The incidence of different forms of ileus following surgery for abdominal birth defects in infants: a systematic review with a meta-analysis method
-
Laurens D. Eeftinck Schattenkerk
, Gijsbert D. Musters
Abstract
Objectives
Ileus following surgery can arise in different forms namely as paralytic ileus, adhesive small bowel obstruction or as anastomotic stenosis. The incidences of these different forms of ileus are not well known after abdominal birth defect surgery in infants. Therefore, this review aims to estimate the incidence in general between abdominal birth defects.
Content
Studies reporting on paralytic ileus, adhesive small bowel obstruction or anastomotic stenosis were considered eligible. PubMed and Embase were searched and risk of bias was assessed. Primary outcome was the incidence of complications. A meta-analysis was performed to pool the reported incidences in total and per birth defect separately.
Summary
This study represents a total of 11,617 patients described in 152 studies of which 86 (56%) had a follow-up of at least half a year. Pooled proportions were calculated as follows; paralytic ileus: 0.07 (95%-CI, 0.05–0.11; I 2=71%, p≤0.01) ranging from 0.14 (95% CI: 0.08–0.23) in gastroschisis to 0.05 (95%-CI: 0.02–0.13) in omphalocele. Adhesive small bowel obstruction: 0.06 (95%-CI: 0.05–0.07; I 2=74%, p≤0.01) ranging from 0.11 (95% CI: 0.06–0.19) in malrotation to 0.03 (95% CI: 0.02–0.06) in anorectal malformations. Anastomotic stenosis after a month 0.04 (95%-CI: 0.03–0.06; I 2=59%, p=0.30) ranging from 0.08 (95% CI: 0.04–0.14) in gastroschisis to 0.02 (95% CI: 0.01–0.04) in duodenal obstruction. Anastomotic stenosis within a month 0.03 (95%-CI 0.01–0.10; I 2=81%, p=0.02) was reviewed without separate analysis per birth defect.
Outlook
This review is the first to aggregate the known literature in order approximate the incidence of different forms of ileus for different abdominal birth defects. We showed these complications are common and the distribution varies between birth defects. Knowing which birth defects are most at risk can aid clinicians in taking prompt action, such as nasogastric tube placement, when an ileus is suspected. Future research should focus on the identification of risk factors and preventative measures. The incidences provided by this review can be used in those studies as a starting point for sample size calculations.
Introduction
Ileus following surgery, consisting of both paralytic and mechanical causes, is a frequent complication after abdominal surgery, leading to increased morbidity, mortality, medical costs, and increased length of hospital stay [1], [2], [3], [4]. It is a clinical diagnosis which is characterized by intolerance to oral feeds, vomiting, abdominal distention, and the absence of flatus or stool.
Ileus following surgery can arise in different forms which depend on the definition used. Common causes are paralytic ileus, adhesive small bowel obstruction (SBO) and anastomotic stenosis. Paralytic ileus is a transient form of ileus which arises shortly after the operation in a response to surgical stress and is based on temporarily intestinal paralysis [5]. Anastomotic stenosis and SBO are mechanical forms of ileus that present later after surgery and could lead to reoperation.
Since abdominal birth defects are rare, the incidence of these forms of ileus are not well known. Yet, knowing the incidences would provide context for clinical decision making as well as a starting point for future research into preventative measures. Therefore, the objective of this review is to systematically aggregate the available data on the incidence of different forms of ileus following surgery for birth defects in infants.
Methods
Studies were selected according to the criteria outlined below based on the PRISMA Guidelines [6]. Our protocol has been registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 7 March 2019 (registration number: CRD42019119268).
Participants
All studies reporting on any form of ileus following surgery for birth defects as primary of secondary endpoint were considered eligible. Only articles that described infants (≤three years) and specifically named the different forms of ileus were included. Animal studies, in vitro studies, non-English or non-Dutch articles, congress abstracts and studies with less than 10 cases were excluded.
Search strategy
The electronic databases of the National Institutes of Health PubMed and EMBASE were systematically searched in February 2020 using both simple search terms as well as hierarchical family forms (e.g. MESH). The search strategy was designed together with a medical information specialist (RV). It combined four groups of search terms and their equivalents [1]: terms related to the age group of the patients at the moment of surgery (e.g. infantile patients) [2]; terms related to the location of surgery (e.g. abdominal surgery) [3]; terms related to congenital abdominal anomalies (e.g. gastroschisis) [4]; terms related to post-operative complications (e.g. adhesive ileus). Mesh and search terms used in Pubmed are included in Appendix 1.
Primary and secondary outcomes
The primary endpoint was the pooled percentage of the three forms of ileus. We separately reviewed anastomotic stenosis within a month and after one month. Secondary endpoint was the pooled percentage per birth defect.
Terms included in paralytic ileus are: ileus (not related to anastomotic stricture) and post-operative ileus. Terms that only implied feeding problems without specifying the reason were not included. Terms included in adhesive small bowel obstruction are: intestinal obstruction, small bowel obstruction, adhesive ileus and stricture (not related to anastomosis). No additional terms or definitions were used for anastomotic stenosis; each article that specifically stated anastomotic stenosis was included. The early anastomotic stenosis, occurring within one month, were excluded for the analysis into late onset anastomotic stenosis.
For each complication separately, a Forest plot was created containing the estimated overall pooled proportion and the corresponding 95%-CIs. In each Forest plot, we also reported the pooled proportion and CIs per disease if [1]; at least three studies reported the specific complication in the disease or [2] if the total number of patients with the disease was ≥100 combined [3]; there was at least one event of a complication present in all studies on a specific disease combined. Birth defects that did not meet these criteria were present in the overall pooled proportion and reported as residuals. Follow-up was reported when relevant.
For all studies with multiple arms, data of both trial-arms were combined. If only one arm matched the inclusion criteria, the appropriate arm was used. Additionally extracted parameters were: author, country of conduct, year of publication, journal, study design, duration of follow-up, number of participants and type of birth defect.
Data extraction
Titles and abstracts were screened to exclude nonrelated publications. Screening was done by two independent authors (LES, DN) using Rayyan. Disagreements were resolved by discussion between the two reviewers. If no consensus could be reached, a third specialist author was consulted (JD, GM). Then, the full texts of the remaining articles were read to determine eligibility for inclusion (LES, DN). If the full text was not found the authors were contacted. The reference lists of the included articles were cross checked to find additional articles.
Validity and eligibility assessment
All included articles were assessed for the methodological quality and risk of bias. For cohort studies the Newcastle Ottawa quality assessment scale was used [7]. In randomized controlled trials this was done using the Jadad scoring system [8]. The assessment was done by LES and DN separately.
Data synthesis
For each complication and each disease in a study, a weighted average of the logit proportions was determined by the use of the generic inverse variance method. The logit proportions were back transformed to the summary estimate and 95%-CIs were obtained in a summary proportion representing the pooled proportion of the form of ileus. Heterogeneity was assessed using the I 2 and χ 2 statistics. Analyses were performed with the use of R-studio version 3.6.1 (package “meta” (Schwarzer, 2007) and “metaprop” (Viachtbauer, 2010)). The random-effects model was used for interpretation. Heterogeneity was deemed significant if the pooled data’s p value was <0.05 or χ 2 statistics were ≥75. Heterogeneity was interpreted as small (I 2≤0.25), medium (I 2=0.25–0.50) or strong (I 2≥0.50), according to Higgins [9].
Results
Study characteristics
In total, 5,784 records were identified. After automated removal of duplicates, 3,909 records were left for title and abstract screening. Of the 3,909 records, 722 were included and assessed for full text. Following full text evaluation 152 studies were included for quantitative analysis (Figure 1). Of the 152 studies, 118 were retrospective cohort studies, 25 were prospective cohort studies, four were retrospective multicentre cohort studies, two were retrospective matched case-control studies, two were randomized controlled trials and one was a combined study of a prospective and retrospective cohort. Studies were conducted in 31 different countries. Asian countries were most prominent with 58 studies, European studies represented 41, North- & South-America represented 38, Africa represented 9, The Middle-East 4 and Oceania represented 2. Of the 152 studies, 86 (57%) reported a follow-up of at least half a year.
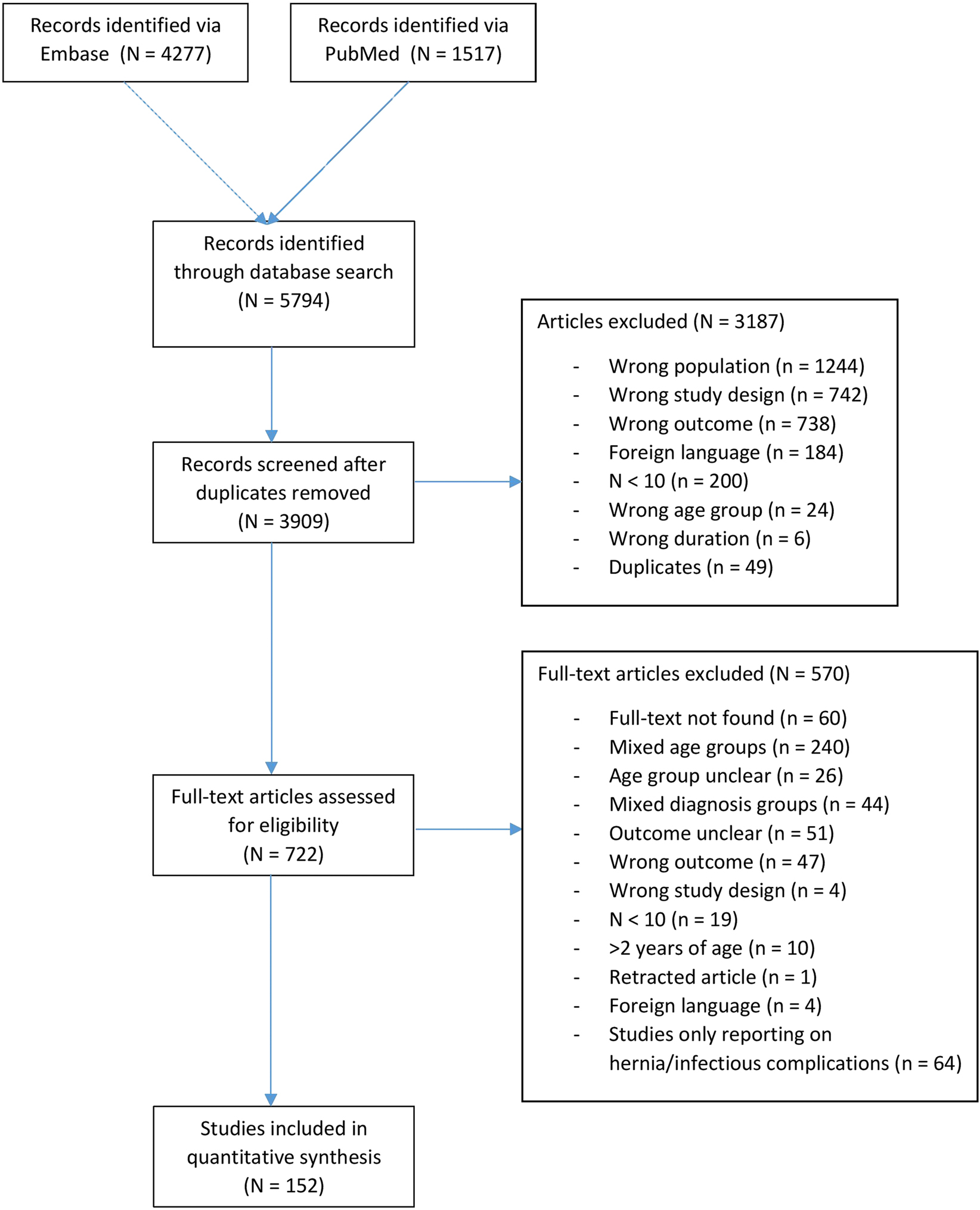
Flow-chart article selection.
This systematic review and meta-analysis represent 11,617 patients described in 152 studies presented in Table 1 []. Among these patients, the congenital conditions were divided as follows: Hirschsprung’s disease (n=4,341, 37%); gastroschisis (n=1,558, 13%); duodenal obstruction (n=1,068, 9%); anorectal malformations (n=1,047, 9%); small intestinal atresia (n=794, 7%); congenital diaphragmatic hernia (n=778, 7%); biliary atresia (n=681, 6%); malrotation (n=608, 5%); omphalocele (n=464, 4%); choledochal cyst (n=148, 1%); meconium ileus (n=54, >1%); Meckel’s diverticula (n=46, >1%); colonic atresia (n=30, >1%).
Study characteristics.
