Effects of a focused training on first-year osteopathic medical students’ ability to incorporate point-of-care ultrasound in assessment of the anterior knee
-
Christina Weaver
, Deborah M. Heath
, Kamalani Hanamaika’i
Abstract
Context
Patients frequently present to the outpatient clinic, urgent care, or emergency department with a painful, swollen knee. Differentiating the underlying etiology can be a challenge for both medical students and seasoned clinicians alike. Because this scenario can represent a time-sensitive emergency, developing skills to diagnose the underlying cause quickly and accurately is essential for proper management, whether the patient would benefit from osteopathic manipulation, prompt administration of antibiotics, or a more invasive procedure like joint aspiration or surgery.
Objectives
The objectives are to determine the effects of a focused ultrasound training on first-year osteopathic medical students’ ability to identify normal sonographic anatomy of the anterior knee and to differentiate between three common pathologies: joint effusion, prepatellar bursitis, and cellulitis.
Methods
First-year osteopathic medical students voluntarily participated in this cross-sectional study. The study protocol included a focused ultrasound training (online materials, brief didactic and single hands-on sessions) followed by a hands-on assessment. A written test and 5-point Likert scale questionnaire were administered before and after the focused training. Nine weeks later, students completed a follow-up written test. The proportion of students who correctly identified common pathologies on written tests before (pretest) and after (posttest) training and on the follow-up written test were compared utilizing the Fisher’s exact test. A t test was utilized to compare data from the pretraining and posttraining questionnaires.
Results
Of 101 students completing the written pretest and pretraining questionnaire, 95 (94.1 %) completed the written posttest and posttraining questionnaire, and 84 (83.2 %) completed the follow-up written test. Students had limited previous experience with ultrasound; 90 (89.1 %) students had performed six or fewer ultrasound examinations before the focused ultrasound training. On written tests, students accurately identified joint effusion (22.8 % [23/101] pretest, 65.3 % [62/95] posttest, 33.3 % [28/84] follow-up test), prepatellar bursitis (14.9 % [15/101] pretest, 46.3 % [44/95] posttest, 36.9 % [31/84] follow-up test), and cellulitis (38.6 % [39/101] pretest, 90.5 % [86/95] posttest, 73.8 % [62/84] follow-up test). Differences were found between pretest and posttest for identification of all three pathologies (all p<0.001) and between the pretest and 9-week follow-up test for identification of prepatellar bursitis and cellulitis (both p≤0.001). For questionnaires, (where 1=strongly agree, 5=strongly disagree), the mean (standard deviation [SD]) confidence for correctly identifying normal sonographic anatomy of the anterior knee was 3.50 (1.01) at pretraining and 1.59 (0.72) at posttraining. Student confidence in the ability to differentiate joint effusion, prepatellar bursitis, and cellulitis utilizing ultrasound increased from 4.33 (0.78) at pretraining to 1.99 (0.78) at posttraining. For the hands-on assessment, 78.3 % (595 correct/760 aggregated responses) of the time students correctly identified specific sonographic landmarks of the anterior knee. When the evaluation combined real-time scanning with a prerecorded sonographic video clip of the anterior knee, 71.4 % (20/28) accurately identified joint effusion, 60.9 % (14/23) correctly diagnosed prepatellar bursitis, 93.3 % (28/30) recognized cellulitis, and 47.1 % (8/17) diagnosed the normal knee.
Conclusions
Our focused training was effective at immediately increasing basic knowledge, as well as confidence of first-year osteopathic medical students when assessing the anterior knee with point-of-care ultrasound. However, spaced repetition and deliberate practice may be useful for learning retention.
Patients frequently present to the outpatient clinic, urgent care, or emergency department with a painful, swollen knee. Differentiating the underlying etiology can be a challenge for both medical students and seasoned clinicians alike. In a previous study investigating 44 knees with known rheumatoid arthritis [1], point-of-care ultrasound detected 27 (61.4 %) knee joint effusions, whereas clinical examination alone identified only 16 (36.4 %), suggesting that ultrasound is a more useful tool for examining these structures. Because a painful knee can represent a time-sensitive emergency, developing skills to diagnose the underlying cause quickly and accurately is essential for proper management, such as determining whether the patient would benefit from osteopathic manipulation, prompt administration of antibiotics, or a more invasive procedure like joint aspiration or surgery. In a study by Adhikari and Blaivas [2], 54 patients presented to the emergency room with joint pain, erythema, and swelling of the knee, ankle, or elbow joint, and 39 (72.2 %) joint aspirations were planned based on physical examination alone. However, only 20 (37.0 %) invasive procedures were performed after point-of-care ultrasound showed an absence of joint effusion [2].
Because of advances in ultrasound technology during the past 2 decades, such as increased portability, the use of ultrasound in medical education has been studied extensively [3], [4], [5]. For example, ultrasound is increasingly utilized in undergraduate medical education to help students recognize anatomic landmarks when learning anatomy or osteopathic manipulation and later in clinical training to enhance bedside decision-making and patient safety through the use of ultrasound-guided procedures [6, 7]. All osteopathic medical students receive specialized training in palpation skills, osteopathic principles, and osteopathic manipulative treatment (OMT). At our institution, students must also be prepared to work with patients earlier than most because they spend their second through fourth years at a federally qualified community health center and start seeing patients in a supervised clinical setting at the beginning of their second year, as discussed by Vora and Kinney [8]. Because of this, our curriculum includes an early introduction to ultrasound in the clinical decision-making process.
Point-of-care ultrasound in medical education is thought to enhance future efficiency, reduce costs, and improve patient outcomes [9]. Therefore, the purpose of the current study was to determine the effects of a focused ultrasound training on first-year osteopathic medical students’ ability to identify normal sonographic anatomy of the anterior knee and differentiate between three common pathologies: joint effusion, prepatellar bursitis, and cellulitis. We hypothesized that with a focused training approach, even medical students with limited point-of-care ultrasound experience could learn these basic skills.
