Abstract
Objectives
The rate of cesarean delivery (CD) in Qatar is rising at an alarming rate. Vaginal birth after cesarean section (VBAC) is associated with lower maternal morbidity and is an important option for younger mothers. This study compared the pregnancy outcomes of second pregnancies in women with prior CD, according to their age groups, with the aim of individualising VBAC counselling.
Methods
This retrospective study divided women in their second pregnancies based on age: young group (YG<25 years), control group (CG, 25–35 years), and advanced age group (AG>35 years). The primary outcome was the mode of delivery.
Results
Out of 2,729 women, 18.2 % had a VBAC (27.4 % in YG vs. 9.5 % in AG). Nearly 48 % agreed to a TOLAC (57.9 % in YG and 41.8 % in AG), 38 % of whom had a successful VBAC. Among those who opted for TOLAC, 47.3 % in YG had a successful VBAC, compared to only 22.8 % in AG (p<0.001). While hypertension, diabetes, macrosomia and preterm birth reduced VBAC, postdated and uncomplicated pregnancies increased the rates. Compared to CG, YG had 35 % lower odds of repeat CD (aOR=0.64, CI=0.49–0.85, p=0.002), while AG had nearly two times higher odds (CI=1.26–2.95, p=0.003), after adjusting for confounders.
Conclusions
Maternal age emerged as an important predictor of repeat cesarean, with younger mothers having a much higher chance of successful VBAC. More than half with uncomplicated pregnancies opted for an elective CD, highlighting the requirement for improving counselling services that motivate women to take up VBAC and improve their confidence in the healthcare system.
Introduction
Owing to changing demographics of pregnant women and increased perception of an easy and safe delivery, the prevalence of cesarean deliveries (CD) worldwide has increased steadily to nearly 21 % of all births, and is expected to rise further over the next decade [1]. The rates range from as low as 8–9% in Sub-Saharan Africa to as high as 40–50 % in Latin America. Qatar has seen a similar trend, with current local data suggesting that more than one-third of births are CDs [2], 3]. Nearly 60 % of them are repeat CDs [4], the main contributor to the worldwide increase [5]. CDs, more specifically repeat CDs, are associated with higher maternal morbidity, including surgical complications, infections, requirement for blood transfusions, longer hospital stay, thrombosis and future pregnancy concerns such as adherent placenta [4], 6].
In countries of the Middle East, early marriages and subsequently early childbearing are considered societal norms. As per national statistics, nearly twice as many Qatari women are aged<25 years in their first pregnancy compared to other nationalities residing in the country [7]. Early conception, combined with the expectation of having larger families, places them at a higher risk of repeat CDs and their consequences [8]. A trial of labour after cesarean (TOLAC) and successful vaginal birth after cesarean (VBAC) hold significant importance in these young mothers, to reduce maternal morbidity and mortality associated with the potential multiple cesareans [9] over their longer reproductive lives. Fortunately, studies indicate that younger women are more likely to have successful VBACs compared to older women, in part owing to a higher incidence of comorbidities such as hypertension, diabetes, and obesity in older women, complicating pregnancy and labour, and making a repeat CD a safer option [10], [11], [12].
A large proportion of repeat CDs are not medically indicated [9] and maternal preferences play a major role in this choice. Advice from healthcare professionals, maternal perception of safety in undergoing a repeat CD due to lack of awareness about operative complications, and previous traumatic deliveries tend to influence decision-making [12], 13]. While in older mothers, the choice is considerably affected by comorbidities, younger mothers can be motivated to opt for TOLAC with evidence-based counselling by motivated healthcare professionals, especially in those who have yet to experience a vaginal birth. Studies exploring the impact of age on TOLAC decisions in the region, particularly in Qatar, are lacking. This study compares the pregnancy outcomes of second pregnancies in women with a prior CD, according to their age groups, with the aim of individualising VBAC counselling and subsequently encouraging younger mothers to choose a trial of labour.
Subjects and methods
Study design
A population‐based retrospective cohort study was conducted among women delivering in the secondary and tertiary care maternity centres in Qatar between January 2017 and April 2018. The study utilised data from a maternity registry, including all deliveries over the study period, to investigate outcomes among women in their second pregnancies who had previously undergone cesarean delivery (CD). The study was approved by the Medical Research Centre, Hamad Medical Corporation (MRC‐01‐24‐012) and was exempt from informed consent, since only existing data extracted from patient electronic health records was used.
Study participants
All women in their second viable pregnancies were eligible for inclusion in the study. Those with a previous CD who had antenatal care in government settings, and had a singleton, viable birth of ≥24 weeks gestational age (GA) were included in the study. The participants were divided into exposure groups based on their age at the time of delivery: young age group, YG (<25 years), advanced age group, AG (>35 years), and those with an average age of 25–35 years being the control group (CG), based on definitions of young and advanced maternal age used commonly in obstetric research [11], 14]. The main outcome was the incidence of VBAC, defined as the proportion of women having vaginal births (entire cohort as denominator). Women with missing data in the main exposure and outcome variables were excluded from the analysis.
Data source and variables
The data used for analysis were extracted from the PEARL Peristat maternity registry, excluding all patient-identifying variables. The primary exposure variable was the maternal age at the time of delivery, recorded as a continuous variable in years and then categorised as mentioned. The outcome for adjusted analysis was the mode of delivery (MOD): VBAC vs. repeat CD (including elective and emergency CD for any indication). Those who did not have a planned CD were considered to have opted for TOLAC (VBAC success being number of women having VBAC in those opting for TOLAC). Additionally, women who initially chose for CD but presented in advanced labour and subsequently delivered vaginally were included in this group. Other demographic variables included maternal nationality, body mass index (BMI) at delivery in kg/m2-divided into normal, overweight and obesity categories according to the WHO classification of BMI [15], assisted reproductive technology (ART) for conception, maternal preexisting comorbidities, and location of antenatal care and delivery (central tertiary or peripheral secondary care). These variables were considered important confounders in the association between age and mode of delivery.
Other pregnancy outcomes of interest included gestational diabetes mellitus (GDM)- defined as an abnormal 75 gm glucose tolerance test, anytime between 16 and 32 weeks of gestation depending on the patient’s risk factors [16], gestational hypertension (GHT) defined as the occurrence of high blood pressure after 20 weeks of gestation, including preeclampsia (including severe forms that can involve maternal hepatic, renal, pulmonary and cerebral systems) or eclampsia [17], gestational age- GA at delivery-preterm birth (PTB) if GA<37 completed weeks and post-dated birth if GA>40 weeks, use of oxytocin in women having a successful VBAC [18], birthweight of the baby measured immediately after birth in grams-low birthweight- LBW if<2500 g, and macrosomia if≥4,000 g [19], small for gestation (SGA) based on birthweight centiles<10 % customised for maternal characteristics such as nationality, height, weight, biological sex and GA at delivery, and large for gestation (LGA) based on birthweight centiles≥90 % [20]. The impact of these pregnancy outcomes on MOD was explored to provide insight into the mediating factors between maternal age and MOD. A complicated pregnancy was defined as a pregnancy having any maternal preexisting or new-onset comorbidities or any pregnancy complications, including fetal growth concerns.
Statistical analysis
For the descriptive analysis, all continuous variables were reported as means with standard deviations (SD) or medians with interquartile ranges (IQR), depending on the distribution of the variable. The distributions were analysed using histograms and Shapiro-Wilk test for normality if appropriate. They were compared using One-way ANOVA for means or Kruskal-Wallis test for medians. Categorical variables were described as frequencies and percentages, with comparisons done using the Chi-Square test or Fisher’s exact test as appropriate. The maternal demographics and pregnancy outcomes variables, including MOD, were compared between the three age groups. Additionally, the MOD in women developing other pregnancy outcomes were explored using bar graphs. For descriptive analysis, MOD was divided into three groups- VBAC, emergency CD and elective CD.
