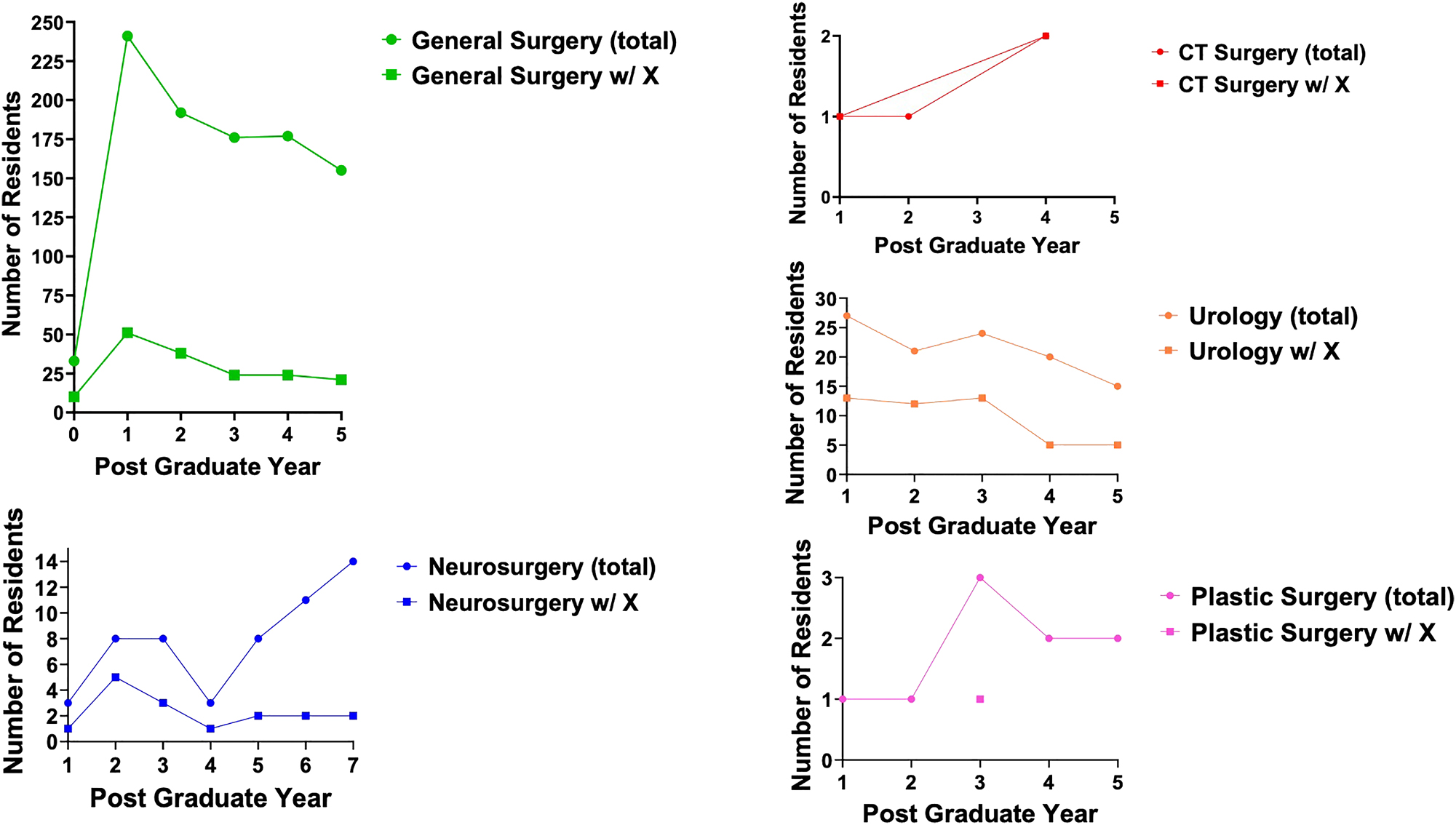
The number of residents training in surgical specialties over postgraduate years. The graphs show the number of residents in various surgical specialties (General Surgery in green, CT Surgery in red, Urology in orange, Neurosurgery in blue, and Plastic Surgery in pink) by postgraduate year. Each plot differentiates between total residents (circles) and those with an X account (squares). Trends indicate variability in resident numbers across specialties and years, comparing total residents vs. those with X accounts. CT, cardiothoracic; w/, with.
