Abstract
Objectives
D-dimer molecules are formed as a result of fibrinolysis and elevation of D-dimer levels are suggestive for thrombosis. The elevation of D-dimer levels and its correspondence with thromboembolism in orthopedic and general surgeries are well studied, but there are only a few studies in literature that investigates this issue in head and neck surgery. We aimed to investigate D-dimer levels and its course throughout the perioperative period in patients who underwent head and neck cancer surgery.
Methods
We conducted a prospective, observational study in patients who underwent neck dissection along with primary tumor resection in our otorhinolaryngology clinic between January 2022 and June 2023. D-dimer levels were measured from blood samples preoperatively and postoperatively days 0–7 and on postoperative 14th day. D-dimer levels were compared statistically.
Results
Twenty-one patients were included in the study. D-dimer values peaked on the first day then gradually decreased and reached a level slightly below 2 times of the preoperative values on the 14th day. The change in D-dimer levels between preoperative and postoperative days 1–14 was statistically significant. The difference between D-dimer levels measured on each day of the first week and levels on 14th day was found to be significant. Also, difference of D-Dimer levels between postoperative day 0 and day 7 was statistically significant.
Conclusions
The trend of D-dimer levels following surgery in head and neck cancer patients may prove useful in clinical practice to rule out thrombotic events, in accordance with other risk factors and symptomatology.
Introduction
D-dimer (DD) molecules are generated through the degradation of cross-linked fibrin during fibrinolysis. Plasmin digestion of the fibrin clot results in formation of DD molecule. The presence of DD molecule is suggestive but not conclusive of thrombosis. DD is reported to be elevated in venous thromboembolism (VTE), pulmonary embolism (PE), disseminated intravascular coagulation, acute myocardial infarction and thrombotic thrombocytopenic purpura (TTP) [1].
DD levels were found to be elevated after various surgical procedures independent of the occurrence of VTE [2]. There are various studies in literature pointing out the elevation of DD levels after surgical interventions such as abdominal or orthopedic surgeries. As a result, although the value of the DD test in the diagnosis of VTE is well known, controversial findings have been reported about the cut-off values that would suggest VTE in postsurgical patients [2], [3], [4], [5], [6], [7]. There are few studies in the literature reporting the rate of VTE after otolaryngological head and neck surgeries (OHNS) and the rate is reported between 0.1 and 5 %. In addition, it has been reported that rates as high as 5 ng/mL occur after cancer and flap reconstruction surgeries. Especially cancer surgeries with neck dissection are highly invasive procedures in which the hemostatic system is massively activated as reported above. They are associated with thromboembolic events more frequently than other surgeries. To our best knowledge, although there are studies in the literature about DD levels after orthopedic and abdominal surgeries, there are no studies evaluating DD levels after head and neck surgeries, especially with neck dissection. It is well known that the deep vein thrombosis incidence is relatively lower in head and neck surgery. Routine perioperative work-up does not include checking DD levels; it is only recommended if there is suspition for thromboembolic events, since false positive results are frequent and can be caused by various pathologies [8]. Determining the fluctuations caused by surgery in this population has potential to aid clinical judgement, since there is no predetermined cut-off value for DD to diagnose thrombosis. Clarifying the natural course of DD levels in this setting may prevent unnecessary diagnostic and therapeutic interventions. In this study, we investigated the perioperative DD levels in patients who underwent neck dissection along with resection of the primary tumor due to head and neck cancer.
Materials and methods
This study was designed as a prospective observational study in our otorhinolaryngology clinic. The study included head and neck cancer patients who underwent neck dissection along with resection of primary tumor at Ankara Bilkent City Hospital between January 10, 2022 and June 20, 2023. Exclusion criteria in the study were as follows; recent trauma or surgical intervention, history of liver or kidney disease, history of former VTE. The primary outcome was to determine the course of DD levels through the first two weeks of head and neck surgery.
Blood samples were taken from all the patients one day before surgery and on days 0–7 and 14 after surgery and DD levels were determined.
