Abstract
Context
Chronic low back pain (cLBP) is the second leading cause of disability in the United States, with significant physical and financial implications. Development of a multifaceted treatment plan that is cost effective and optimizes patients’ ability to function on a daily basis is critical. To date, there have been no published prospective studies comparing the cost of osteopathic manipulative treatment to that of standard care for patients with cLBP.
Objectives
To contrast the cost for standard of care treatment (SCT) for cLBP with standard of care plus osteopathic manipulative treatment (SCT + OMT).
Methods
This prospective, observational study was conducted over the course of 4 months with two groups of patients with a diagnosis of cLBP. Once consent was obtained, patients were assigned to the SCT or the SCT + OMT group based on the specialty practice of their physician. At enrollment and after 4 months of treatment, all patients in both groups completed two questionnaires: the 11 point pain intensity numerical scale (PI-NRS) and the Roland Morris Disability Questionnaire (RMDQ). Cost data was collected from the electronic medical record of each patient enrolled in the study. Chi-square (χ2Yates) tests for independence using Yates’ correction for continuity were performed to compare the results for each group.
Results
There was a total of 146 patients: 71 (48.6%) in the SCT + OMT group and 75 (51.4%) in the SCT group. The results showed no significant differences between the mean total costs for the SCT + OMT ($831.48 ± $553.59) and SCT ($997.90 ± $1,053.22) groups. However, the utilization of interventional therapies (2; 2.8%) and radiology (4; 5.6%) services were significantly less for the SCT + OMT group than the utilization of interventional (31; 41.3%) and radiology (17; 22.7%) therapies were for the SCT group (p<0.001). Additionally, the patients in the SCT + OMT group were prescribed fewer opioid medications (15; 21.1) than the SCT (37; 49.3%) patients (p.001). Patients in the SCT group were approximately 14.7 times more likely to have received interventional therapies than patients in the SCT + OMT group. Likewise, the patients in the SCT group were approximately four times more likely to have received radiological services. Paired t tests comparing the mean pre- and 4 month self reported pain severity scores on the RMDQ for 68 SCT + OMT patients (9.91 ± 5.88 vs. 6.40 ± 5.24) and 66 SCT patients (11.44 ± 6.10 vs. 8.52 ± 6.14) found highly significant decreases in pain for both group (<0.001).
Conclusions
The mean total costs for the SCT and SCT + OMT patients were statistically comparable across 4 months of treatment. SCT + OMT was comparable to SCT alone in reducing pain and improving function in patients with chronic low back pain; however, there was less utilization of opioid analgesics, physical therapy, interventional therapies, radiologic, and diagnostic services for patients in the SCT + OMT group.
Chronic low back pain (cLBP) is characterized by pain lasting longer than 3 months [1] and is accompanied by physical disabilities and psychological distress [2]. CLBP is the second leading cause of disability in the United States, impacting more than 32 million Americans with an annual economic burden of $177 billion [3]; it is also now the leading cause of disability worldwide [4]. Disability and costs associated with cLBP are projected to increase in the future [4]. Although cLBP affects people of all incomes, age groups, and ethnicities [4], several features increase an individual’s risk for low back pain, including being over 30 years of age, having a BMI
Considering the physical and financial implications of cLBP, development of an appropriate treatment plan is crucial. Treatment for low back pain can be multifaceted [6]. Pharmacologic therapy ranges from over the counter medications such as acetaminophen or ibuprofen to nonsteroidal anti inflammatories to muscle relaxants and opiates [7]. Nonpharmacologic treatments are also available, including physical therapy, acupuncture, exercise therapy, behavioral therapy, and osteopathic manipulative treatment (OMT) [8]. More invasive treatments such as steroid injections, facet injections, and epidural injections may also be utilized in the management of low back pain [8]. All of these treatment options have an associated cost, as well as an impact on patients’ ability to function on a daily basis, but as of this writing, there were no previously published prospective studies comparing the treatment options for cost.
We designed this study to compare the differences in cost associated with standard of care treatment (SCT) vs. SCT + OMT in patients with cLBP. We hypothesized that the costs associated with SCT + OMT would be lower than costs related to SCT. A secondary outcome of this study was to examine utilization of treatments and the comparative clinical effectiveness.
Methods
This study was approved by the Institutional Review Boards at Rowan University School of Osteopathic Medicine (RowanSOM) and Michigan State University and funded by a grant from the American Osteopathic Association. It was registered at ClinicalTrials.gov (No. NCT03532230).
