Abstract
Japan’s medical education system has evolved significantly over recent decades, adapting to societal demands, an aging population, and technological advancements in healthcare. Grounded in universal health coverage, Japan’s healthcare framework emphasizes accessibility and high-quality care, necessitating a medical education system capable of producing competent and compassionate physicians. The six-year undergraduate medical program progresses through foundational sciences, clinical exposure, and hands-on training, culminating in national licensing examinations. Key milestones include assessments such as the objective structured clinical examination (OSCE) and computer-based test (CBT), which became nationally standardized in 2023. The post-graduate pathway incorporates outcome-based residency system and specialized training programs. This structured approach ensures that Japanese physicians are prepared for the complexities of modern healthcare, including team-based care models and interdisciplinary collaboration. Recent reforms in the “Model Core Curriculum” emphasize outcome-based education, focusing on patient-centered care and technological adaptability. Challenges such as physician overwork, workforce shortages, and integrating advanced technologies remain, prompting systemic reforms like work style changes and task shifting. By addressing these challenges, embracing innovations, and maintaining alignment with global standards, Japan’s medical education system continues to prepare healthcare professionals to meet evolving demands and sustain the nation’s healthcare excellence.
Introduction: background of the Japanese medical education
Medical education in Japan has evolved significantly over the past few decades, adapting to the changing needs of the healthcare system and the demands of modern medical practice. As a background of medical education, the Japanese healthcare system, known for its universal health coverage (UHC) [1], places a high emphasis on the quality and accessibility of medical services. Japan’s UHC ensures that all citizens have access to medical care. This system is supported by public health insurance schemes. Long-term care insurance, introduced in 2000, provides coverage for elderly care, reflecting the country’s aging population. These insurance systems ensure that medical education produces doctors capable of working within a framework that prioritizes accessibility and comprehensive care.
The Public Assistance in Japan ensures that even those without sufficient financial means can access necessary medical services [2]. Free access to healthcare facilities allows patients to visit most hospitals or clinics without restrictions. This system necessitates a medical education framework that prepares future doctors to manage a diverse range of medical conditions and patient demographics.
Advanced treatment hospitals are integral to medical education in Japan because all of them are representative university hospitals in Japan. These 88 major hospitals across the country serve as hubs of advanced medical care, research, and education, offering medical students and interns invaluable opportunities for practical hands-on training. The Ministry of Education, Culture, Sports, Science and Technology (MEXT) oversees medical education up to graduation, ensuring alignment with academic and professional standards, while the Ministry of Health, Labour and Welfare (MHLW) takes charge of post-graduation medical training, ensuring it meets national healthcare requirements.
Structure of medical education in Japan
Undergraduate medical education
Medical education in Japan starts with a six-year undergraduate program, where students are trained in both basic sciences and clinical skills. For example, the curriculum of Kyushu University School of Medicine is divided into three phases: the introductory phase (the first year), the basic and developmental phase (the second to the fourth years), and the integration phase (the fifth and sixth years). In the introductory phase, the education focuses on liberal arts education, designed to cultivate critical thinking, ethical reasoning, and a broad understanding of various disciplines. This foundation aims to prepare students for the multi-disciplinary nature of modern medicine. In the basic and developmental phase, the curriculum shifts to foundational medical sciences, including anatomy, physiology, biochemistry, pathology, and pharmacology. These subjects are taught through a combination of traditional lectures and hands-on simulations, ensuring that students acquire both theoretical knowledge and practical skills essential for clinical practice.
Before entering the integration phase, students are required to pass two common achievement tests as critical assessments at the end of the fourth year: pre-clinical clerkship objective structured clinical examination (Pre-CC OSCE) and the computer-based test (CBT), which are organized by the Common Achievement Tests Organization (CATO). These assessments test the student’s readiness to transition into clinical practice and ensure a uniform competency standard across all medical schools in Japan. The Pre-CC OSCE and CBT were officially certified as national examinations in Japan in 2023. All students who pass these exams receive a certification badge, which is required to progress to the next phase and begin clinical training.
