Abstract
Objective
Myocarditis is an inflammatory disease of the cardiac muscle. Prognosis is most often good but, in some patients, the disease can be fulminant. Our aim with this study was to determine interleukin-9 (IL-9) and interleukin-17 (IL-17) levels in myocarditis cases with different etiologies.
Materials and methods
Thirty one patients with myocarditis and 30 healthy controls of similar age and gender without a history of chronic disease were included in the study. All 31 patients were clinically myocarditis. In some of these patients, the cause of myocarditis is acute rheumatic fever or Kawasaki disease. Serum samples of the patients were taken during diagnosis in order to analyze serum IL-9 and IL-17 levels and sedimentation rate, CRP, ASO, pro-BNP, CK-MB, and Troponin-I tests were performed.
Results
It was found that IL-17 levels were statistically significant in all acute rheumatic fever, Myocarditis and Kawasaki patients compared to the control group (p = 0.001) and that cut-off was 4.30 pg/mL. This value was determined to be 71% sensitive and 67% specific for IL-17 (AUC = 0.761).
Conclusions
Both of the mean and median levels of IL-17 were significantly higher in pediatric patients with myocarditis than in healthy children. Our study made us think that complications of myocarditis and associated morbidity can be prevented by IL17 inhibitors. The high levels of IL17 found in our study may be a reference for future study.
Öz
Amaç
Miyokardit, kalp kasını tutan inflamatuar bir hastalıktır. Prognoz genel olarak iyidir, ancak bazı hastalarda hastalık fulminant seyredebilir. Bu çalışma ile amacımız, farklı etiyolojili miyokardit olgularında IL-9 ve IL-17 düzeylerini belirlemektir.
Gereç ve yöntem
Çalışmaya 31 miyokarditli hasta ve kronik hastalık öyküsü olmayan benzer yaş ve cinsiyet te 30 sağlıklı kontrol dahil edildi. 31 hastanın tümü klinik olarak miyokardit idi. Bu hastaların bazılarında, miyokarditin nedeni akut romatizmal ateş veya Kawasaki hastalığıdır. Serum IL-9 ve IL-17 düzeylerini analiz etmek için tanı sırasında serum örnekleri alındı ve sedimantasyon hızı, CRP, ASO, pro-BNP, CK-MB ve Troponin-I testleri yapıldı.
Bulgular
Kontrol grubu ile karşılaştırıldığında Akut romatizmal ateş, Kawasaki ve diğer nedenlerle oluşan tüm miyokardit hastalarında IL-17 düzeylerinin istatistiksel olarak anlamlı fark olduğu bulundu (p = 0.001) ve cut-of değeri 4.30 pg/mL idi. Bu değerin IL-17 için %71 duyarlı ve %67 spesifik olduğu tespit edildi (AUC = 0.761).
Sonuçlar
Miyokarditli pediatrik hastalarda IL-17’nin ortalama ve ortanca düzeyleri sağlıklı çocuklardan anlamlı derecede yüksekti. Çalışmamız, miyokardit komplikasyonlarının ve myokardite bağlı morbiditenin IL-17 inhibitörleri tarafından önlenebileceğini düşündürdü. Çalışmamızda bulunan yüksek IL-17 düzeyleri gelecekteki çalışmalar için referans olabilir.
Introduction
Myocarditis is characterized with inflammation and necrosis of myocardium and is developed independently from coronary artery disease [1]. Among acquired cardiac diseases, it has very high morbidity and mortality in childhood and young adults, especially in the neonatal period [2]. Therefore, in our study, we received myocarditis cases with various causes such as acute rheumatic fever (ARF), Kawasaki disease which affect the heart throughout life. We have investigated interleukin-9 (IL-9) and interleukin-17 (IL-17) levels, which have previously been involved in inflammatory diseases by thinking that there is an autoinflammatory process in myocarditis cases with different etiologies.