Sites
This study was conducted through RowanSOM in southern New Jersey, Pain Associates in southern New Jersey, and Michigan State University. The NeuroMusculoskeletal Institute at RowanSOM houses the clinical department of osteopathic manipulative medicine (OMM), was the site of SCT + OMT, and partnered with the Pain Associates to provide SCT. Michigan State University has a clinical department of OMM that provided SCT + OMT and a pain management clinic that provided care for the SCT group. These two sites were selected to control for possible regional differences in treatments for back pain. The study was intended to encompass multiple sites across the country, but the sites in Michigan and New Jersey were the only sites interested in participation in this study. Other sites were invited to participate in the study. Recruitment for the study occurred at a biannual Educational Council of Osteopathic Principles meeting. The requirements for inclusion were an OMM clinic and local partnering in a pain management clinic. Unfortunately, no other sites were able to meet the deadline for participation.
Patients
Beginning on March 19, 2019, patients between the ages of 18 and 84 years who had been diagnosed with cLBP lasting more than 3 months (confirmed with ICD-10 codes M54.5, M54.16, G57.01, G57.02, M48.062, M48.062, M47.816, M48.07, M54.41, and M54.42) and who were being treated at RowanSOM, Pain Associates, and Michigan State University were invited to participate in this prospective, observational study. Patients with a history or presence of diabetic neuropathy, congenital lumbar or sacral abnormalities, lumbar fracture, multiple myeloma, metastatic bone disease, spinal surgery or low back pain lasting less than 3 months were excluded from the study. Patients were categorized into SCT or SCT + OMT based on the specialty certification of the physician treating the patient and that physician’s management plan. Those in the SCT group were seen by physicians specializing in physical medicine and rehabilitation who do not provide osteopathic manipulative treatments to patients. Patients in the SCT + OMT group were seen by physicians specializing in physical medicine and rehabilitation (J.B., R.J.), who perform OMT regularly or referred patients to colleagues in the same practice who specialized in OMT (D.C., J.B.).
The duration of the entire study was 18 months (June 2018–December 2019), but each patient only participated in the study for approximately 4 months. Written informed consent was obtained from each participant prior to the start of any study related activities.
Treatment
All patients in both groups received SCT for cLBP, which may have included prescription medications (i.e., opiate pain relievers, nonsteroidal anti inflammatories, and muscle relaxants); steroid injections; and referrals for imaging, physical therapy, psychotherapy, spinal cord stimulators, spinal pump insertions, and other therapies. The SCT + OMT group additionally received OMT for cLBP. No specific OMT techniques were required for the study, but data on the number of OMT sessions per patient was collected.
Outcomes measures
The 11 point Pain Intensity Numerical Rating Scale (PI-NRS) [9] and Roland Morris Disability Questionnaire (RMDQ) [10] were administered at the time of enrollment and after 4 treatment months for both groups. These self reported instruments were specifically developed to measure changes in chronic pain and have been widely used to investigate the severity of chronic back pain. Both instruments have demonstrated strong convergent validity with respect to other measures of back pain and have high test-retest reliabilities [11]. The PI-NRS rating scale ranges from 0 (no pain) to 10 (worst possible pain), whereas the RMDQ is scored by counting the number of items checked by the patient as “Yes.”
The primary outcome of this study was the mean total cost per patient from each group for 4 months of treatment. The cost data were collected from the electronic medical record of each patient enrolled in the study. Because the costs for comparable treatments varied with respect to different socioeconomic and geographical regions in the United States, the mean total healthcare cost per patient was calculated based on codes for 2018 Medicare fee schedules listed in the current procedural terminology (CPT) for office visits, OMT, interventional procedures, and radiological/diagnostic testing [12]. The costs were also standardized according to the 2018 Medicare fees for physical therapy sessions for the patients at both sites. The total morphine milligram equivalents for the various prescribed pain medications were calculated and summed to permit comparisons across the three centers, as well as at admission and after 4 months of treatment.
Data analysis
Before performing any statistical analyses, the distributional characteristics for all variables were examined, and skewness indices were calculated for each of the continuous variables, such as age, morphine milligram equivalents, and mean cost (US dollars) for each type of treatments. The skewness indices for most of the cost data were positive and ranged from a low of 0.26 for age to 5.70 for interventional therapies. The latter skewness index was especially high for interventional costs, because one SCT patient was billed $52,700 for the insertion of a spinal pump after having been admitted to the study. Because the majority of the skewness indices were >2.0, square root and log10 transformations were employed to not only decrease the levels of skewness, but also to achieve or approximately approach normality as confirmed by Kolmogorov–Smirnov (K–S) tests for normality. The transformations were able to reduce all of the skewness indices to <2.0, and even the K–S test value of 0.12 for interventional procedures was not significant (p<0.20), indicating that the transformed interventional costs were normally distributed. Therefore, the transformed cost data were considered to be appropriately distributed for parametric analyses, such as independent t tests. To determine whether the magnitudes of the mean decreases in pain were different between the two groups, two analyses of covariance (ANCOVA) were performed using baseline scores as the covariate and type of group as the main effect for both the RMDQ and PI-NRS scores.