X has restrictions for accounts that are not following nor subscribed to X’s premium services; thus, the ability to contact residents with X accounts was limited. The ability to be contacted was analyzed, and it was found that Neurosurgery residents had the highest contact rate at 50 %, with 8 out of 16 residents reachable. This was significantly higher than General Surgery, in which only 3.5 % (6 out of 173) could be contacted. Engagement activities revealed that direct tweeting on X proved to be an effective strategy for Neurosurgery, with a high signup rate postcomment.
There were significant variances of the use of X across specialties. The odds of having an X account were notably higher in subspecialties than in General Surgery, with CT Surgery having an odds ratio (OR) of 11.13 (p=0.02), Urology with an OR of 4.132 (p<0.0001), and Neurosurgery with an OR of 1.943 (p=0.047) (Figure 2).
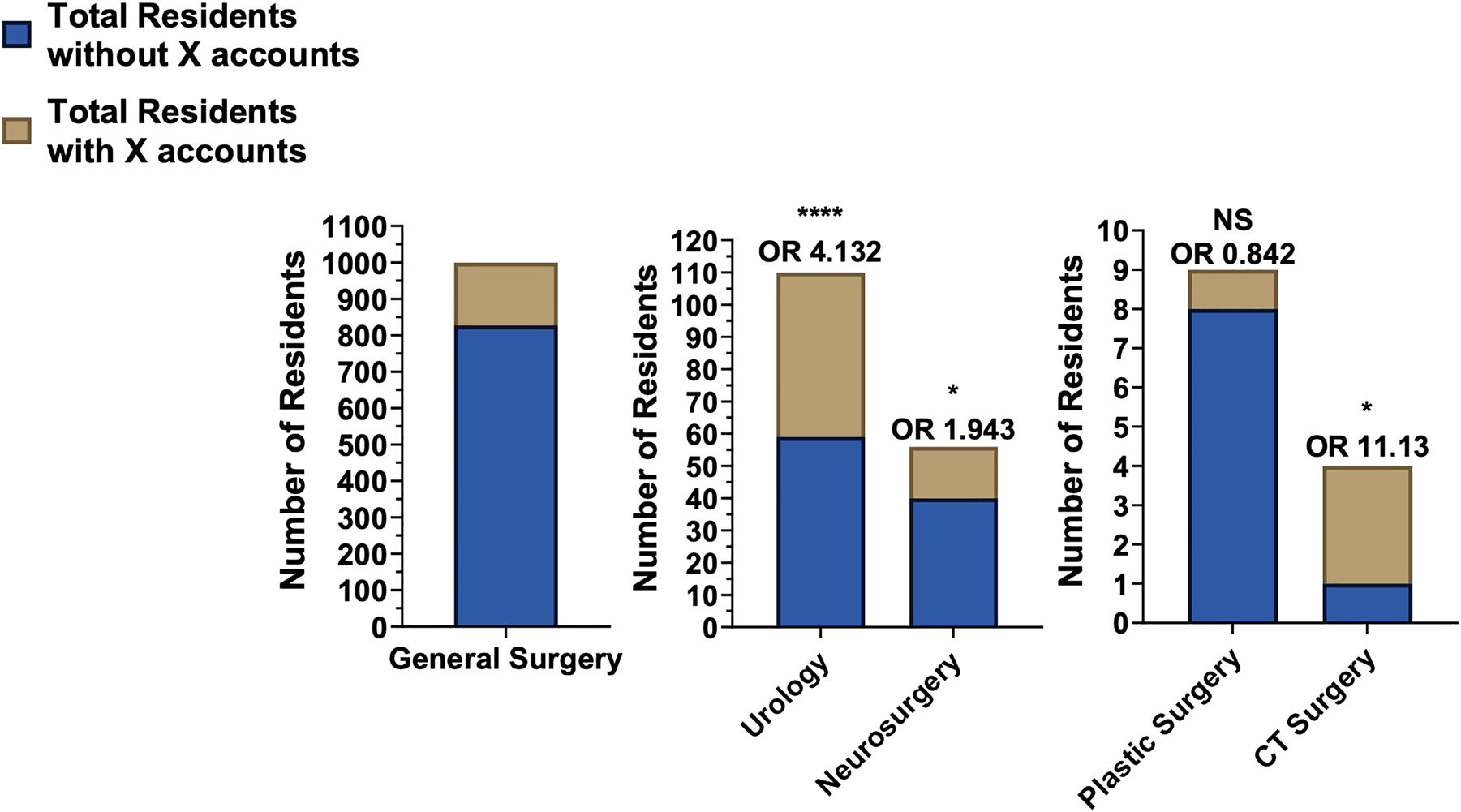
The total number of residents in various surgical specialties with and without X. Graphs are divided into those without X accounts (blue) and those with X accounts (brown). The OR was determined for each specialty as compared to General Surgery. CT, Cardiothoracic; NS, nonsignificant; OR, odds ratio.
There were also significant engagement differences, with CT Surgery showing an 18.38 times likelihood of engaging through X, although this was not statistically significant (p=0.099). Active engagement revealed that out of all of