Acute neonatal appendicitis: the potential value of laparoscopy as a diagnostic and therapeutic tool
-
Joana Dias
, Arnaldo Cerqueira
Abstract
Appendicitis is the most common cause of acute abdominal pain requiring surgical intervention in children, but it is very rare in infants and neonates. Nonspecific clinical features and low index of suspicion make its diagnosis and management particularly challenging, which may result in high chances of complications such as perforation and peritonitis, thus increasing morbidity and mortality. We present the case of a female late preterm newborn with bloody stools and bilious gastric aspirates on the second day of life. After 24 h of clinical, laboratory and radiological surveillance, which evidenced deterioration in the newborn’s condition, an exploratory laparoscopy was performed, showing generalized peritonitis and perforated inflammatory appendix. A laparoscopic appendicectomy was performed. Histology confirmed the appendicitis diagnosis. The authors enhance the value of diagnostic laparoscopy and its potential as a therapeutic tool in neonates.
Introduction
Acute appendicitis remains the most common acute surgical condition in children and a major cause of childhood morbidity [4]. In newborns, the lack of specific signs, its rarity and low index of suspicion make its early diagnosis a challenge. Moreover, the diagnostic delay leads to high morbidity and mortality [7]. Diagnostic laparoscopy has been recently described as a valuable tool to manage newborns with acute abdomen, enabling a prompt diagnosis and allowing operative intervention, with potential to avoid the recognized morbidity of a laparotomy [5].
Case report
A female infant was born at 36 weeks of gestation to a 30-year-old woman by spontaneous vaginal delivery. The mother was positive for Streptococcus group B and received adequate intrapartum chemoprophylaxis with ampicillin. She had no signs of chorioamnionitis. The APGAR scores were 9, 10 and 10 at 1, 5 and 10 min, respectively. The birth weight was 2760 g. The baby was admitted at 2 h of life due to hypoglycemia (35 mg/dL) and poor feeding. Intravenous fluids containing glucose at 4.5 mg/kg per minute were initiated, with an increase in glucose levels to more than 60 mg/dL. She presented no subsequent episodes of hypoglycemia and started enteral feeding with formula. Whole blood examination and C reactive protein (CRP) on admission were normal. On the second day of life, the infant appeared to be uncomfortable and presented with bloody stools and bile-stained gastric aspirate. Whole blood analysis, CRP and routine coagulation tests were repeated, revealing no abnormalities. Abdominal X-ray showed signs of suspected obstruction, and the abdominal ultrasound revealed a small quantity of free abdominal fluid. Antibiotics (ampicillin and gentamicin) were started. The infant continued to pass bloody stools, bile-stained and bloody gastric aspirate, and abdominal distension. On day 3, she presented with leukopenia of 2700/mm3 (neutrophils 50%) and platelet count of 144,000/mm3. CRP increased to a maximum of 63 mg/L. At this point metronidazole was added. Abdominal ultrasound revealed an increase in free abdominal fluid compared with the previous examination; the mesenteric vein/mesenteric artery ratio was preserved. Abdominal X-ray showed a fixed loop, outlining a whirlpool sign, and no signs of intestinal pneumatosis (Figure 1). A diagnostic laparoscopy was performed. A 5-mm supraumbilical port was inserted. This procedure showed good intestinal vascularization, slight delegate distension and normal colon. Then 3-mm instruments were inserted under direct vision via stab incisions, enabling identification of generalized peritonitis secondary to inflammatory process in the right iliac fossa, likely to be appendicitis. Laparoscopic appendectomy was performed (Figure 2). There were no intraoperative complications, and the infant had a good postoperative recovery. She received regular paracetamol for pain relief and did not require morphine. The patient started feeding 3 days after surgery and received full feeds by the fifth postoperative day. She was treated with antibiotics for 10 days and discharged at day 9 postoperatively.

Abdominal X-ray showing a fixed loop and outlining a whirlpool sign (arrow).
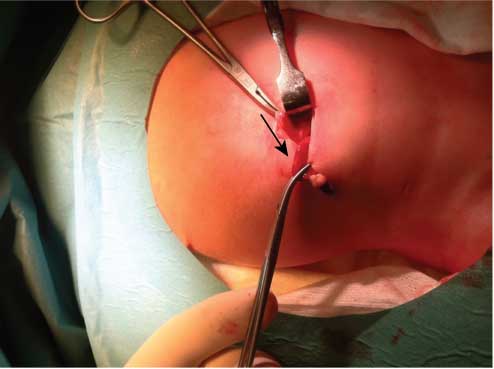
Intraoperative photograph of the appendix (arrow).
