Abstract
Objectives
Community births in the United States – including planned home and freestanding birth center deliveries – have increased in recent years. Understanding how these patterns have evolved across racial and ethnic groups, particularly in the post-pandemic period, is essential for clinical practice and health policy. Objective: To analyze national trends in community births from 2016 through 2024 by race and ethnicity, and to discuss clinical, ethical, and policy implications.
Methods
Birth certificate data from the CDC natality database were examined for 2016–2024. Community births were defined as intended home or freestanding birth center births. Trends were assessed overall and stratified by race/ethnicity, with relative changes indexed to 2016.
Results
From 2016 to 2024, community births increased overall but diverged by group. Non-Hispanic White and Hispanic women demonstrated sustained increases relative to 2016, while non-Hispanic Black women showed an increase during the pandemic followed by decline, and non-Hispanic Asian women displayed a modest upward trend. These shifts occurred against the backdrop of declining total births in some groups, affecting proportional comparisons. International comparisons are limited by the distinctive U.S. context, where midwifery is less integrated and credentialing standards are variable.
Conclusions
Community birth patterns since the pandemic reveal both growth and divergence across racial and ethnic groups. These findings highlight the need for policy interventions to address maternity care deserts and harmonize midwifery credentialing. Clinically, professional responsibility requires fully informed consent leading to directive counseling, which should not be misinterpreted as paternalism but as an ethical duty to recommend hospital birth as the safest option while respecting patient autonomy.
Introduction
Community births, defined as intended home births and births in freestanding birth centers, account for only a small proportion of U.S. deliveries but have grown steadily in recent years. These settings are associated with higher risks of neonatal morbidity and mortality compared with hospital births, yet the number of families choosing them continues to rise [1].
The American College of Obstetricians and Gynecologists considers the hospital as the safest place for delivery and outlined strict criteria for the selection of appropriate candidates for home birth [2]. But these criteria have not been widely implemented by midwives practicing outside hospitals with increased risk profiles during the COVID-19 pandemic. [3], [4], [5], [6]. This gap has contributed to a significantly higher risk of adverse outcomes, including elevated rates of neonatal morbidity and mortality [7], 8]. Although international systematic reviews have reported comparable or even favorable outcomes for low-risk women delivering at home or in birth centers, these findings are limited to carefully selected low-risk populations within integrated maternity systems [9], 10]. This limitation does not reflect the reality of U.S. community births, where risk profiles are often higher and midwifery services are less consistently integrated into the healthcare system, resulting in outcomes that differ substantially from those reported in low-risk international cohorts. In contrast, in the United States, a large proportion of women who pursue community births have high-risk conditions such as prior cesarean delivery, advanced maternal age, twins, breech presentation, or medical comorbidities, making direct comparison misleading and safety concerns more pronounced [11]. Families nevertheless turn to community births for multiple reasons, including the desire for a more natural or personalized experience, concerns about cesarean delivery and other hospital interventions, dissatisfaction from prior hospital encounters, and, more recently, fears about hospital care during the COVID-19 pandemic [12]. Behavioral science insights have suggested that cognitive biases may contribute to underestimation of risks and overemphasis on perceived benefits of home birth, while structured approaches to counseling may help ensure more balanced decision-making [12].
In contrast to countries such as England and the Netherlands, where out-of-hospital birth is fully integrated into the maternity system and rates have remained stable or declined, the United States stands out for continued increases despite well-documented safety concerns. Understanding how birthplace patterns vary across racial and ethnic groups, and how they changed during and after the pandemic, is essential for shaping clinical counseling and health system responses.
The objective of this study is to evaluate national trends in birthplaces by race and ethnicity, with particular attention to changes observed during the COVID-19 pandemic and in the years that followed.
