Abstract
Objectives
Demonstration of the advantage of 3D/4D ultrasound compared to 2D imaging in the precise detection and parental counseling of isolated fetal limb defects.
Methods
Prospective observational study of 201 fetal limb defects over a 30-year period (1994–2023) in a level III center.
Results
Comparison of 2D and 3D ultrasound showed a benefit in the precise demonstration of isolated limb abnormalities in 154 of the 201 cases (76.6 %), particularly in subtle malformations. In the demonstration of the defects to the parents-to-be, 3D/4D ultrasound was superior to 2D ultrasound in 100 % of cases by the fact that the abnormalities could be better understood by the parents when using a spatial presentation.
Conclusions
3D/4D ultrasound is superior to 2D sonography in the demonstration of isolated limb defects, particularly in subtle limb defects.
Introduction
Limb malformations can be structural or functional, isolated or non-isolated. They may affect bones, joints, muscles and soft tissue. The sonographic detection of isolated limb abnormalities during a routine examination is a challenge and depends on various factors: gestational age, amniotic fluid conditions, location of the fetus, quality of the ultrasound device, experience of the examiner and a systematic examination of the entire fetus. While an examination in the first trimester provides a good overview of the fetal limb anatomy under normal amniotic fluid conditions, the assessment of the extremities in the second or third trimester may be significantly more difficult or even impossible if the fetus is in an unfavourable position or if the amount of amniotic fluid is reduced.
In contrast to 2D ultrasound examination, 3D/4D sonography offers a variety of imaging modes (Table 1) [1]. The surface mode allows an almost photographic representation of isolated defects or axial deviations in the extremities as well as the detection of supernumerary digits in hands and feet. The demonstration of the long limb bones in the multiplanar mode allows precise measurement of the bone length in the correct adjusted biometric axis [2]. With the transparency mode, bone abnormalities, such as missing bones, fractures and axial deviations, can be displayed in a targeted manner. 4D ultrasound enables the operator to depict the entire extremities from the outer aspect or just the skeleton in motion.
Overview of 3D/4D visualization modes applicable to prenatal diagnosis [1].
| 3D display mode | 4D display mode |
|---|---|
| Multiplanar mode | Multiplanar mode |
| Multislice/tomographic ultrasound imaging (TUI) | Multislice/TUI |
| 3D surface mode | 3D surface mode |
| Transparent mode | Transparent mode |
| Glass body mode | Glass body mode |
| Inversion mode | Inversion mode |
| Volume contrast imaging (VCI) | VCI |
| OmniView | OmniView |
| 3D animation (cine) | Spatio-temporal image correlation (STIC) |
| HDlive (high definition) | HDlive |
| HDlive silhouette | HDlive silhouette |
| HDlive studio | HDlive studio |
Detection of isolated fetal limb anomalies using 3D/4D ultrasound
The etiology of limb defects is very complex [3], [4], [5], [6], [7] (Table 2). Nowadays for many of those anomalies a genetic defect is known [4]. However, in several cases no identifiable cause for the limb defect can be found.
Known causes of isolated limb defects.
| – | Exposure to a teratogen (thalidomide, valproic acid) |
| – | Vascular accident |
| – | Maternal diabetes |
| – | Amniotic band syndrome (strands of amnion entangle or fuse with fetal tissue) |
| – | Genetic abnormalities (single gene disorders, including autosomal dominant, autosomal recessive, and X-linked recessive disorders) |
| – | Component of various congenital syndromes/chromosome abnormalities |
Description of limb deficiencies
For a precise description of limb deficiencies, several parameters should be taken into account (Table 3).
Description of limb deficiencies [8].
| Total or partial – amelia/meromelia |
| Axis of the defect – transverse/longitudinal |
| Limb involved – upper/lower |
| Side involved – right/left |
| Deficient bone(s) – femur/radius/metacarpal 2–5 etc. |
| Portion of bone deficient – proximal, middle, distal |
Nomenclature for limb abnormalities
Table 4 gives an overview of the most common terminology for limb abnormalities.
Descriptive terms for limb abnormalities.
| Amelia | Absence of one or more limbs |
| Phocomelia | Hands and feet are directly attached to the trunk |
| Peromelia | Absence or deformity of the terminal part of a limb or limbs |
| Hemimelia | Absence of the distal portion of one limb (form of peromelia) |
| Meromelia | Partial absence of a limb |
| Ectromelia | Hypoplasia of the long bones of the limbs |
| Acheira | Absence of one or both hands |
| Apodia | Absence of one or both feet |
| Acheiropodia | Absence of hands and feet |
| Adactyly | Absence of fingers or toes |
| Oligodactyly | Subnormal number of fingers or toes |
| Polydactyly Preaxial Postaxial |
Supernumerary fingers or toes – Extra digit on radial or tibial side – Extra digit on ulnar or fibular side |
| Brachydactyly | Abnormal shortness of the fingers or toes |
| Ectrodactyly | Absence of all or part of a digit (split hand, lobster claw) |
| Sirenomelia | Anomaly in which the lower extremities are fused |
| Syndactyly | A fusion of two or more fingers or toes |
| Clinodactyly | Permanent medial or lateral deflection of one or more fingers |
| Camptodactyly | Permanent flexion of fingers or toes |
| Talipes varus | Clubfoot (heel and foot are turned inward) |
| Talipes valgus | Valgus deformity (heel and foot are turned outward) |
There is some concern to use terms derived from Greek or Latin roots, such as meromelia, hemimelia, ectromelia, and peromelia, since these terms are not universal nor easily translated into languages that have no relation to the classical languages [9].
Sonographic classification
From the sonographic aspect, four groups can be distinguished:
Limb deficiency disorders
Fusion defects
Supernumerary structures
Limb/bone abnormalities with axis deviation
Limb deficiency disorders (LDDs)
The incidence of limb deficiency disorders is approximately 1:1,300 to 2,000 births [4]. LDDs are classified based on the type and location of the deficiency. The two main categories include longitudinal and transverse deficiencies.