| Author | Year | Journal | Country | Design | FU>0.5y | Study duration | Anomaly | POI | SBO | AS < month | ÀS > month |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stollman | 2008 | Journal of Paediatric Surgery | Netherlands | Retrospective cohort study | No | 1971–2004 | Small intestinal atresia | 2/110 | 12/110 | 1/110 | 6/110 |
| Guo | 2010 | Transplantation Proceedings | China | Retrospective cohort study | No | 2006–2009 | Biliary atresia | 2/22 | X | X | X |
| Walter-Nicolet | 2009 | Journal of Paediatric Gastroenterology and Nutrition | France | Prospective cohort study | Yes | 2004–2006 | Gastroschisis | X | 2/73 | X | X |
| Wang | 2013 | Hepatobiliary Pancreat Dis Int | China | Retrospective cohort study | Yes | 2008–2011 | Biliary atresia | X | 2/73 | X | X |
| Lee | 2012 | Paediatric Surgery International | South Korea | Retrospective cohort study | No | 2001–2010 | Small intestinal atresia | X | 3/11 | X | X |
| Cox | 2005 | Paediatric Surgery International | South Africa | Retrospective cohort study | Yes | 1966–2004 | Colonic atresia | X | 0/14 | 2/14 | 0/14 |
| Festen | 2002 | Journal of Paediatric Surgery | Netherlands | Multi-centre (5) retrospective cohort | Yes | 1980–1992 | Small intestinal atresia | 1/15 | X | 4/15 | 1/14 |
| Escobar | 2005 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 1972–2004 | Hirschsprung’s disease | X | 5/33 | X | 5/33 |
| Yan | 2017 | Biomedical Research | China | Prospective cohort study | Yes | 2011–2014 | Hirschsprung’s disease | 2/38 | 2/38 | X | 2/38 |
| Mirshemirani | 2007 | Acta Medica Iranica | Iran | Prospective cohort study | Yes | 1993–2003 | ARM | X | X | 0/30 | 0/30 |
| Dariel | 2015 | European Journal of Paediatric Surgery | Canada | Retrospective cohort study | Yes | 2006–2010 | Gastroschisis | X | 6/63 | X | X |
| Mendez-Martinez | 2016 | European Journal of General Medicine | Mexico | Prospective cohort study | No | 2008–2013 | Gastroschisis | 6/42 | 7/42 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Hirschsprung’s disease | X | 19/65 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Malrotation | X | 13/45 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Small intestinal atresia | X | 11/40 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Gastroschisis | X | 9/85 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Duodenal obstruction | X | 10/93 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Omphalocele | X | 4/44 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Congenital diaphragmatic hernia | X | 6/75 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | ARM | X | 4/58 | X | X |
| Fredriksson | 2015 | British Journal of Surgery | Sweden | Retrospective cohort study | Yes | 1976–2011 | Biliary atresia | X | 0/28 | X | X |
| Werbeck | 2010 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 1991–2010 | Gastroschisis | X | 2/13 | X | X |
| Demirogullari | 2011 | Paediatric Surgery International | Turkey | Retrospective cohort study | No | 1998–2011 | ARM | X | 2/112 | X | X |
| Rouzrokh | 2010 | Paediatric Surgery International | Iran | Retrospective cohort study | Yes | 2006–2009 | Hirschsprung’s disease | X | X | X | 12/86 |
| S. Li | 2017 | European Review for Medical and Pharmacological Sciences | China | Retrospective cohort study | Yes | 2006–2013 | Hirschsprung’s disease | X | X | 0/15 | X |
| Ghosh | 2016 | ANZ Journal of Surgery | Australia | Retrospective cohort study | Yes | 2005–2012 | Hirschsprung’s disease | X | 3/50 | X | 2/50 |
| Chen | 2014 | World J. Paediatric Surgery | China | Retrospective cohort study | Yes | 2003–2012 | Duodenal obstruction | X | 4/287 | X | X |
| Bianchi | 1998 | Seminars in Paediatric Surgery | England | Retrospective cohort study | Yes | 1984–1997 | Hirschsprung’s disease | X | 2/13 | X | X |
| Mattioli | 1998 | Journal of Paediatric Surgery | Italy | Retrospective cohort study | No | 1993–1996 | Hirschsprung’s disease | X | X | 0/8 | 0/8 |
| Teitelbaum | 1998 | Seminars in Paediatric Surgery | USA | Retrospective cohort study | Yes | X | Hirschsprung’s disease | X | 4/24 | X | 0/24 |
| Demirbilek | 1999 | Paediatric Surgery International | Turkey | Retrospective cohort study | Yes | 1987–1997 | ARM | X | X | X | 1/31 |
| Santos | 1999 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1988–1999 | Hirschsprung’s disease | X | 4/65 | X | X |
| de la Torre | 2000 | Journal of Paediatric Surgery | Mexico | Retrospective cohort study | Yes | 1994–2000 | Hirschsprung’s disease | X | 0/10 | X | X |
| Fleet | 2000 | Journal of Paediatric Surgery | England | Retrospective cohort study | Yes | 1991–1997 | Gastroschisis | X | X | X | 1/10 |
| Fleet | 2000 | Journal of Paediatric Surgery | England | Retrospective cohort study | Yes | 1991–1997 | Small intestinal atresia | X | X | X | 1/6 |
| Fleet | 2000 | Journal of Paediatric Surgery | England | Retrospective cohort study | Yes | 1991–1997 | Colonic atresia | X | X | X | 0/3 |
| Hay | 2000 | Journal of Paediatric Surgery | Egypt | Retrospective cohort study | No | X | Biliary atresia | X | 1/21 | X | X |
| Langer | 2000 | Journal of Paediatric Surgery | USA | Prospective cohort study | No | X | Hirschsprung’s disease | X | 2/22 | 10/22 | X |
| Patwardhan | 2001 | Journal of Paediatric Surgery | England | Retrospective cohort study | Yes | 1994–1999 | ARM | X | 5/49 | X | X |
| Snyder | 2001 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1969–2000 | Gastroschisis | X | 21/199 | X | X |
| Snyder | 2001 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1969–2000 | Small intestinal atresia | X | 9/25 | X | X |
| Höllwarth | 2002 | Journal of Paediatric Surgery | Austria | Retrospective cohort study | Yes | 1988–2000 | Hirschsprung’s disease | X | X | X | X |
| Saxena | 2001 | The world journal of Hernia | Germany | Prospective cohort study | Yes | 1984–1998 | Omphalocele | 1/50 | 2/50 | X | X |
| Saxena | 2001 | Paediatric Surgery International | Germany | Prospective cohort study | Yes | 1984–1998 | Gastroschisis | X | 10/70 | X | X |
| Önen | 2003 | Paediatric Surgery International | Turkey | Prospective/retrospective cohort | No | 1990–2000 | Meckel’s diverticulum | X | 2/34 | X | X |
| Shah | 2003 | Journal of Paediatric Surgery | India | Prospective cohort study | Yes | X | ARM | X | X | X | 0/12 |
| Weidner | 2003 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1998–2001 | Hirschsprung’s disease | X | 0/15 | X | X |
| Escobar | 2004 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 1972–2001 | Duodenal obstruction | X | 5/169 | X | 1/169 |
| Kubota | 2004 | Journal of Paediatric Surgery | Japan | Prospective cohort study | Yes | 1990–2001 | Hirschsprung’s disease | X | 1/41 | X | X |
| Wester | 2004 | Journal of Paediatric Surgery | Finland | Retrospective cohort study | No | 2000–2003 | Hirschsprung’s disease | X | X | 0/15 | 0/15 |
| Majid | 2015 | Pakistan Paediatric Journal | Pakistan | Prospective cohort study | Yes | X | Duodenal obstruction | X | 3/27 | X | X |
| Sauer | 2005 | Journal of Paediatric Surgery | Canada | Retrospective cohort study | No | 1999–2003 | Hirschsprung’s disease | X | 2/24 | X | 0/24 |
| Thepcharoennirund | 2005 | Journal of Medical Association of Thailand | Thailand | Retrospective cohort study | No | 1987–2004 | Gastroschisis | 12/129 | X | X | X |
| Chiu | 2006 | Journal of Perinatal Medicine | USA | Retrospective cohort study | No | 1994–2004 | Gastroschisis | X | 1/43 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 1998–2003 | Gastroschisis | X | 2/32 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 1999–2003 | ARM | X | 0/46 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2000–2003 | Omphalocele | X | 0/25 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2001–2003 | Meconium ileus | X | 5/20 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2001–2003 | Malrotation | X | 3/23 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2001–2003 | Diaphragmatic hernia | X | 1/25 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2001–2003 | Hirschsprung’s disease | X | 2/33 | X | X |
| Choudhry | 2006 | Paediatric Surgery International | England | Retrospective cohort study | Yes | 2001–2003 | Small intestinal atresia | X | 4/36 | X | X |
| Lee | 2006 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 1981–2002 | Omphalocele | 1/20 | X | X | X |
| A. Li | 2006 | Chinese Medical Journal | China | Retrospective cohort study | Yes | 1999–2004 | Hirschsprung’s disease | X | 1/252 | X | 16/252 |
| Liem | 2006 | Asian Journal of Surgery | Vietnam | Prospective cohort study | Yes | 2002–2004 | Hirschsprung’s disease | 0/53 | X | X | X |
| Maksoud-Filho | 2006 | Paediatric Surgery International | Brazil | Retrospective cohort study | No | 1998–2005 | Gastroschisis | X | 1/43 | X | X |
| Owen | 2006 | Journal of Paediatric Surgery | England | Retrospective cohort study | No | 1990–2004 | Gastroschisis | X | 0/48 | X | X |
| Banieghbal | 2007 | Journal of Paediatric Surgery | South Africa | Prospective cohort study | Yes | 2002–2005 | Small intestinal atresia | X | X | 2/16 | X |
| Dutta | 2007 | Journal of laparoendoscopic | USA | Retrospective cohort study | No | 2002–2005 | Biliary atresia | X | 2/10 | X | X |
| Menon | 2007 | Journal of Paediatric Surgery | India | Prospective cohort study | Yes | 1997–2005 | ARM | X | X | X | 0/46 |
| Riehle | 2007 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1993–2004 | Congenital diaphragmatic hernia | X | 7/125 | X | X |
| Stringer | 2007 | Journal of Paediatric Surgery | United Kingdom | Prospective cohort study | Yes | 1994–2006 | Biliary atresia | X | 2/60 | X | X |
| Baglaj | 2007 | European Journal of Paediatric Surgery | United Kingdom | Retrospective cohort study | No | 1986–2006 | Small intestinal atresia | X | X | X | 2/26 |
| Henrich | 2007 | Paediatric Surgery International | Germany | Prospective cohort study | No | 1994–2004 | Gastroschisis | 11/40 | X | X | X |
| Henrich | 2007 | Paediatric Surgery International | Germany | Prospective cohort study | No | 1994–2004 | Omphalocele | 3/26 | X | X | X |
| Ishikawa | 2008 | Paediatric Surgery International | Japan | Retrospective cohort study | No | 1990–2001 | Hirschsprung’s disease | X | 1/49 | X | X |
| Shinall | 2008 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 1997–2001 | Hirschsprung’s disease | X | X | X | 3/60 |
| Spilde | 2008 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 2003–2007 | Duodenal obstruction | X | X | 2/29 | X |
| Tongsin | 2008 | Journal of Medical Association of Thailand | Thailand | Retrospective cohort study | No | 1988–2007 | Small intestinal atresia | 9/142 | 3/142 | X | 8/142 |
| van Eijck | 2008 | Journal of Paediatric Surgery | Netherlands | Retrospective cohort study | No | 1971–2004 | Gastroschisis | X | 14/55 | X | X |
| van Eijck | 2008 | Journal of Paediatric Surgery | Netherlands | Retrospective cohort study | No | 1971–2004 | Omphalocele | X | 12/92 | X | X |
| Zheng | 2008 | Paediatric Surgery International | China | Retrospective cohort study | No | 2004–2007 | ARM | X | 1/38 | X | X |
| Dassinger | 2009 | Paediatric Surgery International | USA | Retrospective cohort study | No | 1993–2008 | Colonic atresia | X | X | 0/12 | X |
| Ferreira | 2009 | Surgical Endoscopy | France | Prospective cohort study | No | X | Congenital diaphragmatic hernia | 1/30 | X | X | X |
| Gourlay | 2008 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 1993–2003 | Congenital diaphragmatic hernia | X | 4/38 | X | X |
| Hua | 2009 | Ghang Gung Medical Journal | Taiwan | Retrospective cohort study | Yes | 1991–2006 | Choledochal cyst | X | 1/30 | X | X |
| Liu | 2009 | Journal of Laparoendoscopic | China | Retrospective cohort study | Yes | 2003–2007 | Biliary atresia | X | 0/10 | X | X |
| Obermayr | 2008 | European Journal of Paediatric Surgery | Germany | Retrospective cohort study | Yes | 2002–2007 | Hirschsprung’s disease | X | X | X | 1/22 |
| Takahashi | 2009 | Journal of Paediatric Surgery | Japan | Retrospective cohort study | Yes | 1963–2008 | Biliary atresia | 1/12 | X | X | X |
| Gunnarsdottir | 2009 | European Journal of paediatric Surgery | Sweden | Prospective cohort study | Yes | 2000–2007 | Hirschsprung’s disease | X | 1/29 | X | X |
| Hong | 2010 | European journal of Obstetrics & Gynaecology | China | Prospective cohort study | Yes | 2004–2008 | Gastroschisis | 1/17 | 1/17 | X | X |
| Payne | 2010 | Journal of Neonatal-Perinatal Medicine | USA | Matched case-control study | Yes | 1999–2007 | Gastroschisis | X | 9/127 | X | X |
| Vu | 2010 | Paediatric surgery International | Vietnam | Prospective cohort study | Yes | 2004–2009 | Hirschsprung’s disease | X | X | X | 4/51 |
| de Vos | 2011 | South African Journal of Science | South Africa | Retrospective cohort study | Yes | 2000–2009 | ARM | X | X | X | 4/39 |
| Hill | 2011 | Journal of Laparoendoscopic | USA | Retrospective cohort study | No | 2001–2010 | Duodenal obstruction | 14/58 | X | X | 0/58 |
| Karimi | 2011 | Paediatric Surgery International | Netherlands | Retrospective cohort study | No | 1984–2007 | Meconium ileus | X | 4/34 | X | X |
| Kozlov | 2010 | European Journal of Surgery | Russia | Retrospective cohort study | No | 2005–2009 | Duodenal obstruction | X | X | 0/27 | X |
| Travassos | 2011 | Journal of Paediatric Surgery | Netherlands | Retrospective cohort study | Yes | 1988–2010 | Hirschsprung’s disease | X | 1/15 | X | 0/15 |
| van der Zee | 2011 | World J. Surgery | Netherlands | Retrospective cohort study | Yes | 2000–2010 | Duodenal obstruction | X | X | X | 1/28 |
| Li | 2012 | Paediatric surgery International | China | Retrospective cohort study | No | 2009–2012 | Small intestinal atresia | X | 3/35 | X | X |
| Liem | 2012 | Journal of Paediatric Surgery | Vietnam | Prospective cohort study | Yes | 2008–2010 | ARM | X | X | X | 0/10 |
| Romao | 2012 | Journal of Paediatric Surgery | Canada | Retrospective cohort study | Yes | 2000–2009 | Congenital diaphragmatic hernia | X | 3/22 | X | X |
| Sato | 2012 | Paediatric Surgery International | Japan | Retrospective cohort study | No | 2005–2011 | Small intestinal atresia | 1/25 | X | X | X |
| Sato | 2012 | Paediatric Surgery International | Japan | Retrospective cohort study | No | 2005–2011 | ARM | 1/13 | X | X | X |
| Weil | 2011 | Journal of Paediatric Surgery | USA | Retrospective cohort study | No | 2000–2009 | Gastroschisis | X | X | X | X |
| Ghaffarpour | 2013 | Journal of Paediatric Surgery | Sweden | Retrospective cohort study | No | X | Duodenal obstruction | X | 0/28 | X | X |
| Ferreira | 2013 | Journal of Paediatric Surgery | France | Retrospective cohort study | Yes | 2006–2010 | Congenital diaphragmatic hernia | X | 9/37 | X | X |
| Jensen | 2013 | Journal of Laparoendoscopic | USA | Retrospective cohort study | No | 2005–2011 | Duodenal obstruction | X | X | X | 1/66 |
| Nam | 2013 | World Journal of Surgery | South Korea | Retrospective cohort study | Yes | 2008–2011 | Congenital diaphragmatic hernia | X | 5/50 | X | X |
| Nio | 2013 | Paediatric Surgery International | Japan | Prospective RCT | Yes | 2006–2011 | Biliary atresia | 2/69 | X | X | X |
| van der Zee | 2013 | World Journal of Surgery | Netherlands | Retrospective cohort study | Yes | 2000–2011 | ARM | X | 1/19 | X | 1/19 |
| Diao | 2014 | International Journal of Surgery | China | Retrospective cohort study | Yes | 2011–2013 | Choledochal cyst | X | 0/27 | X | X |
| Diao | 2014 | Journal of Paediatric Surgery | China | Retrospective cohort study | Yes | 2011–2012 | ARM | X | X | X | 0/31 |
| Elder | 2014 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 2000–2011 | Malrotation | X | 13/102 | X | X |
