Abstract
Context
Opioid abuse has developed into a public health emergency within the last decade because opioid medications, while addictive, are effective and commonly used for pain management. In 2016, over 42,000 deaths were attributed to opioids. Chronic pain affects about 50% of people experiencing homelessness in the US, and they have a higher overall rate of chronic pain than the general population; opioids are among the methods they might use to manage that pain. Complementary and alternative therapies for pain management have largely gone unexplored in the homeless population.
Objectives
To determine, among people experiencing homelessness, the willingness to use and current use of complementary and alternative treatments (physical and massage therapy, chiropractic treatments). A secondary objective was to investigate awareness and perception of osteopathic manipulative treatment (OMT) as a complementary treatment for chronic pain among the homeless population.
Methods
A 32 question survey was administered verbally to guests of True Worth Place Homeless Shelter in Fort Worth, Texas in three 4 hour sessions from February 2019 to April 2019. If participants gave verbal consent, a researcher read the questionnaire, one question at a time, and recorded the participant’s responses. The survey included queries for opioid and nonopioid treatment modalities (physical and massage therapy, chiropractic, and OMT) to assess the perception of and current use of each among the population. Appropriate nonparametric statistical analysis was conducted to assess significance and correlations among the treatment groups.
Results
Of the 200 survey participants, 126 (91.3%) reported a history of opiate use for pain, but 136 (68.0%) believed that a nondrug pain intervention could better treat their pain. Additionally, 150 participants (75.0%) believed that regular manipulation, including OMT, would decrease their need for pain medications. Participants with a history of opioid use for pain were more likely to believe that the availability of regular manipulation, including OMT, at True Worth Place could decrease their need for pain medication (odds ratio=3.7143; 95% confidence interval=1.6122–8.5572; p=0.0009). Moreover, some participants (141; 70.5%) were already pursuing nondrug pain management modalities such as PT, massage therapy, and chiropractic care. The greatest barriers to receiving OMT were transportation and cost.
Conclusions
This survey study was conducted to determine whether a homeless population would be willing to use nonopioid treatment, particularly OMT, for chronic pain management. Results revealed both a willingness to use and a previous use of nonopioid treatments for pain, along with a high prevalence of opiate use. Despite limited exposure to OMT, this population reported being potentially willing to pursue manipulation, including OMT, as a complementary treatment for pain relief alongside opioids if readily available.
Pain is a complex biopsychosocial phenomenon and opioids provide a temporary reduction of pain through analgesic effects and a rewarding release of dopamine [1]. This release of dopamine, alongside other endorphins, contributes to the addictive nature of opioids. In 2016 alone, there were over 42,000 deaths due to opioid overdose [2], yet opioids are still commonly prescribed to treat pain.
A significant portion of people experiencing homelessness also have chronic pain. Approximately 50% of the homeless population in the United States report chronic pain, and this population has higher overall rates of chronic pain than the general population [2], [3]. The total number of people experiencing homelessness in the United States was reported to be 552,830 in 2019 [4]. In 2010, Texas reported 25,848 people experiencing homelessness, with 2,028 living in Tarrant County [5], [6]. Of the homeless population in Tarrant County, 64% are men and 36% are women [6]. True Worth Place (TWP) is one of the 18 homeless shelters in Fort Worth, Texas, a city in Tarrant County. Guests must be at least 18 years old to enter the shelter. According to internal (unpublished) data from TWP, they hosted 8,476 guests and served an average of 477 guests per day from April 1 to December 31, 2019. Internal data collected by a TWP representative also showed that the population at TWP in 2019 was 34.7% women, 65.1% men, 0.2% of a sex or gender not reported, with 48.2% White, 50.1% Black, 0.5% Asian, and 1.2% of a race or ethnicity not reported.
Previous literature has documented that over the counter medications, alcohol, and drugs, which include prescription and illicit opioids, are common treatments for pain amongst people experiencing homelessness [2], [7], although no prior literature (to our knowledge) has compared the use rates of these treatments between the homeless and general populations. Use and efficacy of complementary and alternative therapies for pain treatment in the adult homeless population has been underexplored, but the use of complementary and alternative medicine (CAM) in a pediatric homeless population has been previously studied [8]. CAM in that study included chiropractic techniques, acupuncture, naturopathy, herbal medicines, massages, megavitamins, homeopathy, aromatherapy, and meditation. The results showed that 137 of the 157 (87.3%) CAM participants achieved “some” or “a lot” of pain relief [8]. Again, we were only able to identify one article [8] that examined the use of CAM therapies – such as OMT, chiropractic treatment, massage therapy, and physical therapy – to relieve pain in the homeless population, and there have been no studies regarding the adult homeless population’s perception of this mode of treatment.