Longitudinal defects
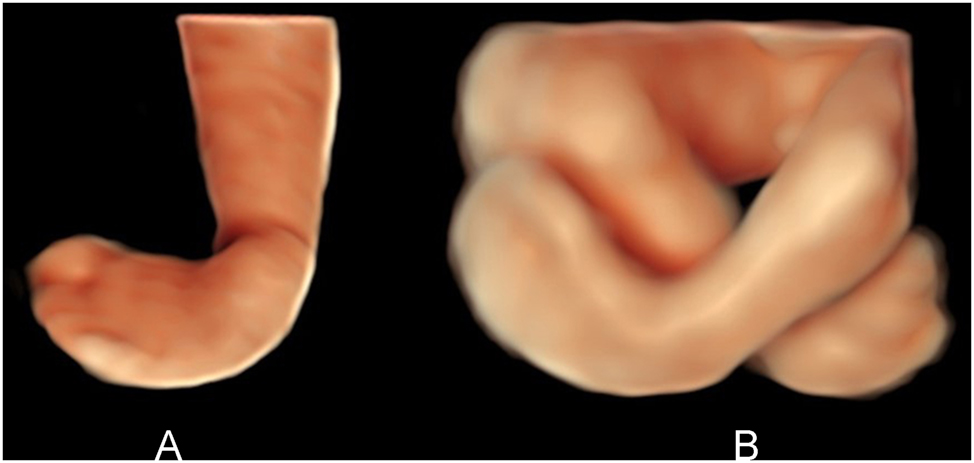
Longitudinal defects extend along the long axis of the limb, such as the absence of the radius or fibula. Typical longitudinal defects are amelia (Figure 1A), phocomelia, peromelia (Figure 1B), aplasia of radius (Figure 2), split hand (Figure 3A) and split foot (Figure 3B). Although most longitudinal deficiencies are genetic or sporadic, some are teratogenic [4]. The most severe defects have been found during thalidomide therapy. Longitudinal deficiencies can involve one limb or may be symmetric [4].
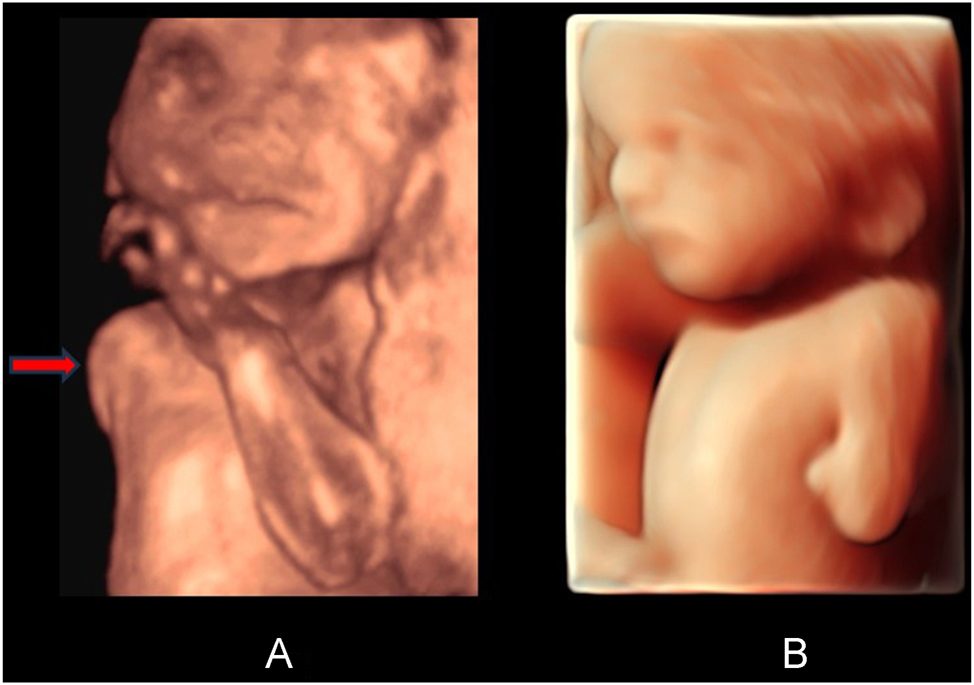
(A) Surface view of amelia on the right side (red arrow), 22 weeks’ gestation. The left arm shows a normal appearance. (B) Surface view (HDlive) of peromelia on the left side. 30 weeks’ gestation.
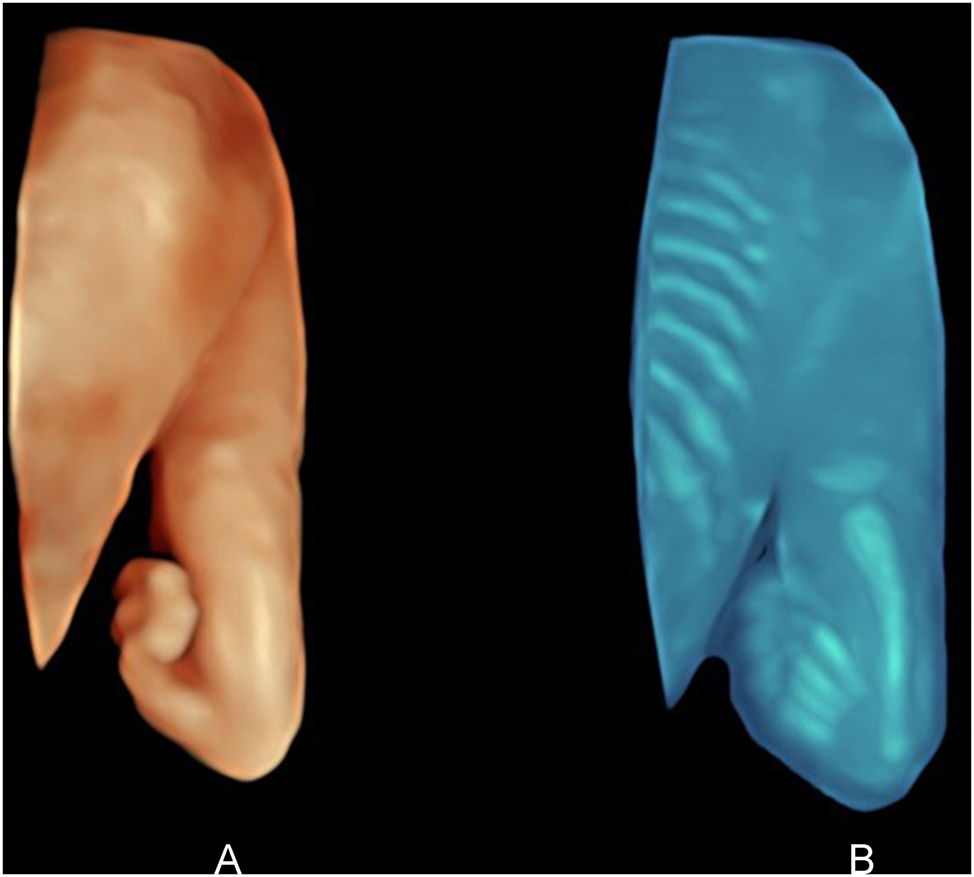
(A) Dorsal surface view (HDlive) of hemimelia right with severe angulation of the hand with only four fingers. (B) The transparent view of the same arm reveals radius aplasia. 23 weeks’ gestation.
