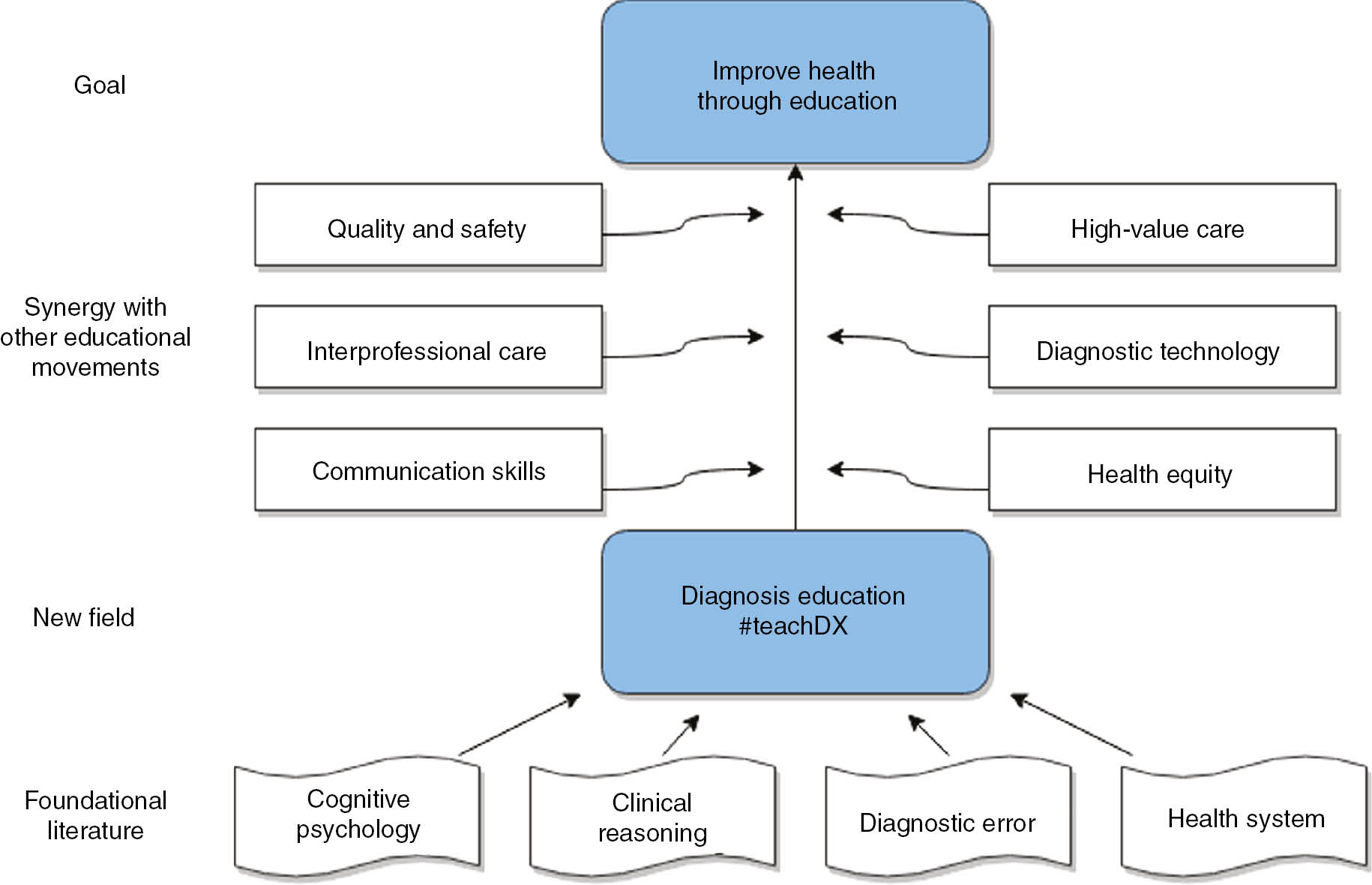
There has been a longstanding need to improve how we teach diagnosis in health professions education programs. The substantial progress in the overlapping disciplines of clinical reasoning, cognitive psychology, and diagnostic error has yet to be translated into widespread curricular innovations. The methods we use to teach diagnosis to today’s learners are strikingly similar to the approach used for decades: transfer of knowledge and “dwell time” in the clinical environment. In this special issue of Diagnosis, we celebrate scholars who have forged new approaches to promote diagnostic excellence and the reduction of diagnostic error through education. Their work represents the cutting edge of the emerging field of diagnosis education (Figure 1).
