Abstract
Objectives
This study aims to develop a theoretical framework for medical humanities competency (MHC) within the five-year medical undergraduate education in China and suggest effective strategies to enhance MHC of medical undergraduates that can be derived from these studies.
Methods
Grounded theory methodology was utilized to develop a theoretical framework for MHC. A combination of purposive and theoretical sampling was used to engage 32 participants, including educators and students, from 10 universities spanning seven provinces in China. Data collection involved semi-structured interviews, complemented by supplementary materials like online documents, newspapers, and related literature. The amassed data was analyzed employing Strauss and Corbin’s triphasic coding technique, consistent with the constant comparative method intrinsic to grounded theory.
Results
A meticulous three-tier coding process discerned 28 third-level categories, 12 subcategories, and four principal categories crucial in formulating the final framework for MHC. This MHC framework embodies core components dubbed as the “4C” framework: comprehension of humanities, communication capacity, cooperation skills, and concern for “LEE” (law abidance, ethical reasoning, and emotional care). Concurrently, the study introduces “4R” (rules, relevance, responsiveness, and reflective practice) strategies to amplify the humanistic competencies of medical undergraduates.
Conclusions
This research proffers a theoretical MHC framework, positioning itself as a beacon for crafting medical humanistic syllabi in undergraduate medical programs. Medical educators, while acknowledging diverse cultural underpinnings, can adeptly harness both the “4C” framework and the “4R” strategies to nurture and augment the humanistic competence of medical students.
Introduction
Medicine is regarded as the most humane of sciences, the most empirical of arts, and the most scientific of human endeavors [1]. The inclusion of humanities in medical education plays a crucial role in the training of future doctors, as it encompasses the arts and social sciences, which are integral to everyday medical practice [2]. Incorporating humanities in medical education promotes interdisciplinary interactions, enhancing relationships between doctors and the broader world. Additionally, the humanities impart valuable skills to medical students that are applicable in clinical situations [3]. Medical humanities competence (MHC) can prepare medical students to respond appropriately to complicated clinical problems [4]. MHC has gained recognition and is in high demand in undergraduate medical education. Its significance has been highlighted in various reports worldwide, such as “Tomorrow’s Doctors” published by The General Medical Council (GMC) and the global minimum essential requirements (GMER) outlined by The Institution for International Medical Education (IIME), The IIME report identified MHC as one of the seven essential skills for physicians [5], 6]. The 2010 Global Commission’s report on medical education underscores the importance of nurturing compassionate medical professionals [7]. China also recognized the revival of medical humanities through its “Healthy China 2030” plan and subsequent directives in 2016 and 2020 [8].
Previous research has shown that doctors with MHC have the potential to improve health outcomes and reduce legal issues within the healthcare system. Moreover, studies have indicated that medical university students who possess a dual background in humanities and science outperform their peers who solely pursued a science background in practical settings [9], 10]. In China, current medical students are lacking essential humanistic competencies, which is a cause for concern [11]. Current courses in medical humanities were arbitrarily established due to lack of framework of MHC [12]. Medical disputes and the lack of trust between doctors and patients in China have been attributed to the insufficient provision of proper medical humanities education at the medical student levels [13]. Therefore, it is crucial to educate students about humanistic competencies and incorporate them into the curriculum. This not only helps cultivate physicians with the necessary humanistic qualifications but also aligns with the shift from the traditional biomedical model to a more comprehensive bio-psycho-social approach in medicine [14], 15].
However, currently, the theoretical framework of MHC among medical students in China remains a “black box” that has yet to be fully unveiled, there is limited research addressing the question of which essential humanistic competencies medical schools should teach, calling for urgent exploration and investigation. Further exploration in this area will significantly contribute to enhancing the overall quality of medical education and improving patient care in China.
This study aimed to address what essential medical humanistic competencies should medical undergraduates in China possess by the end of the fifth year.
Methods
Grounded theory methodology
Our research is based on the Charmaz’s constructive philosophical perspective [16], which asserts that new knowledge is actively constructed and the value of the embedded researcher acknowledged. We also acknowledge that knowledge is intimately linked to its context [17], 18]. Therefore, readers are encouraged to draw locally relevant inferences in light of the cultural and context-dependent complexities within the field of MHC.
A grounded theory methodology (GTM) was employed within a qualitative design framework to conduct coding and analysis, aiming to provide a qualitative perspective on the dimensions of medical humanistic competence. The primary data collection involved semi-structured interviews and document analysis, followed by inductive analysis using different GTM coding techniques, such as simultaneous data collection, constant comparison, memo writing [19], and coding, until theoretical saturation was achieved [20], 21]. This meticulous and iterative process not only yielded valuable insights but also facilitated a comprehensive understanding of MHC.
Data collection and sampling
From December 2022 to March 2023, we utilized purposive and theoretical sampling methods to recruit clinical educators and medical undergraduates from 10 medical universities in China [22]. For the clinical medical educators, the selection criteria included: (1) engagement in clinical medicinal practice and teaching, and (2) a minimum of two years of experience working in a hospital. Clinical educators without Chinese clinical doctor qualifications or teaching certification were excluded. As for the medical undergraduates, the inclusion criteria were: (1) being senior clinical medical undergraduates in their fifth year in China with a deeper understanding of medical humanities, and (2) having practiced in a clinical setting for more than three months. Data collection involved conducting semi-structured interviews with participants in various formats, including face-to-face and online video interviews, based on the preferences of each interviewee. The interviews were conducted in a comfortable and safe setting.
The interviewer was a female medical researcher who held a Doctor of Education (Ed.D) degree. Prior to this study, she received comprehensive training in qualitative research and had accumulated extensive experience in conducting interviews. The first and co-first author transcribed the audio recordings within 24 h after each interview to facilitate further analysis.
