Teaching design for chapter “primary liver cancer” in surgery course based on the clinical theory and clerkship synchronization model in the era of New Medicine
-
Feng Ye
, Qiang Cai
, Xiaoli Wang
und Yuan Qiao
Abstract
Objectives
The chapter on primary liver cancer in the surgery course is designed to align with the New Medicine paradigm, emphasizing the integration of clinical theory with clerkship experiences to foster a comprehensive understanding of the disease.
Methods
The teaching design incorporates innovative strategies such as outcome-based objectives, interactive learning activities, and the clinical theory and clerkship synchronization teaching model. The learning objectives are defined to balance technical proficiency with interdisciplinary knowledge and humanistic qualities. The curriculum content is restructured to include advanced topics and case studies that reflect the latest advancements in liver cancer management. A blended teaching model is employed, utilizing online platforms and in-class discussions to enhance student engagement and critical thinking.
Results
With regard to the acquisition of the fundamental knowledge of primary liver cancer, the class that employed the novel teaching model demonstrated significantly higher scores than the class that did not. Based on the results of students’ feedback questionnaire, the self-improvement ratings were found to be significantly higher in classes that employed the synchronization model.
Conclusions
The implementation of the clinical theory and clerkship synchronization teaching model has been effective in enhancing students’ knowledge, skills, and professional attitudes towards primary liver cancer management.
Background
The emergence of New Medicine represents a transformative approach to medical education in response to rapid advancements in science, technology, and societal healthcare needs [1]. This concept integrates traditional medical knowledge with cutting-edge innovations, interdisciplinary collaboration, and a patient-centered approach to cultivate professionals equipped for modern medical challenges. In this context, surgical education requires reimagining to meet these evolving demands and ensure the development of competent and compassionate surgeons [2]. As an example, the design and implementation process for the chapter on primary liver cancer in a surgery course is demonstrated. This example highlights how innovative teaching strategies, such as outcome-based objectives, interactive learning activities, and clinical theory and clerkship synchronization teaching model, can be employed to enhance students’ knowledge, skills, and professional attitudes, aligning with the core principles of New Medicine [1].
In the surgical curriculum, “primary liver cancer” holds a pivotal role due to its complex, multidisciplinary treatment, requiring students to develop a deep understanding of not just surgical techniques, but also diagnostic, interventional, and oncological management. Compared to other chapters, it stands out for its integration of preoperative, operative, and postoperative care, as well as its focus on advanced surgical procedures like liver transplantation and hepatectomy. Moreover, the emphasis on pathophysiology, risk factors, diagnostics, and the global impact of liver cancer further distinguishes it as a unique and essential topic in surgical education.
In many surgical programs, traditional classroom-based teaching remains the primary method for delivering core knowledge. Classroom teaching tends to focus on theoretical knowledge, with less emphasis on clinical reasoning, problem-solving, and decision-making skills that are essential for surgeons. This can lead to low engagement, where students are less likely to interact, ask questions, or actively participate in the learning process. In traditional classroom settings, feedback is often limited to exams or written assignments, with fewer opportunities for immediate feedback on clinical skills or decision-making abilities [3]. To overcome these limitations, it is essential to incorporate more interactive and experiential learning methods, such as clinical clerkships, case-based learning (CBL), and team-based problem-solving [4], 5]. These methods will help bridge the gap between theoretical knowledge and practical application, ensuring that students are better prepared for the complexities of modern surgical practice [6]. Therefore, the teaching design and implementation presented in this paper will contribute to providing new ideas and methods for the development of surgical courses under the context of the New Medical Education.
This chapter is intended for 8-year clinical medicine undergraduate students. The class consists of 23 students, and this chapter is part of the “General Surgery” course, taught in the first semester of their fourth year. The total teaching time for this chapter is 80 min.
Teaching design
Redefining learning objectives
Surgical curricula must clearly define outcomes that align with New Medicine’s goals, balancing technical proficiency with interdisciplinary knowledge and humanistic qualities [1]. The redefinition of teaching objectives for the “primary liver cancer” chapter in the surgery course is crucial in the context of New Medical Education to address the evolving demands of healthcare education. The “ASK” educational philosophy is applied to the design of learning objectives (Figure 1). “ASK” stands for “attitude”, “skill” and “knowledge”, and represents an educational philosophy that places a strong emphasis on the holistic development of the student [7], 8]. The teaching objectives for the “primary liver cancer” chapter in the surgery course need to be aligned with the comprehensive goals of “ASK”. These goals should be tailored to promote interdisciplinary integration, clinical competence, patient-centered care, and evidence-based practice (Figure 2).
The “ASK” educational philosophy for teaching surgery. “ASK” stands for “attitude”, “skill” and “knowledge”.
Comprehensive goals of “ASK”. “ASK” stands for “attitude”, “skill” and “knowledge”.
Adapting to New Medical Education trends
The New Medicine emphasizes the integration of multiple disciplines, such as genomics, artificial intelligence, and bioinformatics, into traditional medical education. This requires a shift in focus from purely theoretical knowledge to competencies that integrate these new domains. Traditional medical education often focuses on content delivery without clear measurable outcomes. The outcome-based education (OBE) framework ensures that students achieve specific competencies, making it necessary to redefine objectives with clearly stated outcomes [9], 10].
Bridging the gap between theory and practice
Surgery students must be able to apply theoretical knowledge in real clinical scenarios, such as diagnosing primary liver cancer, formulating treatment plans, and managing complications. The redefined objectives must emphasize hands-on practice, clinical reasoning, and decision-making. New educational models promote simultaneous learning of theory and clinical practice [2]. Teaching objectives need to reflect this synchronization, ensuring that students gain not only conceptual understanding but also practical application skills.
Addressing advances in liver cancer management
The management of primary liver cancer has evolved significantly with innovations in imaging, molecular diagnostics, and minimally invasive treatments. Objectives must be updated to include these advancements and prepare students for modern clinical practice. Liver cancer treatment often involves a team of specialists [11]. Redefined objectives must focus on equipping students with the ability to collaborate in multidisciplinary settings, understanding the roles of surgery, oncology, radiology, and hepatology [12].
Enhancing professional competence
Traditional objectives often overlook psychomotor skills such as interpreting imaging or conducting preoperative evaluations. The new objectives need to include measurable skill development to ensure clinical competence. In managing liver cancer, ethical considerations, such as patient selection for liver transplantation and equity in treatment allocation, are critical. Updated objectives should address these professional and ethical challenges to prepare students for holistic patient care.
Aligning with student-centered learning
New Medical Education emphasizes active and critical learning over rote memorization. The objectives should encourage problem-solving, decision-making, and reflective practices. Students have diverse interests and career goals [10], 13]. Redefined objectives under the OBE framework allow flexibility for students to achieve core competencies while exploring areas of individual interest.
Building on the above principles and adopting the backward design strategy, we have formulated the learning objectives for the “primary liver cancer” chapter tailored to 8-year clinical medicine undergraduate students. Based on the OBE philosophy and Bloom’s Taxonomy, the teaching objectives for this session are as follows [14]:
Understand the pathophysiology and etiology of primary liver cancer, including its relationship with chronic liver diseases such as cirrhosis and hepatitis.
Identify the risk factors for liver cancer and understand the epidemiological trends.
Gain skills in interpreting diagnostic imaging (CT, MRI, etc.) and understanding biomarkers like alpha-fetoprotein (AFP) in diagnosing liver cancer.
Understand and practice preoperative assessment and management strategies for liver cancer patients.