Methods
The study protocol included a focused ultrasound training session, a hands-on assessment with a standardized patient, a written test before (pretest) and after (posttest) the training, and a questionnaire before (pretraining) and after (posttraining) the training. The focused training session and assessments took place in the same day, 1 week after students received online training materials. A written follow-up test was administered 9 weeks later to assess learning retention.
Participants
This cross-sectional, single-center design study was conducted from March through May 2018 at A.T. Still University’s School of Osteopathic Medicine in Mesa, Arizona and was considered exempt by the A.T. Still University-Arizona Institutional Review Board. First-year osteopathic medical students, with little to no point-of-care ultrasound experience, were recruited to participate on a voluntary basis. Each student provided informed and written consent before participation. All learning activities occurred in the osteopathic manipulative medicine (OMM) laboratory, and additional materials were posted online. All students were offered the same educational experiences whether they participated in the study or not, and their grades were unaffected. Various steps related to training and assessment for the current study are illustrated in Figure 1. The overall duration of the study was approximately 10 weeks from students receiving the online study materials to the follow-up written test.
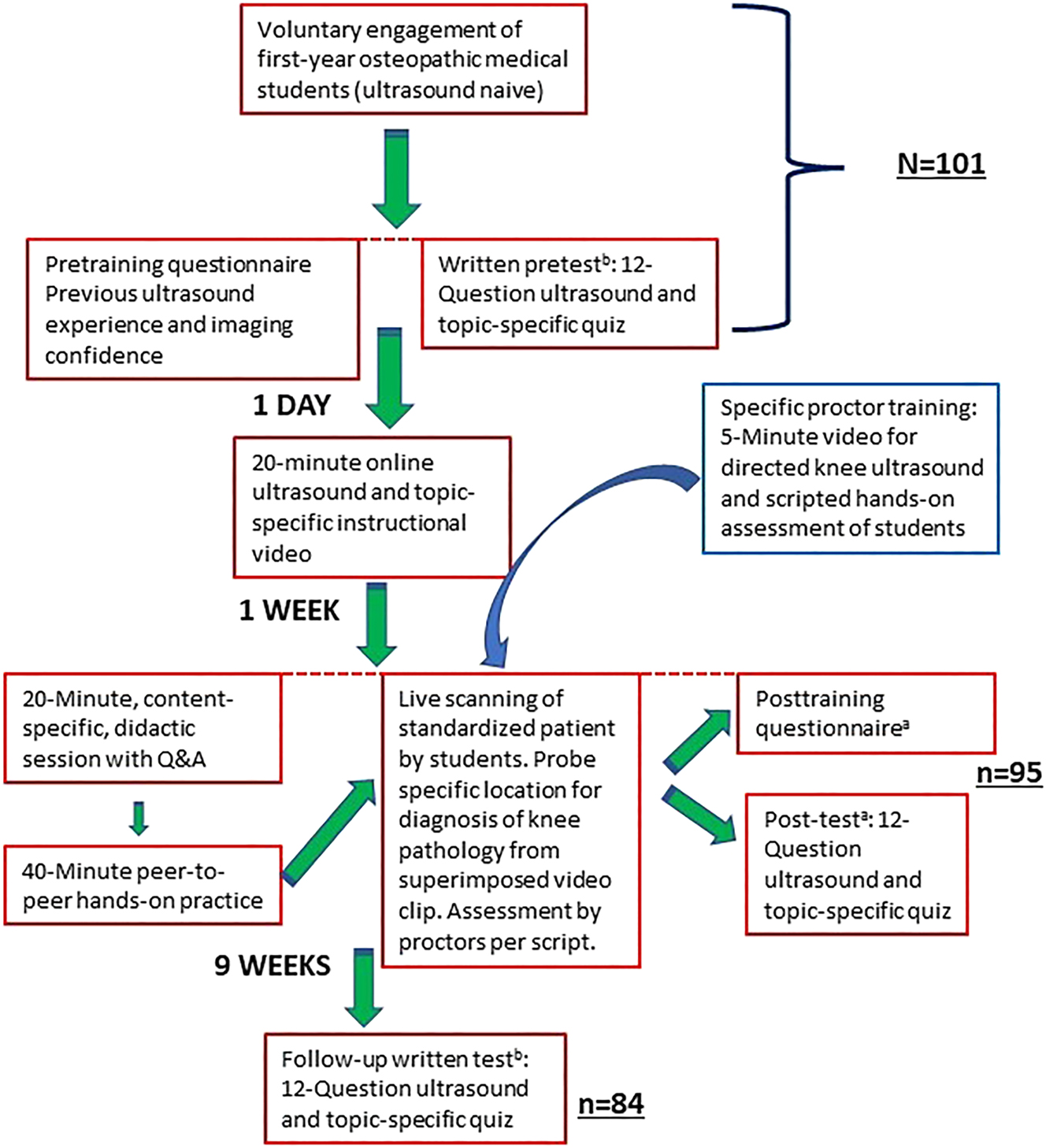
Study flowchart for effectiveness of a focused training on first-year osteopathic medical students’ ability to incorporate point-of-care ultrasound in assessment of the anterior knee. aOrder of test questions modified from previous test.
Pretraining: written pretest and pretraining questionnaire
One week before the focused ultrasound training, students were given the pretraining questionnaire (Supplementary Material). The eight-item questionnaire asked for information about previous ultrasound experience and assessed self-reported confidence levels regarding their ability to identify normal anatomy and common pathologies of the anterior knee. Confidence levels were measured on a 5-point Likert scale, where 1 was strongly agree and 5 was strongly disagree.
Next, students completed a 12-question, multiple-choice pretest to assess baseline knowledge, including ultrasound findings for joint effusion, prepatellar bursitis, cellulitis, and the normal anterior knee. Questions also focused on ultrasound knobs, probes, and orientation, as well as echogenicity, patient diagnosis, and next best step in management (e.g., antibiotics, arthrocentesis, OMT and/or rest, ice, compression) based on sonographic images and clinical vignettes for a patient with a painful swollen knee. The paper pretest and questionnaire were administered during OMM laboratory and took approximately 15 min to complete.