the residents with X accounts, 33.3 % (n=1) of CT Surgery, 18.6 % (n=3) of Neurosurgery, 7.9 % (n=4) of Urology, and 2.9 % (n=5) of General Surgery residents signed up for the mentorship program, with no Plastic Surgery residents participating in the mentorship program (Table 1). Notably, General Surgery had the highest number of residents with X accounts (173), but only five of them were contactable, and only five signed up after the initial contact. However, it should be noted that 1,000 General Surgery residents were identified (Figure 3).
A summary of the data captured during the study. This table demonstrates the distribution of residents with and without X accounts across various surgical specialties, including the percentages of total residents with an X account, the percentage of those with X accounts who are contactable, and the percentage of those with X accounts who signed up.
| Total number of surgeons | No. of residents without X | No. of residents with X | % Of residents with X | % Of residents with X that are contactable | % Of residents with X who signed up | |
|---|---|---|---|---|---|---|
| General surgery | 1,000 | 827 | 173 | 17.3 % | 3.5 % | 2.9 % |
| CT surgery | 4 | 1 | 3 | 75 % | 33.3 % | 33.3 % |
| Urology | 110 | 59 | 51 | 46.4 % | 3.9 % | 7.8 % |
| Plastic surgery | 9 | 8 | 1 | 11.1 % | 0 % | 0 % |
| Neurosurgery | 56 | 40 | 16 | 28.6 % | 50 % | 18.8 % |
| Totals | 1,179 | 935 | 244 | |||
-
CT, cardiothoracic; %, percentage.
