Abstract
Context
Research plays a critical role in the medical field, driving progress and shaping clinical guidelines. It has become particularly significant in the residency application process due to the advent of “pass or fail” scoring for Step 1. Unfortunately, there is a marked discrepancy between the quantity of research conducted by osteopathic and allopathic students, disadvantaging many osteopathic residency applicants.
Objectives
Lake Erie College of Osteopathic Medicine (LECOM)-Bradenton established the Summer Research Internship Program in 2023 to improve research self-efficacy, facilitate research participation, and encourage lifelong research engagement in Doctor of Osteopathic Medicine (DO) students. The purpose of this study was to evaluate participant research experience and self-efficacy through pre- and postprogram surveys.
Methods
This study consisted of an experimental group of 18 students who participated in this program. A control group consisted of 20 students not enrolled in the program who had minimal research experience and no plans to conduct research throughout the study’s duration. Participants completed pre- and postprogram surveys, assessing research experience and self-efficacy across four domains: knowledge of research foundations, ability to identify scholarly literature, motivation to conduct research, and likelihood of future engagement. Data were analyzed via a quantitative Likert scale.
Results
The experimental group reported significantly greater (p<0.05) research experience pre- and postprogram including poster creation, LECOM Research Day participation, and publication history. The experimental group also had significantly (p<0.05) more experience with manuscript preparation postprogram compared to the controls. For the self-efficacy survey, the experimental group had higher (p<0.05) motivation to perform research prior to the start of the program compared to the controls. Moreover, this group gained greater (p<0.05) experience in research foundations and identification of the literature postprogram compared with controls.
Conclusions
The LECOM Summer Research Internship Program significantly enhanced research experience and self-efficacy among participants when compared to controls. This program study may serve as a model for other institutions seeking to expand student research engagement and build a culture of scholarly activity. Expanding successful structured research programs may also help address the disparity in research output between osteopathic and allopathic medical students.
Research holds great importance in the medical field. Clinical practice guidelines utilized by physicians to provide the best care for patients are recommended based upon rigorous screening of the published literature [1], 2]. Thus, research is the source of innovation, driver of progress, and the foundation on which clinical practice is established. As an investigator, one can expect to gain a deeper understanding of the topic at hand, and also grow as a critical thinker and develop problem-solving skills [3]. Studies have shown that research allows physicians to practice evidence-based medicine that contributes to better patient outcomes [4]. Despite these clear benefits, osteopathic medical students and physicians (Doctor of Osteopathic Medicine [DO]) face significant barriers to conducting research. Studies have shown the National Institutes of Health (NIH) preferentially award their flagship R01 grants to allopathic physicians (Doctor of Medicine [MD]) rather than their osteopathic counterparts. In the past decade, no NIH R01 grants in general surgery were awarded to osteopathic physicians, while 58.0 % R01 grant recipients were allopathic doctors [5]. Similarly, between 2008 and 2018, no osteopathic neurosurgeons received R01 grants, though 81 allopathic neurosurgeons received this type of funding [6]. Research is not only important as a practicing physician, but contribution to the collective knowledge of medicine is also an important rite of passage for future physicians.
Research plays a major role in educational training and is necessary for a residency application. Clear relationships exist between research productivity and match rate in specialties, such as general surgery [7]. Likewise, program directors for other residencies, such as radiation oncology, have noted the importance of research in the matching process [8]. Even beyond residency, surgical fellowship directors cited research within the field of interest as the best measure for successful osteopathic fellowship applications [9]. Quantity of research productivity for residency applications also appears to be an important factor in matching to a program. According to a recent study, the number of research publications, abstracts, and presentations has increased in number for applicants of every specialty measured by the National Residency Matching Program between 2009 and 2020 [10].
Despite the benefits of research, osteopathic students face obstacles not experienced by their allopathic medical student peers. Often, MD schools have research built into their curriculum [11], unlike many DO medical schools. In fact, one study found that as many as one-third of osteopathic medical students felt that their schools did not offer research opportunities, or they were unaware of them [12]. In addition, 96.0 % of osteopathic students noted the importance of research, but only 54.0 % were interested in or currently conducting research while pursuing their degree [13]. The lack of research funding toward osteopathic medical schools may explain the disparities in both research opportunities and interest [14].
