Abstract
Objectives
Circumvallate placenta is a rare abnormality of placental shape. Current data indicates that a circumvallate placenta can be a risk factor for severe adverse obstetric and neonatal outcomes such as antepartum bleeding, premature delivery, oligohydramnios, intrauterine growth restriction and placental abruption. An unusual insertion of the umbilical cord can cause a reduction of perfusion and can also lead to pregnancy complications. However, the clinical significance of these pathoanatomical findings often remains unclear.
Case presentation
We report a case of a 22-year-old third gravida nullipara in 28+2 pregnancy weeks with a pathological cardiotocography (CTG) and a growth restricted fetus with oligohydramnios and pathological umbilical blood flow. Due to recurrent decelerations of fetal heart rate the baby was delivered via cesarean section. The examination of the placenta showed a circumvallate placenta and fixated umbilical cord mimicking a battledore insertion.
Conclusions
It can be concluded that circumvallate placenta may predispose to severe obstetric complications. Women with circumvallate placenta and abnormal cord insertion probably benefit from stringent follow ups in a specialized perinatal center. Histopathological examination of the placenta can be a diagnostic tool in women with recurrent obstetric complications.
Introduction
Circumvallate placenta is a morphological abnormality defined as a thickened placenta with a raised margin in an annular shape [1]. The prevalence is estimated to 1–7% [2]. Circumvallate placentae are a result of a membranous fold of chorion and amnion. In circumvallate placentae the chorionic plate is smaller than the basal plate which leads to an area of uncovered placenta where antepartum bleedings may occur [3].
Different authors described the antepartum diagnosis of circumvallate placenta by antenatal ultrasonography screening. Circumvallate placenta can lead to an atypical echogenicity, irregular cavities and an elevated placental margin []. Nevertheless, a placental abnormality is often undetected until postpartum gross examination of the placenta.
As data is inconsistent and large systematic trials are missing, the clinical significance of this pathoanatomical finding still remains unclear.
Different authors showed that circumvallate placenta is associated with vaginal bleeding, preterm rupture of the membranes, preterm delivery, and placental abruption, the need for emergency cesarean section and also for fetal and neonatal complications such as intrauterine growth restriction, neonatal death or admission to neonatal intensive care units. [8], [9], [10].
There is also recent data that shows that antenatally diagnosed circumvallate placenta has no impact on adverse obstetric or neonatal outcomes [11].
Nonetheless the significance of placental abnormalities for pregnancy complications and the monitoring of such risk pregnancies are still controversial and further research is needed.
Marginal (battledore) cord insertion has a prevalence of 7% and may also lead to pregnancy complications such as intrauterine growth retardation, fetal distress, intrauterine fetal demise and emergency cesarean delivery [12].
Case presentation
A 22-year-old third gravida nullipara was referred at 28+2 pregnancy weeks to our perinatal center with a pathological cardiotocography (CTG) with a deep deceleration of the fetal heart rate.
The patient previously had two late miscarriages at 17 and 20 weeks. She had no other significant medical or surgical history. The current pregnancy had been uneventful with no antenatal bleeding episodes. In a detailed second trimester screening at 21+1 weeks of gestation there were no signs of structural abnormalities. Placental shape and the fetal weight were normal. The cord insertion was concentric without signs for a velamentous insertion (Figure 1).
