Readmission Risk Factors and Heart Failure With Preserved Ejection Fraction
-
Dustin Harmon
Abstract
Context
Cases of heart failure with preserved ejection fraction (HFpEF) exacerbations continue to affect patients' quality of life and cause significant financial burden on our healthcare system.
Objective
To identify risk factors for readmission in patients discharged with a diagnosis of HFpEF.
Methods
Electronic health records of patients over 18 years of age with a primary diagnosis of HFpEF treated between August 1, 2017 and March 1, 2018 in a community hospital were retrospectively reviewed. The study population included patients with HFpEF greater than 40% who were screened but did not qualify for the ongoing CONNECT- HF trial being conducted by Duke Clinical Research. To be included, subjects had to fall into 1 of 2 classifications (NYHA Class II-IV or ACC/AHA Stage B-D) and have a life expectancy greater than 6 months. Patients were excluded if they had terminal illness other than HF, a prior heart transplant or were on a transplant list, a current or planned placement of a left ventricular assist device, chronic kidney disease requiring hemodialysis, inability to use mobile applications, or inability to participate in longitudinal follow up. Readmission rate was analyzed at 30 and 90 days along with patients’ demographics and associated comorbidities, including peripheral vascular disease, anemia, pulmonary hypertension, arrythmia, and valvular heart disease. Patients were risk stratified using the LACE index readmission score and the Charlson comorbidity index.
Results
Of the 492 cases of HFpEF identified during the 7-month study period, 212 patients were included. The majority of patients were women (126; 59.4%), had a median body mass index above 30 kg/m2 (123; 58%), and had pulmonary hypertension (94; 44.3%), anemia (146; 68.8%), and arrhythmia (101, 47.6%). Forty-five (21.2%) patients were readmitted for HFpEF within 90 days of initial discharge; 32 of those (71.1%) were readmitted within 30 days of initial discharge. Patients with higher LACE and Charlson comorbidity index scores were more likely to be readmitted within 90 days. Peripheral vascular disease (P=.002), tricuspid regurgitation (P=.001), pulmonary hypertension (P=.049), and anemia (P=.029) were risk factors associated with readmissions. Use of ACEi/ARBs (P=.017) was associated with fewer readmissions.
Conclusion
Anemia, peripheral vascular disease, pulmonary hypertension, and valvular heart disease are not only postulated mechanisms of HFpEF, but also important risk factors for readmission. These study findings affirm the need for continued research of the pathophysiology and associated comorbidities of the HFpEF population to improve quality of life and lower healthcare costs.
Heart failure (HF) hospitalizations account for a significant proportion of the rising financial pressure on the healthcare system. HF is a major cause of premature morbidity and mortality, with approximately 50% of people with symptomatic HF dying within 5 years of diagnosis.1 One assumption of heart failure etiology may be related to an inability to maintain circulatory support without hemodynamic compromise leading to left heart congestion, diastolic dysfunction, left atrial hypertension, pulmonary vascular disease, right ventricular [RV] dysfunction, and plasma volume expansion.2 A second possible etiology relates to molecular mechanisms such as systemic microvascular inflammation, cardiometabolic functional abnormalities, and cellular (titin)/extracellular (fibrosis) structural abnormalities.2
Heart failure with preserved ejection fraction (HFpEF) is now more common than heart failure with reduced ejection fraction (HFrEF) and affects more than 50% of the heart failure population.3 Despite being more common, clinical trials on HFpEF have not resulted in evidence-based treatment to improve overall survival.3 Clinical trials using cardiac-targeted medications such as beta blockers and angiotensin-converting enzyme inhibitors (ACEI) that reduce mortality in HFrEF have not shown improvement in mortality or morbidity for patients with HFpEF. 4
Prior to undertaking this study, we subjectively observed that significant portion of heart failure readmissions at our community hospital were patients with an ejection fraction (EF) greater than 40%. As the prevalence of HF and the cost of caring for these patients rise, there is an increased urgency to achieve and maintain a euvolemic state to decrease patients’ length of stay and hospital readmissions. Stabilization of the patient is often achieved in the hospital, but a functional, euvolemic state must be maintained through close follow up in the outpatient setting and continued management of chronic comorbidities. Heart failure patients have multiple comorbidities and are prescribed an average of 8 medications when discharged from the hospital following an exacerbation. 5 Managing the chronic comorbidities associated with HFpEF is of paramount importance because it may lead to better outcomes and less hospitalizations. We retrospectively reviewed the health records of patients discharged from our hospital with a diagnosis of HFpEF to identify the most common associated risks for readmission in our population.
