Abstract
Cardiovascular diseases (CVDs) are the leading cause of global mortality, and three-quarters of the world’s deaths from CVDs occur in low- and middle-income countries. Improving spatial access to care facilities is a way of reducing the disease burden through early detection and treatment. Determining the number of facilities to provide and the locations in order to improve accessibility is central to healthcare facility planning. The maximal covering location problem (MCLP) was used in the identification and determination of where to place additional CVD treatment facilities in Lagos State for better accessibility. The primary objective of this study was to optimize the placement of CVD facilities to maximize coverage for both patients and non-patients alike. The optimization model utilized data on the population of Lagos State, the locations of CVD patients, the location of existing CVD care facilities, and the locations of general hospitals (GHs) within the state. The MCLP implementation was carried out using the maxcovr. The results of the models indicated that the addition of two facilities at the Isolo and Ile-Epo GHs would enhance CVD patient coverage from 70 to 87.4%, reducing the average travel distance from 9,038 to 6,466 m. Similarly, the introduction of two facilities at the Ikorodu and Ajegunle GHs improved population coverage from 40.3 to 70.8%, reducing the average travel distance of 18,788 m by over 5,000 m. These findings are expected to offer valuable insights for public health decision-makers who face the challenge of prioritizing limited budgets.
1 Introduction
Cardiovascular diseases (CVDs) are the leading cause of global mortality and a significant contributor to disability [1]. According to the Global Burden of Disease Study 2019, the number of individuals affected by CVD nearly doubled, increasing from 271 million in 1990 to 523 million in 2019, while CVD-related deaths increased from 12.1 to 18.6 million during the same period [1]. This increasing burden makes CVD the most prominent disease worldwide [2]. Notably, over three-quarters of CVD-related deaths occur in low- and middle-income countries (LMICs) [3]. Unfortunately, individuals in these regions often lack access to primary healthcare programs for early detection and management of CVD risk factors [3], which is exacerbated by limited healthcare funding [4,5]. The most economically vulnerable populations bear the brunt of this burden, as CVDs and other non-communicable diseases (NCDs) contribute to poverty through significant healthcare expenses and high out-of-pocket spending [3].
One effective strategy to reduce the burden of CVDs is through early detection and treatment [3], achievable by improving spatial access to care facilities. The maximal covering location problem (MCLP) is a well-established optimization technique in facility location analysis that determines optimal locations for facilities to maximize coverage while considering capacity constraints and minimizing costs [6,7]. In healthcare contexts, MCLP has been widely applied, including for locating CVD care facilities [8,9]. Timely access to appropriate care facilities is crucial for effectively managing and treating CVDs [10]. Consequently, the location of these care facilities is critical for ensuring equitable access to quality healthcare services for affected populations.
Studies have applied MCLP across various healthcare domains, including primary care facilities [9], emergency services [11,12], and specialized care units [13,14]. Although research specifically focusing on MCLP applications for CVD care facility locations is limited, it is emerging. These studies aim to optimize the placement of CVD care facilities to maximize coverage and ensure accessibility for affected populations, addressing key themes such as demand and accessibility modeling, multi-objective optimization, capacity constraints, and resource allocation [9,15].
Kapwata and Manda [15] aimed to spatially evaluate the geographic healthcare access of individuals diagnosed with CVD in South Africa, focusing on their proximity to health facilities and assessing the density of the facility network. The spatial locations of healthcare facilities and the residences of participants diagnosed with CVD were integrated into a Geographic Information System (GIS) to define accessibility based on travel times and distances. In a facility assessment study conducted in Madhya Pradesh, India, Pakhare et al. [9] evaluated primary care facilities for their preparedness to manage CVD. The study identified critical gaps in essential resources needed for managing NCDs at the primary care level.
Similarly, due to the large geographical area and low population density of Hokkaido, Japan, leading to significant disparities in healthcare access, particularly for stroke treatment, Bando et al. [16] evaluated the balance of supply and demand for mechanical thrombectomy (MT) services to identify high-priority areas for enhancing stroke centers without increasing the number of facilities. Implementing a capacitated MCLP model, the coverage of demand points increased from approximately 53%–85% across different scenarios, and areas with low coverage were identified, highlighting the need for targeted enhancements in specific primary stroke centers (PSCs).
With the aim to optimize healthcare service delivery by addressing the challenges posed by congested environments and patient preferences in choosing healthcare facilities in Karachi, Pakistan, Pouraliakbari et al. [6] employed a modified maximal covering location–allocation problem (MCLAP) model that incorporates user choice behavior, allowing for a more realistic representation of how patients select healthcare providers based on factors like distance and service quality. The analysis reveals that incorporating user choice significantly impacts the effectiveness of location–allocation decisions, leading to improved access to healthcare services.
Even though the application of MCLP for locating CVD care facilities is an emerging research area within healthcare facility planning, the method has been found to confer advantages such as optimal distribution of facilities, improved access to care, efficient use of resources, and effective spatial planning [13,15,17]. Given these advantages in facility location planning and the limited funds available for healthcare in developing countries [18], there is a need to consider the adoption of MCLP for better care and outcomes related to CVDs.
Studies have been conducted on the location of health facilities in Lagos State, Nigeria, but none have considered the placement of healthcare facilities specifically for NCDs. Omogunloye et al. [19] investigated the spatial distribution and utilization of dental clinics in Lagos State using GIS techniques, concluding that the government should establish dental clinics outside general hospitals (GHs) to achieve a more even distribution, as existing clinics were clustered. Similarly, Olowofoyeku et al. [20] used GIS to examine the spatial distribution of primary healthcare (PHC) facilities in Ikorodu Local Government Area (LGA) of Lagos State for treating malaria and sickle cell disease. They found that facility coverage was 48% within a 2 km catchment radius and only 15% within a 1 km catchment of existing PHCs, suggesting a need to increase the number of optimally located facilities to reduce travel distances and expand coverage.