The association between age categories and MOD was explored using logistic regression models, yielding crude odds ratios (OR) with 95 % confidence intervals (CI). The logistic regressions were run with no VBAC (or repeat CD including both elective and emergency) vs. VBAC, as the reference category. Variables such as maternal nationality, BMI, assisted conception, preexisting comorbidities and location of antenatal care and delivery were considered as potential confounders and adjusted for, in multivariable logistic regression models to obtain adjusted ORs, after testing for collinearity. The model parameters were represented as a nomogram, which provided a visual representation of the model and provided the probability of having a repeat CD based on the age categories and other covariates in the model. The regression models were repeated in those with a complicated pregnancy vs. uncomplicated pregnancy. A p-value of<0.05 was considered strong evidence against a null hypothesis of no difference between the groups. All analyses were performed using STATA statistical software, version 18 (StataCorp, College Station, TX: StataCorp LLC) [21].
Results
Descriptive analyses
Among the 2,729 women included, 321 belonged to YG, 273 in AG, and the remaining in CG, as shown in Figure 1. The mean age in YG and AG was 22.5 (±1.6) and 38.1 (±2.2) years, respectively, with the youngest mother being 16 years old and the oldest 50. A higher proportion of YG were Qatari, while more than half (55.7 %) in AG belonged to other non-Arab nationalities (Table 1). The mothers in AG had higher BMI, with nearly 62 % belonging to the obesity category. More than three times higher proportion had ART in AG. As expected with advancing age, all preexisting comorbidities, except asthma, were statistically significantly higher in the AG group. Nearly 60 % of all antenatal care was in the tertiary care centre, with lower proportions in YG choosing to attend secondary care facilities.
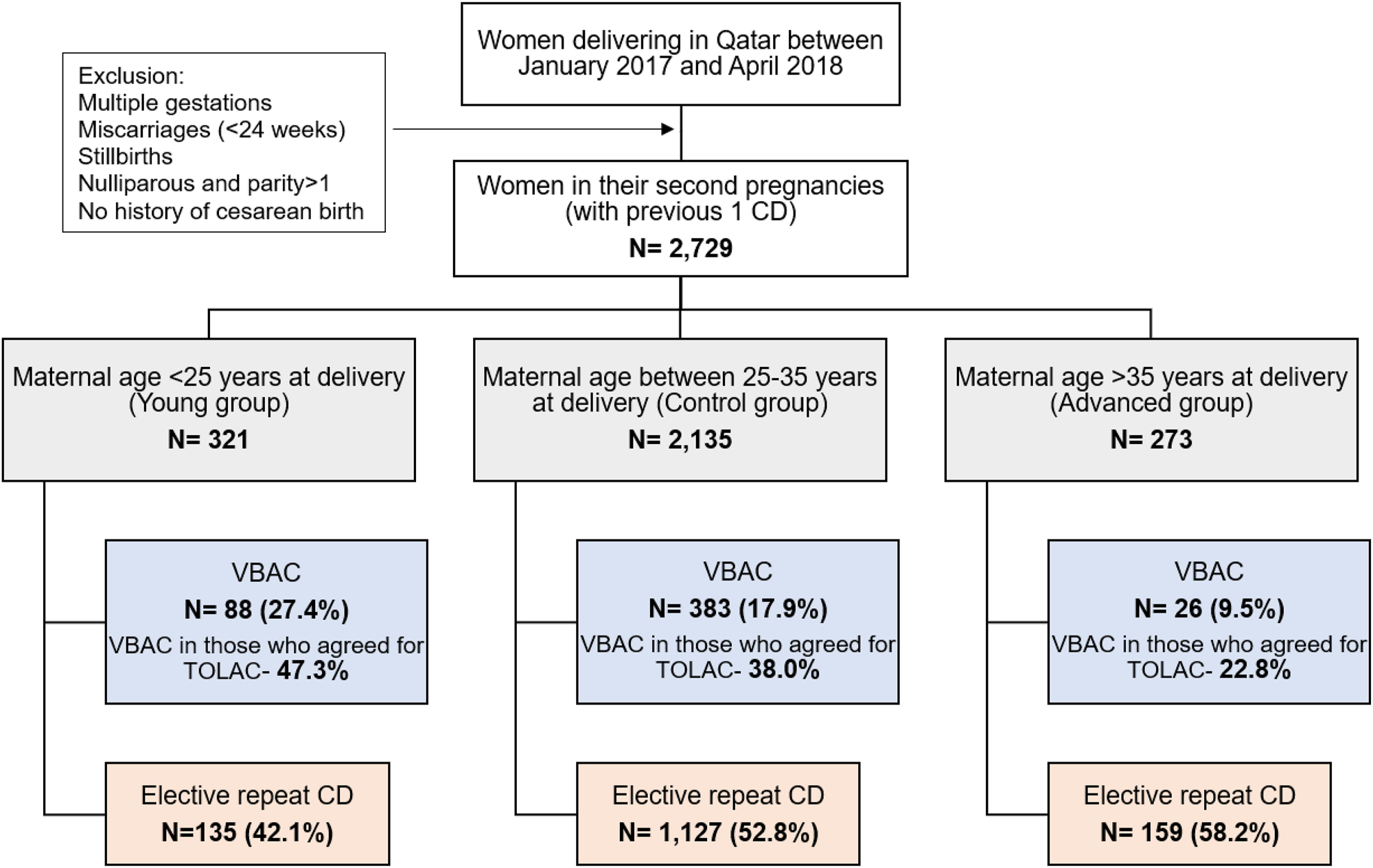
Study population and comparison groups; CD- Cesarean delivery, VBAC- vaginal birth after cesarean; TOLAC- trial of labour after cesarean.
Demographic variables in the three maternal age groups.
| Demographics total n=2,729 |
<25 Years (young) n=321 |
25–35 Years (control) n=2,135 |
>35 Years (advanced) n=273 |
p-Value | |
|---|---|---|---|---|---|
| Maternal age in years (mean ± SD) | 22.5 ± 1.6 | 29.6 ± 2.9 | 38.1 ± 2.2 | <0.001 | |
| Nationality, n, % | Qatari | 76 (23.7 %) | 258 (12.1 %) | 31 (11.4 %) | <0.001 |
| Arabs | 161 (50.2 %) | 929 (43.5 %) | 90 (33.0 %) | ||
| Other nationalities | 84 (26.2 %) | 948 (44.4 %) | 152 (55.7 %) | ||
| Maternal height in cm (mean ± SD) | 158.3 ± 6.0 | 158.9 ± 6.3 | 158.2 ± 6.5 | 0.058 | |
| Maternal weight at delivery in kg (mean ± SD) | 77.6 ± 14.4 | 80.3 ± 15.3 | 80.4 ± 15.0 | 0.012 | |
| Maternal BMI at delivery in kg/m2 (mean ± SD) | 31.0 ± 5.3 | 31.7 ± 5.5 | 32.1 ± 5.7 | 0.023 | |
| Maternal BMIa, n, % | Normal | 38 (11.8 %) | 177 (8.3 %) | 16 (5.9 %) | 0.025 |
| Overweight | 117 (36.5 %) | 695 (32.6 %) | 88 (32.2 %) | ||
| Obesity | 166 (51.7 %) | 1,262 (59.1 %) | 169 (61.9 %) | ||
| Assisted reproduction, n, % | 0 (0 %) | 43 (2.0 %) | 19 (7.0 %) | <0.001 | |
| GA at booking in weeks (median, IQR) | 21 (13–32) | 18 (11–29) | 17 (11–29) | 0.002 | |
| Maternal preexisting diabetes, n, % | 4 (1.3 %) | 53 (2.5 %) | 14 (5.1 %) | 0.009 | |
| Maternal chronic hypertension, n, % | 0 (0 %) | 19 (1.0 %) | 12 (4.4 %) | <0.001 | |
| Maternal thyroid disease, n, % | 13 (4.1 %) | 215 (10.1 %) | 37 (13.6 %) | <0.001 | |
| Maternal anemia, n, % | 44 (13.7 %) | 200 (9.4) | 22 (8.1 %) | 0.031 | |
| Maternal asthma, n, % | 6 (1.9 %) | 41 (1.9 %) | 2 (0.7 %) | 0.420 | |
| Antenatal care and delivery care provider | Tertiary care | 222 (69.2 %) | 1,212 (56.8 %) | 168 (61.5 %) | <0.001 |
| Secondary care 1 | 72 (22.4 %) | 703 (32.9 %) | 76 (27.8 %) | ||
| Secondary care 2 | 20 (6.2 %) | 150 (7.0 %) | 12 (4.4 %) | ||
| Secondary care 3 | 7 (2.2 %) | 70 (3.3 %) | 17 (6.2 %) | ||
-
SD, standard deviation; BMI, body mass index; GA, gestational age; IQR, interquartile range; WWRC, Women’s Wellness and Research Centre; Means compared using ANOVA; amissing data in BMI, 1; medians compared using Kruskal Wallis test; proportions compared using Chi-square/fishers test; bold font type-statistical significance at p<0.05.