In-depth interview implementation
The effectiveness of these interviews largely depends on the interviewers’ ability to ask appropriate questions. To ensure the quality of the research, specific interview guidelines focusing on the research question have been designed. The interview outline includes the following questions: (1) What behaviors exhibited by a physician make you think that they are competent in medical humanistic skills? (2) Which medical humanities abilities are currently being cultivated through medical humanities education? In what areas do improvements need to be made? (3) What essential humanistic competencies should medical undergraduate possess? (4) What are the most important humanistic competencies that should be taught in medical schools? (5) Please provide a detailed description of a key event during your clinical practice where you utilized your humanistic competencies. By utilizing these interview guidelines, we aimed to gather valuable insights and data on the topic at hand.
Semi-structured interviews were conducted with the interviewee’s consent. Theoretical sampling pinpointed 32 participants from 10 universities across seven Chinese provinces, encapsulating 22 clinical medical educators, and 10 senior medical undergraduates. Verbal informed consent preceded each interview, which lasted between 1.5 and 2.0 h. Supplementary data were gleaned from direct or virtual participatory teaching observations and associated teaching blueprints, serving as triangulation evidence. These 32 co-researchers were involved in multiple interview rounds, adhering strictly to qualitative research standards. Participant details are enumerated in Table 1.
Basic information clinical medical educator interviewees.
| ID | Gender | Age | Professional title | Subject |
|---|---|---|---|---|
| CO1 | Female | 45 | Professor | Respiratory |
| CO2 | Male | 40 | Associate Professor | Neurosurgery |
| CO3 | Male | 55 | Lecturer | Pediatrics |
| CO4 | Female | 60 | Associate Professor | Dermatology |
| CO5 | Female | 46 | Associate Professor | Oncology |
| CO6 | Female | 36 | Lecturer | Gastroenterology |
| CO7 | Female | 37 | Assistant | Ophthalmology |
| CO8 | Male | 52 | Assistant | Cardiology |
| CO9 | Male | 40 | Professor | Hepatobiliary |
| C10 | Male | 39 | Professor | Otorhinolaryngology |
| C11 | Female | 38 | Associate Professor | Obstetrics and gynecology |
| C12 | Female | 51 | Associate Professor | Infectious diseases |
| M01 | Female | 36 | Professor | Medical psychology |
| M02 | Male | 47 | Professor | Medical ethics |
| M03 | Male | 56 | Associate Professor | Medical humanities education |
| M04 | Female | 32 | Associate Professor | Medical education |
| M05 | Female | 49 | Lecturer | Medical ethics |
| M06 | Female | 41 | Lecturer | Endocrinology |
| P02 | Female | 59 | Associate Professor | Anatomy |
| P03 | Male | 35 | Associate Professor | Pathology |
| P04 | Male | 46 | Professor | Biochemistry |
| P05 | Male | 29 | Professor | Immunology |
Data analysis
Thematic analysis of the primary data was conducted using the tri-level coding methodology of grounded theory. The process involved initially organizing, distilling, and synthesizing textual information that was relevant to the structure of medical undergraduates’ humanities competency. Figure 1 illustrates the data collection and analysis process.
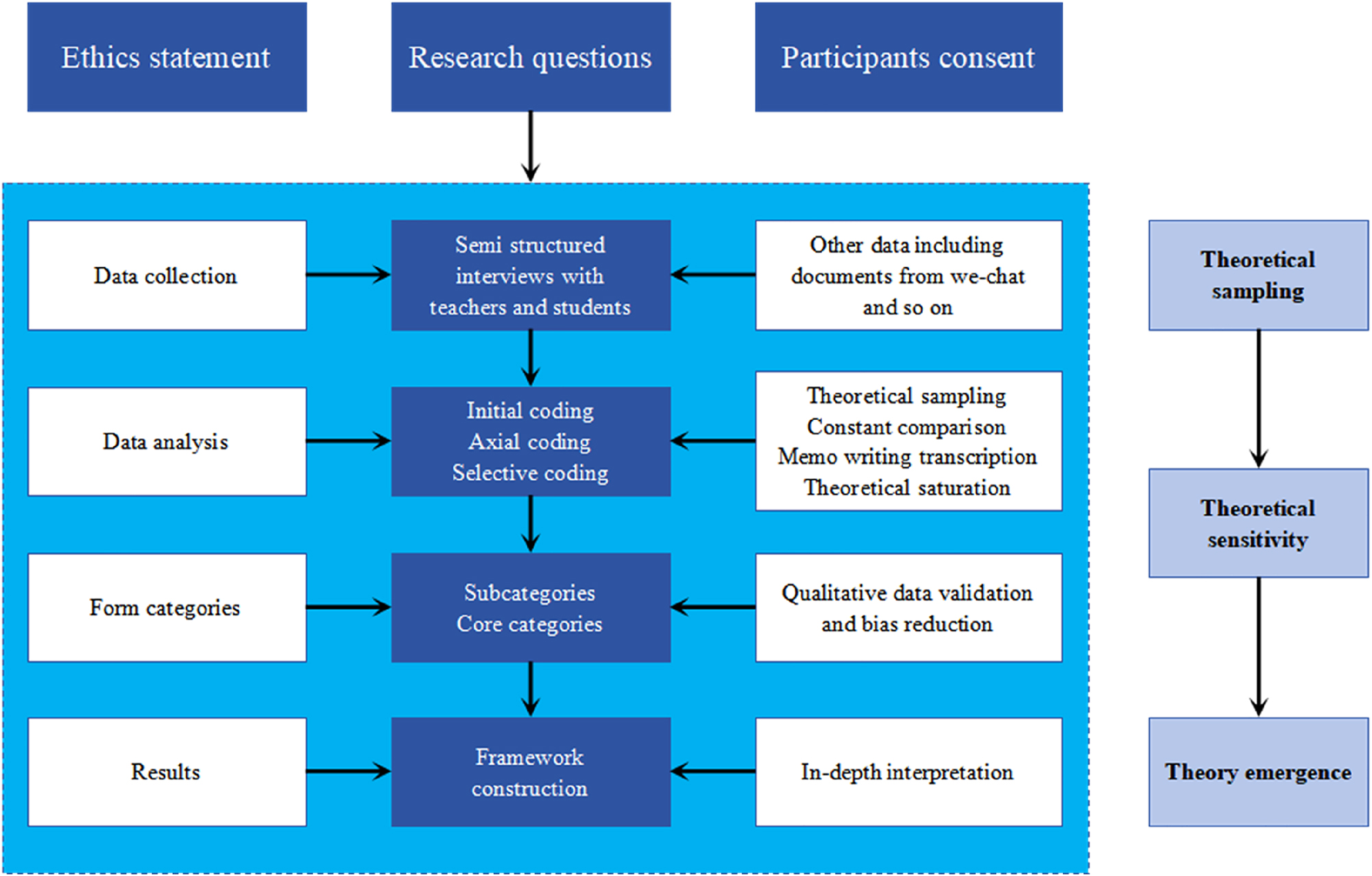
Data collection and analysis process.