Outside of research, osteopathic students face other challenges in applying for residency that include competition with MD students and barriers to securing audition rotations. Since 2020, the Accreditation Council for Graduate Medical Education (ACGME) became the sole accreditor for all medical residencies, merging osteopathic and allopathic residency programs [15]. This change has posed additional challenges for osteopathic students, because they now compete with allopathic counterparts for traditionally osteopathic residency positions. Additionally, many medical students feel that audition rotations where residency candidates rotate at a hospital of interest may play a crucial role in securing residency positions [16]. Despite their value, there are hospitals that do not extend “away rotations” to osteopathic students or charge them more for these opportunities [17]. In addition, residency programs previously utilized the United States Medical Licensing Exam (USMLE) Step 1 scores to compare applicants. With the advent of “pass or fail” scoring for Step 1, a critical metric of comparison between applicants is lost. One study states that beyond USMLE Step 1 and Step 2 scores, the extent of student research experiences is highly correlated with successful match into the medical specialties that have traditionally been viewed as competitive [18]. Thus, research is now more crucial than ever in the match of osteopathic students into residency programs. Unfortunately, there is an evident disparity between the research conducted by osteopathic and allopathic students [19], 20]. This discrepancy is due to many factors that include decreased funding, opportunities, and interest. Although this is the case, medical student research is a vital part of acceptance into residency programs and is actively being addressed by many osteopathic medical schools, such as the Lake Erie College of Osteopathic Medicine (LECOM).
LECOM is the nation’s largest medical school, with 2,751 students enrolled in its DO program in the Fall of 2023 [21]. Its inaugural campus is in Erie, PA, with additional locations in Greensburg, PA, Elmira, NY, and Bradenton, FL. As noted in the mission statement, LECOM is dedicated to preparing future osteopathic physicians by emphasizing excellence in education, research, clinical care, and community service, with the overarching goal of improving the quality of life and healthcare for all humanity [22]. To help fulfill the research goals set forth in its mission statement, a Summer Research Internship Program was established in 2023 by LECOM-Bradenton with several distinct goals and potential outcomes. First, this program was designed to provide a structured and mentored research experience for DO students. Second, there was an intention to nurture a culture of research and scholarship among aspiring osteopathic physicians through engagement in scholarly experiences and opportunities to become producers as well as evaluators of medical knowledge. Third, a platform was provided for recognizing faculty members’ support as mentors for the student doctors’ research journeys. Finally, the achievements of students were celebrated in their scholarly pursuits, cultivating an atmosphere of academic excellence within the institution. This initiative builds upon literature calling for more equitable access to mentored research experiences [23], 24]. Previous initiatives such as the program at the Texas College of Osteopathic Medicine (TCOM) have demonstrated improvements in students’ understanding of biostatistics and epidemiology through curriculum enhancements [25]. However, the program in this study distinguishes itself by providing comprehensive quantitative data on research self-efficacy, research success, and internal program implementation.
To meet the aforementioned goals and objectives, students participated in a number of experiences through the Research Summer Internship Program, including faculty-guided research, a lecture series on research topics, and a culminating Capstone event, showcasing the students’ research projects and completion of the program. To further measure the success of the program, a series of pre- and postprogram surveys were administered. Therefore, the aim of this study was to quantitatively examine research experience and efficacy before and after the completion of the Research Summer Internship Program, hypothesizing that those in the program will have greater research experience and self-efficacy upon completion compared to a control group.
Methods
Institutional approval
This study was determined to be exempt from the LECOM Institutional Review Board review and approval. A protocol number (30–103) was established. All data recorded in this study were recorded without identifiers to preserve subject anonymity.
Informed consent
All participants in this study provided written informed consent prior to participation.
Participant compensation
No compensation was provided to the participants.