(A) Surface view (HDlive) of ectrodactyly (split hand), showing only two fingers. 21 weeks’ gestation. (B) Frontal surface view (HDlive) of split foot with only two toes. 22 weeks’ gestation.
An absent or hypoplastic middle phalanx of digit 5 has been shown to be a sonographic marker for trisomy 21 [10] (Figure 4).
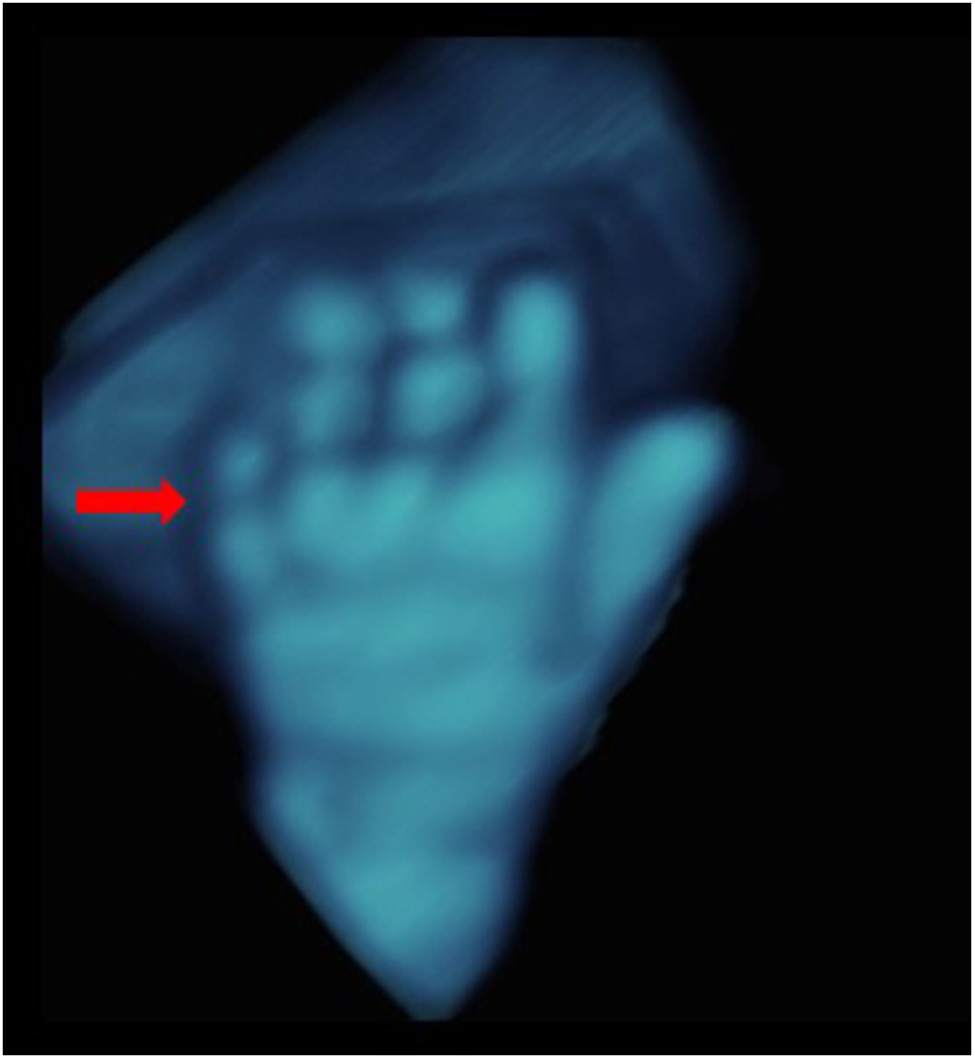
Transparent view of the left hand from dorsal, demonstrating absent middle phalanx of digit 5 (red arrow), typical for trisomy 21. 22 weeks’ gestation.
Transverse defects
Transverse defects are across the long axis of the limb, such as a complete amputation of the hand or foot. The main cause for such defects is seen in the amniotic band syndrome [4], 11], 12], in which severe entanglement of the limb by an amniotic strand leads to severe damage of the distal part or even to complete amputation.
Fusion defects
Fusion defects are caused by a failure in the separation of developing structures during organogenesis. They represent rare malformations with an estimated incidence of 1/2,500 live births [13].
Syndactyly may occur as complete syndactyly (fingers joined all the way to tip) (Figure 5A and B) or incomplete syndactyly (fingers joined part way up). Common conditions involving syndactyly are oro-facial-digital syndrome, Apert syndrome, Jeune syndrome and Trisomy 13.
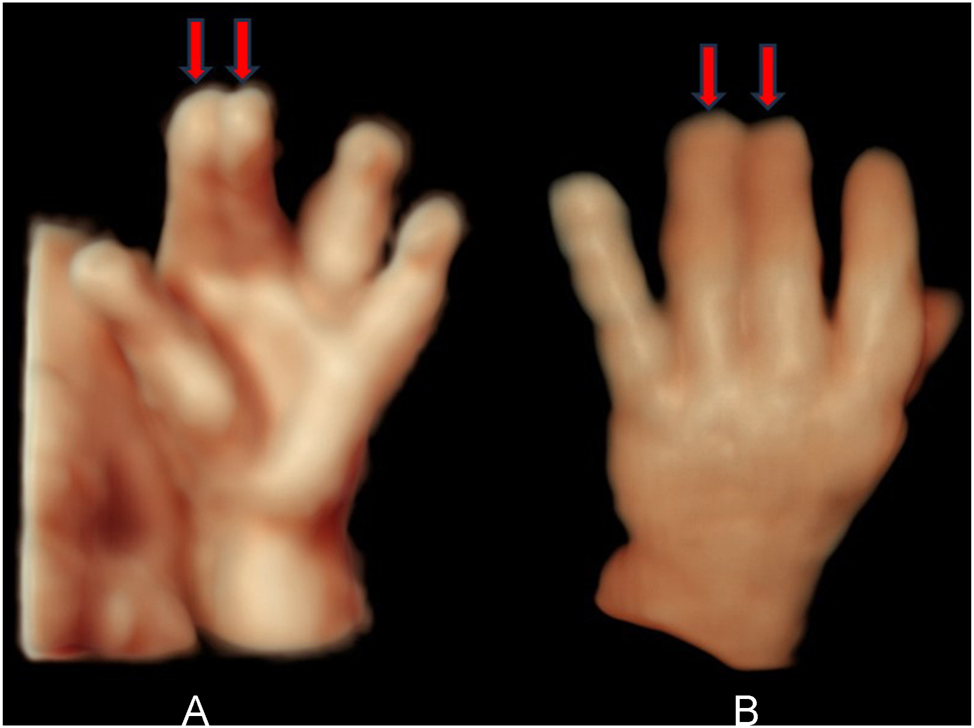
(A) Frontal HDlive surface view of the left hand, showing complete syndactyly between digit 2 and 3 (red arrows). 23 weeks’ gestation. (B) Dorsal HDlive view of the left hand, showing complete syndactyly between digit 3 and 4. 35 weeks’ gestation (red arrows).