Chi-square (χ2Yates) tests for independence using Yates’ correction for continuity were performed to compare the percentages use for different treatments between groups, and phi (φ) correlations were calculated to estimate the effect sizes of the proportional differences. Before comparing the grand total mean treatment costs and specific mean treatment costs for each of the treatment modalities, correlations between each treatment modality with sex and age were calculated to determine whether either variable or both had to be controlled for in subsequent statistical analyses.
Results
This study recruited 146 total patients: 71 patients (48.6%) in the SCT + OMT group and 75 patients (51.4%) in the SCT group (Table 1). The percentages of the patients recruited to each group were comparable between the two sites in New Jersey (STC + OMT, 35 [49.3%]) and Michigan (STC + OMT, 37 [49.3%]). With respect to patient sex, the percentage of women in the SCT + OMT group (59; 83.1%) was significantly higher than the percentage of women in the SCT group (49; 65.3%; p<0.05). However, the φ correlation of sex with type of group was only 0.20, indicating a small effect size based on Cohen’s interpretive guidelines [13]; those effect-size guidelines for φ correlations of 0.10, 0.30, and 0.50, were described, respectively in a separate study, as small, medium, and large [11]. The mean (± standard deviation [SD]) age of the patients in the SCT + OMT group was 58.1 ± 13.0 years (range, 29–80 years), and the mean ± SD age of the patients in the SCT group was 53.77 ± 16.22 years (range, 23–83 years); these two mean ages were comparable (t[144] = 1.78). The mean difference in ages between the two groups was 4.35 years, which represented a medium effect size of 0.30.
Patient demographic characteristics and treatment types.
| Characteristics | SCT + OMT (n=71) n (%) | SCT (n=75) n (%) | χ2Yates (1, n=146) | φ | p |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 12 (16.9) | 26 (34.7) | 5.09 | 0.20 | <0.05 |
| Female | 59 (83.1) | 49 (65.3) | |||
| State | |||||
| New Jersey | 35 (49.3) | 37 (49.3) | 0 | 0 | |
| Michigan | 36 (50.7) | 38 (50.7) | |||
| Use of interventional therapies | |||||
| Yes | 2 (2.8) | 31 (41.3) | 28.77 | 0.46 | <0.01 |
| No | 69 (97.2) | 44 (58.7) | |||
| Use of medications | |||||
| Yes | 44 (62.0) | 58 (77.3) | 3.39 | 0.17 | |
| No | 27 (38.0) | 17 (22.7) | |||
| Use of opioids | |||||
| Yes | 15 (21.1) | 37 (49.3) | 12.65 | 0.29 | <0.001 |
| No | 56 (79.9) | 38 (50.7) | |||
| Use of physical therapy | |||||
| Yes | 4 (5.6) | 7 (9.3) | 0.28 | 0.07 | |
| No | 67 (94.4) | 68 (90.7) | |||
| Use of radiological services | |||||
| Yes | 4 (5.6) | 17 (22.7) | 7.27 | 0.24 | <0.01 |
| No | 67 (94.4) | 58 (77.3) | |||
| Use of referral services | |||||
| Yes | 12 (16.9) | 12 (16.0) | 0 | 0 | |
| No | 59 (83.1) | 63 (84.0) | |||
SCT, standard of care without osteopathic manipulative treatment; SCT + OMT, standard of care with osteopathic manipulative treatment.
The number of patients treated in each group is also shown in Table 1. The use of referral services was comparable (SCT + OMT, 12 [16.9%] vs. SCT, 12 [16.0%]). Only four patients (5.6%) in the SCT + OMT group received physical therapy compared with seven patients (9.3%) in the SCT group. The use of medications was also comparable (SCT + OMT, 44 [62.0%] vs. SCT, 58 [77.3%]). However, the utilization of interventional therapies (2; 2.8%) and radiology services (4; 5.6%) were significantly lower for the SCT + OMT group than the utilization of interventional therapies (31; 41.3%) and radiology services (17; 22.7%) therapies for the STC group (p<0.001). Additionally, fewer patients in the SCT + OMT group were prescribed opioid medications (15; 21.1%) than in the SCT group (37; 49.3%; p<0.001). Patients in the SCT group were 14.7 times more likely to have received interventional therapies than the patients in the SCT + OMT group. Likewise, the patients in the SCT group were four times more likely to have received radiological services. In addition, the mean ± SD morphine milligram equivalent dose of the various medications prescribed to the 15 SCT + OMT patients (23.76 ± 2.98) was comparable to the mean morphine milligram equivalent dose of the various medications prescribed for the 37 SCT patients (34.70 ± 18.11; t[50] = 1.61; d = 0.49).