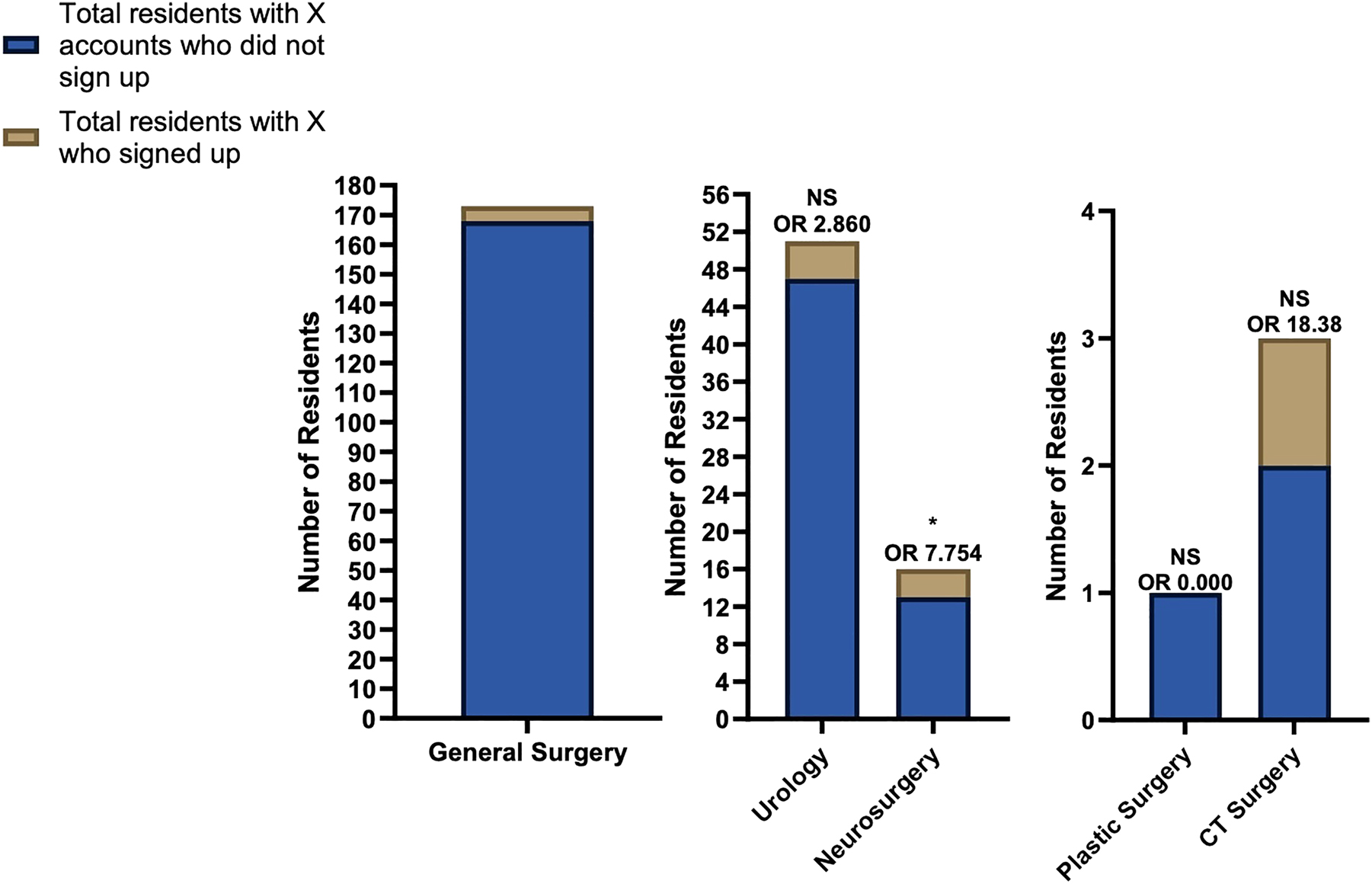
The total number of residents who joined the mentorship match program. The bar graphs distinguish residents with X accounts who did not sign up (blue) and those who signed up (brown) to be mentors. ORs were determined in comparison to general surgery. CT, cardiothoracic; NS, nonsignificant; OR, odds ratio.
Discussion
This study explored the current landscape of osteopathic surgical residents on social media, specifically X, and its potential to foster mentor–mentee relationships in the surgical disciplines. Previous studies have documented X as a frequently utilized platform by medical professionals [11]. The breadth of an X account presence parallels the increase in General Surgery residency programs with X accounts in recent years [12]. The results from our study also indicate that, overall, 20.7 % of osteopathic surgical residents have an X account, with representation from each specialty studied: General Surgery, CT Surgery, Urology, Plastic Surgery, and Neurosurgery. However, the percentage of residents with an account varied widely by specialty. CT Surgery had the highest percentage of residents with an X account at 75 %, followed by Urology at 46.4 %. Plastic Surgery had the lowest percentage with 11.1 %, and it was also the least contactable specialty.