Diagnosis Education in the landscape of Health Professions Education – built on many areas of study, diagnosis education will be most effective in synergy with other emerging fields.
Three innovation reports in this issue integrate technology with traditional case-based learning. Kinnear and colleagues describe a workshop that introduces foundational concepts of Bayesian reasoning and demonstrates how to make these concepts actionable when seeing patients by using smartphone apps [1]. Goyal and colleagues describe how a time-honored tradition in medical education – morning report – can make clinical reasoning explicit to learners and be enhanced and retooled to incorporate point-of-care ultrasound [2]. Their report illustrates how educators can integrate new technology with bedside medicine while engaging the patient in the diagnostic process. Altabbaa and colleagues examine an underused resource in diagnosis education: simulation [3]. The authors present a novel scenario design and debriefing process to educate learners about cognitive and systems pitfalls in diagnosis.
Nearly all innovations, however, share one fundamental, rate-limiting resource – teachers who are prepared to implement them. Grubenhoff and colleagues identify knowledge gaps among faculty about cognitive biases as well as their limited comfort in discussing diagnostic errors [4]. Schaye and colleagues describe a faculty development program in which teachers learned clinical reasoning concepts and then trialed their new skills with immediate feedback [5]. The authors go beyond self-efficacy measures and show a significant improvement of teaching performance through a group objective structured teaching exercise (GOSTE). This report underscores how we must apply the same rigor to evaluating faculty development programs that we do to evaluating curricula for learners. Iyer and colleagues remind us of the importance of developing residents as clinicians and teachers through their curriculum on clinical reasoning [6]. Clinicians have to navigate diagnostic uncertainty with their patients, but clinicians-educators must also discuss diagnostic uncertainty with their learners. In their commentary, Santhosh and colleagues identify challenges to addressing diagnostic uncertainty and propose a novel framework to aid learners, faculty, and patients in maneuvering through uncertainty in the diagnostic process [7].
All fields of study are built on a foundation of basic science which generates new theories and insights. McBee and colleagues used think aloud protocols to delineate the clinical reasoning tasks of medical students and found that medical students verbalize reasoning tasks in purposeful but non-sequential patterns [8]. This finding suggests that effective clinical reasoning instruction may involve modeling and encouraging multiple pathways when solving a diagnostic problem. All theories need to be subjected to rigorous testing. Braun and colleagues conducted a series of experiments suggesting that scaffolding in diagnostic reasoning is ineffective at improving medical students’ decision-making [9]. Kilian and colleagues question the effectiveness of a checklist, which is one form of the “diagnostic timeout” – a mainstay of many patient safety initiatives [10]. While these studies are not definitive, they do emphasize our field’s obligation to establish which theory-derived practices are effective by empirical study rather than by belief or anecdote alone.
Diagnosis education curricula are developed with the goal of improving learners’ diagnostic performance, and this too requires empiric testing. Bonifacino and colleagues created a brief clinical reasoning curriculum for internal medicine clerkship students, and in a pseudo-randomized design, show that a fundamental workplace activity for all medical students – documenting diagnostic reasoning in the admission note – was improved among students who participated in the curriculum [11]. Howard-Anderson and colleagues extend the study of diagnosis to a real-world setting, showing that the diagnostic steps medical residents take when evaluating a febrile patient at night are heavily influenced by sign-out instructions from a colleague, highlighting how diagnosis, like much of medicine, is a social process [12].