Coronary thrombus, myocardial infarction, and correspondingly sudden death can develop in patients diagnosed with Kawasaki disease who do not receive treatment. The risk of coronary artery disease significantly reduces with early diagnosis and treatment [3].
Cardiac involvement is seen in nearly half of the cases in ARF, the most common and most important cause of acquired cardiac diseases in childhood [4], [5]. In acute rheumatic fever, cardiac involvement varies from mild and temporary cardiac involvement to exudative pancarditis showing a mortal course [6].
The pathological basis of myocarditis is associated with viral cytopathic effect [7], whereas, it is associated with infectious agents and superantigen theory in Kawasaki disease [8] and with cross-reactivity of antibodies produced against streptococci in ARF [9], [10]. These findings show that these diseases have an immunological basis.
Th-17 cells produce IL-17. IL-17 is involved in the inflammatory process. IL-17 is the key cytokine in the invocation, activation and migration of neutrophils. Th-17 cells are among the main triggers of tissue inflammation and they have been found to be related to the pathogenesis of the most of experimental autoimmune diseases and various inflammatory events in humans. IL-17-mediated inflammation is not protective, has serious immunopathological consequences and carries a risk of activation of autoimmunity [11]. IL-9 is a cytokine that has a pleiotropic effect on different cell types and that is produced by T cells. Biological functions of IL-9; stimulating proliferation of activated T cells, increasing the production of immunoglobulin in B cells, stimulating the proliferation and differentiation of mast cells and stimulating hematopoietic stem cells [12].
During the literature review, it was determined that there are several studies on IL-9 and IL-17. However, there is no study conducted with myocarditis patients. This makes our study first in investigating the relation with IL-17 and IL-9 in myocarditis patients.
Methods
Myocarditis cases who applied to Kahramanmaras Sutcu Imam University, Faculty of Medicine Research and Application Hospital Pediatrics Department between February and August 2017 and who developed myocarditis due to various etiologies were included in the study.
The Ethics Committee approval was obtained for this study. The content of the study was explained to the relatives of the patients included in the study in detail and their written consents were taken. In this study, there were 31 patients in the patient group and 30 individuals in the control group. Patients who were aged between 0 and 18 years and who were recently diagnosed with myocarditis, ARF and Kawasaki disease were included in the study. All of our patients have myocarditis but six patients had myocarditis due to ARF and seven patients had myocarditis due to Kawasaki disease. Patients were evaluated with echocardiography (ECO) who were diagnosed clinically compatible with myocarditis. The diagnosis of myocarditis was confirmed by ECO. The control group consisted of 30 healthy children who were in the similar age group and gender with the patient group, who did not have a history of the previous known cardiac disease, who did not have chronic disease history and who did not get any infection diagnosis. The age and gender were similar in the patient and control groups.
Blood samples of the patients included in the study were taken for sedimentation rate, CRP, ASO, Pro-BNP, CK-MB and Troponin-I during the diagnosis and tested on the same day. 4–5 cc venous blood samples were collected from the patients during the diagnosis in order to analyze IL-9 and IL-17 levels in biochemistry tubes. Samples stored at −80°C were dissolved at room temperature. Based on the recommendations of the company, samples were analyzed using ‘Enzyme-Linked Immunosorbent Assay’ (ELISA) method with Human IL-17A Platinum ELISA and Human IL-9 Platinum ELISA kits in the ELISA reader (Thermo Scientific Multiscan FC Elisa Reader). The results obtained were given in pg/mL.