Focused ultrasound training
The next day, a 20 min instructional video was posted online for students to view. They were informed about the video after completing the pretest and again by email once it was posted. The instructional video was developed specifically for the current study and consisted of the following: a brief discussion on ultrasound fundamentals, transducers, scanning technique, and echogenicity; normal sonographic anatomy of the anterior knee; and examples of the three primary pathologies for joint effusion, prepatellar bursitis, and cellulitis of the knee. The presentation also briefly covered clinical presentation, physical examination findings, and appropriate next-step management of each condition. Students were asked to view the video before the following week’s OMM laboratory, which also included the study’s hands-on evaluation.
Faculty and sonographers involved with the in-person focused training and hands-on evaluation also received training for the current study. They were given access to a PowerPoint (Microsoft Corporation, Redmond, WA) and 5 min video created for review of ultrasound techniques of the anterior knee and specific evaluation criteria to ensure consistency during the hands-on student assessment. Proctors included: one ultrasound fellowship-trained emergency physician, one physician and two registered diagnostic medical sonographers credentialed by the American Registry for Diagnostic Medical Sonography, one PGY-4 radiology resident, one biomedical engineer, and two predoctoral OMM fellows.
For the in-person focused ultrasound training, students were divided into their usual morning and afternoon OMM laboratory groups (approximately 50 students each). A 20 min didactic session was presented and included an overview of the online materials and learning objectives (Figure 2). Any questions that the students had were answered in real time. After the didactic presentation, groups of five or six students practiced scanning the anterior knee on each other for approximately 40 min. Students located and identified anatomical landmarks and tissue types while describing features of echogenicity on ultrasound. Each group was supervised by an instructor.
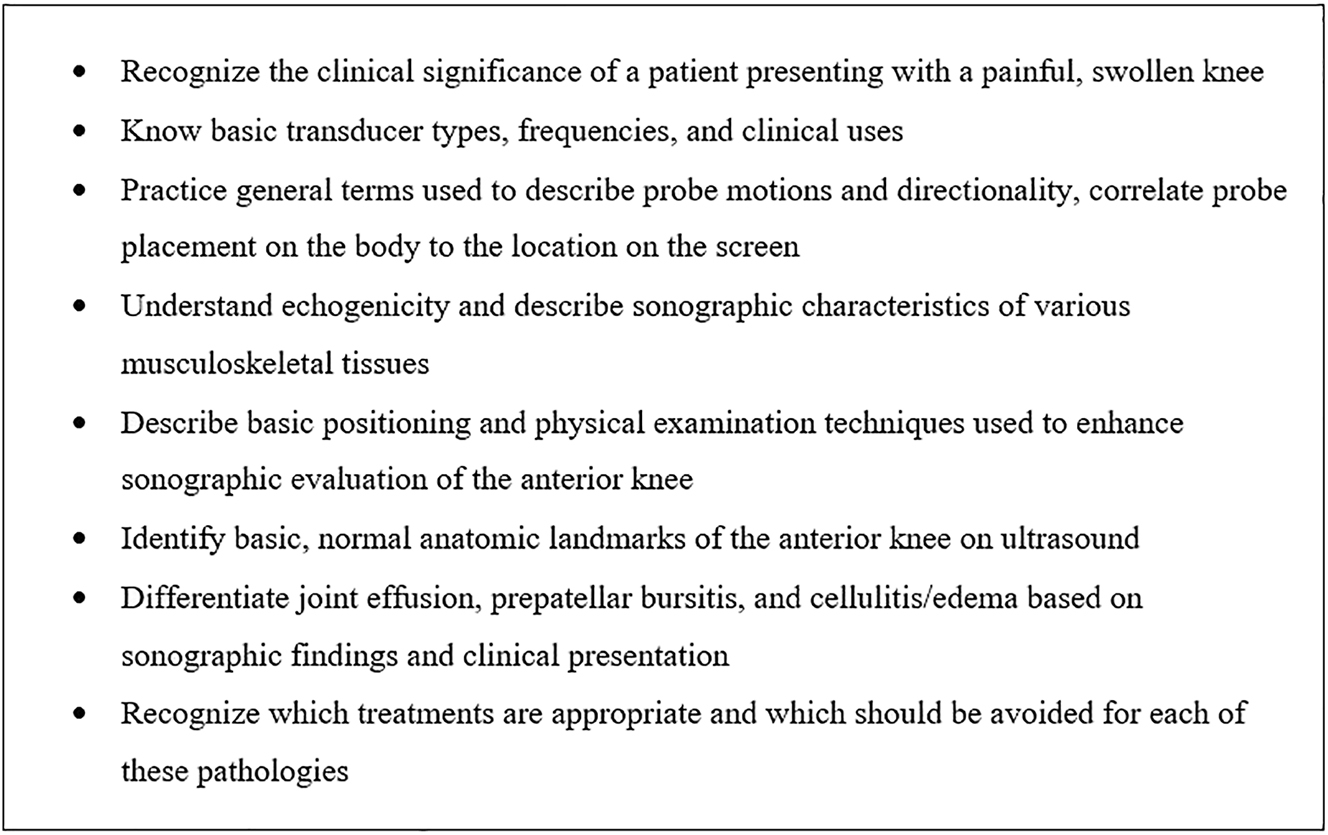
Learning objectives for the focused training session in the current study.
Calibration of standardized patients
Before the hands-on assessment, each standardized patient was examined and scanned by the study’s primary investigator (CW). Height, weight, body mass index, and knee circumference directly over the patella and 2 cm proximal were recorded for each standardized patient. The calibration was intended to verify that students could identify the required anatomical landmarks and determine the absence or presence of joint effusion, prepatellar bursitis, and cellulitis. Results of the calibration were utilized as the gold standard for the hands-on assessment. Although they represented a variety of shapes and sizes, none of the standardized patients had clinically relevant pathology of the knee.
