Abstract
Background and aims
Health-related quality of life (HRQoL) assessments have been widely used in pain medicine as they are able to reflect the subjective and multidimensional nature of chronic pain. Studies have shown a consistent impairment in HRQoL in different chronic pain conditions. However, it is not known whether HRQoL is impaired in chronic orofacial pain (OFP). The generic 15D HRQoL instrument has been shown to fare as well as or better than other generic HRQoL instruments in the study of chronic pain. The aim was to investigate HRQoL in patients with chronic OFP using the generic 15D HRQoL instrument. The validity of the instrument was tested by studying the association of the 15D data with pain interference.
Methods
One hundred fifty-one patients (mean age 50 years, SD 15 years, 119 females) were recruited from three tertiary facial pain clinics. HRQoL data of the participants were contrasted with that of an age- and gender- standardized sample of general population by comparing the mean 15D scores and profiles. The data for the general population came from the National Health 2011 Survey representing Finnish population aged 18 years and older. Pain interference was assessed using Brief Pain Inventory. Based on pain interference distribution the participants were divided into tertiles. Statistical comparison between patient and population HRQoL values were performed using Monte-Carlo-type simulations. Statistical significance for the hypothesis of linearity was evaluated by using generalized linear models.
Results
The mean 15D score of OFP patients (0.824, SD 0.113) was statistically significantly lower than that of the age- and gender-standardized general population (0.929, SD 0.019) (p < 0.001). The difference between the patients and the general population was also clinically important, i.e. over the minimum clinically important difference in the 15D score. All mean 15D dimension values were significantly lower compared with the general population values (p < 0.001 for all dimensions). The largest differences were seen in the dimensions of discomfort and symptoms (0.418, SD 0.222 vs. 0.816, SD 0.027), sleeping (0.693, SD 0.258 vs. 0.838, SD 0.029), and vitality (0.702, SD 0.221 vs. 0.884 SD 0.026). There was a statistically significant linear decrease in the 15D dimension values (p < 0.001) with increasing pain interference. The greatest differences were found on the dimensions of discomfort and symptoms, sleeping and vitality.
Conclusions
HRQoL is significantly impaired in patients with chronic OFP. A decrease in the 15D dimension values with increasing pain interference indicated convergent validity between 15D and pain interference.
Implications
The findings suggest that 15D is an appropriate instrument for use in the assessment of HRQoL in OFP patients. By showing the usefulness of the 15D, the present study may encourage further use of generic HRQoL assessments in the study of chronic OFP, and contribute e.g. to the implementation of HRQoL as one of the core outcome measures in future treatment studies on chronic OFP.
1 Introduction
Orofacial pain (OFP) can be a symptom of various disorders. The most common chronic OFP conditions are temporomandibular disorders (TMD), burning mouth syndrome (BMS), neuropathic facial pain, and persistent idiopathic facial pain [1]. The prevalence of chronic OFP is in the range of 8–15% [2]. It has considerable economic impact through lost workdays and direct health care costs [2], [3].
Assessment of health-related quality of life (HRQoL) provides information on the subjective effects of chronic health conditions on the lives of those affected [4]. The generic HRQoL instruments describe the patient’s comprehensive health with a single index that reflects the health state in relation to full health and death. Generic HRQoL assessments are increasingly used as patient-reported treatment outcome measures as they provide important information on the beneficial and adverse effects of treatments from the subject’s perspective. Preference-based HRQoL expand upon generic instruments by applying various methods to incorporate patient opinion concerning the value of a particular health state [5], and can be used to perform cost-utility analyses [6].
HRQoL assessments have been widely used in pain medicine, as these measures are able to reflect the subjective and multidimensional nature of chronic pain. The studies have shown a consistent impairment in HRQoL in different chronic pain conditions [5], [7], [8]. Whether this applies to chronic OFP conditions is not fully understood as the few studies on orofacial pain utilizing generic HRQoL measures have focused on individual orofacial pain conditions. In the only previous study on a chronic OFP patient population, Durham and colleagues [9] showed that the EQ-5D-5L, one of the most widely used generic HRQoL instruments, had convergent validity with a multidimensional pain measure in quantifying the impacts of chronic OFP. Comparisons of the HRQoL of chronic OFP patients with that of the general population or patients with other chronic health conditions have not been reported.
Until lately, none of the many HRQoL instruments had been validated in chronic pain [10]. We have recently shown that the 15D, a generic, preference-based HRQoL instrument with good reliability, validity and discriminative power [11], [12], [13], was more strongly associated with commonly-used measures of chronic pain severity than the EQ-5D-3L, indicating better validity. The 15D also showed better discriminatory power, especially, for patients with good health [14]. A previous study using the 15D in a large population of chronic pain patients indicated that the impact of pain (i.e. how much pain interfered with usual activities) was strongly associated with the 15D score [8].
In general, measuring interference of pain is considered to provide a global overview of daily function and psychosocial impact of a pain condition [15]. Pain interference is a widely used and thoroughly studied assessment method in chronic OFP: it has been shown that patients reporting most severe pain interference report highest levels of psychological distress [16], [17], [18], [19], and report their general health as poorer compared with those with lower disability [16], [18], [19], [20]. Based on the previous findings, it can be hypothesized that patients with chronic OFP have impaired HRQoL, and that the interference caused by the pain strongly associates with the HRQoL.
The aim of the present study was to assess, using the 15D instrument, the impact of chronic OFP on HRQoL by comparing the HRQoL of the patients with that of an age- and gender-standardized sample of the general population. Further, as the 15D has not earlier been used to study orofacial pain, we wanted to test its validity and discriminatory power by studying the association of the 15D data with pain interference.