Methods
We conducted a retrospective, descriptive, population-based cohort study of all recorded term live births in the United States from 2016 through 2024, using publicly available natality data from the CDC WONDER database [13]. Data were stratified by year, birthplace, and race/ethnicity. According to the CDC classification, place of births were classified as: Hospital, Freestanding birth center, Home (intended), Home (not intended), Unknown or other. For subgroup analyses, “home (not intended)” and “home (unknown if intended)” were combined. We used the following CDC categories: Hispanic, non-Hispanic (NH) White, NH Black, NH Asian, NH American Indian/Alaska Native (AmInd), NH Native Hawaiian/Pacific Islander (Haw), NH more than one race (>1), and Unknown ethnicity. We assessed absolute counts and proportions per year by birthplace. The primary outcome was the change in community births (intended home+freestanding birth center) between 2016 and 2024. We did not conduct formal statistical tests of trend; rather, our analyses were descriptive.
Results
Overall trends
Table 1 shows the proportion change of birthplace for each year from 2016 to 2024, Figure 1 shows relative changes in Community Births (intended home plus birth center births) by years for the 4 main racial/ethnic groups and Figure 2 shows relative changes in birthplaces by years overall and for each racial/ethnic group. Between 2016 and 2024, the proportion of hospital births decreased from 98.3 % (3,494,408) to 97.6 % (3,157,655), a decline of 0.8 percentage points. During the same period, the proportion of intended home births rose from 0.82 % (29,016) to 