Develop an understanding of multidisciplinary management for liver cancer, including surgery, chemotherapy, and liver transplantation.
Evaluate and reflect on clinical cases to make informed decisions about treatment options.
Curriculum content restructuring
In conventional medical education, the “primary liver cancer” chapter within the surgery curriculum typically covers the following topics: overview, pathology, pathogenesis, clinical manifestations, diagnosis, staging, treatment, prevention, and follow-up. Building upon the existing traditional teaching content, the following advanced, innovative, and challenging teaching materials have been added to achieve the above learning objectives.
Changes in the epidemiology of primary liver cancer in China
Recent studies show a gradual decrease in liver cancer incidence and mortality rates in China. This trend is attributed to better control of risk factors such as hepatitis B virus (HBV) and the implementation of nationwide vaccination programs [15], 16]. Non-alcoholic fatty liver disease (NAFLD) and metabolic syndrome are emerging as significant contributors due to lifestyle changes, including increased prevalence of obesity and diabetes. Liver cancer remains more prevalent in rural areas compared to urban regions, likely due to disparities in healthcare access, education, and environmental factors [17].
The discussion of epidemiological changes and emerging risk factors directly supports this cognitive objective by providing updated, evidence-based insights into liver cancer trends in China. Students can analyze how HBV vaccination and lifestyle changes have reshaped the risk profile of liver cancer, improving their understanding of disease etiology and public health impact. Teaching these changes encourages students to critically evaluate epidemiological data and develop skills in data interpretation and its application in clinical decision-making. Highlighting the role of public health initiatives like HBV vaccination fosters an appreciation of the broader social and systemic efforts required for disease prevention [18].
Treatment overview for intermediate and advanced liver cancer
The main treatment options for middle to late-stage liver cancer include local therapy, systemic therapy, and combined treatment approaches. Transarterial chemoembolization (TACE) is widely regarded as the first-line treatment for intermediate-stage hepatocellular carcinoma (HCC). TACE combines targeted chemotherapy with vascular embolization to reduce tumor size and progression. Molecular targeted drugs such as sorafenib and lenvatinib remain standard first-line treatments for advanced-stage HCC. Immune checkpoint inhibitors (ICIs) such as atezolizumab (anti-PD-L1 monoclonal antibody) combined with bevacizumab (anti-VEGF monoclonal antibody) represent a breakthrough, offering superior efficacy compared to sorafenib as a first-line treatment in advanced cases [19], 20]. The main challenges in treating middle to late-stage liver cancer are the heterogeneity of the disease, the accessibility of treatment options, and the management of adverse drug reactions.
Discussing the updated treatment modalities enhances students’ knowledge of contemporary therapeutic approaches, their indications, and mechanisms. Explaining how ICIs like atezolizumab improve survival rates for advanced HCC demonstrates cutting-edge advancements, fostering a deeper understanding of treatment strategies. Incorporating treatment algorithms and case studies enables students to practice clinical decision-making and treatment planning. Highlighting challenges such as treatment accessibility or balancing efficacy with quality of life helps students develop empathy and ethical sensitivity. Discussions on disparities in access to therapies like ICIs in rural China can encourage students to reflect on their roles as advocates for equitable healthcare. This approach ensures students are equipped not only with up-to-date knowledge and practical skills but also with the ethical and empathetic perspectives necessary for managing complex cancer cases effectively.
Advances in early diagnosis of liver cancer
Early-stage HCC often lacks specific symptoms, leading to delayed detection. In addition to AFP, significant progress has been made in the early diagnosis of liver cancer. AFP-L3 is a specific isoform of AFP associated with malignant tumors, offering better specificity compared to total AFP [21], 22]. Using AFP with markers like des-γ-carboxyprothrombin (DCP) and glypican-3 enhances diagnostic accuracy [23]. Contrast-enhanced ultrasound (CEUS), dynamic CT, and MRI have improved sensitivity for detecting small liver lesions. Circulating tumor DNA (ctDNA), exosomal RNA, and microRNA are promising areas of research for non-invasive early detection [24]. Artificial intelligence applications in imaging and data analysis are enhancing early detection capabilities.
Teaching AFP’s discovery, limitations, and its integration with advanced methods enhances students’ foundational knowledge of diagnostic principles and practices. Students learn to assess AFP levels and imaging findings within a diagnostic framework, building critical analytical skills. By incorporating the history, current application, and advancements of AFP and other diagnostic tools into teaching, educators can comprehensively address the cognitive, psychomotor, and affective domains. This ensures students gain updated knowledge, practical diagnostic skills, and a deeper understanding of the broader social and economic context of liver cancer diagnosis.
Milestones in the development of liver surgery in China
Dr. Mengchao Wu was known as the “father of Chinese hepatobiliary surgery.” He pioneered techniques for precise liver segmentation, which revolutionized surgical precision and safety in hepatectomy. The “anatomical hepatectomy” technique based on liver blood supply significantly reducing intraoperative blood loss [25]. Dr. Zhaoyou Tang was a leader in combining clinical practice with basic research. He proposed the “elimination plus transformation theory” of liver cancer, emphasizing the importance of Chinese and Western Medicine integration [26]. He advocated for integrating chemotherapy and immunotherapy with surgery, contributing to long-term survival improvements [27]. Dr. Xiaoping Chen advanced laparoscopic and minimally invasive techniques in liver surgery. His work on laparoscopic liver resections has set international benchmarks for minimally invasive surgery [28]. These pioneers have collectively transformed liver surgery in China, improving surgical outcomes, long-term survival rates, and global recognition.
Incorporating the history and contributions of Chinese pioneers in liver surgery into teaching not only provides medical knowledge but also inspires students to connect scientific advancements with clinical practice. Discussing the personal journeys and challenges faced by these surgeons fosters respect for the medical profession and inspires students to pursue excellence. Teaching the contributions of Chinese liver surgery pioneers not only aligns with the OBE framework but also provides a well-rounded educational experience. Students gain technical knowledge, practical insights, and ethical perspectives, preparing them to contribute to the future development of clinical medicine and patient care. By showcasing the evolution of liver surgery in China, educators can inspire a sense of national pride and professional responsibility in medical students.
Cutting-edge teaching content
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) is an innovative surgical approach designed for patients with liver tumors who have insufficient future liver remnant (FLR) to undergo traditional hepatectomy [29]. It offers faster liver hypertrophy compared to conventional portal vein embolization. However, this approach is associated with high morbidity and mortality rates, particularly in patients with compromised liver function. This also requires careful patient selection and expertise. Conversion therapy involves the use of systemic therapies or locoregional treatments to shrink unresectable liver tumors, making them resectable. Targeted agents such as lenvatinib and immunotherapies like atezolizumab + bevacizumab are increasingly used for conversion. TACE or hepatic artery infusion chemotherapy (HAIC) can reduce tumor size, facilitating subsequent resection. Conversion therapy has significantly improved resection rates and survival in patients with advanced liver cancer, bridging the gap between systemic and surgical treatments [30].
Integrating ALPPS, conversion therapy, and other innovations into teaching equips students with a thorough understanding of cutting-edge techniques in liver surgery, aligning with multiple learning objectives. Students can learn to evaluate tumor burden, liver volume, and response to conversion therapy to decide on treatment pathways. Hands-on activities, such as interpreting CT images of patients undergoing ALPPS, encourage application of theoretical knowledge in practical scenarios.