In light of Nigeria’s plans to adopt universal health coverage (UHC) as a policy, Obubu et al. [21] evaluated the existing human resource capacity and distribution of health facilities in Lagos State using descriptive statistics and discovered that the distribution was inequitable between rural and urban areas, and concluded that this disparity could negatively impact the UHC policy in the state. Akintuyi et al. [22], focusing on Surulere LGA of Lagos State, assessed the geographical distribution of healthcare facilities considering population, distance from water bodies, roads, and elevation using a fuzzy analytical hierarchy process. Based on proximity to roads or water bodies, their study suggested optimal locations for new primary healthcare centers to address the observed imbalance in existing facilities.
Consequently, this study explored the use of the MCLP in the location of CVD care facilities in Lagos State, Nigeria, to improve accessibility to care for the people of the state.
2 Materials and methods
2.1 Study population
CVD refers to a group of disorders that affect the heart and blood vessels. It encompasses various conditions, including: coronary heart disease, involving the blood vessels supplying the heart muscle, leading to issues like angina and heart attacks; cerebrovascular disease pertains to blood vessels supplying the brain, often resulting in strokes; peripheral arterial disease affects blood vessels supplying the arms and legs; rheumatic heart disease, results from damage to the heart muscle and valves due to rheumatic fever; and congenital heart disease refers to structural abnormalities of the heart present at birth, impacting normal cardiac function and anatomy [3,23].
This study was conducted retrospectively and considered, in one part, CVD patients aged 18 years and above who were attending the clinic at Lagos University Teaching Hospital (LASUTH), Ikeja, Lagos, and in the second part, the entire population of the state. The data for the first part of the study spanned from 2008 to 2018, excluding data from 2011, which was unavailable during the time of the study. The street addresses of patients were extracted from their case files and geocoded.
Although the two teaching hospitals in the state (LASUTH and Lagos University Teaching Hospital [LUTH], Idi-Araba) were approached for relevant data, it was only LASUTH that provided the requisite data at the required scale. The request for street-level data, which was central to the study, was turned down by the authorities of LUTH; instead, the data provided were at the LGA level. Distributed across the state are 26 GHs owned and run by the Lagos State Government. However, due to the specialist manpower and equipment required in the treatment of CVDs, the GHs refer patients to the LASUTH for appropriate care.
The risk of bias in the data is, however, reduced given that the locations of the two health institutions are not too far apart; the data from LASUTH were almost four times the one from LUTH; and the Lagos State Government has in place a Strategic Health Development Plan, with the goal “to protect, promote, and restore the health of Lagosians and to facilitate the unfettered access to qualitative healthcare services without financial or other barriers,” [24] which makes the LASUTH a preferred health institution for the residents of the state.
2.2 Study area
Lagos State (Figure 1) is located in the southwestern part of Nigeria along the Gulf of Guinea. It is the second most populous state in the country [25], with a population exceeding 13 million [26]. Despite being the smallest state by area, covering only 3,577 km2, Lagos contains 22% of Lagos is made up of lagoons and creeks [27]. Its significant economic and commercial importance extends beyond Nigeria, as it serves as a critical endpoint for three major trans-African highways [28]. As Nigeria’s financial capital, Lagos is highly urbanized and industrialized, contributing a significant portion of the national GDP. However, it also faces challenges such as a high prevalence of CVDs and related risk factors among its residents [29,30].
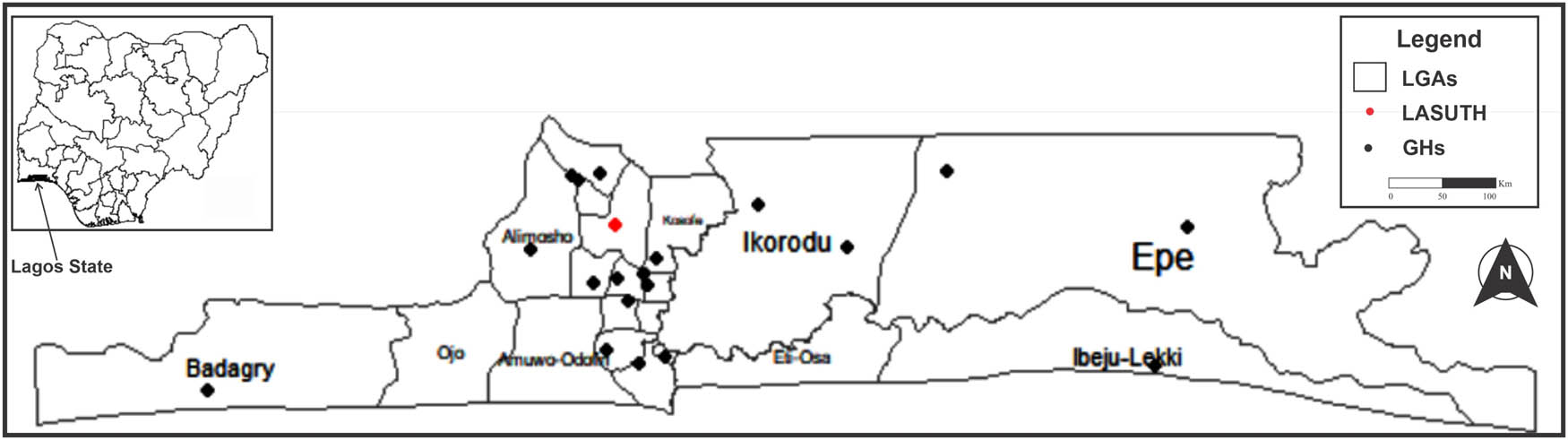
Map of Lagos State showing LGAs, the LASUTH, and GHs. Source: Authors.
2.3 Ethical approval
Ethical approval for this study was sought and obtained from the Social Sciences/Humanities Research Ethics Committee of the University of Ibadan, with the assigned number UI/SSHREC/2018/0012. All information extracted from patients’ records was treated as confidential and anonymized. Since the study was retrospective in nature, it was not necessary to obtain informed consent from the patient.