Among YG, 27.4 % underwent a VBAC, compared to 17.9 % in CG and only 9.5 % in AG (p<0.001), the VBAC rate in the whole cohort being 18.2 % (Table 2). Nearly 48 % of the cohort agreed to a TOLAC (57.9 % in YG and 41.8 % in AG), 38 % of whom had a successful VBAC. Among those who opted for TOLAC, 47.3 % in YG had a successful VBAC, compared to only 22.8 % in AG (p<0.001). Nearly 58 % of AG chose to have an elective repeat CD, compared to 42.1 % in YG and 52.8 % in the controls.
Pregnancy outcomes in the three maternal age groups.
| Pregnancy outcomes total n=2,729 |
<25 Years (young) n=321 |
25–35 Years (control) n=2,135 |
>35 Years (advanced) n=273 |
p-Value | |
|---|---|---|---|---|---|
| Gestational diabetes, n, % | 64 (20.2 %) | 659 (31.7 %) | 109 (42.1 %) | <0.001 | |
| Pregnancy-induced hypertension, n, % | 4 (1.3 %) | 78 (3.7 %) | 18 (6.6 %) | 0.003 | |
| GA at delivery in completed weeks (median, IQR) | 39 (38–40) | 39 (38–39) | 39 (38–39) | 0.010 | |
| Preterm birth (<37 weeks), n, % | 26 (8.1 %) | 155 (7.3 %) | 25 (9.2 %) | 0.495 | |
| Post-dated birth (>40 weeks), n, % | 22 (6.9 %) | 118 (5.5 %) | 15 (5.5 %) | 0.626 | |
| Mode of delivery, n, % | Vaginal birth (VBAC) | 88 (27.4 %) | 383 (17.9 %) | 26 (9.5 %) | <0.001 |
| Emergency cesarean | 98 (30.5 %) | 625 (29.3 %) | 88 (32.2 %) | ||
| Elective planned cesarean | 135 (42.1 %) | 1,127 (52.8 %) | 159 (58.2 %) | ||
| Women going into active labour, for TOLAC, n, % | 186 (57.9 %) | 1,008 (47.2 %) | 114 (41.8 %) | <0.001 | |
| Vaginal birth among those going into active labour (successful VBAC), n, % | 88 (47.3 %) | 383 (38.0 %) | 26 (22.8 %) | <0.001 | |
| Use of oxytocin in those having vaginal birth | 15 (17.1 %) | 63 (16.5 %) | 5 (19.2 %) | 0.930 | |
| Birth weight in grams (mean ± SD) | 3,212 ± 529 | 3,271 ± 519 | 3,206 ± 639 | 0.043 | |
| Low birth weight (<2,500 g), n, % | 23 (7.2 %) | 141 (6.6 %) | 24 (8.8 %) | 0.397 | |
| Small for date baby as per customised birthweight centiles <10 %, n, % | 42 (13.1 %) | 214 (10.0 %) | 34 (12.5 %) | 0.148 | |
| Macrosomia at birth (>4,000 g), n, % | 16 (5.0 %) | 135 (6.3 %) | 19 (7.0 %) | 0.567 | |
| Large for date baby as per customised birthweight centiles ≥90 %, n, % | 38 (11.8 %) | 320 (15.0 %) | 39 (14.3 %) | 0.326 | |
| Uncomplicated pregnancy (no comorbidities or other pregnancy complications) | 134 (41.7 %) | 744 (34.9 %) | 74 (27.1 %) | 0.001 | |
-
SD, standard deviation; GA, gestational age; TOLAC, trial of labour after cesarean delivery; VBAC, vaginal birth after cesarean; NICU, neonatal intensive care unit; means compared using ANOVA; medians compared using Kruskal Wallis test; proportions compared using Chi-square/fishers test; bold font type-statistical significance at p<0.05.
While 42.1 % in AG had GDM compared to only 20 % in YG (p<0.001), nearly 7 % in AG had PIH compared to only 1.3 % in YG (p=0.003). There were no clinically relevant differences in the incidence of preterm, post-dated births or SFD. Similarly, there were no statistically significant differences in the incidence of LFD, LBW or macrosomia. Nearly 42 % of YG had an uncomplicated pregnancy compared to only 27 % in AG (p=0.001).
The chances of having a successful VBAC were reduced in those having PIH (only 4 %), with a macrosomic or LFD baby (10–12 %), having GDD (13.7 %) or preterm birth (15.5 %), compared to 22.9 % in those who had an uncomplicated pregnancy (Figure 2). In contrast, having a baby with SFD and post-dated pregnancy increased the chances compared to the VBAC rate in the overall cohort. The proportion of women having emergency CD was highest (68 %) in those having a preterm birth, followed by PIH (52 %). Interestingly, 51 % of the whole cohort with an uncomplicated pregnancy chose to have an elective CD. When evaluating the impact of age groups in uncomplicated pregnancies, the VBAC success rates reached 60 % in YG, compared to 29 % in AG (Figure 3).
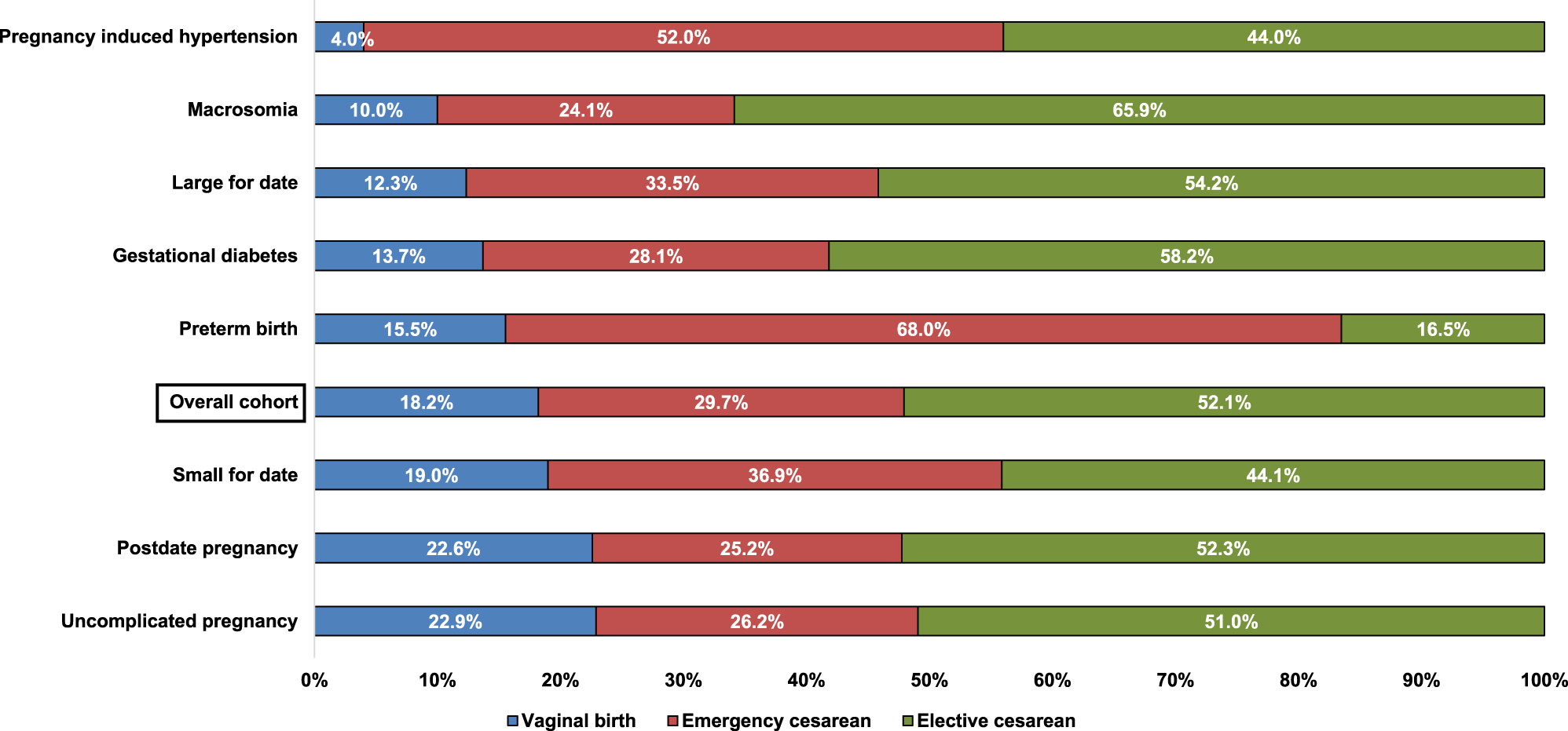
Proportion of women delivering vaginally or by cesarean delivery in each of the pregnancy complication groups compared to the overall cohort and women with uncomplicated pregnancies.
