A 59-year-old woman presented with isolated peritoneal metastases in the context of elevated serum AFP levels (Figure 1A and B). No primary tumour was found, notably from the liver, the gastrointestinal or gynecological tracts. A laparoscopic assessment reported a peritoneal cancer index (PCI) reaching 22/39 and biopsies performed disclosed hepatocellular carcinoma (HCC). A chemotherapy followed by a cytoreductive surgery/hyperthermic intraoperative intra-peritoneal chemotherapy (HIPEC) was given, leading to a complete macroscopic clearance. Ultimately, liver metastases appeared, resulting in death.
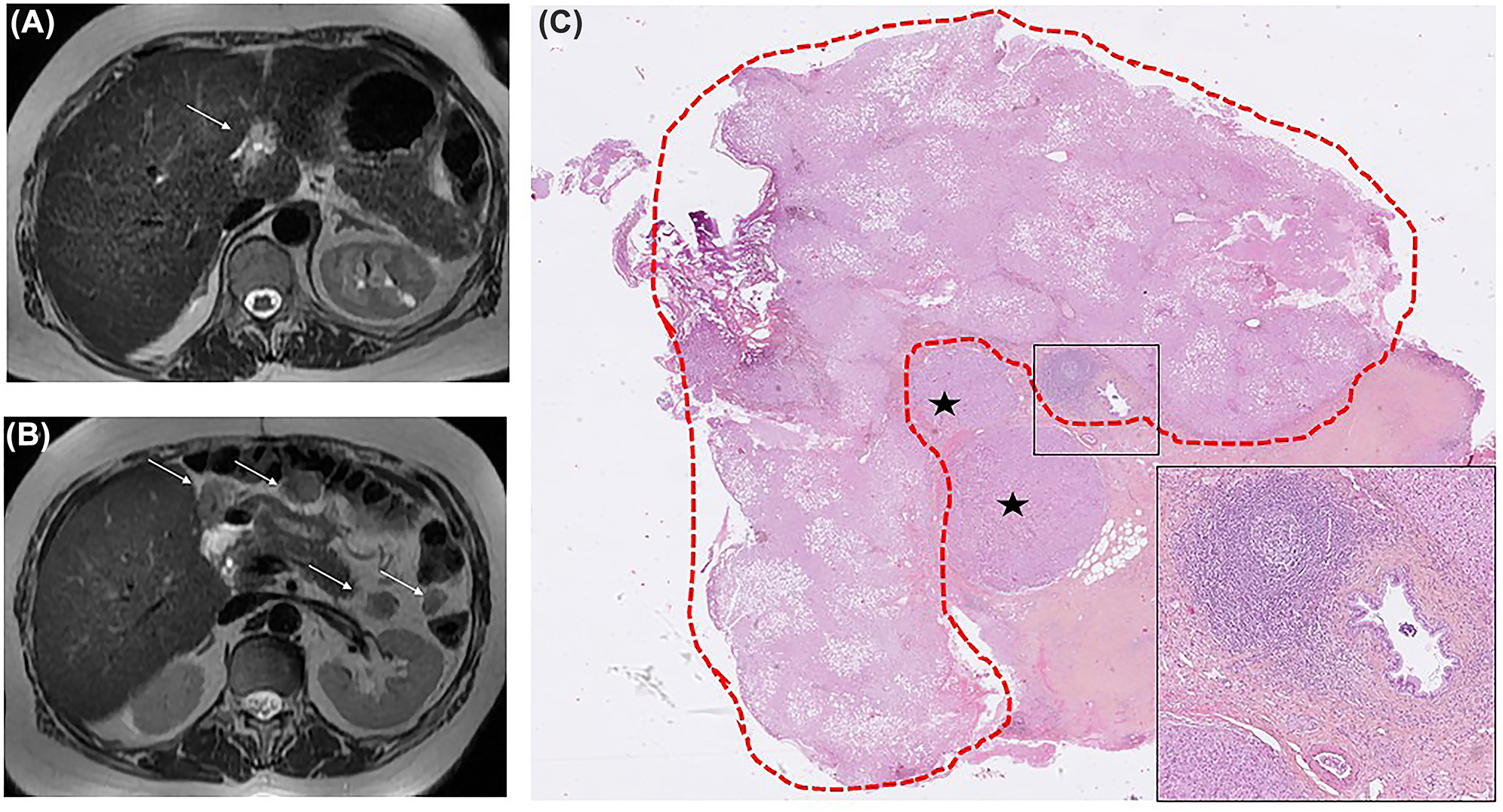
Magnetic resonance imaging (MRI) of the liver and peritoneum (axial T2 weighted images).