Neither sex (r=0.08) nor age (r=0.08) was significantly correlated with mean grand total costs for the 145 patients for whom sex, age, and total cost data were available. Consequently, we elected not to control for sex or age in any of the subsequent mean cost comparisons. Table 2 lists the mean total costs or each of the seven treatment modalities (OMT, office visits, referrals, physical therapy, interventional therapies, radiology services, and medications) along with the total costs for all services incurred during the 4 months. Figure 1 shows the mean costs by group across different treatment modalities.
Medical costs by group.
| SCT + OMT | SCT | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | t | dfs | d | |
| OMT | 70 | 213.66 | 106.36 | 0 | |||||
| Office visits | 71 | 319.42 | 145.78 | 73 | 278.30 | 165.63 | 1.77 | 1.42 | 0.30 |
| Referrals | 12 | 16,708 | 78.85 | 12 | 147.43 | 73.32 | 0.69 | 22 | 0.28 |
| Physical therapy | 4 | 430.10 | 138.26 | 7 | 651.83 | 270.44 | |||
| Interventional therapies | 2 | 175.15 | 167.68 | 31 | 2,378.57 | 10,104.92 | |||
| Radiology services | 4 | 161.37 | 110.58 | 17 | 294.21 | 225.68 | |||
| Medications | 44 | 393.73 | 567.58 | 59 | 488.91 | 927.45 | 0.20 | 100 | 0.02 |
| Grand total | 71 | 831.48 | 553.59 | 74 | 997.90 | 1,053.22 | 0.11 | 143 | 0.06 |
SD, standard deviation; SCT, standard care without osteopathic manipulative treatment; SCT + OMT, standard care with osteopathic manipulative treatment.
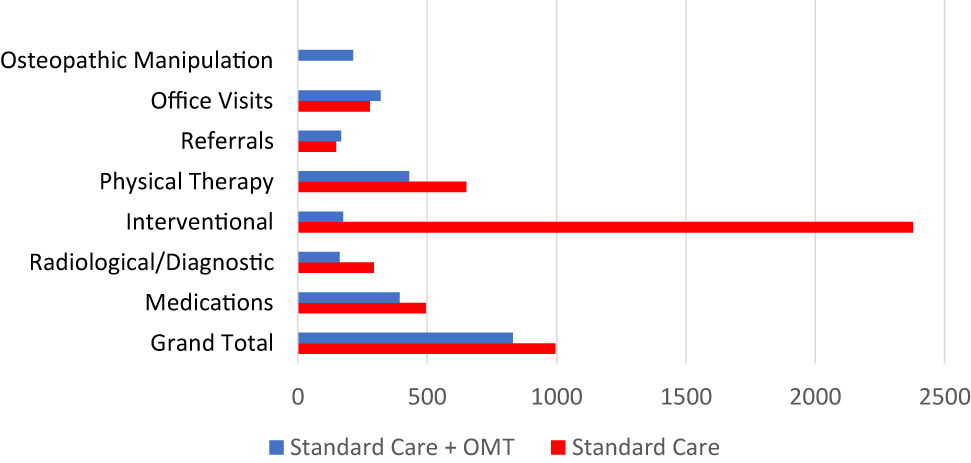
Mean costs (US dollars) by standard care with or without osteopathic manipulative treatment for chronic back pain.
Transformed scores were employed in all statistical analyses, but raw means and standard deviations are listed in the text and tables to facilitate interpretation. The mean number of OMT visits (3.83 ± 1.63) for the 36 patients treated at the Michigan site was significantly higher than the mean number for 35 patients seen at the New Jersey site (3.03 ± 1.58; t(69) = 2.11; d = 0.50, p<0.05). The mean difference of 0.50 represented a large effect size, indicating that approximately one additional OMT visit per patient had occurred at the Michigan site.
The mean costs for office visits made by 71 SCT + OMT patients ($319.42 ± $145.78) and 73 SCT patients [278.30 ± 165.63] were comparable (t[142] = 1.77; d = 0.30). Likewise, the mean costs for the 12 SCT + OMT patients who were referred for services ($167.08 ± $78.85) and the 12 SCT patients who were also referred for services ($147.43 ± $73.32) were comparable (t[22] = 0.69; d = 0.28). As Table 1 shows, no statistical mean comparison could be made between the SCT + OMT and SCT groups with respect the costs of physical therapy, interventional therapies, and radiology/diagnostic services because fewer than SCT + OMT patients had incurred costs for these services. The mean medication costs for 44 SCT + OMT patients ($393.73 ± $567.58) and 59 SCT patients ($488.91 ± $927.45) were also comparable (t[100] = 0.20; d = 0.02). Importantly, the grand total 4 month mean treatment costs for the 71 SCT + OMT patients ($831.48 ± $553.59) and the 74 SCT patients ($997.90 ± $1,053.22) for the seven treatment modalities did not significantly differ (t[143] = 0.11; d = 0.06).