The findings obtained from the experiments were analyzed using “SPSS 16.0 for Windows” statistical package software. The conformity of the data to a normal distribution was tested using Kolmogorov-Smirnov Test and the homogeneity of variances was tested using “Homogeneity of Variance Test-Levene Statistic”. “Independent Sample T Test” was used for the independent samples in the analysis of the data that were not conforming to a normal distribution and that were not homogeneous variances. “Mann-Whitney U Test” and “Kruskal-Wallis Variance Analysis” were used for the analysis of the data that were non-conforming to a normal distribution and that were non-homogeneous data. Mann-Whitney U-test was used for the double comparisons and statistical significance was evaluated by performing Bonferroni correction. “Chi-square test” was used for the analysis of the qualitative data. For statistical significance, the probability value (p-value) was selected as 0.05. Test results that had a p-value lower than 0.05 were considered significant. All values were given as “mean±standard deviation”.
Results
There were 31 patients in the patient group and 30 individuals in the control group. Of the patients, 23 were male and 8 were female and the mean age was found as 8.7 years (1 year–17 years).
Biochemical parameters were assessed in patients with ARF, myocarditis and Kawasaki disease. The mean CRP value was 69.71 mg/L in patients with acute rheumatic fever and 16.94 mg/L in myocarditis group, and there was a significant difference found between them (p=0.005). ASO levels of patient subgroups were compared and ASO levels of patients with ARF (949.86 IU/mL) were found to be significantly higher than those in patients with Kawasaki disease (89.33 IU/mL) and with myocarditis (254.33 IU/mL) (p<0.05). There was no statistically significant difference found between subgroups in terms of sedimentation rate, pro-BNP, CKMB, and Troponin-I.
There was no statistically significant difference determined between the control group and the patient group in terms of serum IL-9 level (p=0.077) (Table 1). There was no statistically significant difference found among the patient subgroups (ARF-Kawasaki, ARF-Myocarditis and Kawasaki-Myocarditis) in terms of IL-9 measurement (p-values: 0.568, 0.952, 0.368, respectively).
IL-9 and IL-17 measurements in patient and control groups.
| Groups/parameters | IL-9 (pg/mL) | IL-17 (pg/mL) |
|---|---|---|
| Control | 4.412±0.730 | 4.272±0.743 |
| Patient | 4.049±0.841 | 4.805±0.832a |
| ARF | 4.053±0.720 | 5.353±1.357 |
| Kawasaki | 4.255±4.433 | 5.002±0.699 |
| Myocarditis | 3.978±0.995 | 4.527±0.459 |
aUsing “Kruskal-Wallis Variance Analysis”, p<0.05, significant.
There was a statistically significant difference noticed between the control group and the patient group in terms of serum IL-17 level (p=0.001) (Table 1). It was found that IL-17 levels were statistically significantly higher in all patients with myocarditis. There was no statistically significant difference found between ARF-Kawasaki, ARF-Myocarditis and Kawasaki-Myocarditis subgroups in terms of IL-17 measurement (p-values: 0.668, 0.155, 0.205, respectively) (Figures 1 and 2).
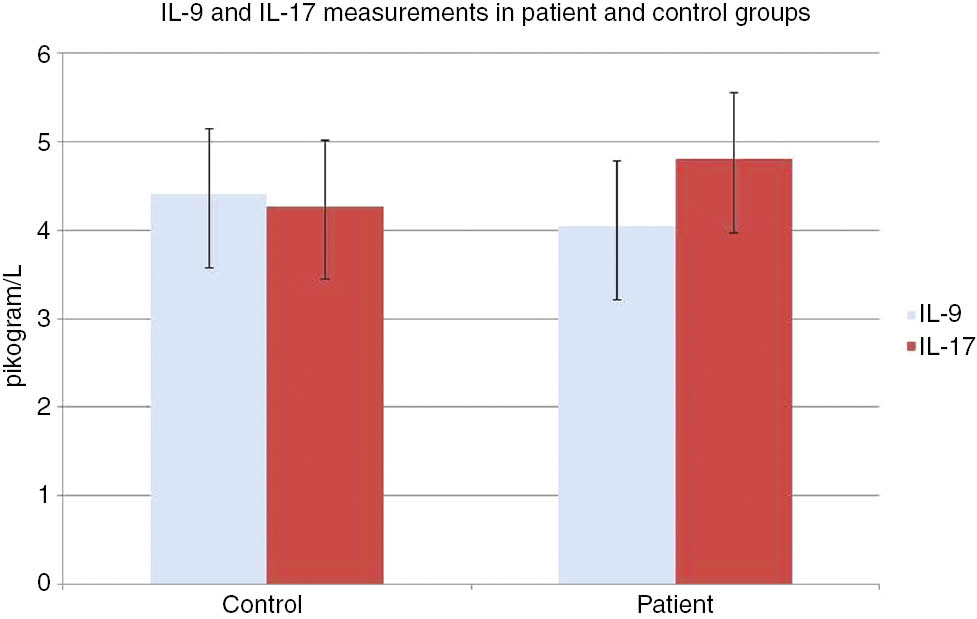
IL-9 and IL-17 measurements in patient and control groups.