Participants
Thirty-eight osteopathic medical students (20 control and 18 experimental) in the graduating class of 2026 participated in the study. These participants were sampled from a college-wide email explaining the internship program and its study goals. Students were assigned to the experimental group or control group based on survey participation and their answers to the questions. The control group included 20 students from the class of 2026 who were selected based on their answers of “no” to questions 2–5 (Table 1). The experimental group consisted of 18 students who participated in the LECOM-Bradenton Summer Research Internship Program initiated in the early summer. Applicants for the program were required to have a 3.0 grade point average (GPA) for their first semester on campus (Fall 2022) without any concern about academic performance. In addition, three essay questions, a curriculum vitae, and one letter of recommendation from a current faculty member or former research mentor were required for the application process.
Survey questions utilized to recruit control subjects.a
| 1 | Are you interested in participating in this research study? |
| 2 | Are you participating in the LECOM summer research internship program? |
| 3 | Are you participating in a summer research program outside of LECOM? |
| 4 | Are you currently conducting research with a LECOM faculty member or outside researcher? |
| 5 | Are you planning to conduct research with a LECOM faculty member or outside researcher within the next year (now through May 2024)? |
-
aRespondents answered yes or no. LECOM, Lake Erie College of Osteopathic Medicine.
All 18 students in the experimental group attended an orientation session for the Summer Research Internship Program on May 17, 2023. At this orientation session, faculty members participating in the program presented their research interests and previous projects and interacted with students for potential summer research ideas. Within the next few months, the summer research interns were matched to faculty according to their mutual research interests.
Experimental protocol
A timeline highlighting the Summer Research Internship Program is depicted in Figure 1. Members of both the control and experimental groups were assigned random identification numbers, and each participated in a two-part pre-program questionnaire. Participants in the control group completed this survey on May 16, 2023, and the participants in the experimental group completed them at the orientation session on the next day during the orientation event. For the first part of the questionnaire (Table 2), participants were asked questions for yes or no answers, assessing previous research experiences and opportunities. For the second part of the questionnaire, they were instructed to complete a 15-question survey on research self-efficacy (Table 3). This survey was utilized to assess the research self-efficacy of participants in four distinct categories: (1) knowledge of research practice foundations; (2) ability to identify types of scholarly literature and sources; (3) individual motivations for conducting research; and (4) likelihood for future research being conducted. Question responses were on a Likert scale (1–5), in which 1=strongly disagree, 2=somewhat disagree, 3=neutral, 4=somewhat agree, and 5=strongly agree.
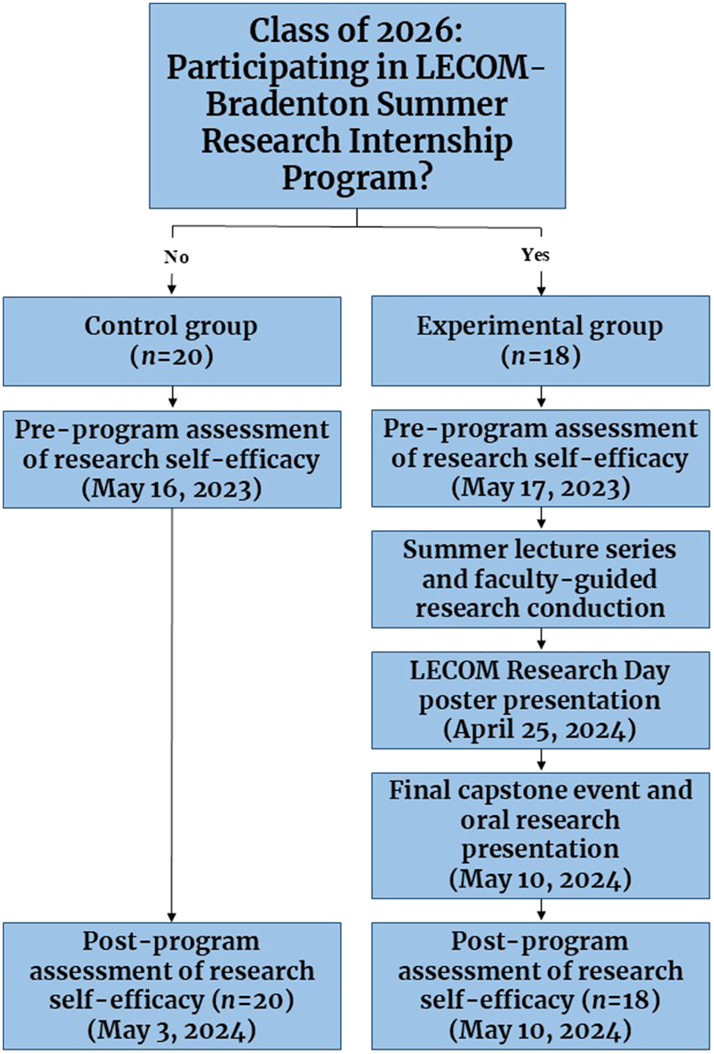
An overview of the class of 2026 LECOM summer research internship program study design.
