Abstract
Artificial Intelligence (AI) is bringing an unprecedented evolution in human history. As it develops, the utilization of AI in clinical practice becomes one of the hot topics that attracts the attention of the medical field as well as the public. While we know that AI will be heavily involved in the medical system, a critical question is what we expect for the future AI medical doctor. To answer this question, it is important to understand that the developing patterns of any other discovery and industrialization do not fit the pattern of AI development, because it acts more like a human instead of simply being a machine or tool. Thus, AI doctors function like human doctors to provide patient-centered reasoning, intellectual judgment, and ethical decision-making rather than just mechanical data processing. Here we present such a likely development process, including current AI status, expected AI doctors, challenges, and future directions.
Introduction
While everyone knows that AI is another evolution for human beings, it is essential to understand that AI is not the same as any medical device or other technology. It works with its logical thinking and learning capacity, mimicking the human brain [1]. As such, the evolution it brings will be the one that we have ever seen in human history. Accordingly, we expect that it will follow the path of medical doctors to function in the medical field. Thus, in the future, we will have a humanized AI system, a population of AI doctors with centralized management systems [2]. We also expect that AI doctors will specialize in every special medical field, with individualized medical capacity, and under the system of AI doctor management, perhaps based on different regions, countries, or worldwide organizations, in the best scenario. The application of AI is both forward-moving and self-reinforcing. The distinguishing feature of AI is its dual nature: initially guided by human input, and then AI systems increasingly gain autonomous activation and reasoning analogous to the human brain. Soon, AI will not virtuously act upon human instructions but will also make decisions based on what it learned and analyzed, form its own judgments, and provide recommendations, or even directives to humans [3].
Current AI models as assistants for doctors
Currently, there are two categories of AI models that can be or will be used as the assistant to or act as doctors: The large language models (LLMs) and the specialized models for individual diseases or specialized functions in disease diagnosis [4] (Supplementary Table 1). They are currently widely used by the public, patients, and physicians. As they learn, the accumulated knowledge will enable them to serve as great assistants for the physicians. While LLM hallucinations exist as a weakness, a different study has indicated that LLM can outperform traditional nurse triage in identifying high-acuity patients (Supplementary Table 2). The specialized deep learning models, on the other hand, focus on diagnosis and treatment options for single diseases [5]. All of them need the input of one or more pieces of information and then the model will provide answers. They in certain degree act as an assistant for physician and as a consultant for patients.
The ideal future AI medical doctors
What is a perfect AI doctor from the point of view of a patient? First, it should be able to listen to what a patient says. Then it should be able to communicate or discuss with the patient. After interviewing the patient, it should be able to instruct the patient on what to do next, such as to be examined or tested for certain samples. After the results coming out, it should be able to read the reports and make a judgement on what disease or disorder the patient has. Then it should be able to discuss with the patient the options of treatment. Next, the AI doctor may make the decision on the treatment for the patient.
An important capability of the AI doctor is communication among AI doctors. This is important not only for the discussion of patient’s condition and treatment, but also for the subsequent steps for the treatment of the patient’s disease. For example, after an AI doctor made the decision on a surgery procedure for a patient, this AI doctor may need to communicate with the AI surgeon for exchange of information of the patient and necessary items of attention during and after surgery. Communication capability is essential for the development of AI doctors. To achieve this capacity of the ideal AI doctor, one way is the combination of robotics with AI models. These robots have capabilities of listening, speaking, thinking, and facial or limb gesture expression [6] (Figure 1A). In addition, they can walk, sit, see, and recharge themselves. With such capabilities, these robots can communicate with patients, nurses, medical staff, and among themselves [7] (Figure 1B). AI robots can be categorized into different specialists. They can act as a physician in primary care, surgical specialties, medical specialties, and other specialties, such as a pathologist. They can also be nurses and medical support staff members (Figure 1C). Importantly, they can have a meeting among themselves for discussion of patient’s disease and treatment options. They may attend scientific meetings to present and listen to others (Figure 1D).