Posttraining: hands-on assessment, written posttest, and posttraining questionnaire
For the hands-on assessment, each student was evaluated at one of six similar testing stations and given 12 min to complete the process. While the student interacted with the standardized patient, a trained instructor asked scripted questions and documented student responses (Figure 3). Students utilized either a GE LOGIQ e (GE Ultrasound, Milwaukee, WI), Sonosite Edge II (FUJIFILM SonoSite, Inc., Bothell, WA), or Sonosite M-Turbo ultrasound machine with a high-frequency (12–5 MHz) linear probe for scanning. To begin, each student was asked to identify several anatomical landmarks of the anterior knee: skin/subcutaneous tissues, muscle, quadriceps tendon, patella, femur, suprapatellar recess, distal patellar tendon, and tibial plateau.
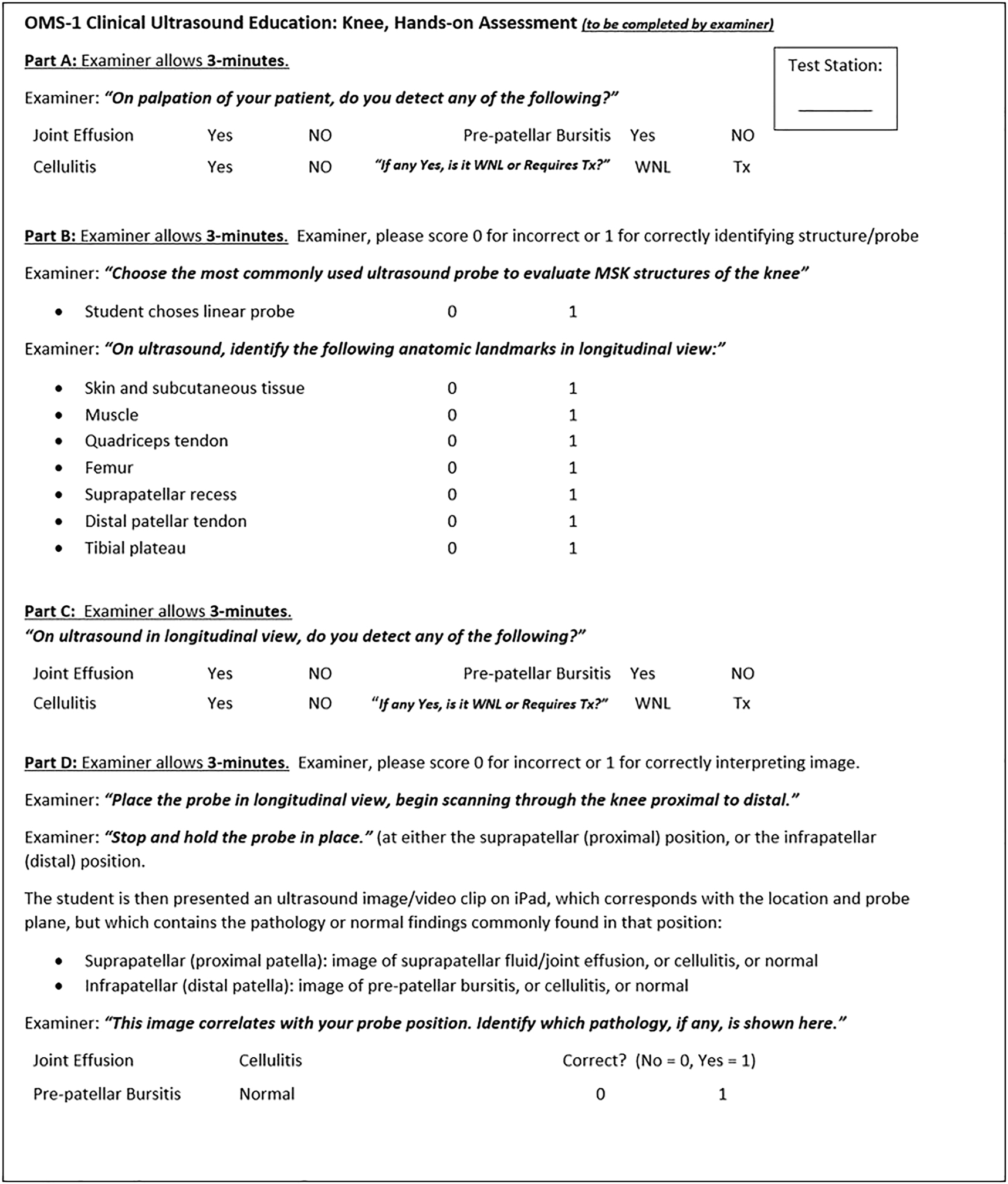
Combined script and checklist utilized by proctors in the current study during the hands-on assessment. Tx, treatment; WNL, within normal limits.
Next, and unique to this study, students were instructed to “place the probe in longitudinal view, begin scanning through the knee, proximal to distal. Now stop and hold the probe in place” (Figure 4). A digital tablet with a prerecorded sonographic video clip matching the same anatomical location of the student’s probe placement on the standardized patient was then superimposed in front of the ultrasound screen. Depicting either joint effusion, prepatellar bursitis, cellulitis, or the normal knee, students were then asked to combine their knowledge of probe placement, anatomy, and sonographic findings from the superimposed video clip to make a point-of-care diagnosis (Figure 5).

Point-of-care ultrasound of the anterior knee. Students described the anatomy seen on ultrasound as they scanned the standardized patient’s knee.

A novel approach to providing reliable sonographic pathology when scanning a standardized patient. Once students have the correct probe placement and image in view, a digital tablet with the same anatomic view plus one of our three focused pathologies is manually superimposed over the ultrasound screen. Students were asked to consider their probe placement, underlying anatomy, and the image on the “new” screen to make a diagnosis.
Immediately after the hands-on assessment, students spent approximately 15 min completing the written posttest and posttraining questionnaire. The posttest had the same 12 questions as the pretest, but questions were presented in a different order to limit memorization of answers. The posttraining questionnaire repeated four questions from the pretraining questionnaire and included an additional question on whether students felt the ultrasound training would change how they diagnosed and managed a patient with a swollen, painful knee in future practice (Supplementary Material).
Learning retention: follow-up written test
Nine weeks later, students were asked to complete the follow-up written test, which was identical to the posttest. Like previous parts of the study, completion of the follow-up written test was voluntary. It was administered during OMM laboratory and took approximately 10 min to complete.