Teachers can find inspiration and synergy with other fields that are not traditionally aligned with diagnosis and clinical reasoning education. Lewis and colleagues highlight the limited teaching about diagnostic error in emergency medicine training programs and suggest that diagnostic error can be integrated with medical liability, quality assurance, and risk management instruction [13]. Radhakrishnan and colleagues apply the novel lens of a manufacturing and quality improvement paradigm (lean) to describe the diagnostic process for medical students [14]. Viewing diagnosis through the perspectives of different fields may prove to be a highly effective way to instill and reinforce diagnostic excellence and error mitigation.
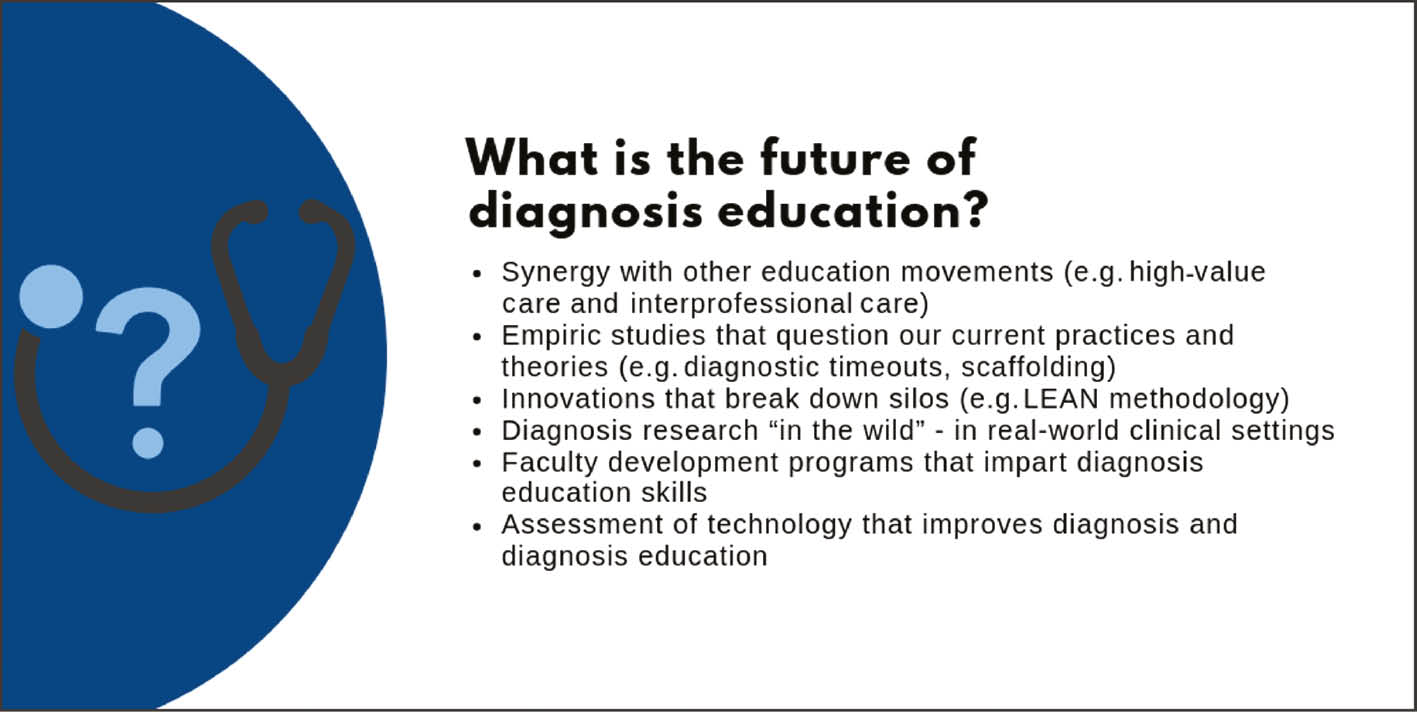
What diagnosis education articles do we hope to see in the future? (Figure 2). We eagerly anticipate expansion of many of the ideas presented in this special issue. However, we must ensure that teaching and learning about diagnosis is not a niche topic for which a committed few advocate amidst the many other worthy competing interests in health professions education. Diagnosis education is an interdisciplinary and evolving field that has origins in the clinical reasoning, cognitive psychology, diagnostic error, and health systems literature. Our community’s ideas for improving diagnosis will reach more learners and have more impact if we forge curricular collaborations with other successful education movements, such as high-value care, interprofessional education, and quality and safety. We must join forces with other groups that share the same goal of improving health through education.