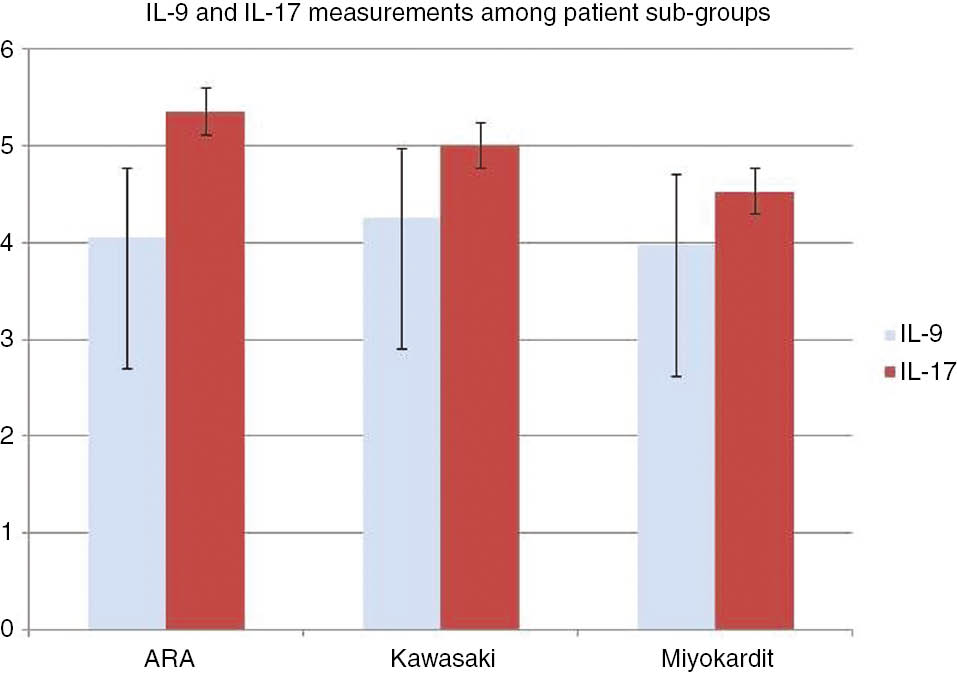
IL-9 and IL-17 measurements among patient subgroups.
Roc Analysis was performed for the IL-17 level which was found to be statistically high at a significant level and cut-off was found as 4.30 pg/mL. This value was determined as 71% sensitive and 67% specific for IL-17 (AUC=0.761).
Discussion
Inflammatory factors are involved in the etiopathogenesis of myocarditis [13]. For this reason, which are inflammatory markers, IL-9 and IL-17, were evaluated in our study. It has been reported that IL-9, one of the interleukins involved in inflammatory response, is responsible for airway hypersensitivity and increased mucus secretion generally in asthmatic patients and experimental asthma models in the studies. In a previous study conducted on rats, it has been shown that increased IL-9 in transgenic mouse lungs leads to mast cell hyperplasia, increased airway inflammation and bronchial hyperreaction [14]. In another study, it has been reported that the expression of IL-9 increases the mucus secretion by affecting the sub-groups of mucin genes both in vivo and in vitro [15]. In our study, serum IL-9 level was found to be higher in the patient group than in the control group; however, it was not statistically significant. Our study is an original study in terms of IL-9 assessment in cardiac patients. In future studies, significant findings in terms of IL-9 may be obtained by performing repeated measurements in larger patient groups and at different stages of the diseases in cardiac diseases.