Teaching focus and strategies
Clinical manifestations and diagnosis of primary liver cancer
The early detection and accurate diagnosis of primary liver cancer are pivotal for determining treatment strategies and patient prognosis. The non-specific nature of early clinical symptoms (e.g., fatigue and weight loss) makes timely diagnosis challenging. Understanding clinical manifestations and diagnostic tools is essential for clinicians to make informed decisions on appropriate interventions. Early diagnosis is closely associated with better survival rates, as early-stage liver cancer can be treated effectively through surgery or locoregional therapies. Teaching students how to recognize early signs and use diagnostic tools is crucial in improving patient outcomes and ensuring effective treatment.
Using CBL, interactive lectures and hands-on methods such as simulation-based learning and flipped classrooms, students will be equipped with the necessary skills to recognize symptoms and utilize diagnostic tools effectively in clinical practice. We introduced real clinical cases where students must identify the symptoms of liver cancer and suggest appropriate diagnostic methods. Interactive lectures and discussions presenting key clinical signs and diagnostic procedures will engage students interactively. Case studies and diagnostic images are used to demonstrate how clinicians identify HCC in practice. Visual representation of clinical and imaging findings helps students understand the differences between benign and malignant lesions in the liver, which is critical for accurate diagnosis. Integration of laboratory tests and biomarkers help students understand the utility of biomarkers in clinical practice, particularly in the early detection of liver cancer. Assigning preparatory readings or videos on liver cancer symptoms and diagnostic tools, followed by in-class discussions and interactive quizzes, encourages active learning and reinforces key concepts about clinical manifestations and diagnostic methods through peer discussions and teacher feedback. Organizing small group discussions where students analyze real-life case scenarios of HCC and present their diagnostic strategies, encourages collaborative learning and allows students to practice clinical reasoning, helping them consolidate their knowledge on liver cancer diagnosis.
Treatment options and surgical indications for primary liver cancer
Primary liver cancer has a diverse range of treatment options, including liver resection, liver transplantation, and locoregional therapies (such as TACE and ablation). These options are highly dependent on the stage of the disease, liver function, and patient comorbidities, making treatment decisions complex and nuanced. Students must understand how to integrate multiple factors, such as tumor size, location, liver reserve, and vascular invasion, into a comprehensive treatment plan. New technologies such as liver transplantation protocols are continuously evolving, and their indications, benefits, and risks are not universally standardized. Understanding when and how to apply these advanced techniques requires advanced clinical knowledge, making it a challenging area for students.
The complexity of treatment choices and surgical indications for primary liver cancer makes this topic a challenging area of teaching. However, using strategies such as CBL, a multidisciplinary approach, interactive decision-making models, and structured decision-making frameworks can help students navigate these difficulties. By providing real-life scenarios, engaging with up-to-date evidence, and utilizing innovative teaching methods like flipped classrooms, we can equip students with the skills and knowledge necessary to make informed decisions about HCC treatment.
Case design
Traditional lecture-based approaches often result in passive learning, which may fail to fully engage students. For the purpose of reflecting the New Medicine paradigm’s focus on fostering clinical competence, critical thinking, and interdisciplinary collaboration, it is recommended that this subject be taught in the form of CBL. It is therefore essential to conduct case design.
Case description
Patient: A 35-year-old male, with a long history of chronic HBV infection, presents with complaints of right upper abdominal discomfort for the past 2 months. The discomfort is described as a dull ache with occasional bloating but no overt pain. The patient denies fever, weight loss, or jaundice. He has no history of alcohol consumption or smoking, and there is no family history of liver cancer.
Medical history: The patient was diagnosed with HBV at the age of 25 and has been on anti-viral therapy intermittently. Liver function tests have been periodically monitored, but he has never had a liver biopsy or imaging studies beyond routine follow-up. He reports occasional fatigue but is otherwise active.
Current symptoms: Right upper quadrant discomfort, occasional nausea, no vomiting, no significant weight loss.
Physical examination
General appearance: The patient appears well-nourished and in no acute distress.
Vital signs:
Blood pressure: 120/78 mmHg;
Heart rate: 78 bpm;
Respiratory rate: 16/min;
Temperature: 36.7 °C.
Abdominal examination:
Inspection: No visible distention or jaundice;
Palpation: Mild tenderness in the right upper quadrant, no rebound tenderness or guarding;
Percussion: Liver dullness is noted below the costal margin, suggesting hepatomegaly;
Auscultation: Normal bowel sounds, no bruit over the liver.
Other systems: No signs of edema, ascites, or encephalopathy.
Laboratory diagnosis
Liver function tests:
Alanine aminotransferase (ALT): 120 U/L (elevated);
Aspartate aminotransferase (AST): 110 U/L (elevated);
Total bilirubin: 1.2 mg/dL (within normal range);
Albumin: 4.0 g/dL (normal).
International normalized ratio (INR): 1.1 (normal)
HBV serology:
Hepatitis B surface antigen (HBsAg): Positive;
HBV DNA: 8.0 × 105 IU/mL (elevated);
Anti-hepatitis B core antibody (HBc): Positive.
AFP: 50 ng/mL (mildly elevated)
Other tests:
Complete blood count (CBC): Normal;
Renal function: Normal;
Coagulation profile: Normal.
Radiologic examination
Abdominal ultrasound: Hepatomegaly noted with a hypoechoic lesion in the right lobe of the liver measuring 9.5 cm × 14.0 cm (Figure 3); no ascites or portal vein thrombosis observed.
Contrast-enhanced CT: A 14 cm mass in the right liver lobe with early arterial phase enhancement and washout in the portal venous phase, suggesting a malignant lesion. The mass appears well-circumscribed, with no major vascular invasion (Figure 3).
MRI: A lesion with characteristics consistent with HCC, exhibiting arterial phase hyperenhancement and washout in the venous phase (Figure 3).
Questions for students
What is your most likely diagnosis for this patient? Why?
How would you stage this patient’s liver cancer? Which staging systems are commonly used for HCC, and how do they influence treatment decisions?
Based on the clinical presentation and radiologic findings, would you consider this patient a candidate for surgery? What are the criteria for surgical resection or liver transplantation in HCC patients?
What other treatment options would you consider for this patient, and why?
Given the patient’s age and medical history, what ethical considerations should be taken into account when deciding on treatment options?
Teaching model and methods
In order to bridge the gap between theoretical knowledge and real-world clinical application, synchronizing clinical theory with clinical practice in the surgery curriculum under the New Medicine paradigm is implemented. Throughout the teaching process, a problem-oriented instructional approach is primarily employed. Well-designed questions in advance facilitate students’ independent thinking, while teachers provide corresponding educational resources both online and offline. The teaching process is divided into four distinct yet closely interconnected phases: pre-class, theoretical-class, clerkship-class, and post-class (Figure 4).