| Friedmacher | 2014 | Paediatric surgery International | Austria | Retrospective cohort study | Yes | 1975–2008 | Gastroschisis | X | 27/108 | X | 8/108 |
| Ming | 2014 | Journal of Paediatric Surgery | China | Retrospective cohort study | Yes | 1992–2012 | ARM | X | X | X | 3/66 |
| Nasr | 2014 | Journal of Paediatric Surgery | Canada | Retrospective matched case control cohort study | No | 2000–2010 | Hirschsprung’s disease | 15/54 | 1/54 | X | 4/54 |
| Shrestha | 2014 | Journal Nepal Paediatric Society | Nepal | Prospective cohort study | Yes | 2008–2013 | Hirschsprung’s disease | X | 0/12 | X | 0/12 |
| Sulkowski | 2014 | Journal of Paediatric Surgery | USA | Retrospective multi-centre database research | Yes | 1999–2009 | Hirschsprung’s disease | X | 82/1,555 | X | 83/1,555 |
| Yang | 2014 | Journal of Paediatric Surgery | China | Retrospective cohort study | No | 2011–2013 | ARM | X | X | X | 0/20 |
| Madadi-Sanjani | 2015 | Biomedical Research International | Germany | Retrospective cohort study | No | 1975–2008 | Biliary atresia | X | 5/153 | X | X |
| Martinez-Criado | 2015 | Cirugia Espanola | Spain | Retrospective cohort study | No | 2003–2012 | Hirschsprung’s disease | X | 6/73 | X | 4/73 |
| Miyano | 2015 | Journal of Laparoendoscopic | Japan | Retrospective cohort study | Yes | 2007–2012 | Malrotation | X | 1/14 | X | X |
| Shangjie | 2014 | Cell Biochemical Biophysiology | China | Prospective cohort study | No | 2009–2014 | Hirschsprung’s disease | 28/281 | 27/281 | X | X |
| Almosallam | 2016 | Ann Saudi Medicine | Saudi Arabia | Retrospective cohort study | No | 2000–2014 | ARM | X | 4/104 | X | X |
| Diao | 2016 | Surgical Endoscopy | China | Retrospective cohort study | No | 2013–2014 | ARM | X | X | X | X |
| Guerra | 2016 | Journal of Paediatric Surgery | Canada | Retrospective cohort study | No | 1995–2014 | Hirschsprung’s disease | X | X | X | 5/36 |
| Inoue | 2016 | Surgical endoscopy | Japan | Retrospective cohort study | Yes | 2000–2014 | Congenital diaphragmatic hernia | X | 4/24 | X | X |
| Matsumoto | 2016 | Surgical Today | Japan | Retrospective cohort study | No | 1997–2015 | Choledochal cyst | X | 2/13 | X | X |
| Raitio | 2016 | European Journal of Paediatric Surgery | England | Retrospective cohort study | Yes | 2002–2014 | Malrotation | X | X | X | X |
| Diao | 2017 | Surgical endoscopy | China | Retrospective cohort study | No | 2013–2016 | ARM | X | X | X | 0/15 |
| Dingemann | 2017 | European Journal of Paediatric Surgery | Germany | Multicentre retrospective cohort | No | 2007–2012 | Omphalocele | X | 1/54 | X | X |
| C. Lu | 2017 | Journal of Paediatric Surgery | China | Multicentre retrospective cohort | Yes | 2005–2012 | Hirschsprung’s disease | X | X | X | 21/650 |
| Y. Lu | 2017 | Transplantation Proceedings | China | Retrospective cohort study | No | 2009–2014 | Biliary atresia | X | X | X | X |
| Oh | 2017 | Surgical Endoscopy | South Korea | Retrospective cohort study | No | 2005–2015 | Duodenal obstruction | X | X | X | 0/22 |
| Risby | 2017 | Journal of Paediatric Surgery | Denmark | Retrospective cohort study | Yes | 1997–2009 | Gastroschisis | X | 12/47 | X | X |
| Son | 2017 | Journal of Paediatric Surgery | Vietnam | Retrospective cohort study | No | 2009–2015 | Duodenal obstruction | X | X | X | 2/112 |
| Tyson | 2017 | Journal of Laparoendoscopic | USA | Retrospective cohort study | No | 2007–2015 | Congenital diaphragmatic hernia | X | 5/54 | X | X |
| van den Eijnden | 2017 | World Journal of Surgery | Netherlands | Retrospective cohort study | No | 1989–2014 | Choledochal cyst | X | 1/30 | 0/30 | X |
| Zani | 2017 | Paediatric Surgery International | Canada | Retrospective cohort study | Yes | 2004–2014 | Duodenal obstruction | X | 4/92 | X | 6/92 |
| Zmora | 2016 | American Journal of Surgery | USA | Retrospective cohort study | No | 2007–2015 | Gastroschisis | X | 1/11 | X | X |
| Zmora | 2016 | American Journal of Surgery | USA | Retrospective cohort study | No | 2007–2015 | Omphalocele | X | 0/6 | X | X |
| Avci | 2018 | Eastern Journal of Medicine | Turkey | Retrospective cohort study | No | 2008–2017 | Duodenal obstruction | X | 2/32 | X | X |
| Peng | 2018 | Journal of Paediatric Surgery | China | Retrospective cohort study | No | 2011–2015 | Small intestinal atresia | X | 2/41 | X | X |
| Xiao | 2018 | Medicine | China | Prospective cohort study | Yes | 2011–2014 | ARM | X | X | X | 0/56 |
| Xiao | 2018 | Journal of Surgical Research | China | Prospective RCT | Yes | 2011–2015 | Biliary atresia | X | 5/166 | X | X |
| Zhang | 2018 | Journal of Paediatric Surgery | China | Retrospective cohort study | Yes | 2011–2014 | Hirschsprung’s disease | X | X | X | 0/23 |
| England | 2012 | Journal of Paediatric Surgery | South Africa | Retrospective cohort study | Yes | 2005–2009 | ARM | X | X | X | 12/42 |
| Wakhlu | 2000 | Journal of Paediatric Surgery | India | Retrospective cohort study | Yes | 1972–1998 | Omphalocele | X | 2/64 | X | X |
| Pratap | 2007 | Journal of Paediatric Surgery | India | Retrospective cohort study | Yes | 2002–2006 | Hirschsprung’s disease | X | X | X | x |
| Abbas | 2016 | Journal of Paediatric Surgery | USA | Retrospective cohort study | Yes | 2002–2015 | Malrotation | X | 6/56 | X | X |
| Chan | 2019 | Journal of laparoendoscopic | Hong Kong | Retrospective database | Yes | 1993–2007 | Biliary atresia | X | 2/22 | X | X |
| de Bie | 2019 | Journal of Paediatric Surgery | Belgium | Retrospective multicentre database | Yes | 2000–2016 | Congenital diaphragmatic hernia | X | 1/62 | X | X |
| Dewberry | 2019 | Journal of Paediatric Surgery | USA | Retrospective cohort | No | 2008–2018 | Congenital diaphragmatic hernia | X | 5/70 | X | X |
| Dewberry | 2019 | Journal of surgical research | USA | Retrospective cohort | Yes | 2007–2017 | Small intestinal atresia | X | 2/47 | X | 2/47 |
| Dübbers | 2002 | European Journal of Paediatric Surgery | Germany | Retrospective cohort | Yes | 1990–2000 | Hirschsprung’s disease | X | 2/35 | X | X |
| Gabler | 2018 | South African Medical Journal | South Africa | Retrospective cohort | No | X | ARM | X | 0/50 | X | X |
| Gao | 2019 | Journal of International Medical Research | China | Retrospective cohort | No | 2018 | Meckel’s diverticulum | X | 0/12 | X | X |
| Gao | 2019 | Journal of International Medical Research | China | Retrospective cohort | No | 2018 | Hirschsprung’s disease | X | 0/35 | X | X |
| He | 2016 | Journal of Laparoendoscopic | China | Retrospective cohort | Yes | 2011–2016 | Congenital diaphragmatic hernia | X | 1/14 | X | X |
| Joda | 2019 | Updates in Surgery | Iraq | Prospective cohort | Yes | 2010–2017 | Small intestinal atresia | X | 3/34 | X | 4/34 |
| Jona | 2001 | Paediatric Endo-Surgery & Innovative Techniques | USA | Retrospective cohort | No | 1993–2000 | Hirschsprung’s disease | X | 0/44 | X | X |
| Long | 2019 | Arch Dis Child Fetal Neonatal Ed | England | Retrospective national database cohort | Yes | 2009–2010 | Congenital diaphragmatic hernia | X | 9/140 | X | X |
| Marei | 2019 | Egyptian Paediatric Association Gazette | Egypt | Retrospective cohort | Yes | 2014–2017 | Small intestinal atresia | 3/22 | X | 1/22 | X |
| Narang | 2019 | Journal of Obstetrics & Gynaecology | New Zealand | Retrospective cohort study | Yes | 2011–2016 | Gastroschisis | X | 6/71 | X | X |
| Narang | 2019 | Journal of Obstetrics & Gynaecology | New Zealand | Retrospective cohort study | Yes | 2011–2016 | Omphalocele | X | 0/22 | X | X |
| Jung | 1995 | Journal of Paediatric Surgery | South Korea | Retrospective cohort study | No | 1980–1991 | Hirschsprung’s disease | X | 2/77 | X | X |
| Ren | 2018 | Journal of Laparoendoscopic | China | Retrospective cohort study | Yes | 2005–2016 | ARM | 1/25 | X | X | X |
| Ryu | 2019 | Annals of Surgery Treatment and Research | South Korea | Retrospective cohort study | No | 2001–2018 | Choledochal cyst | X | 1/43 | X | X |
| Sakaguchi | 2019 | World journal of Paediatric Surgery | Japan | Retrospective cohort study | No | 1995–2004 | ARM | 3/39 | X | X | X |
| Sato | 1998 | Journal of Paediatric Surgery | Japan | Retrospective cohort study | No | 1970–1997 | Small intestinal atresia | X | 2/88 | X | 2/88 |
| Sola | 2018 | Paediatric Surgery International | USA | Retrospective cohort study | No | 1999–2016 | Hirschsprung’s disease | X | 4/100 | X | X |
| Yang | 2019 | Medicine | China | Retrospective cohort study | Yes | 2013–2016 | Small intestinal atresia | X | 2/42 | X | 3/42 |
| H. Zhu | 2019 | Journal of Paediatric Surgery | China | Retrospective cohort study | Yes | 2008–2017 | Small intestinal atresia | X | 4/39 | X | 3/39 |
| H. Zhu | 2019 | Paediatric Surgery International | China | Retrospective cohort study | Yes | 2003–2017 | Malrotation | X | 10/252 | X | X |
| T. Zhu | 2019 | International Journal of Colorectal Disease | China | Retrospective cohort study | Yes | 2010–2015 | Hirschsprung’s disease | X | X | X | 0/157 |
Risk of bias was assessed and is shown in Table 2. Most studies included reported fair quality on the NOS which was also the case for the two RCTs using the Jadad score. The mean scores on the NOS of articles describing paralytic ileus and early anastomotic stenosis was slightly lower (5, 5) compared to articles describing adhesive small bowel obstruction and late onset anastomotic stenosis [6].
Assessment risk of bias.
| Author | Year | Jadad |
New Ottawa scale (NOS) | |||
|---|---|---|---|---|---|---|
| Score | Selection | Comparability | Outcome | Total | ||
| (0–5) | (0–4*) | (0–2*) | (0–3*) | (0–9) | ||
| Stollman | 2008 | *** | * | *** | 7 | |
| Guo | 2010 | *** | * | ** | 6 | |
| Walter-Nicolet | 2009 | *** | ** | *** | 8 | |
| Wang | 2013 | *** | * | *** | 7 | |
| Lee | 2012 | *** | * | ** | 6 | |
| Cox | 2005 | *** | – | *** | 6 | |
| Festen | 2002 | ** | ** | ** | 6 | |
| Escobar | 2005 | *** | – | *** | 6 | |
| Yan | 2017 | *** | ** | *** | 8 | |
| Mirshemirani | 2007 | *** | – | *** | 6 | |
| Dariel | 2015 | *** | * | *** | 7 | |
| Mendez-Martinez | 2016 | *** | * | ** | 6 | |
| Fredriksson | 2015 | *** | – | *** | 6 | |
| Werbeck | 2010 | ** | – | ** | 4 | |
| Demirogullari | 2011 | ** | – | ** | 4 | |
| Rouzrokh | 2010 | *** | * | *** | 7 | |
| S. Li | 2017 | ** | * | *** | 6 | |
| Ghosh | 2016 | ** | * | *** | 6 | |
| Chen | 2014 | *** | ** | *** | 8 | |
| Bianchi | 1998 | *** | – | *** | 6 | |
| Mattioli | 1998 | ** | – | ** | 4 | |
| Teitelbaum | 1998 | ** | – | *** | 5 | |
| Demirbilek | 1999 | *** | – | *** | 6 | |
| Santos | 1999 | *** | – | *** | 6 | |
| de la Torre | 2000 | *** | – | *** | 6 | |
| Fleet | 2000 | ** | * | *** | 6 | |
| Hay | 2000 | *** | – | *** | 6 | |
| Langer | 2000 | *** | * | ** | 6 | |
| Patwardhan | 2001 | *** | * | ** | 6 | |
| Snyder | 2001 | *** | ** | ** | 7 | |
| Höllwarth | 2002 | *** | – | *** | 6 | |
| Saxena | 2001 | *** | * | *** | 7 | |
| Önen | 2003 | *** | – | ** | 5 | |
| Shah | 2003 | ** | – | *** | 5 | |
| Weidner | 2003 | ** | ** | ** | 6 | |
| Escobar | 2004 | *** | * | ** | 6 | |
| Kubota | 2004 | ** | * | ** | 5 | |
| Wester | 2004 | *** | – | ** | 5 | |
| Majid | 2015 | *** | ** | *** | 8 | |
| Sauer | 2005 | ** | ** | ** | 6 | |
| Thepcharoennirund | 2005 | ** | – | ** | 4 | |
| Chiu | 2006 | *** | * | ** | 6 | |
| Choudhry | 2006 | *** | – | *** | 6 | |
| Lee | 2006 | ** | * | *** | 6 | |
| A. Li | 2006 | *** | * | *** | 7 | |
| Liem | 2006 | ** | – | ** | 4 | |
| Maksoud-Filho | 2006 | *** | – | ** | 5 | |
| Owen | 2006 | ** | ** | ** | 6 | |
| Banieghbal | 2007 | ** | – | *** | 5 | |
| Dutta | 2007 | ** | – | ** | 4 | |
| Menon | 2007 | ** | – | *** | 5 | |
| Riehle | 2007 | *** | – | ** | 5 | |
| Stringer | 2007 | *** | * | ** | 6 | |
| Baglaj | 2007 | ** | * | ** | 5 | |
| Henrich | 2007 | *** | – | * | 4 | |
| Ishikawa | 2008 | *** | – | ** | 5 | |
| Shinall | 2008 | *** | ** | ** | 7 | |
| Spilde | 2008 | *** | * | ** | 6 | |
| Tongsin | 2008 | *** | * | ** | 6 | |
| van Eijck | 2008 | *** | – | ** | 5 | |
| Zheng | 2008 | *** | – | *** | 6 | |
| Dassinger | 2009 | *** | – | ** | 5 | |
| Ferreira | 2009 | ** | – | ** | 4 | |
| Gourlay | 2008 | *** | – | *** | 6 | |
| Hua | 2009 | *** | * | *** | 7 | |
| Liu | 2009 | *** | * | *** | 7 | |
| Obermayr | 2008 | *** | * | *** | 7 | |
| Takahashi | 2009 | ** | – | *** | 5 | |
| Gunnarsdottir | 2009 | *** | ** | *** | 8 | |
| Hong | 2010 | ** | * | ** | 5 | |
| Payne | 2010 | **** | * | *** | 8 | |
| Vu | 2010 | *** | * | *** | 7 | |
| de Vos | 2011 | *** | – | *** | 6 | |
| Hill | 2011 | *** | – | ** | 5 | |
| Karimi | 2011 | *** | – | ** | 5 | |
| Kozlov | 2010 | *** | ** | ** | 7 | |
| Travassos | 2011 | *** | ** | *** | 8 | |
| van der Zee | 2011 | *** | – | *** | 6 | |
| Li | 2012 | *** | – | ** | 5 | |
| Liem | 2012 | ** | * | ** | 5 | |
| Romao | 2012 | ** | * | *** | 6 | |
| Sato | 2012 | *** | * | ** | 6 | |
| Weil | 2011 | *** | * | *** | 7 | |
| Ghaffarpour | 2013 | *** | * | ** | 6 | |
| Ferreira | 2013 | *** | – | *** | 6 | |
| Jensen | 2013 | *** | ** | ** | 7 | |
| Nam | 2013 | *** | ** | *** | 8 | |
| Nio | 2013 | 2 | – | – | – | – |
| van der Zee | 2013 | ** | – | *** | 5 | |
| Diao | 2014 | ** | * | *** | 6 | |
| Elder | 2014 | *** | – | *** | 6 | |
| Friedmacher | 2014 | *** | ** | *** | 8 | |
| Ming | 2014 | *** | * | *** | 7 | |
| Nasr | 2014 | *** | * | *** | 7 | |
| Shrestha | 2014 | *** | – | *** | 6 | |
| Sulkowski | 2014 | *** | ** | *** | 8 | |
| Yang | 2014 | ** | – | ** | 4 | |
| Madadi-Sanjani | 2015 | *** | ** | ** | 7 | |
| Martinez-Criado | 2015 | *** | ** | ** | 7 | |
| Miyano | 2015 | *** | – | *** | 6 | |
| Shangjie | 2014 | *** | * | ** | 6 | |
| Almosallam | 2016 | *** | – | ** | 5 | |
| Diao | 2016 | ** | – | *** | 5 | |
| Guerra | 2016 | *** | * | ** | 6 | |
| Inoue | 2016 | ** | – | *** | 5 | |
| Matsumoto | 2016 | *** | * | ** | 6 | |
| Raitio | 2016 | *** | – | *** | 6 | |
| Diao | 2017 | ** | – | ** | 4 | |
| Dingemann | 2017 | *** | * | *** | 7 | |
| C. Lu | 2017 | *** | – | *** | 6 | |
| Y. Lu | 2017 | *** | * | *** | 7 | |
| Oh | 2017 | *** | ** | ** | 7 | |
| Risby | 2017 | *** | – | ** | 5 | |
| Son | 2017 | *** | ** | ** | 7 | |
| Tyson | 2017 | *** | * | ** | 6 | |
| van den Eijnden | 2017 | *** | * | *** | 7 | |
| Zani | 2017 | *** | * | *** | 7 | |
| Zmora | 2016 | *** | – | ** | 5 | |
| Avci | 2018 | *** | * | ** | 6 | |
| Peng | 2018 | *** | * | ** | 6 | |
| Xiao | 2018 | 3 | – | – | – | – |
| Zhang | 2018 | ** | * | *** | 6 | |
| England | 2012 | *** | – | *** | 6 | |
| Wakhlu | 2000 | *** | – | ** | 5 | |
| Pratap | 2007 | *** | – | *** | 6 | |
| Abbas | 2016 | *** | * | *** | 7 | |
| Chan | 2019 | ** | * | ** | 5 | |
| de Bie | 2019 | ** | * | *** | 6 | |
| Dewberry | 2019 | *** | ** | ** | 7 | |
| Dübbers | 2002 | *** | – | ** | 5 | |
| Gabler | 2018 | *** | – | ** | 5 | |
| Gao | 2019 | ** | – | ** | 4 | |
| He | 2016 | **** | * | *** | 8 | |
| Joda | 2019 | *** | ** | *** | 8 | |
| Jona | 2001 | ** | – | ** | 4 | |
| Long | 2019 | *** | ** | *** | 8 | |
| Marei | 2019 | ** | * | *** | 6 | |
| Narang | 2019 | ** | * | *** | 6 | |
| Jung | 1995 | ** | – | * | 3 | |
| Ren | 2018 | ** | * | ** | 5 | |
| Ryu | 2019 | *** | * | ** | 6 | |
| Sakaguchi | 2019 | *** | * | ** | 6 | |
| Sato | 1998 | *** | – | ** | 5 | |
| Sola | 2018 | *** | * | ** | 6 | |
| Yang | 2019 | *** | * | ** | 6 | |
| H. Zhu | 2019 | ** | ** | *** | 7 | |
| T. Zhu | 2019 | *** | * | ** | 6 | |
Paralytic ileus
In total, 22 studies reported on paralytic ileus and entailed 1,332 patients and 120 events of paralytic ileus [35, 42, 46, 48, 49, 51, 61, 65, 81, 82, 96, 98, 100, 103, 109, 112, 114, 115, 132, 151, 153, 155]. The pooled proportion of total paralytic ileus was 0.07 (95%-CI: 0.05–0.11; I 2=71%, p≤0.01).