A high level of IL-17 in patients with myocarditis was the most important finding in our study. In this study, the mean serum IL-17 level was determined to be higher in the patient group compared to the control group and the difference was statistically significant (p=0.001). It has been reported in previous studies that IL-17 has an active role in autoimmune diseases, in particular; and that high IL-17 levels in rheumatologic diseases are associated with poor prognosis. In a study conducted on patients with rheumatoid arthritis, it has been shown that TNF, IL-1 and IL-17 cytokine expressions are high in patients and that this high level is a determinant for joint damage [16]. In our study, the fact that IL-17 levels were statistically significantly high in patients with ARF, myocarditis, and Kawasaki diseases that involve autoimmunity in etiology supports this study in terms of the relation between autoimmunity and IL-17.
There is no study on IL-17 in myocarditis; however, there are studies supporting the fact that IL-17 level is high in acute coronary syndromes among cardiac diseases. IL-17 levels were found to be higher in patients with the acute coronary syndrome [17]. In another study conducted on the acute coronary syndrome, it has been thought that IL-17 and other pro-inflammatory cytokines are involved in the pathogenesis of acute coronary syndrome [18]. There are also studies investigating IL-17 levels in atherosclerosis cases. In mice in which experimental atherosclerosis model has been developed by creating Apolipoprotein E deficiency, it has been found that IL-17A is functionally blocked, resulting in decreased infiltration of inflammatory cells into atheroma plaques and development of vascular inflammation [19]. All these studies support the fact that IL-17 leads to inflammation in cardiac diseases. In a study conducted on patients with the acute coronary syndrome, there was a positive relation determined between IL-17A levels and it has been reported that IL-17 leads to platelet aggregation by using the ERK2 signaling pathway [20].
In a study conducted on psoriasis patients, it has been found that Th17 increases in skin lesions of patients and that anti-TNF agent used in the treatment of psoriasis disease have an effect by decreasing Th17 cells [11]. In our study, the fact that IL-17 was determined to be high suggests that the use anti-TNF agents may give positive results in the treatment processes of these diseases in terms of prognosis. There has been a significant improvement in plaques with secukinumab treatment, the first anti-IL-17A agent that is rapidly used in recent years in the treatment of moderate and severe plaque psoriasis [21]. On the contrary, there is no study conducted on secukinumab treatment in childhood. The fact that a significant response is obtained with anti-IL-17A treatment in psoriasis disease suggested that treatments such as anti IL-17 may be beneficial in patients with myocarditis; that the disease may be taken under control with early treatment before the development of sequelae, in this study. In two different studies conducted, it has been found that cerebrospinal fluid and serum of patients with multiple sclerosis contains a high level of IL-17 [22], [23], [24], [25]. In this study, it was suggested that measurement of IL-17 levels from pleural effusion fluid in patients with cardiac involvement progressing with pericardial effusion may contribute to the diagnosis and prognosis.
Studies conducted on IL-17 are usually designed to investigate asthma and its pathophysiology. In these studies, the common opinion was that IL-17 is also associated with fibrosis of basal membranes in the pathophysiology of asthma [26]. Some ARF, myocarditis, and Kawasaki patients have a good prognosis while some have severe and progressive cardiac involvement. The fact that the high IL-17 level determined in asthmatic patients is associated with fibrosis and is therefore poorly prognostic factors suggests that the high IL-17 levels in our study may lead to cardiac fibrosis in patients with severe and progressive cardiac involvement. Future studies may allow the clinical classification of these patients as mild, moderate and severe cardiac involvement and the association of IL-17 levels with prognosis.