The significant variability of X usage between specialties is noteworthy. The most notable difference exists between General Surgery and the surgical subspecialties. This discrepancy is evident in the presence of an X account and the level of engagement on X. These findings within the osteopathic surgery community corroborates with previous findings regarding surgical subspecialties more broadly.
More frequent use of social media has been found in plastic surgeons, colorectal surgeons, and head and neck surgeons compared to general surgeons [13], [14], [15], [16]. The results from this study highlight CT Surgery (OR: 11.13) and Urology (OR: 4.132) as specialties with higher ORs, suggesting that they may offer more engagement for connection and mentorship. This could be attributed partly to social media’s collaborative research opportunities [17]. Students applying to surgical subspecialties often possess a considerable number of research publications and experiences to be seen as competitive applicants [18]. This has the potential to increase the utilization of social media within these specialties as a means to pursue external and collaborative research opportunities. This may also explain the high ability for contact of Neurosurgery residents (50 %). It is of note that surgical subspecialties that historically have higher research metrics for match also had the highest percentage of sign-up for mentorship: CT Surgery (33 %) and Neurosurgery (18.8 %).
Social media, notably X for this study, presents an opportunity for osteopathic medical students to find mentors. It can facilitate mentorship by forming new mentor–mentee relationships to transcend geographic and institutional barriers, thus allowing DO students pursuing surgery to connect with mentors at institutions across the United States [19]. Social media also introduces additional opportunities for mentorship because information about networking opportunities that lead to attaining mentors is frequently disseminated on X. Furthermore, mentorship programs for various surgical specialties are often shared on X. Many students might not have otherwise encountered these opportunities without being on X.
While this phase of the study aimed to assess X engagement among DO surgical residents to establish a mentorship program, future steps will focus on evaluating the mentor–mentee pairings. Aspects of mentoring are unique to each pairing and may include factors such as advice in applying to residency and collaborative research works. Plans include conducting assessments at 3 and 6 months to help determine whether quality mentors can be recruited through X and whether mentorship is effective. Additionally, they will explore the extent to which these relationships benefit DO medical students by either strengthening their interest in surgical specialties or expanding their scholarly work to enhance competitiveness for residency. The collection of longitudinal data is necessary for understanding how sustained relationships evolve over time, and lead to measurable outcomes in student development and career progression.
Limitations
A limitation of this study is that only 13 residents signed up for the mentorship program, resulting in a small sample size. In addition, this study relies on publicly available data, presenting a limitation because the reliability of the data depends on the residency program’s diligence in updating its information annually. Not all residency programs have publicly available information about their residents, so information about all residency programs cannot be found. However, the majority of surgical residency programs have their residents present on their website. Also, it must be noted that there is an inability to fully verify whether the identified social media accounts belonged to the residents. Accounts were cross-referenced with program rosters and residency websites when possible and excluded those lacking identifiable information, such as names or institutional affiliations. However, complete verification was not feasible without direct confirmation from account holders. A limitation of this study is that certain residents who utilized X actively during medical school have since ceased utilizing the platform upon entering residency, rendering them uncontactable through this medium. This limitation restricts the accuracy of assessing mentorship interest solely based on X engagement, because non-usage does not equate to a lack of interest in mentoring. It is essential to recognize that many osteopathic surgical residents may not have an X account at all, suggesting that low engagement rates on X should not be interpreted as indicative of a general disinterest in mentoring among DO surgical residents. These factors may affect the representation of true mentorship interest within this study. Alternative methods for approaching residents, such as disseminating flyers with pictures through X or offering compensation discounts for registration at ACOS conferences, were not evaluated. Additionally, changes to the verbiage of the initial X solicitation were not made.