Data analysis
Identification of the three common pathologies—joint effusion, prepatellar bursitis, and cellulitis—were reported as proportions for the written pretest to posttest and for the pretest to 9-week follow-up written test. These data were compared utilizing the Fisher’s exact test. An independent sample t test was utilized to compare questionnaire results. A preliminary analysis indicated that the data met normality assumption requirements. Data were summarized utilizing frequency and percentage and mean and standard deviation (SD). The questionnaire and written test responses were anonymous and pooled for analysis. Paired tests were not utilized because results could not be matched by student. Instead, we assumed that the groups were independent for analysis. A p value of <0.05 was considered statistically significant. All analyses were conducted utilizing Stata 15 (College Station, TX).
Results
A total of 101 students voluntarily completed the written pretest and pretraining questionnaire before participating in the focused ultrasound training. Immediately after the focused training, 95 (94.1 %) students voluntarily completed the hands-on assessment, written posttest, and posttraining questionnaire. Nine weeks later, 84 (83.2 %) students completed the follow-up written test.
Hands-on assessment
Overall, 78.3 % (595 correct of 760 aggregated responses) of the time students successfully identified sonographic landmarks of the anterior knee. Specifically, they correctly identified the following structures: skin (93.7 %, 89/95), muscle (72.6 %, 69/95), quadriceps tendon (90.5 %, 85/95), patella (94.7 %, 90/95), femur (89.5 %, 85/95), suprapatellar recess (73.7 %, 70/95), distal patellar tendon (89.5 %, 85/95), and tibial plateau (23.2 %, 22/95).
When asked to diagnose a prerecorded ultrasound image while scanning the corresponding location on the standardized patient’s knee, 71.4 % (20/28) of students accurately identified joint effusion, 60.9 % (14/23) correctly diagnosed prepatellar bursitis, and 93.3 % (28/30) recognized cellulitis.
Written tests
On the written tests, students accurately identified joint effusion (22.8 % [23/101] pretest, 65.3 % [62/95] posttest, 33.3 % [28/84] follow-up test), prepatellar bursitis (14.9 % [15/101] pretest, 47.4 % [44/95] posttest, 36.9 % [31/84] follow-up test), and cellulitis (38.6 % [39/101] pretest, 90.5 % [86/95] posttest, 73.8 % [62/84] follow-up test) (Figure 6). Differences were found between pretest and posttest for student identification of the three pathologies (all p<0.001) and between pretest and 9-week follow-up test for identification of prepatellar bursitis and cellulitis (both p≤0.001).
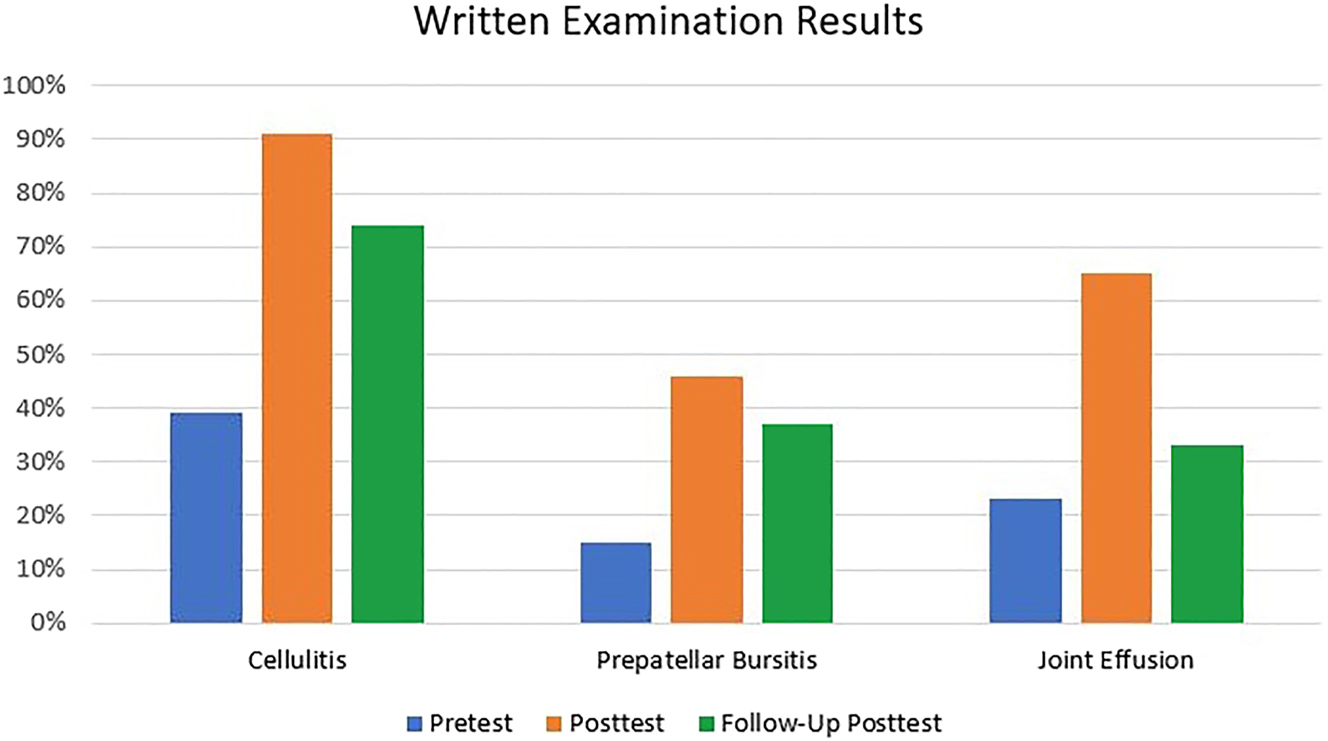
The percent of correct responses of first-year osteopathic medical students on written tests for identification of joint effusion, prepatellar bursitis, and cellulitis from ultrasound images of the anterior knee.