The integration phase, also called bedside learning (BSL) or clinical clerkship, introduces students to patient care in real-world settings through rotations in various specialties, including internal medicine, surgery, obstetrics, pediatrics, and psychiatry. This hands-on training helps students bridge the gap between theoretical knowledge and practical application. Students also participate in team-based learning activities and engage in case discussions, further refining their clinical reasoning and communication skills. In this phase, students are also sent to clinics, home visits, and regional hospitals to gain the ability to manage common diseases and provide care for elderly people or patients.
In Japan, the academic year begins in April and concludes in March of the following calendar year. In the last school year (sixth grade), the students will have a post clinical clerkship OSCE (Post-CC OSCE) at the end of the clinical clerkship. Some universities will also have their own examinations for graduation qualification (e.g. Kyushu University has the graduation examination in October). These examinations are not national examinations but the most important test of the six-year program to be certificated to graduate from the school of medicine. After these examinations, in the coming February, the students will join the National Medical Licensing Examination (NMLE) just two months before their graduation (Figure 1). The students can graduate and proceed to the junior residency after they get the national medical license.
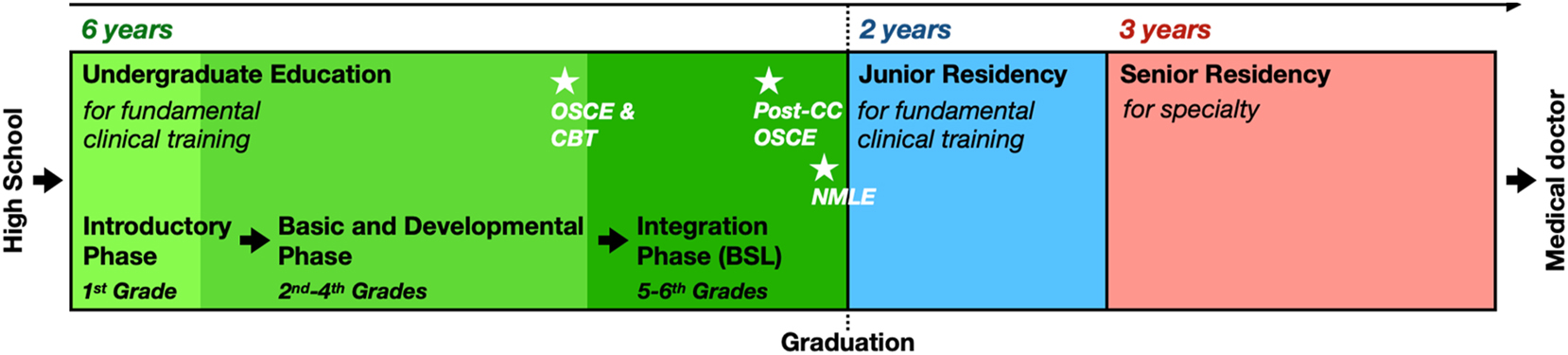
The general schedule of the medical education and residency system in Kyushu University School of Medicine. OSCE, objective structured clinical examination; CBT, computer-based test; Post-CC, post clinical clerkship; BSL, bedside learning; NMLE, National Medical Licensing Examination.
Residency system in Japan
After graduation, students begin a two-year junior residency program which is arranged through the Japan Residency Matching Program (JRMP), a merit-based system established in 2004. During this phase, known as kenshu-i in Japanese, junior residents rotate through various departments, including internal medicine, surgery, and emergency medicine, gaining diverse clinical exposure. This period is crucial for developing diagnostic acumen, procedural skills, and patient management strategies.
The JRMP ensures that residents are placed in hospitals that match their preferences and abilities. The process involves written examinations, interviews, and a ranking system. University hospitals play a pivotal role in this phase, acting as both sending institutions and receiving centers for trainees. The months of March and April, marking the transition between academic years, are particularly hectic as these hospitals coordinate graduations and placements.