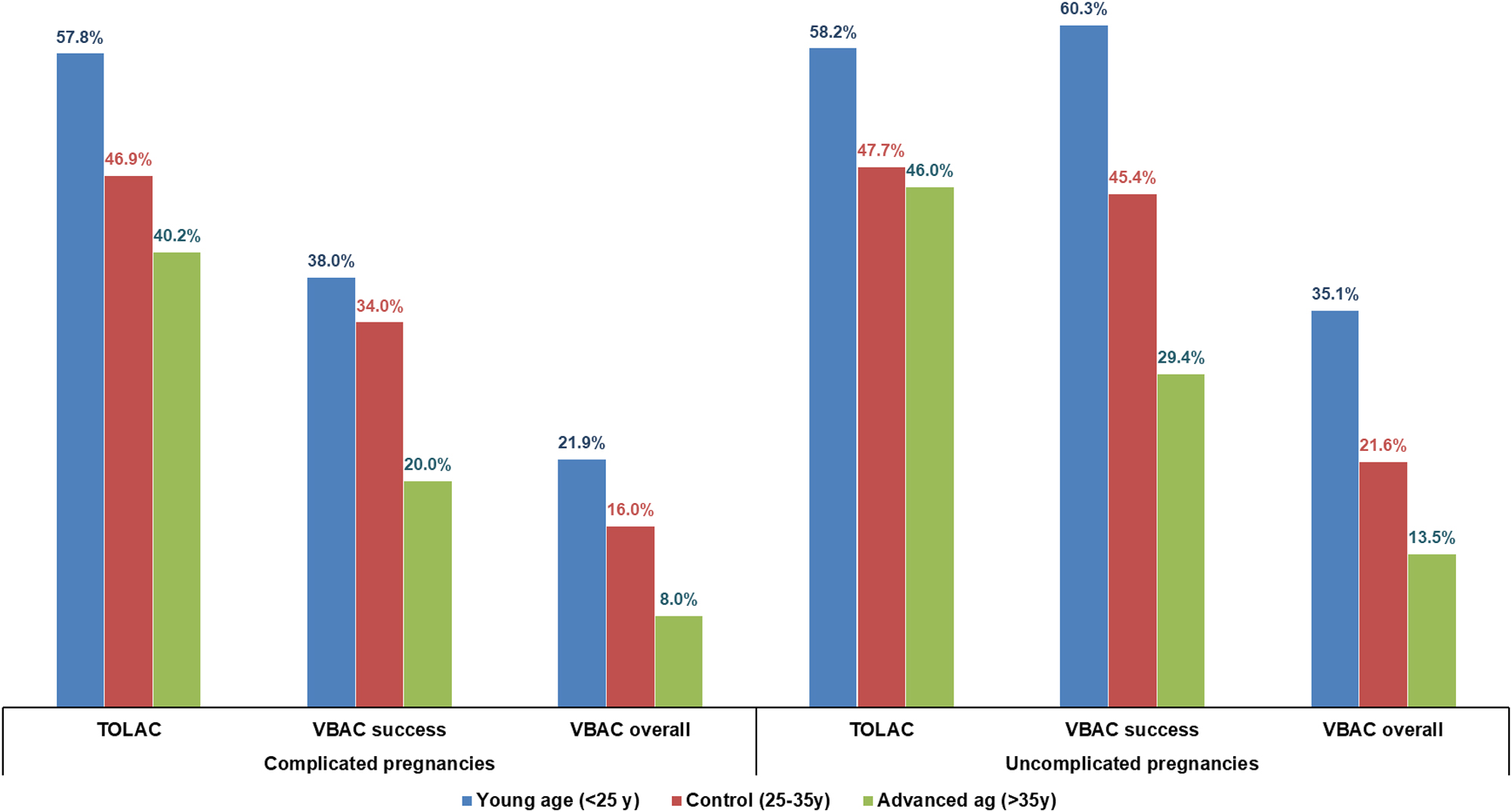
Comparison of TOLAC, VBAC success and VBAC rates in the age groups in complicated vs. uncomplicated pregnancies.
Measures of association between age categories and MOD
Compared to the control group, YG had 43 % lower odds of having a repeat CD (crude OR=0.57, 95 % CI=0.44–0.76, p<0.001), while AG had nearly 2.1 times higher odds (crude OR=2.08, CI=1.37–3.16, p=0.001). After adjustment for confounders (Table 3), the magnitude and direction of the association remained roughly the same (aOR=0.65, CI=0.49–0.85, p=0.002; aOR=1.93, CI=1.26–2.95, p=0.003, respectively).
Association between covariates and mode of delivery (repeat CD vs. vaginal), with crude and adjusted odds ratios.