Questionnaire assessing previous research experience and opportunities.a
| 1 | I have previous research experience prior to May 18, 2023. |
| 2 | I have had research education (structured course or research program including undergraduate course work, postgraduate program) prior to matriculation to medical school. |
| 3 | I have contributed to the creation of a research poster. |
| 4 | I have presented at LECOM research day. |
| 5 | I have contributed to a manuscript that has been submitted to a journal for publication. |
| 6 | I am a listed author of a research publication. |
| 7 | I have conducted research independent of the LECOM summer research internship program between the dates of May 18, 2023 and May 10, 2024.b |
-
aRespondents answered yes or no. bThis question was not on the preprogram survey. LECOM, Lake Erie College of Osteopathic Medicine.
The questionnaire utilized to assess research self-efficacy.a
| Category 1 – Assess knowledge of research practice foundations |
|---|
| 1. I know how to formulate a strong research question. |
| 2. I know how to utilize the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines for conducting a systematic review project. |
| 3. I know how to analyze data. |
| 4. I know how to write a manuscript (full or part). |
|
|
| Category 2 – Assess ability to identify types of scholarly literature and sources |
|
|
| 5. I know how to choose a journal to publish my research. |
| 6. I know the difference between a systematic review and a meta-analysis. |
| 7. I know the difference between a primary and secondary source of literature. |
| 8. I know how to utilize scholarly databases like PubMed, ScienceDirect, or scopus to find literature sources. |
|
|
| Category 3 – Assess individual motivations for conducting research |
|
|
| 9. A motivation of mine for conducting research is to build a strong resume/CV. |
| 10. A motivation of mine for conducting research is to help others. |
| 11. A motivation of mine for conducting research is for my own personal enjoyment. |
| 12. A motivation of mine for conducting research is to be competitive for residency applications. |
|
|
| Category 4 – Assess future research conduction |
|
|
| 13. I am aware of research opportunities provided by faculty at LECOM Bradenton. |
| 14. I Will conduct research as a future practicing physician. |
| 15. Conducting research is necessary for advances in the field of medicine. |
-
aResponses were based the Likert Scale: 1=strongly disagree, 2=somewhat disagree, 3=neutral, 4=somewhat agree, 5=strongly agree. LECOM, Lake Erie College of Osteopathic Medicine.
To build foundational knowledge on research basics and application, the students in the experimental group attended five distant live learning sessions on topics presented by two LECOM faculty and one third year DO student (Class of 2025) in the summer of 2023. Topics included research design, systematic reviews and meta-analyses, statistical analyses in research, writing manuscripts, and selecting journals. At the conclusion of the lecture series, students completed a knowledge assessment utilizing ExamSoft® consisting of multiple-choice questions. Additionally, the students received a questionnaire to provide feedback on the effectiveness of the presentations for each presenter, based on a 5-point Likert scale.