Methods
This study was approved by the Institutional Review Board at the Ascension Macomb Hospital in Warren, Michigan.
Electronic health records were retrospectively reviewed in October 2018 by several authors (J.R., F.R., H.G., and I.P.) for patients admitted between August 1, 2017 and March 1, 2018 to Ascension Macomb-Oakland Hospital with a diagnosis of HFrEF greater than 40% who were screened but did not qualify for the ongoing, nationwide CONNECT-HF trial, for which our hospital was enrolling patients at the time of this report and which was being conducted by Duke Clinical Research. CONNECT-HF is a quality improvement initiative based on clinical outcomes, medication use, quality-of life assessments for HF patients with reduced left ventricular EF.6
Patients 18 years or older who fell into 1 of 2 classifications (New York Heart Association Class [NYHA] II-IV or American College of Cardiology/American Heart Association [ACC/AHA] Stage B-D) and who had a life expectancy greater than 6 months were included. NYHA classification separates patients with heart failure based on symptom and ACC/AHA separates patients with heart failure based on structural abnormality.1 Patients were excluded if they had terminal illness other than HF, a prior heart transplant or were on a transplant list, a current or planned placement of a left ventricular assist device, chronic kidney disease requiring hemodialysis, inability to use mobile applications, or inability to participate in longitudinal follow up.
Data Collection and Outcomes Measures
Patient demographic data (age, gender, body mass index [BMI], and race) and clinical data (brain natriuretic peptide [BNP], troponin on admission, peak troponin, and hemoglobin) were analyzed in this study. Additionally, transthoracic echocardiography (TTE) reports were reviewed for any existing valvular heart disease, EF value, and estimated pulmonary pressure. Supplementary data including cardiovascular (CV) comorbidities (myocardial infarction, history of arrhythmia, history of stroke, peripheral arterial disease, and pulmonary hypertension) and cardiac medications upon discharge were also evaluated. Furthermore, a LACE index score and Charlson comorbidity index score were calculated for all patients to evaluate any statistical significance between index scores and hospital readmissions.7,8 The LACE index readmission score predicts risk of death or nonelective readmission at 30 days, and the Charlson comorbidity index predicts 10-year survival of patients with multiple comorbidities.
We compared patients with at least 1 readmission for HF at 90 days to those with no HF readmission by 90 days after initial HF admission. Categorical variables were provided as counts and percentage frequencies. All continuous variables were provided as either mean values with standard deviation (SD) or median (25th and 75th percentile) values, depending on the normality of the data, followed by the minimum to maximum. Categorical variables were examined with Chi- square tests when expected frequency was greater than 5 in 80% of cells; otherwise, Fisher's Exact tests were used. Continuous data was examined with Wilcoxon rank sum tests. SAS for Windows 9.4 (SAS Institute) was used for all analysis.
Results
Of 492 patients treated for HFrEF during the retrospective study period, 250 patients had left ventricular ejection fraction >40, and 212 patients met our inclusion and exclusion criteria (Figure 1). Demographic distributions are shown in Table 1. Our patients were 59.4% (126) women, 40.5% (86) men, had a mean age of 72 years (standard deviation [SD], +/- 13.3), and had an average BMI of 33.4 kg/m2. Of the 212 patients included, 123 had a BMI greater than 30 kg/m2. Detailed chart review found a total of 45 (21.23%) patients readmitted for HFpEF within 90 days of initial discharge. Of the 45 readmitted, 32 (71.11%) patients were readmitted within 30 days of initial discharge.