Sirenomelia sequence (mermaid syndrome), is a defect of the lower body characterized by the apparent fusion of the legs into a single lower limb. The reported incidence of human sirenomelia varies between 1.1 and 4.2 per 100,000 births [14]. According to Stocker and Heifetz [15] seven different types can be differentiated. Figure 6 shows sirenomelia type VI (Sympus apus). Owing to visceral abnormalities, sirenomelia is usually incompatible with life [14].

HDlive surface view sirenomelia type VI, 14 weeks’ gestation.
Supernumerary structures
Supernumerary structures are characterized by a total or partial duplication of structures.
Polydactyly is the most common defect, occurring in 4–8 out of 10,000 live births [13].
Postaxial hexadactyly (extra digit on the ulnar or fibular side) is the most common form and is generally an isolated defect (Figure 7A and B).
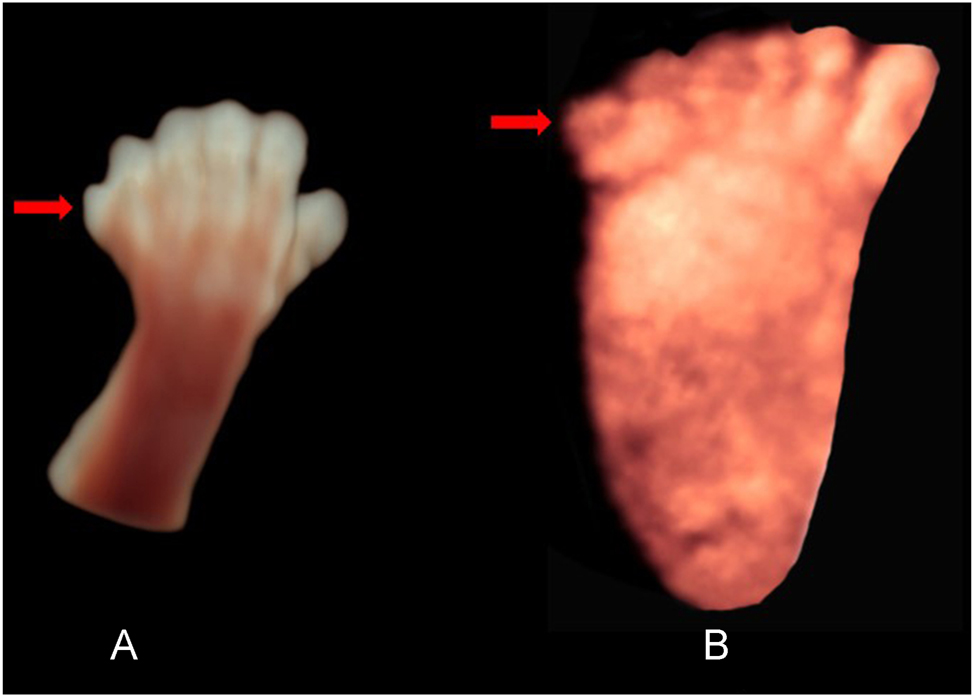
(A) HDlive surface view of the left hand, showing postaxial hexadactyly (red arrow). 13 weeks’ gestation. (B) Plantar surface view of the right foot with postaxial hexadactyly (red arrow). 23 weeks’ gestation.
Preaxial hexadactyly (extra digit on the radial or tibial side) is most likely a part of a syndrome [13].
Limb abnormalities with axis deviation
Limb abnormalities with axis deviation may occur in hands, feet and in long bones. Overlapping fingers are seen in trisomy 18 and 13. In particular overlapping of the index finger over the middle finger and the fifth finger over the ring finger is characteristic of trisomy 18 (Figure 8A).
(A) HDlive surface view of the left hand with overlapping of the index finger over the middle finger and the fifth finger over the ring finger, characteristic of trisomy 18. 31 weeks’ gestation. (B) HDlive surface view of the left foot with overlapping of the second toe over the first toe. 31 weeks’ gestation.
Overlapping toes can be found in several deletion syndromes, Nager syndrome, Smith-Lemli-Opitz syndrome and Kniest syndrome (Figure 8B).
Clinodactyly represents a permanent medial or lateral deflection of one or more fingers [16] (Figure 9).
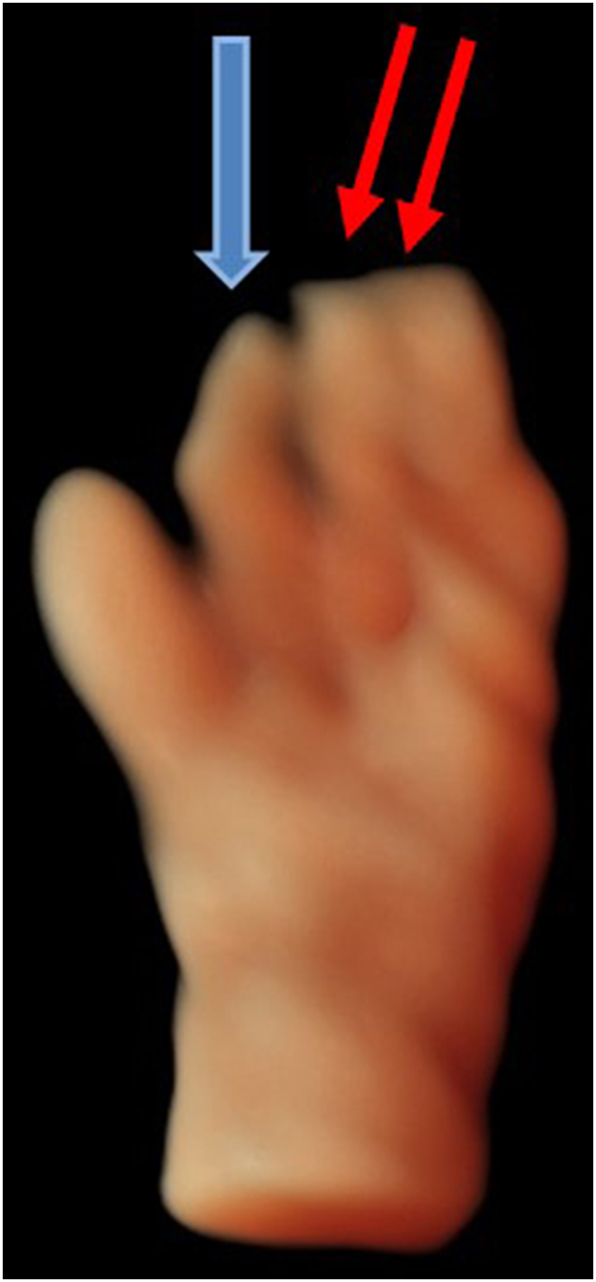
HDlive surface view of the left hand with clinodactyly (index finger) (blue arrow) and syndactyly between finger 3 and 4 (red arrows). 18 weeks’ gestation.