Separate pooled proportions were calculated for the following conditions: Hirschsprung’s disease 0.07 (95%-CI: 0.02–0.24; n=45/426; I 2=91%; p≤0.01); small intestinal atresia 0.05 (95%-CI: 0.03–0.09; n=16/314; I 2=18%; p=0.25); gastroschisis 0.14 (95%-CI: 0.08–0.23; n=30/228; I 2=52%; p=0.03); biliary atresia 0.05 (95%-CI: 0.02–0.11; n=5/103; I 2=0%; p=0.45); omphalocele 0.05 (95%-CI: 0.02–0.13; n=5/96; I 2=8%; p=0.27); anorectal malformations 0.06 (95%-CI: 0.03–0.15; n=5/77; I 2=0%; p=0.83). Duodenal obstruction (n=58) and congenital diaphragmatic hernia (n=30) are included in the overall proportion but did not meet the criteria for separate statistical analysis (Figure 2).
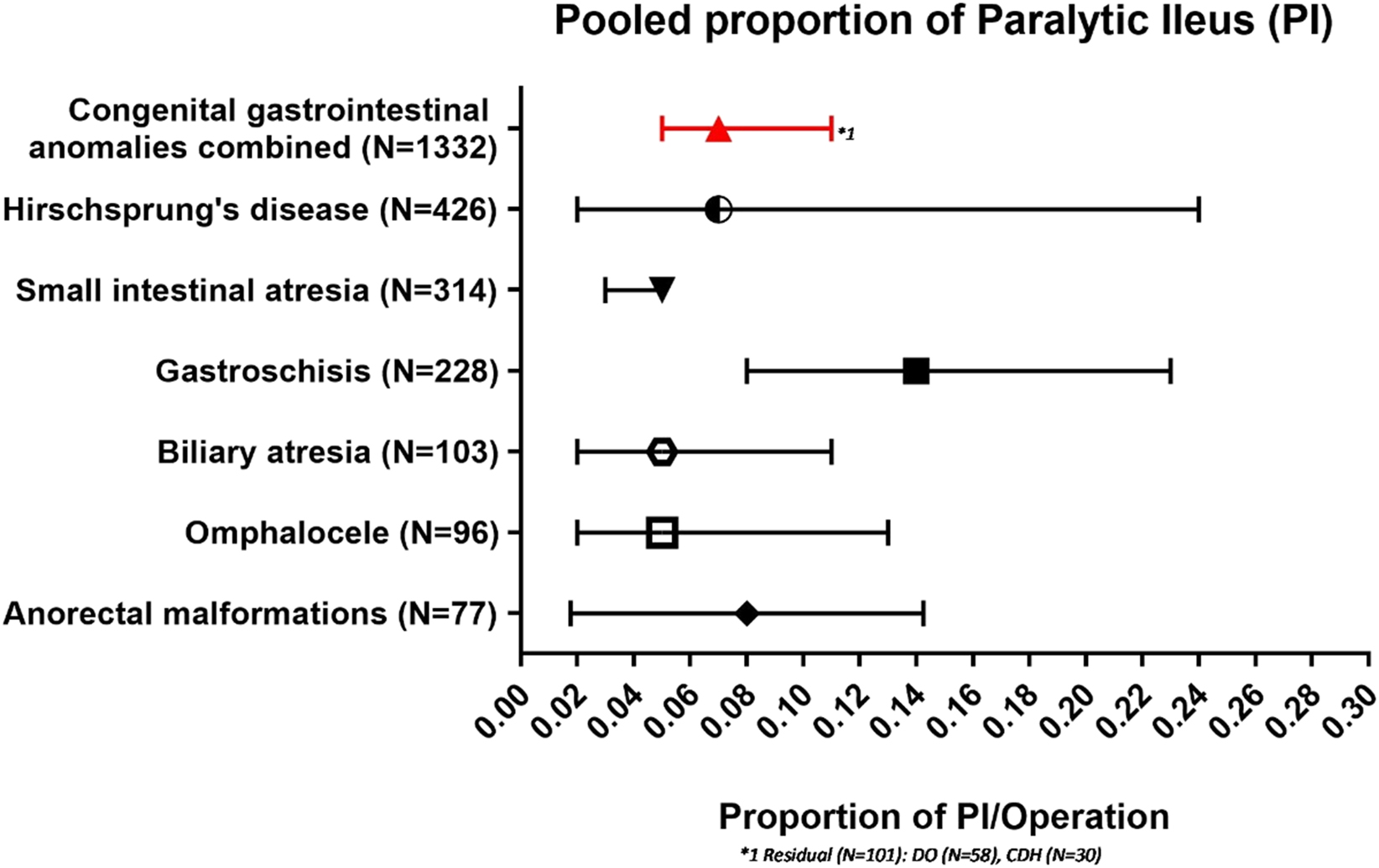
Pooled proportion of paralytic ileus.
Adhesive small bowel obstruction (SBO)
In total, 99 studies reported on small bowel obstruction entailing 8,470 patients and 572 events of SBO all anomalies combined [10, 11, 14], [15], [16], [17], [18], [19, 21, 24, 26, 29], [30], [31, 33, 34, 37], [38], [39], [40], [41, 43, 45, 47, 49, 51], [52], [53], [54, 56], [57], [58], [59], [60, 62, 63, 67, 70], [71], [72], [73], [74, 79], [80], [81, 85], [86], [87], [88], [89, 92], [93], [94, 96, 97, 99], [100], [101, 103, 105, 106, 109], [110], [111, 113, 115], [116], [117], [118], [119], [120], [121, 123], [124], [125], [126, 128, 131, 132, 134, 136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150, 152, 154, 156], [157], [158], [159], [160]. Length of follow up was at least half a year in 56 (57%) of the studies.
The pooled proportion of total SBO was 0.06 (95%-CI: 0.05–0.07; I 2=74%, p≤0.01). Separate proportions were calculated for the following conditions: Hirschsprung’s disease 0.05 (95%-CI: 0.03–0.07; n=174/3,044; I 2=77%; p≤0.01); gastroschisis 0.09 (95%-CI: 0.06–0.14; n=130/1,147; I 2=75%; p≤0.01); congenital diaphragmatic hernia 0.08 (95%-CI: 0.06–0.11; n=60/736; I 2=35%; p=0.09); duodenal obstruction 0.04 (95%-CI: 0.02–0.08; n=28/728; I 2=61%; p=0.01); small intestinal atresia 0.09 (95%-CI: 0.05–0.14; n=60/690; I 2=74%; p≤0.01); biliary atresia 0.03 (95%-CI: 0.02–0.05; n=19/543; I 2=0%; p=0.48); malrotation 0.11 (95%-CI: 0.06–0.19; n=46/492; I 2=73%; p≤0.01); anorectal malformations 0.03 (95%-CI: 0.02–0.06; n=17/476; I 2=37%; p=0.54); omphalocele 0.04 (95%-CI: 0.02–0.24; n=21/357; I 2=51%; p=0.31); choledochal cyst 0.03 (95%-CI: 0.01–0.08; n=5/143; I 2=0%; p=0.48). Meconium ileus (n=54), Meckel’s diverticula (n=46) and colonic atresia (n=14) are included in the overall proportion but did not meet the criteria for separate statistical analysis (Figure 3).
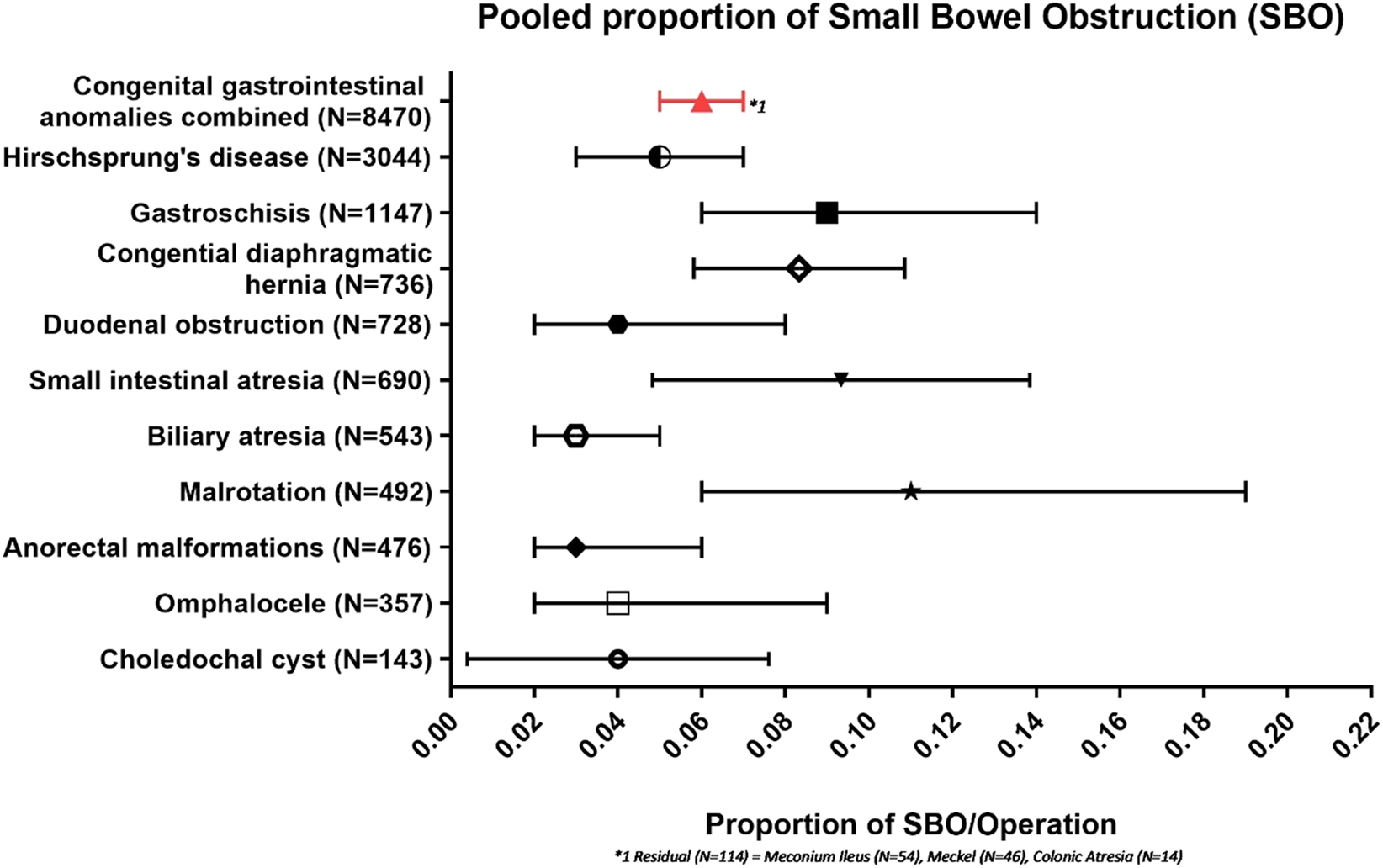
Pooled proportion of small bowel obstruction.
Anastomotic stenosis
Of the 14 studies reporting on anastomotic stenosis within one month of follow-up, 365 patients were included and 22 events of anastomotic stenosis occurred [13, 18, 20, 35, 57, 59, 64, 75, 78, 108, 109, 118, 129, 151].
The pooled proportion of total anastomotic stenosis within a month was 0.03 (95%-CI: 0.01–0.10; I 2=81%, p=0.02). Diseases reported on were: small intestinal atresia (n=8/163), Hirschsprung’s disease (n=10/60), duodenal obstruction (n=2/56), anorectal malformations (n=0/30), choledochal cyst (n=0/30) and colonic atresia (n=2/26).