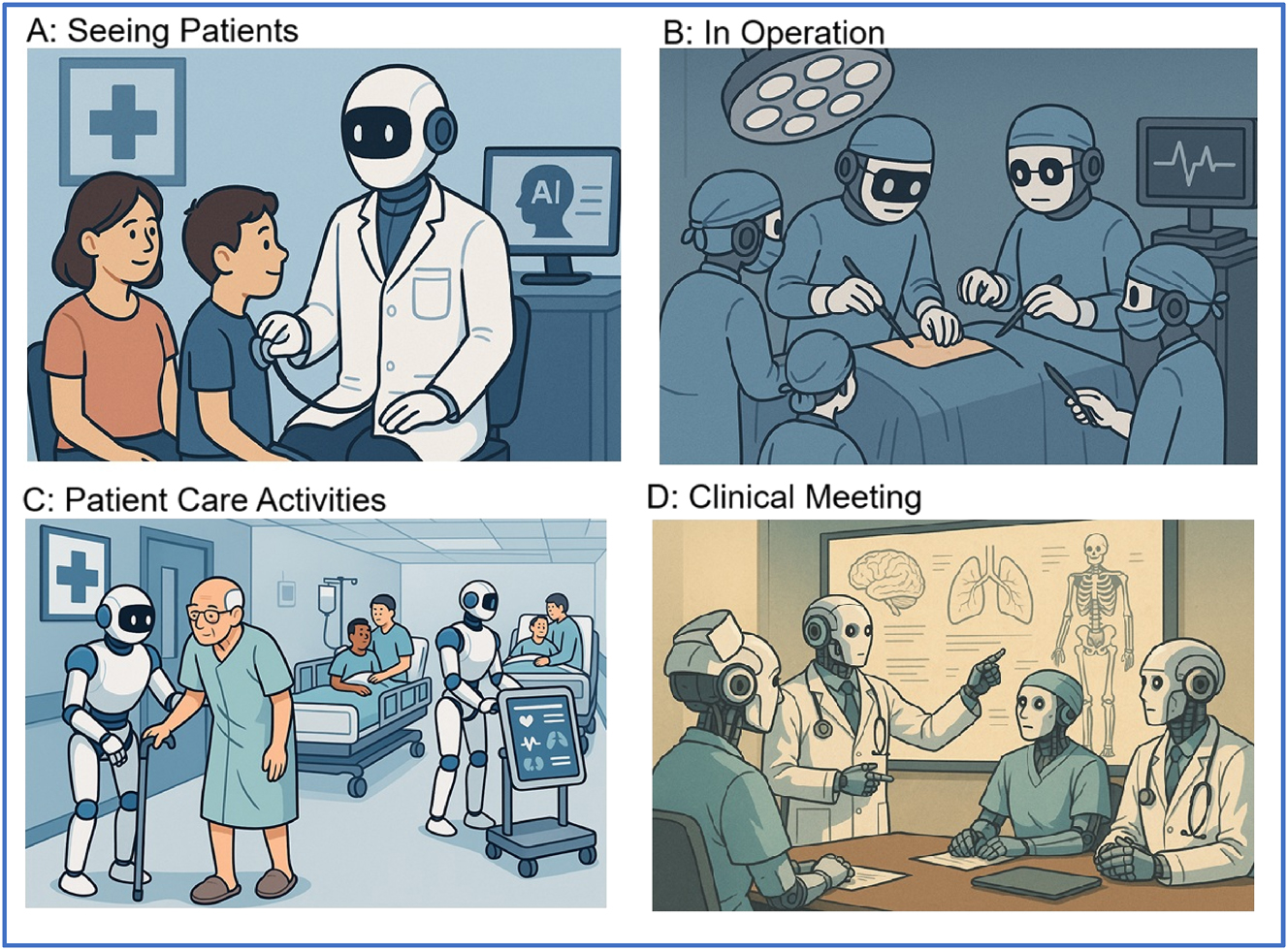
Activities of future AI medical robots in hospital. A. AI robotic doctor can see a patient like a human doctor and give correct diagnosis. B. AI robots act as surgeons and nurses perform surgery on patients. C. AI robots can perform other activities or duties of human’s nurses and other medical staff. D. AI robots can communicate with each other and have meetings to discuss patients’ illness and treatment options.
Advantages of AI medical robots
It is expected that AI medical robots will have multiple advantages over human doctors [7]. The expected advantages include: 1) Updated treatment knowledge by every individual robot. Thus, every robot is the best doctor in the world. 2) With knowledge and skills in multiple medical fields. Therefore, AI robots may see patients with multiple diseases with the best diagnosis [8]. 3) Fewer medical errors in comparison with humans. Medical robots may work tirelessly all day, 24 h a day and 7 days a week without medical errors. 4) Treat patients equally with less discrimination [9]. Thus, AI robots do not dislike or like a particular population or an ethnic group. 5) They learn quickly and improvement from one robot may immediately transfer to all other AI robots, because they are individual robots working in different hospitals, but all can be connected to each other electronically. And 6) Every patient can receive treatment whenever it is needed. AI robots can be made as many as necessary and they can immediately start to work without years of training like that for humans.
Anything may go wrong?
Perhaps the main concern from the human point of view is that someday the robots will be out of humans‘ control. It is important not to forget that the programs in robots are designed by humans, humans should be able to control the activities of robots. The programmer designer should have a control button for the shutdown of the robots. Even if the shutdown button does not work, humans should know the weakness of the program and the robots.
Is there any possibility that the medical robots will hurt the patients purposely. That could happen but the chance is small [10]. Even in human populations, doctors may hurt patients. Careful monitoring activities of robots are critical for the prevention of any wrongdoing by robots.