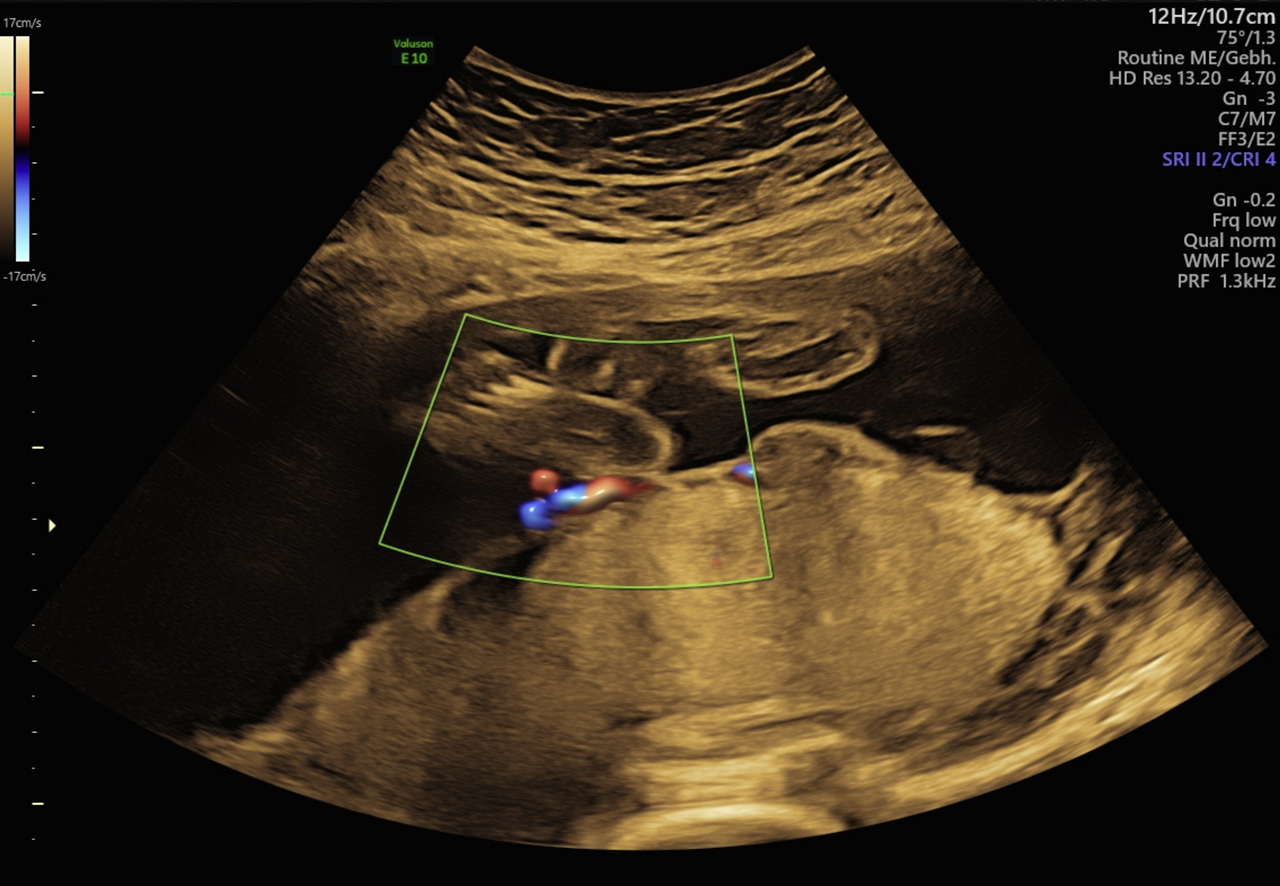
Examination of the cord insertion in 22+1 weeks: normal aspect.
The patient had no contractions, membranes were intact and the cervix was 4 cm and closed. Vital parameters and urine dipstick were normal. At the CTG monitoring the fetus showed periodic decelerations of the heart rate every 25 min without uterine contractions.
The ultrasound showed a growth restricted fetus with an estimated weight of 815 g (<third percentile) and oligohydramnios. Umbilical blood flow was reduced with an absent end-diastolic flow in the umbilical artery while the blood flow in the uterine artery and in the middle cerebral artery were normal. Fetal movements were present. The placenta appeared enlarged with a spherical shape.
The patient received antenatal steroid therapy for fetal lung maturation during continuous CTG monitoring. After a prolonged bradycardia on the CTG an emergency cesarean section in spinal anesthesia was performed without major complications.
The newborn, a boy of 815 g, had an APGAR score of 8/9/9 and an umbilical cord arterial pH of 7.21 and was admitted to the neonatal intensive care unit.
Gross examination of the placenta showed a thickened circumvallate placenta with a firm white annular margin. Beginning at the paracentral insertion, the umbilical cord was tightly fixated on the placental surface to the placental margin, at first glance mimicking a battledore insertion. The pathohistological examination showed an arrest of placental villi ripening, an amnion nodosum and increased growth of stromal syncytial buds.