Demographic Data on HFpEF Patients With and Without Heart Failure Readmissions
| Demographics | No CHF readmission (n=167) | CHF readmission (n=45) | P value |
|---|---|---|---|
| Sex Men Women | 63 (37.7%)104 (62.3%) | 23 (51.1%)22 (48.9%) | .10 |
| Age Mean ± SD Minimum-maximum | 73 ± 12 (74) 33-95 | 74 ± 16 (78) 40-101 | .39 |
| BMI Mean ± SD Minimum-maximum | 34 ± 10 (32) 17-68 | 33 ± 11 (32) 17-64 | .65 |
| Race White Black or African American Asian Native Hawaii/Pacific | 124 (74.2%) 39 (23.5%) 2 (1.2%) 2 (1.2%) | 33 (73.3%) 12 (26.7%) 0 0 | .89 |
Abbreviations: CHF, congestive heart failure; HFpEF, heart rate with reduced ejection fraction.
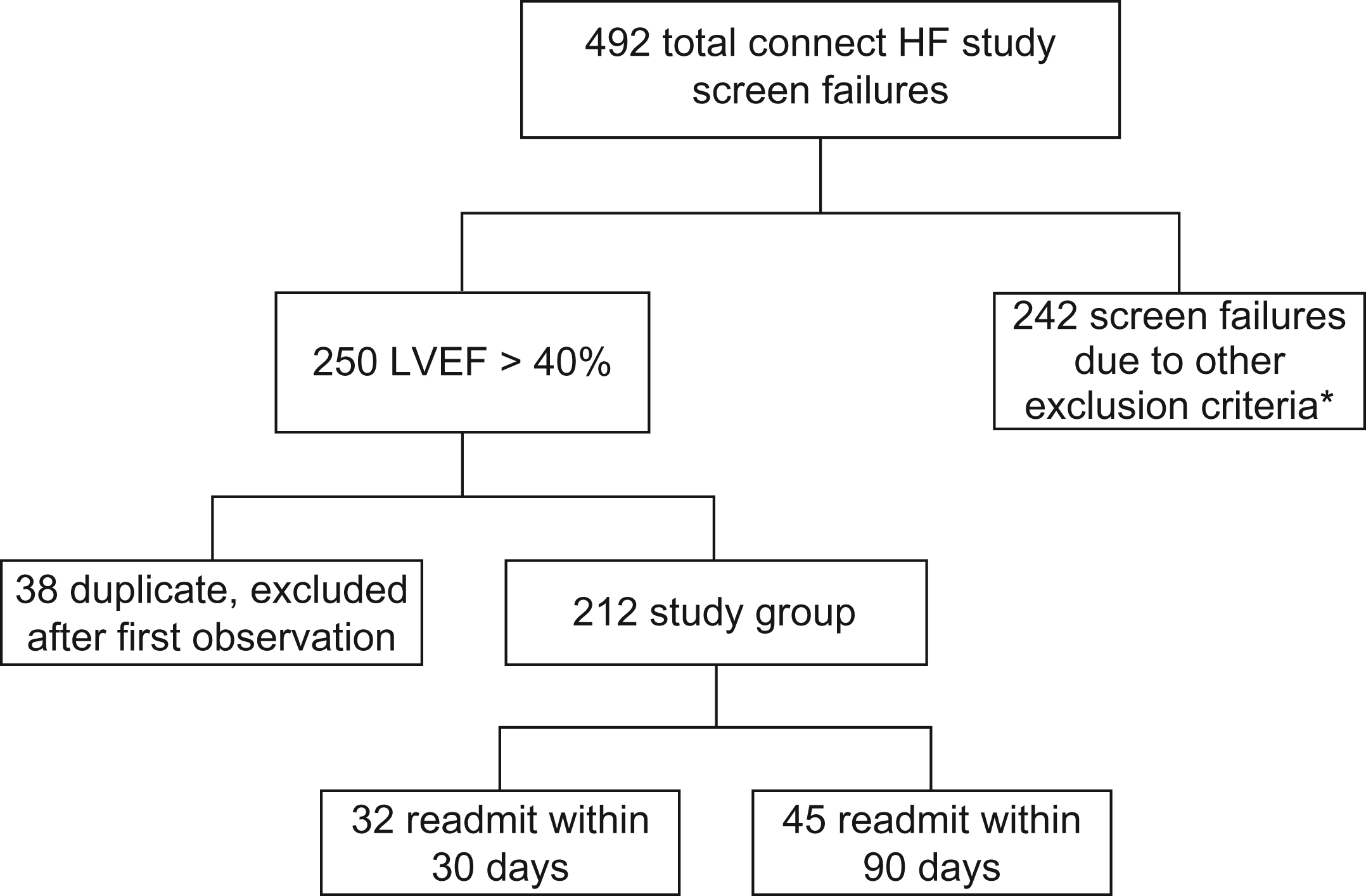
Inclusion and exclusion criteria for heart failure patients during the retrospective study period.*Terminal illness other than HF, prior heart transplant or were on a transplant list, current or planned placement of a left ventricular assist device, chronic kidney disease requiring hemodialysis, inability to use mobile applications, and unable to participate in longitudinal follow up.