1.45 % (47,045), representing a 62 % relative increase. Freestanding birth center births also grew, from 0.55 % (19,617) to 0.69 % (22,308), a 25 % relative increase. Births at home without intention increased slightly, while the “unknown/other” category declined. Overall, community births (intended home plus freestanding birth center) increased from 1.37 % of U.S. births in 2016 to 2.14 % in 2024.
Proportion of birthplace by year 2016–2024.
| Year | Hospital | Freestanding birth center | Home (intended) | Home (not intended) | Unknown or other |
| 2016 | 98.32 % (3,494,408) | 0.55 % (19,617) | 0.82 % (29,016) | 0.11 % (3,853) | 0.20 % (7,202) |
| 2017 | 98.30 % (3,410,796) | 0.57 % (19,772) | 0.82 % (28,402) | 0.11 % (3,885) | 0.20 % (7,025) |
| 2018 | 98.26 % (3,349,861) | 0.58 % (19,754) | 0.85 % (28,921) | 0.11 % (3,815) | 0.20 % (6,914) |
| 2019 | 98.23 % (3,302,486) | 0.59 % (19,916) | 0.86 % (29,019) | 0.11 % (3,809) | 0.20 % (6,695) |
| 2020 | 97.89 % (3,177,971) | 0.67 % (21,729) | 1.07 % (34,809) | 0.13 % (4,195) | 0.24 % (7,824) |
| 2021 | 97.65 % (3,200,289) | 0.71 % (23,382) | 1.32 % (43,205) | 0.15 % (4,837) | 0.17 % (5,477) |
| 2022 | 97.58 % (3,205,030) | 0.72 % (23,800) | 1.38 % (45,330) | 0.16 % (5,260) | 0.15 % (4,980) |
| 2023 | 97.53 % (3,139,845) | 0.71 % (22,977) | 1.45 % (46,565) | 0.16 % (5,184) | 0.15 % (4,753) |
| 2024 | 97.55 % (3,157,655) | 0.69 % (22,308) | 1.45 % (47,045) | 0.16 % (5,138) | 0.15 % (4,867) |
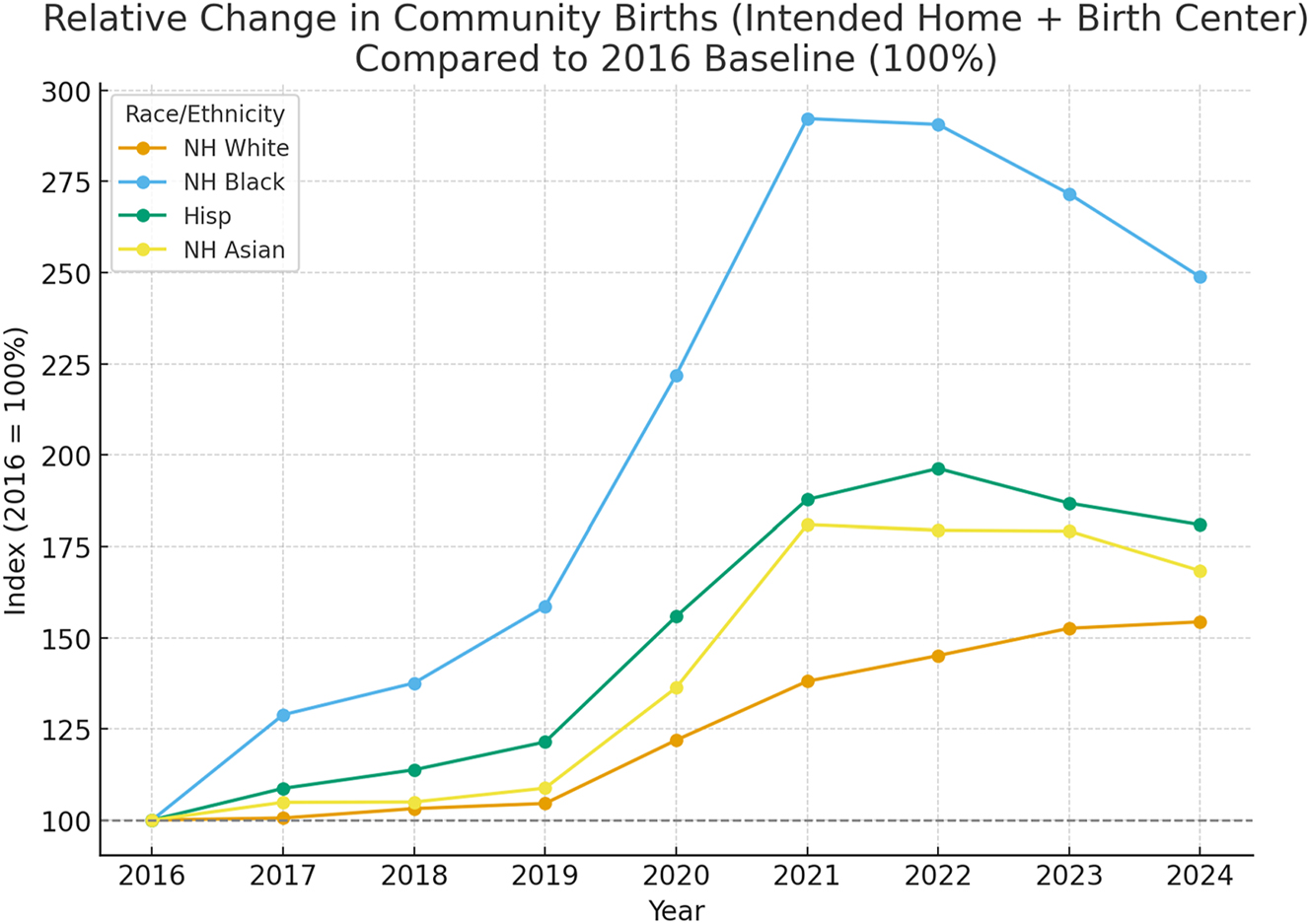
Relative changes in community births (intended home plus birth center births) by years and 4 main racial/ethnic groups with 2016 as baseline (100 %).