Upon completing the junior residency, doctors can pursue specialist training, which typically lasts three to five years and is governed by the Japanese Board of Medical Specialties (JBMS). This training allows doctors to specialize in fields such as cardiology, gastroenterology, neurology, and surgery. The curriculum emphasizes practical training, research, and mentorship under senior specialists or doctors in hospitals or other medical fields. Specialist training in Japan is structured to balance clinical service with academic development. Trainees will work as doctors as daily work and are also encouraged to participate in research and present findings at academic conferences. This dual focus on clinical and academic excellence ensures that specialists are well-equipped to handle complex cases while contributing to advancements in medical science. Japan’s postgraduate training system is often compared to the UK’s structured pathway, where residents follow a defined curriculum tailored to their specialty.
Lifelong medical education and medical specialist
In Japan, medical licensure is permanent and does not require renewal, unlike in countries such as the United States, where continuing medical education (CME) is mandatory for license maintenance. While the Japan Medical Association (JMA) offers a lifelong education system for its members, participation is voluntary and not legally enforced. Continuing education after the senior residency period is largely self-directed, relying on individual physicians’ commitment to professional development.
However, after completing the 2-year junior residency, most doctors choose their specialty and join a related academic society. These societies not only provide structured opportunities for continued education, including participation in academic conferences, specialized training workshops, and educational lectures, but also offer certification as a medical specialist in the chosen field. To obtain and maintain specialist certification, physicians must actively engage in these activities, as presenting research or attending conferences is often required. Specialist certification is also beneficial for career development, as it can be advertised in private practice settings, making it a valuable credential. Consequently, many physicians – especially those in independent clinics – continue their education through society-organized academic activities to maintain their specialist status and stay updated with advancements in their field.
Curriculum, schools, evaluation, and accreditation
The “Model Core Curriculum”
The Model Core Curriculum for Medical Education in Japan, revised in 2022, provides a standardized yet adaptable framework designed to ensure consistent, high-quality medical education across all universities [3]. Developed under the MEXT, this curriculum outlines essential competencies and learning objectives that medical students must achieve to meet the ever-evolving demands of healthcare and society. Covering approximately two-thirds of the total study hours, the curriculum allows individual universities the flexibility to customize their remaining program components based on their unique institutional goals.
The 2022 revision addresses critical societal and medical challenges expected by 2040, including an aging population, the prevalence of chronic diseases, increasing health disparities, and the rapid advancement of medical technologies. It adopts an outcome-based educational approach, emphasizing ten core competencies that every graduate must develop to succeed in modern healthcare as shown in Table 1 [4].
Basic qualities and abilities required of physicians and their explanations, defined by the Model Core Curriculum for Medical Education in Japan (2022 revision).
