Long-term functional outcomes and predictors of efficacy in thulium laser enucleation of the prostate (ThuLEP) for benign prostatic hyperplasia (BPH): a retrospective observational study
-
Lorenzo Spirito
, Celeste Manfredi
, Federico Capone
Abstract
Objectives
Benign prostatic hyperplasia (BPH) is a common urological condition affecting aging men worldwide. Among the treatment options available for BPH, transurethral resection of the prostate (TURP) is the gold-standard invasive intervention. To reduce the TURP-related non-negligible morbidity, loss-of-ejaculation rate, hospitalization, blood loss and catheterization time several laser techniques have been developed, such as the Thulium Laser Enucleation of the Prostate (ThuLEP). To investigate the efficacy outcomes of the ThuLEP as a treatment option for benign prostatic hyperplasia (BPH) we performed a retrospective observational study at Moriggia Pelascini Hospital (Como, Italy) between January 2015 and September 2018.
Methods
We included 265 patients who underwent ThuLEP at a specific hospital between defined dates. Data on various parameters, including post-void residue volume, peak urinary flow rate (Qmax), International Prostate Symptom Score (IPSS) for urinary symptoms, IPSS Quality of Life (QoL) score, and International Index of Erectile Function (IIEF) score for erectile dysfunction, were collected at baseline and follow-up.
Results
The analysis revealed significant improvements in voiding efficiency, urinary flow, urinary symptoms, quality of life, and erectile function following ThuLEP. Furthermore, certain baseline characteristics, such as post-void residue, peak urinary flow rate, age, prostate volume, and aspirin usage, were found to influence treatment outcomes.
Conclusions
Despite the study’s limitations, these findings contribute to understanding ThuLEP’s effectiveness in managing BPH and can aid in making informed clinical decisions for patient care. Prospective studies with longer follow-up periods are recommended to validate and extend these results.
Introduction
Benign prostatic hyperplasia (BPH) is a common condition that affects aging men worldwide [1, 2]. BPH is associated with the non-cancerous enlargement of the prostate gland, leading to lower urinary tract symptoms (LUTS), which can significantly impact the quality of life of affected individuals [3–5]. The combination of an alpha(1)-blocker and a 5alpha-reductase inhibitor has been demonstrated as the most effective medical therapy for benign prostatic hyperplasia (BPH) in reducing the risk of disease progression and alleviating lower urinary tract symptoms (LUTS) [6]. Among the treatment options available for BPH, transurethral resection of the prostate (TURP) remains the gold-standard invasive intervention, although several transurethral ablative techniques based on innovative medical devices have been introduced as alternative treatment options for BPH [7]. The introduction of laser techniques has helped to reduce patient hospitalization, blood loss and catheterization time, due to the thermal effect of lasers, which guarantees the achievement of point coagulation and hemostasis [8]. In this regard, thulium (Tm:YAG) was introduced in the urological landscape in 2005 and continues to be used thanks to its unique characteristic which consists of the 2013 nm wavelength and the continuous delivery of energy with minimal tissue penetration and excellent point coagulation and hemostasis [9]. ThuLEP aims to alleviate urinary obstruction by removing excess prostate tissue, thereby improving urinary flow and relieving LUTS [10]. While ThuLEP has demonstrated its efficacy and safety over the years [10], there is still a need for comprehensive assessments of treatment outcomes and factors influencing long-term effectiveness. Understanding the long-term outcomes and factors influencing the success of ThuLEP in the management of BPH can aid clinicians in making informed treatment decisions and optimizing patient care [11].
In this retrospective observational analysis, we aim to explore the clinical outcomes of patients who underwent ThuLEP for BPH at Moriggia Pelascini Hospital (Como, Italy) between January 2015 and September 2018. Through a comprehensive analysis of selected outcomes, including post-void residue volume, peak urinary flow rate (Qmax), International Prostate Symptom Score (IPSS) for urinary symptoms [12], IPSS Quality of Life (QoL) score [12], and International Index of Erectile Function (IIEF) score for erectile dysfunction [13], we intend to gain insights into the effectiveness of ThuLEP as a treatment option for BPH and identify potential factors that may influence treatment outcomes.