2 Methods
2.1 Subjects
This cross-sectional, observational study is part of the multi-center study KROKIETA, Chronic Pain, Life Style Factors and Quality of Life, study in Finland. The study patients were recruited from facial pain clinics at three hospitals in Finland (Turku and Kuopio University Hospitals and Central-Finland Central Hospital) between November 2013 and November 2016. Consecutive patients aged 18–75 years referred to pain management in tertiary care because of chronic OFP were invited to participate in the study and were provided with written information about the study protocol (n=164). Headache patients were not included. Neither were patients with cancer-related pain nor patients unable to answer the study questionnaire independently. The Ethics Committee of the Helsinki University Hospital approved the study (decision no. 29/13/03/00/2012), and each hospital gave permission for the study.
Four patients refused to participate. Nine patients from the remaining sample of 160 patients did not return questionnaires or answered them incompletely. The final number of patients included in the study was 151 (119 females, mean age 50 years, SD 15 years). All participants gave written informed consent.
2.2 Measures
2.2.1 15D – the 15-dimensional health-related quality of life measure
The 15D is a generic, preference-based, self-administered standardized instrument for the measurement of HRQoL with proven reliability, validity, discriminatory power and responsiveness to change [11], [12], [13], [21], [22]. It consists of 15 questions describing various dimensions of health: mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. Each of the dimensions has five levels of severity from which the patient chooses the one best describing his or her situation at that moment. The 15D can be used both as a profile and a single index score measure. The single index 15D score, representing the overall HRQoL on a 0–1 scale (1=full health, 0=being dead), and the dimension level values, reflecting the goodness of the levels relative to “no problems” (=1) and to “being dead” (=0), are calculated from the health state descriptive system by using a set of population-based preference weights. These weights have been elicited from representative population samples by using magnitude estimation in a 3-stage valuation process based on the multi-attribute utility theory [12]. The scores thus reflect the population’s preferences of a certain health state over death and full health. The minimum important change (MIC) in the 15D score has been established to be 0.015 [23].
In the current study, the Finnish language version of the 15D was used. For the English language version, see Supplementary file.
2.2.2 The Brief Pain Inventory (BPI)
The Brief Pain Inventory [24] is a commonly used method to assess the intensity and interference of pain. Pain intensity during the last week is assessed by four questions (worst, least, average and right now) on a numerical rating scale (NRS) from 0 (no pain) to 10 (worst imaginable pain). Pain interference is assessed with seven questions about the interference of pain with different daily activities (general activity, walking, work, mood, enjoyment of life, relations with others and sleep), on NRS from 0 (no interference) to 10 (interferes completely). The intensity and interference scores are commonly presented on a scale from 0 to 10, obtained by calculating the mean of the sum total of the respective NRS scores.
2.2.3 The Pain Anxiety Severity Scale (PASS-20)
The 20-item version of the Pain Anxiety Severity Scale measures negative beliefs, avoidance behavior, fears and anxiety related to pain [25]. The measure is based on the fear-avoidance model of chronic pain. Participants rate the frequency of occurrence of each of the behaviors on a 6-point scale from 0 (never) to 5 (always).
2.2.4 The Beck Depression Inventory II (BDI II)
The BDI II is one of the most frequently used measures to investigate depressive symptoms [26]. It contains 21 questions, each answer scored on a scale from 0 to 3, where higher scores indicate more severe depressive symptoms.
2.2.5 The Basic Nordic Sleep Questionnaire
Sleep and sleep disturbances were assessed with the Basic Nordic Sleep Questionnaire (BNSQ) [27]. Five multiple-choice questions of BNSQ were chosen to be analyzed in this study. The questions concerned the severity of difficulty in falling asleep, waking up during the night, use of sleep medication, and tiredness in the evening and in the morning. The individual questions were scored from 0 to 4 to indicate increasing severity and the sum score of the five questions was used as a single index value.
2.2.6 Occurrence of pain in other areas
The study participants were asked to mark all sites where they had pain on a whole-body pain drawing. The drawings were analyzed and the information obtained was divided as follows: pain only in the head region (score=0) or pain in other body areas as well (score=1).
2.2.7 Duration of facial pain
The duration of pain was asked for and participants were divided into three groups: pain duration less than 1 year, from 1 to 2 years and more than 2 years.
2.2.8 Socioeconomic factors
Questions measuring socioeconomic background variables were based on FINRISK-survey, a Finnish national health survey [28]. For the present study, information on years of education, marital status, employment, smoking status, use of alcohol, and leisure time activities were extracted.
Information on working status was divided into three classes: still actively working, retired, unemployed. Information on marital status was divided into two classes: cohabiting with someone or living alone. Smoking habit was divided into current smoking and non-smoking. Use of alcohol was assessed using Alcohol Use Disorders Identification Test (AUDIT), a 10-question test with a 0 – 4 scale where larger numbers indicate more severe alcohol abuse behaviors.
Leisure time physical activity was inquired about as follows: “How often do you practice leisure time exercise for at least 20 min so that you feel slightly breathless and sweaty?” The information was divided into three classes: less than once a week (low activity), 1–3 times a week (moderate activity) and more than 3 times a week (high activity).
2.2.9 Study design
All the study participants were asked to fill in the above-mentioned questionnaires before or during their first visit to the facial pain clinic.
The HRQoL of the patients was contrasted with that of the general population by comparing their mean 15D scores and profiles with those of a representative sample of the general population. The data for the general population came from the National Health 2011 Survey representing Finnish population aged 18 years and older [29]. Because age and gender are important determinants of HRQoL, a subsample (n=1306) of individuals who were in the age range of the participants was chosen and weighted to reflect the age and gender distribution of the participants.
To study the association of HRQoL with pain interference, BPI/interference subscore was calculated by obtaining the mean of the seven individual NRS questions on pain interference. Based on pain interference distribution the participants were divided into tertiles: Class I BPI interference <2.5 (n=50), class II 2.5–5.6 (n=50) and class III 5.7–10 (n=51). Further, to examine the validity and discriminatory power of the interference division, the psychosocial characteristics of the participants in different interference tertiles were described and analyzed.