| Covariates | Vaginal birth (baseline) | Repeat CD | Crude OR (95 % CI) | p-Value | Adjusted OR (95 % CI) | p-Value | |
|---|---|---|---|---|---|---|---|
| Maternal age groups | Group 1 (young group) | 88 (27.4 %) | 233 (72.6 %) | 0.57 (0.44–0.76) | <0.001 | 0.64 (0.49–0.85) | 0.002 |
| Group 2 (control group) | 383 (17.9 %) | 1,752 (82.1 %) | Reference | – | Reference | – | |
| Group 3 (advanced group) | 26 (9.5 %) | 247 (90.5 %) | 2.08 (1.37–3.16) | 0.001 | 1.93 (1.26–2.95) | 0.003 | |
| Maternal BMI | Normal | 54 (23.4 %) | 177 (76.6 %) | Reference | – | Reference | – |
| Overweight | 216 (24.0 %) | 684 (76.0 %) | 0.97 (0.69–1.36) | 0.843 | 0.98 (0.69–1.38) | 0.891 | |
| Obese | 227 (14.2 %) | 1,370 (85.8 %) | 1.84 (1.32–2.58) | <0.001 | 1.88 (1.33–2.64) | <0.001 | |
| Nationality | Qatari | 71 (19.5 %) | 294 (80.6 %) | Reference | – | Reference | – |
| Arabs | 227 (19.2 %) | 953 (80.8 %) | 1.01 (0.75–1.36) | 0.928 | 0.90 (0.66–1.23) | 0.510 | |
| Other nationalities | 199 (16.8 %) | 985 (83.2 %) | 1.20 (0.88–1.61) | 0.245 | 1.00 (0.72–1.39) | 0.992 | |
| Conception | Spontaneous | 491 (18.4 %) | 2,176 (81.6 %) | Reference | – | Reference | – |
| Assisted reproduction | 6 (9.7 %) | 56 (90.3 %) | 2.11 (0.90–4.92) | 0.085 | 1.66 (0.70–3.95) | 0.248 | |
| Antenatal care and delivery care provider | Tertiary | 321 (20.0 %) | 1,281 (80.0 %) | Reference | – | Reference | – |
| Secondary care 1 | 134 (15.8 %) | 717 (84.3 %) | 1.34 (1.07–1.67) | 0.009 | 1.37 (1.09–1.73) | 0.008 | |
| Secondary care 2 | 35 (19.2 %) | 147 (80.8 %) | 1.05 (0.71–1.55) | 0.796 | 1.08 (0.72–1.61) | 0.708 | |
| Secondary care 3 | 7 (7.5 %) | 87 (92.6 %) | 3.11 (1.43–6.79) | 0.004 | 3.23 (1.46–7.11) | 0.004 | |
| Preexisting diabetes | No | 492 (18.5 %) | 2,166 (81.5 %) | Reference | – | Reference | – |
| Yes | 5 (7.0 %) | 66 (93.0 %) | 3.00 (1.20–7.48) | 0.019 | 2.58 (1.03–6.51) | 0.044 | |
| Chronic hypertension | No | 495 (18.6 %) | 2,203 (81.7 %) | Reference | – | Reference | – |
| Yes | 2 (6.5 %) | 29 (93.6 %) | 3.26 (0.77–13.70) | 0.107 | 2.08 (0.48–8.92) | 0.326 | |
| Anemia | No | 457 (18.6 %) | 2,006 (81.5 %) | Reference | – | Reference | – |
| Yes | 40 (15.0 %) | 226 (85.0 %) | 1.29 (0.91–1.83) | 0.159 | 1.43 (1.00–2.05) | 0.050 | |
| Thyroid | No | 458 (18.6 %) | 2,006 (81.4 %) | Reference | – | Reference | – |
| Yes | 39 (14.7 %) | 226 (85.3 %) | 1.32 (0.93–1.89) | 0.122 | 1.15 (0.80–1.66) | 0.426 | |
-
BMI, body mass index; CD, cesarean delivery; OR, odds ratio; CI, confidence intervals; ORs obtained from logistic regression models (vaginal birth – reference group); adjusted ORs obtained after adjusting for every other variable in the table; p<0.05 considered statistically significant. The text in bold represents the estimates for maternal age (main exposure) and all other significant p-values.
In the multivariable model, among the medical illnesses, preexisting diabetes and maternal anaemia increased the odds of CD (aOR=2.58, CI=1.03–6.51, p=0.044; aOR=1.43, CI=1.00–2.05, p=0.050, respectively). Maternal essential hypertension also doubled the odds, although was non-significant. Obesity nearly doubled the odds of CD (aOR=1.88, CI=1.33–2.64, p<0.001). Interestingly, antenatal care in the secondary care hospitals increased the odds more than three times compared to the central tertiary centre (aOR=3.23, CI=1.46–7.11, p=0.004).
The multivariable model was visually represented in the nomogram shown in Figure 4. Apart from the care location, maternal age categories had the most impact on the probability of having a repeat CD, specifically the AG group, followed by preexisting diabetes, hypertension, and maternal BMI (presence of any of the above giving a score of atleast 5/10). The visual representation of the model provided an easy assessment of the risk of CD based on the included factors. For example, a woman in the AG group, with preexisting diabetes, in the obese category will have at least 95 % probability of having a CD (total score of 23.2).
As shown in Table 4, in complicated pregnancies, YG had a non-significant 29 % reduced odds of repeat CD, whereas AG had more than double the odds (aOR=2.07, CI=1.21–3.54; p=0.008). Interestingly, in uncomplicated pregnancies, the VBAC rate was 35.1 % compared to only 13.5 % in AG, and the reduced odds of CD in YG remained statistically significant (aOR=0.59, CI=0.39–0.88; p=0.010).
Association between covariates and mode of delivery (repeat CD vs. vaginal), with crude and adjusted odds ratios in complicated vs. uncomplicated pregnancies.
| Covariates |
|
Vaginal birth (baseline) |
Repeat CD |
Crude OR (95 % CI) |
p-Value |
Adjusted OR (95 % CI) |
p-Value |
|---|---|---|---|---|---|---|---|
| Complicated pregnancies (with any pregnancy complications or preexisting comorbidities) | |||||||
| Maternal age groups | Group 1 (young group) | 41 (21.9 %) | 146 (78.1 %) | 0.68 (0.46–0.98) | 0.041 | 0.71 (0.49–1.04) | 0.082 |
| Group 2 (control group) | 222 (16.0 %) | 1,169 (84.0 %) | Reference | – | Reference | – | |
| Group 3 (advanced group) | 16 (8.0 %) | 183 (92.0 %) | 2.17 (1.28–3.69) | 0.004 | 2.07 (1.21–3.54) | 0.008 | |
|
|
|||||||
| Uncomplicated pregnancies (no pregnancy complications or preexisting comorbidities) | |||||||
|
|
|||||||
| Maternal age groups | Group 1 (young group) | 47 (35.1 %) | 87 (64.9 %) | 0.51 (0.34–0.76) | 0.001 | 0.59 (0.39–0.88) | 0.010 |
| Group 2 (control group) | 161 (21.6 %) | 583 (78.4 %) | Reference | – | Reference | – | |
| Group 3 (advanced group) | 10 (13.5 %) | 64 (86.5 %) | 1.77 (0.89–3.52) | 0.105 | 1.66 (0.83–3.34) | 0.152 | |
-
CD, cesarean delivery; OR, odds ratio; CI, confidence intervals; ORs obtained from logistic regression models (vaginal birth – baseline group); adjusted ORs obtained after adjusting for BMI, nationality, assisted reproduction and antenatal care provider; p<0.05 considered statistically significant. The text in bold represents the estimates for maternal age (main exposure) and all other significant p-values.