DD test was measured on the CS-5100 System device using the Siemens INNOVANCE D-dimer test kit (Siemens Medical Solutions Diagnostics, Deerfield, IL, USA). A citrated platelet poor plasma sample was used as the sample. The test method is a particle-enhanced, immunoturbidimetric assay. In this method, polystyrene particles covalently coated with monoclonal mouse antibody (8D3) are aggregated when mixed with samples containing D-dimer, and then turbidimetrically detected by increasing turbidity. Decreased transmitted light caused by aggregates is measured at 570 nm, D dimer concentration is directly proportional with the agglutination degree. According to the manufacturer’s specifications; measuring range of the assay is 0.17–4.40 mg/L fibrinogen equivalent units (FEU). The Limit of Detection is 0.05 mg/L FEU. The within-lab coefficients of variation (CVs) is 2.2 and 4.3 %; repeatability CVs 1.4 and 4.1 % for the high and low control samples, respectively. Values 0.55 mg/L and below are considered normal in accordance with the recommendations of manufacturer. The study was approved by the local Ethics Committee. Written informed consent was obtained from all patients participating in the study.
Statistical analysis was performed using IBM SPSS version 26 software. The distribution of the variables was examined using visual (histogram and probability graphs) and analytical methods (Shapiro-Wilk test). The statistical significance of the change in DD levels over time was examined using the Friedman test. Pairwise comparisons were made using the Wilcoxon test and evaluated using the Bonferroni correction when necessary. Type-1 error level was determined as 5 % for statistical significance.
Results
Twenty-one patients were included in the study. Ages of the patients were between 40 and 86 with a mean of 63.9 years. Six of the patients were female and 15 were male. Age, gender of the patients and the location of the primary tumor are shown in Table 1. In addition to resection of the primary tumor, six of the patients underwent unilateral and 15 patients underwent bilateral modified neck dissection. Three (14.3 %) of the patients had thyroid, 11 (52.3 %) had oral cavity, 1 (4.8 %) had parotid, 5 (23.8 %) had larynx and 1 (4.8 %) had nasal dorsum cancer.
Age, gender of the patients, location of primary tumor and presence of neck dissection.
| Age, years ± SD | 63.95 ± 2.93 | |
|---|---|---|
| Number of patients, n | Percent | |
| Gender | ||
| Male | 14 | 66.6 % |
| Female | 7 | 33.3 % |
| Location of primary tumor | ||
| Thyroid | 3 | 14.3 % |
| Oral cavity | 11 | 52.3 % |
| Parotid | 1 | 4.8 % |
| Larynx | 5 | 23.8 % |
| Nasal dorsum | 1 | 4.8 % |
| Neck dissection | ||
| Unilateral | 6 | 28.6 % |
| Bilateral | 15 | 71.4 % |
-
SD, standard deviation.

Preoperative and postoperative D-dimer levels. It was observed that the average DD values peaked on the first (approximately 5 times of the preoperative values) day, then gradually decreased and reached a level slightly below 2 times of the preoperative values on the 14th day.