Materials and methods
Study design and participants
This study was designed as a retrospective observational analysis of patient records from a cohort of individuals who underwent ThuLEP for BPH at Moriggia Pelascini Hospital (Como, Italy) between January 2015 and September 2018. Inclusion criteria comprised patients with complete baseline and follow-up data for peak flux (Qmax), post-void residue volume, erectile function, quality of life, and urinary symptoms. Patients with missing data or a history of prior prostate surgery were excluded.
Data collection
Patient records were meticulously reviewed to extract relevant information, including age, preoperative prostate volume, preoperative PSA, preoperative Qmax, preoperative post-void residual, duration of the surgical procedure, duration of enucleation, duration of morcellation, histological weight of resected prostate tissue, presence of diabetes, and use of aspirin. Additionally, baseline International Prostate Symptom Score (IPSS) for urinary symptoms, baseline IPSS Quality of Life (QoL) score, histological weight of prostate tissue, baseline International Index of Erectile Function (IIEF) score for erectile dysfunction, baseline PSA, baseline Qmax (peak urinary flux), baseline post-void residue (PVR), and baseline prostate volume were recorded.
Outcome assessment
At the latest available follow-up, data on post-void residue volume, Qmax, IPSS score for urinary symptoms, IPSS QoL score, and IIEF score for erectile dysfunction were extracted from patient records.
Statistical analysis
Baseline characteristics of the study cohort were summarized using descriptive statistics. ANOVA for repeated measures was employed to compare the mean variation in post-void residue volume (PVR), Qmax, IPSS score for urinary symptoms, IPSS QoL score, and IIEF score at the latest follow-up compared to baseline. Furthermore, ANOVA for repeated measures was used to assess the association between the selected baseline variables (age, use of aspirin, history of diabetes, baseline PSA, baseline Qmax, baseline post-void residue, and baseline prostate volume) and treatment effectiveness. The selected variables were categorized into quartiles, except for diabetes and aspirin, which were considered binary. The analysis was performed using the MedCalc software.
Ethical considerations
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki. Approval for retrospective data analysis was obtained from the Institutional Review Board of Moriggia Pelascini Hospital.
Results
Patients’ characteristics
The study involved a total of 265 patients who underwent transurethral resection of the prostate (ThuLEP) for benign prostatic hyperplasia (BPH). The patients’ demographic and clinical characteristics were assessed, and the median and interquartile range (25th–75th percentile) was calculated for each variable of interest. The duration of catheterization following the procedure was found to have a consistent median of 2 h for all patients. The median age of the participants was 69 years, with the 25th–75th percentile spanning from 63 to 75 years. The International Prostate Symptom Score (IPSS), a measure of urinary symptoms, had a median score of 22, with a range of 18–27. The IPSS Quality of Life (QoL) score, assessing the impact of symptoms on the patients’ quality of life, showed a median of 5, with a range of 4–6. The histological weight of the resected prostate tissue, indicative of the size of the removed prostate tissue, had a median of 45 g, with the 25th–75th percentile ranging from 33 to 72 g. The International Index of Erectile Function (IIEF) score, reflecting erectile function, showed a median of 12, with a range of 9–16. The baseline prostate-specific antigen (PSA) levels, used to assess prostate health, had a median of 2.6 ng/mL, with the 25th–75th percentile varying from 1.6 to 6 ng/mL. Baseline peak urinary flux (Qmax) exhibited a median of 7 mL/s, with a range of 6–8.5 mL/s. The post-void residue (PVR), representing the amount of urine remaining in the bladder after voiding, had a median of 120 mL, ranging from 50 to 300 mL. Baseline prostate volume, an indicator of prostate size, had a median of 52 mL, with the 25th–75th percentile spanning from 36 to 80 mL. Median follow-up duration was 15 months (interquartile range, 9–22) (Table 1).
Overall characteristics of the study population at baseline.
| n | Median | 25–75 p-Value | |
|---|---|---|---|
| Catheterization duration | 265 | 2 | 2–2 |
| Enucleation duration | 263 | 53 | 38.5–74.1 |
| Surgical procedure duration | 263 | 70 | 50–95 |
| Morcellation duration | 263 | 15 | 11.5–19.9 |
| Age | 265 | 69 | 63–75 |
| IPSS score | 265 | 22 | 18–27 |
| IPSS QoL score | 265 | 5 | 4–6 |
| Histological weight of prostate tissue | 265 | 45 | 33–72 |
| IIEF score | 265 | 12 | 9–16 |
| PSA | 265 | 2.6 | 1.6–6 |
| Baseline Qmax | 228 | 7 | 6–8.5 |
| Post-void residue | 265 | 120 | 50–300 |
| Prostate volume | 265 | 52 | 36–80 |
-
PVR, post-void residue; Qmax, peak urinary flux; IPSS, International Prostate Symptom Score; IIEF, International Index of Erectile Function.