| Basic qualities and abilities | Explanations |
|---|---|
| PR: professionalism | Acknowledge the professional responsibility of physicians to be deeply involved in people’s lives and to protect health; respect diversity and humanity; and take an altruistic approach to medical practice throughout one’s career |
| GE: generalism | Take a multi-systemic view of the patient’s problems and consider the patient’s psychosocial background in order to provide comprehensive, flexible medical care that responds to the needs of the patient and is not limited to one’s own specialty, supporting the achievement of individual and societal well-being |
| LL: lifelong learning | Continuously reflect on one’s own practice and train collaboratively with other physicians and healthcare professionals, actively engaging in lifelong education and self-directed learning, in order to practice safe and high-quality medical care |
| RE: research | Understand the importance of medical research for the advancement of medicine and medical care, and support innovation in medicine through involvement in academic and research activities, developing one’s scientific thinking skills |
| PS: problem-solving | Acquire knowledge and expertise in medicine and related disciplines, and use evidence-based medicine and professional experience to solve problems faced by patients |
| IT: information technology | Recognize the impact of continuing technological developments on society, and make use of information science and technology, such as artificial intelligence, when engaging in medical research and clinical practice |
| CS: clinical skills | Practice medical care with an emphasis on quality and patient safety by giving full consideration to patients’ pain and anxiety, and by developing reliable and dependable clinical skills |
| CM: communication | Practice safe and high-quality medical care by building good relationships with patients and other people involved in their care, taking patients’ own circumstances into account, and supporting them in their decision-making |
| IP: interprofessional collaboration | Understand the roles of all people involved with patients and their families, including medical care, health care, welfare, and nursing care professionals, and build collaborative working relationships with them, collectively sharing and cooperating on issues that affect patients, their families, and local communities |
| SO: medicine in society | Recognize that medicine plays a key societal role in promoting health, and strive to provide equitable medical care, maintaining an economic, regional, and international perspective to improve public health |
The curriculum is hierarchically structured, with broad competencies broken down into specific, measurable learning objectives. This structure ensures clear alignment between educational goals and evaluation methods, particularly for national assessments such as the common achievement tests (CBT and OSCE). These assessments evaluate students’ readiness for clinical practice while establishing uniform competency standards across all medical schools in Japan. Only after passing these evaluations can students advance to the participatory clinical clerkship phase, where they gain supervised, hands-on experience in real-world medical settings.
In addition to its educational focus, the curriculum reflects broader healthcare trends and policy reforms. For example, it places emphasis on geriatric and palliative care in response to Japan’s aging population. It also integrates interdisciplinary collaboration training to prepare students for team-based care models, which are increasingly essential in modern healthcare systems. The inclusion of public health and societal medicine equips graduates with the skills to address community health issues and promote equitable healthcare delivery. Furthermore, the curriculum incorporates training in advanced technologies, such as data analytics and artificial intelligence (AI), to ensure graduates can leverage these tools effectively in both clinical practice and research.
In Japan’s six-year undergraduate medical program, students are also trained in scientific research to cultivate critical thinking and analytical skills essential for medical practice and innovation. The “Model Core Curriculum” explicitly includes “Research” as one of the required competencies, emphasizing the ability to engage in evidence-based medical research. A key component of this training is the “Research laboratory assignment”, where students are assigned individually or in small groups to a specific laboratory research task. The duration of this research experience varies by university, typically ranging from one to six months. During this period, students gain hands-on experience in research methodologies, experiments, and data analysis under the guidance of faculty mentors. This training not only enhances their ability to assess medical evidence but also fosters an interest in scientific exploration, encouraging future contributions to academic medicine and clinical research.
The curriculum is designed to align with international standards to ensure global competitiveness and maintain quality in medical education. Streamlined and digitized for modern accessibility, the 2022 revision ensures usability for educators and students alike. By focusing on professionalism, adaptability, and technological integration, the curriculum enables Japan’s medical education system to remain at the forefront of global healthcare challenges, producing physicians who are both competent and compassionate.
In addition to the “Model Core Curriculum”, which serves as an official guideline for medical education, the MEXT regularly conducts comprehensive reviews and policy discussions on broader issues related to medical education in Japan. These discussions are documented in official reports and advisory council meetings, addressing key challenges such as the uneven distribution of medical doctors, declining research capabilities, and work style reforms for doctors. One such initiative is the MEXT Expert Panel on the Future of Medical Education, which periodically evaluates these systemic issues and proposes strategic directions for improvement. Incorporating insights from these official discussions provides a more comprehensive perspective on how Japan is actively addressing both current and future challenges in medical education. Relevant documents and updates can be accessed through MEXT’s official website [5].
Medical schools in Japan
Currently, Japan has 82 medical schools nationwide. Among them, 81 institutions are overseen by the MEXT, comprising 42 national universities with medical faculties, 8 public medical universities or schools operated by prefectural or municipal governments, 2 public-private medical universities, and 29 private medical universities or schools. The remaining institution, the National Defense Medical College, falls under the management of the Japanese Ministry of Defense.