In total, 40 studies reported on anastomotic stenosis after one month of follow-up entailing 4,468 patients and 214 events of anastomotic stenosis occurred [12, 18, 22, 23, 25, 32], [33], [34], [35], [36, 38, 40, 44, 49, 55, 62, 66, 68, 73, 75], [76], [77], [78, 81, 83, 84, 95, 99, 102, 104, 105, 107, 109, 111, 113, 115, 116, 119, 120, 122, 129, 130, 132], [133], [134], [135, 142, 156, 158, 159, 161]. Length of follow up was at least half a year in 29 (73%) of the studies.
The pooled proportion of anastomotic stenosis was 0.04 (95%-CI: 0.03–0.06; I 2=59%, p=0.30). Separate proportions were calculated for the following conditions: Hirschsprung’s disease 0.04 (95%-CI: 0.03–0.07; n=162/3,238; I 2=70%; p=0.11); small intestinal atresia 0.06 (95%-CI: 0.04–0.08; n=32/548; I 2=0%; p=0.77); duodenal obstruction 0.02 (95%-CI: 0.01–0.04; n=11/547; I 2=42%; p=0.29); gastroschisis 0.08 (95%-CI: 0.04–0.14; n=9/118; I 2=0%; p=0.77). Colonic atresia (n=17) is included in the overall proportion but did not meet the criteria for separate statistical analysis (Figure 4).
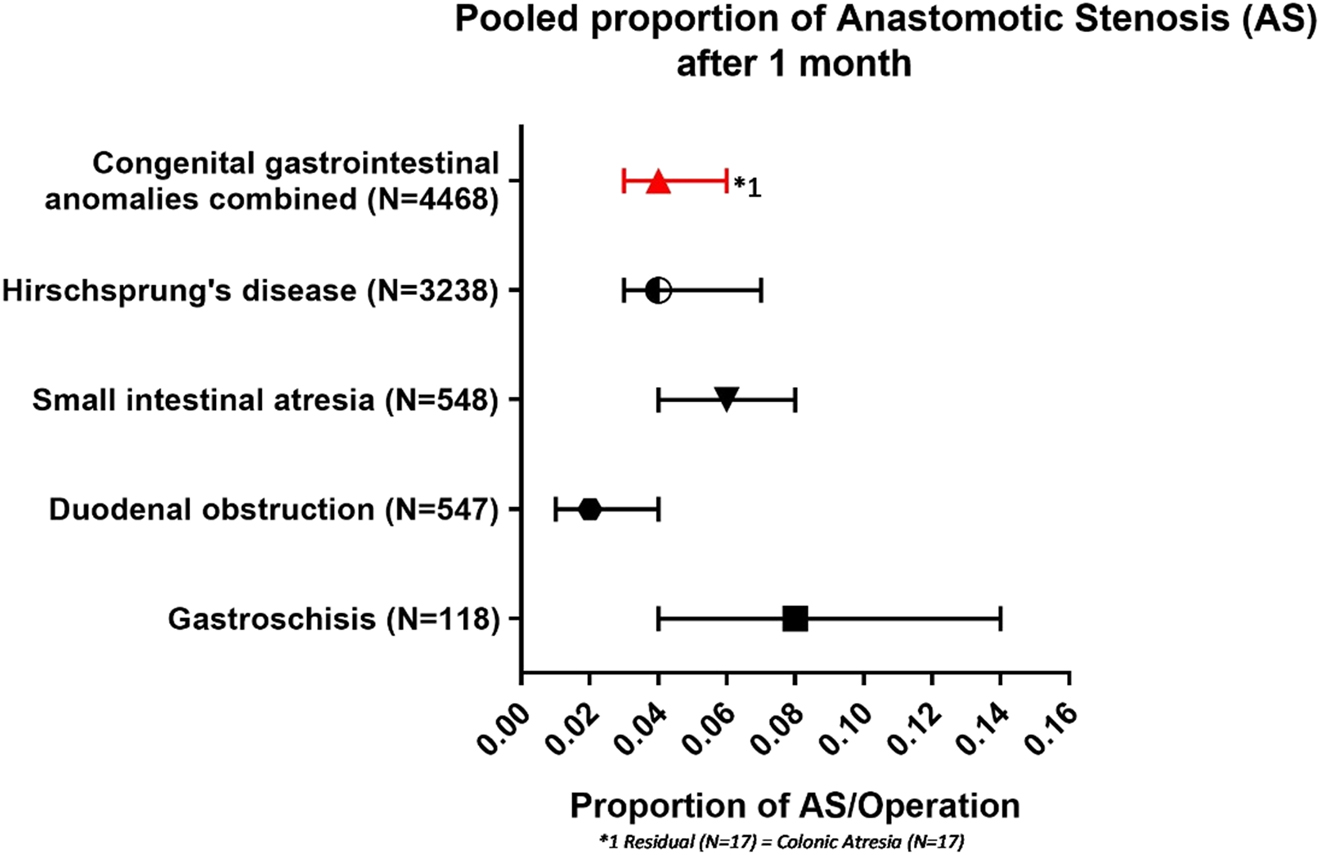
Pooled proportion of anastomotic stenosis after 1 month.
Discussion
This systematic review pooled the reported proportions on different types of ileus following abdominal surgery for birth defects in infants. These proportions can be seen as an approximation of the incidences of these complications. According to our reported approximation, these incidences were 7% for paralytic ileus, 6% for adhesive small bowel obstruction, 3% for anastomotic stenosis within one month after surgery and 4% after one month. Within the different birth defects there is a large variation in the occurrence and the spread of these forms of ileus. Although risk factor identification is beyond the scope of this review, the available literature gives some suggestions why these diseases seem to be more at risk.
Out of all diseases paralytic ileus was most common in gastroschisis patients (14%). In these patients, a defect of the abdominal wall leads to extrusion of abdominal content antenatally. Postnatally, this content is reduced intra-abdominally either by primary closure or temporally use of silo and delayed closure. During both procedures the intestine is manipulated severely, which is known to increase the incidence and duration of paralytic ileus in adults [4].
Adhesions, which cause SBO, have long been accepted as a partly inevitable consequence of surgery. They occur as part of the natural healing process. It is hard to define the clinical significance of adhesions, since most are asymptomatic, but when they lead to small bowel obstruction, they can be fatal with mortality rates in children between 2 and 15% [121, 162, 163]. Recently duration of surgery and staged procedures have been identified as risk factors for SBO [37, 162, 164].
Our reported pooled incidence of 6% is comparable to most recent large (n≥100) individual cohort studies reporting on abdominal surgery in infants. These studies report an incidence of SBO between 6 and 10% [37, 165]. It is important to acknowledge that this review entails an aggregated incidence for birth defects only. Acquired diseases such as necrotizing enterocolitis, which seems to be at high risk with a reported incidence of SBO between 25 and 64%, are therefore not included [37, 162].
We found that patients with a malrotation, small intestinal atresia or gastroschisis were relatively most at risk of SBO. This is in concordance with previous studies [37, 121, 162], [163], [164], [165].
We divided anastomotic stenosis into two groups based on reported occurrence within or after one month of surgery since early onset is suggested to be caused by technical error or tissue oedema, whereas a delayed onset and stricture formation is related to chronic inflammation in time leading to anastomotic scarring [166].
Early onset of an anastomotic stenosis is not widely reported and might even be overlooked in the infantile cohort. This review shows that early stenosis does occur and should be considered when conducting research into post-operative complications in the infantile cohort. Technical factors, such as suture reportion speed or mode of suturing, of influence during anastomotic creation should be evaluated to identify risk factors.
Gastroschisis, and to a smaller extent intestinal atresias, were most at risk for late onset anastomotic stenosis. The process of anastomotic healing is to a great extent unclear. Most research has focussed on surgical innovations and techniques without the results leading to a conclusive resolution. Future research in the pathobiology at the cellular level might bring clarification on this matter [166].
This study has its limitations. Because of the variety in study designs and reported outcomes we were not able to look into risk factors which could have lowered heterogeneity. Although it must be noted that, by stratifying for birth defect, some outcomes had moderate to low heterogeneity. Another limitation was that because certain birth defects such as gastroschisis only occur in neonates, our stratification might have resulted in differences in mean age when comparing birth defects. This age difference could be an important reason why certain birth defects are more at risk of certain form of ileus. However, it is not the aim of this review to compare different birth defects but rather report an incidence for each individually. Thus, we believe that this age difference will not hinder the message of our review. If we had only included neonates in this review important birth defects, such as Hirschsprung’s disease, diagnosed beyond the neonatal period would have been excluded. Furthermore, it has to be stated that our results are based on retrospective cohorts available in the literature most of which did not have ileus as a primary outcome. This has undoubtedly increased the chances of occurrence of forms of bias such as selection, publication and reporting bias. Our risk of bias assessment showed most articles to have only fair quality mostly caused by the retrospective, observational nature of most included studies. Moreover, most studies did not have a strict definition of complications possibly resulting in observer bias. Lastly, only 57% of the included articles had a follow-up of at least half a year. Many other articles were unclear about the length of follow up. This lack of long-term follow-up might result in an underestimate of the real incidence of SBO and anastomotic stenosis. SBOs, for instance mostly arise within a year after surgery however episodes are reported 28 years after the initial laparotomy [17, 37, 121, 162], [163], [164], [165]. Although these limitations might have influenced the pooled analyses, at this moment the presented data is the best available approximation of these complications in this cohort.
Conclusion
This review is the first to aggregate the known literature in order to approximate the incidence of different forms of ileus for each abdominal birth defect. We showed these complications are common and the distribution differs between birth defects. Knowing which birth defects are most at risk might aid clinicians in taking prompt action when an ileus is suspected. Future research should focus on the identification of risk factors and preventative measures. The incidences provided by this review can be used as a starting point for sample size calculations.
Acknowledgments
We would like to thank Shaffy Roell for the support with the development of the illustrations.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Not applicable.
-
Ethical approval: Not applicable.
References
1. Catania, VD, Lauriti, G, Pierro, A, Zani, A. Open versus laparoscopic approach for intestinal malrotation in infants and children: a systematic review and meta-analysis. Pediatr Surg Int 2016;32:1157–64. https://doi.org/10.1007/s00383-016-3974-2.Search in Google Scholar
2. Schneuer, FJ, Adams, SE, Bentley, JP, Holland, AJ, Huckel Schneider, C, White, L, et al.. A population-based comparison of the post-operative outcomes of open and laparoscopic appendicectomy in children. Med J Aust 2018;209:80–5. https://doi.org/10.5694/mja17.00541.Search in Google Scholar
3. Langer, JC, Rollins, MD, Levitt, M, Gosain, A, Torre, L, Kapur, RP, et al.. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int 2017;33:523–6. https://doi.org/10.1007/s00383-017-4066-7.Search in Google Scholar
4. Bragg, D, El-Sharkawy, AM, Psaltis, E, Maxwell-Armstrong, CA, Lobo, DN. Postoperative ileus: recent developments in pathophysiology and management. Clin Nutr 2015;34:367–76. https://doi.org/10.1016/j.clnu.2015.01.016.Search in Google Scholar
5. Venara, A, Neunlist, M, Slim, K, Barbieux, J, Colas, PA, Hamy, A, et al.. Postoperative ileus: pathophysiology, incidence, and prevention. J Visc Surg 2016;153:439–46. https://doi.org/10.1016/j.jviscsurg.2016.08.010.Search in Google Scholar
6. Shamseer, L, Moher, D, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al.. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. https://doi.org/10.1136/bmj.g7647.Search in Google Scholar
7. Wells, GA, Shea, B, Higgins, JP, Sterne, J, Tugwell, P, Reeves, BC. Checklists of methodological issues for review authors to consider when including non-randomized studies in systematic reviews. Res Synth Methods 2013;4:63–77. https://doi.org/10.1002/jrsm.1077.Search in Google Scholar
8. Jadad, AR, Moore, RA, Carroll, D, Jenkinson, C, Reynolds, DJ, Gavaghan, DJ, et al.. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Contr Clin Trials 1996;17:1–12. https://doi.org/10.1016/0197-2456(95)00134-4.Search in Google Scholar
9. Higgins, JPT, Thompson, SG, Deeks, JJ, Altman, DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.Search in Google Scholar PubMed PubMed Central
10. Almosallam, OI, Aseeri, A, Shanafey, SA. Outcome of loop versus divided colostomy in the management of anorectal malformations. Ann Saudi Med 2016;36:352–5. https://doi.org/10.5144/0256-4947.2016.352.Search in Google Scholar PubMed PubMed Central
11. Avci, V, Bilici, S, Düz, E, Beger, B, Değer, İ. Congenital duodenal obstruction: ten-year results of a tertiary center. E J Med 2018;23:191–4. https://doi.org/10.5505/ejm.2018.04909.Search in Google Scholar
12. Baglaj, M, Carachi, R, Lawther, S. Multiple atresia of the small intestine: a 20-year review. Eur J Pediatr Surg 2008;18:13–8. https://doi.org/10.1055/s-2007-965771.Search in Google Scholar
13. Banieghbal, B, Beale, PG. Minimal access approach to jejunal atresia. J Pediatr Surg 2007;42:1362–4. https://doi.org/10.1016/j.jpedsurg.2007.03.034.Search in Google Scholar
14. Bianchi, A. One-stage neonatal reconstruction without stoma for Hirschsprung’s disease. Semin Pediatr Surg 1998;7:170–3. https://doi.org/10.1016/s1055-8586(98)70013-7.Search in Google Scholar
15. Chen, QJ, Gao, ZG, Tou, JF, Qian, YZ, Li, MJ, Xiong, QX, et al.. Congenital duodenal obstruction in neonates: a decade’s experience from one center. World J Pediatr 2014;10:238–44. https://doi.org/10.1007/s12519-014-0499-4.Search in Google Scholar PubMed
16. Chiu, B, Lopoo, J, Hoover, JD, Almond, PS, Arensman, R, Madonna, MB. Closing arguments for gastroschisis: management with silo reduction. J Perinat Med 2006;34:243–5. https://doi.org/10.1515/JPM.2006.043.Search in Google Scholar PubMed
17. Choudhry, MS, Grant, HW. Small bowel obstruction due to adhesions following neonatal laparotomy. Pediatr Surg Int 2006;22:729–32. https://doi.org/10.1007/s00383-006-1719-3.Search in Google Scholar PubMed
18. Cox, SG, Numanoglu, A, Millar, AJ, Rode, H. Colonic atresia: spectrum of presentation and pitfalls in management. A review of 14 cases. Pediatr Surg Int 2005;21:813–8. https://doi.org/10.1007/s00383-005-1488-4.Search in Google Scholar PubMed
19. Dariel, A, Poocharoen, W, Silva, N, Pleasants, H, Gerstle, J. Secondary plastic closure of gastroschisis is associated with a lower incidence of mechanical ventilation. Eur J Pediatr Surg 2014;25. https://doi.org/10.1055/s-0034-1395487.Search in Google Scholar PubMed
20. Dassinger, M, Jackson, R, Smith, S. Management of colonic atresia with primary resection and anastomosis. Pediatr Surg Int 2009;25:579–82. https://doi.org/10.1007/s00383-009-2401-3.Search in Google Scholar PubMed
21. De la Torre, L, Ortega, A. Transanal versus open endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg 2000;35:1630–2. https://doi.org/10.1053/jpsu.2000.18338.Search in Google Scholar PubMed
22. De Vos, C, Arnold, M, Sidler, D, Moore, SW. A comparison of laparoscopic-assisted (LAARP) and posterior sagittal (PSARP) anorectoplasty in the outcome of intermediate and high anorectal malformations. S Afr J Surg 2011;49:39–43.Search in Google Scholar
23. Demirbilek, S, Atayurt, HF. Anal transposition without colostomy: functional results and complications. Pediatr Surg Int 1999;15:221–3. https://doi.org/10.1007/s003830050560.Search in Google Scholar PubMed