In the “open coding” stage, the raw data was carefully deconstructed, examined, compared, and categorized. Categories emerged and concepts were refined through line-by-line and sentence-by-sentence coding, utilizing the original terms employed by the interviewees. Continuous comparison during the iterative process resulted in the abstraction of themes such as respect, empathy, narrative discourse, and therapeutic acknowledgment. From the interviews conducted with 32 participants, a total of 28 concepts were identified. During the “axial coding” stage, the objective was to discern and formalize relationships between established concepts and categories, showcasing their interplay. The 28 identified concept were grouped into five sub-categories: MHC, effective expression, therapeutic recognition, ethical compliance, and narrative competence. Moving to the “selective coding” stage, the aim was to identify core category and develop preliminary theories by linking the core category with ancillary ones. The comprehensive transcripts revealed four dimensions: comprehension of humanities, communication capacity, cooperation skill, and concern for “LEE” (law abidance, ethical reasoning, and emotional care).
Verification of theoretical saturation
Our iterative approach to data collection and interviewing ensured that the main categories remained consistent, with no novel categories emerging. This consistency demonstrated that our research had achieved theoretical saturation [23].
Ensuring study integrity
We implemented three strategies to bolster the study’s credibility.
Peer reviewing: Initial coding was executed by a primary researcher and scrutinized by another. Discrepancies were addressed by emphasizing the interviewee’s original language to enhance reliability.
Feedback mechanism: Preliminary findings were shared with peers and colleagues. Feedback from six academic experts on our initial coding results informed necessary refinements.
Triangulation: Data from interviews, observations and archival were juxtaposed and cross-verified. This multiple sourcing ensured a comprehensive understanding of the research data, strengthened the evidence base for our conclusions, and enhanced the credibility of our findings.
Furthermore, we drew upon reflexive grounded theory model to buttress both the study’s reliability and validity [24].
Results
The framework of the MHC model was developed through multiple stages of coding and constant comparison. The coding process is described in detail in Table 2. The model illustrates the four categories of MHC, which are presented in Figure 2.
Coding process of medical humanities competency for Chinese medical students.
| Selective coding (four primary categories) | Axial coding (12 sub-categories) | Open coding (28 tertiary indicators) |
|---|---|---|
| Comprehension of humanities | Medical humanities concept | Respect and care |
| Paramount life | ||
| Fairness and justice | ||
| Altruism | ||
| Medical humanities cognition | Knowledge of medical humanities | |
| Understanding the essence of medical humanities | ||
| Recognition of fundamental values of medical humanities | ||
| Medical humanities expression | Building relationships | |
| Continuous attention | ||
| Responding to patients | ||
| Communication capacity | Interpersonal communication | Active listening |
| Empathy | ||
| Effective expression | ||
| Multi-dimensional narration skill | Listening and understanding | |
| Verbal narration skill | ||
| Text narration skill | ||
| Cross-cultural communication ability | Cultural knowledge and understanding culture sensitivity | |
| Adaptability and flexibility | ||
| Cooperation skill | Team-building skills | Role assignment and conflict resolution |
| Facilitating collaboration | ||
| Interdisciplinary collaboration | Knowledge integration | |
| Team dynamics management | ||
| Shared problem-solving | Community consultation | |
| Shared decision-making | ||
| Concern for “LEE” | Law abidance | Legal awareness |
| Compliance with the law | ||
| Ethical reasoning | Ethical consciousness | |
| Ethical care | ||
| Emotional care | Attention to the patient | |
| Attention to self |
-
“LEE” stands for law abidance, ethical reasoning, and emotional care.