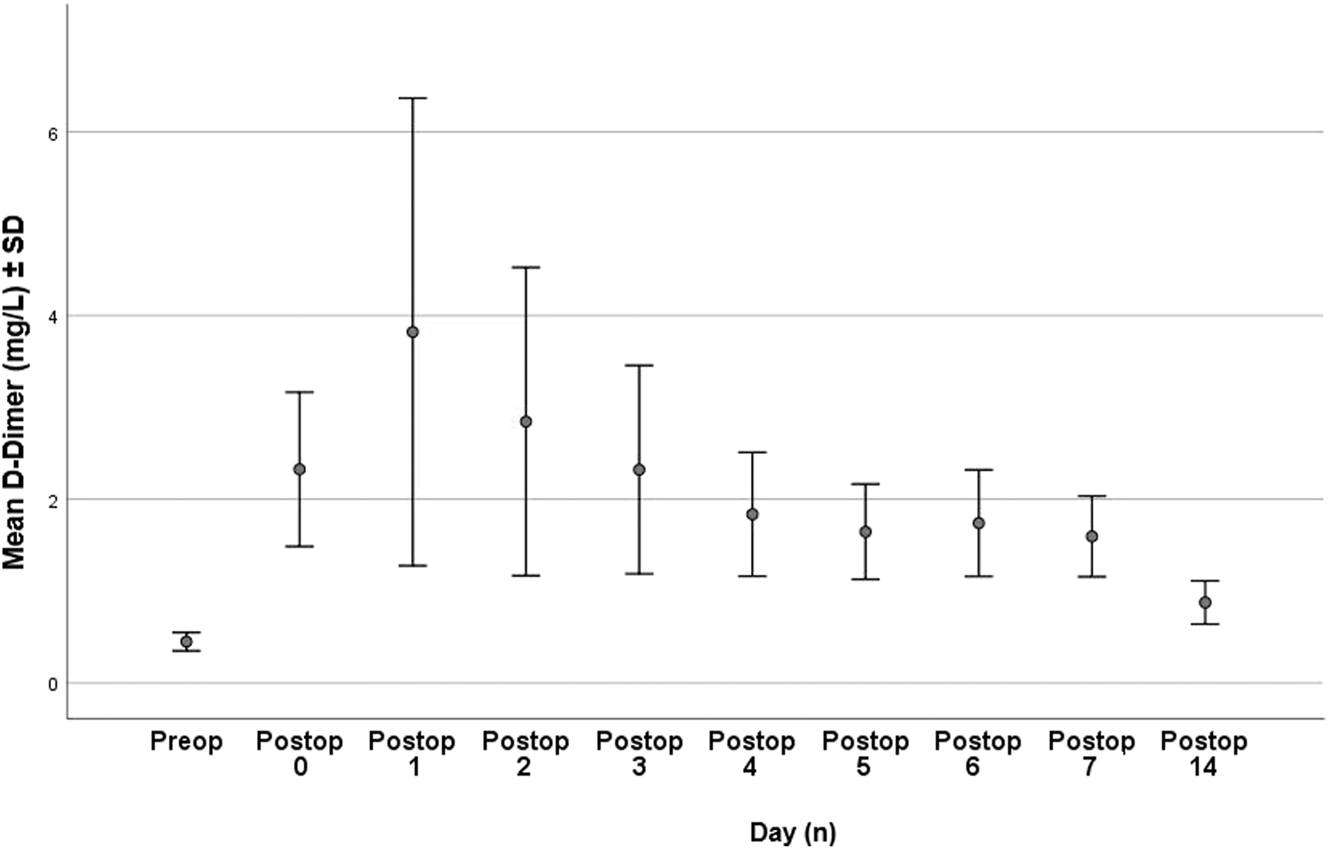
Means and standard deviations of D-dimer levels on each day. The means and standard deviations of each day is summarized. DD levels peaked at 2.58 (0.34–6.48) ng/mL on the postoperative first day and decreased gradually and reached a level slightly below 2 times the preoperative levels on the 14th day.
The change in D-dimer levels between preoperative and postoperative days 1–14 was statistically significant when evaluated by Friedman analysis (p<0.001, Table 2). Pairwise comparisons were evaluated with Wilcoxon test to determine which days caused the difference individually (Figures 1 and 2).
Preoperative and postoperative D-dimer levels on each day.
| Mean (± SD), mg/L | ||
|---|---|---|
| Preoperative | 0.44 (0.23) | p<0.01a |
| Postoperative 0 | 2.32 (1.92) | |
| Postoperative 1st day | 3.82 (5.83) | |
| Postoperative 2nd day | 2.84 (3.84) | |
| Postoperative 3rd day | 2.32 (2.60) | |
| Postoperative 4th day | 1.83 (1.54) | |
| Postoperative 5th day | 1.64 (1.18) | |
| Postoperative 6th day | 1.73 (1.32) | |
| Postoperative 7th day | 1.59 (1.00) | |
| Postoperative 14th day | 0.87 (0.54) |
-
aFriedman test, SD, standard deviation.