This survey study was conducted to investigate willingness to use and current use of CAM treatments (physical and massage therapy, chiropractic treatments) among the homeless adult population at TWP as well as their awareness and perception of osteopathic manipulative treatment (OMT) as a complement to opioids for the treatment of chronic pain. The aim of this study was to serve as a foundation to understand the willingness of individuals who are experiencing homelessness to pursue nonopioid treatments (physical and massage therapy, chiropractic treatments, and OMT) for chronic pain, so that this data might support future efforts increase the utilization of OMT as an adjunct to chronic pain management or replacement for opiate use in the homeless population to address the opioid crisis.
Methods
Participants
The 200 voluntary participants interviewed for this study were guests of TWP in Fort Worth, Texas and were not screened for opioid addiction or use of pain medication before beginning the questionnaire. TWP was chosen because the shelter is a site for the University of North Texas Health Science Center’s (UNTHSC) Homeless Outreach through Medical Education (HOME) Clinic. TWP provided written consent allowing research to take place at their location. This study was approved by North Texas Regional Institutional Review Board (IRB# 1340830-1).
Materials
A consent form was provided to participants that outlined the purpose of the study, risks and benefits, an agreement to participate, a confidentiality statement, instructions on how to leave the study, and contact information for the principal investigator for questions after completion of the study. Other materials included a page defining terms used in the survey, stamp cards provided by TWP, stamps borrowed from TWP, and the survey (Supplementary Material). (One stamp on the TWP stamp card was given upon completion of the questionnaire; the stamp cards could be redeemed at TWP for laundry, lunch, toiletries, clothing, et cetera.) The stamp cards were provided by TWP and the stamps were borrowed and returned to TWP upon completion of the study at no cost to the investigators. The survey was designed by the researchers (K.F., J.B., A.P.) and is not validated nor based on a validated survey. It included three demographic questions about the participants’ age, sex, and ethnicity in an open ended format, as well as 22 binary (yes/no) questions and seven multiple choice questions, one of which had a free response option. These questions assessed the perception and current use of each of the opioid and nonopioid treatment modalities (physical and massage therapy, chiropractic treatments, and OMT) among the study population. The questionnaire did not collect any protected health information (PHI) that could be used to identify the study subjects.
Design and procedure
Surveys (Supplementary Material) were conducted during three 4 hour sessions from February 2019 to April 2019 during the hours of the UNTHSC HOME Clinic. Participants were included in the study if they were over 18 years of age and English-speaking. Exclusion criteria included pregnancy (determined by asking if the participant was pregnant), cognitive impairment (determined by if the participant could verbally demonstrate they understood information presented in the consent process), and employment at TWP. Participants were approached in the common areas of TWP by researchers clearly identifiable as UNTHSC students (K.F., J.B., H.N., F.P., A.W.) and were asked if they were interested in participating in a questionnaire. Potential participants were explicitly told they had the right to refuse to participate at any time during the survey. If they agreed to participate, the researcher verbally reviewed the consent form with the participant. If the participant needed clarification about different terms, they were provided with standardized definitions and examples. OMT was described as, “OMT is a hands-on approach performed by physicians to treat pain caused by bones, muscles, and nerves.” Physical therapy was described as, “Physical therapy is a way to treat injuries that include exercise, stretching, and massage.” Massage therapy was defined as, “A massage therapist uses his or her hands to rub muscles and joints of the body to relieve pain.” Chiropractic treatments were described as, “Chiropractors use hands-on manipulation to align the body’s bones, particularly the spine.” Examples of opioid medications included, “Tylenol 3, Tylenol 4, Ultram, Oxycontin, methadone, and morphine.” If the participant gave verbal consent after reviewing the consent form, the researcher read the questionnaire, one question at a time, and recorded the participant’s responses through multiple choice, binary, and free text components on a paper questionnaire. After the questionnaire was completed, the participants received the consent form for their records and one stamp on their TWP stamp card.