Future directions for diagnosis education – we must continue to push the field forward through novel innovations and rigorous study.
Certainly, there is much work to do – diagnostic errors remain far too common. We hope the work of the teachers and scholars featured in this issue inspires and energizes our readers with the progress already being made.
Educational initiatives of the Society to Improve Diagnosis in Medicine (SIDM).
| – | Virtual patient cases for undergraduate medical education in partnership with Aquifer |
| – | Continuing professional development modules on diagnostic error in partnership with the American College of Physicians and the Society of Hospital Medicine |
| – | Consensus Curriculum on Diagnosis, funded by the Josiah H. Macy, Jr Foundation, to transform diagnosis education through a competency-based, interprofessional approach |
| – | Monthly #teachdx Twitter chats |
| – | Education Precourses at the Diagnostic Error in Medicine Conference |
| – | SIDM Assessment of Reasoning Tool |
| – | SIDM Clinical Reasoning Toolkit |
| – | SIDM Fellowship in Diagnostic Excellence |
More information available at www.improvediagnosis.org.
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: None declared.
Employment or leadership: None declared.
Honorarium: None declared.
References
1. Kinnear B, Hagedorn PA, Kelleher M, Ohlinger C, Tolentino J. Integrating Bayesian reasoning into medical education using smartphone apps. Diagnosis 2019;6:85–9. 10.1515/dx-2018-0065Suche in Google Scholar PubMed
2. Goyal A, Garibaldi B, Liu G, Desai S, Manesh R. Morning report innovation: case oriented report and exam skills. Diagnosis 2019;6:79–83.10.1515/dx-2018-0086Suche in Google Scholar PubMed
3. Altabbaa G, Raven AD, Laberge J. A simulation-based approach to training in heuristic clinical decision-making. Diagnosis 2019;6:91–9.10.1515/dx-2018-0084Suche in Google Scholar PubMed
4. Grubenhoff JA, Ziniel SI, Bajaj L, Hyman D. Pediatric faculty knowledge and comfort discussing diagnostic errors: a pilot survey to understand barriers to an educational program. Diagnosis 2019;6:101–7.10.1515/dx-2018-0056Suche in Google Scholar PubMed
5. Schaye V, Janjigian M, Hauck K, Shapiro N, Becker D, Lusk P, et al. A workshop to train medicine faculty to teach clinical reasoning. Diagnosis 2019;6:109–13.10.1515/dx-2018-0059Suche in Google Scholar PubMed
6. Iyer S, Goss E, Browder C, Paccione G, Arnsten J. Development and evaluation of a clinical reasoning curriculum as part of an Internal Medicine Residency Program. Diagnosis 2019;6:115–9.10.1515/dx-2018-0093Suche in Google Scholar PubMed
7. Santhosh L, Chou CL, Connor DM. Diagnostic uncertainty: from education to communication. Diagnosis 2019;6:121–6.10.1515/dx-2018-0088Suche in Google Scholar PubMed
8. McBee E, Blum C, Ratcliffe T, Schuwirth L, Polston E, Artino AR Jr, et al. Use of clinical reasoning tasks by medical students. Diagnosis 2019;6:127–35.10.1515/dx-2018-0077Suche in Google Scholar PubMed
9. Braun LT, Borrmann KF, Lottspeich C, Heinrich DA, Kiesewetter J, Fischer MR, et al. Scaffolding clinical reasoning of medical students with virtual patients: effects on diagnostic accuracy, efficiency, and errors. Diagnosis 2019;6:137–49.10.1515/dx-2018-0090Suche in Google Scholar PubMed
10. Kilian M, Sherbino J, Hicks C, Monteiro SD. Understanding diagnosis through ACTion: evaluation of a point-of-care checklist for junior emergency medical residents. Diagnosis 2019;6:151–6.10.1515/dx-2018-0073Suche in Google Scholar PubMed
11. Bonifacino E, Follansbee WP, Farkas AH, Jeong K, McNeil MA, DiNardo DJ. Implementation of a clinical reasoning curriculum for clerkship-level medical students: a pseudo-randomized and controlled study. Diagnosis 2019;6:165–72.10.1515/dx-2018-0063Suche in Google Scholar PubMed