There was a statistically significant difference between preoperative DD levels and DD levels on the first seven days and the 14th day (p<0.01).
When the DD levels on postoperative day 0 and on the following 7 days were compared among themselves, the difference was not significant, except for day 0 and 7. The difference between DD levels measured on each day of the first week and levels on 14th day was found to be significant (p<0.01), Figure 3.

Comparison of D-dimer levels of postoperative day 0 and postoperative days. Comparisons of the following days with postoperative day 0 DD levels are summarized. Each day in the first week and postoperative day 14 is significantly higher than levels on postoperative day 0.
The findings suggest that the significance found in Friedman test is mostly due to the difference between DD levels of days 1–7 and day 14. Also, preoperative DD levels differ significantly from each postoperative day, as do DD levels of postoperative day 0 and day 7.
Discussion
Venous thromboembolism comprising both VTE and PE is one of the major causes of perioperative morbidity and mortality [9], [10], [11].
This condition is responsible for 5–10 % of all hospital deaths in the USA. Surgery increases the risk of VTE nearly 20-fold [9].
The incidence of symptomatic VTE following abdominal surgery has been reported to vary between 0.3 and 2.8 %, depending on the type of surgery [3]. While the CHEST guideline published in 2012 provides recommendations for the prevention of VTE in orthopedic and non-orthopedic surgeries, there are no recommendations regarding OHNS [8]. Recent studies have demonstrated that although the risk of VTE is generally lower in otolaryngologic interventions, there is a significantly higher risk of VTE in head and neck cancer surgeries accompanied by neck dissection and reconstructive surgeries [9], 10]. In a meta-analysis published in 2018, the overall prevalence of VTE in head and neck cancer patients who underwent resection was reported to be 5 % [10]. Due to this high VTE risk seen in cancer patients, early diagnosis and treatment is important. Although the role of detecting DD elevation in the diagnosis of VTE in postsurgical patients is controversial, it is now widely accepted that a value less than a given threshold rules out the presence of concurrent thrombotic pathologies [6].
In a retrospective study including patients with malignancies, Kiyaoki et al. reported that the DD cut-off value for the diagnosis of VTE in this group is 4.0 μg/mL [12]. In another retrospective VTE study, Vitali K et al. reported that values more than 10-fold above the reference limit may provide diagnostic information, while lower concentrations may be useful in ruling out VTE [13].
Although there are studies reporting the risk of VTE as high as 5 % in patients who underwent head and neck cancer surgery, there are no studies about DD levels after head and neck cancer surgery.
Dindo D. et al. investigated DD levels after general surgery and reported that DD levels increased after surgeries that did not include abdominal cavity and reached its peak on day 7, but did not exceed upper limits. They demonstrated that after intraabdominal operations, it reached an average of 1,500 ng/mL (200–7,800) and returned to normal after 25 days. They also found that after retroperitoneal and liver surgery it reached an average of 4,000 ng/mL (500–14,400) and returned to normal after 38 days. They also concluded that DD levels can be predicted after abdominal surgeries and can be used in the diagnostic algorithm of VTE [3].
In another study, DD levels were investigated after laparoscopic cholecystectomy and hip surgery and following results were reported: After laparoscopic cholecystectomy, DD levels increased persistantly until the postoperative 15th day. On the other hand, two peaks were observed on days 1 and 7 after hip surgery. As a result, the authors concluded that the different DD values resulting from the heterogenous responses of hematopoetic system depending on the underlying pathology and the type of surgery limits the use of this test in the diagnosis of VTE [6].
In our study, it was observed that DD levels peaked at 2.58 (0.34–6.48) ng/mL on the postoperative first day and decreased gradually and reached a level slightly below 2 times the preoperative levels on the 14th day.