Data analysis
At the end of each session, survey responses were recorded by the student researchers (K.F., J.B.) on a spreadsheet. The survey responses were exported to the NCSS software package (NCSS 11 Statistical Software 2016; NCSS LLC) for analysis. Appropriate descriptive statistics for nonparametric data were selected to test for significant differences between the five treatment modalities (opiates, OMT, physical therapy, chiropractic, and massage therapy) addressed in the survey. For binary response questions, Cochran’s Q test was first employed to test for significance (p<0.05) amongst the groups, followed by multiple comparisons using absolute difference to test for pairwise proportional differences among treatment groups. The correlation between two nonparametric variables was tested by calculating the odds ratio (OR) and confidence interval (CI); significance was verified by McNemar test (p<0.05).
Results
Table 1 shows the demographics of the participants surveyed at TWP. Of the 200 participants, 121 were men (60.5%), 77 were women (38.5%), and 2 answered “N/A” when queried about gender (1%). Eighty-two participants were White (41%), 89 were Black (44.5%), 13 were Hispanic (6.5%), 1 was Asian (0.5%), and 15 selected “other” as their self reported ethnicity (7.5%). The youngest participant was 19 years old and the oldest was 74 years old (mean age, 50 years). Table 1 also lists the national demographics of the homeless population from 2019 for comparison.
Participant and 2019 national demographics.
| True Worth Place population | National population [12] (n=552,830) | |
|---|---|---|
| Characteristic | n (%) | % |
| Sex | ||
| Men | 121 (60.5%) | 70% |
| Women | 77 (38.5%) | 30% |
| N/A | 2 (1.0%) | |
| Race | ||
| White | 82 (41.0%) | 50% |
| Black | 89 (44.50%) | 40% |
| Asian | 1 (0.50%) | 1% |
| Not reported or “other” | 28 (14.0%) | 9% |
| Total | 200 (100%) | |
| Age, years, mean (range) | 50 (19–74) | |
As Table 2 demonstrates, the majority of survey respondents (134; 67.0%) had taken opiate pain medicine before. Thirty-one participants (15.6%) reported having heard of OMT before study participation and 14 participants (7.0%) had previously received OMT (Figure 1). Of the 14 people who had received OMT previously, 12 (85.7%) received OMT for pain, and all 12 reported improvement in their pain levels.
Survey responses.
| Survey item | Yes, n (%) | No, n (%) | Total responses |
|---|---|---|---|
| Opiate medicine | |||
| Have you taken opiate pain medicine before? | 134 (67.0%) | 66 (33.0%) | 200 |
| Did you take the opiate pain medicine for pain? | 126 (91.3%) | 12 (8.7%) | 138 |
| Osteopathic manipulative treatment | |||
| Have you ever heard of OMT (Osteopathic Manipulative Treatment)? | 31 (15.6%) | 168 (84.4%) | 199 |