2.4 Data analysis
Using Google Earth, a geobrowser that utilizes satellite and aerial imagery along with other geographic data accessible online, the street addresses of all diagnosed CVD cases were geocoded. This process extracted the geographical coordinates (longitude and latitude) corresponding to these addresses. The resulting coordinates were then used to plot the locations of diagnosed CVD cases in Lagos State. To maintain confidentiality, the plotted locations were not exact. However, out of the total cases, only 6,370 (92.5%) could be plotted. While the street addresses of some patients were not available, some were difficult to decipher, and certain streets could not be accurately located on Google Earth.
A series of 50 concentric buffers around the LASUTH in Ikeja were created at 500 m intervals. These buffers were plotted alongside the coordinates of the residences of individuals diagnosed with CVDs. Using the point-in-polygon method, the number of CVD cases within each buffer was determined. This information was utilized to create a graph illustrating the number of diagnosed CVD cases based on the distance to the hospital, as well as a bar chart showing the distribution of cases across different zones. The analysis of these plots revealed how cases were distributed in relation to the hospital’s location and surrounding buffers. Given the challenging traffic conditions in the state [31] and the apparent distance decay in the data, a maximum distance threshold of 10,000 m was established, indicating the farthest distance patients should travel to reach the hospital.
To enhance the physical accessibility of CVD patients to healthcare services in Lagos State, the objective was to identify suitable locations for additional CVD care facilities. This task was approached as an MCLP, which aims to determine the optimal placement of multiple facilities to maximize coverage of the target population. The concept of MCLP involves strategically locating facilities to provide the best possible coverage for those in need. Previous studies by Taiwo and Orunmuyi [13], Zarandi et al. [32], and Taiwo [33] have explored this problem in various contexts.
The problem was formulated as follows:
where i, I are the index and set of demand nodes, j, J are the index and set of eligible facility sites, a i is the population or demand at node i, d ij is the shortest distance (or time) from demand node i to facility at node j, S is the distance (or time) standard within which coverage is expected, N i = {j|d ij ≤ S} are the nodes j that are within a distance of S to node i, p is the number of facilities to be established, x j is a binary variable that is equal to 1 when a facility is sited at the jth node and 0 otherwise, and y i is a binary variable, which is equal to 1 if node i is covered by one or more facilities stationed within S, and 0 otherwise.
To examine the feasibility of establishing additional care facilities, two scenarios were considered based on the assumption that patients would seek care from the nearest facility. First, using the diagnosed cases of CVDs as the target population, the potential impact of one or two additional facilities was analyzed. Second, considering that the diagnosed cases represented only a portion of Lagos State’s population, the possibility of locating one or two additional facilities to provide coverage for the entire population was explored. For the analysis of the second scenario, the centroids of the 377 electoral wards in Lagos State were utilized as reference points for the population. Data from these wards were obtained from the GRID3 Nigeria project (www.grid3.gov.ng). The existing 26 GHs in the state were considered as potential sites for the additional facilities. The problem was addressed using several R packages, including maxcovr [34], dplyr [35], and maptools [36]. The base map and observation window for the analysis was the Lagos State LGA map.
Although capacity considerations can enhance certain models of MCLP, it was not considered in this study because the objective is to improve accessibility by maximizing coverage. Prioritizing coverage over capacity in the location of emergency services or healthcare facilities can lead to better service outcomes and resource allocation strategies [37]. Incorporating capacity into MCLP significantly increases its complexity, making it NP-hard, a complexity that can hinder practical applications. By omitting capacity considerations, practitioners can utilize simpler algorithms and heuristics that yield faster and more efficient solutions [32,38].
By employing these methodologies and tools, the study assessed the viability and potential impact of introducing one or two additional care facilities in the context of CVD management in Lagos State.
3 Results
Out of a total of 6,780 cases, 51.2% were female, and 48.7% were male, with a majority of the cases occurring in individuals aged 50 years or older. When analyzing the relationship between the cases and the distances patients traveled, it was observed that the highest number of cases occurred at a distance of 7,000 m from LASUTH. Specifically, the 12th to 15th buffers, which represent a radius of 6–7.5 km, exhibited the highest concentration of cases. Subsequently, the number of cases decreased sharply and then stabilized after the 15th buffer. It was noted that approximately 70% of the cases were accounted for when the distance reached 10,000 m (Figure 2).
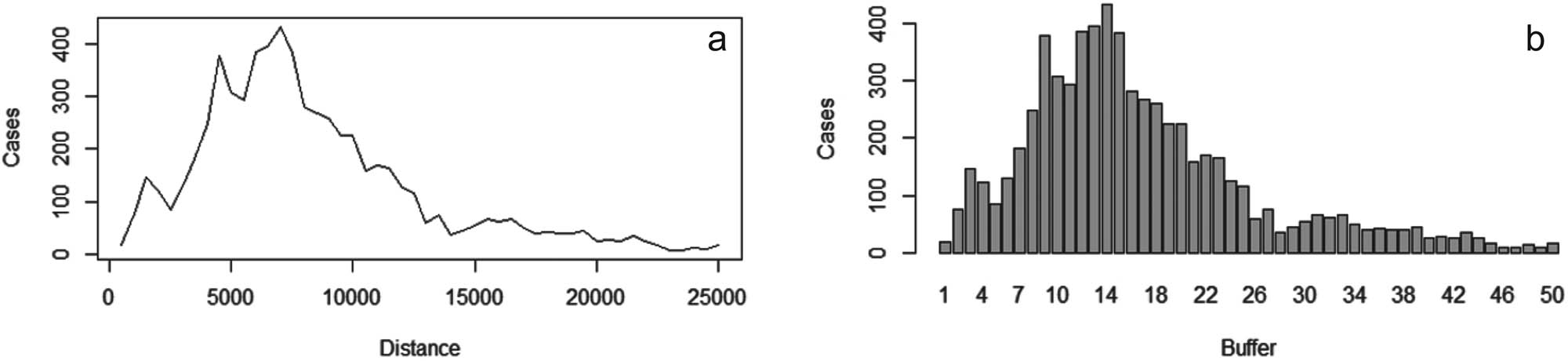
(a) Distances of the residence of cases to the care facility. (b) Buffers of the hospital and the corresponding cases. Source: Authors.