Camptodactyly is a digital flexion deformity in the proximal interphalangeal joint. It involves predominantly the 4th and 5th fingers [16].
A hitchhiker thumb represents a malposition of the thumb, where the thumb is abnormally abduced. A hitchhiker thumb is typically found in diastrophic dysplasia [17].
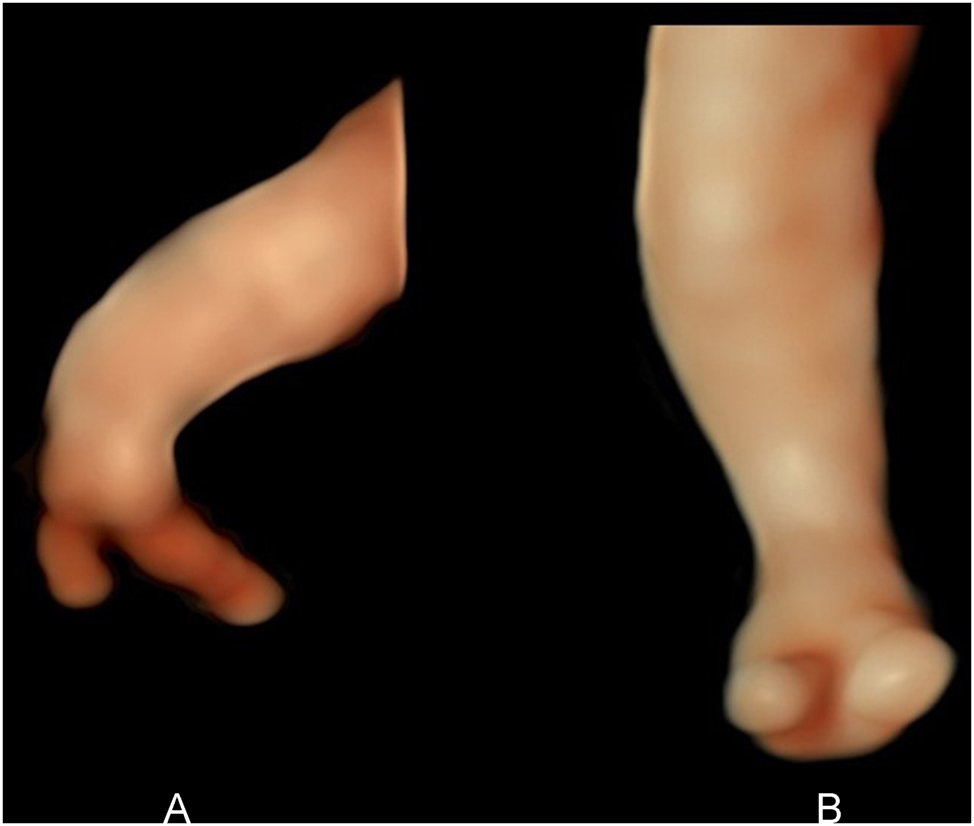
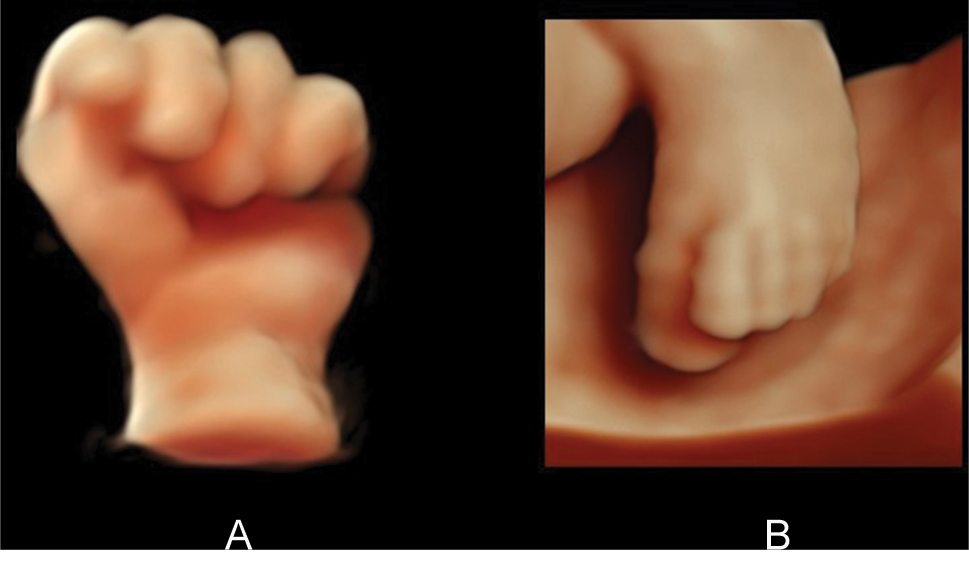
Clubfoot is the most common congenital malformation of the foot with an incidence of 1 per 1,000 births [18]. The foot is rotated inwards and downwards. In approximately 50 % of cases, clubfoot affects both feet (Figure 10A and B). 80 % of cases are idiopathic and include environmental, vascular, positional, and genetic factors [19]. Clubfoot occurs as an isolated anomaly or in association with spina bifida, several syndromes (e.g., Down syndrome, Edwards syndrome, Meckel-Gruber syndrome, Pena-Shokeir syndrome, Seckel syndrome, Smith-Lemli-Opitz syndrome and Campomelic syndrome) and arthrogryposis multiplex congenita [20], 21]. In trisomy 18, it is found in approxmately 15 % of cases [20]. Clubfoot is also seen in cases with severe oligohydramnios.