Conclusions
The widespread implications of social media access and use in the medical field remains relatively underexplored and will continue to be studied. However, utilizing social media as a bridge to connect mentors and mentees is an opportunity to provide medical students with insight into the surgical disciplines. Mentorship and engagement from seniors in medicine have been the foothold that has provided each new generation of surgeons. The most opportune platform for establishing this connection has yet to be established and compared. The variability in social media usage across different surgical specialties suggests that while some fields are less engaged, others may benefit from increased utilization of these platforms to establish mentorship. In the modern era, social media provides a unique opportunity to overcome geographic and institutional barriers, allowing some osteopathic medical students to connect with mentors nationwide. Further studies should assess other social media platforms, such as LinkedIn, TikTok, and Instagram, to determine the platforms where surgical residents would have higher levels of engagement in the medical community.
Acknowledgments
The authors would like to thank Gina Qualter, JD, for her contribution to this study, as well as the American College of Osteopathic Surgeons (ACOS) Resident and Medical Student sections.
-
Research ethics: The local Institutional Review Board deemed the study exempt from review.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Kemp, S. Digital 2024 April Global Statshot Report. https://datareportal.com/reports/digital-2024-global-overview-report?utm_source=Global_Digital_Reports&utm_medium=Partner_Article&utm_campaign=Digital_2024 [Accessed 31 May 2024].Search in Google Scholar
2. Bisset, CN, Moug, SJ. Collaboration is key: the role of social media in advancing surgical research. Surgery 2023;174:392–4. https://doi.org/10.1016/j.surg.2023.04.053.Search in Google Scholar PubMed
3. Grossman, R, Sgarbura, O, Hallet, J, Soreide, K. Social media in surgery: evolving role in research communication and beyond. Langenbeck’s Arch Surg 2021;406:505–20. https://doi.org/10.1007/s00423-021-02135-7.Search in Google Scholar PubMed PubMed Central
4. Wong, R, Mayrovitz, HN. Perspectives of osteopathic medical students on preclinical urology exposure: a single institution cross-sectional survey. J Osteopath Med 2025;125:71–7. https://doi.org/10.1515/jom-2023-0284.Search in Google Scholar PubMed
5. Bhatnagar, V, Diaz, S, Bucur, PA. The need for more mentorship in medical school. Cureus 2020;12:e7984. https://doi.org/10.7759/cureus.7984.Search in Google Scholar PubMed PubMed Central
6. Vogel, AD, Wynn, AB, Richards, MC, Sindoni, M, Brennan, Z, Hamilton, CL, et al.. Interest in cardiothoracic surgery among the American College of Osteopathic Surgeons’ medical students. Cureus 2024;16:e65672. https://doi.org/10.7759/cureus.65672.Search in Google Scholar PubMed PubMed Central
7. Brazdzionis, J, Savla, P, Oppenheim, R, Kim, GJ, Conrad-Schnetz, K, Burns, B, et al.. Comparison of osteopathic (DO) and allopathic (MD) candidates matching into selected surgical subspecialties. Cureus 2023;15:e40566. https://doi.org/10.7759/cureus.40566.Search in Google Scholar PubMed PubMed Central
8. Harrell, KN, Vervoort, D, Luc, JGY, Tracy, BM, Daniel Stanley, J. Social media in surgery. Am Surg 2021;87:1021–4. https://doi.org/10.1177/0003134820972979.Search in Google Scholar PubMed
9. Khan, MT, Patnaik, R, Wheeler, C, Ibrahim, M, Wolf, H, Baumgardner, KC, et al.. Cross-sectional study of osteopathic general surgeons in university-based general surgery departments. Cureus 2022;14:e24791. https://doi.org/10.7759/cureus.24791.Search in Google Scholar PubMed PubMed Central
10. Heard, MA, Buckley, SE, Burns, B, Conrad-Schnetz, K. Identifying attitudes toward and acceptance of osteopathic graduates in surgical residency programs in the era of single accreditation: results of the American College of Osteopathic Surgeons Medical Student Section Questionnaire of Program Directors. Cureus 2022;14:e22870. https://doi.org/10.7759/cureus.22870.Search in Google Scholar PubMed PubMed Central