The findings from the maximum cover analysis, as presented in Table 1, indicate that within the 10,000 m distance threshold, LASUTH provides coverage for approximately 70% of the cases, with an average distance traveled of 9,038 m. However, to enhance coverage, the inclusion of a CVD care facility at GH, Isolo (as shown in Figure 3b), resulted in a decrease in the average distance traveled to 7,604 m and an increase in the percentage of patients covered to 79.7%. The addition of another CVD care facility at GH, Ile-Epo (as depicted in Figure 3c), further raised the percentage coverage of patients to 87.4% while reducing the average distance traveled by patients to 6,466 m.
Effect of additional healthcare facilities on coverage of diagnosed CVD cases in Lagos State
| n_added | distance_within | n_cov | pct_cov | n_not_cov | pct_not_cov | dist_avg | dist_sd |
|---|---|---|---|---|---|---|---|
| 0 | 10,000 | 5,039 | 0.709 | 2,066 | 0.291 | 9,038 | 7,003 |
| 1 | 10,000 | 5,660 | 0.797 | 1,445 | 0.203 | 7,640 | 6,704 |
| 2 | 10,000 | 6,207 | 0.874 | 898 | 0.126 | 6,466 | 6,611 |
n_added = number of new facilities; distance_within = distance used to determine coverage; n_cov = number of events covered; n_not_cov = number of events not covered; pct_cov = percentage of events covered; pct_not_cov = percentage of events not covered; dist_avg = average distance to the nearest facility; dist_sd = standard deviation of the distance to the nearest facility.
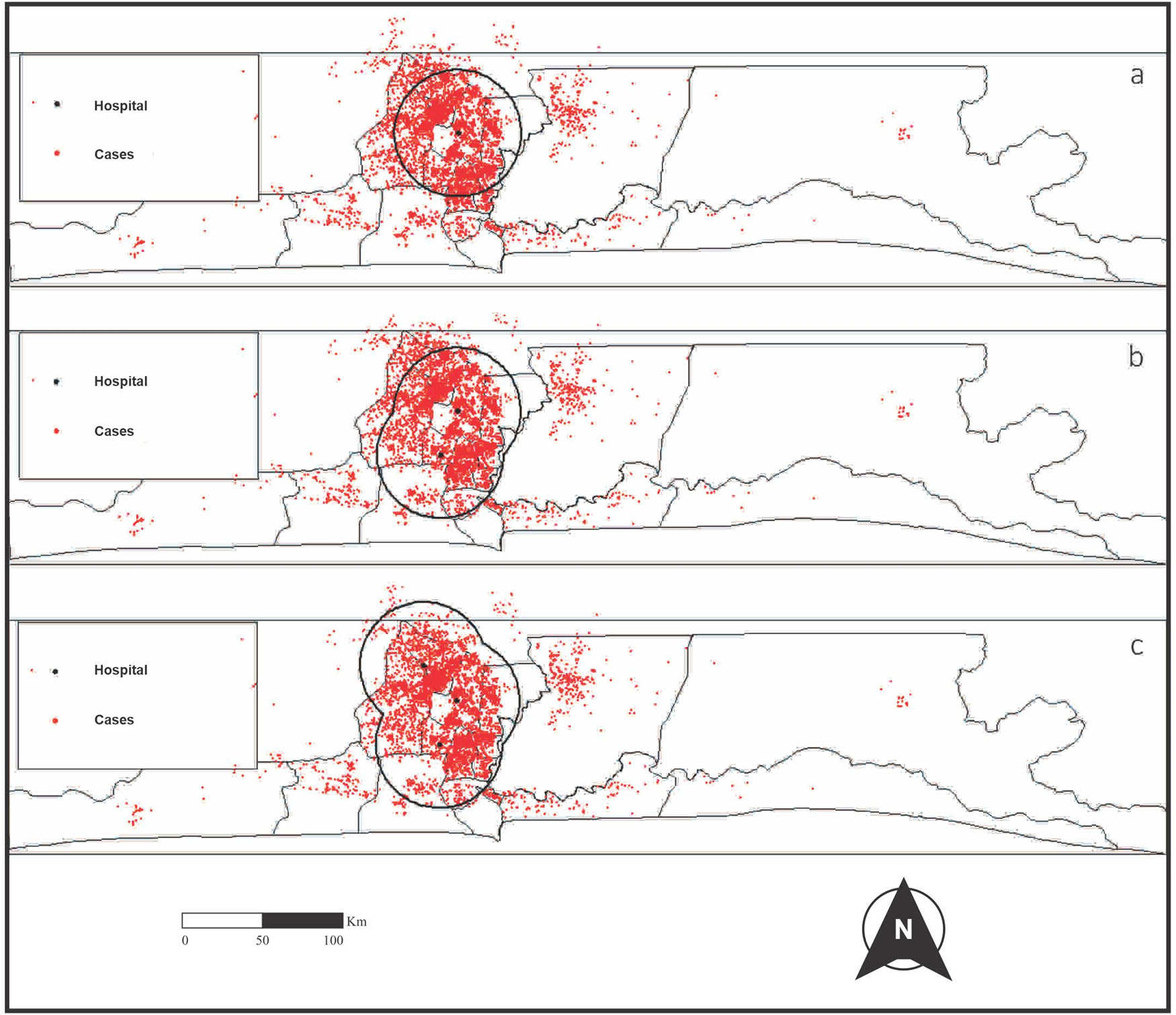
Facility coverages of diagnosed CVD cases in Lagos State: (a) existing facility, (b) one additional facility, and (c) two additional facilities. Source: Authors.
However, considering that the majority of diagnosed cases of CVDs are concentrated in the central region of the state and that the utilization of healthcare facilities decreases as the distance increases, we examined the extent to which the current facility adequately serves the overall population of Lagos State. We also considered potential scenarios for enhancing access to CVD care facilities in the state, as the current number of cases may not accurately reflect the actual burden of the disease in the region.