Functional outcomes
The analysis revealed significant associations between the variables and the variation of the outcome measures. Firstly, for post-void residue (PVR), there was a substantial decrease in post-void residue following the procedure, with a mean difference of −169.645 (95 % CI: −148.911 to −190.379; p<0.0001). This indicates a significant improvement in voiding efficiency after the treatment. Secondly, for peak urinary flux (Qmax), there was a considerable increase in peak urinary flux, with a mean difference of 17.934 (95 % CI: 16.556 to 19.312; p<0.0001), suggesting a significant improvement in urinary flow following the procedure.
Moreover, for the International Prostate Symptom Score (IPSS) for urinary symptoms, there was a substantial decrease in the score, with a mean difference of −19.502 (95 % CI: 18.645 to 20.359; p<0.0001), indicating a significant reduction in urinary symptoms after the treatment. Similarly, for the IPSS Quality of Life (QoL) Score, there was a significant improvement, with a mean difference of −4.257 (95 % CI: 4.105 to 4.408; p<0.0001), suggesting a considerable enhancement in the patients’ quality of life following the procedure. Lastly, for the International Index of Erectile Function (IIEF) Score for Erectile Dysfunction, there was a significant increase, with a mean difference of 1.845 (95 % CI: 1.592 to 2.099; p<0.0001), indicating a notable improvement in erectile function after the treatment. These results are reported in Table 2 and in Figure 1.
Outcome measures before and after treatment.
| Variable | Mean difference | 95 % confidence interval | p-Value |
|---|---|---|---|
| PVR | −169.645 | −148.911 to −190.379 | <0.0001 |
| Qmax | 17.934 | 19.312 to 16.556 | <0.0001 |