(A) HDlive surface view of a unilateral clubfoot right (view from plantar). 21 weeks’ gestation. (B) HDlive surface view of bilateral clubfoot (frontal view). 19 weeks’ gestation.
An isolated joint contracture is defined when only one joint is fixed in a flexed or a straightened position, If two or more joints are affected it is defined as arthrogryposis multiplex congenita (Figure 11). This is not a specific diagnosis but is more a descriptive term for many pathologic processes (e.g., neuropathies, myopathies, connective tissue disorders or severe oligohydramnios) that cause immobilization of the fetal limbs in different joints [22].

HDlive surface view of the left hand with fixed position of the wrist and fingers, due to arthrogryposis multiplex congenita, 22 weeks’ gestation.
An axis deviation of the forearm or lower leg is found in a bending or fracture of a long tubular bone (Figure 12A and B).
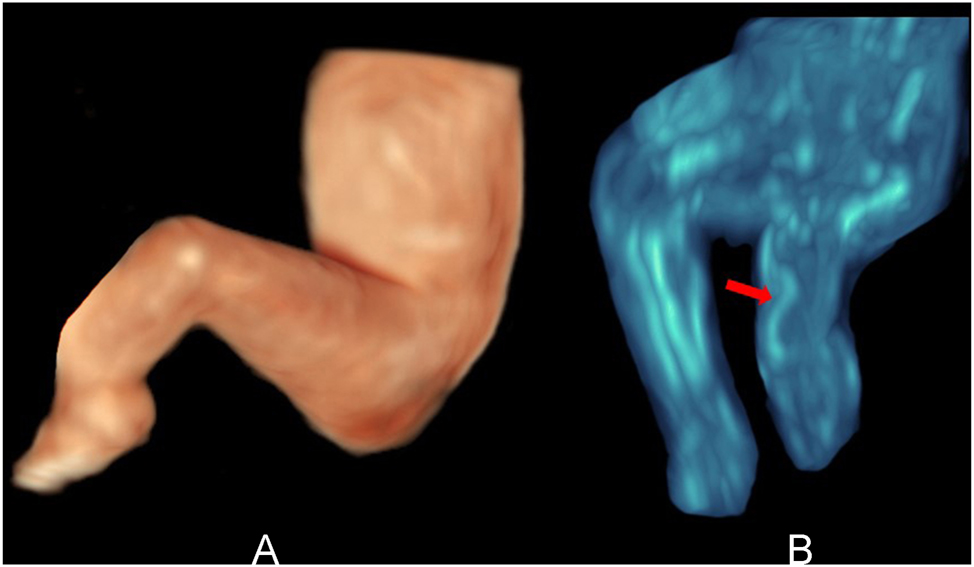
(A) HDlive surface view of the left leg with bowing of the lower leg. 19 weeks’ gestation. (B) Transparent view of the same fetus, revealing bowing of tibia (red arrow) and aplasia of fibula. 19 weeks’ gestation.
Materials and methods
In a time period of 30 years (1994–2023), 201 isolated fetal limb malformations between 13 and 35 weeks of gestation could be diagnosed in our level III center (Table 5). All patients were of Caucasian origin and had been referred for a general anomaly scan. All suspicious findings were controlled by an experienced level III operator (medical doctor). Osteochondrodysplasias were excluded in this study.
Isolated limb anomalies detected with 3D/4D ultrasound.
| Amelia | n=3 |
| Phocomelia | n=5 |
| Ectromelia | n=6 |
| Peromelia | n=18 |
| Hemimelia/radial aplasia | n=17 |
| Apodia | n=1 |
| Sirenomelia | n=4 |
| Split hand/split foot | n=6 |
| Polydactyly | n=28 |
| Syndactyly | n=12 |
| Clinodactyly | n=7 |
| Camptodactyly/overlapping fingers or toes | n=13 |
| Hitchhiker thumb | n=2 |
| Missing middle phalanx digit V | n=18 |
| Club foot | n=53 |
| Joint contractures | n=8 |
| Total | n=201 |
All examinations were initially performed with 2D ultrasound and in addition with 3D/4D ultrasound (Voluson 530, Voluson 730, Voluson E8, Voluson E10) using abdominal and transvaginal 3D/4D probes.
2D and 3D/4D results were compared for a more accurate representation. Better visualization was defined as a more precise demonstration of the anomaly in the multiplanar, surface or transparency mode, resulting in an increased confidence in the diagnosis.
In addition, the parents were shown the pathological findings with 2D and 3D images and the parents were asked to decide which image representation was more informative for them.
The study protocol was approved by the local Ethics Committee. All participants gave written informed consent.
Results
In the comparison of 2D and 3D ultrasound, 3D/4D sonography with the different visualization modes provided the level III operator with a better representation of the limb abnormalities in 154 of 201 cases (78.2 %) than 2D sonography. In four cases the diagnosis could even with 3D/4D ultrasound not be clarified during the first examination due to an unfavourable position of the fetus. However, the correct diagnosis could be made during the follow-up examination. In all cases the prenatal findings were confirmed postnatally. No false positive or negative results could be observed.
With regard to parents counseling 3D images were appreciated by the parents in understanding the severity of the malformations in 100 %.
Discussion
The prenatal detection of limb defects, particulary isolated limb defects, during routine 2D scan is generally low since complete examination of all extremities is not required in current second trimester screening programs. Arduc [6] reported estimated prenatal detection rates of 57 % for transverse reduction defect, 46 % for longitudinal reduction defect, 31 % for polydactyly, and 17 % for syndactyly. Abnormalities of the limbs can only be exactly recognized with a targeted examination of all four limbs which is time consuming when the fetus is in an unfavorable position or in case of oligohydramnios. Particularly the demonstration of defects of the fingers is only possible when the fetus shows the hand with extended digits. An optimal time for examining the fetal extremities is during the first trimester screening, as this provides a good overview of all four limbs. In contrast to 2D ultrasound, 3D/4D sonography offers the advantage of storing volumes instead of only images. As soon as the volumes with the limbs or parts of the limbs are stored in the memory of the ultrasound device, the limbs are in a fixed position and the volumes can be rotated in all three dimensions to demonstrate the limbs/bones in the preferred axis. This allows correct measurement of all long limb bones in their maximum length [2], recognition of limb defects or axis deviations. In general, if a limb defect is found, a careful sonographic search for further abnormalities should be carried out. The presence of associated malformations may indicate a chromosome abnormality or a syndrome. Early prenatal detection allows for genetic counseling, fetal karyotyping, molecular testing and delivery planning.