2.2.10 Statistical methods
Descriptive statistics include means and SDs for continuous variables and numbers and percentages for categorical (ordinal) variables. Statistical significances for the unadjusted hypothesis of linearity across tertiles of pain interference were calculated by using the Cochran-Armitage test for trend and analysis of variance (ANOVA) with an appropriate contrast (orthogonal polynomial). Adjusted hypotheses of linearity across tertiles of pain interference and the 15D dimensions were evaluated by using bootstrap-type (5,000 replications) analysis of covariance (ANCOVA). Models included age and years of education as covariates. Statistical comparisons between the participants’ and the age- and gender-standardized population sample’s 15D scores were done using Monte-Carlo-type simulations [30]. Correlations are expressed with Spearman’s correlation coefficients with bootstrapped 95% confidence intervals. The normality of the variables was evaluated graphically and using the Shapiro–Wilk W test. All statistical analyses were carried out with Stata, version 15.0 (StataCorp, College Station, TX, USA).
3 Results
The sociodemographic and pain-related psychosocial characteristics are presented in Table 1. Mapping of these characteristics in different pain interference tertiles displayed differences especially in the psychosocial characteristics of the patients. With increasing pain interference a statistically significant increase was noted in pain intensity, pain chronicity, presence of pain in other areas, depressive symptoms, anxiety and sleep disturbances, whereas a decrease was noted in leisure time physical activity (Table 1).
Sociodemographic and pain-related psychosocial characteristics of all participants and for participants divided into tertiles according to pain interference.
| All | Pain interference tertiles |
p-Valuea | |||
|---|---|---|---|---|---|
| I (<2.5) n=50 | II (2.5–5.6) n=50 | III (≥5.7) n=51 | |||
| Number of females (%) | 119 (79) | 37 (74) | 41 (82) | 41 (80) | 0.44 |
| Age, mean (SD) | 50 (15) | 48 (16) | 49 (15) | 52 (13) | 0.23 |
| Education years, mean (SD) | 13.7 (3.7) | 13.9 (4.0) | 13.8 (3.5) | 13.3 (3.7) | 0.45 |
| Working status, n (%) | 0.33 | ||||
| Working | 52 (34) | 16 (32) | 14 (28) | 22 (43) | |
| Unemployed | 83 (55) | 30 (60) | 31 (62) | 22 (43) | |
| Retired | 16 (11) | 4 (8) | 5 (10) | 7 (14) | |
| Cohabiting, n (%) | 104 (69) | 34 (68) | 38 (76) | 32 (73) | 0.56 |
| Smoking, n (%) | 25 (17) | 11 (22) | 8 (16) | 6 (12) | 0.17 |
| AUDIT, mean (SD) | 2.5 (2.7) | 2.1 (2.1) | 2.8 (2.9) | 2.7 (3.1) | 0.29 |
| Leisure time physical activity, n (%) | 0.016 | ||||
| Low | 46 (30) | 10 (20) | 15 (30) | 21 (41) | |
| Moderate | 67 (44) | 26 (52) | 18 (36) | 23 (45) | |
| High | 38 (25) | 14 (28) | 17 (34) | 7 (14) | |
| Sleep score, mean (SD) | 9.0 (4.5) | 6.4 (3.1) | 8.9 (3.7) | 11.8 (4.7) | <0.001 |
| BDI, mean (SD) | 9.7 (8.3) | 4.3 (4.3) | 9.6 (7.0) | 14.9 (9.3) | <0.001 |
| PASS, mean (SD) | 38 (19) | 26 (18) | 37 (16) | 49 (17) | <0.001 |
| Pain intensity, mean (SD) | 4.87 (1.97) | 3.10 (1.52)) | 5.06 (1.45) | 6.42 (1.29) | <0.001 |
| Pain in other areas, n (%) | 127 (84) | 39 (78) | 40 (80) | 48 (94) | 0.027 |
| Duration of pain, n (%) | 0.048 | ||||
| <1 year | 26 (17) | 11 (22) | 7 (14) | 8 (16) | |
| 1–2 years | 20 (13) | 10 (20) | 7 (14) | 3 (6) | |
| >2 years | 105 (70) | 29 (58) | 36 (72) | 40 (78) | |
-
a p for linearity across tertiles of pain interference.
The mean 15D score of OFP patients (0.824, SD 0.113) was significantly lower than that of the age- and gender-standardized sample of the general population (0.929, SD 0.019) (p<0.001). The difference between the patients and the general population was also clinically important, i.e. over the minimum clinically important difference in the 15D score of 0.015 [23].
All mean 15D dimension values were statistically significantly lower than those of the general population (p<0.001 for all dimensions) (Fig. 1). The largest differences were seen on the dimensions of discomfort and symptoms (0.418, SD 0.222 vs. 0.816, SD 0.027), sleeping (0.693, SD 0.258 vs. 0.838, SD 0.029), and vitality (0.702, SD 0.221 vs. 0.884 (SD 0.026).

The mean (95% CI) values of different dimensions of the 15D and the 15D score. The dashed line shows the mean scores in the general Finnish population weighted to match the gender and age distribution of the study population.
There was a statistically significant linear decrease in the 15D score (p<0.001) and for all dimension values, except for two (vision and eating), with increasing pain interference. The greatest differences were found on the dimensions of discomfort and symptoms, sleeping and vitality (Table 2, Fig. 2).