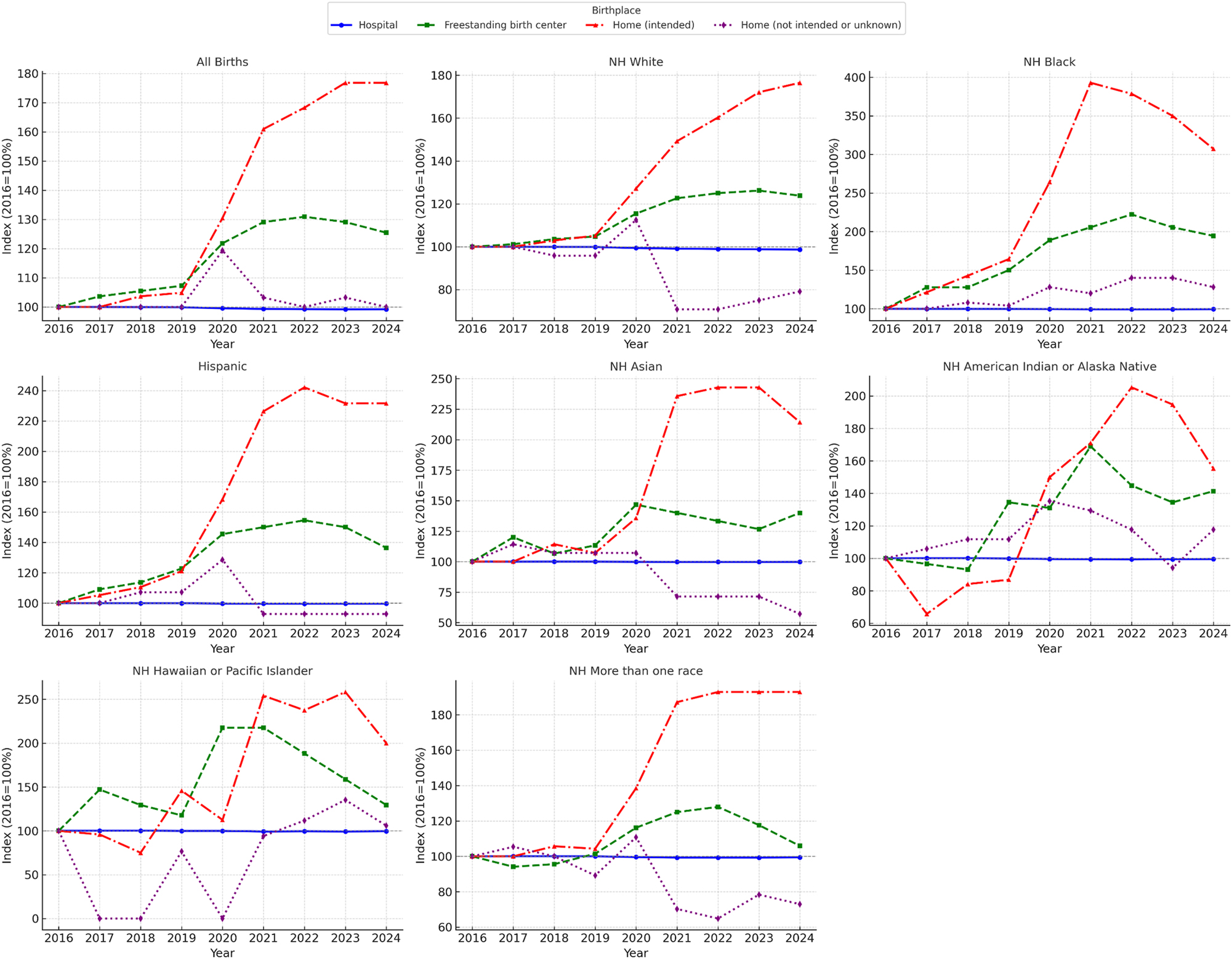
Relative changes in birthplaces by years and for each racial/ethnic group with 2016 as baseline (100 %).
Results by race and ethnicity
Non-Hispanic White
NH White births declined in absolute numbers (−14 % between 2016 and 2024), but the proportion of community births increased steadily. The proportion of intended home births rose from 1.36 to 2.40 %, and freestanding birth center births from 0.84 to 1.04 %. The proportion of Hospital births decreased correspondingly, with no evidence of reversal after the pandemic.