The pretreatment and 4 month posttreatment means, SD, and correlations of the RMDQ and PI-NRS scales are displayed in Table 3 for both groups. The RMDQ total scores decreased significantly from 11.44 ± 6.10 to 8.52 ± 6.14 for the SCT group (p<0.001) and from 9.91 ± 5.88 to 6.40 ± 5.24 for the SCT + OMT group over 4 months (p<0.001). The PI-NRS total scores only decreased for SCT patients, from 5.17 ± 2.35 to 4.61 ± 2.23 (p<0.05). The d statistics (0.64) given in Table 3 indicated that the RMDQ mean decrease for SCT + OMT patients represented a large effect size. Likewise, the d statistic of 0.53 for the mean decrease in the RMDQ total scores for SCT patients also reflected a large effects size, whereas the mean decreases in PI-NRS scores over time for both groups indicated small effect sizes of 0.23 for SCT + OMT patients and 0.25 for the SCT patients. The adjusted mean decreases in pain for RMDQ and PI-NRS were comparable (SCT + OMT, F[1, 131] = 2.50 partial η2 = 0.02; SCT, F[1,129] = 0, partial η2 = 0). Furthermore, the morphine milligram equivalent dose for each group was not significantly correlated with decreases in RMDQ (r=0.05) or PI-NRS (r=0.15) scores. Likewise, the number of OMT sessions performed on SCT + OMT patients was not significantly correlated with decreases in RMDQ (r=0.03) or PI-NRS (r=0.04) scores.
Pain scales by group.
| Pretreatment | Posttreatment (4 months) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Scale | n | Mean | SD | Mean | SD | r | Paired t | (dfs) | d | p |
| SCT + OMT | ||||||||||
| RMDQ | 68 | 9.91 | 5.88 | 6.40 | 5.28 | 0.52 | 5.25 | 67 | 0.64 | <0.001 |
| PI-NRS | 70 | 4.48 | 2.11 | 3.99 | 2.31 | 0.54 | 1.95 | 69 | 0.23 | |
| SCT | ||||||||||
| RMDQ | 66 | 11.44 | 6.10 | 8.52 | 6.14 | 0.60 | 4.34*** | 65 | 0.53 | <0.001 |
| PI-NRS | 66 | 5.17 | 2.35 | 4.61 | 2.23 | 0.52 | 2.05* | 65 | 0.25 | <0.05 |
SD, standard deviation; SCT, standard care without osteopathic manipulative treatment; SCT + OMT, standard care with osteopathic manipulative treatment; RMDQ, Roland Morris Disability Questionnaire; PI-NRS, numerical rating scale for pain.
Discussion
The initial objective of this study was to compare the costs associated with standard of care treatment with or without OMT for cLBP. We hypothesized that the SCT + OMT group would have lower costs than the SCT group, but our results showed no significant differences in mean total cost.
However, the utilization of interventional therapies and radiology services were significantly different between the groups. Only 2.8% of patients in the SCT + OMT group received interventional therapies as part of the treatment plan compared with 41.3% of patients in the SCT group. Additionally, only 5.6% of the SCT + OMT group had included radiology services in their treatment plan as opposed to 22.7% of the SCT group. This difference may not be attributable to OMT, but might be related to the structural examination that preceded treatment. The osteopathic structural examination can inherently identify biomechanical and fascial dysfunctions contributing to low back pain that are not identifiable on standard neurologic and musculoskeletal examinations. During an osteopathic physical and structural examination, identifying somatic dysfunction in the absence of historical red flags or neurologic deficits affords the provider an opportunity to correct these dysfunctions and offer an immediate treatment modality to the patient. If the patient has an improvement or resolution of symptoms, both the provider and the patient may opt to assess the effects of OMT before pursuing radiology services or interventional therapies. This theory is also supported by previous research from Licciardone et al. [1] in a randomized, controlled trial.
Radiological studies are not completely risk free for the patient, as they result in radiation exposure. Lumbar spine lateral X-rays, for example, can have an effective dose of 0.38–0.5 mSv of radiation exposure [14]. Limiting a patient’s exposure to unnecessary radiation is a critical consideration in quality patient care. Additionally, interventional therapies may be indicated for appropriate management of a patient’s pain, but they are not entirely risk free. Between 2000 and 2014, the utilization of lumbar transforaminal epidural steroid injections (L-TFESI) increased more than 600% per 100,000 Medicare patients [15]. L-TFESIs and lumbar facet injections can expose a patient to 0.24 and 0.1 mSv of radiation, respectively [16]. While OMT does have some risks of adverse response such as muscle pain and soreness, it does not carry the same risks of exposure to radiation and adverse effects of interventional therapies. Our results also showed that osteopathic physicians are obtaining appropriate compensation for OMT, which explains the cost equivalency even in comparison with the SCT group. We hope this evidence will encourage more osteopathic physicians to continue incorporating OMT into the care of their patients regardless of their speciality.