The values (mean, SD) of 15D dimensions according to pain interference tertiles in patients with chronic orofacial pain.
| Pain interference tertiles |
p-Valuea | |||
|---|---|---|---|---|
| I (<2.5) | II (2.5-5.6) | III (≥5.7) | ||
| Mobility | 0.977 (0.079) | 0.899 (0.156) | 0.870 (0.183) | <0.001 |
| Vision | 0.945 (0.159) | 0.956 (0.120) | 0.880 (0.198) | 0.16 |
| Hearing | 0.969 (0.100) | 0.949 (0.116) | 0.869 (0.168) | <0.001 |
| Breathing | 0.929 (0.138) | 0.926 (0.156) | 0.803 (0.223) | 0.001 |
| Sleeping | 0.782 (0.240) | 0.751 (0.204) | 0.550 (0.265) | <0.001 |
| Eating | 0.986 (0.070) | 0.958 (0.116) | 0.951 (0.123) | 0.078 |
| Speech | 0.964 (0.097) | 0.964 (0.097) | 0.901(0.173) | 0.035 |
| Excretion | 0.887 (0.174) | 0.862 (0.179) | 0.739 (0.240) | <0.001 |
| Usual activities | 0.932 (0.135) | 0.811 (0.216) | 0.659 (0.276) | <0.001 |
| Mental function | 0.943 (0.132) | 0.859 (0.186) | 0.750 (0.233) | <0.001 |
| Discomfort and symptoms | 0.576 (0.223) | 0.391 (0.181) | 0.291 (0.157) | <0.001 |
| Depression | 0.953 (0.107) | 0.860 (0.170) | 0.776 (0.199) | <0.001 |
| Distress | 0.886 (0.163) | 0.804 (0.206) | 0.782 (0.236) | 0.001 |
| Vitality | 0.846 (0.156) | 0.702 (0.170) | 0.563 (0.232) | <0.001 |
| Sexual activity | 0.931 (0.137) | 0.813 (0.229) | 0.635 (0.98) | <0.001 |
| 15D score | 0.901 (0.062) | 0.835 (0.086) | 0.738 (0.117) | <0.001 |
-
a p for linearity adjusted for gender, age, education and duration of pain.

The figure depicts the differences in the mean 15D dimension values and the 15D score between patients with orofacial pain and the Finnish general population, divided according to pain interference tertiles. Error bars show 95% confidence intervals.
Correlation was noted between the 15D score and BPI/interference (Fig. 3).
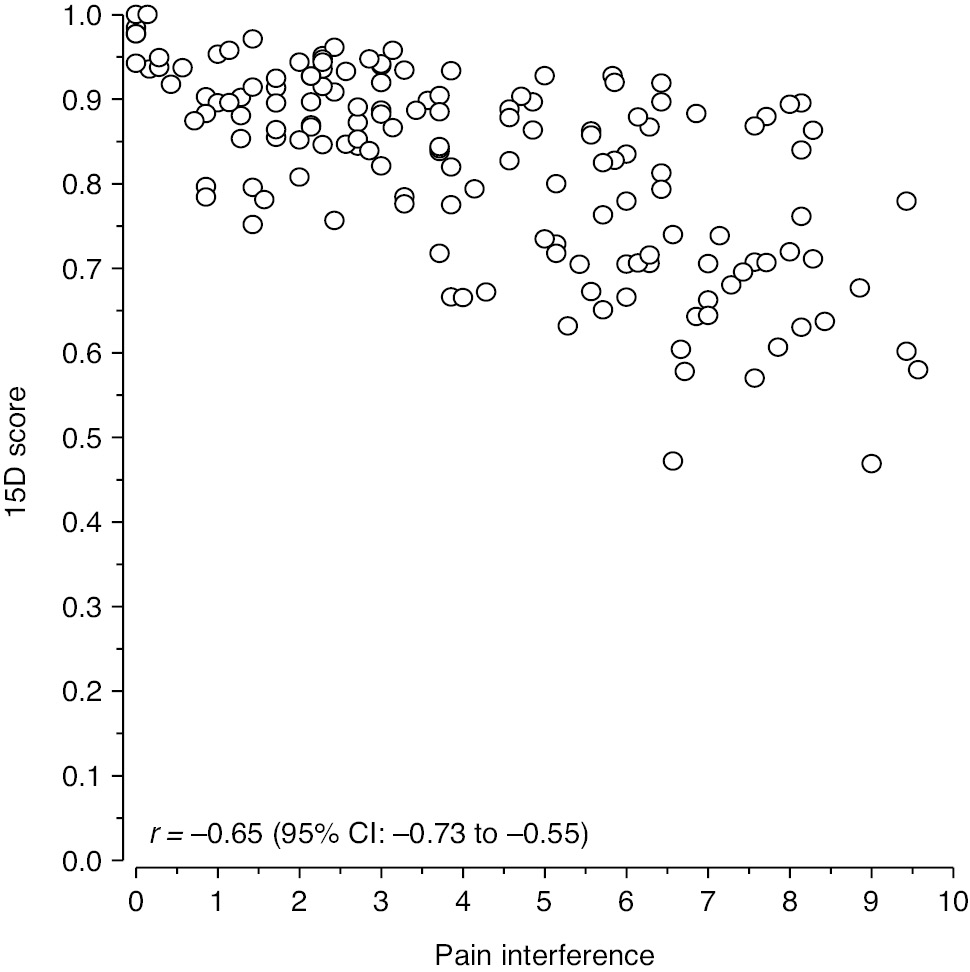
The individual participants’ 15D scores compared to the individual BPI/interference scores.
4 Discussion
4.1 Main findings
The results of the study indicate that chronic OFP substantially reduces the HRQoL of these patients. The self-reported HRQoL of OFP patients (0.824) was statistically significantly and clinically importantly lower than that of an age- and gender-standardized sample of the Finnish population (0.929). From the different dimensions of health described by the 15D, discomfort and symptoms, sleep and vitality were most affected. The results also indicated convergent validity between the results of the 15D and interference in daily functioning caused by the pain by showing a statistically significant linear decrease in the 15D dimension score values and in most individual dimension values with increasing pain interference, as well as an inverse correlation (r=−0.65) between the 15D score and pain interference. These findings suggest that 15D is an appropriate instrument for use in the assessment of HRQoL in OFP patients.