24. Demirogullari, B, Yilmaz, Y, Yildiz, G, Ozen, İ, Karabulut, R, Turkyilmaz, Z, et al.. Ostomy complicatIons in patients with anorectal malformations. Pediatr Surg Int 2011;27:1075–8. https://doi.org/10.1007/s00383-011-2955-8.Search in Google Scholar PubMed
25. Diao, M, Li, L, Guan, KP, Zhang, Z, Cheng, W. A novel laparoscopic technique for anorectal malformation with low recto-bulbar fistulae. Surg Endosc 2017;31:4326–30. https://doi.org/10.1007/s00464-017-5483-3.Search in Google Scholar PubMed
26. Diao, M, Li, L, Li, Q, Ye, M, Cheng, W. Challenges and strategies for single-incision laparoscopic Roux-en-Y hepaticojejunostomy in managing giant choledochal cysts. Int J Surg 2014;12:412–7. https://doi.org/10.1016/j.ijsu.2014.03.007.Search in Google Scholar PubMed
27. Diao, M, Li, L, Ye, M, Cheng, W. Single-incision laparoscopic-assisted anorectoplasty using conventional instruments for children with anorectal malformations and rectourethral or rectovesical fistula. J Pediatr Surg 2014;49:1689–94. https://doi.org/10.1016/j.jpedsurg.2014.08.010.Search in Google Scholar PubMed
28. Diao, M, Li, L, Ye, M, Guan, KP, Wei, YD, Cheng, W. Congenital anomaly rectified at birth: one-stage single-incision laparoscopic-assisted anorectoplasty for newborns with anorectal malformations and recto-urethral fistula. Surg Endosc 2016;30:5156–64. https://doi.org/10.1007/s00464-016-4841-x.Search in Google Scholar PubMed
29. Dingemann, C, Dietrich, J, Zeidler, J, Blaser, J, Gosemann, JH, Lacher, M, et al.. Surgical management of congenital abdominal wall defects in Germany: a population-based study and comparison with literature reports. Eur J Pediatr Surg 2017;27:516–25. https://doi.org/10.1055/s-0037-1598250.Search in Google Scholar PubMed
30. Dutta, S, Woo, R, Albanese, CT. Minimal access portoenterostomy: advantages and disadvantages of standard laparoscopic and robotic techniques. J Laparoendosc Adv Surg Tech A 2007;17:258–64. https://doi.org/10.1089/lap.2006.0112.Search in Google Scholar PubMed
31. Elder, CT, Metzger, R, Arrington, C, Rollins, M, Scaife, E. The role of screening and prophylactic surgery for malrotation in heterotaxy patients. J Pediatr Surg 2014;49:1746–8. https://doi.org/10.1016/j.jpedsurg.2014.09.007.Search in Google Scholar PubMed
32. England, RJ, Warren, SL, Bezuidenhout, L, Numanoglu, A, Millar, AJ. Laparoscopic repair of anorectal malformations at the red cross war Memorial Children’s Hospital: taking stock. J Pediatr Surg 2012;47:565–70. https://doi.org/10.1016/j.jpedsurg.2011.08.006.Search in Google Scholar PubMed
33. Escobar, MA, Grosfeld, JL, West, KW, Scherer, LR, Rouse, TM, Engum, SA, et al.. Long-term outcomes in total colonic aganglionosis: a 32-year experience. J Pediatr Surg 2005;40:955–61. https://doi.org/10.1016/j.jpedsurg.2005.03.043.Search in Google Scholar PubMed
34. Escobar, MA, Ladd, AP, Grosfeld, JL, West, KW, Rescorla, FJ, Scherer, LR3rd, et al.. Duodenal atresia and stenosis: long-term follow-up over 30 years. J Pediatr Surg 2004;39:867–71. https://doi.org/10.1016/j.jpedsurg.2004.02.025.Search in Google Scholar PubMed
35. Festen, S, Brevoord, JC, Goldhoorn, GA, Festen, C, Hazebroek, FW, van Heurn, LW, et al.. Excellent long-term outcome for survivors of apple peel atresia. J Pediatr Surg 2002;37:61–5. https://doi.org/10.1053/jpsu.2002.29428.Search in Google Scholar PubMed
36. Fleet, MS, de la Hunt, MN. Intestinal atresia with gastroschisis: a selective approach to management. J Pediatr Surg 2000;35:1323–5. https://doi.org/10.1053/jpsu.2000.9324.Search in Google Scholar PubMed
37. Fredriksson, F, Christofferson, RH, Lilja, HE. Adhesive small bowel obstruction after laparotomy during infancy. Br J Surg 2016;103:284–9. https://doi.org/10.1002/bjs.10072.Search in Google Scholar PubMed
38. Friedmacher, F, Hock, A, Castellani, C, Avian, A, Hollwarth, ME. Gastroschisis-related complications requiring further surgical interventions. Pediatr Surg Int 2014;30:615–20. https://doi.org/10.1007/s00383-014-3500-3.Search in Google Scholar PubMed
39. Ghaffarpour, N, Svensson, PJ, Svenningsson, A, Wester, T, Mesas Burgos, C. Supraumbilical incision with U-u umbilicoplasty for congenital duodenal atresia: the Stockholm experience. J Pediatr Surg 2013;48:1981–5. https://doi.org/10.1016/j.jpedsurg.2013.06.028.Search in Google Scholar PubMed
40. Ghosh, DN, Liu, Y, Cass, DT, Soundappan, SSV. Transition zone pull-through in Hirschsprung’s disease: a tertiary hospital experience. ANZ J Surg 2017;87:780–3. https://doi.org/10.1111/ans.13745.Search in Google Scholar PubMed
41. Gomes Ferreira, C, Kuhn, P, Lacreuse, I, Kasleas, C, Philippe, P, Podevin, G, et al.. Congenital diaphragmatic hernia: an evaluation of risk factors for failure of thoracoscopic primary repair in neonates. J Pediatr Surg 2013;48:488–95. https://doi.org/10.1016/j.jpedsurg.2012.09.060.Search in Google Scholar PubMed
42. Gomes Ferreira, C, Reinberg, O, Becmeur, F, Allal, H, De Lagausie, P, Lardy, H, et al.. Neonatal minimally invasive surgery for congenital diaphragmatic hernias: a multicenter study using thoracoscopy or laparoscopy. Surg Endosc 2009;23:1650–9. https://doi.org/10.1007/s00464-009-0334-5.Search in Google Scholar PubMed
43. Gourlay, DM, Cassidy, LD, Sato, TT, Lal, DR, Arca, MJ. Beyond feasibility: a comparison of newborns undergoing thoracoscopic and open repair of congenital diaphragmatic hernias. J Pediatr Surg 2009;44:1702–7. https://doi.org/10.1016/j.jpedsurg.2008.11.030.Search in Google Scholar PubMed
44. Guerra, J, Wayne, C, Musambe, T, Nasr, A. Laparoscopic-assisted transanal pull-through (LATP) versus complete transanal pull-through (CTP) in the surgical management of Hirschsprung’s disease. J Pediatr Surg 2016;51:770–4. https://doi.org/10.1016/j.jpedsurg.2016.02.020.Search in Google Scholar PubMed
45. Gunnarsdottir, A, Larsson, LT, Arnbjornsson, E. Transanal endorectal vs. Duhamel pull-through for Hirschsprung’s disease. Eur J Pediatr Surg 2010;20:242–6. https://doi.org/10.1055/s-0030-1252006.Search in Google Scholar PubMed
46. Guo, CB, Li, YC, Zhang, MM, Yan, LN, Pu, CL, Kang, Q, et al.. Early postoperative care of liver transplantation for infants with biliary atresia during pediatric intensive care unit stay. Transplant Proc 2010;42:1750–4. https://doi.org/10.1016/j.transproceed.2010.02.086.Search in Google Scholar PubMed
47. Hay, SA, Soliman, HE, Sherif, HM, Abdelrahman, AH, Kabesh, AA, Hamza, AF. Neonatal jaundice: the role of laparoscopy. J Pediatr Surg 2000;35:1706–9. https://doi.org/10.1053/jpsu.2000.19217.Search in Google Scholar PubMed
48. Henrich, K, Huemmer, HP, Reingruber, B, Weber, PG. Gastroschisis and omphalocele: treatments and long-term outcomes. Pediatr Surg Int 2008;24:167–73. https://doi.org/10.1007/s00383-007-2055-y.Search in Google Scholar PubMed
49. Hill, S, Koontz, CS, Langness, SM, Wulkan, ML. Laparoscopic versus open repair of congenital duodenal obstruction in infants. J Laparoendosc Adv Surg Tech A 2011;21:961–3. https://doi.org/10.1089/lap.2011.0069.Search in Google Scholar PubMed
50. Hollwarth, ME, Rivosecchi, M, Schleef, J, Deluggi, S, Fasching, G, Ceriati, E, et al.. The role of transanal endorectal pull-through in the treatment of Hirschsprung’s disease – a multicenter experience. Pediatr Surg Int 2002;18:344–8. https://doi.org/10.1007/s00383-002-0747-x.Search in Google Scholar PubMed
51. Hong, L, Wu, YM, Yan, ZL, Chen, S, Wang, J. Modified silo technique–an easy and effective method to improve the survival rate of neonates with gastroschisis in Shanghai. Eur J Obstet Gynecol Reprod Biol 2010;148:31–4. https://doi.org/10.1016/j.ejogrb.2009.09.022.Search in Google Scholar PubMed
52. Hua, MC, Chao, HC, Lien, R, Lai, JY, Lai, MW, Kong, MS. The different clinical and liver pathological characteristics between the newborns and infants with choledochal cysts. Chang Gung Med J 2009;32:198–203.Search in Google Scholar
53. Inoue, M, Uchida, K, Otake, K, Nagano, Y, Mori, K, Hashimoto, K, et al.. Thoracoscopic repair of congenital diaphragmatic hernia with countermeasures against reported complications for safe outcomes comparable to laparotomy. Surg Endosc 2016;30:1014–9. https://doi.org/10.1007/s00464-015-4287-6.Search in Google Scholar PubMed
54. Ishikawa, N, Kubota, A, Kawahara, H, Hasegawa, T, Okuyama, H, Uehara, S, et al.. Transanal mucosectomy for endorectal pull-through in Hirschsprung’s disease: comparison of abdominal, extraanal and transanal approaches. Pediatr Surg Int 2008;24:1127–9. https://doi.org/10.1007/s00383-008-2231-8.Search in Google Scholar PubMed
55. Jensen, AR, Short, SS, Anselmo, DM, Torres, MB, Frykman, PK, Shin, CE, et al.. Laparoscopic versus open treatment of congenital duodenal obstruction: multicenter short-term outcomes analysis. J Laparoendosc Adv Surg Tech A 2013;23:876–80. https://doi.org/10.1089/lap.2013.0140.Search in Google Scholar PubMed PubMed Central
56. Karimi, A, Gorter, RR, Sleeboom, C, Kneepkens, CM, Heij, HA. Issues in the management of simple and complex meconium ileus. Pediatr Surg Int 2011;27:963–8. https://doi.org/10.1007/s00383-011-2906-4.Search in Google Scholar PubMed PubMed Central
57. Kozlov, Y, Novogilov, V, Yurkov, P, Podkamenev, A, Weber, I, Sirkin, N. Keyhole approach for repair of congenital duodenal obstruction. Eur J Pediatr Surg 2011;21:124–7. https://doi.org/10.1055/s-0030-1268455.Search in Google Scholar PubMed
58. Kubota, A, Kawahara, H, Okuyama, H, Oue, T, Tazuke, Y, Okada, A. Clinical outcome of laparoscopically assisted endorectal pull-through in Hirschsprung’s disease: comparison of abdominal and perineal approaches. J Pediatr Surg 2004;39:1835–7. https://doi.org/10.1016/j.jpedsurg.2004.08.015.Search in Google Scholar PubMed
59. Langer, JC, Seifert, M, Minkes, RK. One-stage Soave pull-through for Hirschsprung’s disease: a comparison of the transanal and open approaches. J Pediatr Surg 2000;35:820–2. https://doi.org/10.1053/jpsu.2000.6849.Search in Google Scholar PubMed
60. Lee, SH, Cho, YH, Kim, HY, Park, JH, Byun, SY. Clinical experience of complex jejunal atresia. Pediatr Surg Int 2012;28:1079–83. https://doi.org/10.1007/s00383-012-3131-5.Search in Google Scholar PubMed
61. Lee, SL, Beyer, TD, Kim, SS, Waldhausen, JH, Healey, PJ, Sawin, RS, et al.. Initial nonoperative management and delayed closure for treatment of giant omphaloceles. J Pediatr Surg 2006;41:1846–9. https://doi.org/10.1016/j.jpedsurg.2006.06.011.Search in Google Scholar PubMed
62. Li, AW, Zhang, WT, Li, FH, Cui, XH, Duan, XS. A new modification of transanal Soave pull-through procedure for Hirschsprung’s disease. Chin Med J (Engl) 2006;119:37–42. https://doi.org/10.1097/00029330-200601010-00007.Search in Google Scholar
63. Li, B, Chen, WB, Wang, SQ, Liu, SL, Li, L. Laparoscopy-assisted surgery for neonatal intestinal atresia and stenosis: a report of 35 cases. Pediatr Surg Int 2012;28:1225–8. https://doi.org/10.1007/s00383-012-3216-1.Search in Google Scholar
64. Li, SX, Zhang, HW, Cao, H, Zou, HX, Yin, YY, Sui, F, et al.. Clinical effects of ascending colon patching ileorectal heart-shaped anastomosis on total colonic aganglionosis. Eur Rev Med Pharmacol Sci 2017;21(4 Suppl):90–4.Search in Google Scholar
65. Liem, NT, Hau, BD. Primary laparoscopic endorectal colon pull-through for Hirschsprung’s disease: early results of 61 cases. Asian J Surg 2006;29:173–5. https://doi.org/10.1016/s1015-9584(09)60081-6.Search in Google Scholar
66. Liem, NT, Quynh, TA. Laparoscopic rectal pull-through for persistent cloaca: an easier approach for a complex anomaly. J Pediatr Surg 2012;47:815–8. https://doi.org/10.1016/j.jpedsurg.2012.02.004.Search in Google Scholar PubMed
67. Liu, SL, Li, L, Cheng, W, Hou, WY, Huang, LM, Wang, WY, et al.. Laparoscopic hepatojejunostomy for biliary atresia. J Laparoendosc Adv Surg Tech A 2009;19(1 Suppl):S31–5. https://doi.org/10.1089/lap.2008.0119.supp.Search in Google Scholar PubMed
68. Lu, C, Hou, G, Liu, C, Geng, Q, Xu, X, Zhang, J, et al.. Single-stage transanal endorectal pull-through procedure for correction of Hirschsprung disease in neonates and nonneonates: a multicenter study. J Pediatr Surg 2017;52:1102–7. https://doi.org/10.1016/j.jpedsurg.2017.01.061.Search in Google Scholar PubMed
69. Lu, Y, Xia, Q, Yang, Y, Wan, P, Hou, J, Wang, Y, et al.. Effect of preoperative growth status on clinical outcomes after living-donor liver transplantation in infants. Transplant Proc 2017;49:1848–54. https://doi.org/10.1016/j.transproceed.2017.06.036.Search in Google Scholar PubMed
70. Madadi-Sanjani, O, Carl, N, Longerich, T, Petersen, C, Andruszkow, JH. Inguinal hernias represent the most frequent surgical complication after Kasai in biliary atresia infants. BioMed Res Int 2015;2015:383791. https://doi.org/10.1155/2015/383791.Search in Google Scholar PubMed PubMed Central