Results of our study demonstrated that 49.3% of SCT patients were prescribed opioid medications for pain management compared with 21.1% of SCT + OMT patients. This indicates another important difference between study groups. Currently, in the United States, the opioid crisis has become the worst drug epidemic in history [17]. A large portion of the opioid abuse epidemic is related to exposure through prescription medications, which has risen dramatically since the 1980s [17]. Thus, appropriately prescribing opioids can help to reduce this issue [18]. In addition to the high potential for addiction, opioid medications also carry side effects like sedation, nausea, vomiting, delirium, myoclonus, and pruritus [18]. All patients taking opioids must be educated on proper bowel regimens to treat opioid induced constipation [18]. The most severe and potentially fatal side effect is respiratory depression [18]. Crow et al. [19] indicated that providing OMT in addition to SCT for patients with cLBP could aid in decreasing patient exposure to opioids and associated adverse effects. Our study supports this finding. A previous randomized, controlled trial of 155 subjects by Andersson et al. [20] also demonstrated a statistically significant decrease (p<0.001) in nonsteroidal anti inflammatory drug (NSAID) and muscle relaxant use in an OMT group. In the standard care group in that study, 54.3% of subjects received prescriptions for NSAIDs, whereas only 24.3% of subjects received prescriptions for NSAIDs in the OMT group [20]. Although that study did not show significant differences in pain improvement when spinal manipulation was compared with SCT for lower back pain management, Andersson et al. [20] indicated that spinal manipulation for lower back pain should be investigated more closely due to the reduction in medication usage.
Our SCT + OMT and SCT treatment groups showed similar decreases in pain. According to the RMDQ and PI-NRS, both groups reported comparable decreases in pain after 4 months, despite 49.3% of SCT patients and 21.1% of SCT + OMT patients having been prescribed opioids. The mean morphine milligram equivalent doses prescribed for both groups were comparable, but neither group’s morphine milligram equivalent dose was significantly correlated with decreases in pain according to the RMDQ and PI-NRS. Decreases in pain could be associated with the number of OMT visits, but the number of OMT visits was not significantly related to decreases in pain according to the RMDQ and PI-NRS. Thus, our study demonstrated that OMT was an effective non pharmaceutical treatment in reducing pain levels for patients with cLBP and does not carry the risks of opioids. Guidelines from the American Osteopathic Association (AOA) on OMT for patients with low back pain also supported the idea that OMT can effectively reduce chronic non specific low back pain [21].
In the most basic sense, OMT provides a biomechanical treatment for biomechanical problems (somatic dysfunctions), which in the case of cLBP can include innominate, sacral, and lumbar dysfunctions as well as functional leg length discrepancies. Osteopathic structural exams can diagnose myofascial and ligamentous asymmetries that cannot be detected in radiologic or laboratory studies. These asymmetries can contribute to symptoms of low back pain; moreover, opioids cannot correct the aforementioned biomechanical dysfunctions and myofascial asymmetries. Providers who utilize OMT regularly can educate patients on the potential causes of non malignant low back pain, which offers patients another treatment modality aside from medications. The AOA Guidelines recommended that osteopathic physicians utilize OMT when there is a diagnosis of somatic dysfunction and other causes of lower back pain have been excluded or deemed doubtful [21]. Previous research from Von Korff et al. [22] supported the notion that physicians who educate their patients about conditions such as low back pain and encourage activity prescribe fewer medications compared with physicians who do not [22]. Gamber et al. [23] also demonstrated that OMT plus SCT can benefit patients with fibromyalgia, which is a diagnosis of exclusion. Patients in that study who received OMT and education along with their current medications showed more functional and affective improvements as well as increases in pain thresholds at various fibromyalgia tender points when compared with subjects who did not receive OMT [23]. Fibromyalgia treatment plans heavily rely on patient education and prudent use of appropriate analgesic medications, a notion that also concurs with the features of effective treatment plans for cLBP [20]. OMT does not cure low back pain and can require multiple treatments, sometimes on a monthly basis, but opioids also offer no cure and many require frequent dosing.