Histologic examination of the appendix showed that the lumen was filled with concretions with dense fibrinosuppurative infiltrate and transmural granulation at the site of perforation. Follow-up showed no signs of underlying disease.
Discussion
Acute appendicitis is a rare condition in neonates. In the majority of reported cases of neonatal appendicitis, the patients also had coexistent diagnoses such as prematurity, inguinal hernias and Hirschsprung’s disease [2]. However, in this case, operative findings, histologic examination and clinical follow-up showed no signs of underlying disease.
Various factors such as persistent funnel shape appendicular configuration, soft liquid diet, recumbent posture and infrequent occurrence of viral-induced appendiceal hyperplasia explain the rarity of appendicular involvement in inflammatory process in neonates. The high incidence of perforation can be attributed to thin appendicular wall, small omentum insufficient to wall off infection, undistensible cecum and small capacity of abdominal cavity resulting in early dissemination of infection. The situation demands an early diagnosis so as to reduce mortality, which remains high at 28% despite recent improvements in mortality rates [3].
In addition to the raised probability of perforation and dissemination, the high mortality reported is due to the nonspecific signs and symptoms and late diagnosis, which delay surgical exploration [2].
In the neonatal period, the most frequent signs and symptoms of appendicitis are abdominal distension, vomiting, anorexia, temperature instability, leukocytosis/left shift and abdominal tenderness. Hematochezia has been described in <10% of the reported cases [4, 6].
A reduction of morbidity and mortality has been possible due to the advance in the techniques leading to earlier exploratory laparoscopy in the acute neonatal abdomen that poses a diagnostic dilemma [5].
In the reported case, such as described in the literature, the newborn presented with nonspecific signs and symptoms [4] which clearly pointed to an abdominal source.
Exploratory laparoscopy or laparotomy is recommended in these cases. Laparoscopy is considered the “gold standard” since it is less invasive, without reducing diagnostic accuracy [5, 7], enabling curative intervention with less morbidity.
Although there is limited evidence in this age group, the potential advantages of laparoscopy have an even higher value in neonates. The possible morbidity of relatively large transverse laparotomy wounds in neonates is not insignificant. Postoperative morphine requirements can result in longer ventilator support and delayed onset of feeding leading to an extended hospital stay. Laparoscopy may also reduce the risk of subsequent adhesions and provide a better cosmetic outcome [5].
Review articles are increasingly supporting the use of laparoscopic techniques in newborns, with reports of no significant increase in morbidity and mortality [1]. As recently described by Malakounides et al. [5], laparoscopic approach is a safe and feasible diagnostic tool and, with technical modifications, can be a therapeutic tool.
In this case, exploratory laparoscopy proved to be valuable in the diagnostic approach of a deteriorating neonate, allowing a prompt diagnosis as well as therapeutic intervention with reduced morbidity.
References
[1] Hall NJ, Pacilli M, Eaton S, Reblock K, Gaines BA, Pastor A, et al. Recovery after open versus laparoscopic pylorotomy for pyloric stenosis: a double- blind multicentric randomized controlled trial. Lancet. 2003;373:390–8.10.1016/S0140-6736(09)60006-4Search in Google Scholar
[2] Jancelewicz T, Kim G, Miniat D. Neonatal appendicitis: a new look at an old zebra. J Pediatr Surg. 2008;43:1–5.10.1016/j.jpedsurg.2008.05.014Search in Google Scholar PubMed
[3] Karaman A, Cavusoglu YH, Karaman I, Cakmak O. Seven cases of neonatal appendicitis with a review of the English language literature of the last century. Pediatr Surg Int. 2003;19:707–9.10.1007/s00383-003-1030-5Search in Google Scholar PubMed
[4] Khan RA, Menon P, Rao KLN. Beware of neonatal appendicitis. J Indian Assoc Pediatr Surg. 2010;15:67–9.10.4103/0971-9261.70646Search in Google Scholar PubMed PubMed Central
[5] Malakounides G, John M, Rex D, Mulhall J, Nandi B, Mukhtar Z. Laparoscopic surgery for acute neonatal appendicitis. Pediatr Surg Int. 2011;27:1245–8.10.1007/s00383-011-2972-7Search in Google Scholar PubMed
[6] Sachwitz D, Hass HJ, Aumann V, Herrmann K, Krause H. Incidental finding of an acute appendicitis in a premature newborn with haematochezia. Zentralbl Chir. 2009;134:557–9.10.1055/s-0028-1098922Search in Google Scholar PubMed
[7] Schwartz KL, Gilad E, Sigalet D, Yu W, Wong AL. Neonatal acute appendicitis: a proposed algorithm for timely diagnosis. J Pediatr Surg. 2011;46:2060–4.10.1016/j.jpedsurg.2011.07.018Search in Google Scholar PubMed
-
The authors stated that there are no conflicts of interest regarding the publication of this article.