Clinical findings of pertinent underlying CV diseases included: 22 (10.33%) patients with a history of previous myocardial infarction (MI); 101 (47.41%) with a history of arrhythmia (atrial fibrillation/atrial flutter); 32 (15.02%) with a history of stroke (CVA); 27 (12.68%) with known peripheral vascular disease (PVD); 140 (66.99%) with documented pulmonary hypertension; 94 (44.13%) with COPD; and 172 (80.75%) with a documented history of HF.
Clinical laboratory data analyzed in our study included hemoglobin, BNP, troponin on admission, and peak troponin levels (Table 2). The median BNP of HFpEF patients was 2727 pg/mL, while the median troponin on admission was 0.03ng/ml and the median peak troponin level was also 0.03 ng/ml. Interestingly, both baseline and peak mean values were found to be statistically significantly higher in the patients who were not readmitted within 90 days (baseline, P=.035; peak, P=.014). Significant anemia was defined as a hemoglobin less than 10 mg/dL, which was found in 146 (68.86%) of the reviewed charts and noted to be a statistically significant factor for readmissions (P=.029)
BNP and Troponin at Admission in HFpEF With and Without Heart Failure Readmissions
| Lab data | No CHF readmission | CHF readmission | P-value |
|---|---|---|---|
| BNP Median Median (25th,75th) Minimum-maximum | n=142 2628 1225,6866 49-70001 | n=37 4729 1673,9307 49-70001 | .22 |
| Troponin at admission Mean Medium (25th, 75th) Minimum-maximum | n=154 0.81 ± 0.31 0.03 (0.03,0.04) 0.03-3.85 | n=40 0.06 ± 0.08 0.03 (0.03,0.08) 0.03-0.46 | .04 |
Abbreviations: BNP, brain natriuretic peptide; CHF, congestive heart failure.
Echocardiographic findings were included to assess the significance of valvular stenosis or regurgitation and pulmonary hypertension on HFpEF patients. Echocardiographic information was reviewed on all 212 patients and all abnormalities were recorded based on the final signed report by a cardiologist. In our studied population, 38 patients were found to have moderate-to-severe pulmonary hypertension (defined as systolic pulmonary pressure greater than 50 mmHg) with concomitant anemia. Of those 38 patients, 16 (42%) were readmitted for HF within 90 days (P=.24).
Discharge medication review found that ACEI or angiotensin receptor blockers (ARB) were more frequently prescribed on discharge in the group of patients who were not readmitted for heart failure within 90 days of initial discharge (80 [48.8%] vs. 13 [28.9%]; P=.017).
The median LACE score was higher in patients who were readmitted within 90 days vs those were not readmitted (16 vs 13; P<.001). The median Charlson comorbidity index was also higher for those the readmission group compared to those who were not readmitted (6 vs 4; P<.002), reaffirming utility of LACE index score and Charlson comorbidity index to stratify patients at risk for readmission. Results are reported in Table 3.
Comorbidity Score in HFpEF With and Without Heart Failure Readmission
| Comorbidity Score | No CHF readmission (n=167) | CHF readmission (n=45) | P-value |
|---|---|---|---|
| LACE score Median (25th,75th) Minimum-maximum | 12 (11,16) 4-38 | 16 (13,18) 9-27 | <.0001 |
| Charlson index Median | 6 | 4 | <.002 |
Abbreviations: CHF, congestive heart failure; HFpEF, heart rate with reduced ejection fraction.