Non-Hispanic Black
NH Black women experienced the most distinct pandemic-related surge. The proportion of intended home births rose from 0.14 % in 2016 to 0.55 % in 2021, and birth center births from 0.18 to 0.37 %. However, both proportions declined thereafter, with intended home births falling back to 0.43 % and birth center births to 0.35 % in 2024. Hospital births, while still dominant, recovered slightly in the last three years. Overall, 2024 levels remain higher than in 2016 but below the 2020–2021 peak.
Hispanic
Among Hispanic women, births increased overall (+6.1 %). The proportion of community births grew consistently across the study period: intended home births rose from 0.19 to 0.44 %, and birth center births from 0.22 to 0.30 %. Unlike NH Blacks, the rise did not reverse after the pandemic.
Non-Hispanic Asian
NH Asian women showed gradual increases in community births, with the proportion of intended home births rising from 0.14 to 0.30 % and birth center births from 0.15 to 0.21 %. Hospital births declined in parallel. There was no pandemic-driven surge; instead, growth was steady and incremental.
American Indian/Alaska Native
Despite declining overall births, NH American Indian/Alaska Native women increased intended home births from 0.38 to 0.59 %. Birth center births rose modestly, while hospital births decreased slightly. The trend was relatively steady rather than pandemic driven.
Native Hawaiian/Pacific Islander
NH Hawaiian/Pacific Islander women, though small in absolute numbers, more than doubled intended home births from 0.24 % in 2016 to 0.48 % in 2024. Birth center births fluctuated but trended upward, while hospital births declined.
More than one race
Multiracial women showed some of the largest relative increases. Intended home births nearly doubled, from 0.70 % in 2016 to 1.35 % in 2024, and birth center births also grew slightly. Hospital births decreased proportionally, with the increase most pronounced during and after the pandemic.
Because of the small absolute numbers in subgroups such as Native Hawaiian/Pacific Islander and American Indian/Alaska Native women, proportional changes may exaggerate differences. These findings should be interpreted with caution.
Pandemic years
The pandemic years of 2020–2021 were marked by the steepest increases in community births across nearly all groups, especially for NH Black women. While most racial and ethnic groups maintained elevated levels through 2024, the trajectory for NH Black women was distinct: community births peaked during the pandemic but then declined modestly, suggesting a partial reversion toward hospital births. In contrast, NH White, Hispanic, Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and multiracial groups demonstrated sustained post-pandemic increases, indicating that for these populations the shift toward out-of-hospital birth has become an enduring trend.
Discussion
This national analysis demonstrates that community births in the United States continued to increase beyond 2022 and through 2024 [1]. However, the trajectories varied substantially by race and ethnicity. For most groups – including non-Hispanic White, Hispanic, Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and multiracial women – the pandemic surge in community births has persisted, suggesting that out-of-hospital birth is becoming a more established feature of the U.S. maternity landscape. By contrast, among non-Hispanic Black women, community births peaked during 2020–2021 but subsequently declined, underscoring that the pandemic-related rise was not uniform in its durability.
It is important to consider potential biases introduced by changing denominators across racial and ethnic groups. For example, non-Hispanic White births declined by more than 10 % between 2016 and 2024, while Hispanic births increased. In smaller populations, even modest absolute shifts can appear disproportionately large when expressed as percentages. This limitation is important for contextualizing subgroup findings and should be borne in mind when interpreting differences across groups, proportional comparisons may overstate or understate the magnitude of change within groups, particularly for smaller populations such as American Indian/Alaska Native or Native Hawaiian/Pacific Islander women. Absolute numbers remain low in some subgroups, and even small shifts can appear large when expressed as percentages.