PTE was detected by pulmonary computerized angiography in one patient (who was excluded from the scope of study) with a DD value of 26.88 ng/mL and complaints of dyspnea and chest pain on the postoperative first day. Although this finding is insufficient to be evaluated statistically, it is compatible with the pulmonary embolism rate reported in the literature after head and neck cancer surgery. Also, it is notable that the patient’s DD level was much more than 5-fold of the mean DD level of the patients without detectable thrombosis on day 1.
Although our findings are somewhat similar to findings after hip surgery, they differ significantly from the results of abdominal surgery.
It should also be noted as an important point that laboratory results are not fixed numbers and vary mainly from two sources: laboratory-related and biological variations. Biological variations data have been widely used for the evaluation of the utility of population based reference intervals so reliable data are essential in the application of the biological variations of measurands in clinical practice [14]. Furthermore, it is known that coagulation parameters are susceptible to various sources of interference, which also may complicate the interpretation of the results [15]. The data obtained with this study will contribute to the determination of variations in DD levels after such surgeries.
Considering the average peak values of our data, we can recommend that an increase of more than 5 times the reference values may be suggestive for thrombotic events in similar patients and further diagnostic procedures may be warranted, considering other risk factors and symptomatology. Also, the highest DD value detected in the study group was 11.64, noticably lower than the patient’s value who was diagnosed with PTE. It is also notable that DD levels tend to decrease gradually after postoperative day 1 and persistent higher values, especially after postoperative day 7 may be suggestive of DVT and other thrombotic events. Although these findings cannot be generalized to all populations, since there are no studies about head and neck cancer patients underwent surgery with neck dissection and trends of DD levels, these findings, especially providing information about the decreasing trend of DD value may be useful in clinical practice.
There are several limitations to our study. Despite our study provides information about the changes in DD levels in this setting, since only one patient had a thromboembolic event, comparison between groups could not be made possible. However, although cannot be compared statistically and suggested as a cut-off value since there is only one case, this patient had a DD level of more than 5 times of the upper limit, substantially higher than all other patients. Moreover, although the number of patients were sufficient and in accordance with our initial power analysis, some subgroups may have been underrepresented due to the rarity of the pathologies, which causes heterogeneity and could have influenced outcomes. Also, our findings need validation with randomized prospective studies to increase generalizability. Despite these limitations, the trend of DD levels following surgery may prove useful in clinical practice to help rule out thrombotic events. It should also be emphasized that at this time, there is no single coagulation test to guide management in this population, and other risk factors, symptomatology and physical examination findings are essential to improve patient outcomes.
Acknowledgments
The authours would like to thank the staff of the Deparment of Otolaryngology in Ankara City Hospital for their contributions.
-
Research ethics: The study was approved by Ankara City Hospital 2nd Clinical Research Ethics Committee (E.Kurul-E1-22-2392). All procedures were carried out in accordance with the ethical rules and the principles of the Declaration of Helsinki.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: Authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Data available on reasonable request.