71. Majid, F, Sheikh, AH, Ramzan, M, Siddique, M. Duodenal obstruction in neonates: management and outcome. Pak Paediatr J 2015;39:93–7.Search in Google Scholar
72. Maksoud-Filho, JG, Tannuri, U, da Silva, MM, Maksoud, JG. The outcome of newborns with abdominal wall defects according to the method of abdominal closure: the experience of a single center. Pediatr Surg Int 2006;22:503–7. https://doi.org/10.1007/s00383-006-1696-6.Search in Google Scholar PubMed
73. Martinez-Criado, Y, Cabrera, R, Moya, MJ, Valladares, JC, Lopez-Alonso, M, De Agustin Asensio, JC. Results of transanal endorrectal descent in Hirschprung’s disease. Cir Esp 2015;93:561–6. https://doi.org/10.1016/j.cireng.2015.03.006.Search in Google Scholar
74. Matsumoto, M, Urushihara, N, Fukumoto, K, Yamoto, M, Miyake, H, Nakajima, H. Laparoscopic management for prenatally diagnosed choledochal cysts. Surg Today 2016;46:1410–4. https://doi.org/10.1007/s00595-016-1319-3.Search in Google Scholar PubMed
75. Mattioli, G, Buffa, P, Martinelli, M, Ivani, G, Jasonni, V. All mechanical low rectal anastomosis in children. J Pediatr Surg 1998;33:503–6. https://doi.org/10.1016/s0022-3468(98)90098-7.Search in Google Scholar
76. Menon, P, Rao, KL. Primary anorectoplasty in females with common anorectal malformations without colostomy. J Pediatr Surg 2007;42:1103–6. https://doi.org/10.1016/j.jpedsurg.2007.01.056.Search in Google Scholar PubMed
77. Ming, AX, Li, L, Diao, M, Wang, HB, Liu, Y, Ye, M, et al.. Long term outcomes of laparoscopic-assisted anorectoplasty: a comparison study with posterior sagittal anorectoplasty. J Pediatr Surg 2014;49:560–3. https://doi.org/10.1016/j.jpedsurg.2013.11.060.Search in Google Scholar PubMed
78. Mirshemirani, AR, Kouranlou, J, Rouzrokh, M, Sadeghian, M, Khaleghnezhad, A. Primary posterior sagittal anorectoplasty without colostomy in neonates with high imperforate anus. Acta Med Iran 2007;45:121–5.Search in Google Scholar
79. Miyano, G, Fukuzawa, H, Morita, K, Kaneshiro, M, Miyake, H, Nouso, H, et al.. Laparoscopic repair of malrotation: what are the indications in neonates and children? J Laparoendosc Adv Surg Tech A 2015;25:155–8. https://doi.org/10.1089/lap.2014.0236.Search in Google Scholar PubMed
80. Nam, SH, Cho, MJ, Kim, DY, Kim, SC. Shifting from laparotomy to thoracoscopic repair of congenital diaphragmatic hernia in neonates: early experience. World J Surg 2013;37:2711–6. https://doi.org/10.1007/s00268-013-2189-0.Search in Google Scholar PubMed
81. Nasr, A, Haricharan, RN, Gamarnik, J, Langer, JC. Transanal pullthrough for Hirschsprung disease: matched case-control comparison of Soave and Swenson techniques. J Pediatr Surg 2014;49:774–6. https://doi.org/10.1016/j.jpedsurg.2014.02.073.Search in Google Scholar PubMed
82. Nio, M, Muraji, T. Multicenter randomized trial of postoperative corticosteroid therapy for biliary atresia. Pediatr Surg Int 2013;29:1091–5. https://doi.org/10.1007/s00383-013-3377-6.Search in Google Scholar PubMed
83. Obermayr, F, Szavay, P, Beschorner, R, Fuchs, J. Outcome of transanal endorectal pull-through in patients with hirschsprung’s disease. Eur J Pediatr Surg 2009;19:220–3. https://doi.org/10.1055/s-0029-1220682.Search in Google Scholar PubMed
84. Oh, C, Lee, S, Lee, SK, Seo, JM. Laparoscopic duodenoduodenostomy with parallel anastomosis for duodenal atresia. Surg Endosc 2017;31:2406–10. https://doi.org/10.1007/s00464-016-5241-y.Search in Google Scholar PubMed
85. Onen, A, Cigdem, MK, Ozturk, H, Otcu, S, Dokucu, AI. When to resect and when not to resect an asymptomatic Meckel’s diverticulum: an ongoing challenge. Pediatr Surg Int 2003;19:57–61. https://doi.org/10.1007/s00383-002-0850-z.Search in Google Scholar PubMed
86. Owen, A, Marven, S, Jackson, L, Antao, B, Roberts, J, Walker, J, et al.. Experience of bedside preformed silo staged reduction and closure for gastroschisis. J Pediatr Surg 2006;41:1830–5. https://doi.org/10.1016/j.jpedsurg.2006.06.048.Search in Google Scholar PubMed
87. Patwardhan, N, Kiely, EM, Drake, DP, Spitz, L, Pierro, A. Colostomy for anorectal anomalies: high incidence of complications. J Pediatr Surg 2001;36:795–8. https://doi.org/10.1053/jpsu.2001.22963.Search in Google Scholar PubMed
88. Payne, NR. A cross-sectional, case-control follow-up of infants with gastroschisis. In: Gilmore, L, editor. Journal of neonatal-perinatal medicine; 2010. https://doi.org/10.3233/npm-2010-0117.Search in Google Scholar
89. Peng, Y, Zheng, H, He, Q, Wang, Z, Zhang, H, Chaudhari, PB, et al.. Is the Bishop-Koop procedure useful in severe jejunoileal atresia? J Pediatr Surg 2018;53:1914–7. https://doi.org/10.1016/j.jpedsurg.2018.03.027.Search in Google Scholar PubMed
90. Pratap, A, Gupta, DK, Shakya, VC, Adhikary, S, Tiwari, A, Shrestha, P, et al.. Analysis of problems, complications, avoidance and management with transanal pull-through for Hirschsprung disease. J Pediatr Surg 2007;42:1869–76. https://doi.org/10.1016/j.jpedsurg.2007.07.017.Search in Google Scholar PubMed
91. Raitio, A, Green, PA, Fawkner-Corbett, DW, Wilkinson, DJ, Baillie, CT. Malrotation: age-related differences in reoperation rate. Eur J Pediatr Surg 2016;26:34–7. https://doi.org/10.1055/s-0035-1563677.Search in Google Scholar PubMed
92. Riehle, KJ, Magnuson, DK, Waldhausen, JH. Low recurrence rate after Gore-Tex/Marlex composite patch repair for posterolateral congenital diaphragmatic hernia. J Pediatr Surg 2007;42:1841–4. https://doi.org/10.1016/j.jpedsurg.2007.07.009.Search in Google Scholar PubMed
93. Risby, K, Husby, S, Qvist, N, Jakobsen, MS. High mortality among children with gastroschisis after the neonatal period: a long-term follow-up study. J Pediatr Surg 2017;52:431–6. https://doi.org/10.1016/j.jpedsurg.2016.08.022.Search in Google Scholar PubMed
94. Romao, RL, Nasr, A, Chiu, PP, Langer, JC. What is the best prosthetic material for patch repair of congenital diaphragmatic hernia? Comparison and meta-analysis of porcine small intestinal submucosa and polytetrafluoroethylene. J Pediatr Surg 2012;47:1496–500. https://doi.org/10.1016/j.jpedsurg.2012.01.009.Search in Google Scholar PubMed
95. Rouzrokh, M, Khaleghnejad, AT, Mohejerzadeh, L, Heydari, A, Molaei, H. What is the most common complication after one-stage transanal pull-through in infants with Hirschsprung’s disease? Pediatr Surg Int 2010;26:967–70. https://doi.org/10.1007/s00383-010-2648-8.Search in Google Scholar PubMed
96. Méndez-Martinez, S, García-Carrasco, M, Mendoza-Pinto, C. Surgical complications of simple and complex gastroschisis in newborn. Eur J gen med 2016.Search in Google Scholar
97. Santos, MC, Giacomantonio, JM, Lau, HY. Primary Swenson pull-through compared with multiple-stage pull-through in the neonate. J Pediatr Surg 1999;34:1079–81. https://doi.org/10.1016/s0022-3468(99)90570-5.Search in Google Scholar
98. Sato, K, Uchida, H, Tanaka, Y, Takazawa, S, Jimbo, T, Deie, K. Stapled intestinal anastomosis is a simple and reliable method for management of intestinal caliber discrepancy in children. Pediatr Surg Int 2012;28:893–8. https://doi.org/10.1007/s00383-012-3146-y.Search in Google Scholar PubMed PubMed Central
99. Sauer, CJ, Langer, JC, Wales, PW. The versatility of the umbilical incision in the management of Hirschsprung’s disease. J Pediatr Surg 2005;40:385–9. https://doi.org/10.1016/j.jpedsurg.2004.10.025.Search in Google Scholar PubMed
100. Saxena, A, Willital, GH. Omphalocele: clinical review and surgical experience using dura patch grafts. Hernia 2002;6:73–8. https://doi.org/10.1007/s10029-002-0058-0.Search in Google Scholar PubMed
101. Saxena, AK, Hulskamp, G, Schleef, J, Schaarschmidt, K, Harms, E, Willital, GH. Gastroschisis: a 15-year, single-center experience. Pediatr Surg Int 2002;18:420–4. https://doi.org/10.1007/s00383-002-0799-y.Search in Google Scholar PubMed
102. Shah, AJ, Bhattacharjee, N, Patel, DN, Ganatra, JR. Anal shift: preliminary results. J Pediatr Surg 2003;38:196–8. https://doi.org/10.1053/jpsu.2003.50042.Search in Google Scholar PubMed
103. Shangjie, X, Xiaochun, Z, Wenyi, Y, Wuping, G, Ying, Z, Qiuming, H, et al.. TGF-beta1, Ghrelin, Neurexin, and Neuroligin are predictive biomarkers for postoperative prognosis of laparoscopic surgery in children with Hirschsprung disease. Cell Biochem Biophys 2015;71:1249–54. https://doi.org/10.1007/s12013-014-0338-1.Search in Google Scholar PubMed
104. Shinall, MCJr, Koehler, E, Shyr, Y, Lovvorn, HN3rd Comparing cost and complications of primary and staged surgical repair of neonatally diagnosed Hirschsprung’s disease. J Pediatr Surg 2008;43:2220–5. https://doi.org/10.1016/j.jpedsurg.2008.08.048.Search in Google Scholar PubMed
105. Shrestha, MK, Sherchan, M, Dhaubhadel, BK, Basnet, RB. Early experience with single-stage transanal endorectal pull through for rectosigmoid Hirschsprung’s disease. J Nepal Paediatr Soc 2014;34:188–92.10.3126/jnps.v34i3.11617Search in Google Scholar
106. Snyder, CL, Miller, KA, Sharp, RJ, Murphy, JP, Andrews, WA, Holcomb, GW3rd, et al.. Management of intestinal atresia in patients with gastroschisis. J Pediatr Surg 2001;36:1542–5. https://doi.org/10.1053/jpsu.2001.27040.Search in Google Scholar PubMed
107. Son, TN, Kien, HH. Laparoscopic versus open surgery in management of congenital duodenal obstruction in neonates: a single-center experience with 112 cases. J Pediatr Surg 2017;52:1949–51. https://doi.org/10.1016/j.jpedsurg.2017.08.064.Search in Google Scholar
108. Spilde, TL, St Peter, SD, Keckler, SJ, Holcomb, GW3rd, Snyder, CL, Ostlie, DJ. Open vs laparoscopic repair of congenital duodenal obstructions: a concurrent series. J Pediatr Surg 2008;43:1002–5. https://doi.org/10.1016/j.jpedsurg.2008.02.021.Search in Google Scholar
109. Stollman, TH, de Blaauw, I, Wijnen, MH, van der Staak, FH, Rieu, PN, Draaisma, JM, et al.. Decreased mortality but increased morbidity in neonates with jejunoileal atresia; a study of 114 cases over a 34-year period. J Pediatr Surg 2009;44:217–21. https://doi.org/10.1016/j.jpedsurg.2008.10.043.Search in Google Scholar
110. Stringer, MD, Davison, SM, Rajwal, SR, McClean, P. Kasai portoenterostomy: 12-year experience with a novel adjuvant therapy regimen. J Pediatr Surg 2007;42:1324–8. https://doi.org/10.1016/j.jpedsurg.2007.03.026.Search in Google Scholar
111. Sulkowski, JP, Cooper, JN, Congeni, A, Pearson, EG, Nwomeh, BC, Doolin, EJ, et al.. Single-stage versus multi-stage pull-through for Hirschsprung’s disease: practice trends and outcomes in infants. J Pediatr Surg 2014;49:1619–25. https://doi.org/10.1016/j.jpedsurg.2014.06.002.Search in Google Scholar
112. Takahashi, Y, Matsuura, T, Saeki, I, Zaizen, Y, Taguchi, T. Excellent long-term outcome of hepaticojejunostomy for biliary atresia with a hilar cyst. J Pediatr Surg 2009;44:2312–5. https://doi.org/10.1016/j.jpedsurg.2009.07.051.Search in Google Scholar
113. Teitelbaum, DH, Coran, AG. Primary pull-through in the newborn. Semin Pediatr Surg 1998;7:103–7. https://doi.org/10.1016/s1055-8586(98)70021-6.Search in Google Scholar
114. Thepcharoennirund, S. Primary fascial closure in 112 infants with gastroschisis. J Med Assoc Thai 2005;88:492–7.Search in Google Scholar
115. Tongsin, A, Anuntkosol, M, Niramis, R. Atresia of the jejunum and ileum: what is the difference? J Med Assoc Thai 2008;91(3 Suppl):S85–9.Search in Google Scholar
116. Travassos, DV, van der Zee, DC. Is complete resection of the aganglionic bowel in extensive total aganglionosis up to the middle ileum always necessary? J Pediatr Surg 2011;46:2054–9. https://doi.org/10.1016/j.jpedsurg.2011.06.029.Search in Google Scholar PubMed
117. Tyson, AF, Sola, RJr, Arnold, MR, Cosper, GH, Schulman, AM. Thoracoscopic versus open congenital diaphragmatic hernia repair: single tertiary center review. J Laparoendosc Adv Surg Tech A 2017;27:1209–16. https://doi.org/10.1089/lap.2017.0298.Search in Google Scholar PubMed
118. van den Eijnden, MHA, de Kleine, RHJ, de Blaauw, I, Peeters, P, Koot, BPG, Oomen, MWN, et al.. Choledochal malformation in children: lessons learned from a Dutch national study. World J Surg 2017;41:2631–7. https://doi.org/10.1007/s00268-017-4064-x.Search in Google Scholar PubMed PubMed Central
119. van der Zee, DC. Laparoscopic repair of duodenal atresia: revisited. World J Surg 2011;35:1781–4. https://doi.org/10.1007/s00268-011-1147-y.Search in Google Scholar
120. van der Zee, DC, Dik, P, Beek, FJ. Laparoscopy-assisted anorectal pull-through in anorectal malformations: a reappraisal. World J Surg 2013;37:1934–9. https://doi.org/10.1007/s00268-013-2017-6.Search in Google Scholar
121. van Eijck, FC, Wijnen, RM, van Goor, H. The incidence and morbidity of adhesions after treatment of neonates with gastroschisis and omphalocele: a 30-year review. J Pediatr Surg 2008;43:479–83. https://doi.org/10.1016/j.jpedsurg.2007.10.027.Search in Google Scholar
122. Vu, PA, Thien, HH, Hiep, PN. Transanal one-stage endorectal pull-through for Hirschsprung disease: experiences with 51 newborn patients. Pediatr Surg Int 2010;26:589–92.10.1007/s00383-010-2599-0Search in Google Scholar