| Have you ever had OMT (Osteopathic Manipulative Treatment)? | 14 (7.0%) | 185 (93.0%) | 199 |
| Did you go to OMT because you had pain? | 12 (85.7%) | 2 (14.3%) | 14 |
| Did OMT improve your pain? | 12 (100.0%) | 0 (0.0%) | 12 |
| Physical therapy | |||
| Have you ever had physical therapy before? | 119 (59.5%) | 81 (40.5%) | 200 |
| Did you go to physical therapy because you had pain? | 104 (88.1%) | 14 (11.9%) | 118 |
| Did physical therapy improve your pain? | 78 (75.0%) | 26 (25.0%) | 104 |
| Massage therapy | |||
| Have you ever had massage therapy before? | 77 (38.7%) | 122 (61.3%) | 199 |
| Did you get the massage because you had pain? | 62 (80.5%) | 15 (19.5%) | 77 |
| Did massage improve your pain? | 58 (93.5%) | 4 (6.5%) | 62 |
| Chiropractics | |||
| Have you ever been to a chiropractor? | 82 (41.0%) | 118 (59.0%) | 200 |
| Did you go to the chiropractor because you had pain? | 78 (95.1%) | 4 (4.9%) | 82 |
| Did the chiropractic treatment improve your pain? | 62 (79.5%) | 16 (20.5%) | 78 |
| Non-drug pain intervention | |||
| Do you think a non-drug pain intervention would be better to treat your pain? | 136 (68.0%) | 64 (32.0%) | 200 |
| If you could receive regular manipulation at this clinic, do you believe it would decrease your need for pain medications? | 150 (77.3%) | 44 (22.7%) | 194 |
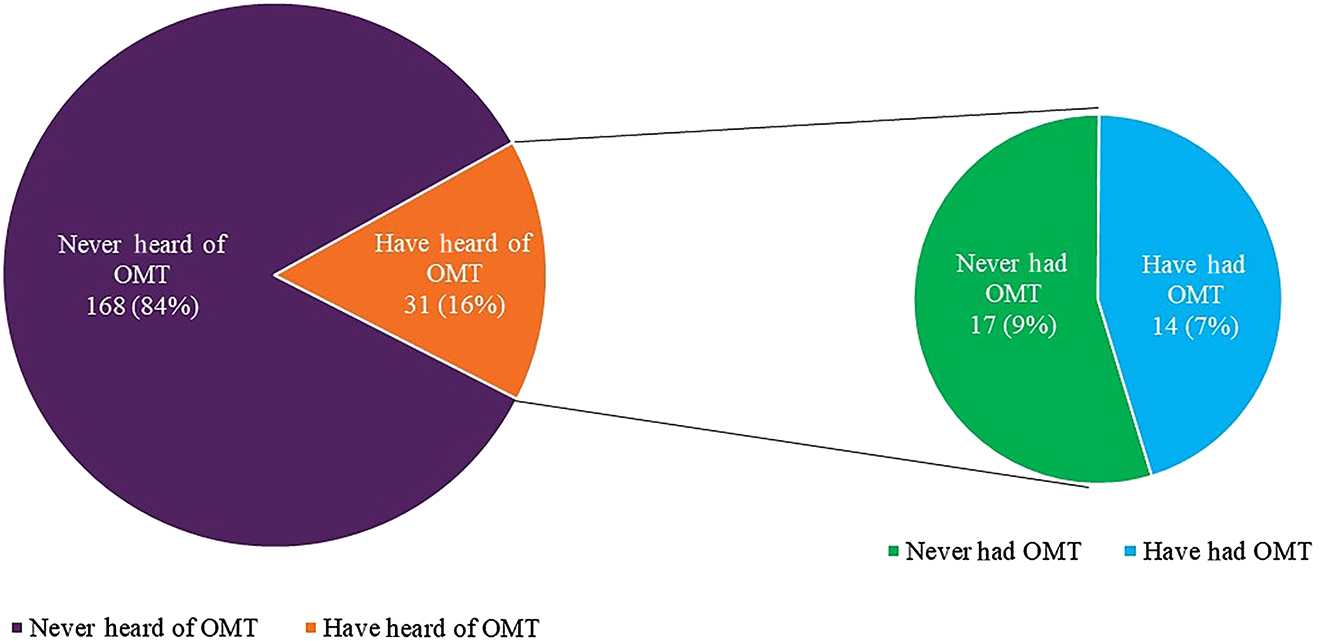
Prior exposure of guests at True Worth Place homeless shelter to osteopathic manipulative treatment (OMT). Of 199 respondents to the relevant question, 15.6% (n=31) had heard of OMT, and 7% (n=14) had previously received OMT.
When excluding OMT from analysis due to a small number of respondents having utilized OMT in the past, results revealed no difference when comparing which treatment modalities had been pursued for pain relief (χ2=2.3077; df=3; p=0.5111). However, of those who reported that they had received CAM treatments for their pain, 78 of 104 (75.0%) reported that physical therapy improved their pain, 62 of 78 (79.5%) reported that chiropractic treatments improved their pain, 58 of 62 (93.5%) reported that massage therapy improved their pain, and 12 of 12 (100%) reported that OMT improved their pain (Table 2).
Cochran’s Q test (Table 3) indicated a significant difference among the utilization of the five treatment modalities (χ2=199.6901; df = 4; p<0.0001). The greatest difference in the absolute proportion was between opiates and OMT at 60.1% followed by OMT and PT at 52.5%. There was no difference between opiates and physical therapy (p=0.086) nor between massage therapy and chiropractic treatments (p=0.649). Multiple comparisons using the McNemar test (Table 3) further demonstrated similar patterns with significant differences and the greatest difference was seen between opiates and OMT (χ2=115.13; p<0.0001).