11. Sterling, M, Leung, P, Wright, D, Bishop, TF. The use of social media in graduate medical education: a systematic review. Acad Med 2017;92:1043–56. https://doi.org/10.1097/ACM.0000000000001617.Search in Google Scholar PubMed PubMed Central
12. Bludevich, BM, Fryer, M, Scott, EM, Buettner, H, Davids, JS, LaFemina, J. Patterns of general surgery residency social media use in the age of COVID-19. J Surg Educ 2021;78:e218–25. https://doi.org/10.1016/j.jsurg.2021.04.017.Search in Google Scholar PubMed PubMed Central
13. Cho, MJ, Li, AY, Furnas, HJ, Rohrich, RJ. Current trends in the use of social media by plastic surgeons. Plast Reconstr Surg 2020;146:83e–91e. https://doi.org/10.1097/PRS.0000000000006936.Search in Google Scholar PubMed
14. Long, LE, Leung, C, Hong, JS, Wright, C, Young, CJ. Patterns of internet and social media use in colorectal surgery. BMC Surg 2019;19:52. https://doi.org/10.1186/s12893-019-0518-4.Search in Google Scholar PubMed PubMed Central
15. Oyewumi, M, Lee, J, Vescan, A. Social media in otolaryngology-head and neck surgery. Ear Nose Throat J 2017;96:E29–33.Search in Google Scholar
16. Zerrweck, C, Arana, S, Calleja, C, Rodríguez, N, Moreno, E, Pantoja, JP, et al.. Social media, advertising, and internet use among general and bariatric surgeons. Surg Endosc 2020;34:1634–40. https://doi.org/10.1007/s00464-019-06933-5.Search in Google Scholar PubMed
17. George, DR, Green, MJ, Navarro, AM, Stazyk, KK, Clark, MA. Medical student views on the use of Facebook profile screening by residency admissions committees. Postgrad Med J 2014;90:251–3. https://doi.org/10.1136/postgradmedj-2013-132336.Search in Google Scholar PubMed
18. Lavertue, SM, Terry, R. A comparison of surgical subspecialty match rates in 2022 in the United States. Cureus 2023;15:e37178. https://doi.org/10.7759/cureus.37178.Search in Google Scholar PubMed PubMed Central
19. Saade, K, Shelton, T, Ernst, M. The use of social media for medical education within urology: a journey still in progress. Curr Urol Rep 2021;22:57. https://doi.org/10.1007/s11934-021-01077-3.Search in Google Scholar PubMed PubMed Central
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2024-0213).
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- General
- Original Article
- Determining the effects of social media engagement on surgery residents within the American College of Osteopathic Surgeons
- Medical Education
- Commentary
- Pioneering the future: incorporating lifestyle medicine tools in osteopathic medical education
- Musculoskeletal Medicine and Pain
- Original Article
- Urinary incontinence in elite female powerlifters aged 20–30: correlating musculoskeletal exam data with incontinence severity index and survey data
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Effects of a single osteopathic manipulative treatment on intraocular pressure reduction: a pilot study
- Public Health and Primary Care
- Original Article
- Impact of a clinician-directed educational program on communicating with patients regarding gun violence at two community urban healthcare centers
- Clinical Image
- Pityriasis lichenoides chronica presenting in skin of color
Articles in the same Issue
- Frontmatter
- General
- Original Article
- Determining the effects of social media engagement on surgery residents within the American College of Osteopathic Surgeons
- Medical Education
- Commentary
- Pioneering the future: incorporating lifestyle medicine tools in osteopathic medical education
- Musculoskeletal Medicine and Pain
- Original Article
- Urinary incontinence in elite female powerlifters aged 20–30: correlating musculoskeletal exam data with incontinence severity index and survey data
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Effects of a single osteopathic manipulative treatment on intraocular pressure reduction: a pilot study
- Public Health and Primary Care
- Original Article
- Impact of a clinician-directed educational program on communicating with patients regarding gun violence at two community urban healthcare centers
- Clinical Image
- Pityriasis lichenoides chronica presenting in skin of color