The diversity of medical schools in Japan has led to variations in medical education, particularly in terms of tuition fees and financial structures. National and public medical schools generally have significantly lower tuition costs compared to private institutions. For the six-year undergraduate medical program, tuition at national universities is standardized nationwide, regardless of location, totaling approximately 3.5 million Japanese Yen for the entire program. Public medical schools, which slightly rely on the financial situation of prefectural or municipal governments, typically have tuition fees comparable to those of national universities. In contrast, private medical schools have a much wider range of tuition fees, varying from 18 million to nearly 50 million Japanese Yen for the six-year program. These differences depend on factors such as the financial status of the institution and the level of financial support received from the national or local government. Consequently, tuition disparities between public and private institutions contribute to differences in accessibility and financial burden for students pursuing medical education in Japan.
Besides tuition fees, variations also exist among institutions in terms of admission policies, educational focus, and specialized training programs. One key difference lies in regional admission quotas, introduced as part of government efforts to address the uneven distribution of physicians across Japan. Some medical schools allocate specific spots for students from some regions, requiring them to commit to practicing in these areas after graduation, called Chiikiwaku in Japanese [6]. This system improved the situation of the shortage of doctors in rural areas. However, it also faces challenges as some students opt out due to its long obligation period (nine years) of their work in the local area after graduation [7]. Additionally, specialized universities cater to particular healthcare needs. Among them, the two public-private universities – established and financially supported by the government but operated privately – each have distinct missions. The University of Occupational and Environmental Health (UOEH) focuses on training occupational physicians to address workplace-related medical concerns, while Jichi Medical University was founded to train physicians dedicated to local healthcare and community medicine, playing a crucial role in ensuring medical services reach remote areas. These distinctions highlight the diverse approaches taken by Japanese medical schools in balancing national standards with unique institutional objectives, shaping the country’s medical education landscape.
Evaluation and licensing exams
Evaluation plays a pivotal role in Japan’s medical education system, ensuring students meet rigorous standards at every stage of their training. As mentioned above, during their undergraduate years, students must pass two critical assessments: Pre-CC OSCE and CBT. These exams evaluate both theoretical knowledge and practical competencies, ensuring students are adequately prepared for the clinical phase of their education. The final and most significant examination is the NMLE, which all medical graduates must pass to practice medicine in Japan. With a pass rate of approximately 92 %, this exam underscores the high standards of education and preparation provided by Japanese medical schools. Together, these evaluations ensure a consistently high level of competence among graduating doctors, providing them with the foundation they need for successful careers.
International accreditation and quality assurance
Japan’s medical education system is aligned with international standards through a robust accreditation framework. The Japan Accreditation Council for Medical Education (JACME) ensures that medical schools meet stringent criteria, including the requirements set by the World Federation for Medical Education (WFME) [8]. This international recognition not only guarantees the quality of Japanese medical education but also facilitates the global mobility of graduates. By adhering to these standards, Japan reinforces its commitment to maintaining excellence in medical education. This alignment also ensures that graduates from Japanese medical schools are well-prepared to work and collaborate in diverse healthcare settings worldwide, solidifying the reputation of Japanese medical education on a global stage.
Challenges, reforms, and future directions
Work style reforms
One of the most pressing challenges in Japan’s healthcare system and medical education is the excessive workload faced by doctors. Long working hours, high patient loads, and administrative tasks contribute to chronic stress and fatigue. These conditions have led to serious issues such as burnout, overwork deaths (“karoshi” in Japanese), and even suicides among healthcare professionals. The impact extends beyond individuals, affecting healthcare quality, patient safety, and the sustainability of the workforce. Recognizing these problems, the MHLW has implemented a series of reforms aimed at promoting work-life balance and reducing stress among medical professionals [9].