| IPSS | −19.502 | 18.645 to 20.359 | <0.0001 |
| IPSS QoL score | −4.257 | 4.105 to 4.408 | <0.0001 |
| IIEF | 1.845 | 2.099 to 1.592 | <0.0001 |
-
PVR: post-void residue; Qmax: peak urinary flux; IPSS: International Prostate Symptom Score; IIEF: International Index Of Erectile Function.
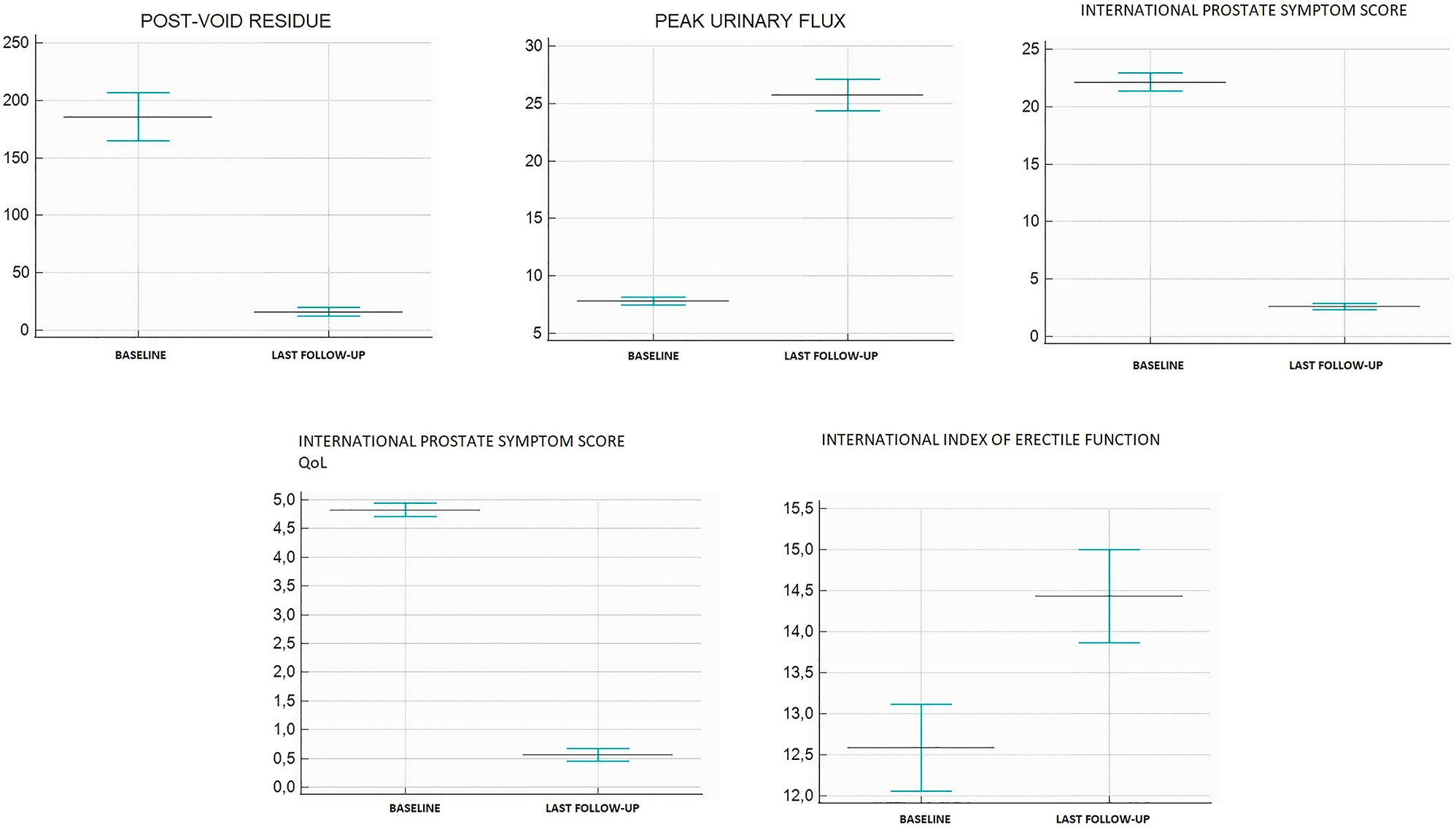
Mean variations in clinical outcomes.
The analysis revealed significant associations between different quartiles of several variables and the variation of the outcome measures. Firstly, for post-void residue (PVR), there was a significant difference in the variation of the outcome among patients in different PVR quartiles at baseline (p=0.024). Secondly, for peak urinary flux (Qmax), patients in different Qmax quartiles at baseline exhibited significantly different variations in Qmax (p<0.001) Additionally, the analysis showed significant associations between the quartiles of urinary symptoms and Qmax (p=0.030 and p<0.001, respectively), indicating diverse variations in urinary symptoms and peak urinary flux within different quartile groups. Moreover, erectile function was significantly associated with quartiles of age (p<0.001) and prostate volume (p=0.001), suggesting varied changes in erectile function based on age and prostate volume quartiles. Lastly, ASA (aspirin usage) showed a significant association with the variation in erectile function (p=0.033) (the most clinically relevant associations are depicted in Figures 2 and 3).

Mean variations in international index of erectile function divided per quartiles of peak urinary flux (on the left) and post-void residual volume (on the right). Quartiles are ordered in ascending order, with the lowest quartile on the left and the highest quartile on the right.