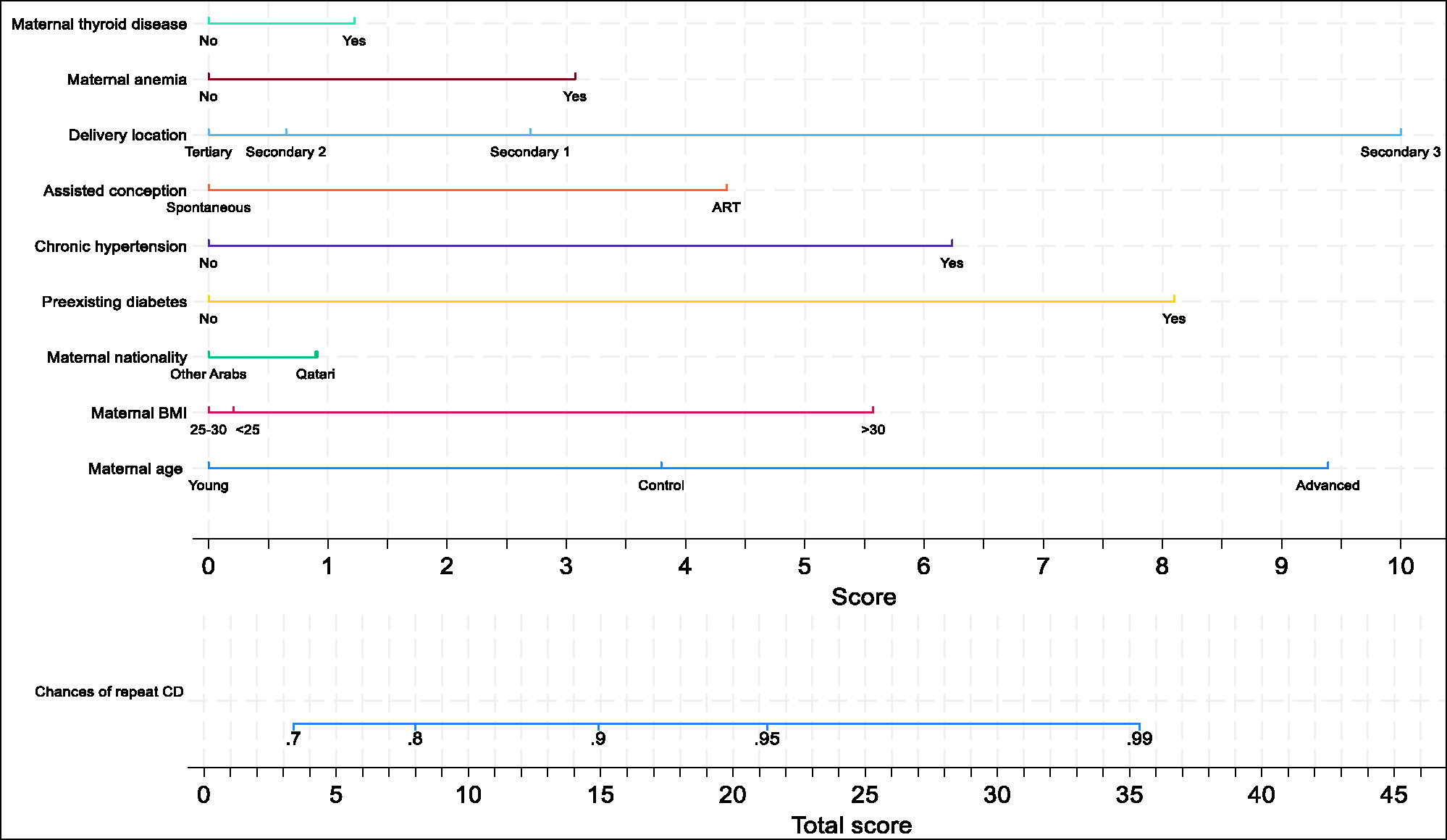
Nomogram showing the probability of having a repeat cesarean delivery based on the covariates included in the adjusted logistic regression model shown in Table 2; ART- assisted reproduction techniques; CD- cesarean delivery.
Discussion
Summary of main findings
The results of this study demonstrate an association between extremes of maternal age and mode of delivery after cesarean. Nearly three times higher proportion of younger women had a successful VBAC compared to those in the advanced age group. After adjusting for potential confounders, older women nearly doubled their odds of having a repeat CD. Complications occurring during pregnancy, such as GDM, PIH and larger birthweight, were detrimental towards VBAC rates and were also observed to be higher in older mothers. Despite having fewer complications during pregnancy and a VBAC success rate reaching 60 % in uncomplicated pregnancies, more than two-fifths of younger mothers opted for an elective CD, exposing them to the morbidity associated with future higher-order repeat CDs.
Interpretation of results and comparison with previous literature
Recommendations regarding offering VBAC emerged in the 1980s, as a means of controlling the rates of repeat CDs. Although initially popular, increased incidence of complications and the associated legal implications have reduced the rates [9]. Clinician and patient perspectives regarding TOLAC vary worldwide, resulting in a wide variation in VBAC rates. The definitions also play a part in the disparity, as VBAC rates consider the proportion of vaginal births in the entire cohort of women with previous cesarean (as endorsed by the American College of Obstetricians and Gynecologists, ACOG), whereas VBAC success considers the same, but among those who opted for a TOLAC [22]. Additionally, VBAC attempt rates have also been reported, referring to the proportion of women opting for TOLAC among the total cohort [22], 23]. For example, a large cohort study from UK in 2013 reported a VBAC incidence of 33 % in women in their second pregnancies similar to our study; however, 52.2 % opted for TOLAC, among whom 63.4 % had a successful VBAC [24].
Other European countries, such as Ireland, Italy and Germany, report high VBAC success rates reaching 75–80 %; however, these numbers included women with previous vaginal births [25]. Finland, Sweden, and the Netherlands similarly report TOLAC rates between 45 and 55 %, contrasting with 10–12 % in the USA and Australia [23]. A study comparing a 10-group CD classification system between Norway, Ireland and Slovenia report VBAC rates of 54 %, 39%, 25 % respectively, including all women with previous cesarean and singleton term births [26]. Countries of the Middle East, such as Saudi Arabia report VBAC success rate above 70 % in women without prior vaginal births [27], 28]. In our study consisting of women with no prior vaginal births, nearly 48 % opted for TOLAC, with 38 % being successful (overall VBAC incidence- 18.2 %). The concern is that more than half of the women with uncomplicated pregnancies were still choosing to have elective CDs-representing the challenging path ahead towards addressing patient concerns and improving physician confidence and counselling regarding TOLAC.
The physiological impact of advanced age on vaginal birth has been explored in several studies, attributing the higher risk of labour dystocia and CD to intrapartum decreased myometrial function, uterine blood flow and function of oxytocin receptors [29] in older mothers. Additionally, higher comorbidities such as higher BMI, preexisting diabetes and pregnancy complications such as hypertensive disorders, growth restriction and requirement for early induction of labour in them impact delivery choices, often favouring CD, perceived to be the easy and safe option [30]. These factors obviously impact TOLAC and VBAC rates, as evidenced in our study. However, what is striking is that 54 % of AG mothers with uncomplicated pregnancies opted for elective CD. This could be because majority of AG were expatriates of other nationalities, not hoping for larger families [2], biased towards CD, and who are likely to have an undocumented prior CD of unclear indication that can influence physician acceptance of VBAC.
Although there is scope for improving acceptance of VBAC in older mothers, our study results show that the other extreme age group (YG) is the key to improving the VBAC rates, especially since the VBAC success in this group goes up to 60 % in uncomplicated pregnancies, similar to the success rates in several European countries [24], 25]. Plenty of existing literature emphasises the role of age in TOLAC uptake and VBAC, with prediction models (including the validated Grobman calculator) suggesting nearly 15–20 % reduction in VBAC success for every 5-year age increment [29], 31], in those opting for TOLAC. In our study, we demonstrate a nearly 60 % reduction in VBAC success in AG when directly comparing to YG. Our nomogram also demonstrates that among the predictors included in the model, maternal age contributes most towards increasing the probability of repeat CD in this cohort. The difference noted reflects the fact that we have analysed a specific group who have not delivered vaginally prior.
The concern is that young mothers, especially those starting their reproductive journey just after adolescence, have a longer journey ahead. A larger proportion of nationals belong to this age group, and they need to satisfy the societal expectations of having larger families. Opting for repeat CD simply increases the likelihood of undergoing multiple repeat cesarean deliveries, without any striking benefit over a successful VBAC in those with no clinical contraindications. Fetal morbidity is very low in VBAC, comparable to that of nulliparous delivery, and the incidence of uterine rupture is rare [32]. Repeat CDs carry risks such as morbidly adherent placenta, adhesions, and surgical complications, which increase with each additional cesarean [4], 9]. Promoting VBAC in younger women helps reduce these risks, preserves future fertility and reduces the likelihood of severe complications in future pregnancies. Successful VBACs also result in shorter recovery times, lower infection rates, and fewer long-term health issues such as chronic pain or surgical complications from adhesions [33]. It is also the single most important predictor influencing future VBAC chances [31]. Effective counselling in this age group must include an unbiased discussion of current and future consequences of both MODs, while exploring the underlying reasons for not opting for TOLAC. The results from our study will provide valuable improvements to patient counselling by individualising the risks according to patient characteristics.