Analysis of Cochran’s Q test and McNemar test comparing respondents’ history of treatment options.
| χ2 | df | p-Value* | |
|---|---|---|---|
| Cochran’s Q test | 199.6901 | 4 | <0.0001 |
| Cochran’s Q test multiple comparisons | McNemar multiple comparison test | ||
| Treatment comparison | |π1−π2| | χ2 | p-Value* |
| Opiate – Osteopathic manipulative treatment | 60.1 | 115.13 | <0.0001 |
| Opiate – Physical therapy | 7.58 | 3.3582 | 0.0864 |
| Opiate – Massage therapy | 28.28 | 34.087 | <0.0001 |
| Opiate – Chiropractic treatment | 25.76 | 31.3373 | <0.0001 |
| OMT – Physical therapy | 52.53 | 98.3273 | <0.0001 |
| OMT – Massage therapy | 31.82 | 55.9017 | <0.0001 |
| OMT – Chiropractic treatment | 34.34 | 62.4865 | <0.0001 |
| Physical therapy – Massage therapy | 20.71 | 20.7531 | <0.0001 |
| Physical therapy – Chiropractic treatment | 18.18 | 17.5135 | <0.0001 |
| Massage therapy – Chiropractic treatment | 2.53 | 0.3247 | 0.6488 |
* Bold values indicate statistical significance (p-Value ≤0.05).
Despite high use of opiates for pain relief amongst the participants who had used opiate pain medication in the past (126 of 138; 91.3%), a majority of all study participants believed that a nondrug intervention would be better to treat their pain (136; 68.0%) and that receiving regular manipulation at TWP would decrease their need for pain medication (150; 77.3%). Also, 141 (70.5%) participants had already pursued nonopioid treatments for pain. Those who had taken opiates for pain in the past (138; 69.0%) were more likely to believe that regular availability of manipulation at TWP place could decrease their need for pain medication (OR=3.7143; 95% CI=1.6122–8.5572; p=0.0009). Participants who believed that regular availability of manipulation at TWP could decrease their need for pain medications (150; 75.0%) were more likely to believe that a nondrug pain intervention would be better to treat their pain (OR=1.8095; 95% CI=1.0620–3.0833; p=0.0269).
When respondents were asked which barriers limited them from seeking or continuing manipulation as treatment for pain, cost (100; 50.0%) and transportation (131; 65.5%) were the most frequently reported factors (Figure 2).
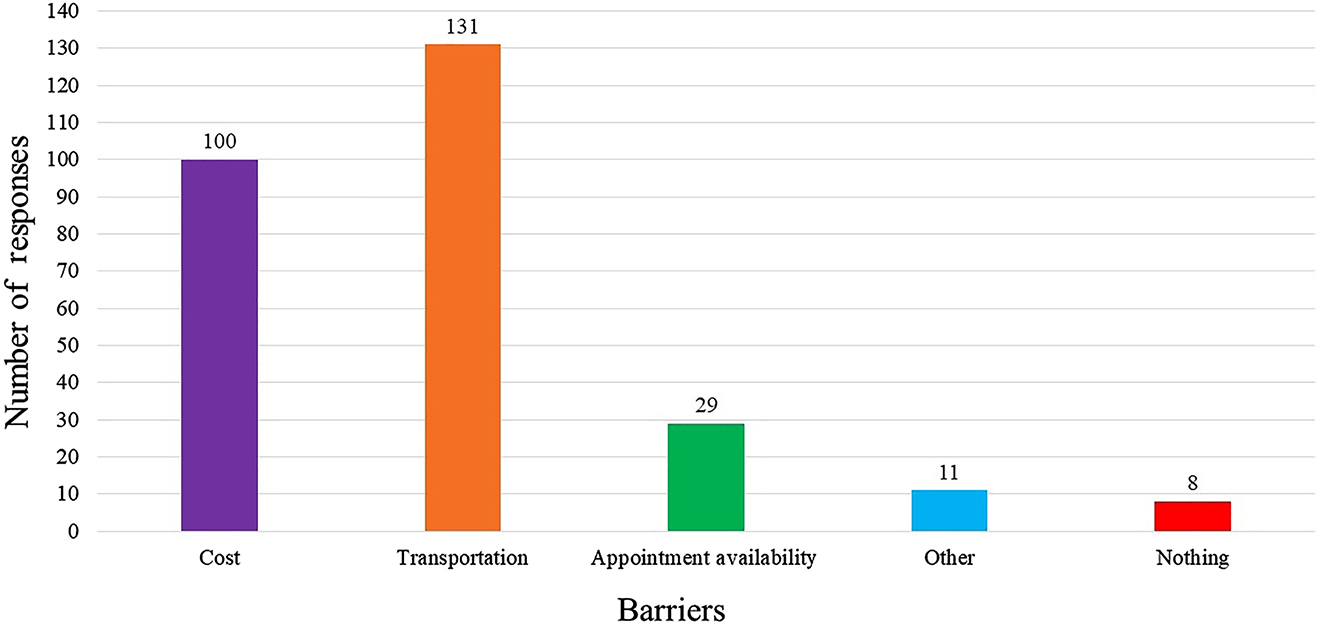
Reported barriers to receiving manipulation at True Worth Place homeless shelter.*
* Participants were allowed to choose more than one factor. There was one open ended response recorded as “other,” which 11 participants reported. In the “other” category, the most commonly reported barrier was “insurance” (5; 45.5%).
