A 56-year-old male patient known with hypogammaglobulinemia on monthly intravenous immunoglobulins, presented with worsening facial rash. He has been diagnosed with cutaneous T cell lymphoma based on punch biopsies from skin bumps on his extremities, and he was treated with ultraviolet (UV) phototherapy. He presented with worsening facial rash and white pustules superimposed on the rash. He was clinically diagnosed with rosacea with pustules and papules, and he was treated successfully with doxycycline and topical minocycline (Figure 1).
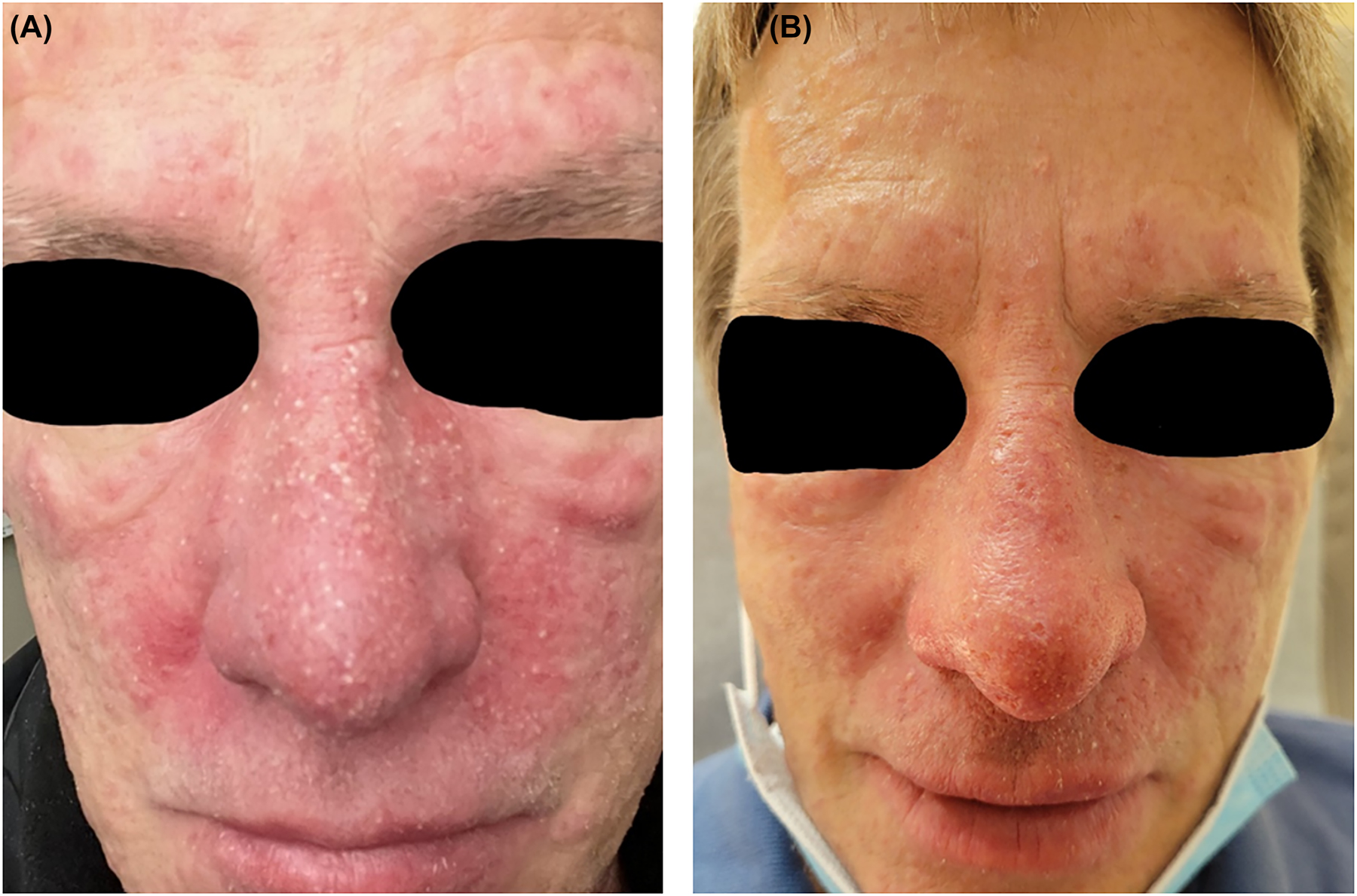
Rosacea flair with inflamed papules and pustules, (A) before and (B) after treatment.