We conducted an extended screening including tests for HIV, hepatitis B, hepatitis C, cytomegalovirus, coxsackievirus, parvovirus, varicella virus, rubella, Epstein-Barr virus, herpes simplex and also for Treponema pallidum and toxoplasma. The screening showed no abnormalities. SFlt/PlGF ratio was 189. The C-reactive protein was slightly increased at 15.4 mg/L.
All other parameters, especially the complete blood count and the transaminases, were normal.
The postpartum period of our patient was unremarkable. The neonate initially required airway support via CPAP and showed a stable growth and a good general development. After 105 days of intensive neonatal care the newborn was discharged from hospital.
Conclusions
We report a case of a growth restricted fetus caused by a circumvallate placenta as a rare finding which may be associated with further severe pregnancy complications. It can be diagnosed antepartum by ultrasound screening or as a visual diagnosis after birth (Figures 2 and 3).
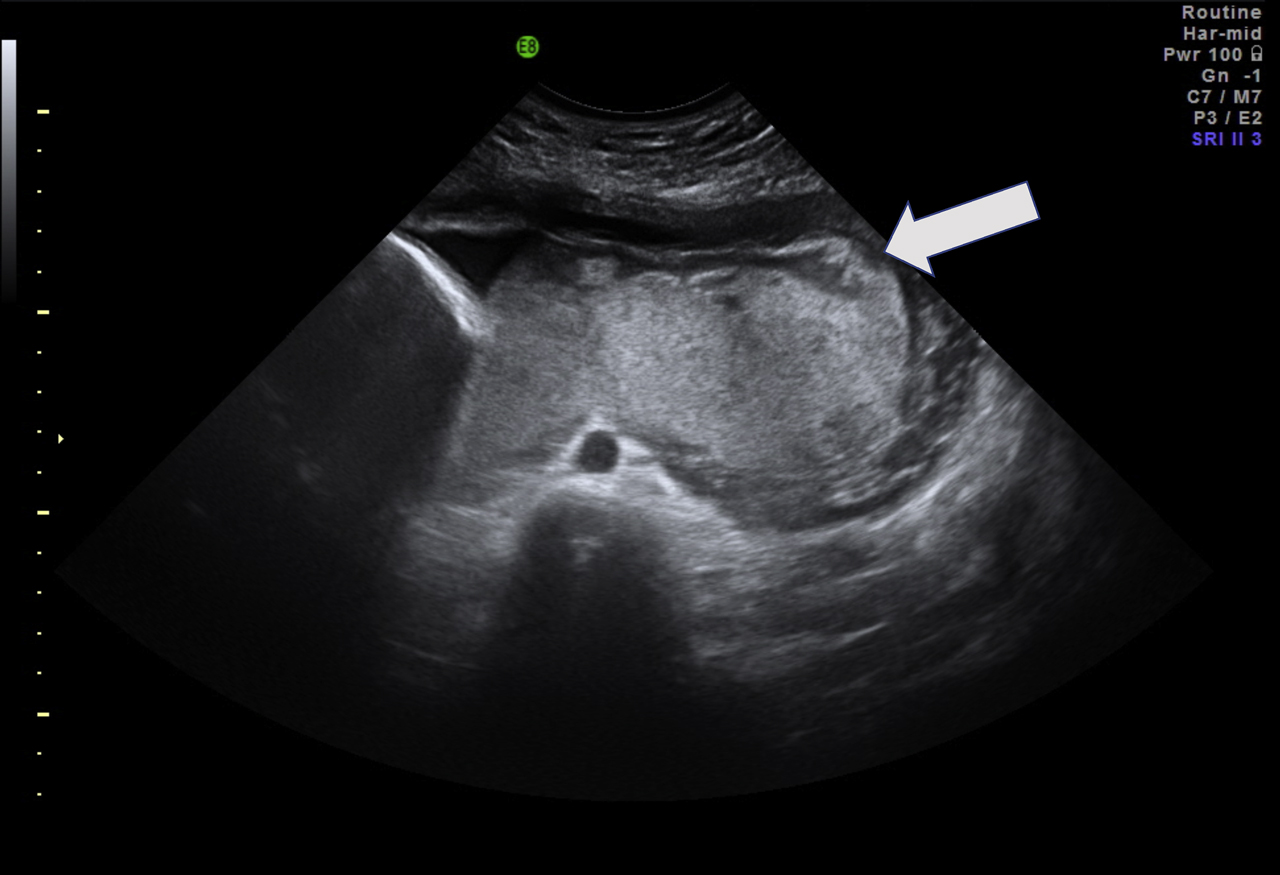
Thickened placenta with atypical echogenicity at 28+2 weeks of pregnancy. Arrow: circumvallate margin.