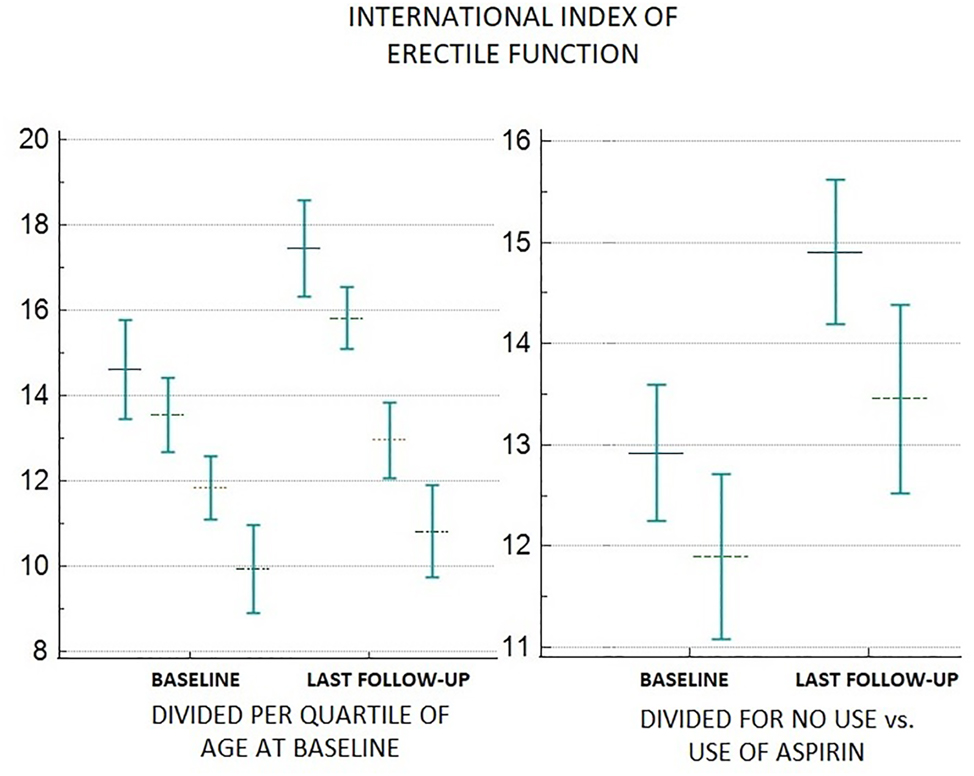
Mean variations in International Index of Erectile function divided per quartiles of age (on the left) and aspirin use (on the right). Quartiles are ordered in ascending order, with the lowest quartile on the left and the highest quartile on the right, while non-aspirin users are reported on the left and aspirin users are reported on the right.
Discussion
Transurethral resection of the prostate (TURP) is considered the standard treatment for benign prostatic hyperplasia (BPH). In a prospective study involving 10,654 patients who underwent TURP in the state of Bavaria, Germany, from January 2002 to December 2003, detailed case records were maintained, capturing preoperative status, operation details, complications, and immediate outcomes. The study revealed a low mortality rate of 0.10 % and a cumulative short-term morbidity rate of 11.1 %. Notable complications included failure to void (5.8 %), surgical revision (5.6 %), significant urinary tract infection (3.6 %), bleeding requiring transfusions (2.9 %), and transurethral resection syndrome (1.4 %). Importantly, the procedure led to a significant improvement in urinary peak flow rate and post-void residual volume, demonstrating its effectiveness as a treatment option for BPH [14].
Another recently conducted study confirmed the surgical outcomes of transurethral resection of the prostate (TURP) in elderly patients with chronic urinary retention (CUR) at a high-volume university teaching hospital. Among the 147 catheterized patients aged 80 years and older who underwent TURP, 80.3 % were catheter-free or using intermittent self-catheterization at the initial 3-month follow-up, and 79.6 % remained catheter-free at the 1-year follow-up. The study identified risk factors for surgical failure, including postvoid residual >1,500 mL, age ≥90, and poor the World Health Organization performance status. Importantly, a subset of patients excluding these risk factors demonstrated a catheter-free rate of 88.8 % at the 3-month follow-up [15].
In this retrospective observational study, we investigated the functional outcomes of thulium laser enucleation of the prostate (ThuLEP) for benign prostatic hyperplasia (BPH) in a cohort of 265 patients at Moriggia Pelascini Hospital (Como, Italy). Our findings provide valuable insights into the effectiveness of ThuLEP as a treatment option for BPH and shed light on the factors that may influence treatment outcomes. Our study population comprised patients with complete baseline and follow-up data for various parameters, including peak urinary flow rate (Qmax), post-void residue volume, erectile function, quality of life, and urinary symptoms. This comprehensive dataset allowed us to assess the impact of ThuLEP on multiple aspects of urinary and erectile function, as well as patients’ overall quality of life.