Limitations
One of the limitations of our study was the homogenous population; another was short follow up. The majority of patients were women, of middle age (between 40 and 60 years of age), and White. Further, we only followed them during the 4 months of treatment for cLBP. Additionally, both clinical sites in Michigan and New Jersey were affiliated with osteopathic medical schools, which may have influenced the number of patients treated with OMT and limited the number of patients available for the study who were treated for low back pain but did not have OMT. Another limitation is that the proposed target sample size of 35 patients per clinic did not provide a sufficient number of patients representing three of the treatment modalities (physical therapy, interventional services, and radiology/diagnostic testing). As a result, the costs of those services were adjusted based on skew and limited a true generalized cost comparison between groups. Another limitation was the duration of this study. In looking at the costs of care between the two groups over our 4 month study period, those in the SCT group had an exponential increase in costs over the 4 months, while the SCT + OMT group had a steady cost with little increase. If the period had been longer, there would have been a statistically significant difference in cost between the two groups, based on our 4 month results. A final limitation is the manner in which OMT and office visit costs were billed; office visits were only billed twice per month for the SCT + OMT group according to insurance regulations.
Conclusions
Although the mean total costs for SCT and SCT + OMT patients were statistically comparable across 4 months of treatment, the types of treatments differed. Patients in the SCT group (41.3%) were approximately 13 times more likely to have been treated with interventional therapies than patients in the SCT + OMT group (2.8%). Likewise, the patients in the SCT group were approximately four times more likely to have received radiological/diagnostic services. Despite limitations in our study, the data demonstrates important evidence that OMT can be as effective as SCT treatment alone for patients with cLBP, and has distinct advantages in that it utilizes fewer opiates and interventional therapies. Thus, utilization of OMT should be encouraged by osteopathic physicians who treat patients with cLBP.
Research funding: This current study was funded by a grant from the American Osteopathic Association (Grant No. 3011806720). The funds covered honoraria, subcontracts, and travel expenses for conference presentations. Participants were not reimbursed for participation in the study.
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests: Authors state no conflict of interest.
Informed consent: Written informed consent was obtained from each participant prior to the start of any study related activities.
Ethical approval: This study was approved by the Institutional Review Boards at Rowan University School of Osteopathic Medicine and Michigan State University. This study was registered at ClinicalTrials.gov (No. NCT03532230).
References
1. Licciardone, JC, Gatchel, RJ, Aryal, S. Recovery from chronic low back pain after osteopathic manipulative treatment. J Am Osteopath Assoc 2016;116:144–55. https://doi.org/10.7556/jaoa.2016.031.Search in Google Scholar
2. Andersen, TE, Lahav, Y, Ellegaard, H, Manniche, C. A randomized controlled trial of brief somatic experiencing for chronic low back pain and comorbid post-traumatic stress disorder symptoms. Eur J Psychotraumatol 2017;8:1–9. https://doi.org/10.1080/20008198.2017.1331108.Search in Google Scholar
3. Gooch, CL, Pracht, E, Borenstein, AR. The burden of neurological disease in the United States: a summary report and call to action. Ann Neurol 2017;81:479–84. https://doi.org/10.1002/ana.24897.Search in Google Scholar
4. Hartvigsen, J, Hancock, MJ, Kongsted, A, Louw, Q, Ferreira, ML, Genevay, S, et al.. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–67. https://doi.org/10.1016/S0140-6736(18)30480-X.Search in Google Scholar
5. Alleva, J, Hudgins, T, Belous, J, Kristin Origenes, A. Chronic low back pain. Dis Mon 2016;62:330–3. https://doi.org/10.1016/j.disamonth.2016.05.012.Search in Google Scholar
6. Delitto, A, George, SZ, Van Dillen, L, Whitman, JM, Sowa, G, Shekelle, P, et al.. Low back pain. J Orthop Sports Phys Ther 2012;42:A1–A57. https://doi.org/10.2519/jospt.2012.42.4.A1.Search in Google Scholar
7. Will, JS, Bury, DC, Miller, JA. Mechanical low back pain. Am Fam Physician 2018;98:421–8.Search in Google Scholar
8. Last, AR, Hulbert, K. Chronic low back pain: evaluation and management. Am Fam Physician 2009;79:1067–74.10.1080/20786204.2010.10873969Search in Google Scholar
9. Farrar, JT, Young, JPJr, LaMoreaux, L, Werth, JL, Poole, MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58. https://doi.org/10.1016/S0304-3959(01)00349-9.Search in Google Scholar
10. Roland, MO, Morris, RW. A study of the natural history of back pain. Part 1: development of a reliable and sensitive measure of disability in low back pain. Spine 1983;8:141–4. https://doi.org/10.1097/00007632-198303000-00004.Search in Google Scholar