Higher-order test questions pertaining to the treatment of these conditions utilized sonographic images and clinical vignette to determine the next best steps in management; students identified correct treatment for the joint effusion case (38.6 % [39/101] pretest, 48.4 % [46/95] posttest, 44.0 % [37/84] follow-up test), cellulitis case (17.8 % [18/101] pretest, 58.9 % [56/95] posttest, 28.6 % [24/84] follow-up test), and the sonographic normal knee with overuse case (81.2 % [82/101] pretest, 94.7 % [90/95] posttest, 88.1 % [74/84] follow-up test). Significant differences were found between pretest and posttest for treatment utilizing antibiotics in the cellulitis case (p<0.001) but not pretest to 9-week follow-up test (p=0.11). A significant difference in pretest to posttest was found for treatment with OMT and rest, ice, and compression in the overuse case (p=0.004) but not on the 9-week follow-up test (p=0.23). No difference was found pretest to posttest for learning the treatment of joint effusion (p=0.195), and a question regarding treatment of prepatellar bursitis was not asked on the written tests.
Questionnaires
Pretraining and posttraining questionnaires included four common questions. Utilizing a 5-point Likert scale (1 strongly agree to 5 strongly disagree), the mean (SD) self-reported student confidence for correctly identifying normal sonographic anatomy of the anterior knee was 3.50 (1.01) at pretraining and 1.59 (0.72) at posttraining (Table 1). The mean (SD) score for perceived ability to differentiate joint effusion, prepatellar bursitis, and cellulitis utilizing point-of-care ultrasound was 4.33 (0.78) at pretraining and 1.99 (0.78) at posttraining. Student confidence for differentiating these three pathologies utilizing palpation/visual inspection alone went from 3.96 (1.09) at pretraining to 2.08 (0.83) at posttraining. The mean (SD) for self-reported student comfort in handling the ultrasound probe was 2.23 (0.73) at pretraining and 1.77 (0.68) at posttraining (all p<0.001).
Student responses to study questionnaires regarding their confidence level with utilizing point-of-care ultrasound.
| Questionnaire itema | Mean (SD) | p-Value | |
|---|---|---|---|
| Pretraining (n=101) | Posttraining (n=95) | ||
| I feel comfortable handling the ultrasound probe and understand what I am seeing on the screen. | 2.23 (0.73) | 1.77 (0.68) | <0.001 |
| I feel confident in my ability to differentiate various normal tissues and anatomic landmarks of the anterior knee, utilizing point-of-care ultrasound. | 3.50 (1.01) | 1.59 (0.72) | <0.001 |
| I can reliably differentiate joint effusion, prepatellar bursitis, and cellulitis of the anterior knee, utilizing point-of-care ultrasound. | 4.33 (0.78) | 1.99 (0.78) | <0.001 |
| I can reliably differentiate joint effusion, prepatellar bursitis, and cellulitis of the anterior knee, based on palpation/visual inspection. | 3.96 (1.09) | 2.08 (0.83) | <0.001 |
| This ultrasound training will change how I diagnose and manage patients who present with a swollen, painful knee. | NA | 1.49 (0.68) | NA |
-
aStudents were asked to rate the extent to which they agreed or disagreed with items. Responses were rated on a 5-point Likert scale, in which 1 was strongly agree and 5 was strongly disagree. Questionnaires were completed immediately before and after our focused ultrasound training. NA, not applicable; SD, standard deviation.
Unique to the posttraining questionnaire, the majority of students (93.6 %, 89/95) agreed or strongly agreed that this ultrasound training would change how they diagnosed and managed patients who presented with a painful, swollen knee (mean [SD]=1.49 [0.68]).
In terms of previous ultrasound knowledge, the pretraining questionnaire showed that prior to our study, 89.1 % (90/101) of students had performed six or fewer ultrasound examinations. On the posttraining questionnaire, students reported that the majority of their ultrasound training was received in the medical school curriculum through synchronous lectures (69.5 %, 66/95), hands-on learning laboratories (90.5 %, 86/95), or asynchronous online materials (29.5 %, 28/95). Only 5.3 % (5/95) had pursued additional training through online videos, podcasts, or tutorials.
Discussion
Clinical evaluation of an undifferentiated painful, swollen knee requires students to refine palpation skills, recognize tissue texture changes, and carefully assess gait to establish a relationship between form and function. Osteopathic physicians recognize that dysfunction in one part of the body can cause compensatory mechanisms that have long-lasting effects, and unless contraindicated, they have a variety of techniques at their disposal to immediately treat what they find. The patient with a painful, swollen knee presents a clinical challenge for students and experienced physicians alike. Incorporating point-of-care ultrasound can help to quickly identify where a fluid collection is located and tissue damage has occurred, allowing for the most appropriate and timely treatment [2].
The current study examined several outcomes after a focused ultrasound training for first-year osteopathic medical students. Specifically, we assessed their ability to differentiate between three primary pathologies of the anterior knee—joint effusion, prepatellar bursitis, and cellulitis—utilizing point-of-care ultrasound. The focused training session utilized in the current study was loosely modeled after similar methods for theme-based teaching [10].
Although teaching medical students to scan normal anatomy is relatively straightforward, it is difficult to guarantee specific pathology in a patient population on any given day. In 2011, Hoppmann et al. [11] studied the ability of 21 fourth-year medical students to detect knee joint effusion utilizing a cadaver model. All 21 (100 %) students correctly scanned and identified the anatomic landmarks and correctly identified the knee with the larger effusion [11]. However, cadavers often have leaky tissues, and the authors also reported their cadavers were clinically static [11], making it difficult to combine ultrasound findings with physical examination skills. Hence, our study sought to combine reliable pathology with examination of a standardized patient in the preclinical environment.
In the current study, we developed what we believe to be a novel approach, in which students successfully combined hand-eye coordination and probe position on the standardized patient with a superimposed prerecorded video clip of the corresponding sonographic anatomy and specific pathological findings that was placed in front of the ultrasound screen at the appropriate time. With this method, most students were able to identify joint effusion or prepatellar bursitis, and nearly all students were able to diagnose cellulitis. This technique could be further studied as a method for assessing students’ ability to identify other pathologic conditions while utilizing point-of-care ultrasound to scan a standardized patient.