Throughout the term of this program, the students in the experimental group conducted their research studies under the direction of their faculty mentors. For certain projects, more than one student was involved in a study. The types of research included laboratory-based experimental research, osteopathic manipulative treatment (OMT)-related research, retrospective observational research, descriptive research utilizing survey questionnaires, case studies, and systematic reviews. The students presented their research findings in a poster format at LECOM’s Interprofessional Research Day on April 25, 2024. Finally, the students in the experimental group made a short oral presentation (∼10 min) on their research findings during the Capstone event on May 10, 2024. On the same day, the experimental groups completed surveys on previous research/opportunities (Table 2) and research self-efficacy (Table 3) for a second time. The control group completed the same surveys close to the Capstone event. The pre- and postprogram surveys were developed de novo to adequately measure the effectiveness of the program in promoting research self-efficacy.
Data analysis
The questionnaire in Table 2 examined previous research and opportunities for both the control and experimental groups. Yes or no responses were computed for each group for pre- and postprogram. To determine the differences in the responses between groups, a Fisher’s exact test was performed for questions 1–6. The Fisher’s exact test was utilized instead of a chi-square analysis because the sample size was small and did not follow a standard distribution. For this analysis, a p value less than 0.05 was considered statistically significant. Corrections for multiple comparisons were implemented through the Bonferroni Adjustment.
The research self-efficacy for four categories were examined utilizing questions in Table 3. Average responses for each question for each group were determined from the 5-point Likert scale. Separate paired-samples t tests for the experimental and control groups were performed to determine significant changes pre- vs postinternship program for each question in the survey. Separate independent-samples t tests were conducted to determine differences between the groups pre-internship and differences between groups postinternship for each question. For these analyses, a p value less than 0.05 was considered statistically significant. Finally, the data collected on participants’ feedback on the presenter’s performance during summer learning sessions were analyzed. For this assessment, the mean and standard deviation (SD) of the student responses for each presenter were determined.