4.2 Comparison with other chronic conditions
The impact of major chronic health conditions on HRQoL was investigated in a population-based survey in Finland using the 15D [31]. Compared with the results of that study, the findings of the present study indicate that HRQoL of chronic OFP patients is poorer than that of patients suffering from many types of chronic health conditions such as cancer (0.855), depression (0.841), back (0.874) or neck (0.879) problems or osteoarthritis of the hip and knee (0.873), and comparable to that of patients with serious psychiatric conditions (0.829) or coronary heart disease (0.821). Looking at the results of 15D studies with similar study settings, the perceived burden of chronic OFP seems less than that of patients admitted to secondary care because of depression (0.729) [32], but similar to that of secondary care rheumatoid arthritis patients (0.822) [33]. That chronic OFP seems to impact HRQoL more than many serious somatic health conditions may reflect the comprehensive nature of suffering or distress often connected to chronic pain problems. Some of the lowest mean 15D scores (0.710 and 0.714) reported in outpatient populations were those found in recent studies on tertiary care chronic pain patients [8], [34]. The difference in the perceived burden between the tertiary care pain patients and the orofacial pain patients of the present study may be due to the more devastating effects of bodily pains on e.g. mobility and usual activities, compared with those caused by orofacial pain conditions. Having musculoskeletal pain only in the craniomandibular region impairs HRQoL less than more widespread musculoskeletal pain [35]. Similarly, the impact of trigeminal neuropathic pain on HRQoL is less than that of conditions involving bodily neuropathic pains [36].
With one exception [9], earlier studies on HRQoL have focused on different, specific orofacial pain conditions. Further, they have utilized instruments other than the 15D, the SF-36 [20], [37], [38], [39] or EQ-5D [36], [40], [41]. As different HRQoL instruments measure different constructs they can produce variable results in the same patient populations [13], [42]. Thus, direct comparisons of the present results and those of earlier studies are not feasible. However, all studies have shown that chronic orofacial pain conditions impact negatively HRQoL [9], [35], [36], [37], [38], [39], [40], [41].
4.3 HRQoL and pain interference
Statistically significant and clinically important decreases in the mean 15D score and marked, statistically significant decreases in most dimension values were noted with increasing pain interference. In particular, the dimensions discomfort and symptoms, sleeping and vitality deteriorated with increasing pain interference. These are the same dimensions on which OPF patients differed most from the general population. An impairment of most of those 15D dimensions, which are associated with psychosocial aspects of health, has also been noted in another chronic pain population in tertiary care [8].
Patients in the lowest interference tertile, i.e. those reporting low pain-related interference, judged their HRQoL to be as good as that of the general population sample with the exception of the dimension of discomfort and symptoms where the participants had lower values. However, patients in the highest interference tertile reported impaired HRQoL with marked deterioration on almost all 15D dimensions. An association of pain interference and HRQoL, which has also been noted in other studies on chronic pain populations [8], [14] as well as in chronic orofacial pain [41], is logical as both of these measures comprehensively assess the impact of pain. Their concomitant use can, however, be an advantage given the fluctuating manner of orofacial pains, as the reference period of the BPI/interference measure and of the 15D are different (the last week vs. current). Further, IMMPACT [43] and VAPAIN [44] recommendations for core outcome domains and measures in chronic pain trials state that several outcomes should be used, including both pain interference and HRQoL measures.
As in previous studies on chronic OFP patients [16], [17], [18], [19], significant increases in pain intensity, pain duration, presence of pain in other areas, depressive symptoms, anxiety and sleep disturbances, were noted with increasing pain interference in the present study, with a decrease in leisure time physical activity. These results support the validity and discriminative power of the interference division (tertiles) used in the present study.
4.4 Strengths and limitations
The present study is the first to compare the HRQoL of chronic orofacial pain patients with that of an age- and gender-standardized sample of the general population. The use of the generic and preference-based 15D instrument also makes the comparison of the impact of orofacial pain with that of other chronic pains or other chronic health conditions possible. The 15D instrument used in the present study has been shown to fare as well as or better than other preference-based HRQoL instruments [13], [14], [22], [42]. In addition to the single index score measure, the 15D can be used as a profile, which describes the 15 dimensions of health. An analysis of the impaired dimensions gives insight into which aspects of health are affected by a given condition and consequently relevant targets for treatment intervention. Further, with the established MIC value, the 15D is a suitable measure for intervention studies. By showing the usefulness of the 15D in the assessment of chronic OFP, the present study may contribute to the implementation of HRQoL assessment as one of the core outcome measures in future treatment studies on chronic OFP as advised by the IMMPACT recommendations [43].
Limitations of the present study are that the participants were tertiary care facial pain patients, i.e. a selected group of challenging pain patients, and thus the results may not be applicable to all chronic OFP patients. Moreover, the participants were a heterogenous group of OFP patients, not patients with specific orofacial pain diagnoses, which may impact the HRQoL differently. Furthermore, a generic HRQoL instrument was used, which has a possible disadvantage of being less sensitive than condition-specific instruments, as it may not capture all the relevant aspects of the disease. Thus the concomitant use of generic and condition-specific instruments in HRQoL studies is recommended, albeit especially in studies focusing on responsiveness to treatment or disease progression, as these measures are able to assess in greater detail the impact of chronic pain condition on HRQoL [5]. However, to our knowledge, no validated condition-specific instruments exist for chronic orofacial pain conditions.
5 Conclusions
The HRQoL is significantly impaired in patients with chronic orofacial pain. By showing a linear decline in HRQoL with increasing pain-related interference, the results suggest that the 15D is an appropriate instrument for use in the assessment of HRQoL in orofacial pain patients.