Our study also relied on more traditional means of assessment with a written pretest, posttest, and 9-week follow-up test for learning retention. Designated questions on each test asked students to identify joint effusion, prepatellar bursitis, and cellulitis based on an ultrasound image alone. Scores on these questions nearly tripled from pretest to posttest for all three pathologies. Unfortunately, this ability was not completely retained at 9 weeks; only the ability to differentiate prepatellar bursitis and cellulitis was still appreciated. Of the three pathologies, first-year students were best able to recognize key characteristics of cellulitis both on sonographic images in the written posttest and during the hands-on ultrasound assessment. The ability of students to recognize and treat cellulitis immediately after our teaching intervention suggests that commonly taught ultrasound “signs” may be an effective approach in early ultrasound education. For example, the “cobblestone” appearance for cellulitis was the only ultrasound sign taught or tested during our focused training and tests. This finding should be further investigated in future studies aimed at learning retention in point-of-care ultrasound education.
Although our first-year students were able to successfully identify sonographic landmarks and recognize certain pathologies of the anterior knee, translating this to clinical treatment selection proved more challenging. For example, on the written posttest administered immediately after the focused training, the majority of students were able to match ultrasound findings in a clinical vignette to antibiotic treatment for cellulitis; however, this new understanding was lost by the follow-up test 9 weeks later. It should be noted that the focused ultrasound training involved limited time and content that were not addressed elsewhere in the standard curriculum. It appears that while students were able to recognize these three conditions on point-of-care ultrasound, reliable pairing with the appropriate medical management will likely require more in-depth learning and reinforcement throughout the clinical years for better application and retention [12].
In terms of osteopathic treatment, while the majority of students correctly answered the pretest question selecting “OMT and/or rest, ice, compression” for a diagnosis of overuse injury, even before the teaching intervention, there was still a statistically significant increase of correct responses on the posttest for this question. Perhaps once students learned how to confirm a structurally normal knee utilizing ultrasound, their diagnostic confidence was enhanced and willingness to utilize OMT in a case such as this was reinforced.
Replication
Our study found a significant increase in students’ level of confidence for recognizing normal sonographic landmarks and differentiating between joint effusion, prepatellar bursitis, and cellulitis of the anterior knee utilizing ultrasound. A similar protocol could be utilized at other undergraduate medical institutions, whereby the focused ultrasound training could be based on a specific clinical complaint or limited set of possible diagnoses. In this model, we recommend that the teaching intervention be focused, clinically relevant, and as concise as possible. This could be followed by a hands-on assessment incorporating prerecorded video clips of specific sonographic pathology placed in front of the ultrasound screen, which corresponds with probe placement on the standardized patient. As in the current study, written pretests and posttests when combined with pretraining and posttraining questionnaires are useful tools to assess student learning because they are relatively easy to produce and yield valuable insight. Care should also be taken to minimize variability between proctors through the use of specialized instructor training, scripts, and/or checklists. See Figure 3 for an example of the combined script and checklist utilized in the current study.
Limitations
The current study had several limitations. Our sample size was relatively small, and results may have been affected by errors related to self-reported data. One challenge for studies utilizing multiple proctors during assessment is to reduce evaluator bias. We tried to minimize bias in our study by utilizing a large number of proctors with multidisciplinary ultrasound experience, by providing specific proctor training, and through the use of a standardized script and checklist during the hands-on assessment of students. Although these measures likely helped, we still noticed small variations in teaching styles and individual assessment of students. Given the number of outcomes analyzed in the study, we did not perform a separate analysis evaluating uniformity among proctors.
It is difficult to guarantee that specific pathology will be observed on any given day in the clinical setting, and it is even more difficult to ensure in the preclinical years. Therefore, to provide specific findings for our three designated pathologies, we relied on sonographic video clips prerecorded on a digital tablet and placed in front of the ultrasound screen at the appropriate time. Although this protocol is a novel approach, ideally, standardized patients would possess varying degrees of the chosen pathology or, alternatively, the video clips could be loaded directly on the ultrasound system itself, which would help to improve fidelity.
Our protocol deliberately involved a single, focused teaching intervention. Although we did see an immediate increase in student knowledge and self-reported confidence, much of this was lost on the follow-up written test 9 weeks later, and a follow-up hands-on skills assessment was not performed to assess for the retention of technical skills. It should be noted that students were not given additional exposure to the ultrasound content during the 9 weeks leading up to the follow-up written test, which may have affected these scores. In an article about the benefits of spaced repetition, Kang [12] reported that spaced repetition has been shown to benefit memory retention and improve the ability to make what has been learned generalizable to new situations and problem-solving. A recent study by Walsh et al. [13] investigated how repetition of items should be allocated across a fixed number of predetermined sessions to maximize retention. In that study involving 38 participants [13], enhanced learning retention primarily depended on the total number of sessions in which the learner engaged with the content rather than the way in which repetitions occurred. Therefore, it seems reasonable that regular review of the ultrasound content and more frequent scanning opportunities would likely reinforce learning and support retention.
Lastly, the current study took place during OMM laboratory time. Although the initial cohort of students was required to participate in the focused ultrasound training as part of the curriculum, participation in our study was fully voluntary. Therefore, students self-selected to continue participation by completing the written posttest, posttraining questionnaire, and hands-on assessment components of the study and then completing the follow-up written test administered during a subsequent OMM laboratory 9 weeks later. Normal fluctuations in student attendance at laboratory sessions and the choice to continue participating highlight the inherent challenges related to dropout rates that are commonly found in spaced follow-up data collection. Because of these factors, we did not make within-subjects comparisons and all data before and after training were pooled for comparison. To improve participation in future studies, this teaching and testing exercise could be repeated later in the students’ curriculum, when the students are more experienced with ultrasound-based medical education. A different clinical case, centered around a limited number of specific diagnoses, could be utilized.