Postpartum examination of the placenta with firm annular margin (triangles) and fixated umbilical cord (arrow).
Women with a history of adverse pregnancy outcomes should be screened for placental abnormalities with two- or three-dimensional ultrasound during the second trimester. It has to be taken into consideration that ultrasound diagnosis can be difficult due to placental position or maternal overweight.
Radiographic features of the circumvallate placenta can be an abnormal placental thickness (>3 cm), a peripheral echodense rim or an irregular placental edge (placental “shelf”). Similar features can also be found in other placental abnormalities: The most important radiographic differential diagnosis is amnion sheets and amniotic bands.
Although circumvallate placenta is assumed to be a risk factor for adverse obstetric outcomes there is no evidence-based concept for the management of pregnancies with circumvallate placenta. Regular follow-ups at specialized centers and an early birth induction could probably be beneficial for pregnancy outcomes.
The department of obstetrics at Charité university hospital is one of the largest perinatal centers in Berlin and Germany. When dealing with high-risk pregnancies, placental function and the monitoring of fetal growth are some of the most important issues. In the case of an antenatally diagnosed isolated circumvallate placenta, a fetal growth assessment is performed every month. When growth restriction or a restricted fetal or placental blood flow occurs, ultrasound follow-ups are performed weekly, twice a week or even daily combined with a tracking of fetal heart rate.
The isolated finding of a circumvallate placenta does not lead to a cesarean section. Some of the complications linked to placental abnormalities, like sudden placental abruption, pathological fetal cardiotocography changes ore severe growth restriction often do.
Abnormal cord insertions such as battledore insertion have a prevalence of 7%. Cord insertion abnormalities are usually detected in early pregnancy weeks or at a first trimester screening. The clinical significance is still unclear but there are different trials pointing out a poor obstetric outcome due to marginal cord insertion [13].
There is no pathoanatomical term for a fixation of the umbilical cord to the placental surface, but the cross-section of the placenta and umbilical cord resembles the cross-section of a showerhead. It seems to be likely that the blood flow is severely affected by kinking at the insertion into the placental body (Figure 3) and may even lead to an absent end-diastolic blood flow in the umbilical artery.
The turbulent flow resulting of the kinking causes a loss of pressure and hence a reduction of peripheral perfusion of the placenta. Clinical data for the outcome of both abnormal placental shape and abnormal cord insertion is still missing, but an increase of adverse events may be likely.
Different infections in pregnancy can result in a fetal growth restriction and macroscopic abnormalities of placental appearance. Initially normal pregnancies with a sudden growth restriction and a placental enlargement should also lead to serological screening, especially for CMV and Syphilis [14], [15], [16].
When dealing with placental dysfunction, biomarkers such as Sflt/PlGF are used to predict adverse events and to monitor a pregnancy at risk. Circumvallate placentae also seem to be associated with reduced placental diffusing capacity which affects the Sflt/PlGF ratio. This may be a result of the thickness of tissue or a dysfunction of placental villi. Serial measurements of Sflt/PlGF ratio can probably be used to predict imminent placental insufficiency in patients with placental abnormalities.
Further clinical research concerning the role of biomarkers to predict complications related to pathoanatomical placental abnormalities is needed.
Conclusions
Placental abnormalities such as circumvallate placenta and abnormal cord insertions are rare but important due to potential severe pregnancy complications.
Women with antenatal diagnosis of circumvallate placenta probably benefit from regular checkups to monitor fetal growth, fetal blood flow and amniotic fluid. Although an evidence-based protocol for the management of pregnancies with placenta circumvallate is still missing, these pregnancies should be considered as high risk pregnancies and be admitted to specialized perinatal care centers.
