Abstract
Context
Chronic rhinosinusitis (CRS) is a prevalent inflammatory disease of the paranasal sinuses that may significantly impair quality of life. CRS may also benefit from the application of manual techniques through osteopathic manipulative treatment (OMT), which aims to improve venous and lymphatic circulation, sympathetic and parasympathetic outflow, and cervicothoracic somatic dysfunction.
Objectives
This study aimed to assess whether OMT focused on lymphatic drainage of cranial structures can provide immediate, as well as sustained, relief of CRS symptoms.
Methods
This prospective, single-blinded study (WCG IRB study number: 1359444) was conducted at an allergy/immunology practice. Study participants included 43 adult patients, with a diagnosis of CRS, refractory to conventional medical therapy, with prior exposure to OMT. Patients consented to the study and were assigned by the provider to the OMT group or the control group 50/50. A four-question, 5-point Likert scale survey inquiring about the severity of nasal congestion, postnasal drainage, and facial or sinus pain/pressure, as well as the appreciation of the opportunity for an alternative therapy, was administered prior to the intervention. An OMT sequence was applied by the same osteopathic physician to each OMT group participant in the following order: thoracicinlet release, venous sinus drainage, occipital-atlantal decompression, thoracic paraspinal inhibition, facial sinus pressure, and Galbreath technique. A structural examination involving light touch was applied to the control group participants. The same 5-point Likert scale survey was administered immediately after the intervention. Participants were provided a blank copy of the survey to save and complete 10 days after the intervention. A paired t-test was applied for statistical comparison between the pre- and postsurveys.
Results
A total of 43 patients, including 22 patients in the treatment group (51.1 %) and 21 (48.8 %) patients in the control group, consented to and participated in the study, from May 1 to 30, 2024. Study demographics included 76.7 % females (n=33), 23.3 % males (n=10), 97.7 % White (n=42), and they patients had an average age of 54.4 years. Surveys administered before and immediately after the intervention were completed by 100 % of the study participants. All three surveys, including the presurvey and postsurvey completed immediately after and 10 days after the intervention, were completed by 60.5 % of the study participants. The OMT group pre-vs. immediate postsurvey results scored a statistically significant decrease in the severity of nasal congestion (p=0.001), postnasal drainage (p=0.002), and facial or sinus pain or pressure (p=0.0004).
Conclusions
Our single-blinded, prospective survey findings suggested that there was a benefit of OMT application for the immediate relief of CRS symptoms, predominantly in alleviating the severity of sinus pain or pressure. This study is the first large study (n=43) with a control group that shows that OMT techniques improve immediate CRS symptom relief of nasal congestion, postnasal drainage, and facial or sinus pain/pressure when compared to the pretreatment survey. Our study also demonstrated that the symptomatic relief by OMT of rhinosinusitis was not sustained in 10 days. OMT offers a safe, nonpharmacological complementary therapy to relieve lymphatic congestion and improve mucociliary clearance in CRS.
Chronic rhinosinusitis (CRS) is a prevalent inflammatory disease of the paranasal sinuses that may significantly impair quality of life and have implications on functional brain connectivity [1], [2], [3]. The standard approach to CRS management involves patient education, environmental controls, medical management, and consideration of allergen-specific immunotherapy and surgical management. CRS may also benefit from the application of manual techniques through osteopathic manipulative treatment (OMT), which aims to improve venous and lymphatic circulation, sympathetic and parasympathetic outflow, and cervicothoracic somatic dysfunction [4], [5], [6], [7], [8], [9]. Application of manual lymphatic techniques in several experimental animal models enhanced lymphatic circulation of inflammatory mediators, suggesting restored fluid homeostasis [10], 11]. Several small-scale cohort studies reported significantly improved sinusitis-associated symptoms after application of a consistent OMT sequence [12], [13], [14]. There is a deficit of large-scale studies in the osteopathic literature investigating temporary and sustained outcomes of OMT application in CRS. The objective of this study was to assess whether OMT focused on lymphatic drainage of cranial structures can provide immediate, as well as sustained, relief of CRS symptoms. This study is the first large study (n=43) with a control group that shows that OMT techniques improve immediate CRS symptom relief of nasal congestion, postnasal drainage, and facial or sinus pain/pressure when compared to the pretreatment survey. Our study also demonstrated that the symptomatic relief by OMT of rhinosinusitis was not sustained for 10 days.