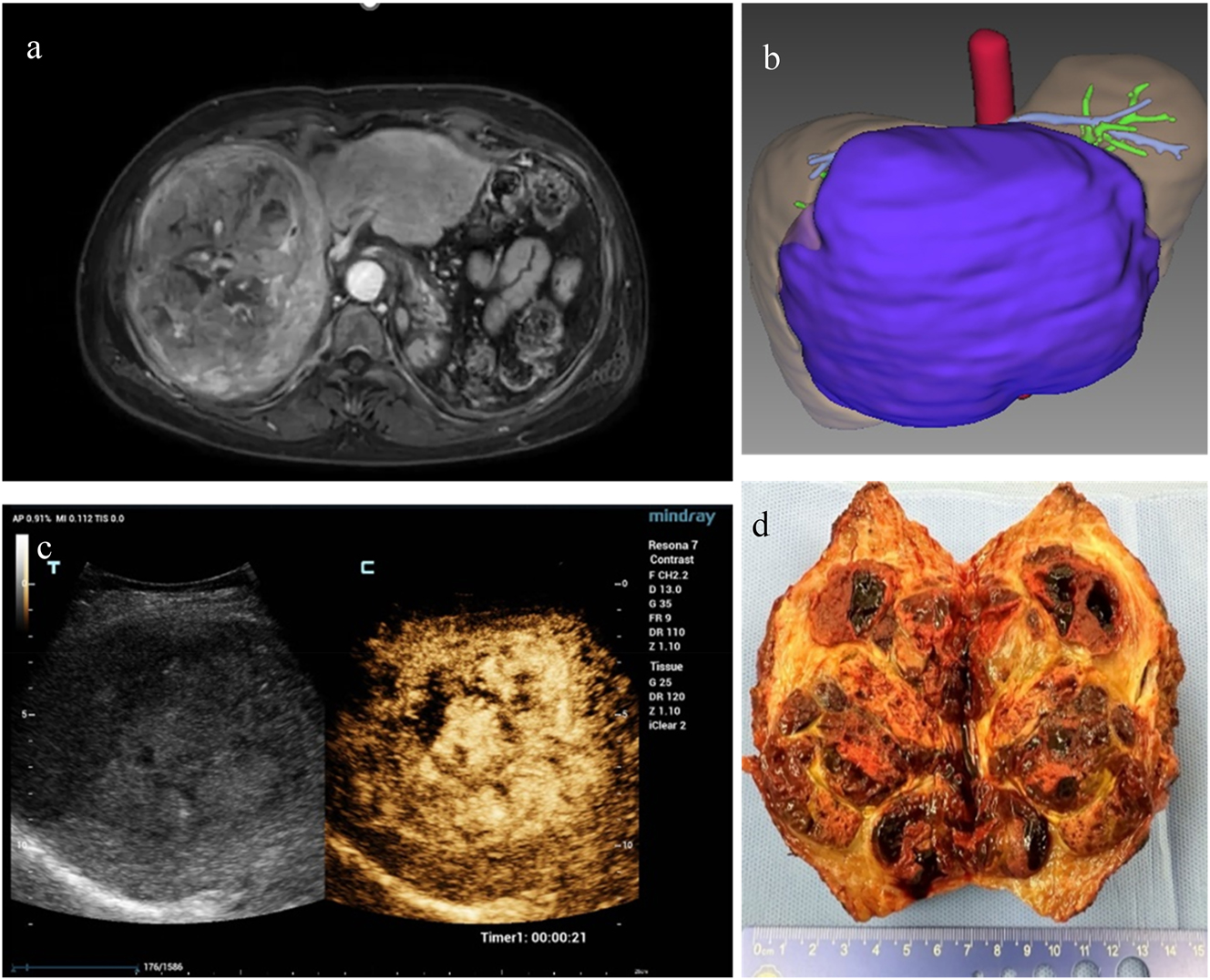
Teaching materials in CBL learning. (a) MRI of a large hepatic mass (T1WI enhancement). (b) CT-based three-dimensional reconstruction image of the liver for surgical planning. (c) Ultrasound contrast imaging of the hepatic lesion. (d) Ex vivo image of surgical specimen after hepatectomy. CBL, case-based learning.
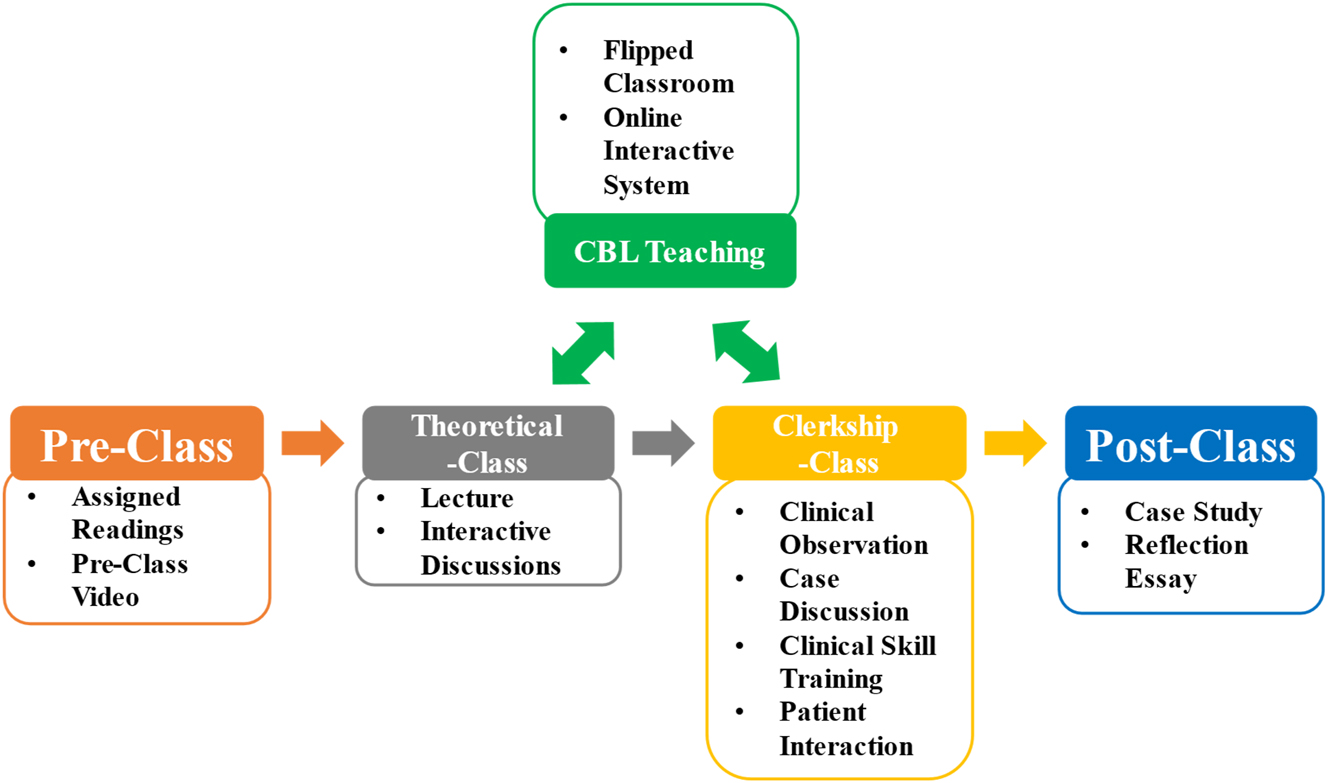
Flow chart of the teaching process. CBL, case-based learning.
Pre-class
This section is designed to prepare students for active engagement during theory-based lessons and clinical practice, ensuring a seamless integration of knowledge and skills. The primary goal of the pre-class preparation is to provide students with foundational knowledge about HCC and its clinical relevance, ensuring they come to class with the necessary background to engage with the theoretical content and clinical discussions.
Assigned readings: Prior to the class, students are assigned specific reading materials, such as recent literature on HCC epidemiology, risk factors, clinical presentation, diagnostic methods, and current treatment guidelines. This provides students with up-to-date, evidence-based knowledge.