(A) Initial MRI: ill-defined T2 hyperintense nodule within the falciform ligament of the liver (arrow). (B) MRI at 3 months: Appearance of several peritoneal metastases (arrows). Note the absence of any parenchymal liver tumour in both images. (C) Histopathological analysis: hepatocellular carcinoma (asterisks) in the falciform ligament of the liver, representing the starting point of the peritoneal disease. Ectopic liver is circled in red (greater axis: 15 mm), with detectable steatosis (HES, ×6). Note the independent vasculo-biliary stalk, highlighted in the inset (HES, ×50). HES: hematoxylin-eosin-saffron.
All surgical specimens histologically showed features of HCC. An unsuspected ectopic liver (EL) was observed within the falciform ligament of the liver, in close vicinity of tumour (Figure 1C), strongly suggesting an EL cancerization [1, 2].
This unusual clinical presentation may first suggest a peritoneal extension from a liver HCC, which is usually encountered in massive-type tumours [3]. Rare hepatoid carcinomas can also be suspected in the context of a primary gastric tumour showing an adenocarcinomatous component with positive Sal-like protein 4 (SALL4) immunostaining [4].
Acknowledgments
Thanks to Mrs Coralie Lautrec for her kind assistance, advices and processing of histological images.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Ethical approval: Not applicable.
References
1. Kawahara, E, Kitamura, T, Ueda, H, Ogino, T, Mai, M, Ooi, A, et al.. Hepatocellular carcinoma arising in the abdominal cavity. An autopsy case of ectopic liver origin. Acta Pathol Jpn 1988;38:1575–81. https://doi.org/10.1111/j.1440-1827.1988.tb02297.x.Search in Google Scholar
2. Arakawa, M, Kimura, Y, Sakata, K, Kubo, Y, Fukushima, T, Okuda, K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology 1999;29:57–61. https://doi.org/10.1002/hep.510290144.Search in Google Scholar
3. Yuki, K, Hirohashi, S, Sakamoto, M, Kanai, T, Shimosato, Y. Growth and spread of hepatocellular carcinoma. A review of 240 consecutive autopsy cases. Cancer 1990;66:2174–9. https://doi.org/10.1002/1097-0142(19901115)66:10<2174::aid-cncr2820661022>3.0.co;2-a.10.1002/1097-0142(19901115)66:10<2174::AID-CNCR2820661022>3.0.CO;2-ASearch in Google Scholar
4. Ushiku, T, Shinozaki, A, Shibahara, J, Iwasaki, Y, Tateishi, Y, Funata, N, et al.. SALL4 represents fetal gut differentiation of gastric cancer, and is diagnostically useful in distinguishing hepatoid gastric carcinoma from hepatocellular carcinoma. Am J Surg Pathol 2010;34:533–40. https://doi.org/10.1097/pas.0b013e3181d1dcdd.Search in Google Scholar
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Role of prophylactic HIPEC in non-metastatic, serosa-invasive gastric cancer: a literature review
- Research Articles
- Abdominal tissue concentrations and penetration of carboplatin in a HIPEC procedure ‒ assessment in a novel porcine model
- Perioperative anaesthetic management in cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC): a retrospective analysis in a single tertiary care cancer centre
- Pressurized intraperitoneal aerosol chemotherapy (PIPAC) in multimodal therapy for patients with oligometastatic peritoneal gastric cancer: a randomized multicenter phase III trial PIPAC VEROne
- Importance of biopsy site selection for peritoneal regression grading score (PRGS) in peritoneal metastasis treated with repeated pressurized intraperitoneal aerosol chemotherapy (PIPAC)
- The effect of metastasis location on outcome after cytoreductive surgery and heated intraperitoneal chemotherapy
- Clinical Images
- Peritoneal metastases of unknown primary with hepatoid features
Articles in the same Issue
- Frontmatter
- Review
- Role of prophylactic HIPEC in non-metastatic, serosa-invasive gastric cancer: a literature review
- Research Articles
- Abdominal tissue concentrations and penetration of carboplatin in a HIPEC procedure ‒ assessment in a novel porcine model
- Perioperative anaesthetic management in cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC): a retrospective analysis in a single tertiary care cancer centre
- Pressurized intraperitoneal aerosol chemotherapy (PIPAC) in multimodal therapy for patients with oligometastatic peritoneal gastric cancer: a randomized multicenter phase III trial PIPAC VEROne
- Importance of biopsy site selection for peritoneal regression grading score (PRGS) in peritoneal metastasis treated with repeated pressurized intraperitoneal aerosol chemotherapy (PIPAC)
- The effect of metastasis location on outcome after cytoreductive surgery and heated intraperitoneal chemotherapy
- Clinical Images
- Peritoneal metastases of unknown primary with hepatoid features