Methods
This prospective, single-blinded study (Western Copernicus Group [WCG] Institutional Review Board [IRB] study number: 1359444) was conducted at an allergy/immunology practice. Study participants included 43 adult patients, with a diagnosis of CRS, refractory to conventional medical therapy, with prior exposure to OMT. The exclusion criteria included patients under 18 years old, pregnant, diagnosed with CRS with nasal polyposis, prescribed oral corticosteroids or acute antibiotics within the past week, uncontrolled with moderate persistent asthma, and currently utilizing tobacco products (Table 1). Patients consented to the study and provided basic demographic information, including their age, sex, and race. Patients were not informed of their group assignment throughout the duration of the study. The provider alternated assignments to the OMT vs. control group equally (50/50), to achieve similar study group numbers. An anonymized, four-question, 5-point Likert scale survey inquiring about the severity of nasal congestion, postnasal drainage, and facial or sinus pain/pressure, as well as the appreciation of the opportunity for an alternative therapy, was administered prior to the intervention (Figure 1). An OMT sequence was applied by the same osteopathic physician to each OMT group participant in the following order: thoracic inlet release, venous sinus drainage, occipital-atlantal decompression, thoracic paraspinal inhibition, facial sinus pressure, and Galbreath technique. A structural examination involving light touch was applied to the control group participants. This involved brief, gentle hand placement at the position of each OMT technique applied to the OMT group, without proceeding to deeper palpation or the complete technique. The same, anonymized 5-point Likert scale survey was administered immediately after the intervention. Participants were provided a blank copy of the survey to save and complete 10 days after the intervention. Each set of surveys was assigned a number for identification and letters A through C to label the presurvey (A), immediate postsurvey (B), and 10-day postsurvey (C). OMT group participants also received a handout with a video link and guide to self-applied techniques to practice at home. A small gift card was provided as compensation to participants who returned their completed third survey. A paired t-test was applied for statistical comparison between the presurvey and postsurvey.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
-
CRS, chronic rhinosinusitis; OMT, osteopathic manipulative treatment.

The survey administered to study participants immediately before and after, as well as 10 days after, the intervention.
Results
A total of 43 patients, including 22 patients in the treatment group (51.1 %) and 21 (48.8 %) patients in the control group, consented to and participated in the study, from May 1 to 30, 2024. Study demographics included 76.7 % females (n=33), 23.3 % males (n=10), 97.7 % White (n=42), and an average age of 54.4 years (range, 18–84 years). The surveys administered before and immediately after the intervention were completed by 100 % of the study participants (Figure 2). All three surveys, including the pre- and postsurveys completed immediately after and 10 days after the intervention, were completed by 60.5 % of the study participants. OMT group pre-vs. immediate postsurvey results scored a statistically significant decrease in the severity of nasal congestion (p=0.001), postnasal drainage (p=0.002), and facial or sinus pain or pressure (p=0.0004) (Figure 3). Less statistical significance was measured in the comparison OMT group pre- vs. immediate postsurvey results scoring appreciation for an alternate therapy (p=0.01). No statistically significant difference was demonstrated in all control group pre-vs. immediate postsurvey results (average p=0.32) (Figure 4). No statistically significant difference was computed, in comparison of pre- vs. 10-day postsurvey results, for both the treatment (average p=0.28) and control groups (average p=0.22).
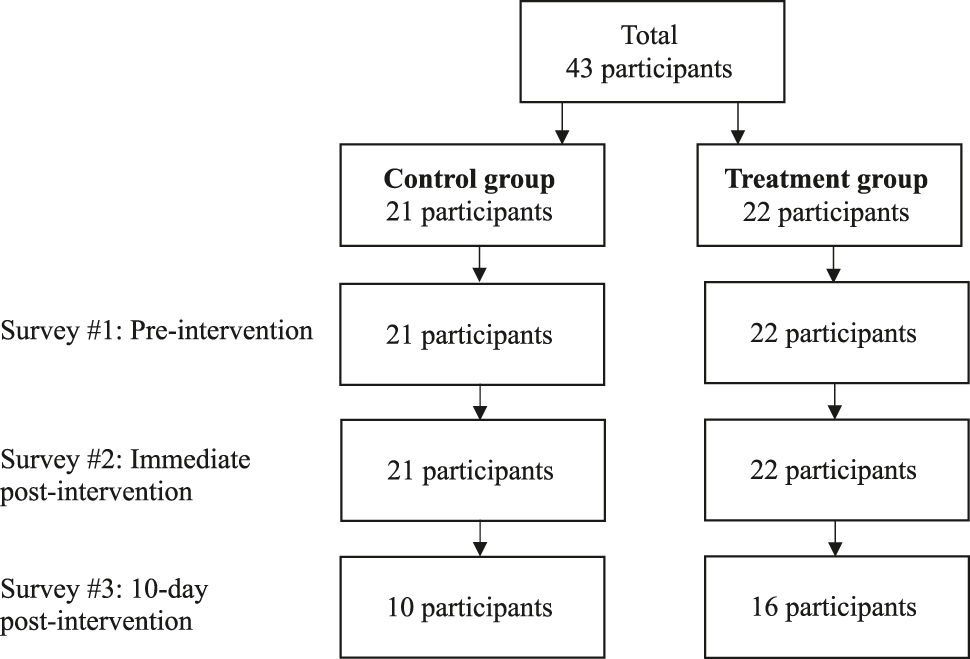
The number of study participants that completed each of the three surveys.