123. Wakhlu, A, Wakhlu, AK. The management of exomphalos. J Pediatr Surg 2000;35:73–6. https://doi.org/10.1016/s0022-3468(00)80017-2.Search in Google Scholar
124. Walter-Nicolet, E, Rousseau, V, Kieffer, F, Fusaro, F, Bourdaud, N, Oucherif, S, et al.. Neonatal outcome of gastroschisis is mainly influenced by nutritional management. J Pediatr Gastroenterol Nutr 2009;48:612–7. https://doi.org/10.1097/mpg.0b013e31818c5281.Search in Google Scholar
125. Wang, Q, Yan, LN, Zhang, MM, Wang, WT, Zhao, JC, Pu, CL, et al.. The pre-Kasai procedure in living donor liver transplantation for children with biliary atresia. Hepatobiliary Pancreat Dis Int 2013;12:47–53. https://doi.org/10.1016/s1499-3872(13)60005-3.Search in Google Scholar
126. Weidner, BC, Waldhausen, JH. Swenson revisited: a one-stage, transanal pull-through procedure for Hirschsprung’s disease. J Pediatr Surg 2003;38:1208–11. https://doi.org/10.1016/s0022-3468(03)00269-0.Search in Google Scholar
127. Weil, BR, Leys, CM, Rescorla, FJ. The jury is still out: changes in gastroschisis management over the last decade are associated with both benefits and shortcomings. J Pediatr Surg 2012;47:119–24. https://doi.org/10.1016/j.jpedsurg.2011.10.029.Search in Google Scholar PubMed
128. Werbeck, R, Koltai, J. Umbilical cord as temporary coverage in gastroschisis. Eur J Pediatr Surg 2011;21:292–5. https://doi.org/10.1055/s-0031-1277222.Search in Google Scholar PubMed
129. Wester, T, Rintala, RJ. Early outcome of transanal endorectal pull-through with a short muscle cuff during the neonatal period. J Pediatr Surg 2004;39:157–60. https://doi.org/10.1016/j.jpedsurg.2003.10.007.Search in Google Scholar PubMed
130. Xiao, H, Huang, R, Chen, L, Diao, M, Cheng, W, Li, L, et al.. The midterm outcomes of 1-stage versus 3-stage laparoscopic-assisted anorectoplasty in anorectal malformations with rectoprostatic fistula and rectobulbar fistula: a retrospective cohort study. Medicine (Baltim) 2018;97: e11843. https://doi.org/10.1097/md.0000000000011843.Search in Google Scholar PubMed PubMed Central
131. Xiao, H, Huang, R, Chen, L, Diao, M, Li, L. The application of a shorter loop in Kasai portoenterostomy reconstruction for Ohi type III biliary atresia: a prospective randomized controlled trial. J Surg Res 2018;232:492–6. https://doi.org/10.1016/j.jss.2018.07.002.Search in Google Scholar PubMed
132. Yan, J, Li, S, Chang, Y, Wang, J, Li, A. Comparison of transcolostomy single-incision laparoscopic and open procedures in secondary operations for Hirschsprung’s disease. Biomed Res 2017;28:3527–31.Search in Google Scholar
133. Yang, L, Tang, ST, Li, S, Aubdoollah, TH, Cao, GQ, Lei, HY, et al.. Two-stage laparoscopic approaches for high anorectal malformation: transumbilical colostomy and anorectoplasty. J Pediatr Surg 2014;49:1631–4. https://doi.org/10.1016/j.jpedsurg.2014.05.014.Search in Google Scholar PubMed
134. Zani, A, Yeh, JB, King, SK, Chiu, PP, Wales, PW. Duodeno-duodenostomy or duodeno-jejunostomy for duodenal atresia: is one repair better than the other? Pediatr Surg Int 2017;33:245–8. https://doi.org/10.1007/s00383-016-4016-9.Search in Google Scholar PubMed
135. Zhang, X, Cao, GQ, Tang, ST, Chang, XP, Li, S, Yang, L, et al.. Laparoscopic-assisted Duhamel procedure with ex-anal rectal transection for total colonic aganglionosis. J Pediatr Surg 2018;53:531–6. https://doi.org/10.1016/j.jpedsurg.2017.06.009.Search in Google Scholar PubMed
136. Zheng, S, Xiao, X, Huang, Y. Single-stage correction of imperforate anus with a rectourethral or a rectovestibula fistula by semi-posterior sagittal anorectoplasty. Pediatr Surg Int 2008;24:671–6. https://doi.org/10.1007/s00383-008-2154-4.Search in Google Scholar PubMed
137. Zmora, O, Castle, SL, Papillon, S, Stein, JE. The biological prosthesis is a viable option for abdominal wall reconstruction in pediatric high risk defects. Am J Surg 2017;214:479–82. https://doi.org/10.1016/j.amjsurg.2017.01.004.Search in Google Scholar PubMed
138. Abbas, PI, Dickerson, HA, Wesson, DE. Evaluating a management strategy for malrotation in heterotaxy patients. J Pediatr Surg 2016;51:859–62. https://doi.org/10.1016/j.jpedsurg.2016.02.037.Search in Google Scholar PubMed
139. Chan, KWE, Lee, KH, Wong, HYV, Tsui, SYB, Mou, JWC, Tam, YHP. Ten-year native liver survival rate after laparoscopic and open Kasai portoenterostomy for biliary atresia. J Laparoendosc Adv Surg Tech A 2019;29:121–5. https://doi.org/10.1089/lap.2018.0350.Search in Google Scholar PubMed
140. De Bie, F, Suply, E, Verbelen, T, Vanstraelen, S, Debeer, A, Cross, K, et al.. Early surgical complications after congenital diaphragmatic hernia repair by thoracotomy vs. laparotomy: a bicentric comparison. J Pediatr Surg 2020:32005504. https://doi.org/10.1016/j.jpedsurg.2019.12.020. https://www.sciencedirect.com/science/article/pii/S0022346819309303?via%3Dihub.Search in Google Scholar
141. Dewberry, L, Hilton, S, Gien, J, Liechty, KW, Marwan, AI. Flap repair in congenital diaphragmatic hernia leads to lower rates of recurrence. J Pediatr Surg 2019;54:2487–91. https://doi.org/10.1016/j.jpedsurg.2019.08.042.Search in Google Scholar
142. Dewberry, LC, Hilton, SA, Vuille-Dit-Bille, RN, Liechty, KW. Is tapering enteroplasty an alternative to resection of dilated bowel in small intestinal atresia? J Surg Res 2020;246:1–5. https://doi.org/10.1016/j.jss.2019.08.014.Search in Google Scholar
143. Dubbers, M, Holschneider, AM, Meier-Ruge, W. Results of total and subtotal colon resections in children. Eur J Pediatr Surg 2003;13:195–200. https://doi.org/10.1055/s-2003-41261.Search in Google Scholar
144. Gabler, TD, Loveland, J, Theron, A, Westgarth-Taylor, C. Anorectal malformations and the impact of HIV on surgical outcome. S Afr Med J 2018;108. https://doi.org/10.7196/SAMJ.2018.v108i11.13168.Search in Google Scholar
145. Gao, R, Yang, H, Li, Y, Meng, L, Li, Y, Sun, B, et al.. Enhanced recovery after surgery in pediatric gastrointestinal surgery. J Int Med Res 2019;47:4815–26. https://doi.org/10.1177/0300060519865350.Search in Google Scholar
146. He, QM, Zhong, W, Zhang, H, Li, L, Wang, Z, Tan, Y, et al.. Standardized indications to assist in the safe thoracoscopic repair of congenital diaphragmatic hernia in neonates. J Laparoendosc Adv Surg Tech A 2016;26:399–403. https://doi.org/10.1089/lap.2015.0327.Search in Google Scholar
147. Joda, AE, Abdullah, AF. Outcomes of end-to-side oblique anastomosis as a surgical technique for jejuno-ileal atresia. Updates Surg 2019;71:587–93. https://doi.org/10.1007/s13304-019-00666-9.Search in Google Scholar
148. Jona, J. Personal experience with 50 laparoscopic procedures for Hirschsprung’s disease in infants and children. Pediatr Endosurg Innovative Tech 2001;5:361–3. https://doi.org/10.1089/10926410152776333.Search in Google Scholar
149. Jung, PM. Hirschsprung’s disease: one surgeon’s experience in one institution. J Pediatr Surg 1995;30:646–51. https://doi.org/10.1016/0022-3468(95)90680-0.Search in Google Scholar
150. Long, AM, Bunch, KJ, Knight, M, Kurinczuk, JJ, Losty, PD. One-year outcomes of infants born with congenital diaphragmatic hernia: a national population cohort study. Arch Dis Child Fetal Neonatal Ed 2019;104:F643–7. https://doi.org/10.1136/archdischild-2018-316396.Search in Google Scholar
151. Marei, MM, Abouelfadl, MH, Rawwash, AAE, Seleim, HM, Mahmoud, WM, Yassin, TYM, et al.. Early outcomes of tapering jejunoplasty by antimesenteric seromuscular stripping and mucosal inversion for proximal jejunal atresia. Egypt Pediatr Assoc Gaz 2019;67:4. https://doi.org/10.1186/s43054-019-0003-9.Search in Google Scholar
152. Narang, A, Carlsen, V, Long, A, Battin, M, Upadhyay, V, Sadler, L, et al.. Anterior abdominal wall defects managed at a tertiary maternal-fetal medicine service in New Zealand: what counselling advice can we offer parents? Aust N Z J Obstet Gynaecol 2019;59:805–10. https://doi.org/10.1111/ajo.12965.Search in Google Scholar
153. Ren, X, Xiao, H, Li, L, Diao, M, Chen, L, Zhou, R, et al.. Single-incision laparoscopic-assisted anorectoplasty versus three-port laparoscopy in treatment of persistent cloaca: a midterm follow-up. J Laparoendosc Adv Surg Tech A 2018;28:1540–7. https://doi.org/10.1089/lap.2018.0225.Search in Google Scholar
154. Ryu, HS, Lee, JY, Kim, DY, Kim, SC, Namgoong, J-M. Minimally-invasive neonatal surgery: laparoscopic excision of choledochal cysts in neonates. Ann Surg Treat Res 2019;97:21–6. https://doi.org/10.4174/astr.2019.97.1.21.Search in Google Scholar
155. Sakaguchi, T, Hamada, Y, Shirai, T, Hamada, H, Shigeta, Y, Nakamura, Y, et al.. Postoperative complications of umbilical loop colostomy for anorectal malformations in neonates compared with the conventional abdominal stoma: a non-randomized study. World J Plast Surg 2019;2: e000031. https://doi.org/10.1136/wjps-2018-000031.Search in Google Scholar
156. Sato, S, Nishijima, E, Muraji, T, Tsugawa, C, Kimura, K. Jejunoileal atresia: a 27-year experience. J Pediatr Surg 1998;33:1633–5. https://doi.org/10.1016/s0022-3468(98)90596-6.Search in Google Scholar
157. Sola, RJr, Poola, AS, Memon, R, Singh, V, Hendrickson, RJ, St Peter, SD, et al.. The relationship of eosinophilia with outcomes of Hirschsprung disease in children. Pediatr Surg Int 2019;35:425–9. https://doi.org/10.1007/s00383-018-04430-9.Search in Google Scholar PubMed
158. Yang, S, Wang, M, Shen, C. Bowel plication in neonatal high jejunal atresia. Medicine (Baltim) 2019;98: e15459. https://doi.org/10.1097/md.0000000000015459.Search in Google Scholar
159. Zhu, H, Gao, R, Alganabi, M, Dong, K, Ganji, N, Xiao, X, et al.. Long-term surgical outcomes of apple-peel atresia. J Pediatr Surg 2019;54:2503–8. https://doi.org/10.1016/j.jpedsurg.2019.08.045.Search in Google Scholar PubMed
160. Zhu, H, Zheng, S, Alganabi, M, Peng, X, Dong, K, Pierro, A, et al.. Reoperation after Ladd’s procedure in the neonatal period. Pediatr Surg Int 2019;35:117–20. https://doi.org/10.1007/s00383-018-4382-6.Search in Google Scholar PubMed
161. Zhu, T, Sun, X, Wei, M, Yi, B, Zhao, X, Wang, W, et al.. Optimal time for single-stage pull-through colectomy in infants with short-segment Hirschsprung disease. Int J Colorectal Dis 2019;34:255–9. https://doi.org/10.1007/s00384-018-3179-3.Search in Google Scholar PubMed
162. Young, JY, Kim, DS, Muratore, CS, Kurkchubasche, AG, Tracy, TFJr, Luks, FI. High incidence of postoperative bowel obstruction in newborns and infants. J Pediatr Surg 2007;42:962–5. https://doi.org/10.1016/j.jpedsurg.2007.01.030.Search in Google Scholar PubMed
163. Lakshminarayanan, B, Hughes-Thomas, AO, Grant, HW. Epidemiology of adhesions in infants and children following open surgery. Semin Pediatr Surg 2014;23:344–8. https://doi.org/10.1053/j.sempedsurg.2014.06.005.Search in Google Scholar PubMed
164. Grant, HW, Parker, MC, Wilson, MS, Menzies, D, Sunderland, G, Thompson, JN, et al.. Adhesions after abdominal surgery in children. J Pediatr Surg 2008;43:152–6. https://doi.org/10.1016/j.jpedsurg.2007.09.038.Search in Google Scholar PubMed
165. Wilkins, BM, Spitz, L. Incidence of postoperative adhesion obstruction following neonatal laparotomy. Br J Surg 1986;73:762–4. https://doi.org/10.1002/bjs.1800730929.Search in Google Scholar PubMed
166. Guyton, KL, Hyman, NH, Alverdy, JC. Prevention of perioperative anastomotic healing complications: anastomotic stricture and anastomotic leak. Adv Surg 2016;50:129–41. https://doi.org/10.1016/j.yasu.2016.03.011.Search in Google Scholar PubMed PubMed Central
Supplementary Material
The online version of this article offers reviewer assessments as supplementary material (https://doi.org/10.1515/iss-2020-0042).
© 2021 Laurens D. Eeftinck Schattenkerk et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Editorial
- Reviews
- The incidence of different forms of ileus following surgery for abdominal birth defects in infants: a systematic review with a meta-analysis method
- Need for transition medicine in pediatric surgery – health related quality of life in adolescents and young adults with congenital malformations
- Image-guided surgery and novel intraoperative devices for enhanced visualisation in general and paediatric surgery: a review
- Original Article
- Ovarian lesions and tumors in infants and older children
Articles in the same Issue
- Frontmatter
- Editorial
- Editorial
- Reviews
- The incidence of different forms of ileus following surgery for abdominal birth defects in infants: a systematic review with a meta-analysis method
- Need for transition medicine in pediatric surgery – health related quality of life in adolescents and young adults with congenital malformations
- Image-guided surgery and novel intraoperative devices for enhanced visualisation in general and paediatric surgery: a review
- Original Article
- Ovarian lesions and tumors in infants and older children