A systematic review exploring maternal perspectives and barriers against VBAC choice reported that apart from fear of risk for the baby, pregnant women felt that inconsistent and incomplete information about the choices from healthcare professionals along with coercive counselling favouring CD contributed to their confidence in TOLAC [34]. A similar evaluation of patient perspectives in Saudi Arabia revealed fear for the baby and recommendation of a CD being the top choices for mothers refusing VBAC [13]. This highlights the importance of our study as results from the local population will equip healthcare professionals with adequate and accurate information about risks and benefits, and provide better support and confidence to these mothers. Awareness about the influence of pregnancy factors on VBAC rate can help mothers and physicians proactively manage complications such as diabetes and macrosomia, and delay delivery up to 40 weeks or beyond in uncomplicated pregnancies to enhance success rates.
Exploration of physicians’ and midwives’ perspectives revealed differences in attitudes towards VBAC, ranging from positive in terms of lower risk and cost benefit to negative in terms of adverse outcomes such as uterine rupture [35]. The review suggests that in countries with higher success rates, main decision-making is from the physicians’, whereas in countries with lower rates, maternal decision-making is more assertive. A thorough dynamic risk assessment is required in YG, motivating them to take up VBAC from early pregnancy. Along with this, a positive mindset and confidence from a strong organisational support need to be demonstrated by counselling physicians or midwives, preferably trained and well-educated about factors influencing VBAC in the local population. Our study shows higher odds of repeat CD in peripheral secondary care hospitals compared to tertiary care, which highlights the confidence imparted by the availability of expertise. Younger mothers might advocate for a planned controlled CD that might allow them to manage work or study and family commitments. However, it is the responsibility of counselling professionals to encourage them to think long-term, beyond immediate social considerations and provide reassurance about expertise and healthcare resources available in the country.
Strengths and limitations
This is the first study from the region that explores the impact of age on choice and success of VBAC. It includes a substantial sample of 2,729 women, taken from a comprehensive maternity registry. The sample is therefore representative of this specific population in the country, and the results are generalizable. The categorisation of participants into three distinct age groups is based on widely accepted cutoffs and allows for valid comparisons with previous studies. Another unique advantage is that the multiethnic residential population in Qatar allows for comparison between women from different nationalities and Qatari citizens.
Since the maternal age is calculated from the date of birth recorded in participants’ national information, there is very little possibility of misclassification of exposure. Similarly, the mode of delivery is an absolute objective outcome variable that is very unlikely to be misclassified, thereby reducing any measurement bias. Adjusting for confounding variables such as maternal BMI, nationality, delivery hospital, and preexisting comorbidities strengthens the validity of the results by isolating the effect of maternal age on VBAC success. The study’s outcome variables are directly relevant to clinical decision-making and maternal health, providing actionable insights for healthcare providers.
Being a retrospective study, it is limited by potential biases in data collection and the accuracy of the medical records. Prospective studies could provide more controlled and precise data. The study is conducted in Qatar, and while it provides valuable insights, the findings may not be entirely generalizable to other countries with different healthcare systems and demographic profiles. Despite adjusting for several important confounders, there may still be unmeasured confounders that could affect the results, such as socio-economic status or indications for the initial CD. Exploration of reasons for the choice of repeat CD is lacking, and further qualitative studies will provide more insight. Future prospective studies could provide more definitive evidence and help refine VBAC guidelines and recommendations for different age groups.
Conclusions
In women with a previous CD in their second pregnancies, 18.2 % had a successful vaginal birth. Maternal age emerged as an important predictor of repeat cesarean, with younger mothers having a much higher chance of successful VBAC and older mothers having nearly double the odds of CD compared to the control group. Notably, in pregnancies uncomplicated by comorbidities or pregnancy complications, the VBAC rate nearly doubled to 35 %, with almost 60 % of those choosing a trial of labour successfully delivering vaginally. However, more than 50 % women with uncomplicated pregnancies opted for an elective CD, highlighting the requirement for improving counselling services that motivate women to take up VBAC and improve their confidence in the healthcare system. The results can help individualise risk assessment and counselling according to patient characteristics and risk factors, thereby improving TOLAC uptake and ultimately reducing repeat CD rates.
Acknowledgments
We would like to acknowledge the members of the PEARL Peristat registry group (Dr Sawsan Al Obaidly, Dr Husam Salama, Dr Mai Al Qubaisi and data collection team) for the dataset used for this study.
-
Research ethics: The study was approved by the Medical Research Centre, Hamad Medical Corporation (MRC‐01‐24‐012) and was exempt from informed consent, since only existing data extracted from patient electronic health records was used.
-
Informed consent: Not applicable.
-
Author contributions: MS, FM and TF conceptualized the study and applied for ethical approval. SAY, NAD and TF provided departmental support for conducting the study and helped ensure the availability of data. FM and TF were involved in the data analysis and interpretation of the results. MS and FM prepared the initial draft, which was later reviewed by SAY, NAD and TF. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The data that support the findings of this study are available on request from the corresponding author, [FM]. The data is not publicly available due to privacy/ethical institutional restrictions.
References
1. World Health Organization. Caesarean section rates continue to rise, amid growing inequalities in access [internet]. [cited 2025 Jul 23]. Available from: https://www.who.int/news/item/16-06-2021-caesarean-section-rates-continue-to-rise-amid-growing-inequalities-in-access.Search in Google Scholar
2. Shittu, S, Alansari, L, Nattouf, F, Olukade, T, Abdallah, N. Impact of maternal nationality on caesarean section rate variation in a high-income country. Qatar Med J 2021;2021:69. https://doi.org/10.5339/qmj.2021.69.Search in Google Scholar PubMed PubMed Central
3. Bashir, M, Abdel-Rahman M, E, Aboulfotouh, M, Eltaher, F, Omar, K, Babarinsa, I, et al.. Prevalence of newly detected diabetes in pregnancy in Qatar, using universal screening. PLoS One 2018;13:e0201247. https://doi.org/10.1371/journal.pone.0201247.Search in Google Scholar PubMed PubMed Central
4. Ajmal, S, Farrell, T, Minisha, F, Al Obaidly, S, AlQubaisi, M, Khenyab, N, et al.. Maternal and neonatal outcomes associated with multiple repeat cesarean deliveries: a registry-based study from Qatar. Qatar Med J 2024;2024:3. https://doi.org/10.5339/qmj.2024.3.Search in Google Scholar PubMed PubMed Central
5. Cheng, YW, Eden, KB, Marshall, N, Pereira, L, Caughey, AB, Guise, JM. Delivery after prior cesarean: maternal morbidity and mortality. Clin Perinatol 2011;38:297–309. https://doi.org/10.1016/j.clp.2011.03.012.Search in Google Scholar PubMed PubMed Central