Pre-class video or lecture: A brief recorded video or online lecture is provided, summarizing key concepts related to HCC, including its pathophysiology, diagnostic methods, staging, and treatment options.
Questions: What are the main risk factors for primary liver cancer, and how do they contribute to its development? How is HCC diagnosed, and what role does imaging play in its detection? What are the most recent advancements in the treatment of HCC, and how do they impact patient outcomes?
Pedagogical considerations: These pre-class activities ensure that students have a solid understanding of the basic concepts of primary liver cancer before the theoretical class, allowing them to come prepared for deeper discussion and critical thinking. The questions aim to stimulate curiosity and prompt students to begin thinking about the clinical implications of HCC.
Theoretical-class
The primary goal of this section is to provide students with an in-depth understanding of primary liver cancer, including its pathophysiology, clinical presentation, diagnostic strategies, and current treatment options. By the end of this part, students should be able to recognize the signs and symptoms of HCC, understand the principles of diagnosis and staging, and evaluate treatment modalities based on evidence-based guidelines.
Lecture topics:
Understanding the molecular mechanisms of hepatocellular carcinoma, including genetic mutations, the role of cirrhosis, and the impact of chronic HBV and hepatitis C virus (HCV) infections;
Exploring the global burden of HCC, with a focus on the risk factors specific to the Chinese population, such as HBV infection and alcohol consumption;
Discussing the common symptoms, signs, and complications associated with primary liver cancer, such as jaundice, ascites, and portal hypertension;
Detailing the use of imaging modalities (ultrasound, CT, and MRI) and laboratory tests (AFP and liver function tests) in diagnosing HCC, as well as the role of biopsy and staging systems (e.g., TNM staging);
Analyzing current treatment options for HCC, including surgical resection, liver transplantation, locoregional therapies (TACE, ablation), and systemic treatments (targeted therapy, immunotherapy).
Interactive discussions: Presenting hypothetical or real-life patient cases to discuss differential diagnosis, treatment planning, and management strategies.
Questions: How would you differentiate between hepatocellular carcinoma and other liver diseases (e.g., cirrhosis or cholangiocarcinoma) based on clinical presentation and diagnostic tests? What role does AFP play in the diagnosis of HCC, and what are its limitations? What are the indications and contraindications for surgical resection of primary liver cancer?
Pedagogical considerations: The primary purpose of this theoretical teaching phase is to ensure students grasp the essential medical knowledge needed to understand the complexities of primary liver cancer. Through interactive discussions and case-based scenarios, students are encouraged to apply theoretical knowledge to clinical situations. The guiding questions are designed to challenge students to think critically, analyze clinical data, and make informed decisions based on current medical guidelines. By exploring both diagnostic and therapeutic strategies, this section aims to integrate theory with clinical practice, preparing students for real-world decision-making in the treatment of primary liver cancer. The concepts discussed in this part will directly feed into the clinical clerkship-class, where students will observe and participate in patient care.
Clerkship-class
The primary goal of the clinical practice phase is to allow students to directly observe and engage in the management of patients with primary liver cancer. This includes the process of diagnosing HCC, interpreting diagnostic imaging, formulating treatment plans, and understanding patient management strategies in the clinical setting. Students will apply the knowledge from the theoretical-class to real clinical situations and gain insight into the decision-making processes that clinicians use.
Clinical observation: Students will observe patients in a liver surgery or hepatology ward, where they can interact with patients diagnosed with primary liver cancer. This may include observing medical history taking, physical examinations, diagnostic procedures (e.g., ultrasound and CT scans), and discussions of treatment options (e.g., surgical resection, liver transplantation, and locoregional therapies).
Case discussions: Students will participate in multidisciplinary team (MDT) meetings, where they will review patient cases of primary liver cancer with senior clinicians. This provides an opportunity for students to witness clinical decision-making and the integration of various diagnostic and treatment modalities.
Clinical skill training: Students will practice clinical skills relevant to liver cancer diagnosis and management, such as conducting liver physical exams, interpreting liver function tests, and performing imaging-guided procedures (e.g., biopsy or ablation) under supervision. Students will also be trained to assess liver function and identify common complications of HCC, such as portal hypertension or ascites.
Patient interaction: Students will interact with patients in a supervised setting to gather clinical histories, ask relevant questions about risk factors (e.g., chronic hepatitis B/C virus infection and alcohol use), and engage in basic patient education about HCC management. They will also observe the impact of the disease on patients’ quality of life and psychosocial aspects.
Pedagogical considerations: Clinical practice in the “primary liver cancer” chapter focuses on bridging the gap between classroom learning and real-world clinical practice. It allows students to observe, engage with, and manage patients diagnosed with primary liver cancer in a supervised environment. Through hands-on experience and direct patient care, students will develop essential clinical skills, improve their diagnostic and decision-making abilities, and understand the multidisciplinary approach to managing HCC. This phase is essential in preparing students for the complexities of clinical practice, fostering professionalism, empathy, and teamwork, all critical components of the New Medicine educational framework.
Post-class
The post-class activities are designed to reinforce and extend the learning experience from the theory lesson, helping students apply what they’ve learned to real-world scenarios and prepare for the clinical practice phase.
Post-class case study: After the class, students are provided with a case study of a patient with primary liver cancer. They are asked to apply diagnostic and treatment approaches discussed in class to the case.
Reflection essay: Students write a reflection essay where they discuss their understanding of HCC, its treatment options, and how they would manage the case based on current clinical guidelines.
Questions: Based on the case study, how would you approach the diagnosis and staging of primary liver cancer? What treatment options would you consider for this patient, and why? Reflecting on the class, what is the most challenging aspect of diagnosing and treating HCC, and how would you overcome it in clinical practice?
Pedagogical considerations: The post-class activities are intended to help students synthesize and apply the knowledge gained during the lecture. The case study encourages critical thinking and decision-making, while the reflection essay allows students to consolidate their learning and self-assess their understanding of the topic.
CBL teaching
In the CBL teaching process, methods such as discussion and flipped classroom have been employed. The utilization of online real-time interactive systems, including the Ruijin Hospital Teaching Center App and Chaoxing Learning Platform, can enhance the classroom teaching atmosphere, increase student engagement, and make the entire learning process more dynamic. Students are divided into groups of 5–6, and they will proceed step by step to complete discussions and interactions based on the designed case and the structured questions, until the entire case-based teaching is concluded.
Teaching outcomes and evaluations
Students’ achievement and learning evaluations
To objectively assess the achievement of teaching objectives, a multifaceted and multidimensional evaluation approach is required for different sections, including pre-class, theoretical-class, clerkship-class and post-class. The evaluation content includes both process evaluation and formative evaluation. Specific evaluation details are presented in Table 1.
Evaluation for the learning of primary liver cancer.
| Teaching section | Evaluation methods | Points (100 in total) | Teaching objectives |
|---|---|---|---|
| Pre-class | Pre-class quizzes | 5 | b, d |
| Completion of online learning resources | 10 | a–d | |
| Theoretical-class | In-class participation | 5 | a, d, e |
| Case analysis assignments | 5 | b–d | |
| Midterm written test | 10 | a, b, d | |
| Clerkship-class | Direct observation | 10 | c–e |
| Case logbooks | 10 | d–f | |
| Oral case presentations | 5 | c–f | |
| Peer discussion performance | 10 | f | |
| Post-class | Post-class reflection essays | 5 | f |
| Post-class quizzes | 10 | b–e | |
| CBL | Discussions (participation, capacity to access information, ability to cooperate and communicate) | 10 | b–d |
| Answers of questions | 5 | b–f |
-
CBL, case-based learning.