12. Howard-Anderson J, Schwab KE, Chang S, Wilhalme H, Graber CJ, Quinn R. Internal medicine residents’ evaluation of fevers overnight. Diagnosis 2019;6:157–63.10.1515/dx-2018-0066Suche in Google Scholar PubMed PubMed Central
13. Lewis JJ, Rosen CL, Grossestreuer AV, Ullman EA, Dubosh NM. Diagnostic error, quality assurance, and medical malpractice/risk management education in emergency medicine residency training programs. Diagnosis 2019;6:173–8.10.1515/dx-2018-0079Suche in Google Scholar PubMed
14. Radhakrishnan NS, Singh H, Southwick FS. Teaching novice clinicians how to reduce diagnostic waste and errors by applying the Toyota Production System. Diagnosis 2019;6:179–85.10.1515/dx-2018-0081Suche in Google Scholar PubMed
©2019 Walter de Gruyter GmbH, Berlin/Boston
Artikel in diesem Heft
- Frontmatter
- Editorial
- Diagnosis education – an emerging field
- Technology in Diagnosis Education
- Morning report innovation: Case Oriented Report and Exam Skills
- Integrating Bayesian reasoning into medical education using smartphone apps
- A simulation-based approach to training in heuristic clinical decision-making
- Educators
- Pediatric faculty knowledge and comfort discussing diagnostic errors: a pilot survey to understand barriers to an educational program
- A workshop to train medicine faculty to teach clinical reasoning
- Development and evaluation of a clinical reasoning curriculum as part of an Internal Medicine Residency Program
- Diagnostic uncertainty: from education to communication
- Basic Science of Diagnosis Education
- Use of clinical reasoning tasks by medical students
- Scaffolding clinical reasoning of medical students with virtual patients: effects on diagnostic accuracy, efficiency, and errors
- Understanding diagnosis through ACTion: evaluation of a point-of-care checklist for junior emergency medical residents
- Studies of Diagnosis in Clinical Contexts
- Internal medicine residents’ evaluation of fevers overnight
- Implementation of a clinical reasoning curriculum for clerkship-level medical students: a pseudo-randomized and controlled study
- Integration with Other Fields
- Diagnostic error, quality assurance, and medical malpractice/risk management education in emergency medicine residency training programs
- Teaching novice clinicians how to reduce diagnostic waste and errors by applying the Toyota Production System
Artikel in diesem Heft
- Frontmatter
- Editorial
- Diagnosis education – an emerging field
- Technology in Diagnosis Education
- Morning report innovation: Case Oriented Report and Exam Skills
- Integrating Bayesian reasoning into medical education using smartphone apps
- A simulation-based approach to training in heuristic clinical decision-making
- Educators
- Pediatric faculty knowledge and comfort discussing diagnostic errors: a pilot survey to understand barriers to an educational program
- A workshop to train medicine faculty to teach clinical reasoning
- Development and evaluation of a clinical reasoning curriculum as part of an Internal Medicine Residency Program
- Diagnostic uncertainty: from education to communication
- Basic Science of Diagnosis Education
- Use of clinical reasoning tasks by medical students
- Scaffolding clinical reasoning of medical students with virtual patients: effects on diagnostic accuracy, efficiency, and errors
- Understanding diagnosis through ACTion: evaluation of a point-of-care checklist for junior emergency medical residents
- Studies of Diagnosis in Clinical Contexts
- Internal medicine residents’ evaluation of fevers overnight
- Implementation of a clinical reasoning curriculum for clerkship-level medical students: a pseudo-randomized and controlled study
- Integration with Other Fields
- Diagnostic error, quality assurance, and medical malpractice/risk management education in emergency medicine residency training programs
- Teaching novice clinicians how to reduce diagnostic waste and errors by applying the Toyota Production System