Will someone design a bad AI doctor? Because robots are designed to work together by groups of scientists or companies, the chance of production of the individual bad robot is rare. However, it is possible a robot is trained for wrongdoing. A rigorous human management and monitoring is essential to prevent any wrongdoing by AI robots.
Will AI doctors make mistakes? Yes. AI doctors can make mistakes. More seriously, in case of the errors in the instructions of the AI design, all AI robots working on the same disease make the same mistake. This is the most important issue that needs to be addressed or paid attention in designing or organizing the activities of medical AI robots.
Altogether, current evidence indicates that AI could make mistakes, however it makes fewer mistakes than humans [10].
Conclusions
The integration of AI into medicine represents a revolutionary shift unlike any previous discovery in medical history. Current LLMs and specialized AI systems already function as valuable assistants to physicians. With rapid advancements in robotics and AI integration, we are moving toward a future where AI medical robots will serve as fully functional doctors capable of diagnosis, treatment, communication, and collaboration. These AI doctors are expected to outperform human counterparts while also offering 24/7 healthcare services. Though concerns exist regarding oversight, errors, and ethical safeguards, these will be addressed through rigorous human supervision and system design.
Funding source: Health Science Center, University of Tennessee
Award Identifier / Grant number: R073290109
Acknowledgments
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: WG and YW developed the concept. TG, XM, and WG participated in data analysis and manuscript drafting. TG, XM, YW, and WG interpreted the data and edited the manuscript.
-
Use of Large Language Models, AI and Machine Learning Tools: During the preparation of this work the authors used AI models to draw pictures. After using this service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
-
Conflict of interest: The authors declare no competing financial interests.
-
Research funding: This work was partially supported by funding from the University of Tennessee Health Science Center (R073290109) to WG in Memphis, TN, USA.
-
Data availability: All data have been presented in the manuscript and available to the public.
References
1. Chiriatti, M, Ganapini, M, Panai, E, Ubiali, M, Riva, G. The case for human-AI interaction as system 0 thinking. Nat Hum Behav2024;8:1829–30. https://doi.org/10.1038/s41562-024-01995-5.Search in Google Scholar PubMed
2. Limb, M. Microsoft claims AI tool can outperform doctors in diagnostic accuracy. BMJ 2025;390:r1385. https://doi.org/10.1136/bmj.r1385.Search in Google Scholar PubMed
3. Kałwa, A, Popek, L, Żurowska, N, Opidowicz, M, Malinowska, K, Jabłońska, A, et al.. Can AI-assisted therapy (PARO robot) be a treatment option for children hospitalised in an acute mental health ward? Psychiatr Pol 2024;2:1–10. https://doi.org/10.12740/PP/OnlineFirst/188053.Search in Google Scholar PubMed
4. Zuluaga, L, Bamby, J, Okhawere, KE, Ucpinar, B, Razdan, S, Badani, KK. Assessing operative variability in robot-assisted radical prostatectomy (RARP) through AI. J Robot Surg 2025;19:99. https://doi.org/10.1007/s11701-025-02225-4.Search in Google Scholar PubMed
5. Kim, K, Lee, JH, Je Oh, S, Chung, MJ. AI-based computer-aided diagnostic system of chest digital tomography synthesis: demonstrating comparative advantage with X-ray-based AI systems. Comput Methods Programs Biomed 2023;240:107643. https://doi.org/10.1016/j.cmpb.2023.Search in Google Scholar
6. Seidlitz, S, Hölzl, K, von Garrel, A, Sellner, J, Katzenschlager, S, Hölle, T, et al.. AI-powered skin spectral imaging enables instant sepsis diagnosis and outcome prediction in critically ill patients. Sci Adv 2025;11:eadw1968. https://doi.org/10.1126/sciadv.adw1968.Search in Google Scholar PubMed PubMed Central
7. Flint, AR, Schaller, SJ, Balzer, F. How AI can help in error detection and prevention in the ICU? Intensive Care Med 2025;51:590–2. https://doi.org/10.1007/s00134-024-07775-z.Search in Google Scholar PubMed PubMed Central
8. Singhal, A, Neveditsin, N, Tanveer, H, Mago, V. Toward fairness, accountability, transparency, and ethics in AI for social media and health care: scoping review. JMIR Med Inform 2024;12:e50048. https://doi.org/10.2196/50048.Search in Google Scholar PubMed PubMed Central
9. Beyaz, S, Özgözen, AL, Turgut, N, Ölke, HC. Artificial intelligence and robotic surgery in clinical medicine: progress, challenges, and future directions. Future Sci OA 2025;11:2540742. https://doi.org/10.1080/20565623.2025.2540742.Search in Google Scholar PubMed PubMed Central
10. Pai, SN, Jeyaraman, M, Shyam, A. The AI orthopedician will see you now - but who is liable if it’s wrong? J Orthop Case Rep 2024;14:1–3. https://doi.org/10.13107/jocr.2024.v14.i12.4994.Search in Google Scholar PubMed PubMed Central
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/mr-2025-0044).
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