The objective of the online pre-class quizzes and completion of online learning resources is to encourages active engagement with learning materials and preparation for classroom discussions. A real-time response system (e.g., clickers) is used to assess students’ participation in discussions about clinical manifestations, diagnostic criteria, and decision-making scenarios, promoting active learning and ensuring real-time engagement during theoretical lectures. Case analysis assignments is used to assess critical thinking and application of knowledge in case-based contexts. Multiple-choice questions, short answers, and problem-solving scenarios can be used to evaluate understanding of theoretical concepts and help comprehensively evaluate knowledge acquisition and retention of the students. Direct observation is applied to evaluate students’ clinical skills, such as conducting physical examinations, presenting patient cases, and interpreting diagnostic tests, using standardized checklists. Logbooks and case presentations encourage self-reflection. Assessment of participation in clerkship-class discussion develops collaborative learning skills through peer interactions. Gathering feedback from supervising clinicians, peers, and even patients (where appropriate) on students’ clinical skills, teamwork, and professionalism will provide a holistic evaluation of clinical competence and interpersonal skills through multi-source feedback. Post-class reflection essays promote self-directed learning by requiring students to reflect on their knowledge gaps and learning progress. Evaluation methods for CBL incorporate formative assessments (e.g., discussion participation) to guide learning and summative assessments (e.g., answers of questions) to evaluate overall achievement of the students.
To evaluate the feasibility and effectiveness of the clinical theory and clerkship synchronization teaching model for the “primary liver cancer” chapter under the New Medicine framework, a quasi-experimental study was conducted, comparing the proposed model with traditional teaching methods. Two groups of fourth-year clinical medicine undergraduate students were studied: an intervention group (synchronization class, Syn-class) using the new model and a control group (conventional class, Con-class) taught through traditional lecture-based methods. Syn-class group consisted 23 students, while the Con-class group consisted 30 students. The study involves post-class assessments to measure theoretical knowledge through written exams.
With regard to the acquisition of the fundamental knowledge of primary liver cancer, particularly in terms of performance on the post-class quiz, the class that employed the novel teaching model demonstrated significantly higher scores than the class that did not (Tables 2 and 3)
Statistical results of pre-class quizzes.
| Class | No. of students | Highest score | Lowest score | Average score | Standard deviation | p-Value |
|---|---|---|---|---|---|---|
| Syn-class | 23 | 5 | 2 | 3.8 | 0.7 | 0.58 |
| Con-class | 30 | 5 | 2 | 3.7 | 0.6 |
Statistical results of post-class quizzes.
| Class | No. of students | Highest score | Lowest score | Average score | Standard deviation | p-Value |
|---|---|---|---|---|---|---|
| Syn-class | 23 | 10 | 7 | 8.8 | 0.8 | <0.001 |
| Con-class | 30 | 9 | 5 | 7.2 | 0.9 |
Students’ feedback and teaching evaluations
Based on the results of students’ feedback questionnaire, the self-improvement ratings were found to be significantly higher in classes that employed the teaching model described above (Table 4).
Survey results of the questionnaire.
| Students’ achievement | Questionnaire content | Statistical results, % | |||||
|---|---|---|---|---|---|---|---|
| Satisfied | Neutral | Not satisfied | |||||
| Syn-class | Con-class | Syn-class | Con-class | Syn-class | Con-class | ||
| Attitude | The instructional process has been instrumental in fostering a professional demeanor in the management of liver cancer | 83 | 60 | 13 | 25 | 4 | 15 |
| The course has underscored the significance of interdisciplinary cooperation in addressing primary liver cancer | 83 | 55 | 17 | 35 | 0 | 10 | |
| My ethical awareness in the treatment of patients with primary liver cancer has been significantly enhanced through this course | 91 | 52 | 9 | 30 | 0 | 18 | |
| The pedagogical approach has fostered an empathetic and patient-centric mindset during case analyses and clinical engagements | 87 | 60 | 9 | 28 | 4 | 12 | |
| Skill | The practical sessions have markedly honed my skills in conducting liver-specific physical examinations | 83 | 43 | 17 | 37 | 0 | 20 |
| I am now adept at interpreting diagnostic instruments, including imaging studies and AFP levels, which are crucial for liver cancer diagnosis | 83 | 52 | 13 | 33 | 4 | 15 | |
| This course has bolstered my capacity to devise personalized treatment plans for primary liver cancer tailored to individual patient needs | 87 | 45 | 13 | 30 | 0 | 25 | |
| My decision-making prowess in the selection of surgical and non-surgical interventions has been considerably strengthened through the course’s methodology | 87 | 43 | 9 | 35 | 4 | 22 | |
| Knowledge | The course has delivered a comprehensive grasp of the pathophysiology and epidemiology underlying primary liver cancer | 87 | 52 | 13 | 33 | 0 | 15 |
| I am highly satisfied with the clarity provided in understanding the diagnostic and staging protocols for primary liver cancer | 87 | 47 | 13 | 35 | 0 | 18 | |
| My knowledge of cutting-edge treatment strategies, such as ALPPS and conversion therapy, has been significantly deepened through the curriculum | 83 | 50 | 13 | 30 | 4 | 20 | |
| The seamless integration of theoretical and practical elements has empowered me to effectively apply my knowledge in real-world clinical settings | 91 | 42 | 9 | 33 | 0 | 25 | |
-
AFP, alpha-fetoprotein; ALPPS, associating liver partition and portal vein ligation for staged hepatectomy.
Teachers can use evaluation results to continuously refine and enhance their teaching design by analyzing student performance, engagement, and feedback. Quantitative data, such as pre-class quiz and midterm written test scores, can help identify areas where students struggled, prompting adjustments in instructional strategies or the depth of content covered. Qualitative feedback from surveys and focus group discussions can provide insights into students’ learning experiences, highlighting the effectiveness of teaching methods and identifying potential gaps. Based on these findings, teachers can revise pre-class materials to make them more accessible, incorporate more interactive elements during theoretical-class sessions, or adapt clinical practice activities to better align with students’ needs. Additionally, feedback from peer observations or teaching assistants can offer a broader perspective, enabling teachers to address overlooked issues. This iterative process ensures that the teaching design evolves to meet learning objectives effectively, enhances student engagement, and maintains alignment with the educational goals of the New Medicine framework.
Discussion
The New Medicine framework emphasizes integrating basic medical knowledge with clinical practice to cultivate highly skilled, innovative, and application-oriented medical professionals [1], 2]. Students in traditional medical education often face challenges in applying theoretical knowledge to real-world clinical scenarios. Synchronous teaching ensures that theoretical concepts are immediately reinforced and contextualized through clinical exposure, enhancing understanding and retention. Combining theoretical learning with clinical practice helps students understand the patient’s journey from diagnosis to treatment, fostering empathy and communication skills. By synchronizing theory and practice, students develop critical thinking, clinical reasoning, and decision-making skills essential for modern healthcare [3], 5]. Advances in medical technology and evolving disease patterns, such as the increasing prevalence of chronic conditions like liver cancer, require physicians to be adept at integrating new knowledge into clinical practice. Synchronous teaching ensures students are well-prepared to meet these demands. However, the student-to-faculty ratio in this teaching reform is approximately 1:5 to 1:6, which demands a high number of teachers, especially clinical instructors. Given the already heavy workload of clinical work, this model is currently more suitable for small-class teaching or medical schools with abundant faculty resources.