A key component of these reforms is the regulation of working hours for physicians. The MHLW has introduced caps on overtime hours to ensure that doctors do not exceed limits that could jeopardize their physical and mental health. Furthermore, hospitals are encouraged to adopt task-shifting strategies, delegating administrative and routine clinical duties to non-physician staff, such as nurse practitioners and medical assistants, to reduce the burden on doctors. Medical schools and training hospitals are also addressing these issues by integrating well-being initiatives into their programs, such as stress management workshops, and promoting mental health awareness.
In parallel, reforms are also being implemented to support women in medicine. With an increasing number of women entering the medical field, ensuring gender equity and creating supportive environments for female doctors – especially those balancing careers and family responsibilities – has become a priority. Initiatives like flexible work arrangements, on-site childcare, and mentorship programs are being adopted to address these challenges.
Transition from individual to team-based care
Traditionally, Japan’s healthcare system has relied heavily on the primary care physician model, where a single doctor oversees all aspects of a patient’s care. While this approach has historically been effective, the increasing complexity of modern medicine has highlighted its limitations. Chronic diseases, multi-morbidity, and aging populations require a multi-disciplinary approach to address patients’ needs comprehensively. This has driven a shift towards team-based care, where multiple healthcare professionals – including doctors, nurses, pharmacists, and allied health workers – collaborate to deliver coordinated and holistic patient care.
Medical education in Japan is adapting to this transition by incorporating interdisciplinary training into its curricula. Future doctors are being trained to work effectively in teams, emphasizing communication, leadership, and collaboration skills. Students now participate in interprofessional education programs, where they learn alongside nursing, pharmacy, and a variety of health professional students to understand each other’s roles and develop mutual respect. This shift also emphasizes shared decision-making, where healthcare teams work together with patients and their families to develop treatment plans that align with patients’ preferences and goals. By fostering a culture of teamwork and mutual accountability, the healthcare system can better meet the demands of modern patient care while reducing the strain on individual practitioners.
Advancements in medical technology and education
The rapid integration of advanced technologies into healthcare is revolutionizing medical education and practice in Japan. AI, telemedicine, robotics, and big data analytics are transforming how healthcare is delivered, creating new opportunities and challenges for medical professionals. To keep pace, medical schools are revising their curricula to include training on these technologies, ensuring that future doctors can utilize them effectively to improve patient outcomes.
AI is being introduced to assist in diagnostics, treatment planning, and research, while telemedicine enables remote consultations, expanding access to care in underserved areas. Robotics is increasingly used in surgery and rehabilitation, requiring physicians to understand and operate advanced systems. Additionally, big data and machine learning tools allow doctors to analyze patient data for personalized medicine approaches, improving the accuracy and efficiency of care. Medical education is embracing these advancements through innovative teaching methods. Simulation-based learning, which incorporates virtual reality and AI-driven scenarios, provides students with a safe and controlled environment to practice procedures, refine decision-making, and experience rare or complex cases. For example, virtual patient simulators allow students to diagnose and treat virtual patients in real-time, enhancing their clinical skills and confidence.
Moreover, digital tools such as e-learning platforms and online medical resources have made education more accessible and flexible. By integrating these technologies into medical education, Japanese medical schools are preparing graduates to navigate the rapidly evolving healthcare landscape and leverage technology to enhance patient care.
Future directions
The “Model Core Curriculum”, as a cornerstone of Japan’s medical education, is continuously updated to reflect emerging challenges and advancements in healthcare. Recent revisions emphasize two critical goals: patient-centered care and technological adaptability.
Patient-centered care is at the forefront of these changes, aiming to train doctors who can approach patients holistically. This involves considering not only the medical but also the psychological, social, and environmental determinants of health. Medical education is increasingly focusing on teaching students to understand patients’ perspectives, foster empathy, and build strong doctor-patient relationships. These skills are essential for managing chronic conditions and providing end-of-life care, both of which are growing areas of need in Japan’s aging population. Technological adaptability is another key focus area. With the rapid pace of innovation in healthcare, doctors must be equipped to understand, evaluate, and integrate new technologies into their practice. This includes not only learning how to use specific tools but also developing critical thinking skills to assess their effectiveness and ethical implications. The incorporation of courses on digital health, AI, and data science into medical curricula ensures that future physicians remain at the cutting edge of medical advancements. Additionally, outcome-based education is becoming a central theme, where the emphasis is on what students can do rather than what they know. This approach aligns with international trends and ensures that graduates are competent, adaptable, and ready to meet the complex demands of modern healthcare. The focus on producing healthcare professionals who are not only technically skilled but also compassionate and patient-focused is shaping the future of Japan’s medical education.