References
1. Johnson, ED, Schell, JC, Rodgers, GM. The D‐dimer assay. Am J Hematol 2019;94:833–9. https://doi.org/10.1002/ajh.25482.Search in Google Scholar PubMed
2. Sudo, A, Wada, H, Nobori, T, Yamada, N, Ito, M, Niimi, R, et al.. Cut-off values of D-dimer and soluble fibrin for prediction of deep vein thrombosis after orthopaedic surgery. Int J Hematol 2009;89:572–6. https://doi.org/10.1007/s12185-009-0323-4.Search in Google Scholar PubMed
3. Dindo, D, Breitenstein, S, Hahnloser, D, Seifert, B, Yakarisik, S, Asmis, LM, et al.. Kinetics of D-dimer after general surgery. Blood Coagul Fibrinolysis 2009;20:347–52. https://doi.org/10.1097/mbc.0b013e32832a5fe6.Search in Google Scholar
4. Jiang, Y, Li, J, Liu, Y, Li, YC, Zhang, WG. Risk factors for deep vein thrombosis after orthopedic surgery and the diagnostic value of D-dimer. Ann Vasc Surg 2015;29:675–81. https://doi.org/10.1016/j.avsg.2014.12.022.Search in Google Scholar PubMed
5. Toner, E, Oputa, T, Robinson, H, McCabe-Robinson, O, Sloan, A. Serum D-dimer should not be used in the diagnosis of venous thromboembolism within 28 days of total knee replacement surgery. Knee Surg Relat Res 2020;32:49. https://doi.org/10.1186/s43019-020-00068-x.Search in Google Scholar PubMed PubMed Central
6. Lippi, G, Veraldi, GF, Fraccaroli, M, Manzato, F, Cordiano, C, Guidi, G. Variation of plasma D-dimer following surgery: implications for prediction of postoperative venous thromboembolism. Clin Exp Med 2001;1:161–4. https://doi.org/10.1007/s10238-001-8029-9.Search in Google Scholar PubMed
7. Qin, L, Fu, Y, Li, C, Chen, S, Lv, Y, Hao, M, et al.. Analysis of risk factors for high postoperative D-dimer levels: a single-center nurse-observational study. Int J Biol Markers 2020;35:23–8. https://doi.org/10.1177/1724600820931861.Search in Google Scholar PubMed
8. Moubayed, SP, Eskander, A, Mourad, MW, Most, SP. Systematic review and meta‐analysis of venous thromboembolism in otolaryngology–head and neck surgery. Head Neck 2017;39:1249–58. https://doi.org/10.1002/hed.24758.Search in Google Scholar PubMed
9. Ahmad, FI, Clayburgh, DR. Venous thromboembolism in head and neck cancer surgery. Cancer Head Neck 2016;1:13. https://doi.org/10.1186/s41199-016-0014-9.Search in Google Scholar PubMed PubMed Central
10. Lundbech, M, Krag, AE, Hvas, A-M. Prevalence of venous thromboembolism following head and neck cancer surgery: a systematic review and meta-analysis. Thromb Res 2018;169:30–4. https://doi.org/10.1016/j.thromres.2018.07.009.Search in Google Scholar PubMed
11. Albertsen, IE, Lyhne, NM, Larsen, TB, Nielsen, PB. Incidence of venous thromboembolism following head and neck surgery. Eur Arch Oto-Rhino-Laryngol 2023;280:5081–9. https://doi.org/10.1007/s00405-023-08112-8.Search in Google Scholar PubMed PubMed Central
12. Niimi, K, Nishida, K, Lee, C, Ikeda, S, Kawai, Y, Sugimoto, M, et al.. Optimal D-dimer cutoff values for diagnosing deep vein thrombosis in patients with comorbid malignancies. Ann Vasc Surg 2024;98:293–300. https://doi.org/10.1016/j.avsg.2023.06.033.Search in Google Scholar PubMed
13. Koch, V, Martin, SS, Gruber-Rouh, T, Eichler, K, Mahmoudi, S, Leistner, DM, et al.. Cancer patients with venous thromboembolism: diagnostic and prognostic value of elevated D‐dimers. Eur J Clin Invest;53. https://doi.org/10.1111/eci.13914.Search in Google Scholar PubMed
14. Çevlik, T, Turkal, R, Haklar, G, Şirikçi, Ö. A case of falsely elevated D-dimer result. Turk J Biochem 2022;47:686–9. https://doi.org/10.1515/tjb-2021-0262.Search in Google Scholar
15. Emre, HO, Karpuzoglu, FH, Coskun, C, Sezer, ED, Ozturk, OG, Ucar, F, et al.. Utilization of biological variation data in the interpretation of laboratory test results – survey about clinicians’ opinion and knowledge. Biochem Med 2021;31:93–102. https://doi.org/10.11613/bm.2021.010705.Search in Google Scholar
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Interaction of fetuin-A with obesity related insulin resistance and diabetes mellitus