11. Chiarotto, A, Boers, M, Devo, RA, Buchbinder, R, Corbin, TP, Costa, LO, et al.. Coreoutcome measurement instruments for clinical trials in nonspecific low back pain. Pain 2018;159:481–95. https://doi.org/10.1097/j.pain.0000000000001117.Search in Google Scholar
12. AAPC. Advancing the Business of Healthcare. Codify. Available from: https://www.aapc.com/resources/medical-coding/cpt.aspx.Search in Google Scholar
13. Cohen, J. A power primer. Psychol Bull 1992;112:155–9. https://doi.org/10.1037/0033-2909.112.1.155.Search in Google Scholar
14. Nickoloff, EL, Lu, ZF, Dutta, AK, So, JC. Radiation dose descriptors: BERT, COD, DAP, and other strange creatures. Radiographics 2008;28:1439–50. https://doi.org/10.1148/rg.285075748.Search in Google Scholar
15. Braun, E, Sack, AM, Sayed, D, Manion, S, Hamm, B, Brimacombe, M, et al.. Reducing radiation exposure in lumbar transforaminal epidural steroid injections with pulsed fluoroscopy: a randomized, double-blind, controlled clinical trial. Pain Physician 2018;21:53–60. https://doi.org/10.36076/ppj.2018.1.53.Search in Google Scholar
16. Dietrich, TJ, Peterson, CK, Zeimpekis, KG, Bensler, S, Sutter, R, Pfirrmann, CWA. Fluoroscopy-guided versus CT-guided lumbar steroid injections: comparison of radiation exposure and outcomes. Radiology 2019;290:752–9. https://doi.org/10.1148/radiol.2018181224.Search in Google Scholar
17. Kolodny, A, Courtwright, DT, Hwang, CS, Kreiner, P, Eadie, JL, Clark, TW, et al.. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Publ Health 2015;36:559–74. https://doi.org/10.1146/annurev-publhealth-031914-122957.Search in Google Scholar
18. McNicol, E, Horowicz-Mehler, N, Fisk, RA, Bennett, K, Gialeli-Goudas, M, Chew, PW, et al.. Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. J Pain 2003;4:231–56. https://doi.org/10.1016/s1526-5900(03)00556-x.Search in Google Scholar
19. Crow, WT, Willis, DR. Estimating cost of care for patients with acute low back pain: a retrospective review of patient records. J Am Osteopath Assoc 2009;109:229–33.Search in Google Scholar
20. Andersson, GB, Lucente, T, Davis, AM, Kappler, RE, Lipton, JA, Leurgans, S. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med 1999;341:1426–31. https://doi.org/10.1056/NEJM199911043411903.Search in Google Scholar
21. Task force on the low back pain clinical practice guidelines. American osteopathic association guidelines for osteopathic manipulative treatment (OMT) for patients with low back pain. J Am Osteopath Assoc 2016;116:536–49. https://doi.org/10.7556/jaoa.2016.107.Search in Google Scholar
22. Von Korff, M, Barlow, W, Cherkin, D, Deyo, RA. Effects of practice style in managing back pain. Ann Intern Med 1994;121:187–95. https://doi.org/10.7326/0003-4819-121-3-199408010-00005.Search in Google Scholar
23. Gamber, RG, Shores, JH, Russo, DP, Jimenez, C, Rubin, BR. Osteopathic manipulative treatment in conjunction with medication relieves pain associated with fibromyalgia syndrome: results of a randomized clinical pilot project. J Am Osteopath Assoc 2002;102:321–5.Search in Google Scholar
© 2021 Danielle Cooley et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Physician wellbeing – what do physicians want?
- Medical Education
- Original Articles
- Meaningful use of COMSAE Phase 1 in preparation for COMLEX-USA Level 1
- The role of extracurricular activities and lectures in mitigating medical student burnout
- Musculoskeletal Medicine and Pain
- Original Article
- Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Cost comparison of osteopathic manipulative treatment for patients with chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Perceptions of nonopioid treatment for pain in a homeless population
- Brief Report
- Osteopathic manipulative medicine in the management of headaches associated with postconcussion syndrome
- Public Health and Primary Care
- Original Article
- National disparities in colorectal cancer screening in patients with comorbid conditions: an analysis of the Behavioral Risk Factor Surveillance System
- Clinical Image
- Orange palpebral spots
Articles in the same Issue
- Frontmatter
- Editorial
- Physician wellbeing – what do physicians want?
- Medical Education
- Original Articles
- Meaningful use of COMSAE Phase 1 in preparation for COMLEX-USA Level 1
- The role of extracurricular activities and lectures in mitigating medical student burnout
- Musculoskeletal Medicine and Pain
- Original Article
- Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Cost comparison of osteopathic manipulative treatment for patients with chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Perceptions of nonopioid treatment for pain in a homeless population
- Brief Report
- Osteopathic manipulative medicine in the management of headaches associated with postconcussion syndrome
- Public Health and Primary Care
- Original Article
- National disparities in colorectal cancer screening in patients with comorbid conditions: an analysis of the Behavioral Risk Factor Surveillance System
- Clinical Image
- Orange palpebral spots