The low number of patients is the limitation of this study. Further studies can be conducted with larger patient groups performing more detailed examinations. Another limitation is that blood samples were collected from the patients for IL-17 only during the diagnosis. In myocarditis cases, the prognostic relation between the course of the disease and IL-17A can be determined by making serial measurements related to IL-17A in early and late periods of the disease.
Conclusion
This study was planned to determine the IL-9 and IL-17 levels in myocarditis patients with different etiologies. In our study, we find that IL-17 levels were statistically significantly higher in all patients with myocarditis. So we suggested that IL-17 may be involved in pathogenesis of myocarditis and its inhibitory secukinumab may be used in diseasing involving the myocardium. This study may be a beginning of this idea.
Acknowledgments
This work was supported by grants from the Kahramanmaras Sutcu Imam University Scientific research project management unit (project number: 2017/5-11D).
Conflict of interest: There is no conflict of interest between the authors.
References
1. Magnani JW, Dec GW. Myocarditis: current trends in diagnosis and treatment. Circulation 2006;113:876–90.10.1161/CIRCULATIONAHA.105.584532Search in Google Scholar
2. McCarthy RE 3rd, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Hare JM, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med 2000;342:690–5.10.1056/NEJM200003093421003Search in Google Scholar
3. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and longterm management of Kawasaki disease: a statement for health professionals from the committee on rheumatic fever, endocarditis, and Kawasaki disease, council on cardiovascular disease in the young. American Heart Association. Circulation 2004;110:2747–71.10.1161/01.CIR.0000145143.19711.78Search in Google Scholar
4. Mirkinson L. The diagnosis of rheumatic fever. Pediatr Rev 1998;19:310–1.10.1542/pir.19.9.310Search in Google Scholar
5. Amigo MC, Martínez-Lavín M, Reyes PA. Acute rheumatic fever. Rheum Dis Clin North Am 1993;19:333–50.10.1016/S0889-857X(21)00190-3Search in Google Scholar
6. Xavier JL Jr, Matos Soeiro Ad, Lopes AS, Spina GS, Serrano CV Jr, Oliveira MT Jr. Clinically manifested myocarditis in acute rheumatic fever. Arq Bras Cardiol 2014;102:e17–20.10.5935/abc.20140017Search in Google Scholar PubMed PubMed Central
7. Wessely R, Henke A, Zell R, Kandolf R, Knowlton KU. Low-level expression of a mutant coxsackieviral cDNA induces a myocytopathic effect in culture: an approach to the study of enteroviral persistence in cardiac myocytes. Circulation 1998;98:450–7.10.1161/01.CIR.98.5.450Search in Google Scholar PubMed
8. Rowley AH, Shulman ST. New developments in the search for the etiologic agent of Kawasaki disease. Curr Opin Pediatr 2007;19:71–4.10.1097/MOP.0b013e328012720fSearch in Google Scholar PubMed
9. Blank M, Aron-Maor A, Shoenfeld Y. From rheumatic fever to Libman-Sacks endocarditis: is there any possible pathogenetic link? Lupus 2005;14:697–701.10.1191/0961203305lu2203oaSearch in Google Scholar PubMed
10. Toor D, Sharma N. T cell subsets: an integral component in pathogenesis of rheumatic heart disease. Immunol Res 2018;66:18–30.10.1007/s12026-017-8978-zSearch in Google Scholar PubMed
11. Korn T, Betteli E, Oukka M, Kuchroo VK. IL-17 and Th17 cells. Annu Rev Immunol 2009;27:485–517.10.1146/annurev.immunol.021908.132710Search in Google Scholar PubMed