A symptomatic comparison of the treatment group short- vs. long-term presurvey vs. postsurvey. A statistically significant improvement was demonstrated for all immediate postsurvey symptoms (p=0.0004-0.002), but it did not extend to the 10-day postsurvey symptomatic assessment (p=0.28).

A control group short- vs. long-term presurvey vs. postsurvey symptomatic comparison. No statistically significant difference was demonstrated in all control group survey results presurvey vs. immediate (p=0.32) and 10-day postsurvey (p=0.22).
Discussion
Our single-blinded, prospective survey findings suggested the benefit of OMT application for immediate relief of CRS symptoms, predominantly in alleviating the severity of sinus pain or pressure. Long-term efficacy of OMT for CRS symptomatic relief was not strongly supported by the data. This study expanded upon previous studies applying OMT to sinusitis management [12], [13], [14], through implementation of a control group, increased sample size, and evaluation of sustained symptomatic relief. Limitations in location, racial diversity, lack of a standardized scale, and duration variability of each encounter may be considered for future iterations of this study. Our study population consisted of patients from one clinic, which may not be representative of all patient populations. Although race identity was not among the exclusion criteria, our study demographics reflected the demographics of the clinic’s patient population, individuals who largely identified as “White” or “Caucasian.” This study also did not establish specific duration for each patient’s intervention, in an effort to individualize the OMT to each patient’s variable somatic dysfunctions, while maintaining consistency with the OMT sequence of techniques. We did not apply a standardized scale, such as the Sino-Nasal Outcome Test applied in Nishida et al. [12], and we developed our survey to evaluate the impact on key symptoms and interest in alternative treatments.
Several small-scale studies have been documented in the literature. Lee et al. [13] conducted a before-and-after intervention study on 22 participants who consented to receiving OMT for the management of sinusitis. Lee et al. [13] applied various techniques, including: cervical soft tissue, myofascial release (MFR), and high-velocity, low-amplitude (HVLA); thoracic muscle energy, scapular release, and HVLA; Chapman points; and intra-oral sphenopalatine ganglion release. Nishida et al. [12] applied thoracic inlet MFR, supraorbital and infraorbital nerve release, and suboccipital decompression in a prospective, randomized, controlled pilot study that demonstrated reduced duration and severity of symptoms in the use of select OMT compared with conventional medical treatment alone. Our study also involved thoracic inlet MFR and other variants of MFR and soft tissue, such as thoracic paraspinal inhibition, facial sinus pressure, and occipital-atlantal decompression, but it also explored cranial and lymphatic techniques, such as venous sinus drainage and the Galbreath technique. We selected these OMT techniques based on osteopathic approaches previously described in the literature for head, eyes, ears, nose, and throat disorders [4], [5], [6, 8], 9]. Our study offered a larger cohort with 43 participants and was designed as single-blinded to mitigate the risk of bias.
Lee-Wong et al. [14] also described an intervention study conducted on 15 participants interested in receiving another possible treatment for relief of their sinus symptoms. Results show an immediate improvement in symptoms for 9 out of the 15 patients, after the use of direct pressure and sinus drainage techniques [14], similar to OMT techniques applied in the present study. However, no control group was involved for comparison [14]. We included a control group of 21 participants to assess the improvement in rhinosinusitis symptoms, in comparison to the OMT treatment group (n=22). Our study results support these previous studies, suggesting that OMT provides significant improvement in symptoms for rhinosinusitis patients.
Conclusions
OMT offers a safe, nonpharmacological complementary therapy to relieve lymphatic congestion and improve mucociliary clearance in CRS [4], [5], [6], [7], [8], [9, [12], [13], [14]. Previous studies demonstrate that OMT techniques are an effective method to relieve rhinosinusitis [12], [13], [14]. This study is the first large study (n=43) with a control group that demonstrates that OMT techniques improve immediate CRS symptom relief of nasal congestion, postnasal drainage, and facial or sinus pain/pressure when compared to the pretreatment survey. Future clinical studies are needed to investigate the role of OMT in long-term outcomes.