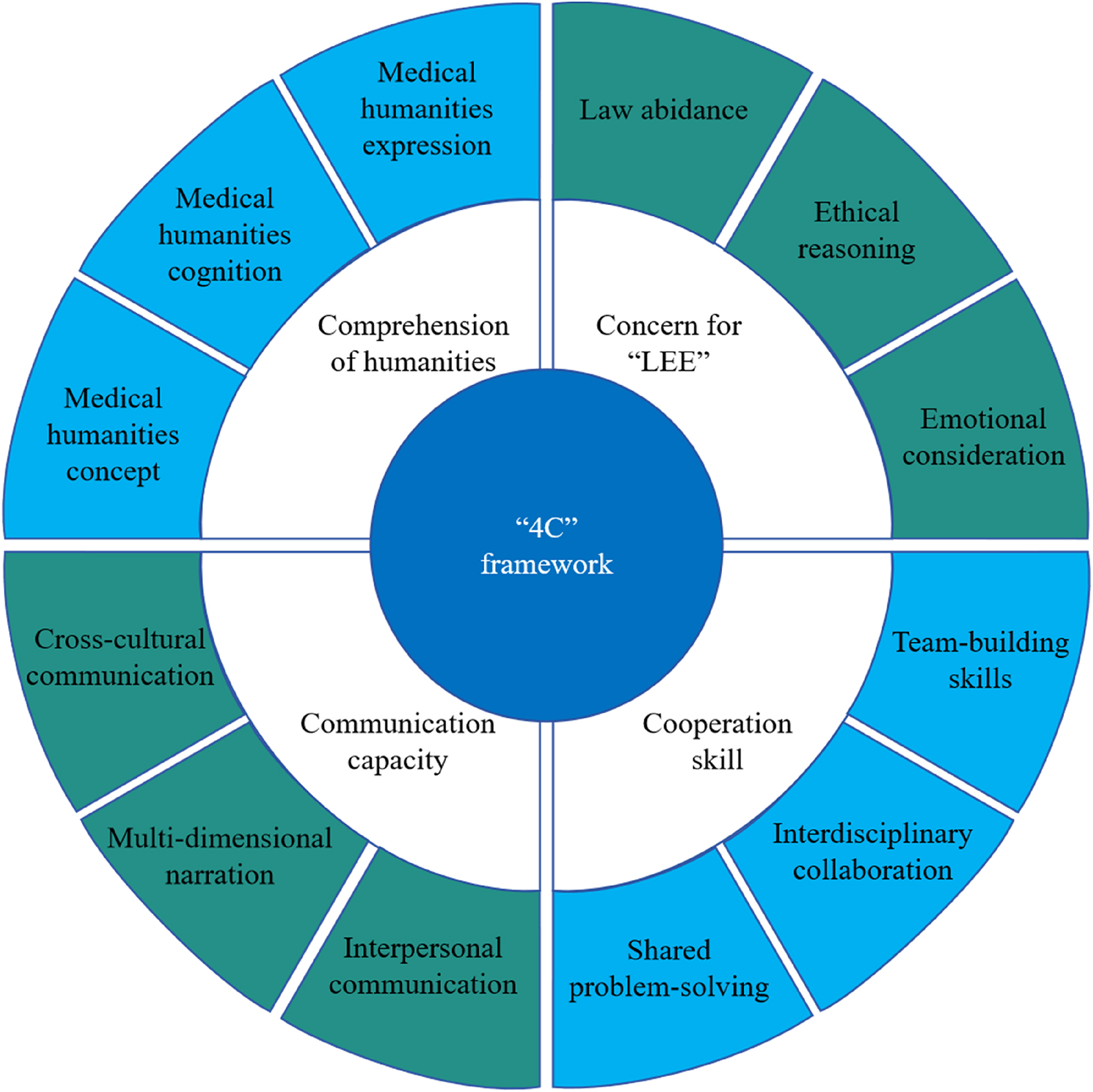
“4C” framework of medical humanities competency for Chinese medical students. “4C” framework: comprehension of humanities, communication capacity, cooperation skills, and concern for “LEE”; “LEE” stands for law abidance, ethical reasoning, and emotional care.
Category 1 – comprehension of humanities: medical humanities concept, medical humanities cognition, and medical humanities expression
The comprehension of humanities dimension is defined as espousing a balanced appreciation of both the scientific and humanistic facets of medicine, encapsulated within the holistic health humanities; understanding the basic connotation, value, and significance of medical humanities, and transforming one’s own cognition of medical humanities and the medical humanistic concept into medical humanistic practice. The results of the coding showed that the understanding of humanities dimension includes three sub-categories.
Medical humanities concept
The idea of medical humanities involves integrating humanistic disciplines with medical sciences in order to improve the quality and humanization of healthcare services. It emphasizes the importance of healthcare providers having a broad understanding of humanities and their applications. The medical humanities approach advocates for healthcare to go beyond the diagnosis and treatment of diseases, and also prioritize the overall well-being and quality of life of patients. It suggests that the practice of medicine should embody a humanistic spirit, while the humanities should be grounded in medical science. Three pivotal elements demarcate this: respect, prioritizing life, and justice. The principle of “respect and care” form the foundation of medical humanities, promoting empathy, reverence for life, and holistic patient care. The principle of “prioritizing life” places patient well-being at the center, while “fairness and justice” advocates for equal treatment, regardless of sociolect-economic differences. Illustratively, a vignette of a student diligently practicing surgical sutures exemplifies the integration of these principles, fostering a patient-centered attitude.
When I worked in both of our affiliated hospitals and support hospitals, I found that some medical interventions commonly used in affiliated hospitals were difficult to implement in the hospitals I supported. I am aware of the influence of different cultures and humanities concept in different regions on disease diagnosis and treatment measures, and I have also deeply experienced the cultural dimension of disease problems. Therefore, when diagnosing and treating diseases, I will not simply explore the biological causes and treatment methods. I will not ignore biology and only talk about social, psychological, and other medical humanistic factors, but consider biological and medical humanistic factors comprehensively.
(Interviewee teacher C07)
Medical humanities cognition
Medical humanities cognition refers to the acquisition and internalization of core principles of medical humanities through academic instruction. This includes gaining an understanding of humanistic foundational principles, reflecting on values derived from the humanities, and acquiring essential knowledge in the field. Medical humanities cognition plays a crucial role in healthcare as it helps healthcare professionals gain a broader perspective in understanding medical practice. For instance, teachers argue that compassion, often seen as an inherent quality, undergoes a transformation throughout medical education. It evolves from being a spontaneous reaction to becoming a deeply ingrained principle. This example illustrates the impact of medical humanities cognition.
Compassion is the starting point of medicine, and it is a spontaneous emotion that everyone has. How to transform this ‘spontaneous’ emotion of compassion into the ‘self-consciousness’ of medical students and finally internalize it into the ‘natural’ medical humanistic concept of medical students is the issue that medical humanistic education needs to consider.
(Interviewee teacher C02)
Medical humanities expression
This subcategory captures the pragmatic expression of imbued humanities knowledge in clinical settings. It underscores the significance of patient engagement, perpetual vigilance, and meaningful patient interactions. A poignant illustration is the empathetic rounds conducted for a terminal lung cancer patient, exemplifying the pinnacle of medical humanities in practice.