Rosacea is a common skin disease in adults. It presents with centro-facial redness around the cheeks, nose, and chin, as well as telangiectasia, flushing, inflamed papules and pustules, and a dry burning sensation. The ocular involvement can occur independently or in association with cutaneous findings [1]. There are many potential contributing factors, some involving the innate immune system abnormalities, UV exposure, genetics, and inflammation triggered by cutaneous microorganisms [2]. The diagnosis is based on the clinical assessment. A skin biopsy is rarely indicated. Therapeutic options include regular sunscreen use, gentle skin care, and avoiding triggers. An ophthalmology referral is required for ocular involvement. The treatment is based on the skin manifestation: topical brimonidine can be utilized for erythema, laser therapy can be utilized for telangiectasias, and topical metronidazole, azelaic acid, ivermectin, or minocycline maybe utilized for papules and pustules. If patients fail topical therapy, or in severe cases, one may add oral tetracycline, doxycycline, or minocycline. Oral isotretinoin can be utilized for refractory cases as well [3].
-
Research funding: None reported.
-
Author contributions: Both authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; both authors drafted the article or revised it critically for important intellectual content; both authors contributed to the analysis and interpretation of data; both authors gave final approval of the version of the article to be published; and both authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Conflicts of interests: None reported.
References
1. Gallo, RL, Granstein, RD, Kang, S, Mannis, M, Steinhoff, M, Tan, J, et al.. Standard classification and pathophysiology of rosacea: the 2017 update by the national rosacea society expert committee. J Am Acad Dermatol 2018;78:148–55. https://doi.org/10.1016/j.jaad.2017.08.037.Search in Google Scholar PubMed
2. Mc Aleer, MA, Lacey, N, Powell, FC. The pathophysiology of rosacea. G Ital Dermatol Venereol 2009;144:663–71.Search in Google Scholar
3. van Zuuren, EJ, Fedorowicz, Z, Carter, B, van der Linden, MM, Charland, L. Interventions for rosacea. Cochrane Database Syst Rev 2015;2015:CD003262. https://doi.org/10.1002/14651858.CD003262.pub5.Search in Google Scholar PubMed PubMed Central
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Original Article
- Effects of the Strong Hearts program after a major cardiovascular event in patients with cardiovascular disease
- Medical Education
- Original Articles
- The relationship between required physician letters of recommendation and decreasing diversity in osteopathic medical school admissions
- Learning abnormal physical examination signs: an introductory course
- Musculoskeletal Medicine and Pain
- Original Article
- Evaluating the underreporting of patient-reported outcomes in carpal tunnel syndrome randomized controlled trials
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Utilization and reimbursement trends of osteopathic manipulative treatment for Medicare patients: 2000–2019
- Public Health and Primary Care
- Original Article
- Trends of colorectal cancer screening methods: an analysis of Behavioral Risk Factor Surveillance System data from 2018–2020
- Clinical Image
- Rosacea with pustules and papules
- Letters to the Editor
- The first step to strengthening graduate level osteopathic education: a national review
- Ensuring adequate power: the importance of statistically significant results in osteopathic research
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Original Article
- Effects of the Strong Hearts program after a major cardiovascular event in patients with cardiovascular disease
- Medical Education
- Original Articles
- The relationship between required physician letters of recommendation and decreasing diversity in osteopathic medical school admissions
- Learning abnormal physical examination signs: an introductory course
- Musculoskeletal Medicine and Pain
- Original Article
- Evaluating the underreporting of patient-reported outcomes in carpal tunnel syndrome randomized controlled trials
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Utilization and reimbursement trends of osteopathic manipulative treatment for Medicare patients: 2000–2019
- Public Health and Primary Care
- Original Article
- Trends of colorectal cancer screening methods: an analysis of Behavioral Risk Factor Surveillance System data from 2018–2020
- Clinical Image
- Rosacea with pustules and papules
- Letters to the Editor
- The first step to strengthening graduate level osteopathic education: a national review
- Ensuring adequate power: the importance of statistically significant results in osteopathic research