Acknowledgements
The authors thank Maarit Pippola for her assistance during the writing process and Les Hearn for proofreading the manuscript.
-
Authors’ statements
-
Research funding: The KROKIETA research project has received financial support from the Finnish Association for the Study of Pain and from Governmental research funding to the Helsinki University Hospital (TYH2014214).
-
Conflict of interest: Harri Sintonen is the developer of the 15D, and reports royalties for the electronic versions of the 15D, outside the submitted work. Eija Kalso reports having received honoraria for advisory board membership from Orion Pharma, Gruenenthal and Laboratoires Pierre Fabre. The other authors report no conflicts of interest that may have affected the work.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Ethical approval: The research complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration. The Ethics Committee of the Helsinki University Hospital approved the study, and each hospital gave permission for the study.
References
[1] Macfarlane TV, Glenny A-M, Worthington HV. Systematic review of population based epidemiological studies on oro-facial pain. J Dent 2001;29:451–67.10.1016/S0300-5712(01)00041-0Search in Google Scholar
[2] Sessle BJ. The societal, political, educational, scientific, and clinical context of orofacial pain. In: Sessle BJ, editor. Orofacial pain: recent advances in assessment, management, and understanding of mechanisms. Washington, DC: IASP Press, 2014:1–15.Search in Google Scholar
[3] Durham J, Shen J, Breckons M, Steele JG, Araujo-Soares V, Exley C, Vale L. Healthcare cost and impact of persistent orofacial pain: the DEEP study cohort. J Dent Res 2016;95:1147–54.10.1177/0022034516648088Search in Google Scholar PubMed
[4] Guyatt GH, Freeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med 1993;118:622–9.10.7326/0003-4819-118-8-199304150-00009Search in Google Scholar PubMed
[5] Vetter TR. A primer on health-related quality of life in chronic pain medicine. Anesth Analg 2007;104:703–18.10.1213/01.ane.0000255290.64837.61Search in Google Scholar PubMed
[6] Bansback N, Harrison M, Brazier J, Davies L, Kopec J, Marra C, Symmons D, Anis A. Health state utility values: a description of their development and application for rheumatic diseases. Arthritis Rheum 2008;59:1018–26.10.1002/art.23813Search in Google Scholar PubMed
[7] Loyland B, Miaskowski C, Paul SM, Dahl E, Rustoen T. The relationship between chronic pain and health-related quality of life in long-term social assistance recipients in Norway. Qual Life Res 2010;19:1457–65.10.1007/s11136-010-9707-4Search in Google Scholar PubMed PubMed Central
[8] Vartiainen P, Heiskanen T, Sintonen H, Roine RP, Kalso E. Health-related quality of life and burden of disease in chronic pain measured with the 15D instrument. Pain 2016;157:2269–76.10.1097/j.pain.0000000000000641Search in Google Scholar PubMed
[9] Durham J, Steele JG, Breckons M, Story W, Vale L. DEEP Study: does EQ-5D-5L measure the impacts of persistent oro-facial pain? J Oral Rehabil 2015;42:643–50.10.1111/joor.12296Search in Google Scholar PubMed PubMed Central
[10] Schofield DJ. How should we measure the impact of chronic pain? Limitations of utility measurement using the EQ-5D and SF-6D. Pain 2014;155:1918–9.10.1016/j.pain.2014.07.020Search in Google Scholar PubMed
[11] Sintonen H. The 15D-measure of health-related quality of life. I. Relability, validity and sensitivity of its health state descriptive system. National Centre for Health Program Evaluation. Working Paper 41. Melbourne1994.Search in Google Scholar
[12] Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med 2001;33:328–36.10.3109/07853890109002086Search in Google Scholar PubMed
[13] Hawthorne G, Richardson J, Day NA. A comparison of the assesment of quality of life (AQoL) with four other generic utility instruments. Ann Med 2001;33:358–70.10.3109/07853890109002090Search in Google Scholar PubMed
[14] Vartiainen P, Mäntyselkä P, Heiskanen T, Hagelberg N, Mustola S, Forssell H, Kautiainen H, Kalso E. Validation of EQ-5D and 15D in the assessment of health-related quality of life in chronic pain. Pain 2017;158:1577–85.10.1097/j.pain.0000000000000954Search in Google Scholar PubMed
[15] Ohrbach R, Durham J, Fillingim R. Self-report assessment of orofacial pain and psychosocial status. In Sessle BJ, editor. Orofacial pain: recent advances in assessment, management, and understanding of mechanisms. Washington, DC: IASP Press, 2014:121–41.Search in Google Scholar
[16] Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain 1992;50:133–49.10.1016/0304-3959(92)90154-4Search in Google Scholar PubMed
[17] Manfredini D, Borella L, Favero L, Ferronato G, Guarda-Nardini L. Chronic pain severity and depression/somatization levels in TMD patients. Int J Prosthodont 2010;23:529–34.Search in Google Scholar
[18] Suvinen TI, Kemppainen P, Le Bell Y, Valjakka A, Vahlberg T, Forssell H. Research diagnostic criteria Axis II in screening and as a part of biopsychosocial subtyping of Finnish patients with tempromandibular disorder pain. J Orofac Pain 2013;27:314–24.10.11607/jop.1145Search in Google Scholar PubMed
[19] Kotiranta U, Suvinen T, Kauko T, Le Bell Y, Kemppainen P, Suni J, Forssell H. Subtyping patients with temporomandibular disorders in a primary health care setting on the basis of the research diagnostic criteria for temporomandibular disorders Axis II pain-related disability: a step toward tailored treatment planning? J Oral Facial Pain Headache 2015;29:126–34.10.11607/ofph.1319Search in Google Scholar PubMed
[20] Kotiranta U, Forssell H, Kauppila T. Painful Temporomandibular Disorders (TMD) and comorbidities in primary care: associations with pain-related disability. Acta Odontol Scand 2019;77:22–7.10.1080/00016357.2018.1493219Search in Google Scholar PubMed