The persistence of elevated community birth rates in many groups beyond the COVID-19 pandemic surge highlights potential structural and cultural drivers that extend beyond pandemic disruptions [12], 13]. These include dissatisfaction with perceived overuse of medical interventions in hospitals, the desire for more personalized and culturally responsive care, and mistrust of institutional settings. Systemic factors such as hospital closures and the expansion of maternity care deserts further exacerbate disparities by limiting access to safe, facility-based obstetric care [14], [15], [16]. For example, American Indian/Alaska Native women and women in rural areas may face geographic barriers that may leave community birth as one of the few accessible options. In contrast, for non-Hispanic Black women, the temporary pandemic surge followed by a decline may reflect a complex interplay of mistrust, heightened awareness of safety risks, and possible targeted outreach efforts after the peak pandemic years.
International comparisons underscore the distinctiveness of the U.S. experience. In countries such as England and the Netherlands, where midwifery is fully integrated into the healthcare system, out-of-hospital birth is embedded within a regulated framework that ensures close collaboration, standardized credentialing, and seamless transfer to hospitals when needed [17]. Outcomes reported from these systems, particularly for carefully selected low-risk women, are therefore not directly comparable to those in the United States. By contrast, U.S. midwifery is characterized by fragmented regulation and variable credentialing, ranging from certified nurse-midwives with rigorous hospital-based training to lay or direct-entry midwives whose education and oversight may be inconsistent across states. This heterogeneity, coupled with the absence of a consistently integrated transfer system, means that out-of-hospital birth in the U.S. carries higher risks and greater variability in outcomes. For these reasons, applying international evidence to the U.S. setting risks obscuring important safety concerns and overestimating the protective effect of midwifery in a context where training, integration, and regulatory safeguards differ substantially.
These findings also highlight the need for policy-level interventions. Addressing maternity care deserts through expansion of hospital-based services and ensuring consistent national standards for midwifery credentialing would reduce unsafe variations in practice and improve equitable access to safe obstetric care.
Fully informed consent is central to counseling of pregnant women, not only about birthplace decisions [5], 18], 19]. Informed consent is not simply the act of signing a document; it requires that patients receive complete, accurate, and comprehensible information about risks, benefits, and alternatives, and that they have the opportunity to ask questions in a supportive environment.
Because out-of-hospital births are consistently associated with higher neonatal risks [2], 3], 7], 8], professional responsibility requires a process of fully informed consent that leads to directive counseling. In this context, clinicians should recommend hospital birth as the safest option while still respecting patient autonomy. This approach is supported by the American College of Obstetricians and Gynecologists, whose 2021 Committee Opinion on informed consent and shared decision-making emphasizes that patients must receive clear, accurate, and comprehensible information about risks, benefits, and alternatives to make meaningful decisions [18]. Directive counseling, when properly practiced, is consistent with these principles: it ensures that patients are informed while also receiving professional guidance about the safest course of action. We recognize that some experts and professional bodies emphasize ‘shared decision-making’ in discussions of birth location. However, we deliberately distinguish informed consent with directive counseling from shared decision-making. Shared decision-making presumes equipoise among options, whereas in the case of community vs. hospital birth, equipoise does not exist because hospital birth is demonstrably safer. Informed consent, properly conducted, ensures accurate disclosure of risks, benefits, and alternatives, preserves patient autonomy, and fulfills the physician’s professional responsibility to recommend hospital birth as the safest course. Importantly, directive counseling must not be equated with paternalism. As articulated in the professional responsibility model, physicians have an ethical duty not only to respect autonomy but also to use their expertise to prevent avoidable harm [20]. Paternalism implies overriding patient choice, whereas directive counseling preserves autonomy while fulfilling the physician’s responsibility to recommend hospital delivery as the option that best protects maternal and neonatal safety. Without this process, women may underestimate risks, undermining both ethical obligations and clinical safety.
The CDC natality database is an important part of assessing maternal and neonatal health in the United States [21]. While the CDC natality database represents a major strength in providing comprehensive national data, reliance on this resource also poses limitations. Misclassification of intended vs. unintended home births remains possible, and the completeness of reporting may vary by jurisdiction. In addition, under the current federal administration, the CDC has experienced budget cuts and organizational changes, raising concern that access, timeliness, and continuity of natality data could be compromised in the future. Any disruption to this dataset would hinder surveillance of maternal and neonatal outcomes and limit the ability of clinicians and researchers to monitor national trends in birthplace.