The pathological and histological examination of macroscopic suspect placentae can supply further information about placental architecture and hopefully more insight into pathophysiological mechanisms, leading to a better risk management in future. In circumvallate placentas the pathologist should focus on altered vessels reducing the blood flow to the periphery of the placenta.
Research funding: None declared.
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Competing interests: Authors state no conflict of interest.
Informed consent: Informed consent was obtained from the patient and her husband.
Ethical approval: All procedures were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
1. Bumm, E. Grundriss zum Studium der Geburtshilfe. München: J.F. Bergmann-Verlag; 1922.Search in Google Scholar
2. Fox, H, Elston, CW. Pathology of the placenta. Major Probl Pathol 1978;7:1–491.10.1016/S0306-3356(21)00030-3Search in Google Scholar
3. Williams, JW. Placenta circumvallata. Am J Obstet Gynecol 1927;13:1–16. https://doi.org/10.1016/s0002-9378(27)90108-2.Search in Google Scholar
4. McCarthy, J, Thurmond, AS, Jones, MK, Sistrom, C, Scanlan, RM, Jacobson, SL, et al. Circumvallate placenta: sonographic diagnosis. J Ultrasound Med 1995;14:21–6. https://doi.org/10.7863/jum.1995.14.1.21.Search in Google Scholar
5. Jauniaux, E, Avni, FE, Donner, C, Rodesch, F, Wilkin, P. Ultrasonographic diagnosis and morphological study of placenta circumvallate. J Clin Ultrasound 1989;17:126–31. https://doi.org/10.1002/jcu.1870170212.Search in Google Scholar
6. Sistrom, CL, Ferguson, JE. Abnormal membranes in obstetrical ultrasound: incidence and significance of amniotic sheets and circumvallate placenta. Ultrasound Obstet Gynecol 1993;3:249–55. https://doi.org/10.1046/j.1469-0705.1993.03040249.x.Search in Google Scholar
7. AboEllail, MA, Kanenishi, K, Mori, N, Kurobe, A, Hata, T. HDlive imaging of circumvallate placenta. Ultrasound Obstet Gynecol 2015;46:513–14. https://doi.org/10.1002/uog.14839.Search in Google Scholar
8. Rolschau, J. Circumvallate placenta and intrauterine growth retardation. Acta Obstet Gynecol Scand Suppl 1978;72:11–4. https://doi.org/10.1111/aogs.1978.57.s72.11.Search in Google Scholar
9. Taniguchi, H, Aoki, S, Sakamaki, K, Kurasawa, K, Okuda, M, Takahashi, T, et al. Circumvallate placenta: associated clinical manifestations and complications-a retrospective study. Obstet Gynecol Int 2014. https://doi.org/10.1155/2014/986230.Search in Google Scholar
10. Suzuki, S. Clinical significance of pregnancies with circumvallate placenta. J Obstet Gynaecol Res 2008;34:51–4. https://doi.org/10.1111/j.1447-0756.2007.00682.x.Search in Google Scholar
11. Temming, LA, Raghuraman, N, Woolfolk, C, Dicke, JM, Tuuli, MG, Macones, GA, et al. 432: clinical significance of circumvallate placenta. Am J Obstet Gynecol 2018;218:S262–3. https://doi.org/10.1016/j.ajog.2017.10.368.Search in Google Scholar
12. Ismail, KI, Hannigan, A, O’Donoghue, K, Cotter, A. Abnormal placental cord insertion and adverse pregnancy outcomes: a systematic review and meta-analysis. Syst Rev 2017;6:242. https://doi.org/10.1186/s13643-017-0641-1.Search in Google Scholar
13. Ebbing, C, Kiserud, T, Johnsen, SL, Albrechtsen, S, Rasmussen, S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: a population-based study of 634,741 pregnancies. PloS One 2013;8: e70380. https://doi.org/10.1371/journal.pone.0070380.Search in Google Scholar
14. Rac, MW, Revell, PA, Eppes, CS. Syphilis during pregnancy: a preventable threat to maternal-fetal health. Am J Obstet Gynecol 2017;216:352–63. https://doi.org/10.1016/j.ajog.2016.11.1052.Search in Google Scholar
15. Crino, JP. Ultrasound and fetal diagnosis of perinatal infection. Clin Obstet Gynecol 1999;42:71–80. https://doi.org/10.1097/00003081-199903000-00013.Search in Google Scholar
16. Benirschke, K, Mendoza, GR, Bazeley, PL. Placental and fetal manifestations of cytomegalovirus infection. Virchows Arch B Cell Pathol 1974;16:121–39. https://doi.org/10.1007/bf02894070.Search in Google Scholar
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/crpm-2020-0020).