[21] Moock J, Kohlmann T. Comparing preference-based quality-of-life measures: results from rehabilitation patients with musculoskeltal, cardiovascular or psychosomatic disorders. Qual Life Res 2008;17:485–95.10.1007/s11136-008-9317-6Search in Google Scholar PubMed
[22] Richardson J, Iezzi A, Khan MA, Chen G, Maxwell A. Measuring the sensitivity and construct validity of 6 utility instruments in 7 disease areas. Med Decis Making 2016;36:147–59.10.1177/0272989X15613522Search in Google Scholar PubMed
[23] Alanne S, Roine RP, Räsänen P, Vainiola T, Sintonen H. Estimating the minimum important change in the 15D scores. Qual Life Res 2015;24:599–606.10.1007/s11136-014-0787-4Search in Google Scholar PubMed
[24] Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 2004;5:133–37.10.1016/j.jpain.2003.12.005Search in Google Scholar PubMed
[25] McCracken LM. Pain Anxiety Symptom Scale (PASS) and Short Version PASS-20. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York, NY: Springer, New York, 2013:1423–4. Available at: http://dx.doi.org/10.1007/978-1-4419-1005-9_907.10.1007/978-1-4419-1005-9_907Search in Google Scholar
[26] Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories –IA and –II in Psychiatric Outpatients. J Pers Assess 1996;67:588–97.10.1207/s15327752jpa6703_13Search in Google Scholar PubMed
[27] Partinen M, Gislason T. Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res 1995;4:150–5.10.1111/j.1365-2869.1995.tb00205.xSearch in Google Scholar PubMed
[28] Borodulin K, Vartiainen E, Peltonen M, Jousilahti P, Juolevi A, Laatikainen T, Mannisto S, Salomaa V, Sundvall J, Puska P. Forty-year trends in cardiovascular risk factors in Finland. Eur J Public Health 2015;25:539–46.10.1093/eurpub/cku174Search in Google Scholar PubMed
[29] Koskinen S, Lundqvist A, Ristiluoma N, editors. Health, functional capacity and welfare in Finland in 2011. National Institute for Health and Welfare (THL), Report 68/2012. Helsinki 2012. Available at: http://urn.fi/URN:ISBN:978-952-245-769-1.Search in Google Scholar
[30] Phillip I. Good resampling methods: a practical guide to data analysis, Second ed. New York: Springer Science & Business Media, 2001.Search in Google Scholar
[31] Saarni SI, Härkänen T, Sintonen H, Suvisaari J, Koskinen S, Aromaa A, Lönnqvist J. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual Life Res 2006;15:1403–14.10.1007/s11136-006-0020-1Search in Google Scholar PubMed
[32] Suominen K, Karlsson H, Rissanen A, Valtonen HM, Räsänen P, Sintonen H, Roine RP. Perceived burden of illness in patients entering for treatment in a university hospital – is the threshold to secondary care higher for patients with depression than for those with somatic disorders? Eur Psychol 2011;26:441–5.10.1016/j.eurpsy.2010.09.008Search in Google Scholar PubMed
[33] Laas K, Roine R, Räsänen P, Sintonen H, Leirisalo-Repo M. HUS QoL Study Group. Health-related quality of life in patients with common rheumatic diseases referred to a university clinic. Rheumatol Int 2009;29:267–73.10.1007/s00296-008-0673-xSearch in Google Scholar PubMed
[34] Heiskanen T, Roine RP, Kalso E. Multidisciplinary pain treatment – Which patients do benefit? Scand J Pain 2012;3:201–7.10.1016/j.sjpain.2012.05.073Search in Google Scholar PubMed
[35] Lobbezoo F, Vissher CM, Naeije M. Impaired health status, sleep disorders, and pain in the craniomandibular and cervical spinal regions. Eur J Pain 2004;8:23–30.10.1016/S1090-3801(03)00061-2Search in Google Scholar PubMed
[36] Smith JG, Elias LA, Yilmaz Z, Barker S, Shah K, Renton T. The psychosocial and affective burden of posttraumatic neuropathy following injuries to the trigeminal nerve. J Orofac Pain 2013;27:293–303.10.11607/jop.1056Search in Google Scholar PubMed
[37] Tjakkes GH, Reinders JJ, Tenvergert EM, Stegenga B. TMD pain: the effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes 2010;8:46.10.1186/1477-7525-8-46Search in Google Scholar PubMed PubMed Central
[38] Lopez-Jornet P, Camacho-Alonso F, Lucero-Berdugo M. Quality of life in patients with burning mouth syndrome. J Oral Pathol Med 2008;37:389–94.10.1111/j.1600-0714.2008.00672.xSearch in Google Scholar PubMed
[39] Souza FTA, Santos TPM, Bernardes VF, Teixeira AL, Kummer AM, Silva TA, Abreu MHNG. The impact of burning mouth syndrome on health-related quality of life. Health Qual Life Outcomes 2011;9:57.10.1186/1477-7525-9-57Search in Google Scholar PubMed PubMed Central
[40] Kim T-Y, Shin J-S, Lee J, Lee YJ, Kim M, Ahn Y Park KB, Hwang D-S, Ha I-H. Gender difference in associations between chronic temporomandibular disorders and general quality of life in koreans: a cross-sectional study. PLoS One 2015;10:e0145002.10.1371/journal.pone.0145002Search in Google Scholar PubMed PubMed Central
[41] Tolle T, Dukes E, Sadosky A. Patient burden of trigeminal neuralgia: results from a cross-sectional survey of health state impairment and treatment patterns in six European countries. Pain Pract 2006;6:153–60.10.1111/j.1533-2500.2006.00079.xSearch in Google Scholar PubMed
[42] Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004;13:873–84.10.1002/hec.866Search in Google Scholar PubMed
[43] Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19.10.1016/j.pain.2004.09.012Search in Google Scholar PubMed
[44] Kaiser U, Kopkow C, Deckert S, Neustadt K, Jacobi L, Cameron P, De Angelis V, Apfelbacher C, Arnold B, Birch J, Bjarnegård A, Christiansen S, C de Williams A, Gossrau G, Heinks A, Huppe M, Kiers H, Kleinert U, Martelletti P, McCracken L, et al. Developing a core outcome domain set to assessing effectiveness of interdisciplinary multimodal pain therapy: the VAPAIN consensus statement on core outcome domains. Pain 2018;159:673–83.10.1097/j.pain.0000000000001129Search in Google Scholar PubMed
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/sjpain-2019-0131).