Discussion
Pain relief is one of the most significant motivators for opioid use [9]. The homeless population is at an increased risk of opioid abuse because they have higher rates of chronic pain than the general population [2], [3]. This survey study explored the knowledge and willingness of people experiencing homelessness to pursue nondrug pain interventions to address chronic pain.
Previous literature has shown that the homeless population suffers from a higher rate of both chronic pain and opioid use and misuse [2, 3, 7]. Of our study population, 67.0% had taken opiate pain medication before; 91.3% of those took it to treat pain. Previous studies have also identified the need for nonopioid treatments for pain [1, 10, 11], and one [8] explored the use of complementary and alternative treatments for pain. That previous study [8] explored the use of complementary and alternative treatments for pain but did not incorporate OMT, whereas we explored previous exposure to and willingness to utilize OMT as a complementary treatment for pain among a population of people experiencing homelessness.
Overall, the total number of people experiencing homelessness in the United States was reported to be 552,830 in 2019 [4]. While our sample at TWP consisted of only 200 participants, our population proportions were representative of the national demographics of the overall US homeless population. In the US in 2019, 70% of the homeless population were men; likewise, 60.5% were men [6]. Also in 2019, the racial/ethnic makeup of people experiencing homelessness was reported to be 50% White, 40% Black, 1% Asian, and 9% “other.” [12] Similarly, our study population was 47.5% White, 44.5% Black, 0.5% Asian, and 7.5% “other.”
Our results showed that participants who had taken opiates for pain were more likely to believe that OMT could decrease their need for pain medication. More importantly, the option of increased availability of regular manipulation such as OMT was positively correlated with the belief that a nondrug pain intervention would be a better management strategy for pain. These results suggest that even with history of opiate use for pain, participants were likely to believe that a nondrug pain intervention would be a better way to treat their pain if a service like OMT was readily available to them at locations like TWP.
Of the treatment modalities experienced by the participants in the study, OMT was significantly underutilized compared with the other four treatment modalities. The disparity in use of OMT as a treatment modality may be due to the lack of exposure of this population to OMT, as only 15.6% reported having heard of OMT before this study. However, despite only 12 participants having previously received OMT for pain, all noted improvement of their pain level. This demonstrates that there is a potential to increase this population’s exposure to OMT and decrease their pain by utilizing OMT. Despite limited exposure to OMT, many participants (150; 75.0%) still believed that OMT could decrease their need for opiates. The lack of statistical difference among those who had pursued specific CAM modalities for pain demonstrates that the homeless population surveyed is already pursuing adjunct treatment to relieve their pain. Although we had to exclude OMT from that analysis due to the small number of people who had previously utilized OMT, our correlational results and their current pursuant of adjunct treatment for pain suggest that if manipulation pain management options, such as OMT, were more widely available, more individuals would pursue it as a treatment option.
The studied population had an apparent willingness to try nonopioid treatments for pain. However, the most common potential barriers to seeking adjunct modalities reported by participants in our study were transportation followed by cost, appointment availability, and other factors such as insurance.
Chronic pain and mental health
Although the causational relationship is unclear, it is known that addiction, depression, and other mental disorders are associated with chronic pain [2], [13]. In some individuals, these mental health issues are due secondarily to their pain, but in others, mental health issues predate the onset of pain. Oftentimes, the presence of these psychiatric issues exacerbates the degree of pain felt by patients and also impedes the rate and significance of recovery [13]. OMT has shown to decrease mental health issues in various studies and more recent studies have addressed the biopsychosocial aspect of OMT treatment [14], [15], [16]. The ROMANS trial found that OMT had significant improvement on short and long term psychological outcomes, even after the physical effects of OMT were no longer significantly different from the control group [16]. In a more recent study, the results revealed that OMT was effective in reducing chronic pain, anxiety, and other psychiatric disorders [14]. A major component of OMT focuses on the musculoskeletal aspect of the human body and can address the physicality of chronic pain. However, these studies show that mental health is implicated in chronic pain, and OMT could potentially address chronic pain, not only at a physical level, but also in cognitive and emotional facets of health. This is especially important as chronic pain and mental health issues are highly prevalent in the homeless population [2], [3].