Using the centroids of the 377 electoral wards in the state as reference points for the population, it was found that the facility located at LASUTH only served 40.3% of the population (Figure 4a), with an average travel distance of 18,788 m (Table 2). To improve the situation, the introduction of an additional facility at GH, Ikorodu (Figure 4b), resulted in a coverage increase of over 25% and a reduction of the average travel distance by more than 3 km. To further enhance accessibility, a third facility established at GH, Ajegunle (Figure 4c), reduced the travel distance by another 2 km, and increased coverage to 70.8%.

Facility coverages of the general population of Lagos State: (a) existing facility, (b) one additional facility, and (c) two additional facilities. Source: Authors.
Effect of additional healthcare facilities on coverage of the general population of Lagos State
| n_added | distance_within | n_cov | pct_cov | n_not_cov | pct_not_cov | dist_avg | dist_sd |
|---|---|---|---|---|---|---|---|
| 0 | 10,000 | 152 | 0.403 | 225 | 0.597 | 18,788 | 18,588 |
| 1 | 10,000 | 248 | 0.658 | 129 | 0.342 | 15,642 | 19,108 |
| 2 | 10,000 | 267 | 0.708 | 110 | 0.292 | 12,915 | 15,486 |
n_added = number of new facilities; distance_within = distance used to determine coverage; n_cov = number of events covered; n_not_cov = number of events not covered; pct_cov = percentage of events covered; pct_not_cov = percentage of events not covered; dist_avg = average distance to the nearest facility; dist_sd = standard deviation of the distance to the nearest facility.
4 Discussion
In some cases, specialized care and equipment are required for the treatment of certain cardiac ailments, and time is often of the essence. The distribution of cases around LASUTH mirrors what Oviasu [39] found in her study on the effect of travel time on patients’ use of the renal facility in Benin City, Nigeria. Oviasu [39] discovered that patients living far from the hospital are most affected by spatial accessibility to the renal facility within the University of Benin Teaching Hospital. This may have resulted in patients not seeking medical treatment early and thus resorting to alternative avenues for cure. Therefore, our study’s findings align with the established inverse relationship between the distance from a facility and its utilization, a phenomenon known as distance decay [40]. However, this situation is compounded by the fact that in Nigeria, most CVD care facilities are located within tertiary health facilities, which are few and far apart. Consequently, this may lead CVD patients to seek unorthodox care, as posited by Oviasu [39].
The number of diagnosed CVD cases peaked at a distance of 7,000 m from the existing CVD healthcare facility in Lagos State, gradually decreasing thereafter. This pattern indicates that the facility is not adequately serving diagnosed CVD cases, as usage declines with increasing distance. The observed trend in Figure 2a suggests that the 10,000 m mark (20th Buffer, Figure 2b) serves as a significant threshold for clinic attendance among diagnosed CVD patients in Lagos State. Furthermore, both extremes of the state recorded annual average cases of fewer than 20 throughout the study period.
Lagos State has 20 LGAs and 26 GHs [26,41], averaging 1.3 GHs per LGA. Refurbishing existing facilities and enhancing medical staffing and equipment to manage CVD cases could elevate patient coverage from 70 to 87.4% while decreasing the average travel distance from 9,038 to 6,466 m. Decentralizing chronic disease management, particularly for CVDs, presents a viable strategy to alleviate the strain on vulnerable healthcare systems [42]. The current 26 GHs in the state offer a significant opportunity for outreach programs that enable itinerant free-testing to facilitate early CVD detection, potentially mitigating the economic impact of these diseases. Peiris et al. [43] and Mensah et al. [44] indicate that a majority of CVD cases in LMICs affect individuals in their prime, resulting in substantial losses in workforce productivity and man-hours.
To enhance the number of CVD healthcare facilities in Lagos State, the addition of two more facilities at the GHs in Ikorodu and Ajegunle has resulted in a coverage of 70.8% for the entire state’s population, with an average travel distance of approximately 13,000 m. From an economic perspective, implementing these changes in the long term would likely be more advantageous for Lagos State. The introduction of these two new facilities is preferable to selecting the GHs in Isolo and Ile-Epo because they provide greater coverage, thereby enhancing accessibility and utilization of healthcare services. Moreover, due to their geographical locations, the CVD care facilities in Ikorodu and Ajegunle are situated closer to both ends of the state compared to Isolo and Ile-Epo. This improved accessibility has the potential to increase attendance at CVD clinics by residents in rural areas. For instance, the distance from Badagry to Ajegunle is more appealing for patients in Badagry than the distance from Badagry to Ikeja. This observation aligns with previous studies demonstrating a positive correlation between proximity to a facility and its usage [39,45].
In both scenarios, the selected locations for the additional CVD care facilities were more peripheral, which improved accessibility for a wider population. Peripheral locations often experience less traffic congestion compared to central areas, resulting in shorter travel times for users. This makes it easier for them to reach the facility quickly, especially during peak hours. Additionally, these locations facilitate access via multiple transportation modes, thereby increasing overall accessibility [46]. Furthermore, situating facilities in such areas helps integrate them into communities, fostering local engagement and ensuring that services meet the specific needs of those populations. This ultimately leads to better utilization of the facilities [47].
5 Conclusion
The study emphasizes the urgent need for enhanced access to CVD care facilities in Lagos State, Nigeria. It identifies an inverse relationship between the distance to existing facilities and the utilization of CVD care, suggesting that as distance increases, usage decreases. The research advocates for leveraging existing GHs in the state to establish new CVD care facilities. This approach aligns with the strategy of decentralizing chronic disease management, which is crucial for alleviating the burden on fragile healthcare systems. To improve accessibility and utilization, the study proposes the establishment of two additional CVD care facilities at GHs located in Ikorodu and Ajegunle. These locations are strategically chosen due to their proximity to underserved areas of the state compared to existing facilities. Overall, the findings offer valuable insights into optimal locations for CVD care facilities in Lagos State and underscore the importance of increasing coverage and minimizing average travel distances as priorities for health policy in the region.
Acknowledgements
The authors appreciate the Management of the Lagos State University Teaching Hospital (LASUTH), Ikeja, especially, the Records Department, under the headship of Prof. Ayeni, for granting access to the data used in this study.