©2013 by Walter de Gruyter Berlin Boston
Articles in the same Issue
- Masthead
- Masthead
- Case reports – Obstetrics
- Orbital hemorrhage as a primary manifestation of disseminated intravascular coagulation (DIC) associated with intrauterine fetal death and placental abruption
- The intrapartum use of antithrombin III in an antithrombin III-deficient patient: a case report and review of the literature
- Cardiac tamponade in a woman with preeclampsia
- Spontaneous hematoma of the rectus abdominal wall in pregnancy
- Budd-Chiari syndrome following vaginal delivery in a patient with Crohn’s disease: a case report and review of the literature
- Postpartum takotsubo cardiomyopathy with reversible cerebral vasoconstriction syndrome: a case report
- Sarcomatoid carcinoma of the oral cavity during pregnancy
- Can peripartum cardiomyopathy be caused by chemotherapy and radiation of breast cancer?
- Case reports – Fetus
- Fetal death associated with diffuse mesangial sclerosis combined with bilateral multicystic kidney
- Prenatal diagnosis of agenesis of the corpus callosum and cerebellar vermian hypoplasia associated with a microdeletion on chromosome 1p32a
- Pulmonary lymphangiomatosis as a cause of first trimester nuchal cysts in a euploid fetus
- Prenatal ultrasound and molecular diagnosis elucidate the prognosis of Pfeiffer syndrome1)
- Prenatal diagnosis of isolated agnathia with two and three-dimensional ultrasound
- Case reports – Newborn
- Sudden death from cardiac tamponade in an extremely low birth weight neonate with an umbilical venous catheter in situ
- Congenital cytomegalovirus infection after maternal persistent immunoglobulin-M antibodies against cytomegalovirus prior to conception
- Aloe vera induced toxic colitis in a breast-feeding baby: a case report
- A rare cause of neonatal hydrocephalus
- Superior vena cava syndrome causing chylothoraces in a preterm neonate: a case report and literature review
- Trisomy 13 with anorectal malformation: an association or an incidental finding?
- Acute neonatal appendicitis: the potential value of laparoscopy as a diagnostic and therapeutic tool
Articles in the same Issue
- Masthead
- Masthead
- Case reports – Obstetrics
- Orbital hemorrhage as a primary manifestation of disseminated intravascular coagulation (DIC) associated with intrauterine fetal death and placental abruption
- The intrapartum use of antithrombin III in an antithrombin III-deficient patient: a case report and review of the literature
- Cardiac tamponade in a woman with preeclampsia
- Spontaneous hematoma of the rectus abdominal wall in pregnancy
- Budd-Chiari syndrome following vaginal delivery in a patient with Crohn’s disease: a case report and review of the literature
- Postpartum takotsubo cardiomyopathy with reversible cerebral vasoconstriction syndrome: a case report
- Sarcomatoid carcinoma of the oral cavity during pregnancy
- Can peripartum cardiomyopathy be caused by chemotherapy and radiation of breast cancer?
- Case reports – Fetus
- Fetal death associated with diffuse mesangial sclerosis combined with bilateral multicystic kidney
- Prenatal diagnosis of agenesis of the corpus callosum and cerebellar vermian hypoplasia associated with a microdeletion on chromosome 1p32a
- Pulmonary lymphangiomatosis as a cause of first trimester nuchal cysts in a euploid fetus
- Prenatal ultrasound and molecular diagnosis elucidate the prognosis of Pfeiffer syndrome1)
- Prenatal diagnosis of isolated agnathia with two and three-dimensional ultrasound
- Case reports – Newborn
- Sudden death from cardiac tamponade in an extremely low birth weight neonate with an umbilical venous catheter in situ
- Congenital cytomegalovirus infection after maternal persistent immunoglobulin-M antibodies against cytomegalovirus prior to conception
- Aloe vera induced toxic colitis in a breast-feeding baby: a case report
- A rare cause of neonatal hydrocephalus
- Superior vena cava syndrome causing chylothoraces in a preterm neonate: a case report and literature review
- Trisomy 13 with anorectal malformation: an association or an incidental finding?
- Acute neonatal appendicitis: the potential value of laparoscopy as a diagnostic and therapeutic tool