We found that ThuLEP led to significant improvements in various functional outcomes. Notably, there was a substantial decrease in post-void residue (PVR) following the procedure, indicating a significant improvement in voiding efficiency. This finding is in line with published studies, confirming the effectiveness of ThuLEP in relieving bladder outlet obstruction and reducing residual urine volume. Furthermore, we observed a considerable increase in peak urinary flow rate (Qmax) after ThuLEP. This improvement in Qmax is indicative of enhanced urinary function and a reduction in lower urinary tract symptoms. The International Prostate Symptom Score (IPSS) for urinary symptoms exhibited a substantial decrease following the procedure, indicating a significant reduction in urinary symptoms. This improvement in IPSS is consistent with the known benefits of TURP in alleviating lower urinary tract symptoms and improving overall urinary function in patients with BPH [16]. Another important finding was the significant improvement in the IPSS Quality of Life (QoL) score following ThuLEP. This improvement suggests a considerable enhancement in the patients’ quality of life, as urinary symptoms can have a profound impact on daily activities and overall well-being. Moreover, we observed a notable increase in the International Index of Erectile Function (IIEF) score for erectile dysfunction after ThuLEP. This finding suggests that ThuLEP may have a positive impact on erectile function in patients with BPH. While the exact mechanism behind this improvement requires further investigation, it is possible that the relief of bladder outlet obstruction and improvement in urinary function may contribute to enhanced erectile function in some patients. Our analysis also explored the associations between different quartiles of various baseline variables and the variation of outcome measures. Our results compare favorably with those obtained by Muntener who investigated sexual function after transurethral resection of the prostate (TURP), in a total of 1,014 patients. Out of the patients who responded, 722 (73.1 %) before TURP and 474 (73.8 %) after TURP stated that they were still sexually active. The mean erectile function score also showed an insignificant improvement from 1.66 to 1.47 (p=0.11) after TURP [17].
We observed significant associations between certain baseline characteristics and treatment effectiveness. Patients in different quartiles of post-void residue (PVR) and peak urinary flow rate (Qmax) at baseline exhibited significantly different variations in these parameters after ThuLEP. Additionally, age and prostate volume quartiles were linked to changes in erectile function, suggesting their potential influence on the response to ThuLEP regarding erectile function improvement [18, 19]. Notably, aspirin usage showed a negative significant association with the variation in erectile function. One possible explanation for the association between age and erectile function improvement is that younger patients may have better overall vascular health and treatment responsiveness, leading to more favorable outcomes. Conversely, older patients may experience more advanced age-related changes in vascular function that could limit the extent of erectile function improvement following ThuLEP. Similarly, the association found for aspirin use may simply be the result of poorer cardiovascular health in aspirin users, although aspirin has even been associated with improved erectile function [20, 21].
It is important to acknowledge the limitations of our study, including its retrospective nature and potential selection bias. Additionally, the follow-up duration may be relatively short for capturing long-term treatment effects. Despite these limitations, our study provides valuable real-world evidence on the functional outcomes of ThuLEP in a well-defined cohort of patients with BPH.
Conclusions