© 2020 Ricarda Dukatz et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Case Reports – Obstetrics
- Fetal pulmonary choristoma: report of first case and literature review
- Ultrasound prenatal diagnosis of a de novo 14q distal duplication associated with foetal anomalies: a case report
- Prenatal diagnosis of Kleefstra syndrome
- Cardiac implant and the risk of infective endocarditis in pregnancy
- Iatrogenic fetal goiter. Conservative management and spontaneous resolution
- Management in cases of large uterine myomas in pregnancy
- Significantly enlarged varix in the free-loop of the umbilical cord during the second trimester
- A case report of co-infection with rhinovirus and SARS-CoV-2 in pregnancy
- Monoamniotic twins pregnancy complicated by a fetal congenital heart defect – a challenge for perinatal decisions
- Favorable outcome after nine minutes of shoulder dystocia preceded by a tight nuchal cord
- Circumvallate placenta and abnormal cord insertion as risk factors for intrauterine growth restriction and preterm birth: a case report
- A rare case of intra-uterine blood transfusion for fetal anemia caused by a giant placental chorioangioma
- Septated fetal bladder in a case of 2q13 deletion
- A case of prenatal diagnosis of single umbilical artery due to thrombosis diagnosed by the ultrasound finding of “wink-sign”
- Ultrasound diagnosis of myelomeningocele: the role of 3D ultrasonography in determining surficial status of the pathological lesion
- Pragmatic approach and variations in the management of pregnant women with type 1 diabetes mellitus on insulin pump: a case series
- A great pre-eclampsia masquerader. Hemophagocytic lymphohistiocytosis (HLH) presenting in pregnancy
- Survival of both twins in a pregnancy complicated by pre-viable cord prolapse at 21 weeks of gestation
- A case report of a pregnant woman diagnosed with intrahepatic cholangiocarcinoma (ICC) complicated by opioid tolerance
- Prenatal and postnatal imaging of an intrapericardial teratoma
- Case report of a ruptured uterine sacculation in the 19th week of pregnancy
- Is thromboelastography reliable in postpartum coagulopathies? Two case reports and a literature review
- Prenatal diagnosis of megacystis-microcolon-intestinal hypoperistalsis syndrome
- Fetal head entrapment within the lower uterine segment
- Case Reports – Fetus
- A case of diprosopus: a rare form of twinning radiology-pathology correlation
- Case Reports – Newborn
- Transmission of SARS-CoV-2 to premature twins from an asymptomatic mother
- Spinal dysraphism, club feet, and dextrocardia with situs inversus totalis in a neonate: a rare association and review
- Giant congenital vascular malformation: diagnostic approach and clinical course
- Transient neonatal myasthenia gravis following maternal myasthenia gravis presenting in pregnancy after treatment with Alemtuzumab
- Congenital pulmonary lymphangiectasia in an extremely low birth weight: a case report
- Congenital kaposiform hemangioendothelioma: don’t let the appearances fool you
- Agnathia-otocephaly complex: a case report and a literature review on recurrence risk
- Perinatal severe hypophosphatasia: a case report
- Recurrent neonatal group B streptococcus cellulitis and adenitis syndrome with late-onset sepsis
- Neonatal hypertension caused by left-to-right shunt flow through a patent ductus arteriosus in a premature infant
- Maternal Babesia infection associated with neonatal extramedullary hematopoiesis and acute myeloid leukemia in late infancy
- Congenital high airway obstruction syndrome complicated with foregut malformation and high airway fistula to the alimentary tract – a case series with four distinct types
- Aplasia cutis congenita as a consequence of fetal reduction in a triplet pregnancy
- Anhydramnios, but prenatally normal kidneys: renal tubular dysgenesis – patient with mutations in the renin-angiotensin system gene AGTR1
- Symptomatic and lethal congenital primary cardiac rhabdomyoma