6. Golandaj, JA, Kampli, MS, Kumar, M, Hallad, JS. Complications and implications of Caesarean delivery: facts and perceptions. Clinical Epidemiol Global Health 2024;29:101770. https://doi.org/10.1016/j.cegh.2024.101770.Search in Google Scholar
7. Registered Live Births by Mother’s Age Group and Birth Order – Total [Internet]. [cited 2025 Jul 23]. Available from: https://qatar.opendatasoft.com/explore/dataset/registered-live-births-by-mother-s-age-group-and-birth-order-total/.Search in Google Scholar
8. Rahman, MM, Al-Ghanim, K, Hossain, Z, Umar, S. Family research in the Arab Gulf States: an introduction. In: Handbook of Families in the Arab Gulf States [Internet], [cited 2025 Jul 23]. Singapore: Springer Nature Singapore; 2025:1–36 pp. Available from: https://library.oapen.org/bitstream/handle/20.500.12657/103590/9789819634125.pdf?sequence=1#page=18.10.1007/978-981-96-3412-5_1Search in Google Scholar
9. Practice Bulletin No. 184: Vaginal Birth After Cesarean Delivery. Obstet Gynecol 2017;130:e217–33.10.1097/AOG.0000000000002398Search in Google Scholar PubMed
10. Landon, MB, Hauth, JC, Leveno, KJ, Spong, CY, Leindecker, S, Varner, MW, et al.. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 2004;351:2581–9. https://doi.org/10.1056/nejmoa040405.Search in Google Scholar
11. Srinivas, SK, Stamilio, DM, Sammel, MD, Stevens, EJ, Peipert, JF, Odibo, AO, et al.. Vaginal birth after caesarean delivery: does maternal age affect safety and success? Paediatr Perinat Epidemiol 2007;21:114–20. https://doi.org/10.1111/j.1365-3016.2007.00794.x.Search in Google Scholar PubMed
12. Wu, Y, Kataria, Y, Wang, Z, Ming, WK, Ellervik, C. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth 2019;19:360. https://doi.org/10.1186/s12884-019-2517-y.Search in Google Scholar PubMed PubMed Central
13. Aloufi, D, Saggaf, O, Alkhalifah, ZA, Alalawi, H, Alhazmi, N. Exploring barriers and facilitators of vaginal birth after caesarean section (VBAC), awareness, and preferences among females in Western Saudi Arabia. J Fam Med Prim Care 2025;14:139. https://doi.org/10.4103/jfmpc.jfmpc-946-24.Search in Google Scholar
14. Esposito, G, Mauri, PA, Cipriani, S, Franchi, M, Corrao, G, Parazzini, F. The role of maternal age on the risk of preterm birth among singletons and multiples: a retrospective cohort study in Lombardy, Norther Italy. BMC Pregnancy Childbirth 2022;22:234. https://doi.org/10.1186/s12884-022-04552-y.Search in Google Scholar PubMed PubMed Central
15. Malnutrition in women [Internet]. [cited 2025 Jul 24]. Available from: https://www.who.int/data/nutrition/nlis/info/malnutrition-in-women.Search in Google Scholar
16. Bashir, M, Ibrahim, I, Beer, S, Shahbic, H, Eltaher, F, Al-Mutawaa, K, et al.. Integrated care of diabetes during pregnancy: a Qatari nationwide cohort. eClinicalMedicine 2024;72:102605. https://doi.org/10.1016/j.eclinm.2024.102605.Search in Google Scholar PubMed PubMed Central
17. Karrar, SA, Martingano, DJ, Hong, PL. Preeclampsia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [cited 2025 Jul 24]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK570611/.Search in Google Scholar
18. Newnham, JP, Dickinson, JE, Hart, RJ, Pennell, CE, Arrese, CA, Keelan, JA. Strategies to prevent preterm birth. [cited 2025 Feb 27]. Front Immunol [Internet] 2014;5. Available from: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2014.00584/full.10.3389/fimmu.2014.00584Search in Google Scholar PubMed PubMed Central
19. Adjei-Gyamfi, S, Musah, B, Asirifi, A, Hammond, J, Aryee, PA, Miho, S, et al.. Maternal risk factors for low birthweight and macrosomia: a cross-sectional study in Northern Region, Ghana. J Health Popul Nutr 2023;42:87. https://doi.org/10.1186/s41043-023-00431-0.Search in Google Scholar PubMed PubMed Central
20. Farrell, T, Minisha, F, Khenyab, N, Ali, NM, Obaidly, SA, Yaqoub, SA, et al.. A customised fetal growth and birthweight standard for Qatar: a population-based cohort study. J Perinat Med 2024;52:878–85. https://doi.org/10.1515/jpm-2024-0060.Search in Google Scholar PubMed
21. StataCorp. Stata statistical software: release 18. College Station, TX: StataCorp LLC; 2023.Search in Google Scholar
22. Ryan, GA, Nicholson, SM, Morrison, JJ. Vaginal birth after caesarean section: current status and where to from here? Eur J Obstet Gynecol Reprod Biol 2018;224:52–7. https://doi.org/10.1016/j.ejogrb.2018.02.011.Search in Google Scholar PubMed
23. Hugill, DMK, British Journal of Midwifery. ‘Once a caesarean, always a caesarean’? Challenging perceptions around vaginal birth after caesarean. [cited 2025 Jul 24]; 2016. Available from: https://www.britishjournalofmidwifery.com/content/clinical-practice/once-a-caesarean-always-a-caesarean-challenging-perceptions-around-vaginal-birth-after-caesarean/.Search in Google Scholar
24. Knight, H, Gurol-Urganci, I, van der Meulen, J, Mahmood, T, Richmond, D, Dougall, A, et al.. Vaginal birth after caesarean section: a cohort study investigating factors associated with its uptake and success. BJOG Int J Obstet Gynaecol 2014;121:183–92. https://doi.org/10.1111/1471-0528.12508.Search in Google Scholar PubMed
25. Grylka-Baeschlin, S, Clarke, M, Begley, C, Daly, D, Healy, P, Nicoletti, J, et al.. Labour characteristics of women achieving successful vaginal birth after caesarean section in three European countries. Midwifery 2019;74:36–43. https://doi.org/10.1016/j.midw.2019.03.013.Search in Google Scholar PubMed
26. Rossen, J, Lucovnik, M, Eggebø, TM, Tul, N, Murphy, M, Vistad, I, et al.. A method to assess obstetric outcomes using the 10-group classification system: a quantitative descriptive study. BMJ Open 2017;7:e016192. https://doi.org/10.1136/bmjopen-2017-016192.Search in Google Scholar PubMed PubMed Central
27. Yamani-Zamzami, TY. Delivery outcomes at term after one previous cesarean section. Saudi Med J 2007;28:1845–9.Search in Google Scholar
28. Alkhamis, F. Pregnancy outcome in women with previous one cesarean section, experience from Kingdom of Saudi Arabia. Egypt J Hosp Med 2019;77:5109–13. https://doi.org/10.21608/ejhm.2019.50257.Search in Google Scholar
29. Smith, GCS, White, IR, Pell, JP, Dobbie, R. Predicting cesarean section and uterine rupture among women attempting vaginal birth after prior cesarean section. PLoS Med 2005;2:e252. https://doi.org/10.1371/journal.pmed.0020252.Search in Google Scholar PubMed PubMed Central
30. Schummers, L, Hutcheon, JA, Hacker, MR, VanderWeele, TJ, Williams, PL, McElrath, TF, et al.. Absolute risks of obstetric outcomes risks by maternal age at first birth: a population-based cohort. Epidemiology 2018;29:379–87. https://doi.org/10.1097/ede.0000000000000818.Search in Google Scholar PubMed PubMed Central
31. Grobman, WA, Sandoval, G, Rice, MM, Bailit, JL, Chauhan, SP, Costantine, MM, et al.. Prediction of vaginal birth after cesarean delivery in term gestations: a calculator without race and ethnicity. Am J Obstet Gynecol 2021;225:664.e1–664.e7. https://doi.org/10.1016/j.ajog.2021.05.021.Search in Google Scholar PubMed PubMed Central
32. RCOG [Internet]. Birth after previous caesarean birth (green-top guideline No. 45). [cited 2025 Jul 26]. Available from: https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/birth-after-previous-caesarean-birth-green-top-guideline-no-45/.Search in Google Scholar
33. Jauniaux, E, Jurkovic, D. Long-term complications after caesarean section. In: Jauniaux, E, Grobman, W, editors. Textbook of Caesarean Section [Internet]. Oxford University Press [cited 2025 Jul 26]. p. 0; 2016.10.1093/med/9780198758563.001.0001Search in Google Scholar
34. Cosmai, G, Biondini, M, Panzeri, M, Serafini, M, Lambicchi, L, Locatelli, A, et al.. The decision-making process in the choice of VBAC: facilitators and barriers from women’s perception, a systematic review. [cited 2025 Jul 26]; Available from: https://www.europeanjournalofmidwifery.eu/The-decision-making-process-in-the-choice-of-VBAC-Facilitators-and-barriers-from,205874,0,2.html.Search in Google Scholar
35. Kanjanakaew, A, Jiramanee, A, Srimoragot, M. Providers’ perspective on vaginal birth after cesarean birth: a qualitative systematic review. BMC Pregnancy Childbirth 2024;24:723. https://doi.org/10.1186/s12884-024-06921-1.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.