Several factors proved to be statistically significant after performing a side-by-side comparison of the above variables in patients who were readmitted within 90 days for heart failure and those who were not. PVD was more common in those readmitted within 90 days (12 [26.7%] vs.15 [9%]; P<.002), as was any valvular heart disease on TTE (31 [68.9%] vs. 86 [51.1%]; P=.037), anemia (37 [82.2%] vs. 109 [65.3%]; P=.029), moderate-to-severe pulmonary hypertension (19 [44.2%] vs. 38 (23%); P=.049) than the group who was not readmitted. Review of patients’ most recent echocardiogram showed that severe tricuspid regurgitation was also more common in the readmission group (11 [24.4%] vs. 10 [6%]; P=.001).
Discussion
Our results provide several important findings that can further improve collective understanding of HFpEF pathophysiology and the impact of its various comorbidities. The majority of our study population had obesity, pulmonary hypertension, anemia, and arrhythmias. Importantly, obesity is among underlying factors of HFpEF, as it is a significant contributor to systemic inflammation leading to myocardial remodeling.9 Based on a 30-day readmission rate of 15% and a 90-day readmission rate of 21.3%, our main goal was to identify the predominant readmission risk factors in HFpEF patients in our community.
Our findings correlate well with existing knowledge about the impact of higher LACE and Charlson comorbidity indices on readmission rate.7,8 These scores could be used as a guide to help providers identify patients at risk for readmission, effectively coordinate care, and provide adequate community resources to reduce readmission rates and hopefully improve patient longevity.
In our study, patients with PVD were more likely (P<.002) to be readmitted within 90 days of discharge, suggesting that comorbidities in patients with HFpEF lead to microvascular inflammation, which adversely affects the adjacent cardiomyocytes through decreased nitric oxide bioavailability, reduced cyclic guanosine monophosphate availability, and altered phosphorylation of titin. Microvascular ischemia, concentric left ventricular remodeling, and fibrosis from endothelial to mesenchymal transition contribute further to diastolic dysfunction in these patients.2,9
After review of the laboratory data on each initial heart failure admission, brain natriuretic peptide (BNP) was not found to be significant as a readmission factor. This insignificance could be a result of the average BMI of patients in our study (33.4 kg/m2) being classified as obese. There is an inverse relationship between obesity and BNP; obesity suppresses plasma BNP levels in acute heart failure.1,10 Obese HFpEF patients were shown to have a lower BNP level, but the range of values obtained was very large (49 to 70001), which could make it difficult to show statistical significance.12 Troponin values were also assessed for baseline and peak levels on initial admission. Interestingly, both baseline and peak mean values were found to be statistically significantly higher in the patients who were not readmitted within 90 days. It is possible that patients who were not readmitted received a more comprehensive workup or medications that were more aggressively titrated, resulting in statistically-significant higher average levels of troponin found at both baseline and peak in our study.
Readmission rates in our study were also higher in patients found to have significant anemia (hemoglobin <10 mg/dL) on initial admission (P=.029). Symptomatic HFrEF patients with iron deficiency anemia who were treated accordingly have been associated with reduced hospitalizations, improved exercise capacity, and quality of life.13 It is unclear whether HFpEF patients will demonstrate similar association to iron deficiency anemia treatment in any of the prospective trials currently in progress.14 Although the goal of this study was not to evaluate the etiology of anemia, impaired myocardial energetics in HFpEF patients suggest that targeting cardiometabolic functional abnormalities may be an important approach in these patients in the future.2
Likewise, patients with TTE findings signifying severe tricuspid regurgitation with estimated moderate-to-severe pulmonary hypertension, defined as a systolic pulmonary pressure greater than 50 mmHg, were more likely to have a HF readmission within 90 days. Although there was no statistical significance in this finding, partly due to small sample size, this trend certainly has meaningful clinical implications.