Articles in the same Issue
- Case Reports – Obstetrics
- Fetal pulmonary choristoma: report of first case and literature review
- Ultrasound prenatal diagnosis of a de novo 14q distal duplication associated with foetal anomalies: a case report
- Prenatal diagnosis of Kleefstra syndrome
- Cardiac implant and the risk of infective endocarditis in pregnancy
- Iatrogenic fetal goiter. Conservative management and spontaneous resolution
- Management in cases of large uterine myomas in pregnancy
- Significantly enlarged varix in the free-loop of the umbilical cord during the second trimester
- A case report of co-infection with rhinovirus and SARS-CoV-2 in pregnancy
- Monoamniotic twins pregnancy complicated by a fetal congenital heart defect – a challenge for perinatal decisions
- Favorable outcome after nine minutes of shoulder dystocia preceded by a tight nuchal cord
- Circumvallate placenta and abnormal cord insertion as risk factors for intrauterine growth restriction and preterm birth: a case report
- A rare case of intra-uterine blood transfusion for fetal anemia caused by a giant placental chorioangioma
- Septated fetal bladder in a case of 2q13 deletion
- A case of prenatal diagnosis of single umbilical artery due to thrombosis diagnosed by the ultrasound finding of “wink-sign”
- Ultrasound diagnosis of myelomeningocele: the role of 3D ultrasonography in determining surficial status of the pathological lesion
- Pragmatic approach and variations in the management of pregnant women with type 1 diabetes mellitus on insulin pump: a case series
- A great pre-eclampsia masquerader. Hemophagocytic lymphohistiocytosis (HLH) presenting in pregnancy
- Survival of both twins in a pregnancy complicated by pre-viable cord prolapse at 21 weeks of gestation
- A case report of a pregnant woman diagnosed with intrahepatic cholangiocarcinoma (ICC) complicated by opioid tolerance
- Prenatal and postnatal imaging of an intrapericardial teratoma
- Case report of a ruptured uterine sacculation in the 19th week of pregnancy
- Is thromboelastography reliable in postpartum coagulopathies? Two case reports and a literature review
- Prenatal diagnosis of megacystis-microcolon-intestinal hypoperistalsis syndrome
- Fetal head entrapment within the lower uterine segment
- Case Reports – Fetus
- A case of diprosopus: a rare form of twinning radiology-pathology correlation
- Case Reports – Newborn
- Transmission of SARS-CoV-2 to premature twins from an asymptomatic mother
- Spinal dysraphism, club feet, and dextrocardia with situs inversus totalis in a neonate: a rare association and review
- Giant congenital vascular malformation: diagnostic approach and clinical course
- Transient neonatal myasthenia gravis following maternal myasthenia gravis presenting in pregnancy after treatment with Alemtuzumab
- Congenital pulmonary lymphangiectasia in an extremely low birth weight: a case report
- Congenital kaposiform hemangioendothelioma: don’t let the appearances fool you
- Agnathia-otocephaly complex: a case report and a literature review on recurrence risk
- Perinatal severe hypophosphatasia: a case report
- Recurrent neonatal group B streptococcus cellulitis and adenitis syndrome with late-onset sepsis
- Neonatal hypertension caused by left-to-right shunt flow through a patent ductus arteriosus in a premature infant
- Maternal Babesia infection associated with neonatal extramedullary hematopoiesis and acute myeloid leukemia in late infancy
- Congenital high airway obstruction syndrome complicated with foregut malformation and high airway fistula to the alimentary tract – a case series with four distinct types
- Aplasia cutis congenita as a consequence of fetal reduction in a triplet pregnancy
- Anhydramnios, but prenatally normal kidneys: renal tubular dysgenesis – patient with mutations in the renin-angiotensin system gene AGTR1
- Symptomatic and lethal congenital primary cardiac rhabdomyoma