-
Funding information: Authors state no funding involved.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal, reviewed all the results and approved the final version of the manuscript. OA and OJT were involved in study design, data interpretation, drafting of the article, and critical revision of the manuscript. OA handled data collection and analysis. Both contributing authors reviewed and approved the manuscript prior to submission.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: Data will be shared on request to the corresponding author with the permission of Lagos University Teaching Hospital (LASUTH).
References
[1] Giovanni A, Enrico A, Aime B, Michael B, Marianne B, Jonathan C, et al. Global Burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020 Dec;76(25):2982–3021.Search in Google Scholar
[2] Li Z, Lin L, Wu H, Yan L, Wang H, Yang H, et al. Global, regional, and national death, and disability-adjusted life-years (DALYs) for cardiovascular disease in 2017 and trends and risk analysis from 1990 to 2017 using the global burden of disease study and implications for prevention. Front Public Health. 2021 Oct;9:559751.10.3389/fpubh.2021.559751Search in Google Scholar PubMed PubMed Central
[3] World Health Organization. Cardiovascular diseases (CVDs) Geneva: WHO; 2021. https://www. who. int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). [Updated 2021 June 11].Search in Google Scholar
[4] Fazal F, Saleem T, Rehman ME, Haider T, Khalid AR, Tanveer U, et al. The rising cost of healthcare and its contribution to the worsening disease burden in developing countries. Ann Med Surg. 2022 Oct 1;82. 10.1016/j.amsu.2022.104683.Search in Google Scholar PubMed PubMed Central
[5] Chang AY, Cowling K, Micah AE, Chapin A, Chen CS, Ikilezi G, et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019 Jun;393(10187):2233–60.Search in Google Scholar
[6] Pouraliakbari M, Mohammadi M, Mirzazadeh A. Analysis of maximal covering location-allocation model for congested healthcare systems in user choice environment. Int J Ind Syst Eng. 2018;28(2):240–74.10.1504/IJISE.2018.089139Search in Google Scholar
[7] Töreyen Ö. Hierarchical maximal covering location problem with referral in the presence of partial coverage. Master’s thesis. Ankara, Turkey: Middle East Technical University.Search in Google Scholar
[8] Eiselt HA. Location science in Canada. INFOR: Inf Syst Oper Res. 2008 Nov;46(4):283–98.10.3138/infor.46.4.283Search in Google Scholar
[9] Pakhare A, Kumar S, Goyal S, Joshi R. Assessment of primary care facilities for cardiovascular disease preparedness in Madhya Pradesh, India. BMC Health Serv Res. 2015 Jun;15:1–8.10.1186/s12913-015-1075-xSearch in Google Scholar PubMed PubMed Central
[10] Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world. Health Aff. 2007 Jan;26(1):13–24.10.1377/hlthaff.26.1.13Search in Google Scholar PubMed PubMed Central
[11] Eaton DJ, Lantigua UHM, Morgan RR, J. Determining ambulance deployment in santo domingo, dominican republic. J Oper Res Soc. 1986 Feb;37(2):113–26.10.1057/jors.1986.21Search in Google Scholar
[12] Current J, O’Kelly M. Locating emergency warning sirens. Decis Sci. 1992 Jan;23(1):221–34.10.1111/j.1540-5915.1992.tb00385.xSearch in Google Scholar
[13] Taiwo OJ, Orunmuyi AT. Maximal covering location problem for nuclear medicine clinics allocation in Nigeria. Spat Inf Res. 2021 Dec;29(6):919–35.10.1007/s41324-021-00405-6Search in Google Scholar
[14] Daniali ZM, Sepehri MM, Sobhani FM, Heidarzadeh M. A regionalization model to increase equity of access to maternal and neonatal care services in Iran. J Prev Med Public Health. 2022 Jan;55(1):49.10.3961/jpmph.21.401Search in Google Scholar PubMed PubMed Central
[15] Kapwata T, Manda S. Geographic assessment of access to health care in patients with cardiovascular disease in South Africa. BMC Health Serv Res. 2018 Dec;18:1–0.10.1186/s12913-018-3006-0Search in Google Scholar PubMed PubMed Central
[16] Bando K, Ohashi K, Fujiwara K, Osanai T, Morii Y, Tanikawa T, et al. The capacitated maximal covering location problem improves access to stroke treatment: a cross-sectional simulation study. Health Serv Insights. 2024 Jul;17:11786329241263699.10.1177/11786329241263699Search in Google Scholar PubMed PubMed Central
[17] Alcalá HE, Albert SL, Roby DH, Beckerman J, Champagne P, Brookmeyer R, et al. Access to care and cardiovascular disease prevention: a cross-sectional study in 2 Latino communities. Medicine. 2015 Aug;94(34):e1441.10.1097/MD.0000000000001441Search in Google Scholar PubMed PubMed Central
[18] Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005 Dec 6;112(23):3547–53.10.1161/CIRCULATIONAHA.105.591792Search in Google Scholar PubMed
[19] Omogunloye OG, Tijani OA, Abiodun EO, Ajayi OG, Odumosu JO. Geospatial distribution and utilization of dental facilities in Lagos State. J Biodivers Endanger Species. 2016;4:163.Search in Google Scholar
[20] Olowofoyeku OO, Shell J, Goodyer E, Deka L. Healthcare facility coverage for malaria and sickle cell disease treatment: a spatial analysis of ikorodu local government area of Lagos State. Int J Health Wellness Soc. 2019;10(2):33.10.18848/2156-8960/CGP/v10i02/33-51Search in Google Scholar
[21] Obubu M, Chuku N, Ananaba A, Sadiq FU, Sambo E, Kolade O, et al. Evaluation of healthcare facilities and personnel distribution in Lagos State: implications on universal health coverage. Hospital Pract. 2023 Mar;51(2):64–75.10.1080/21548331.2023.2170651Search in Google Scholar PubMed
[22] Akintuyi A, Otusanya O, Fashoto B, Afolabi O. Geospatial analysis of healthcare facilities in Surulere Local Government Area of Lagos state. Lagos. J Geogr Issues. 2023 Mar;3(1):38–57.Search in Google Scholar
[23] American Heart Association. What is Cardiovascular Disease? Texas, USA: American Heart Association; 2024. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease.Search in Google Scholar
[24] LSMoH. Lagos state government strategic health development plan (2010-2015). Lagos, Nigeria: Lagos State Ministry of Health; 2010.Search in Google Scholar
[25] National Population Commission. National results: population by state and Sex. Abuja, Nigeria: National Population Commission. http://www.population.gov.ng/files/nationafinal.pdf.Search in Google Scholar
[26] National Population Commission Nigeria. Nigeria Population Projection and Demographic Indicators-State and National. Abuja, Nigeria: National Population Commission of Nigeria.Search in Google Scholar
[27] About L. Lagos State Government. Lagos, Nigeria. https://lagosstate.gov.ng/about-lagos/.Search in Google Scholar
[28] Lagos State Ministry of Health (LSMoH). Lagos state government strategic health development plan (2010-2015). Lagos, Nigeria: Lagos State Ministry of Health; 2010.Search in Google Scholar