The presence and severity of pulmonary hypertension is strongly associated with the development of RV dysfunction. Beyond increased pulmonary pressure, RV-arterial uncoupling plays an important role further contributing to worse outcomes in HFpEF. Therapy directly aimed at pulmonary hypertension to reduce RV afterload, thereby improving RV function in HFpEF, has not been shown to decrease morbidity and mortality in HFpEF patients.2,15
Lastly, we compared all categories of cardiac medications given to patients in our study upon discharge after their initial HF admission. Patients discharged on an ACEI/ARB were noted to have a lower risk of readmission (80 [48.8%] vs. 13 [28.9%]; P<.017). Although this is statistically significant and supports previous evidence that ACEI/ARB may be beneficial in HFpEF patients from trials such as the CHARM-Preserved Trial,16 the I-PRESERVE Trial,17 and a substudy of the BACH trial,18 any clinical significance remains uncertain due to the multiple confounding factors of the patients in our retrospective study.16-18 Based on these previous larger studies, we can suggest, but do not confidently conclude, that readmission rates at our community hospital could be reduced if patients admitted for CHF with an EF >40% were discharged on an ACEI/ARB when clinically indicated. Additionally, data from the CHAMPION trial19 suggests that addressing volume overload via diuresis may be a fundamental component of the optimal management of HFpEF.
Limitations
There were several limitations to our study that merit discussion. First, the sample size was very small compared to larger, previous trials.16,17,19 Second, our study was conducted in a community setting and was retrospective; thus, our sample had limited diversity and our collected data points were dictated by other provider documentation instead of a unified standard with specific providers executing a protocol. Third, the patients were not authorized to be contacted, which prevented any postdischarge follow-up to assess compliance with medications and outpatient appointments. Fourth, patients were all labeled as having HFpEF (EF>40%), instead of being further divided into HF with mildly reduced EF of 45-50% and HFpEF, which could have had a significant impact on statistically significant results. Further, it merits mentioning that a majority of our patients were obese and probably underdiagnosed with obstructive sleep apnea (OSA), which needs to be addressed, but incidence of OSA was difficult to assess in retrospective chart review. Additionally, both anemia and arrhythmia classifications were not further investigated, making it difficult to identify significant contributions. Lastly, medication compliance and mortality could not be accounted for and thus were not made primary endpoints.
Conclusion
HF exacerbations continue to be a large obstacle affecting not only patients' quality of life but causing significant financial burden on our healthcare systems. Although reducing left heart congestion along with left atrial hypertension carries prognostic benefit in HFpEF, it is increasingly recognized that various conditions, especially obesity, anemia, vascular disease, and pulmonary hypertension, are underlying contributors to cardiac remodeling. Early recognition and amelioration of these risk factors is of paramount importance. Our study findings affirm the need to continue to research into the pathophysiology and associated comorbidities for patients with HFpEF to improve their quality of life and lower healthcare system costs.
Author Contributions
All authors provided substantial contribution to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
1. YancyCW, JessupM, BozkurtB, et al.. 2013ACCF/AHA guideline for the management of heart failure: a report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation. 2013;128(16):e240-e327. doi:10.1161/CIR.0b013e31829e8776Search in Google Scholar
2. LamCSP, VoorsAA, de BoerRA, SolomonSD, van Veldhuisen DJ. Heart failure with preserved ejection fraction: from mechanisms to therapies [published correction appears in Eur Heart J. 2019 Feb 7;40(6):528]. Eur Heart J. 2018;39(30):2780-2792. doi:10.1093/eurheartj/ehy301Search in Google Scholar