In sum, the sustained growth of community births beyond the pandemic years highlights potential systemic weaknesses in U.S. maternity care across racial and ethnic groups. Addressing these patterns requires a dual approach: ensuring fully informed consent with directive counseling and reforming hospital-based care to reduce unnecessary intervention and guarantee safe, respectful, and accessible maternity services. Only through this combined strategy can preventable perinatal morbidity and mortality be reduced while addressing the legitimate concerns of diverse patient populations.
Conclusions
From 2016 to 2024, community births in the United States nearly doubled, with sustained increases in most racial and ethnic groups but only a temporary rise among non-Hispanic Black women. Patterns in birthplace clearly shifted during the COVID-19 pandemic, with increases seen across most groups, but the specific drivers remain uncertain. The persistence or decline of these trends beyond 2021 likely reflects multiple, overlapping factors that are difficult to disentangle.
Because out-of-hospital births are consistently associated with higher neonatal risks, fully informed consent is essential. Professional responsibility requires accurate disclosure of risks and alternatives, comprehension by the patient, and the opportunity for meaningful dialogue. It should lead to directive counseling, where clinicians recommend hospital delivery as the safest option while respecting patient autonomy.
Finally, continued access to reliable data is important. The CDC natality database is a vital national source, but its continuity may be threatened by budgetary and organizational changes. Safeguarding this resource is important for public health surveillance and evidence-based guidance. Improving maternal and neonatal outcomes will require both strengthened informed decision-making and reforms in hospital-based care to reduce unnecessary interventions and ensure trust in hospital births.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: We used ChatGPT and Claude as LLM to improve sentences and grammar and create informed consent.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: On CDC website.
References
1. Grünebaum, A, McLeod-Sordjan, R, Bornstein, E, De Four Jones, M, Lewis, D, Chervenak, FA. Trends in racial and ethnic distribution of United States birthplaces 2016–2022. Am J Obstet Gynecol 2024;230:e12–13. https://doi.org/10.1016/j.ajog.2023.10.044.Search in Google Scholar PubMed
2. American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice. Planned home birth. Obstet Gynecol 2017;129:e117–22. https://doi.org/10.1097/AOG.0000000000002024.Search in Google Scholar PubMed
3. Grünebaum, A, McCullough, LB, Sapra, KJ, Arabin, B, Chervenak, FA. Planned home births: the need for additional contraindications. Am J Obstet Gynecol 2017;216:401.e1–e8. https://doi.org/10.1016/j.ajog.2017.01.012.Search in Google Scholar PubMed
4. Grünebaum, A, Bornstein, E, Katz, A, Chervenak, FA. Worsening risk profiles of out-of-hospital births during the COVID-19 pandemic. Am J Obstet Gynecol 2022;226:137–8. https://doi.org/10.1016/j.ajog.2021.11.1346.Search in Google Scholar PubMed PubMed Central
5. Grünebaum, A, McCullough, LB, Bornstein, E, Klein, R, Dudenhausen, JW, Chervenak, FA. Professionally responsible counseling about birth location during the COVID-19 pandemic. J Perinat Med 2020;48:450–2. https://doi.org/10.1515/jpm-2020-0183.Search in Google Scholar PubMed
6. Grünebaum, A, McCullough, LB, Chervenak, FA. Most intended home births in the United States are not low risk: 2016–2018. Am J Obstet Gynecol 2020;222:384–5. https://doi.org/10.1016/j.ajog.2019.11.1245.Search in Google Scholar PubMed