Limitations
One of the limitations of our study is that we did not collect any PHI, so we were unable to prevent repeated sampling. TWP is a short term facility with approximately 8,500 guests per year, so the spacing of questionnaire dates helped decrease the risk of repeat surveys and convenience sampling. To avoid repeat sampling in future studies, PHI could be collected or a question could be added to query about previous participation.
Our survey not being validated could have potentially added bias into the study, and the interpretation of the data is therefore limited. There were multiple surveyors; however, the survey conducted consisted of categorical answers and the free responses in the comment section were not included in the analysis. Moreover, two researchers (K.F., J.B.) were responsible for recording all survey responses.
Because the researchers identified themselves as students from an osteopathic medical school, there may have been reporting bias in the answers, as participants could have provided answers that favored OMT and the osteopathic curriculum. Another limitation is potential sampling bias, as some participants may have been more motivated to participate to acquire stamps to redeem for TWP amenities and services.
One aspect that we did not address was the efficacy of opioid medication on decreasing pain in this population. This was a survey study with the purpose of assessing the willingness of the homeless population to pursue OMT as an adjunct treatment for pain. Although we are unsure whether participants were using opioids during the timeframe that they received OMT treatment (for those who did), our population demonstrated current use of alternate pain management methods and a willingness to try manipulation, including OMT, with increased availability. As such, further research is needed to investigate whether increased OMT awareness and knowledge in this population would affect their utilization of OMT. Efficacy could also be studied by assessing pre- and posttreatment pain levels among guests at homeless shelters, as well as how OMT treatment would affect other biopsychosocial aspects of pain such as addiction, depression, anxiety, and posttraumatic stress disorder.
Conclusions
This is a survey study focusing on the perception of a homeless population regarding nonopioid treatment options for pain. Despite the high proportion of this population having used opiates for pain medication previously, the study revealed that they were already pursuing complementary or alternative treatments for pain. Although there was a reported lack of exposure to OMT, individuals experiencing homelessness were willing to pursue manipulation, including OMT, as a complementary treatment for pain if readily available. Moreover, all participants who had received OMT for pain reported improvement in pain levels. All conclusions made herein are based on a nonvalidated survey; therefore, future studies should utilize a validated survey tool to validate our results.
Research funding: None reported.
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests: None reported.
Informed consent: All participants in this study provided informed consent.
Ethical approval: This study was approved by the North Texas Regional Institutional Review Board (IRB# 1340830-1).
References
1. Garland, EL. Treating chronic pain: the need for non-opioid options. Expet Rev Clin Pharmacol 2014;7:545–50. https://doi.org/10.1586/17512433.2014.928587.Search in Google Scholar PubMed
2. Vogel, M, Frank, A, Choi, F, Strehlau, V, Nikoo, N, Nikoo, M, et al.. Chronic pain among homeless persons with mental illness. Pain Med 2017;18:2280–8. https://doi.org/10.1093/pm/pnw324.Search in Google Scholar PubMed
3. Landefeld, JC, Miaskowski, C, Tieu, L, Ponath, C, Lee, CT, Guzman, D, et al.. Characteristics and factors associated with pain in older homeless individuals: results from the health outcomes in people experiencing homelessness in older middle age (HOPE HOME) study. J Pain 2017;18:1036–45. https://doi.org/10.1016/j.jpain.2017.03.011.Search in Google Scholar PubMed PubMed Central
4. The Council of Economic Advisors. The state of homelessness in America. WhiteHouse.gov, https://www.whitehouse.gov/wp-content/uploads/2019/09/The-State-of-Homelessness-in-America.pdf Published September 2019.Search in Google Scholar
5. Texas Homelessness Statistics. Usich.gov, https://www.usich.gov/homelessness-statistics/tx Published 2019.Search in Google Scholar