[29] Ojikutu RK. The prevalence of cardiovascular disease in the Lagos State, Nigeria. Ghana J Dev Stud. 2009;6(2):41–50.10.4314/gjds.v6i2.61388Search in Google Scholar
[30] Adegoke O, Awolola NA, Ajuluchukwu JN. Prevalence and pattern of cardiovascular-related causes of out-of-hospital deaths in Lagos, Nigeria. Afr Health Sci. 2018 Nov;18(4):942–9.10.4314/ahs.v18i4.13Search in Google Scholar PubMed PubMed Central
[31] Bello EI, Usifo CI. A study of urban traffic management-A case study of lagos state traffic management authority. Adv Mater Res. 2009 Feb;62:599–605.10.4028/www.scientific.net/AMR.62-64.599Search in Google Scholar
[32] Zarandi MF, Davari S, Sisakht SH. The large scale maximal covering location problem. Sci Iran. 2011 Dec;18(6):1564–70.10.1016/j.scient.2011.11.008Search in Google Scholar
[33] Taiwo OJ. Maximal covering location problem (MCLP) for the identification of potential optimal COVID-19 testing facility sites in Nigeria. Afr Geogr Rev. 2021 Oct;40(4):395–411.10.1080/19376812.2020.1838306Search in Google Scholar
[34] Tierney N, Padgham M. Maxcovr: a set of tools for solving the maximal covering location problem. R package version 0.1.3.9200.Search in Google Scholar
[35] Hadley Wickham RF, Henry L, Müller K. dplyr: A grammar of data manipulation. R package version 1.1.3.Search in Google Scholar
[36] Bivand R. maptools: Tools for handling spatial objects. R Package Version 1.1-1; 2021.Search in Google Scholar
[37] Pirkul H, Schilling DA. The maximal covering location problem with capacities on total workload. Manag Sci. 1991 Feb;37(2):233–48.10.1287/mnsc.37.2.233Search in Google Scholar
[38] Bagherinejad J, Shoeib M. Dynamic capacitated maximal covering location problem by considering dynamic capacity. Int J Ind Eng Comput. 2018;9(2):249–64.10.5267/j.ijiec.2017.5.004Search in Google Scholar
[39] Oviasu O. The spatial analysis of diagnosed Chronic Kidney Disease in Nigeria: A case study of Edo State Doctoral dissertation. Sheffield. UK: University of Sheffield.Search in Google Scholar
[40] Zhou X, Yu Z, Yuan L, Wang L, Wu C. Measuring accessibility of healthcare facilities for populations with multiple transportation modes considering residential transportation mode choice. ISPRS Int J Geo-Inf. 2020 Jun;9(6):394.10.3390/ijgi9060394Search in Google Scholar
[41] Lagos State Waste Management Authority. Statistics of healthcare facilities in Lagos State. http://www.lawma.gov.ng/DataBank/LAWMA%20Medical%20Waste%20Management%20Unit.pdf. Accessed Wednesday, August 24, 2016, 11:33:26 PM.Search in Google Scholar
[42] Bowry AD, Lewey J, Dugani SB, Choudhry NK. The burden of cardiovascular disease in low-and middle-income countries: epidemiology and management. Can J Cardiol. 2015 Sep;31(9):1151–9.10.1016/j.cjca.2015.06.028Search in Google Scholar PubMed
[43] Peiris D, Ghosh A, Manne-Goehler J, Jaacks LM, Theilmann M, Marcus ME, et al. Cardiovascular disease risk profile and management practices in 45 low-income and middle-income countries: A cross-sectional study of nationally representative individual-level survey data. PLoS Med. 2021 Mar;18(3):e1003485.10.1371/journal.pmed.1003485Search in Google Scholar PubMed PubMed Central
[44] Mensah GA, Sampson UK, Roth GA, Forouzanfar MH, Naghavi M, Murray CJ, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015 Mar;26(2 H3Africa Suppl):S6.10.5830/CVJA-2015-036Search in Google Scholar PubMed PubMed Central
[45] Keates AK, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: epidemiological profile and challenges. Nat Rev Cardiol. 2017 May;14(5):273–93.10.1038/nrcardio.2017.19Search in Google Scholar PubMed
[46] Liu Y, Gu H, Shi Y. Spatial accessibility analysis of medical facilities based on public transportation networks. Int J Environ Res Public Health. 2022 Dec;19(23):16224.10.3390/ijerph192316224Search in Google Scholar PubMed PubMed Central
[47] Wang J, Zhou J. Spatial evaluation of the accessibility of public service facilities in Shanghai: A community differentiation perspective. PLoS One. 2022 May;17(5):e0268862.10.1371/journal.pone.0268862Search in Google Scholar PubMed PubMed Central
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Predictors of diagnosed cardiovascular diseases and their spatial heterogeneity in Lagos State, Nigeria
- Discourses of risk in public health advertising about underage alcohol consumption
- Utilization of health service and associated factors among women in childbearing age in selected internally displaced persons camps, Hargeisa – Somaliland
- Healthcare workers’ attitudes toward children getting Covid-19 vaccinations in Gaza Strip
- Regional prevalence and spatial modeling of hypertension in South Africa
- Immediate effect of mud pack on resting cardiovascular parameters in hypertensive individuals – A single-arm pilot study
- An analysis of medical scheme-related pregnancy terminations in South Africa in 2022
- Immediate effect of Kaki Mudra on pupillary light reflex among healthy individuals – A study protocol of a Randomized control trial
- Healthy lifestyle perceptions and practices among college students at Yanbu University College for Women in Saudi Arabia
- Food service management perspectives on reducing sodium content in foods served: Opportunities and challenges
- Effects of sanitation on child growth in Serbian Roma communities
- College students’ resilience-promoting behaviors and psychological well-being: A latent class analysis
- Comparative analysis of household deprivation among Jewish and other religious groups in England and Wales
- A study protocol for a randomized controlled trial on the effect of Surya Nadi Pranayama practice on cognitive abilities in school children
- Determinants of health insurance adoption among residents of Lagos, Nigeria: A cross-sectional survey
- Enhancing geographical access to cardiovascular disease healthcare services in Lagos State, Nigeria
- Mortality trends from all causes and diabetes mellitus according to sex between 1998 and 2021
- Developing syndrome of inappropriate antidiuretic hormone secretion in Guillain-Barre syndrome
- Health professionals’ continuing education attitudes and experiences in food and nutrition sustainability
- Nutrition literacy among women participating in a community kitchen program in Antioquia, Colombia: A cross-sectional study
- Review Articles
- Unraveling PCOS: Exploring its causes and diagnostic challenges
- Smart healthcare: Integration of AI and brain cells for advanced healthcare applications
- Disrupting the melody: The interplay of obesity and metabolic dysfunction
- Comparing global trends in gastric cancer and the need for national screening programs: An in-depth literature review
- Social media – Boon or Bane?