Conclusions
3D/4D ultrasound is an excellent technique to assess the fetal limbs. The different visualization modes allow the detection of both surface and bone abnormalities. Particularly in the exact demonstration of small structures 3D ultrasound is superior to 2D sonography. Abnormalities in the extremities can be demonstrated to the expectant parents as if in a photo. Likewise, in cases where there is a risk of recurrence of a limb abnormality, normal findings can be more convincingly shown to the expectant parents, particularly with the 3D surface mode which allows the parents to have a clear view of the normal fetal anatomy.
-
Research ethics: The research has complied with all relevant national regulations and institutional policies and has been approved by the authors’ Institutional Review Board.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Merz, E, Pashaj, S. Advantages of 3D ultrasound in the assessment of fetal abnormalities. J Perinat Med 2017;45:643–50. https://doi.org/10.1515/jpm-2016-0379.Search in Google Scholar PubMed
2. Merz, E, Pashaj, S, Wellek, S. Normal fetal growth profile at 10-41 weeks of gestation - an update based on 10225 normal singleton pregnancies and measurement of the fetal parameters using 3D ultrasound. Ultraschall Med 2023;44:179–87. https://doi.org/10.1055/a-1968-0018.Search in Google Scholar PubMed
3. Ermito, S, Dinatale, A, Carrara, S, Cavaliere, A, Imbruglia, L, Recupero, S. Prenatal diagnosis of limb abnormalities: role of fetal ultrasonography. J Prenat Med 2009;3:18–22.Search in Google Scholar
4. Wilcox, WR, Coulter, CP, Schmitz, ML. Congenital limb deficiency disorders. Clin Perinatol 2015;42:281–300. https://doi.org/10.1016/j.clp.2015.02.004.Search in Google Scholar PubMed
5. Klungsøyr, K, Nordtveit, TI, Kaastad, TS, Solberg, S, Sletten, IN, Vik, AK. Epidemiology of limb reduction defects as registered in the medical birth registry of Norway, 1970-2016: population based study. PLoS One 2019;14:e0219930. https://doi.org/10.1371/journal.pone.0219930.Search in Google Scholar PubMed PubMed Central
6. Arduç, A, van Dijk, SJB, Ten Cate, FJ, van Doesburg, MHM, Linskens, IH, van Leeuwen, E, et al.. Phenotype-to-genotype description of prenatal suspected and postnatal discovered upper limb anomalies: a retrospective cohort study. Prenat Diagn 2025;45:3–14. https://doi.org/10.1002/pd.6714.Search in Google Scholar PubMed PubMed Central
7. Thakur, S, Chaddha, V, Gupta, R, Singh, C, Dagar, S, Shastri, A, et al.. Spectrum of fetal limb anomalies. J Clin Ultrasound 2023;51:96–106. https://doi.org/10.1002/jcu.23273.Search in Google Scholar PubMed
8. Stevenson, RE, Meyer, LC. The limbs. In: Stevenson, RE, Hall, JG, Goodman, RM, editors. Human malformations and related anomalies. New York - Oxford: Oxford University Press; 1993, vol II:699–720 pp.Search in Google Scholar
9. Bedard, T, Lowry, RB, Sibbald, B, Kiefer, GN, Metcalfe, A. Congenital limb deficiencies in Alberta-a review of 33 years (1980-2012) from the Alberta congenital anomalies surveillance system (ACASS). Am J Med Genet 2015;167:2599–609. https://doi.org/10.1002/ajmg.a.37240.Search in Google Scholar PubMed
10. Benacerraf, BR, Harlow, BL, Frigoletto, FDJr. Hypoplasia of the middle phalanx of the fifth digit. A feature of the second trimester fetus with Down’s syndrome. J Ultrasound Med 1990;9:389–94. https://doi.org/10.7863/jum.1990.9.7.389.Search in Google Scholar PubMed
11. Barzilay, E, Harel, Y, Haas, J, Berkenstadt, M, Katorza, E, Achiron, R, et al.. Prenatal diagnosis of amniotic band syndrome - risk factors and ultrasonic signs. J Matern -Fetal Neonat Med 2015;28:281–3. https://doi.org/10.3109/14767058.2014.915935.Search in Google Scholar PubMed
12. Hata, T, Tanaka, H, Noguchi, J. 3D/4D sonographic evaluation of amniotic band syndrome in early pregnancy: a supplement to 2D ultrasound. J Obstet Gynaecol Res 2011;37:656–60. https://doi.org/10.1111/j.1447-0756.2010.01417.x.Search in Google Scholar PubMed
13. Gramellini, D, Fieni, S, Vadora, E. Prenatal diagnosis of isolated limb defects: an updated review. Fetal Diagn Ther 2005;20:96–101. https://doi.org/10.1159/000082430.Search in Google Scholar PubMed
14. Garrido-Allepuz, C, Haro, E, González-Lamuño, D, Martínez-Frías, ML, Bertocchini, F, Ros, MA. A clinical and experimental overview of sirenomelia: insight into the mechanisms of congenital limb malformations. Dis Model Mech 2011;4:289–99. https://doi.org/10.1242/dmm.007732.Search in Google Scholar PubMed PubMed Central
15. Stocker, JT, Heifetz, SA. Sirenomelia. A morphological study of 33 cases and review of the literature. Perspect Pediatr Pathol 1987;10:7–50.Search in Google Scholar
16. Matošević, M, Lamot, L, Antičević, D. Camptodactyly and clinodactyly – new understanding of known deformities. Acta Clin Croat 2022;60:525–31.10.20471/acc.2021.60.03.24Search in Google Scholar PubMed PubMed Central
17. Tongsong, T, Wanapirak, C, Sirichotiyakul, S, Chanprapaph, P. Prenatal sonographic diagnosis of diastrophic dwarfism. J Clin Ultrasound 2002;30:103–5. https://doi.org/10.1002/jcu.10032.abs.Search in Google Scholar
18. Dibello, D, Di Carlo, V, Colin, G, Barbi, E, Galimberti, AM. What a paediatrician should know about congenital clubfoot. Ital J Pediatr 2020;46:78. https://doi.org/10.1186/s13052-020-00842-3.Search in Google Scholar PubMed PubMed Central
19. Di Mascio, D, Buca, D, Khalil, A, Rizzo, G, Makatsariya, A, Sileo, F, et al.. Outcome of isolated fetal talipes: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2019;98:1367–77. https://doi.org/10.1111/aogs.13637.Search in Google Scholar PubMed
20. Warkany, J. Congenital malformations. Chicago: Year Book Medical Publishers; 1971.Search in Google Scholar
21. Society for Maternal-Fetal Medicine, Rac, MWF, McKinney, J, Gandhi, M. Arthrogryposis. Am J Obstet Gynecol 2019;221:B7–9. https://doi.org/10.1016/j.ajog.2019.09.021.Search in Google Scholar PubMed
22. Dieterich, K, Kimber, E, Hall, JG. Central nervous system involvement in arthrogryposis multiplex congenita: overview of causes, diagnosis, and care. Am J Med Genet Part C 2019;181:345–53. https://doi.org/10.1002/ajmg.c.31732.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- The fetus as a patient in the 21st century: science, ethics, technology and global responsibility
- Vision, Education, and the Future of Perinatal Medicine
- Opening – field direction, education, and AI
- Quo vadis neonatologia? Where is neonatology heading in the 21st century?