Conclusions
In the current study, a focused ultrasound training session was effective at immediately increasing the knowledge and confidence of first-year osteopathic medical students in the assessment of the anterior knee. However, results from the follow-up written test 9 weeks later suggested that students did not retain some of their learned knowledge. In the future, medical educators and researchers may want to consider including repetition of content and spaced practice utilizing a series of similarly focused training sessions to improve learning retention and future clinical application utilizing point-of-care ultrasound.
Acknowledgments
The authors would like to thank Asad Patanwala, PharmD, MPH (University of Arizona, Tucson, AZ) for data analysis and interpretation; Deborah Goggin, MA, ELS (scientific writer in the Department of Research Support, A.T. Still University, Kirksville, MO); and Nicole Davidson, PA (A.T. Still University, Mesa, AZ) who proofread this manuscript and provided feedback.
-
Research funding: None reported.
-
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; C.W., I.R.S.M., and S.A. drafted the article or revised it critically for important intellectual content; all authors contributed to the analysis and interpretation of data; all authors final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None reported.
-
Informed consent: Each student provided written informed consent prior to participation.
References
1. Kane, D, Balint, PV, Sturrock, RD. Ultrasonography is superior to clinical examination in the detection and localization of knee joint effusion in rheumatoid arthritis. J Rheumatol 2003;30:966–71.Search in Google Scholar
2. Adhikari, S, Blaivas, M. Utility of bedside sonography to distinguish soft tissue abnormalities from joint effusions in the emergency department. J Ultrasound Med 2010;29:519–26. https://doi.org/10.7863/jum.2010.29.4.519.Search in Google Scholar PubMed
3. Birrane, J, Misran, H, Creaney, M, Shorten, G, Nix, CM. A scoping review of ultrasound teaching in undergraduate medical education. Med Sci Educ 2018;28:45–56. https://doi.org/10.1007/s40670-017-0491-4.Search in Google Scholar
4. Dinh, VA, Dukes, WS, Prigge, J, Avila, M. Ultrasound integration in undergraduate medical education: comparison of ultrasound proficiency between trained and untrained medical students. J Ultrasound Med 2015;34:1819–24. https://doi.org/10.7863/ultra.14.12045.Search in Google Scholar PubMed
5. Rao, S, van Holsbeeck, L, Musial, JL. A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: a pioneer year review. J Ultrasound Med 2008;27:745–9. https://doi.org/10.7863/jum.2008.27.5.745.Search in Google Scholar PubMed
6. Kondrashova, T, Lockwood, MD. Innovative approach to teaching osteopathic manipulative medicine: the integration of ultrasonography. J Am Osteopath Assoc 2015;115:212–20. https://doi.org/10.7556/jaoa.2015.043.Search in Google Scholar PubMed
7. Amini, R, Stolz, LA, Breshears, E. Assessment of ultrasound-guided procedures in preclinical years. Intern Emerg Med 2017;12:1025–31. https://doi.org/10.1007/s11739-016-1525-4.Search in Google Scholar PubMed
8. Vora, RS, Kinney, MN. Connectedness, sense of community, and academic satisfaction in a novel community campus medical education model. Acad Med 2014;89:182–7. https://doi.org/10.1097/ACM.0000000000000072.Search in Google Scholar PubMed
9. Kirkpatrick, JN, Davis, A, Decara, JM. Hand-carried cardiac ultrasound as a tool to screen for important cardiovascular disease in an underserved minority health care clinic. J Am Soc Echocardiogr 2004;17:399–403. https://doi.org/10.1016/j.echo.2004.01.016.Search in Google Scholar PubMed
10. Amini, R, Stolz, LA, Gross, A. Theme-based teaching of point-of-care ultrasound in undergraduate medical education. Intern Emerg Med 2015;10:613–8. https://doi.org/10.1007/s11739-015-1222-8.Search in Google Scholar PubMed
11. Hoppmann, R, Hunt, P, Louis, H. Medical student identification of knee effusion by ultrasound. ISRN Rheumatol 2011;2011:874596. https://doi.org/10.5402/2011/874596.Search in Google Scholar PubMed PubMed Central
12. Kang, SHK. Spaced repetition promotes efficient and effective learning: policy implications for instruction. Policy Insights Behav Brain Sci 2016;3:12–9. https://doi.org/10.1177/2372732215624708.Search in Google Scholar
13. Walsh, MM, Krusmark, MA, Jastrembski, T, Hansen, DA, Honn, KA, Gunzelmann, G. Enhancing learning and retention through the distribution of practice repetitions across multiple sessions. Mem Cognit 2023;51:455–72. https://doi.org/10.3758/s13421-022-01361-8.Search in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2022-0186).
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Case Report
- Sudden cardiac death in a young male endurance athlete
- General
- Original Article
- Optimal hand surgery fellowship interview format
- Medical Education
- Original Articles
- Effects of a focused training on first-year osteopathic medical students’ ability to incorporate point-of-care ultrasound in assessment of the anterior knee
- A student-driven mindfulness curriculum for first-year osteopathic medical students: a pilot study
- Obstetrics and Gynecology
- Original Article
- Implementation of an enhanced recovery after surgery (ERAS) protocol for total abdominal hysterectomies in the division of gynecologic oncology: a network-wide quality improvement initiative
- Public Health and Primary Care
- Brief Report
- Diabetic ketoacidosis diagnosis in a hospital setting
- Clinical Image
- Acute generalized exanthematous pustulosis with systemic involvement
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Case Report
- Sudden cardiac death in a young male endurance athlete
- General
- Original Article
- Optimal hand surgery fellowship interview format
- Medical Education
- Original Articles
- Effects of a focused training on first-year osteopathic medical students’ ability to incorporate point-of-care ultrasound in assessment of the anterior knee
- A student-driven mindfulness curriculum for first-year osteopathic medical students: a pilot study
- Obstetrics and Gynecology
- Original Article
- Implementation of an enhanced recovery after surgery (ERAS) protocol for total abdominal hysterectomies in the division of gynecologic oncology: a network-wide quality improvement initiative
- Public Health and Primary Care
- Brief Report
- Diabetic ketoacidosis diagnosis in a hospital setting
- Clinical Image
- Acute generalized exanthematous pustulosis with systemic involvement