In conclusion, our study confirms that thulium laser enucleation of the prostate (ThuLEP) is an effective treatment option for benign prostatic hyperplasia (BPH), leading to significant improvements in voiding efficiency, urinary flow, urinary symptoms, quality of life, and erectile function. The findings from this study contribute to the growing body of evidence on ThuLEP as a primary surgical intervention for BPH, ultimately improving the overall management and quality of life of patients with this prevalent urological condition. Specifically, baseline characteristics, such as post-void residue, peak urinary flow rate, age, prostate volume, and aspirin usage, may influence treatment outcomes. We believe that these findings provide valuable insights for clinical decision-making in the management of BPH. Further prospective studies with longer follow-up periods are warranted to validate and expand upon our results.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Kaplan, SA. Benign prostatic hyperplasia. J Urol 2023;210:360–2. https://doi.org/10.1097/JU.0000000000003522.Search in Google Scholar PubMed
2. Gentile, F, La Civita, E, Della Ventura, B, Ferro, M, Cennamo, M, Bruzzese, D, et al.. A Combinatorial Neural Network Analysis Reveals a Synergistic Behaviour of Multiparametric Magnetic Resonance and Prostate Health Index in the Identification of Clinically Significant Prostate Cancer. Clin Genitourin Cancer 2022;20:e406–10. https://doi.org/10.1016/j.clgc.2022.04.013.Search in Google Scholar PubMed
3. Ghalayini, IF, Al-Ghazo, MA, Pickard, RS. A prospective randomized trial comparing transurethral prostatic resection and clean intermittent self-catheterization in men with chronic urinary retention. BJU Int 2005;96:93–7. https://doi.org/10.1111/j.1464-410X.2005.05574.x.Search in Google Scholar PubMed
4. Koudonas, A, Anastasiadis, A, Tsiakaras, S, Langas, G, Savvides, E, Mykoniatis, I, et al.. Overview of current pharmacotherapeutic options in benign prostatic hyperplasia. Expet Opin Pharmacother 2023;24:1–14. https://doi.org/10.1080/14656566.2023.2237406.Search in Google Scholar PubMed
5. Miro, C, Di Giovanni, A, Murolo, M, Cicatiello, AG, Nappi, A, Sagliocchi, S, et al.. Thyroid hormone and androgen signals mutually interplay and enhance inflammation and tumorigenic activation of tumor microenvironment in prostate cancer. Cancer Lett 2022;532. https://doi.org/10.1016/j.canlet.2022.215581.Search in Google Scholar PubMed
6. Roehrborn, CG. BPH progression: concept and key learning from MTOPS, ALTESS, COMBAT, and ALF-ONE. BJU Int 2008;101:17–21. https://doi.org/10.1111/j.1464-410X.2008.07497.x.Search in Google Scholar PubMed
7. Gilling, PJ, Wilson, LC, King, CJ, Westenberg, AM, Frampton, CM, Fraundorfer, MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int 2012;109:408–11. https://doi.org/10.1111/j.1464-410X.2011.10359.x.Search in Google Scholar PubMed
8. Kuntz, RM. Current role of lasers in the treatment of benign prostatic hyperplasia (BPH). Eur Urol 2006;49:961–9. https://doi.org/10.1016/j.eururo.2006.03.028.Search in Google Scholar PubMed
9. Trama, F, Lauro, GD, Illiano, E, Iacono, F, Romis, L, Mordente, S, et al.. Ejaculation sparing thulium laser enucleation of the prostate: an observational prospective study. J Clin Med 2022;11. https://doi.org/10.3390/jcm11216365.Search in Google Scholar PubMed PubMed Central
10. Ganem, S, Ambinder, D, Kennedy, A, Wong, NC. A 40-year litigation review of transurethral surgeries for benign prostatic hyperplasia. Urology 2022;168:165–8. https://doi.org/10.1016/j.urology.2022.06.013.Search in Google Scholar PubMed
11. Rieken, M, Bachmann, A, Shariat, SF. Long-term follow-up data more than 5 years after surgical management of benign prostate obstruction: who stands the test of time? Curr Opin Urol 2016;26. https://doi.org/10.1097/mou.0000000000000244.Search in Google Scholar PubMed
12. Barry, MJ, Fowler, FJ, O’Leary, MP, Bruskewitz, RC, Holtgrewe, HL, Mebust, WK, et al.. The American urological association symptom index for benign prostatic hyperplasia. J Urol 1992;148:1549–57. https://doi.org/10.1016/S0022-5347(17)36966-5.Search in Google Scholar PubMed
13. Rosen, RC, Riley, A, Wagner, G, Osterloh, IH, Kirkpatrick, J, Mishra, A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997;49:822–30. https://doi.org/10.1016/S0090-4295(97)00238-0.Search in Google Scholar PubMed
14. Oliver, R, Christian, G, Alexander, B, Michael, S, Boris, S, Peter, H, et al.. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246–9. https://doi.org/10.1016/j.juro.2008.03.058.Search in Google Scholar PubMed
15. Antoniou, V, Edris, F, Akpobire, W, Voss, J, Somani, B. Surgical outcomes for elderly patients undergoing transurethral resection of the prostate for chronic urinary retention and proposal of a management algorithm. J Endourol 2023;37:581–6. https://doi.org/10.1089/end.2022.0654.Search in Google Scholar PubMed