- Shaping the future: advancing maternal-fetal medicine through educational standards and innovations
- Integrating generative AI in perinatology: applications for literature review
- Maternal Hemodynamics, Fetal Physiology, and Surveillance
- Core fetal physiology and maternal-fetal interaction
- Cardiac output-guided maternal positioning may protect the fetal oxygen supply and thereby reduce pregnancy complications
- Effect of antenatal betamethasone on fetal heart rate short-term variability in growth restricted fetuses
- Umbilical venous flow and maternal hemodynamics as predictors of impaired fetal growth in gestational diabetes: a prospective study
- The impact of maternal cardiovascular status prior to labor on birth outcomes: an observational study
- Complex Pregnancies, Placenta, and Fetal Therapy
- Twins, placental disease, fetal intervention, and periviability
- Complications in monochorionic twin pregnancies
- Association of discordance in birth weights of dichorionic twins with the incidence of preeclampsia in pregnant women
- Management and outcomes of periviable infants in Slovenia: a decade of experience
- Successful management of severe hemolytic disease of the fetus and newborn (HDFN) due to anti-Kell
- Systems of Care, Screening, and Population-Level Perinatal Medicine
- Public health, structured care, and national data
- Structured stillbirth management in Slovenia: outcomes and comparison with international guidelines
- Newborn screening for rare diseases: expanding the paradigm in the genomic era
- Ten years of experience with screening for diabetes in pregnancy according to IADPSG criteria in Slovenia
- Gestational diabetes and fetal macrosomia: a dissenting opinion
- Advanced Prenatal Diagnosis
- Imaging and fetal anomaly detectionata
- Detection of isolated fetal limb anomalies using 3D/4D ultrasound
- Ethics, Professional Responsibility, and Patient-Centered Counseling
- The moral and communicative core of “Fetus as a Patient”
- The fetus as a patient: professional responsibility in contemporary Perinatal Medicine
- Placenta-oriented counseling: challenges and opportunities in obstetric practice
- Patient education materials: improving readability to advance health equity
- Global Health, Pandemic, and Humanitarian Perinatal Medicine
- COVID-19, war, immunity, and respectful care
- Clinical factors in SARS-CoV-2 antibody response in unvaccinated mothers
- Serum vitamin D and inflammatory markers in SARS-CoV-2 positive pregnant women
- Perceptions of respectful maternity care in Ukraine during a time of war
- Role of prelabour midwifery consultation in enhancing maternal satisfaction and preparedness for birth
- Obstetric Decision-Making and Postpartum Outcomes
- Clinical controversies and maternal outcomes
- Should we conduct a trial of labor in women with a macrosomic fetus?
- Postpartum maternal complications: a retrospective single-center study
- Annual Reviewer Acknowledgment
- Reviewer Acknowledgment
Articles in the same Issue
- Frontmatter
- Editorial
- The fetus as a patient in the 21st century: science, ethics, technology and global responsibility
- Vision, Education, and the Future of Perinatal Medicine
- Opening – field direction, education, and AI
- Quo vadis neonatologia? Where is neonatology heading in the 21st century?
- Shaping the future: advancing maternal-fetal medicine through educational standards and innovations
- Integrating generative AI in perinatology: applications for literature review
- Maternal Hemodynamics, Fetal Physiology, and Surveillance
- Core fetal physiology and maternal-fetal interaction
- Cardiac output-guided maternal positioning may protect the fetal oxygen supply and thereby reduce pregnancy complications
- Effect of antenatal betamethasone on fetal heart rate short-term variability in growth restricted fetuses
- Umbilical venous flow and maternal hemodynamics as predictors of impaired fetal growth in gestational diabetes: a prospective study
- The impact of maternal cardiovascular status prior to labor on birth outcomes: an observational study
- Complex Pregnancies, Placenta, and Fetal Therapy
- Twins, placental disease, fetal intervention, and periviability
- Complications in monochorionic twin pregnancies
- Association of discordance in birth weights of dichorionic twins with the incidence of preeclampsia in pregnant women
- Management and outcomes of periviable infants in Slovenia: a decade of experience
- Successful management of severe hemolytic disease of the fetus and newborn (HDFN) due to anti-Kell
- Systems of Care, Screening, and Population-Level Perinatal Medicine
- Public health, structured care, and national data
- Structured stillbirth management in Slovenia: outcomes and comparison with international guidelines
- Newborn screening for rare diseases: expanding the paradigm in the genomic era
- Ten years of experience with screening for diabetes in pregnancy according to IADPSG criteria in Slovenia
- Gestational diabetes and fetal macrosomia: a dissenting opinion
- Advanced Prenatal Diagnosis
- Imaging and fetal anomaly detectionata
- Detection of isolated fetal limb anomalies using 3D/4D ultrasound
- Ethics, Professional Responsibility, and Patient-Centered Counseling
- The moral and communicative core of “Fetus as a Patient”
- The fetus as a patient: professional responsibility in contemporary Perinatal Medicine
- Placenta-oriented counseling: challenges and opportunities in obstetric practice
- Patient education materials: improving readability to advance health equity
- Global Health, Pandemic, and Humanitarian Perinatal Medicine
- COVID-19, war, immunity, and respectful care
- Clinical factors in SARS-CoV-2 antibody response in unvaccinated mothers
- Serum vitamin D and inflammatory markers in SARS-CoV-2 positive pregnant women
- Perceptions of respectful maternity care in Ukraine during a time of war
- Role of prelabour midwifery consultation in enhancing maternal satisfaction and preparedness for birth
- Obstetric Decision-Making and Postpartum Outcomes
- Clinical controversies and maternal outcomes
- Should we conduct a trial of labor in women with a macrosomic fetus?
- Postpartum maternal complications: a retrospective single-center study
- Annual Reviewer Acknowledgment
- Reviewer Acknowledgment