-
Research ethics: WCG IRB granted ethical approval for this study (#1359444) on 8/23/2023. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
-
Informed consent: Written informed consent was obtained from all individuals included in this study.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
1. Sedaghat, AR. Chronic rhinosinusitis. Am Fam Physician 2017;96:500–6.Search in Google Scholar
2. Bachert, C, Marple, B, Schlosser, RJ, Hopkins, C, Schleimer, RP, Lambrecht, BN, et al.. Adult chronic rhinosinusitis. Nat Rev Dis Prim 2020;6:86. https://doi.org/10.1038/s41572-020-00218-1.Search in Google Scholar PubMed
3. Jafari, A, de Lima, XL, Bernstein, JD, Simonyan, K, Bleier, BS. Association of sinonasal inflammation with functional brain connectivity. JAMA Otolaryngol Head Neck Surg 2021;147:534–54. https://doi.org/10.1001/jamaoto.2021.0204.Search in Google Scholar PubMed PubMed Central
4. Wu, SS, Graven, K, Sergi, M, Hostoffer, R. Rhinitis: the osteopathic modular approach. J Am Osteopath Assoc 2020;120:351–8. https://doi.org/10.7556/jaoa.2020.054.Search in Google Scholar PubMed
5. Wu, SS, Hostoffer, RW, Gibbons, K, Shaw, HH, Shaw, MB. 48A(1): osteopathic considerations in patients with head, eyes, ears, nose, and throat disorders. In: Seffinger, MA, editor. Foundations of osteopathic medicine: philosophy, science, clinical applications, and research, 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:1386–404 pp.Search in Google Scholar
6. Wu, SS, Hostoffer, RW, Gibbons, K, Shaw, HH, Shaw, MB. 48A(2): rhinosinusitis. In: Seffinger, MA, editor. Foundations of osteopathic medicine: philosophy, science, clinical applications, and research, 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:1404–11 pp.Search in Google Scholar
7. Nelson, KE, Allgeier, J. Chapter 24: the patient with an upper respiratory infection. In: Nelson, KE, Glonek, T, editors. Somatic dysfunction in osteopathic family medicine, 2nd ed. Philadelphia, PA: Wolters Kluwer Heath/American College of Osteopathic Family Physicians; 2015.Search in Google Scholar
8. Kuchera, ML, Kuchera, WA. Osteopathic considerations in HEENT disorders. Dayton, OH: Greyden Press; 2012.Search in Google Scholar
9. DiGiovanna, EL, Phykitt, DE, Ferris, MT. Chapter 111: HEENT applications. In: DiGiovanni, EL, Amen, CJ, Burns, DK, editors. An osteopathic approach to diagnosis and treatment, 4th ed. Lippincott, Williams & Wilkins; 2020:527–37 pp.Search in Google Scholar
10. Schander, A, Downey, HF, Hodge, LM. Lymphatic pump manipulation mobilizes inflammatory mediators into lymphatic circulation. Exp Biol Med (Maywood) 2012;237:58–63. https://doi.org/10.1258/ebm.2011.011220.Search in Google Scholar PubMed
11. Castillo, R, Schander, A, Hodge, LM. Lymphatic pump treatment mobilizes bioactive lymph that suppresses macrophage activity in vitro. J Am Osteopath Assoc 2018;118:455–61. https://doi.org/10.7556/jaoa.2018.099.Search in Google Scholar PubMed
12. Nishida, Y, Sopchak, MM, Jackson, MR. Effect of select osteopathic manipulative treatment techniques on patients with acute rhinosinusitis. AAO J. 2015;25:12–20.Search in Google Scholar
13. Lee, E, Lo, J, Tran, J, Redding, D. Osteopathic manipulative treatment for sinusitis relief: a pilot study. Osteopath Fam Physician 2022;14:10–14. https://doi.org/10.33181/13065.Search in Google Scholar
14. Lee-Wong, M, Karagic, M, Doshi, A, Gomez, S, Resnick, D. An osteopathic approach to chronic sinusitis. J Allergy Ther 2011;2:109. https://doi.org/10.4172/2155-6121.1000109.Search in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Medical Education
- Review Article
- Trends in osteopathic medical education: a scoping review
- Musculoskeletal Medicine and Pain
- Review Article
- Osteopathic approach to injuries of the overhead thrower’s shoulder
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- The effect of osteopathic manipulative treatment on chronic rhinosinusitis
- Obstetrics and Gynecology
- Clinical Practice
- Management of endometriosis: a call to multidisciplinary approach
- Pediatrics
- Case Report
- Non-Herlitz junctional epidermolysis bullosa in a Native American newborn
- Public Health and Primary Care
- Original Article
- Improving vascular access knowledge and assessment skill of hemodialysis staff
Articles in the same Issue
- Frontmatter
- Medical Education
- Review Article
- Trends in osteopathic medical education: a scoping review
- Musculoskeletal Medicine and Pain
- Review Article
- Osteopathic approach to injuries of the overhead thrower’s shoulder
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- The effect of osteopathic manipulative treatment on chronic rhinosinusitis
- Obstetrics and Gynecology
- Clinical Practice
- Management of endometriosis: a call to multidisciplinary approach
- Pediatrics
- Case Report
- Non-Herlitz junctional epidermolysis bullosa in a Native American newborn
- Public Health and Primary Care
- Original Article
- Improving vascular access knowledge and assessment skill of hemodialysis staff