As Japan continues to face challenges such as workforce shortages, aging populations, and evolving patient expectations, its medical education system is rising to the occasion by implementing innovative reforms. By addressing these challenges head-on and embracing new technologies and collaborative care models, Japan is ensuring that its healthcare system remains resilient and capable of delivering high-quality care in the decades to come.
Conclusions
Medical education in Japan is a dynamic and evolving system, deeply intertwined with the nation’s healthcare framework and societal needs. Its structured approach, from undergraduate education to specialist training, ensures that doctors are well-prepared to meet the challenges of modern medicine. While the system boasts many strengths, including rigorous evaluations and international accreditation, it also faces significant challenges, such as work-life balance and the integration of new technologies.
By addressing these challenges and embracing innovative reforms, Japan’s medical education system is poised to remain a global leader, producing doctors who excel in clinical care, research, and patient advocacy. Future efforts should focus on continuous curriculum improvement, promoting work-life balance, and leveraging technological advancements to enhance training and patient care.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Kobayashi, Y. Five decades of universal health insurance coverage in Japan: lessons and future challenges. Japan Med Assoc J 2009;52:263–8.Search in Google Scholar
2. Kondo, N, Shigeoka, H. Effects of universal health insurance on health care utilization, and supply-side responses: evidence from Japan. J Publ Econ 2013;99:1–23. https://doi.org/10.1016/j.jpubeco.2012.12.004.Search in Google Scholar
3. Gomi, H, Matsuyama, Y, Oikawa, S, Kikukawa, M, Shimizu, I, Nomura, O, et al.. The 2022 revision of the model core curriculum for medical education in Japan for healthcare professionals and global trends in health professions education. Igaku Kyoiku 2023;54:194–8.Search in Google Scholar
4. Medical Education Model Core Curriculum Expert Research Committee. Model core curriculum for medical education (2022 revision) [Online]. https://www.mext.go.jp/content/20230323-mxt_igaku-000028108_00003.pdf [Accessed 23 Dec 2024].Search in Google Scholar
5. MEXT Expert Panel on the Future of Medical Education. The 2nd interim report (in Japanese) [Online]. https://www.mext.go.jp/content/20240610-mxt_igaku-000036452.pdf [Accessed 17 Feb 2025].Search in Google Scholar
6. Department of Medical Education, MEXT. Implementation status of regional admission quotas in university medical faculties (in Japanese) [Online]. https://www.mext.go.jp/content/20240125-mxt_igaku-100001063_1.pdf [Accessed 20 Feb 2025].Search in Google Scholar
7. Yamamoto, K, Ozaki, A, Takita, M, Morita, T, Saito, H, Senoo, Y, et al.. Negative aspects of the regional quota system in Japan. Japan Med Assoc J 2019;2:85–6. https://doi.org/10.31662/jmaj.2018-0055.Search in Google Scholar PubMed PubMed Central
8. Asada, Y. Investigation of the current situation of medical education in Japan based on the results of accreditation based on global standards. Int J Inst Res Manag 2020;4:1–16. https://doi.org/10.52731/ijirm.v4.i1.482.Search in Google Scholar
9. Nakashima, Y, Yoshikawa, T, Kido, M, Aizawa, Y, Matsumoto, K. Work time and work style reform among physicians in Japan. Int J Pers Cent Med 2019;9:35–46. https://doi.org/10.5750/ijpcm.v9i3.996.Search in Google Scholar
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