A patient with advanced lung cancer arrived at the emergency department. The diagnosis was clear, and the patient was aware of his/her condition. Despite medical technology being unable to offer any potential interventions, the number of doctor rounds in our group increased due to the inclusion of medical humanities rounds. Through these rounds, we expressed care by greeting the patient with compassionate words, conveying empathy through our eyes, and offering support with a comforting touch on the shoulder. This experience exemplifies the most remarkable medical humanities rounds I have ever seen.
(Interviewee teacher C06)
Category 2 – communication capacity: interpersonal communication, multi-dimensional narration, and cross-cultural communication
Communication capacity is essential for medical students, constituting an amalgamation of knowledge, abilities, and attitudes ensuring effective communication. This skillset is multi-faceted, encapsulating language proficiency, narrative aptitude, reading proficiency, writing capabilities, cognitive insights, and socio-emotional adeptness. The coding results showed three sub-categories of communication skills.
Interpersonal communication
This dimension focuses on the dyadic interaction between medical professionals and patients. It emphasizes the ability to establish and maintain effective communication with patients, including active listening to patient needs, concerns, and feelings, and demonstrating empathy to understand emotions and perspectives from the patient’s standpoint. As stated in the World Medical Association’s Declaration of Fukuoka, the absence of empathy is as detrimental as a technical shortcoming [25]. Compassionate interaction serves as a pivotal aspect of the physician-patient relationship, evolving beyond a humanistic trait into a demonstration of social responsibility. Additionally, medical students should be able to explain medical information using clear and concise language to establish trust and enhance patient engagement.
Multi-dimensional narration
It is a sub-category that intersects with narrative medicine. It involves organizing patient experiences into coherent accounts, whether in written or oral form. These narratives reveal the inner worlds of patients, medical practitioners, and other stakeholders, enabling a deeper understanding and interpretation of diseases and their impact on individuals. This capability encompasses two branches: “listening and comprehension” and “textual and verbal narrations.” “Listening and comprehension” refers to the ability to accurately understand information conveyed by patients and their families through various forms of communication, such as speech, writing, and other mediums. It also involves grasping underlying intentions, emotions, attitudes, and values. Active listening and proficiency in literary reading are the two essential components of this ability. “Textual narrations” serve as scripts, while “verbal narrations” focus on explicit articulation based on these scripts. This culmination leads to the development of humanistic diagnostic and treatment strategies.
Cross-cultural communication
This refers to the ability to effectively communicate with patients from different cultural backgrounds, including appropriate cultural knowledge and understanding, culture sensitivity, and adaptability and flexibility.
Cultural knowledge and understanding: acquiring knowledge about different cultures, traditions, customs, and healthcare practices is essential for effective cross-cultural communication. Understanding cultural nuances and incorporating this knowledge into communication can help build trust and bridge cultural gaps.
Cultural awareness and sensitivity: Having awareness and sensitivity towards different cultural norms, values, beliefs, and practices is crucial for successful cross-cultural communication. Sensitivity involves recognizing and respecting cultural differences and adapting one’s communication style accordingly.
Adaptability and flexibility: Being adaptable and flexible in communication styles, approaches, and problem-solving methods are essential when encountering cultural differences. Adapting to different communication norms, adjusting one’s behavior, and finding creative solutions to overcome challenges is necessary for successful cross-cultural communication.
Medicine’s core is human interaction, underpinned by ethics. This statement highlights the fundamental importance of the doctor-patient relationship. A personal experience with a clinical instructor serves as a poignant reminder of the profound impact that poorly chosen words can have. The memory of the instructor’s insensitive remarks to a young leukemia patient still evokes feelings of sorrow. The child’s silent but piercing gaze in response to these remarks was deeply unsettling, underscoring the significant effects of communication in clinical settings.
(According to interviewee teacher C09)
Category 3 – cooperation skill: team-building skills, interdisciplinary collaboration, and shared problem-solving
Cooperation skill in medical education refers to the ability of medical students and professionals to effectively collaborate and work together in a healthcare setting to provide optimal patient care. It encompasses three key aspects.
Team-building skills
Given the wide range of professionals in healthcare, the ability to build a harmonious and efficient team is essential. Students should have the skills to promote an environment that encourages cooperation and shared decision-making.
Interdisciplinary collaboration
This sub-dimension focuses on teamwork among healthcare professionals from various disciplines. It emphasizes the ability to collaborate effectively in interdisciplinary teams to enhance patient outcomes and foster holistic care.
Shared problem-solving
It refers to the ability of medical students and healthcare professionals to collaborate in analyzing, deliberating, and addressing clinical issues by integrating their collective expertise, experience, and perspectives. This multi-disciplinary team approach allows for comprehensive patient care that is more effective and personalized, as different professionals contribute unique insights that can lead to better clinical decisions and outcomes.
In medical education, developing cooperation skills involves creating learning environments and situations – such as simulations, case discussions, and team-based learning opportunities – where students can practice these skills and receive feedback on their performance. This includes interprofessional education (IPE) where students from various healthcare disciplines learn with, from, and about each other to improve collaboration and the quality of care.
Category 4 – concern for “LEE”: law abidance, ethical reasoning, and emotional consideration
The acronym “LEE” represents the integration of three crucial elements in the provision of medical services: law abidance, ethical reasoning, and emotional care. The concept of concern for “LEE” emphasizes the deep and inseparable integration of medical humanities with medical science. It showcases a distinct humanistic approach to medical thought and practice, highlighting the significance of integrating legal, ethical, and emotional aspects in patient care [26], [27], [28]. This integration can be further classified into three distinct subcategories.
Law abidance
This foundational layer emphasizes the necessity for medical students to navigate their practice within legal boundaries. Acute awareness of relevant laws, ensuring patient privacy, and safeguarding one’s rights within legal confines are vital.
Ethical reasoning
Beyond the realm of law lies the sphere of ethics. Medical students should maintain a strong ethical compass, adhering to both ethical guidelines and moral principles, especially when navigating the intricate relational dynamics within the medical field.