This teaching design integrates OBE objectives, innovative content, and clinical theory-practice synchronization. It responds to the evolving demands of modern medical education, emphasizing interdisciplinary knowledge, practical competence, and patient-centered care [31]. Traditional textbook content has been restructured to address knowledge gaps and incorporate advancements in liver cancer management, including epidemiological trends, novel diagnostic tools, and emerging treatment modalities. Students gain a holistic understanding through interactive teaching models, such as pre-class preparation with targeted readings and videos, theoretical lectures enriched by case-based learning, and clinical clerkships emphasizing hands-on practice. For instance, the inclusion of cutting-edge techniques like ALPPS and conversion therapy, combined with the historical contributions of pioneers in Chinese liver surgery, equips students with both technical expertise and a deeper appreciation of the discipline’s evolution. This approach ensures students meet cognitive, psychomotor, and affective learning objectives. For example, they learn to interpret imaging for liver cancer staging, understand treatment complexities, and reflect on ethical dimensions like equity in healthcare. Post-class activities, such as case studies and reflective essays, reinforce learning, encourage self-assessment, and promote critical thinking. Through this design, students are empowered to translate theoretical knowledge into clinical practice effectively, fostering competence, empathy, and interdisciplinary collaboration [2].
The results of the evaluation indicated that students demonstrated high levels of satisfaction with the clinical theory and clerkship synchronization teaching model, with marked improvements in their learning outcomes. Student feedback showed higher satisfaction and perceived self-improvement in classes that utilized this model, emphasizing its success in fostering active learning and clinical competence. This multifaceted approach enhanced students’ understanding of primary liver cancer and improved their clinical reasoning and decision-making skills. Notably, students’ scores on post-class evaluations and clinical skill assessments were significantly higher than those in the traditional lecture-based control group, highlighting the effectiveness of the pre-class and synchronous learning design in ensuring mastery of essential knowledge and skills. The integration of feedback mechanisms further ensured that the teaching model was continuously refined to meet students’ learning needs. The findings affirm that this innovative model enhances learning outcomes by integrating theory and practice, promoting critical thinking, and equipping students with skills necessary for modern medical practice. However, students who participated in the teaching model reform have not yet entered their professional careers, it is currently not possible to objectively evaluate the long-term impact of this teaching model on the careers of medical students. Follow-up surveys and evaluations will be conducted in the future research.
The teaching evaluations also demonstrated improvements in students’ learning outcomes, engagement, and confidence. Students provided overwhelmingly positive feedback, with high ratings for the model’s ability to bridge theoretical learning and clinical application. They expressed appreciation for the interactive and integrated nature of the teaching process, particularly the use of case-based learning, pre-class preparation, and hands-on clinical practice. Teachers received constructive feedback, which was used to refine the instructional methods further, ensuring the model remained responsive to students’ needs. This feedback-driven approach not only improved the overall teaching quality but also enhanced the learning environment, aligning it with the goals of New Medicine education. The outcomes underscore the model’s success in fostering a dynamic, student-centered, and clinically relevant learning experience.
Conclusions
The novel teaching design of this study equips students with a solid foundation in both theoretical knowledge and practical skills. The integration of traditional surgical education with modern advancements prepares students to meet the challenges of contemporary medical practice. The synchronized model of clinical theory and clerkship enhances students’ ability to apply classroom learning to real-world clinical scenarios. The emphasis on student-centered learning, ethical considerations, and the importance of multidisciplinary collaboration aligns with the core principles of New Medicine, ensuring that graduates are not only technically proficient but also equipped with the professional and empathetic qualities necessary for holistic patient care. This teaching design for the “primary liver cancer” chapter represents a comprehensive and forward-thinking approach to surgical education within the New Medicine paradigm.
Acknowledgments
I extend my deepest gratitude to my mentors, Professor Weiguo Hu and Professor Ren Zhao, for their guidance and affirmation in my research.I would also like to express my sincere appreciation to the technical service staffs, Zhenye Gong, Qian Gu, and Shixiao Wang, for their assistance and support in the research.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: Feng Ye has made a substantial intellectual contribution to the design and has drafted the work; Qiang Cai has participated in teaching design and specific teaching work and has reviewed and revised the work; Yuan Qiao has made a substantial intellectual and practical contribution to the conception and has reviewed the work; Xiaoli Wang has made a substantial intellectual and practical contribution to the design and revised the work critically for important intellectual content. Xiaoyong Gong has made a substantial intellectual contribution to the acquisition and analysis of data for the work of publication; Jiajun Ren has made a substantial practical contribution to the analysis and interpretation of data for the work of publication; Ruixin Sun has made a substantial intellectual contribution to the conception and has reviewed the work; Chang Liu has made a substantial intellectual and practical contribution to the design and revised the work critically for important intellectual content. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interests: The authors state no conflict of interest.
-
Research funding: This research was supported by the Course Ideology Special Funding of the Center for Teaching and Learning Development at Shanghai Jiao Tong University [grant number CTLD24AIP0022].
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Han, L, Wang, Z, Zhou, X, Guo, X. Embarking on the era in new medicine: reshaping the systems of medical education and knowledge. Global Med Educ 2024;1:3–12. https://doi.org/10.1515/gme-2024-0005.Suche in Google Scholar
2. Guo, X. Evolving landscapes in global medical education: navigating challenges and embracing innovation. Global Med Educ 2024;1:1–2. https://doi.org/10.1515/gme-2024-0003.Suche in Google Scholar
3. Vallée, A, Blacher, J, Cariou, A, Sorbets, E. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res 2020;22:e16504. https://doi.org/10.2196/16504.Suche in Google Scholar PubMed PubMed Central
4. Donkin, R, Yule, H, Fyfe, T. Online case-based learning in medical education: a scoping review. BMC Med Educ 2023;23:564. https://doi.org/10.1186/s12909-023-04520-w.Suche in Google Scholar PubMed PubMed Central