12. Renauld JC, Kermouni A, Vink A, Louahed J, Van Snick J. Interleukin-9 and its receptor: involvement in mast cell differentiation and T cell oncogenesis. J Leukocyte Biol 1995;57:353–360.10.1002/jlb.57.3.353Search in Google Scholar PubMed
13. Knowlton KU, Badorff C. The immune system in viral myocarditis: maintaining the balance. Circ Res 1999;85: 559–61.10.1161/01.RES.85.6.559Search in Google Scholar PubMed
14. Temann UA, Geba GP, Rankin JA, Flavell RA. Expression of interleukin 9 in the lungs of transgenic mice causes airway inflammation, mast cell hyperplasia, and bronchial hyperresponsiveness. J Exp Med 1998;188:1307–20.10.1084/jem.188.7.1307Search in Google Scholar PubMed PubMed Central
15. Louahed J, Toda M, Jen J, Hamid Q, Renauld JC, Levitt RC, et al. Interleukin-9 upregulates mucus expression in the airways. Am J Respir Cell Mol Biol 2000;22:649–56.10.1165/ajrcmb.22.6.3927Search in Google Scholar PubMed
16. Kirkham BW, Lassere MN, Edmonds JP, Juhasz KM, Bird PA, Lee CS, et al. Synovial membrane cytokine expression is predictive of joint damage progression in rheumatoid arthritis: a two-year prospective study (the DAMAGE study cohort). Arthritis Rheum 2006;54:1122–31.10.1002/art.21749Search in Google Scholar PubMed
17. Hashmi S, Zeng QT. Role of interleukin-17 and interleukin-17-induced cytokines interleukin-6 and interleukin-8 in unstable coronary artery disease. Coron Artery Dis 2006;17:699–706.10.1097/01.mca.0000236288.94553.b4Search in Google Scholar PubMed
18. Liuzzo G, Trotta F, Pedicino D. Interleukin17 in atherosclerosis and cardiovascular disease: the good, the bad, and the unknown. Eur Heart J 2013;34:556–9.10.1093/eurheartj/ehs399Search in Google Scholar PubMed
19. Madhur MS, Funt SA, Li L, Vinh A, Chen W, Lob HE, et al. Role of interleukin 17 in inflammation, atherosclerosis, and vascular function in apolipoprotein e-deficient mice. Arterioscler Thromb Vasc Biol 2011;31:1565–72.10.1161/ATVBAHA.111.227629Search in Google Scholar PubMed PubMed Central
20. Zhang S, Yuan J, Yu M, Fan H, Guo ZQ, Yang R, et al. IL-17A facilitates platelet function through the ERK2 signaling pathway in patients with acute coronary syndrome. PLoS One 2012;7:e40641.10.1371/journal.pone.0040641Search in Google Scholar PubMed PubMed Central
21. Fala L. Cosentyx (Secukinumab): first IL-17A antagonist receives FDA approval for moderate-to-severe plaque psoriasis. Am Health Drug Benefits 2016;9:60–3.Search in Google Scholar
22. Matusevicius D, Kivisäkk P, He B, Kostulas N, Ozenci V, Fredrikson S, et al. Interleukin-17 mRNA expression in blood and CSF mononuclear cells is augmented in multiple sclerosis. Mult Scler 1999;5:101–4.10.1177/135245859900500206Search in Google Scholar PubMed
23. Duerr RH, Taylor KD, Brant SR, Rioux JD, Silverberg MS, Daly MJ, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science 2006;314:1461–3.10.1126/science.1135245Search in Google Scholar PubMed PubMed Central
24. Molet S, Hamid Q, Davoine F, Nutku E, Taha R, Pagé N, et al. IL-17 is increased in asthmatic airways and induces human bronchial fibroblasts to produce cytokines. J Allergy Clin Immunol 2001;108:430–8.10.1067/mai.2001.117929Search in Google Scholar PubMed
25. Lock C, Hermans G, Pedotti R, Brendolan A, Schadt E, Garren H, et al. Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat Med 2002;8:500–8.10.1038/nm0502-500Search in Google Scholar PubMed
26. Radstake TR, van Bon L, Broen J, Hussiani A, Hesselstrand R, Wuttge DM, et al. The pronounced Th17 profile in systemic sclerosis (SSc) together with intracellular expression of TGFbeta and IFNgamma distinguishes SSc phenotypes. PLoS One 2009;4:e5903.10.1371/journal.pone.0005903Search in Google Scholar PubMed PubMed Central