3. BhuiyanT, MaurerMS. Heart failure with preserved ejection fraction: persistent diagnosis, therapeutic enigma. Curr Cardiovasc Risk Rep. 2011;5(5):440-449. doi:10.1007/s12170-011-0184-2Search in Google Scholar
4. BozkurtB. What is new in heart failure management in 2017? Update on ACC/AHA heart failure guidelines. Curr Cardiol Rep. 2018;20(6):39. doi:10.1007/s11886-018-0978-7Search in Google Scholar
5. CustodisF, RohlehrF, WachterA, BöhmM, SchulzM, LaufsU. Medication knowledge of patients hospitalized for heart failure at admission and after discharge. Patient Prefer Adherence. 2016;10:2333-39. doi:10.2147/PPA.S113912.Search in Google Scholar
6. Care Optimization Through Patient and Hospital Engagement Clinical Trial For Heart Failure. US National Libraries of Medicine. Clinicaltrials.gov website. January 30, 2017. https://clinicaltrials.gov/ct2/show/NCT03035474Search in Google Scholar
7. WangH, RobinsonRD, JohnsonC, et al.. Using the lace index to predict hospital readmissions in congestive heart failure patients. BMC Cardiovasc Disord. 2014;14:97. doi:10.1186/1471-2261-14-97.Search in Google Scholar
8. TamakiS, YamadaT, MoritaT, et al.. Prognostic value of charlson comorbidity index in patients admitted for acute decompensated heart failure with reduced or preserved left ventricular ejection fraction: a prospective study. J Am Coll Cardiol. 2018; 71(11 Supp):A829. doi:10.1016/S0735-1097(18)31370-6Search in Google Scholar
9. PaulusWJ, TschöpeC. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263-271. doi:10.1016/j.jacc.2013.02.092Search in Google Scholar PubMed
10. DameryS, CombesG. Evaluating the predictive strength of the LACE index in identifying patients at high risk of hospital readmission following an inpatient episode: a retrospective cohort study. BMJ Open. 2017;7(7):e016921. doi:10.1136/bmjopen-2017-016921Search in Google Scholar PubMed PubMed Central
11. Lemor, A, Hernandez, GA, Patel, N, et al.. Predictors and etiologies of 30-day readmissions in patients with non-ST-elevation acute coronary syndrome. Catheter Cardiovasc Interv. 2019;93:373–9. https://doi.org/10.1002/ccd.2783810.1002/ccd.27838Search in Google Scholar PubMed
12. MaiselAS, ShahKS, BarnardD, et al.. How b-type natriuretic peptide (bnp) and body weight changes vary in heart failure with preserved ejection fraction compared with reduced ejection fraction: secondary results of the habit (hf assessment with bnp in the home) trial. J Card Fail. 2016;22(4):283-293. doi:10.1016/j.cardfail.2015.09.014Search in Google Scholar
13. PonikowskiP, VoorsAA, AnkerSD, et al.. 2016esc guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the european society of cardiology (esc). Developed with the special contribution of the heart failure association (hfa) of the esc. Eur J Heart Fail. 2016;18(8):891-975. doi:10.1002/ejhf.592Search in Google Scholar
14. Von HaehlingS, EbnerN, EvertzR, PonikowskiP, AnkerSD. Iron deficiency in heart failure: an overview. JACC Heart Fail. 2019;7(1):36-46. doi:10.1016/j.jchf.2018.07.015Search in Google Scholar
15. LamCS, RogerVL, RodehefferRJ, BorlaugBA, EndersFT, RedfieldMM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53(13):1119-1126. doi:10.1016/j.jacc.2008.11.051Search in Google Scholar
16. YusufS, PfefferMA, SwedbergK, et al.. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the charm-preserved trial. Lancet. 2003;362(9386):777-781. doi:10.1016/S0140-6736(03)14285-7Search in Google Scholar
17. AnandIS, RectorTS, ClelandJG, et al.. Prognostic value of baseline plasma amino-terminal pro-brain natriuretic peptide and its interactions with irbesartan treatment effects in patients with heart failure and preserved ejection fraction: findings from the i-preserve trial. Circ Heart Fail. 2011;4(5):569-577. doi:10.1161/CIRCHEARTFAILURE.111.962654Search in Google Scholar