Article note
Previous presentation of the data: Part of the study data has been presented as abstract in EFIC 2017 congress in Copenhagen.
A previous methodological study by our group on the validity of the 15D and another HRQoL instrument, the EQ-5D, in chronic pain (Vartiainen P, Mäntyselkä P, Heiskanen T, Hagelberg N, Mustola S, Forssell H, Kautiainen H, Kalso E. Validation of EQ-5D and 15D in the assessment of health-related quality of life in chronic pain. Pain 2017;158:1577–1585) used data from a large sample of patients with chronic pain (n 373), including a portion (130/151) of the present patients with orofacial pain. In the analysis of the associations of the two HRQoL measures, the data was handled in its entirety, not separating the results concerning patients with orofacial.
Trial register number: ClinicalTrials.gov. ID: NCT03028051
©2020 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved.
Articles in the same Issue
- Frontmatter
- Systematic review
- Are there differences in lifting technique between those with and without low back pain? A systematic review
- Topical reviews
- Pain psychology in the 21st century: lessons learned and moving forward
- Chronic abdominal pain and persistent opioid use after bariatric surgery
- Clinical pain research
- Spinal cord stimulation for the treatment of complex regional pain syndrome leads to improvement of quality of life, reduction of pain and psychological distress: a retrospective case series with 24 months follow up
- The feasibility of gym-based exercise therapy for patients with persistent neck pain
- Intervention with an educational video after a whiplash trauma – a randomised controlled clinical trial
- Reliability of the conditioned pain modulation paradigm across three anatomical sites
- Is rotator cuff related shoulder pain a multidimensional disorder? An exploratory study
- Are degenerative spondylolisthesis and further slippage postoperatively really issues in spinal stenosis surgery?
- Multiprofessional assessment of patients with chronic pain in primary healthcare
- The impact of chronic orofacial pain on health-related quality of life
- Pressure pain thresholds in children before and after surgery: a prospective study
- Observational studies
- An observational study on risk factors for prolonged opioid prescription after severe trauma
- Dizziness and localized pain are often concurrent in patients with balance or psychological disorders
- Pre-consultation biopsychosocial data from patients admitted for management at pain centers in Norway
- Original experimentals
- Local hyperalgesia, normal endogenous modulation with pain report beyond its origin: a pilot study prompting further exploration into plantar fasciopathy
- Pressure pain sensitivity in patients with traumatic first-time and recurrent anterior shoulder dislocation: a cross-sectional analysis
- Cross-cultural adaptation of the Danish version of the Big Five Inventory – a dual-panel approach
- The development of a novel questionnaire assessing alterations in central pain processing in people with and without chronic pain
- Letters to the Editor
- The clinical utility of a multivariate genetic panel for identifying those at risk of developing Opioid Use Disorder while on prescription opioids
- Should we use linked chronic widespread pain and fibromyalgia diagnostic criteria?
- Book review
- Akut och cancerrelaterad smärta – Smärtmedicin Vol. 1
Articles in the same Issue
- Frontmatter
- Systematic review
- Are there differences in lifting technique between those with and without low back pain? A systematic review
- Topical reviews
- Pain psychology in the 21st century: lessons learned and moving forward
- Chronic abdominal pain and persistent opioid use after bariatric surgery
- Clinical pain research
- Spinal cord stimulation for the treatment of complex regional pain syndrome leads to improvement of quality of life, reduction of pain and psychological distress: a retrospective case series with 24 months follow up
- The feasibility of gym-based exercise therapy for patients with persistent neck pain
- Intervention with an educational video after a whiplash trauma – a randomised controlled clinical trial
- Reliability of the conditioned pain modulation paradigm across three anatomical sites
- Is rotator cuff related shoulder pain a multidimensional disorder? An exploratory study
- Are degenerative spondylolisthesis and further slippage postoperatively really issues in spinal stenosis surgery?
- Multiprofessional assessment of patients with chronic pain in primary healthcare
- The impact of chronic orofacial pain on health-related quality of life
- Pressure pain thresholds in children before and after surgery: a prospective study
- Observational studies
- An observational study on risk factors for prolonged opioid prescription after severe trauma
- Dizziness and localized pain are often concurrent in patients with balance or psychological disorders
- Pre-consultation biopsychosocial data from patients admitted for management at pain centers in Norway
- Original experimentals
- Local hyperalgesia, normal endogenous modulation with pain report beyond its origin: a pilot study prompting further exploration into plantar fasciopathy
- Pressure pain sensitivity in patients with traumatic first-time and recurrent anterior shoulder dislocation: a cross-sectional analysis
- Cross-cultural adaptation of the Danish version of the Big Five Inventory – a dual-panel approach
- The development of a novel questionnaire assessing alterations in central pain processing in people with and without chronic pain
- Letters to the Editor
- The clinical utility of a multivariate genetic panel for identifying those at risk of developing Opioid Use Disorder while on prescription opioids
- Should we use linked chronic widespread pain and fibromyalgia diagnostic criteria?
- Book review
- Akut och cancerrelaterad smärta – Smärtmedicin Vol. 1