Emotional consideration
Emotional consideration represents the zenith of this dimension by focusing on the human element of medical practice. At its core, emotional consideration champions a patient-centric ethos and aims to cultivate a sense of community in treatment. It takes into account various contextual factors such as family dynamics, culture, and individual nuances. This approach emphasizes the importance of cultural sensitivity and awareness. It also encompasses addressing the emotional ups and downs experienced by patients, catering to their psychological needs, and providing comprehensive emotional and psychological support [29], 30].
There was a situation where a gout patient, who happened to be a fellow doctor, approached Teacher C05. The patient’s daughter, who was also a medical professional, requested a specific prescription that would exceed the standard medical costs. However, Teacher C05, taking into account the unique circumstances, developed a collaborative treatment strategy. This approach was in line with legal and ethical standards, while also considering the patient’s particular situation and promoting active participation from both the patient and their family in the treatment process.
(According to interviewee teacher C05)
Discussion
Quality analysis of developing a model of MHC
The study aimed to develop a middle-range theory of MHC model for medical undergraduates, utilizing a systematic application of grounded theory methodologies for synchronous data acquisition, analysis, and abstraction of theoretical concepts. Sample selection aligned with theoretical needs, adopting the grounded theory’s theoretical sampling technique. This iterative process continued until reaching theoretical saturation, where no fresh insights emerged. The research findings are deeply rooted in the raw and triangulation verification data. The entire analysis process was data-driven in a “bottom-up” way, which allowed the codes and themes to emerge inductively from the data [31]. Although face-to-face interviews were the primary data source, the research embraced a multi-faceted approach, incorporating diverse data such as observations, documents, articles, charts, and more. This diversified data pool enriched the conceptual generation related to Chinese medical students’ MHC, ensuring the resultant theory’s relevance and robust explanatory strength. Employing feedback methods, among others, ensured the research’s credibility and validity. As a result, the framework presented exhibits a commendable level of reliability and applicability.
The unique trait of the MHC model within Chinese culture context
Within the Chinese cultural context, the MHC model exhibits several distinctive traits. One notable trait is its integration with the competency model of medical undergraduates. This interconnection highlights the significance of MHC as a professional competence, emphasizing its essential role in the comprehensive development of medical students. Additionally, the MHC model is shaped by distinct Chinese cultural attributes. These attributes recognize the importance of cultural sensitivity and empathy in patient care. Chinese culture places great emphasis on harmony, respect, and interpersonal relationships. As such, the MHC model incorporates these values into its framework, emphasizing the need for medical undergraduates to cultivate effective communication skills, empathy, and cultural understanding. Furthermore, the MHC model acknowledges the importance of humanistic education in medical training. It emphasizes the need for a specialized and scientific approach to medical humanities education. This approach aims to deepen medical students’ understanding of the social, cultural, and ethical dimensions of healthcare, enabling them to provide more comprehensive and patient-centered care. By integrating these unique traits, the MHC model within the Chinese cultural context contributes to the cultivation of well-rounded and culturally competent medical professionals. The “4C” framework (comprehension of humanities, communication capacity, cooperation skills, and concern for “LEE”) represents a distinctive Chinese approach to medical humanities education that both complements and contrasts with Western models like CanMEDS (representing for communicator, collaborator, leader, health advocate, scholar, and professional) and ACGME (representing for patient care, medical knowledge, interpersonal and communication skills, professionalism, practice-based learning and improvement, and systems-based practice) in three significant aspects. Structurally, it moves beyond the role-based compartmentalization of Western frameworks by organically integrating narrative medicine, legal-ethical-emotional reasoning, and interdisciplinary collaboration into a unified system – reflecting China’s holistic medical philosophy. Culturally, it embeds Confucian values like ren (benevolence) and physician-patient harmony into its core competencies, offering a collectivist counterpoint to Western individualism. Practically, its innovative legal-ethical-emotional dimension addresses the unique demands of family-centered decision-making prevalent in Chinese clinical contexts. These culturally-grounded innovations provide valuable alternative perspectives while maintaining constructive dialogue with global medical education standards.
The “4C” framework offers several contributions in the field of medical humanities
The “4C” framework makes significant contributions to the field of medical humanities. Firstly, the model provides a comprehensive competency structure, presenting an inclusive framework that meticulously categorizes competencies within medical humanities into well-defined and explicit dimensions. This systematic categorization facilitates the methodical instruction, acquisition, and evaluation of these competencies. The framework expands the understanding and scope of medical students’ communication skills by incorporating narrative medicine as a multi-dimensional narrative competence and incorporating multi-dimensional storytelling into the communication skills dimension. Additionally, it innovatively integrates legal, ethical, and emotional reasoning into the core dimension of “LEE,” viewing it as a form of medical humanistic thinking and action. Secondly, the “4C” framework emphasizes the importance of integrating medical humanities into clinical education and practice. It recognizes medical humanities as a fundamental component of healthcare professional education and highlights its role in enhancing patient-centered care and communication. Thirdly, the framework promotes interdisciplinary collaboration in the field of healthcare. It emphasizes the significance of effective communication and collaboration among healthcare professionals, patients, families, and other members of the healthcare team. This collaborative approach improves patient care outcomes and contributes to a more holistic and compassionate healthcare environment. Fourthly, the “4C” framework recognizes the diverse cultural and social aspects of healthcare. It highlights the need for medical professionals to understand and appreciate cultural diversity, as well as the ability to navigate ethical dilemmas and provide culturally sensitive care. Overall, the “4C” framework adopts a holistic systems approach to construct a structural model of medical humanities literacy for medical students. It offers valuable insights and guidelines for developing medical humanities competence, promoting patient-centered care, facilitating interdisciplinary collaboration, and addressing cultural and ethical complexities in healthcare. This theory contributes to a more comprehensive understanding of medical humanities education and can have an impact on fields such as medical education. By incorporating these principles into medical education, this framework has the potential to elevate the medical profession to new heights, ensuring that healthcare professionals are well-rounded and capable of providing holistic care to their patients [31].