18. ShahK, ParekhN, CloptonP, et al.. Improved survival in patients with diastolic heart failure discharged on beta-blocker and ace inhibitors. J Am Coll Cariol.2013; 61 (10 Supp): E634. doi:10.1016/S0735-1097(13)60634-8Search in Google Scholar
19. AbrahamWT, StevensonLW, BourgeRC, et al.. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the champion randomised trial. Lancet. 2016;387(10017):453-461. doi:10.1016/S0140-6736(15)00723-0Search in Google Scholar
© 2020 American Osteopathic Association
Articles in the same Issue
- ABSTRACTS
- 2020 AOA Research Abstracts and Poster Competition
- ORIGINAL CONTRIBUTION
- An Evaluation of Reporting Guidelines and Clinical Trial Registry Requirements Among Addiction Medicine Journals
- BRIEF REPORT
- Readmission Risk Factors and Heart Failure With Preserved Ejection Fraction
- CASE REPORT
- Mobitz Type II Atrioventricular Heart Block After Candlenut Ingestion
- ORIGINAL CONTRIBUTION
- Toward Resilience: Medical Students' Perception of Social Support
- Undergraduate Knowledge of Osteopathic Medicine: What Premedical Students Know About Osteopathic Medicine and Its Effect on Burnout
- Communication Skills of Grandview/Southview Medical Center General Surgery Residents
- Comparison of State Medical Licensing Board Disclosures Regarding Resident Performance for United States Allopathic, Osteopathic, and Foreign Medical Graduates
- Motivating High School Students From Rural Areas to Attend College and Pursue Careers as Osteopathic Physicians
- REVIEW
- Osteopathic Manual Treatment for Pain Severity, Functional Improvement, and Return to Work in Patients With Chronic Pain
- CASE REPORT
- Osteopathic Approach to the Treatment of a Patient With Idiopathic Iliohypogastric Neuralgia
- ORIGINAL CONTRIBUTION
- Characteristics and Management of Pregnant Patients From a Neuromusculoskeletal Medicine/Osteopathic Manipulative Medicine Clinic
- CASE REPORT
- The Use of Osteopathic Manipulative Medicine in the Management of Recurrent Mastitis
- ORIGINAL CONTRIBUTION
- Remdesivir for the Treatment of Severe COVID-19: A Community Hospital's Experience
- CASE REPORT
- Kikuchi-Fujimoto Disease Heralding Systemic Lupus Erythematosus
- CLINICAL IMAGE
- Sister Mary Joseph Nodule
- Dysphagia Lusoria
- Septic Pulmonary Emboli With Feeding Vessel Sign
- LETTER TO THE EDITOR
- LETTER TO THE EDITOR
Articles in the same Issue
- ABSTRACTS
- 2020 AOA Research Abstracts and Poster Competition
- ORIGINAL CONTRIBUTION
- An Evaluation of Reporting Guidelines and Clinical Trial Registry Requirements Among Addiction Medicine Journals
- BRIEF REPORT
- Readmission Risk Factors and Heart Failure With Preserved Ejection Fraction
- CASE REPORT
- Mobitz Type II Atrioventricular Heart Block After Candlenut Ingestion
- ORIGINAL CONTRIBUTION
- Toward Resilience: Medical Students' Perception of Social Support
- Undergraduate Knowledge of Osteopathic Medicine: What Premedical Students Know About Osteopathic Medicine and Its Effect on Burnout
- Communication Skills of Grandview/Southview Medical Center General Surgery Residents
- Comparison of State Medical Licensing Board Disclosures Regarding Resident Performance for United States Allopathic, Osteopathic, and Foreign Medical Graduates
- Motivating High School Students From Rural Areas to Attend College and Pursue Careers as Osteopathic Physicians
- REVIEW
- Osteopathic Manual Treatment for Pain Severity, Functional Improvement, and Return to Work in Patients With Chronic Pain
- CASE REPORT
- Osteopathic Approach to the Treatment of a Patient With Idiopathic Iliohypogastric Neuralgia
- ORIGINAL CONTRIBUTION
- Characteristics and Management of Pregnant Patients From a Neuromusculoskeletal Medicine/Osteopathic Manipulative Medicine Clinic
- CASE REPORT
- The Use of Osteopathic Manipulative Medicine in the Management of Recurrent Mastitis
- ORIGINAL CONTRIBUTION
- Remdesivir for the Treatment of Severe COVID-19: A Community Hospital's Experience
- CASE REPORT
- Kikuchi-Fujimoto Disease Heralding Systemic Lupus Erythematosus
- CLINICAL IMAGE
- Sister Mary Joseph Nodule
- Dysphagia Lusoria
- Septic Pulmonary Emboli With Feeding Vessel Sign
- LETTER TO THE EDITOR
- LETTER TO THE EDITOR