16. Aisuodionoe-Shadrach, OI, Akporiaye, LE. Outcome of the TURP-TUVP sandwich procedure for minimally invasive surgical treatment of benign prostatic hyperplasia with volume larger than 40cc over a 4-year period in Nigeria. Afr J Urol 2013;19:22–5. https://doi.org/10.1016/j.afju.2012.10.003.Search in Google Scholar
17. Muntener, M, Aellig, S, Kuettel, R, Gehrlach, C, Sulser, T, Strebel, RT. Sexual function after transurethral resection of the prostate (TURP): results of an independent prospective multicentre assessment of outcome. Eur Urol 2007;52:510–16. https://doi.org/10.1016/j.eururo.2007.01.088.Search in Google Scholar PubMed
18. Cantone, E, Massanova, M, Crocetto, F, Barone, B, Esposito, F, Arcaniolo, D, et al.. The relationship between obstructive sleep apnoea and erectile dysfunction: an underdiagnosed link? A prospective cross-sectional study. Andrologia 2022;54:e14504. https://doi.org/10.1111/and.14504.Search in Google Scholar PubMed PubMed Central
19. Romano, L, Pellegrino, R, Sciorio, C, Barone, B, Gravina, AG, Santonastaso, A, et al.. Erectile and sexual dysfunction in male and female patients with celiac disease: a cross-sectional observational study. Andrology 2022;10:910–18. https://doi.org/10.1111/andr.13186.Search in Google Scholar PubMed PubMed Central
20. Irfan, M, Ismail, S, Norhayati, N, Nik Hussain, NH. Efficacy of aspirin for vasculogenic erectile dysfunction in men: a meta-analysis of randomized control trials. Am J Men’s Health 2020;14:1557988320969082. https://doi.org/10.1177/1557988320969082.Search in Google Scholar PubMed PubMed Central
21. Bayraktar, Z, Albayrak, S. Antiplatelet (aspirin) therapy as a new option in the treatment of vasculogenic erectile dysfunction: a prospective randomized double-blind placebo-controlled study. Int Urol Nephrol 2018;50:411–8. https://doi.org/10.1007/s11255-018-1786-0.Search in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorials
- Doctor patient relationship in AI era: trying to decipher the problem
- “Adiponcosis interplay: adipose tissue, microenvironment and prostate cancer”
- Minireview
- Interplay between male gonadal function and overall male health
- Reviews
- How should we differentiate hypoglycaemia in non-diabetic patients?
- Pozelimab, a human monoclonal immunoglobulin for the treatment of CHAPLE disease
- Cannabis effectiveness on immunologic potency of pulmonary contagion
- Exploring the impact of vitamin D on tendon health: a comprehensive review
- The underlying causes, treatment options of gut microbiota and food habits in type 2 diabetes mellitus: a narrative review
- Original Articles
- Long-term functional outcomes and predictors of efficacy in thulium laser enucleation of the prostate (ThuLEP) for benign prostatic hyperplasia (BPH): a retrospective observational study
- Investigating Majhool date (Phoenix dactylifera) consumption effects on fasting blood glucose in animals and humans
- A novel variant in the FLNB gene associated with spondylocarpotarsal synostosis syndrome
- Exploring pathogenic pathways in carpal tunnel syndrome: sterile inflammation and oxidative stress
Articles in the same Issue
- Frontmatter
- Editorials
- Doctor patient relationship in AI era: trying to decipher the problem
- “Adiponcosis interplay: adipose tissue, microenvironment and prostate cancer”
- Minireview
- Interplay between male gonadal function and overall male health
- Reviews
- How should we differentiate hypoglycaemia in non-diabetic patients?
- Pozelimab, a human monoclonal immunoglobulin for the treatment of CHAPLE disease
- Cannabis effectiveness on immunologic potency of pulmonary contagion
- Exploring the impact of vitamin D on tendon health: a comprehensive review
- The underlying causes, treatment options of gut microbiota and food habits in type 2 diabetes mellitus: a narrative review
- Original Articles
- Long-term functional outcomes and predictors of efficacy in thulium laser enucleation of the prostate (ThuLEP) for benign prostatic hyperplasia (BPH): a retrospective observational study
- Investigating Majhool date (Phoenix dactylifera) consumption effects on fasting blood glucose in animals and humans
- A novel variant in the FLNB gene associated with spondylocarpotarsal synostosis syndrome
- Exploring pathogenic pathways in carpal tunnel syndrome: sterile inflammation and oxidative stress