5. Bransen, D, Driessen, EW, Sluijsmans, DMA, Govaerts, MJB. How medical students co-regulate their learning in clinical clerkships: a social network study. BMC Med Educ 2022;22:193. https://doi.org/10.1186/s12909-022-03259-0.Suche in Google Scholar PubMed PubMed Central
6. Satapathy, P, Hermis, AH, Rustagi, S, Pradhan, KB, Padhi, BK, Sah, R. Artificial intelligence in surgical education and training: opportunities, challenges, and ethical considerations – correspondence. Int J Surg 2023;109:1543–4. https://doi.org/10.1097/js9.0000000000000387.Suche in Google Scholar PubMed PubMed Central
7. Ghaddaripouri, K, Mousavi Baigi, SF, Abbaszadeh, A, Mazaheri Habibi, MR. Attitude, awareness, and knowledge of telemedicine among medical students: a systematic review of cross-sectional studies. Health Sci Rep 2023;6:e1156. https://doi.org/10.1002/hsr2.1156.Suche in Google Scholar PubMed PubMed Central
8. Mousavi Baigi, SF, Sarbaz, M, Ghaddaripouri, K, Ghaddaripouri, M, Mousavi, AS, Kimiafar, K. Attitudes, knowledge, and skills towards artificial intelligence among healthcare students: a systematic review. Health Sci Rep 2023;6:e1138. https://doi.org/10.1002/hsr2.1138.Suche in Google Scholar PubMed PubMed Central
9. Vashe, A, Devi, V, Pallath, V, Abraham, RR, Kamath, A. Development and validation of Manipal inventory for curriculum evaluation (MICE): a comprehensive tool for evaluation of hybrid medical curriculum. Bangladesh J Med Sci 2023;22:47–56. https://doi.org/10.3329/bjms.v22i1.61863.Suche in Google Scholar
10. Li, P, Lan, X, Ren, L, Xie, X, Xie, H, Liu, S. Research and practice of the BOPPPS teaching model based on the OBE concept in clinical basic laboratory experiment teaching. BMC Med Educ 2023;23:882. https://doi.org/10.1186/s12909-023-04822-z.Suche in Google Scholar PubMed PubMed Central
11. Oh, JH, Sinn, DH. Multidisciplinary approach for hepatocellular carcinoma patients: current evidence and future perspectives. J Liver Cancer 2024;24:47–56. https://doi.org/10.17998/jlc.2024.02.27.Suche in Google Scholar PubMed PubMed Central
12. Seif El Dahan, K, Reczek, A, Daher, D, Rich, NE, Yang, JD, Hsiehchen, D, et al.. Multidisciplinary care for patients with HCC: a systematic review and meta-analysis. Hepatol Commun 2023;7:e0143. https://doi.org/10.1097/hc9.0000000000000143.Suche in Google Scholar
13. Rathore, E, Riaz, F, Habib, N, Anjum, O, Zahra, R, Salahuddin, MB. A comparison between teacher centered and student centered medical education approach: an experimental research. Pak J Med Health Sci 2022;16:104–6. https://doi.org/10.53350/pjmhs22169104.Suche in Google Scholar
14. Momen, A, Ebrahimi, M, Hassan, AM. Importance and implications of theory of Bloom’s taxonomy in different fields of education. Cham: Springer; 2023:515–25 pp.10.1007/978-3-031-20429-6_47Suche in Google Scholar
15. Shi, J, Cao, M, Wang, Y, Bai, F, Lei, L, Peng, J, et al.. Is it possible to halve the incidence of liver cancer in China by 2050? Int J Cancer 2021;148:1051–65. https://doi.org/10.1002/ijc.33313.Suche in Google Scholar PubMed
16. Ye, F, Ma, D, Gong, XY, Yang, YC, Chen, YJ. Development and validation of risk score for predicting spontaneous rupture of hepatocellular carcinoma. Ann Surg Treat Res 2020;99:268. https://doi.org/10.4174/astr.2020.99.5.268.Suche in Google Scholar PubMed PubMed Central
17. Rumgay, H, Ferlay, J, de Martel, C, Georges, D, Ibrahim, AS, Zheng, R, et al.. Global, regional and national burden of primary liver cancer by subtype. Eur J Cancer 2022;161:108–18. https://doi.org/10.1016/j.ejca.2021.11.023.Suche in Google Scholar PubMed
18. Lin, L, Yan, L, Liu, Y, Qu, C, Ni, J, Li, H. The burden and trends of primary liver cancer caused by specific etiologies from 1990 to 2017 at the global, regional, national, age, and sex level results from the global burden of disease study 2017. Liver Cancer 2020;9:563–82. https://doi.org/10.1159/000508568.Suche in Google Scholar PubMed PubMed Central
19. Karagiannakis, DS. Systemic treatment in intermediate stage (barcelona clinic liver cancer-B) hepatocellular carcinoma. Cancers 2023;16:51. https://doi.org/10.3390/cancers16010051.Suche in Google Scholar PubMed PubMed Central
20. Trevisani, F, Vitale, A, Kudo, M, Kulik, L, Park, JW, Pinato, DJ, et al.. Merits and boundaries of the BCLC staging and treatment algorithm: learning from the past to improve the future with a novel proposal. J Hepatol 2024;80:661–9. https://doi.org/10.1016/j.jhep.2024.01.010.Suche in Google Scholar PubMed
21. Głowska-Ciemny, J, Szymański, M, Kuszerska, A, Malewski, Z, von Kaisenberg, C, Kocyłowski, R. The role of alpha-fetoprotein (AFP) in contemporary oncology: the path from a diagnostic biomarker to an anticancer drug. Int J Mol Sci 2023;24:2539. https://doi.org/10.3390/ijms24032539.Suche in Google Scholar PubMed PubMed Central
22. Kim, DY, Toan, BN, Tan, CK, Hasan, I, Setiawan, L, Yu, ML, et al.. Utility of combining PIVKA-II and AFP in the surveillance and monitoring of hepatocellular carcinoma in the Asia-Pacific region. Clin Mol Hepatol 2023;29:277–92. https://doi.org/10.3350/cmh.2022.0212.Suche in Google Scholar PubMed PubMed Central
23. Norman, JS, Li, PJ, Kotwani, P, Shui, AM, Yao, F, Mehta, N. AFP-L3 and DCP strongly predict early hepatocellular carcinoma recurrence after liver transplantation. J Hepatol 2023;79:1469–77. https://doi.org/10.1016/j.jhep.2023.08.020.Suche in Google Scholar PubMed PubMed Central
24. Zhou, J, Sun, H, Wang, Z, Cong, W, Zeng, M, Zhou, W, et al.. Guidelines for the diagnosis and treatment of primary liver cancer (2022 edition). Liver Cancer 2023;12:405–44. https://doi.org/10.1159/000530495.Suche in Google Scholar PubMed PubMed Central
25. Duan, S. Dr. Wu Mengchao (1922–2021), founder and pioneer of Chinese hepatobiliary surgery. J Med Biogr 2024:9677720241273622. https://doi.org/10.1177/09677720241273622.Suche in Google Scholar PubMed
26. Tang, Z. Elimination plus transformation – Chinese and Western Medicine integration brings hope to protracted war on cancer. Chin J Integr Med 2018;24:563–7. https://doi.org/10.1007/s11655-018-2990-6.Suche in Google Scholar PubMed
27. Wang, Z, Ren, Z, Chen, Y, Hu, J, Yang, G, Yu, L, et al.. Adjuvant transarterial chemoembolization for HBV-related hepatocellular carcinoma after resection: a randomized controlled study. Clin Cancer Res 2018;24:2074–81. https://doi.org/10.1158/1078-0432.ccr-17-2899.Suche in Google Scholar
28. Zhu, P, Liao, W, Zhang, WG, Chen, L, Shu, C, Zhang, ZW, et al.. A prospective study using propensity score matching to compare long-term survival outcomes after robotic-assisted, laparoscopic, or open liver resection for patients with BCLC stage 0-A hepatocellular carcinoma. Ann Surg 2023;277:e103–11. https://doi.org/10.1097/sla.0000000000005380.Suche in Google Scholar
29. Lang, H, de Santibañes, E, Schlitt, HJ, Malagó, M, van Gulik, T, Machado, MA, et al.. 10th anniversary of ALPPS – lessons learned and quo vadis. Ann Surg 2019;269:114–9. https://doi.org/10.1097/sla.0000000000002797.Suche in Google Scholar PubMed
30. Zhou, H, Song, T. Conversion therapy and maintenance therapy for primary hepatocellular carcinoma. Biosci Trends 2021;15:155–60. https://doi.org/10.5582/bst.2021.01091.Suche in Google Scholar PubMed
31. Guo, Z, Bo, L, Zhao, C, Cheng, M. Research and practice on connotation construction and implementation of roadmap of “New Medicine” in local medical colleges by big data analysis. Front Soc Sci Technol 2023;5:1–6.10.25236/FSST.2023.050501Suche in Google Scholar
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