6. 2019 State of the Homeless Address. AhomeWithHope.org, https://www.ahomewithhope.org/wp-content/uploads/2019/03/SOHA-FTW-2019-FINAL2.pdf Published March 21, 2019.Search in Google Scholar
7. Hwang, SW, Wilkins, E, Chambers, C, Estrabillo, E, Berends, J, MacDonald, A. Chronic pain among homeless persons: characteristics, treatment, and barriers to management. BMC Fam Pract 2011;12:73. https://doi.org/10.1186/1471-2296-12-73.Search in Google Scholar PubMed PubMed Central
8. Breuner, CC, Barry, PJ, Kemper, KJ. Alternative medicine use by homeless youth. Arch Pediatr Adolesc Med 1998;152:1071–5. https://doi.org/10.1001/archpedi.152.11.1071.Search in Google Scholar PubMed
9. Han, B, Compton, WM, Blanco, C, Crane, E, Lee, J, Jones, CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 national survey on drug use and health. Ann Intern Med 2017;167:293–301. https://doi.org/10.7326/M17-0865.Search in Google Scholar PubMed
10. Jerome, JA. An osteopathic approach to chronic pain management. J Am Osteopath Assoc 2017;117:306–14. https://doi.org/10.7556/jaoa.2017.056.Search in Google Scholar PubMed
11. Licciardone, JC, Schultz, MJ, Amen, B. Osteopathic manipulation in the management of chronic pain: current perspectives. J Pain Res 2020;13:1839–47. https://doi.org/10.2147/JPR.S183170.Search in Google Scholar PubMed PubMed Central
12. State of Homelessness. 2020 edition. EndHomelessness.org, https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness-2020 Published 2020.Search in Google Scholar
13. Osterweis, M, Kleinman, A, Mechanic, D. Pain and disability: clinical, behavioral, and public policy perspectives. Institute of medicine (US) committee on pain, disability, and chronic illness behavior. Psychiatr Aspects Chron Pain 1987;9.Search in Google Scholar
14. Edwards, DJ, Toutt, C. An evaluation of osteopathic treatment on psychological outcomes with patients suffering from chronic pain: a prospective observational cohort study collected through a health and well-being academy. Health Psychol Open 2018;5. https://doi.org/10.1177/2055102918774684.Search in Google Scholar PubMed PubMed Central
15. Plotkin, BJ, Rodos, JJ, Kappler, R, Schrage, M, Freydl, K, Hasegawa, S, et al.. Adjunctive osteopathic manipulative treatment in women with depression: a pilot study. J Am Osteopath Assoc 2001;101:517–23.Search in Google Scholar
16. Williams, NH, Wilkinson, C, Russell, I, Edwards, RT, Hibbs, R, Linck, P, et al.. Randomized osteopathic manipulation study: pragmatic trial for spinal pain in primary care. Fam Pract 2003;20:662–9. https://doi.org/10.1093/fampra/cmg607.Search in Google Scholar PubMed
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/jom-2020-0239).
© 2021 Kristina A. Fraser et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Physician wellbeing – what do physicians want?
- Medical Education
- Original Articles
- Meaningful use of COMSAE Phase 1 in preparation for COMLEX-USA Level 1
- The role of extracurricular activities and lectures in mitigating medical student burnout
- Musculoskeletal Medicine and Pain
- Original Article
- Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Cost comparison of osteopathic manipulative treatment for patients with chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Perceptions of nonopioid treatment for pain in a homeless population
- Brief Report
- Osteopathic manipulative medicine in the management of headaches associated with postconcussion syndrome
- Public Health and Primary Care
- Original Article
- National disparities in colorectal cancer screening in patients with comorbid conditions: an analysis of the Behavioral Risk Factor Surveillance System
- Clinical Image
- Orange palpebral spots
Articles in the same Issue
- Frontmatter
- Editorial
- Physician wellbeing – what do physicians want?
- Medical Education
- Original Articles
- Meaningful use of COMSAE Phase 1 in preparation for COMLEX-USA Level 1
- The role of extracurricular activities and lectures in mitigating medical student burnout
- Musculoskeletal Medicine and Pain
- Original Article
- Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Cost comparison of osteopathic manipulative treatment for patients with chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Perceptions of nonopioid treatment for pain in a homeless population
- Brief Report
- Osteopathic manipulative medicine in the management of headaches associated with postconcussion syndrome
- Public Health and Primary Care
- Original Article
- National disparities in colorectal cancer screening in patients with comorbid conditions: an analysis of the Behavioral Risk Factor Surveillance System
- Clinical Image
- Orange palpebral spots