- Research Articles
- Preanalytical errors in pediatric blood sampling: a systematic review of common challenges and risks
- The promotive role of reticulocalbin 3 (RCN3) in the pathogenesis of keloid via TGFβ1/Smad2/Smad7 signaling pathway in vitro
- Investigation into drug resistance to cisplatin in cancer stem cell-enriched population in non-small cell lung cancer
- The cytotoxic and antiproliferative effect of Polygala saponin XLIV on the human colorectal carcinoma cell line
- Development of HEK293T cell reference materials for β-thalassemia genetic testing using prime editing
- Investigation of propofol, fentanyl, and midazolam-related toxicity and the protective effect of midazolam on THLE-2 cell lines
- Leucine-rich α-2-glycoprotein 1 can be a novel angiogenic mediator in autosomal dominant polycystic kidney disease
- Asiaticoside reverses the inhibition effect of miR-184 on proliferation, migration and AKT phosphorylation of HTR-8/Svneo cells
- Perioperative D-dimer levels and head and neck cancer surgery: a prospective observational study
- Comprehensive analysis of KRT15 in pan-cancer and verification in lung adenocarcinoma
- Age and sex-dependent effects of nitrosative stress on the osmotic fragility of human red blood cells
- Evaluation of oxidative stress parameters in older patients with urinary incontinence
- Determination of reference change values for thyroid-related biomarkers: TSH, fT3, fT4, Tg, Anti-Tg, and Anti-TPO
- An evaluation of serum boron level in pregnancies with severe pre-eclampsia
- Involvement of SIRT3/FOXO1 and TLR4/NF-κB/NLRP3 pathways in protective effects of Δ(9)-tetrahydrocannabinol on diabetic cardiomyopathy in rats
- Evaluating the potential therapeutic effect of Rosa damascena Mill. essential oil on acetic acid-induced ulcerative colitis in rats
- Assessment of blood collection competency in phlebotomists: a survey study
Articles in the same Issue
- Frontmatter
- Review
- Interaction of fetuin-A with obesity related insulin resistance and diabetes mellitus
- Research Articles
- Preanalytical errors in pediatric blood sampling: a systematic review of common challenges and risks
- The promotive role of reticulocalbin 3 (RCN3) in the pathogenesis of keloid via TGFβ1/Smad2/Smad7 signaling pathway in vitro
- Investigation into drug resistance to cisplatin in cancer stem cell-enriched population in non-small cell lung cancer
- The cytotoxic and antiproliferative effect of Polygala saponin XLIV on the human colorectal carcinoma cell line
- Development of HEK293T cell reference materials for β-thalassemia genetic testing using prime editing
- Investigation of propofol, fentanyl, and midazolam-related toxicity and the protective effect of midazolam on THLE-2 cell lines
- Leucine-rich α-2-glycoprotein 1 can be a novel angiogenic mediator in autosomal dominant polycystic kidney disease
- Asiaticoside reverses the inhibition effect of miR-184 on proliferation, migration and AKT phosphorylation of HTR-8/Svneo cells
- Perioperative D-dimer levels and head and neck cancer surgery: a prospective observational study
- Comprehensive analysis of KRT15 in pan-cancer and verification in lung adenocarcinoma
- Age and sex-dependent effects of nitrosative stress on the osmotic fragility of human red blood cells
- Evaluation of oxidative stress parameters in older patients with urinary incontinence
- Determination of reference change values for thyroid-related biomarkers: TSH, fT3, fT4, Tg, Anti-Tg, and Anti-TPO
- An evaluation of serum boron level in pregnancies with severe pre-eclampsia
- Involvement of SIRT3/FOXO1 and TLR4/NF-κB/NLRP3 pathways in protective effects of Δ(9)-tetrahydrocannabinol on diabetic cardiomyopathy in rats
- Evaluating the potential therapeutic effect of Rosa damascena Mill. essential oil on acetic acid-induced ulcerative colitis in rats
- Assessment of blood collection competency in phlebotomists: a survey study