Results
The results from the previous research/opportunities survey (Table 2) at various time-points are illustrated in Figure 2. As shown in this figure, the experimental group had significantly (p<0.05) more experience with various research-related activities, such as research participation, poster creation and presentation, and publication prior to the start of the LECOM Summer Internship (preprogram) compared to controls, except with previous research education. These findings were mirrored for the postprogram assessment, but the experimental group responded more positively (p<0.05) regarding manuscript contribution. A pre- vs postprogram assessment in the experimental group yielded a significant (p<0.05) positive change for LECOM Research Day presentation items. Interestingly, no significant changes across conditions were found for the control group at two different time-points.
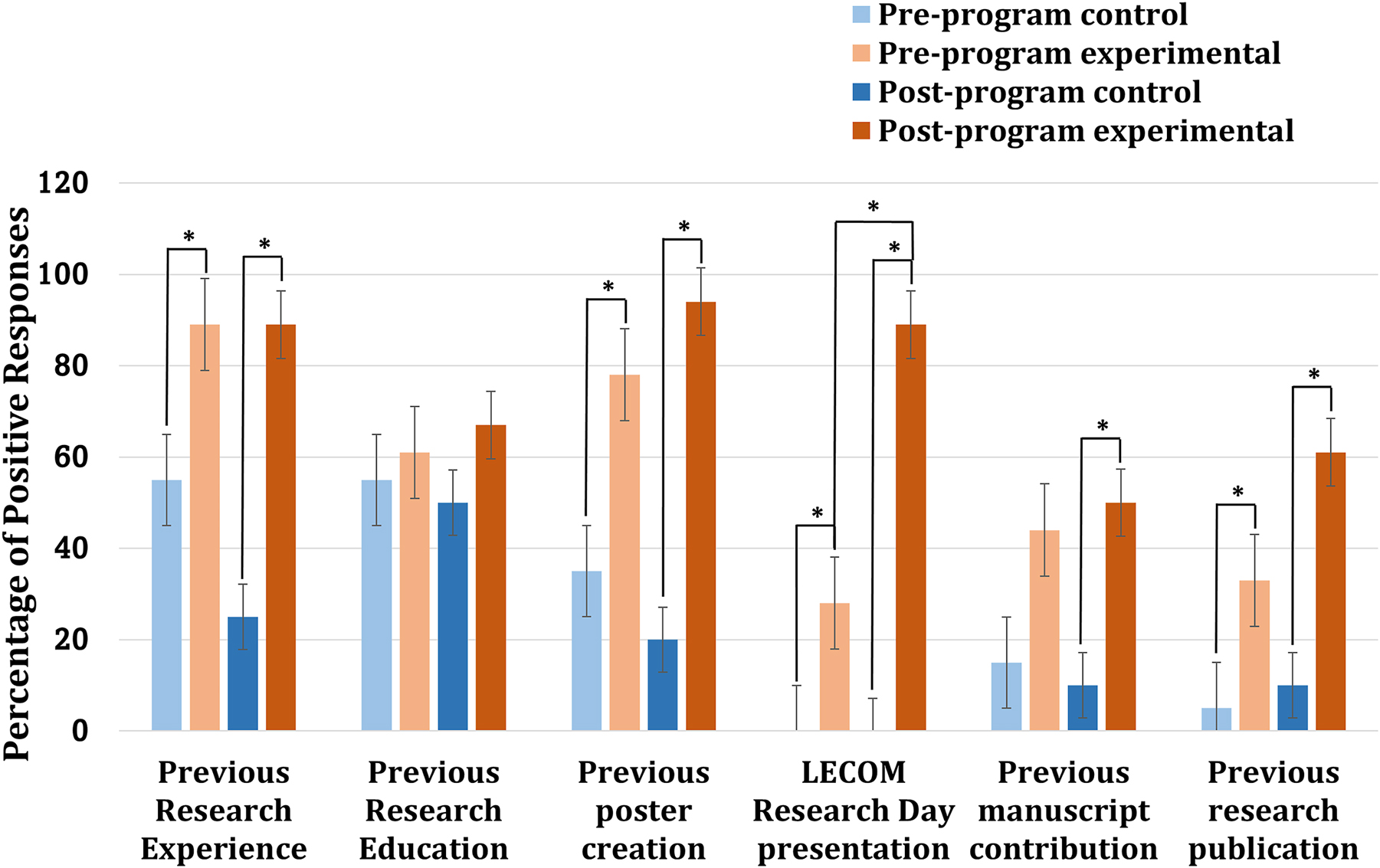
The number of positive responses to yes-or-no questions as part of the previous research/opportunity survey. Data are expressed as mean ± SD (n=18). *p<0.05 based on Fisher’s exact test.
Analyses of the individual 15 questions from the research self-efficacy questionnaire (Table 3) were examined, and the results between groups (experimental vs control) and between conditions (pre- vs postinternship program) are displayed in Figure 3. In essence, the experimental group indicated statistically greater (p<0.05) knowledge on research practices, the ability to identify and distinguish between sources and databases, and more motivation to conduct research for personal and professional reasons, compared with controls, prior to the start of the program. These responses were further accentuated after the conclusion of the program. The experimental group was also significantly (p<0.05) more aware of research opportunities at LECOM postprogram compared to preprogram. The experimental group also expressed greater (p<0.05) interest in conducting research as a future physician prior to and at the end of the program. They also expressed greater need for research to advance the field of medicine compared with controls, but this finding was only significant (p<0.05) during the preprogram survey.