- Advancing rheumatic disease treatment: A journey towards better lives
- Antimicrobial resistance: A significant public health issue of both human and veterinary concern
- Psychological flexibility and celiac disease in adolescents: Understanding adherence and well-being for enhanced care. A rapid narrative review
- Harnessing real-world evidence in pharmacoeconomics: A comprehensive review
- Commentary
- Mixed messages, broken trust, avoidable deaths: A critical appraisal of the UK government’s response to the COVID-19 pandemic
- The psychological profile of Iraq: A nation haunted by decades of suffering
- Metabolic mysteries of the mind: Investigating type 3 diabetes
- Ready to bleed when touched – Moral Injury in the Special Operations Forces military population
- Towards robust pharmacovigilance surveillance systems
- Short Communications
- From click to calories: Navigating the impact of food delivery apps on obesity
- Long-term economic outlook for Japan, as impacted by COVID-19
- Special Issue on Public Health Resilience - Part II
- Reframing the response to the opioid crisis: The critical role of resilience in public health
Articles in the same Issue
- Research Articles
- Predictors of diagnosed cardiovascular diseases and their spatial heterogeneity in Lagos State, Nigeria
- Discourses of risk in public health advertising about underage alcohol consumption
- Utilization of health service and associated factors among women in childbearing age in selected internally displaced persons camps, Hargeisa – Somaliland
- Healthcare workers’ attitudes toward children getting Covid-19 vaccinations in Gaza Strip
- Regional prevalence and spatial modeling of hypertension in South Africa
- Immediate effect of mud pack on resting cardiovascular parameters in hypertensive individuals – A single-arm pilot study
- An analysis of medical scheme-related pregnancy terminations in South Africa in 2022
- Immediate effect of Kaki Mudra on pupillary light reflex among healthy individuals – A study protocol of a Randomized control trial
- Healthy lifestyle perceptions and practices among college students at Yanbu University College for Women in Saudi Arabia
- Food service management perspectives on reducing sodium content in foods served: Opportunities and challenges
- Effects of sanitation on child growth in Serbian Roma communities
- College students’ resilience-promoting behaviors and psychological well-being: A latent class analysis
- Comparative analysis of household deprivation among Jewish and other religious groups in England and Wales
- A study protocol for a randomized controlled trial on the effect of Surya Nadi Pranayama practice on cognitive abilities in school children
- Determinants of health insurance adoption among residents of Lagos, Nigeria: A cross-sectional survey
- Enhancing geographical access to cardiovascular disease healthcare services in Lagos State, Nigeria
- Mortality trends from all causes and diabetes mellitus according to sex between 1998 and 2021
- Developing syndrome of inappropriate antidiuretic hormone secretion in Guillain-Barre syndrome
- Health professionals’ continuing education attitudes and experiences in food and nutrition sustainability
- Nutrition literacy among women participating in a community kitchen program in Antioquia, Colombia: A cross-sectional study
- Review Articles
- Unraveling PCOS: Exploring its causes and diagnostic challenges
- Smart healthcare: Integration of AI and brain cells for advanced healthcare applications
- Disrupting the melody: The interplay of obesity and metabolic dysfunction
- Comparing global trends in gastric cancer and the need for national screening programs: An in-depth literature review
- Social media – Boon or Bane?
- Advancing rheumatic disease treatment: A journey towards better lives
- Antimicrobial resistance: A significant public health issue of both human and veterinary concern
- Psychological flexibility and celiac disease in adolescents: Understanding adherence and well-being for enhanced care. A rapid narrative review
- Harnessing real-world evidence in pharmacoeconomics: A comprehensive review
- Commentary
- Mixed messages, broken trust, avoidable deaths: A critical appraisal of the UK government’s response to the COVID-19 pandemic
- The psychological profile of Iraq: A nation haunted by decades of suffering
- Metabolic mysteries of the mind: Investigating type 3 diabetes
- Ready to bleed when touched – Moral Injury in the Special Operations Forces military population
- Towards robust pharmacovigilance surveillance systems
- Short Communications
- From click to calories: Navigating the impact of food delivery apps on obesity
- Long-term economic outlook for Japan, as impacted by COVID-19
- Special Issue on Public Health Resilience - Part II
- Reframing the response to the opioid crisis: The critical role of resilience in public health