©2019 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Review Article
- Mitochondrial dysfunction and energy deprivation in the mechanism of neurodegeneration
- Research Articles
- Cancer diagnosis via fiber optic reflectance spectroscopy system: a meta-analysis study
- Development of molecularly imprinted Acrylamide-Acrylamido phenylboronic acid copolymer microbeads for selective glycosaminoglycan separation in children urine
- Assessment of LXRα agonist activity and selective antiproliferative efficacy: a study on different parts of Digitalis species
- Computational assessment of SKA1 as a potential cancer biomarker
- In vitro apoptotic effect of Zinc(II) complex with N-donor heterocyclic ligand on breast cancer cells
- A single-tube multiplex qPCR assay for mitochondrial DNA (mtDNA) copy number assessment
- A case–control study on effects of the ATM, RAD51 and TP73 genetic variants on colorectal cancer risk
- Effects of α-lactalbumin and sulindac on primary and metastatic human colon cancer cell lines
- The role of interleukin-9 and interleukin-17 in myocarditis with different etiologies
- Gene silencing of Col1α1 by RNAi in rat myocardium fibroblasts
- A method for high-purity isolation of neutrophil granulocytes for functional cell migration assays
- Role of SNPs of CPTIA and CROT genes in the carnitine-shuttle in coronary artery disease: a case-control study
- Interleukin-6 signaling pathway involved in major depressive disorder: selective serotonin reuptake inhibitor regulates IL-6 pathway
- Simultaneous comparison of L-NAME and melatonin effects on RAW 264.7 cell line’s iNOS production and activity
- Data-mining approach for screening of rare genetic elements associated with predisposition of prostate cancer in South-Asian populations
Articles in the same Issue
- Frontmatter
- Review Article
- Mitochondrial dysfunction and energy deprivation in the mechanism of neurodegeneration
- Research Articles
- Cancer diagnosis via fiber optic reflectance spectroscopy system: a meta-analysis study
- Development of molecularly imprinted Acrylamide-Acrylamido phenylboronic acid copolymer microbeads for selective glycosaminoglycan separation in children urine
- Assessment of LXRα agonist activity and selective antiproliferative efficacy: a study on different parts of Digitalis species
- Computational assessment of SKA1 as a potential cancer biomarker
- In vitro apoptotic effect of Zinc(II) complex with N-donor heterocyclic ligand on breast cancer cells
- A single-tube multiplex qPCR assay for mitochondrial DNA (mtDNA) copy number assessment
- A case–control study on effects of the ATM, RAD51 and TP73 genetic variants on colorectal cancer risk
- Effects of α-lactalbumin and sulindac on primary and metastatic human colon cancer cell lines
- The role of interleukin-9 and interleukin-17 in myocarditis with different etiologies
- Gene silencing of Col1α1 by RNAi in rat myocardium fibroblasts
- A method for high-purity isolation of neutrophil granulocytes for functional cell migration assays
- Role of SNPs of CPTIA and CROT genes in the carnitine-shuttle in coronary artery disease: a case-control study
- Interleukin-6 signaling pathway involved in major depressive disorder: selective serotonin reuptake inhibitor regulates IL-6 pathway
- Simultaneous comparison of L-NAME and melatonin effects on RAW 264.7 cell line’s iNOS production and activity
- Data-mining approach for screening of rare genetic elements associated with predisposition of prostate cancer in South-Asian populations