The “4R” approach for cultivating competencies
A method to enhance MHC among medical students was suggested based on the established theoretical MHC model. This approach encompasses four fundamental principles: rules, relevance, responsiveness, and reflective practice.
“Rules” underscores the adoption of the MHC theoretical model as the foundational framework guiding the implementation of medical humanities education. “Relevance” addresses the need to anchor the educational content of medical humanities, both in classroom and practical settings, to the MHC model. This principle stresses that medical humanities educational initiatives should align with societal expectations and patient needs. “Responsiveness” calls for the continual evaluation and refinement of medical students’ MHC by medical institutions, advocating for ongoing assessments and corresponding adjustments to educational activities based on these evaluations. Lastly, “reflective practice” advocates for the incorporation of reflective exercises – such as journaling, peer discussions, and ethical dilemma analysis – to promote self-awareness and ethical reasoning, thereby enabling medical undergraduates to better their MHC and deliver more compassionate care. The “4R” approach ensures that medical humanities education is in concert with the MHC theoretical framework, with an emphasis on relevance, continuous responsiveness to evolving societal needs, and dynamic adjustments within the medical field [32], 33].
This study verified the effectiveness of the “4C”–“4R” co-cultivation mechanism through typical clinical cases. Taking “tumor condition notification” as an example in humanistic teaching for medical students, the approach integrates medical narrative theory (understanding), SPIKES communication guidelines (communication), and multi-role simulation exercises (cooperation), and ethical reflection reports (“LEE” care). It also involves dynamic adjustments to training content (responsiveness) based on monthly patient satisfaction surveys. This comprehensive training chain significantly improved the excellent rate in humanistic literacy evaluations among medical students and reduced the incidence of medical disputes. This empirical study confirmed the “4R” strategies systematically support the cultivation of “4C” capabilities, which is highly consistent with existing theoretical models.
Limitations
The primary limitation of this study is its exclusive dependence on qualitative research. Despite the intentional design to procure qualitative insights via interviews, the research did not undertake the gathering of quantitative data, which could serve for empirical testing of the findings. Future research should consider executing extensive surveys informed by the current study’s outcomes, collecting both quantitative and qualitative data. This mixed-methods approach would help in substantiating the conclusions drawn from the qualitative data. Nevertheless, as a grounded theory study, it provides an initial, methodologically sound, and scientifically corroborated foundation for the construction of medical humanities indicators.
Conclusions
The study developed a structured framework, known as the “4C” framework, for Chinese medical undergraduates. This framework consists of four dimensions: comprehension of humanities, communication capacity, cooperation skill, and concern for “LEE”. The development of the framework was based on rigorous evidence and scientific methodology. It highlights the complex interplay between these dimensions, with understanding humanities serving as a foundational concept and knowledge, communication and cooperation as essential skills, and concern for “LEE” as a representation of humanistic thinking and action. In the clinical setting, we defined MHC as holistic skills necessary for navigating relationships with oneself, peers, society, and medical technologies. This article addresses the persistent absence of an overarching theoretical framework for medical humanities education. The identification of these competencies will benefit medical students, teachers, health institutions, and governments. They can utilize the “4C” framework to better structure their curriculum and training programs for medical humanities education [33]. Furthermore, it can help identify areas where current medical humanities activities do not meet these competencies. The “4C” framework has the potential to explore new functions of medicine and contribute to the field.
Funding source: Sichuan Province Educational Research Project
Award Identifier / Grant number: SCJG23A031
Funding source: Medical Education of the Chinese Medical Association and National Center for Health Professions Education Development
Award Identifier / Grant number: 2023A39
Acknowledgments
The authors express appreciation for those participating and supporting the research.
-
Research ethics: The study was approved by the Research Ethics Committee of the School of International Education, Southwest Medical University [approval number SIESWMUIRB-202207216]. All participants gave informed consent before participating. All methods were carried out in accordance with relevant guidelines and regulations. All procedures followed the ethical standards of the Declaration of Helsinki.
-
Informed consent: Written informed consent was obtained from all participants prior to the study.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: No AI or machine learning tools were used in the writing or analysis of this manuscript. The final content was verified by the authors.
-
Conflict of interest: All authors declare no conflicts of interest.
-
Research funding: This study was supported by key project of the Chinese medical association medical education branch & national center for health professions education development [grant number 2023A39]; key project of the Sichuan provincial department of education [grant number JG2024-0858].
-
Data availability: The datasets generated during this study are available from the corresponding author upon reasonable request.