7. Grünebaum, A, McCullough, LB, Orosz, B, Chervenak, FA. Neonatal mortality in the United States is related to location of birth (hospital versus home) rather than the type of birth attendant. Am J Obstet Gynecol 2020;223:254.e1–e8. https://doi.org/10.1016/j.ajog.2020.01.045.Search in Google Scholar PubMed
8. Grünebaum, A, Bornstein, E, McLeod-Sordjan, R, Lewis, T, Wasden, S, Combs, A, et al.. The impact of birth settings on pregnancy outcomes in the United States. Am J Obstet Gynecol 2023;228:S965–76. https://doi.org/10.1016/j.ajog.2022.08.011.Search in Google Scholar PubMed
9. Scarf, VL, Rossiter, C, Vedam, S, Dahlen, HG, Ellwood, D, Forster, D, et al.. Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: a systematic review and meta-analysis. Midwifery 2018;62:240–55. https://doi.org/10.1016/j.midw.2018.03.024.Search in Google Scholar PubMed
10. Bovbjerg, ML, Cheyney, M, Caughey, AB, Jolles, D, Brown, J, Stapleton, J, et al.. Planned home births in the United States have outcomes comparable to planned birth center births for low-risk birthing individuals. Med Care 2024;62:820–9. https://doi.org/10.1097/MLR.0000000000002074.Search in Google Scholar PubMed PubMed Central
11. Grünebaum, A, McCullough, LB, Arabin, B, Brent, RL, Levene, MI, Chervenak, FA. Perinatal risks of planned home births in the United States. Am J Obstet Gynecol 2015;212:350.e1–e6. https://doi.org/10.1016/j.ajog.2014.10.021.Search in Google Scholar PubMed
12. Grünebaum, A, Chervenak, FA. Why do women choose home births. J Perinat Med 2024;52:575–85. https://doi.org/10.1515/jpm-2024-0175.Search in Google Scholar PubMed
13. Quattrocchi, P. Policies and practices on out-of-hospital birth: a review of qualitative studies in the time of coronavirus. Curr Sex Health Rep 2023;15:36–48. https://doi.org/10.1007/s11930-022-00354-7.Search in Google Scholar PubMed PubMed Central
14. Fontenot, J, Brigance, C, March, of D. Navigating geographical disparities: access to obstetric hospitals in maternity care deserts across the United States. BMC Pregnancy Childbirth 2024;24:365. https://doi.org/10.1186/s12884-024-06535-7.Search in Google Scholar PubMed PubMed Central
15. Kozhimannil, KB, Interrante, JD, Henning-Smith, C, Admon, LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–2015. Health Aff (Millwood) 2019;38:2077–85. https://doi.org/10.1377/hlthaff.2019.00805.Search in Google Scholar PubMed
16. Hung, P, Henning-Smith, CE, Casey, MM, Kozhimannil, KB. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004–14. Health Aff (Millwood) 2017;36:1663–71. https://doi.org/10.1377/hlthaff.2017.0338.Search in Google Scholar PubMed
17. Offerhaus, PM, de Jonge, A, van der Pal-de Bruin, KM. Change in place of birth in the Netherlands: from home to hospital, between 2000 and 2008. Midwifery 2014;30:345–51. https://doi.org/10.1016/j.midw.2013.06.013.Search in Google Scholar PubMed
18. American College of Obstetricians and Gynecologists. Informed consent and shared decision making in obstetrics and gynecology. Committee Opinion No. 819. Obstet Gynecol 2021;137:e34–1. https://doi.org/10.1097/AOG.0000000000004247.Search in Google Scholar PubMed
19. McCullough, LB, Chervenak, FA. Ethics in obstetrics and gynecology. New York: Oxford University Press; 1994.Search in Google Scholar
20. Chervenak, FA, McCullough, LB, Brent, RL. The professional responsibility model of obstetrical ethics: avoiding the perils of clashing rights. Am J Obstet Gynecol 2011;205:315.e1–e5. https://doi.org/10.1016/j.ajog.2011.06.006.Search in Google Scholar PubMed
21. Ely, DM, Driscoll, AK. Infant mortality in the United States, 2020: data from the period linked birth/infant death file. Natl Vital Stat Rep 2022;71:1–25.10.15620/cdc:111053Search in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.