References
1. Singh, S, Dhaliwal, U, Singh, N. Developing humanistic competencies within the competency-based curriculum. Indian Pediatr 2020;57:1060–6. https://doi.org/10.1007/s13312-020-2036-y.Search in Google Scholar PubMed PubMed Central
2. Petrou, L, Mittelman, E, Osibona, O, Panahi, M, Harvey, JM, Patrick, YAA, et al.. The role of humanities in the medical curriculum: medical students’ perspectives. BMC Med Educ 2021;21:179. https://doi.org/10.1186/s12909-021-02555-5.Search in Google Scholar PubMed PubMed Central
3. Macnaughton, J. The humanities in medical education: context, outcomes and structures. Med Humanit 2000;26:23–30. https://doi.org/10.1136/mh.26.1.23.Search in Google Scholar PubMed
4. Bolton, G. Medicine, the arts, and the humanities. Lancet 2003;362:93–4. https://doi.org/10.1016/s0140-6736(03)13894-9.Search in Google Scholar
5. General Medical Council. Tomorrow’s doctors: recommendations on undergraduate medical education. London: General Medical Council; 1993.Search in Google Scholar
6. Core Committee, Institute for International Medical Education. Global minimum essential requirements in medical education. Med Teach 2002;24:130–5. https://doi.org/10.1080/01421590220120731.Search in Google Scholar PubMed
7. Bhutta, ZA, Chen, L, Cohen, J, Crisp, N, Evans, T, Fineberg, H, et al.. Education of health professionals for the 21st century: a global independent commission. Lancet 2010;375:1137–8. https://doi.org/10.1016/s0140-6736(10)60450-3.Search in Google Scholar
8. Tan, X, Liu, X, Shao, H. Healthy China 2030: a vision for health care. Value Health Reg Issues 2017;12:112–4. https://doi.org/10.1016/j.vhri.2017.04.001.Search in Google Scholar PubMed
9. Coronado-Vázquez, V, Antón-Rodríguez, C, Gómez-Salgado, J, Ramírez-Durán, MDV, Álvarez-Montero, S. Evaluation of learning outcomes of humanities curricula in medical students: a meta-review of narrative and systematic reviews. Front Med 2023;10:1145889. https://doi.org/10.3389/fmed.2023.1145889.Search in Google Scholar PubMed PubMed Central
10. Rolfe, IE, Pearson, S, Powis, DA, Smith, AJ. Time for a review of admission to medical school? Lancet 1995;346:1329–33. https://doi.org/10.1016/s0140-6736(95)92344-6.Search in Google Scholar PubMed
11. Cohen, JJ, Banks, JL, Majid, A. Medical humanities in medical education. South Med J 2019;112:85–7.Search in Google Scholar
12. Chen, L, Zhang, J, Zhu, Y, Shan, J, Zeng, L. Exploration and practice of humanistic education for medical students based on volunteerism. Med Educ Online 2023;28:2182691. https://doi.org/10.1080/10872981.2023.2182691.Search in Google Scholar PubMed PubMed Central
13. Kosik, RO, Fan, AP, Ren, Y, Jiang, B, Hsu, Y, Li, W, et al.. Medical humanities education in China: an exploratory cross-sectional study. Lancet 2018;392:S47. https://doi.org/10.1016/s0140-6736(18)32676-x.Search in Google Scholar
14. Sajid, I, Ashiq, U, Sajid, RI. Paradigm shifting from bio-medical to bio-psycho-social and role of medical social work. Pak J Med Health Sci 2021;15:1047–50. https://doi.org/10.53350/pjmhs211551047.Search in Google Scholar
15. Chen, L. From biomedicine to bio-psycho-human-social medicine. J Xiangya Med 2017;2:1–4.Search in Google Scholar
16. Birks, M, Mills, J. Grounded theory: a practical guide, 2nd ed. London: SAGE Publications; 2015.10.4135/9781473920163.n1Search in Google Scholar
17. Charmaz, K, Thornberg, R, Keane, E. Evolving grounded theory and social justice inquiry. In: Denzin, NK, Lincoln, YS, editors. The SAGE handbook of qualitative research, 5th ed. Thousand Oaks, CA: SAGE Publications; 2017:411–43 pp.Search in Google Scholar
18. Singh, S, Estefan, A. Selecting a grounded theory approach for nursing research. Global Qual Nurs Res 2018;5:2333393618799571. https://doi.org/10.1177/2333393618799571.Search in Google Scholar PubMed PubMed Central
19. Lempert, LB. Asking questions of the data: memo writing in the grounded theory tradition. In: Bryant, A, Charmaz, K, editors. The SAGE handbook of grounded theory. Los Angeles, CA: SAGE Publications; 2007:245–64 pp.10.4135/9781848607941.n12Search in Google Scholar
20. Smith, J, Johnson, A. Understanding the grounded theory methodology: a qualitative approach. J Res Methodol 2022;8:112–30.Search in Google Scholar
21. Al-Eisawi, DA. A design framework for novice using grounded theory methodology and coding in qualitative research: organisational absorptive capacity and knowledge management. Int J Qual Methods 2022;21:1–14. https://doi.org/10.1177/16094069221113551.Search in Google Scholar
22. Moser, A, Korstjens, I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract 2018;24:9–18. https://doi.org/10.1080/13814788.2017.1375091.Search in Google Scholar PubMed PubMed Central
23. Low, J. A pragmatic definition of the concept of theoretical saturation. Sociol Focus 2019;52:131–9. https://doi.org/10.1080/00380237.2018.1544514.Search in Google Scholar
24. Engward, H, Davis, G. Being reflexive in qualitative grounded theory: discussion and application of a model of reflexivity. J Adv Nurs 2015;71:1530–8. https://doi.org/10.1111/jan.12653.Search in Google Scholar PubMed
25. Epstein, RM, Hundert, EM. Defining and assessing professional competence. JAMA 2002;287:226–35. https://doi.org/10.1001/jama.287.2.226.Search in Google Scholar PubMed
26. Engel, GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–36. https://doi.org/10.1126/science.847460.Search in Google Scholar PubMed
27. Borrell-Carrió, F, Suchman, AL, Epstein, RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med 2004;2:576–82. https://doi.org/10.1370/afm.245.Search in Google Scholar PubMed PubMed Central
28. Fekete, AC, Fekete, MC, Greculescu, A. Factors influencing psychosocial communication in the reason/emotion society. Procedia Soc Behav Sci 2014;128:123–7. https://doi.org/10.1016/j.sbspro.2014.03.129.Search in Google Scholar
29. Brown, L. Cultural sensitivity and awareness in healthcare. J Cult Diversity Health Illness 2018;15:78–92.Search in Google Scholar
30. Johnson, R. Emotional considerations in patient care. N Engl J Med 2017;375:789–96.Search in Google Scholar
31. Braun, V, Clarke, V. Successful qualitative research: a practical guide for beginners. London: SAGE Publications; 2013.Search in Google Scholar
32. Stukas, AA, Snyder, M, Clary, EG. Understanding and encouraging volunteerism and community involvement. J Soc Psychol 2016;156:243–55. https://doi.org/10.1080/00224545.2016.1153328.Search in Google Scholar PubMed
33. Carr, SE, Noya, F, Phillips, B, Harris, A, Scott, K, Hooker, C, et al.. Health humanities curriculum and evaluation in health professions education: a scoping review. BMC Med Educ 2021;21:568. https://doi.org/10.1186/s12909-021-03002-1.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