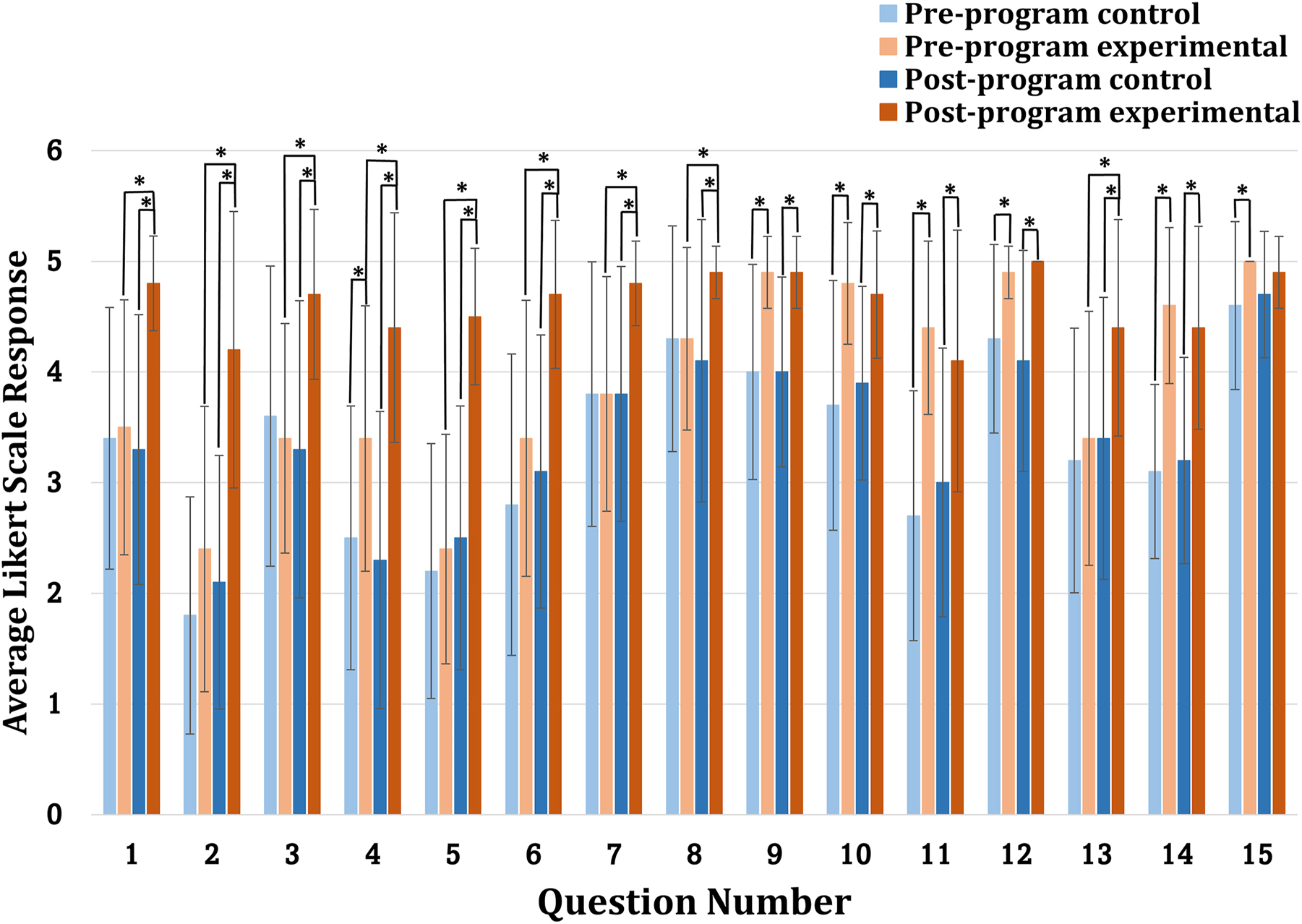
The average Likert scale responses to the research self-efficacy questionnaire. Data are expressed as mean ± SD (n=18). *p<0.05 by paired-samples or independent-samples t-test.
The average responses for the self-efficacy categories of the research self-efficacy questionnaire can be found in Figure 4. Prior to the start of the program, the experimental group expressed more (p<0.05) motivation to perform research compared to controls, but no differences between groups were found for research foundations, identifying literature, and the potential for future research. However, at the conclusion of the program, the experimental group indicated more knowledge of research (p<0.05), ability to identify scholarly sources (p<0.05), and greater motivation for research (p<0.05) than controls. Although mean responses for assessing the likelihood of future research engagement were consistently higher in the experimental group at both time-points, these differences did not reach statistical significance (p>0.05). Finally, the experimental group indicated greater (p<0.05) knowledge in research and identifying sources after the program vs at the beginning. No significant changes across conditions were found in the control group at the two different time-points.
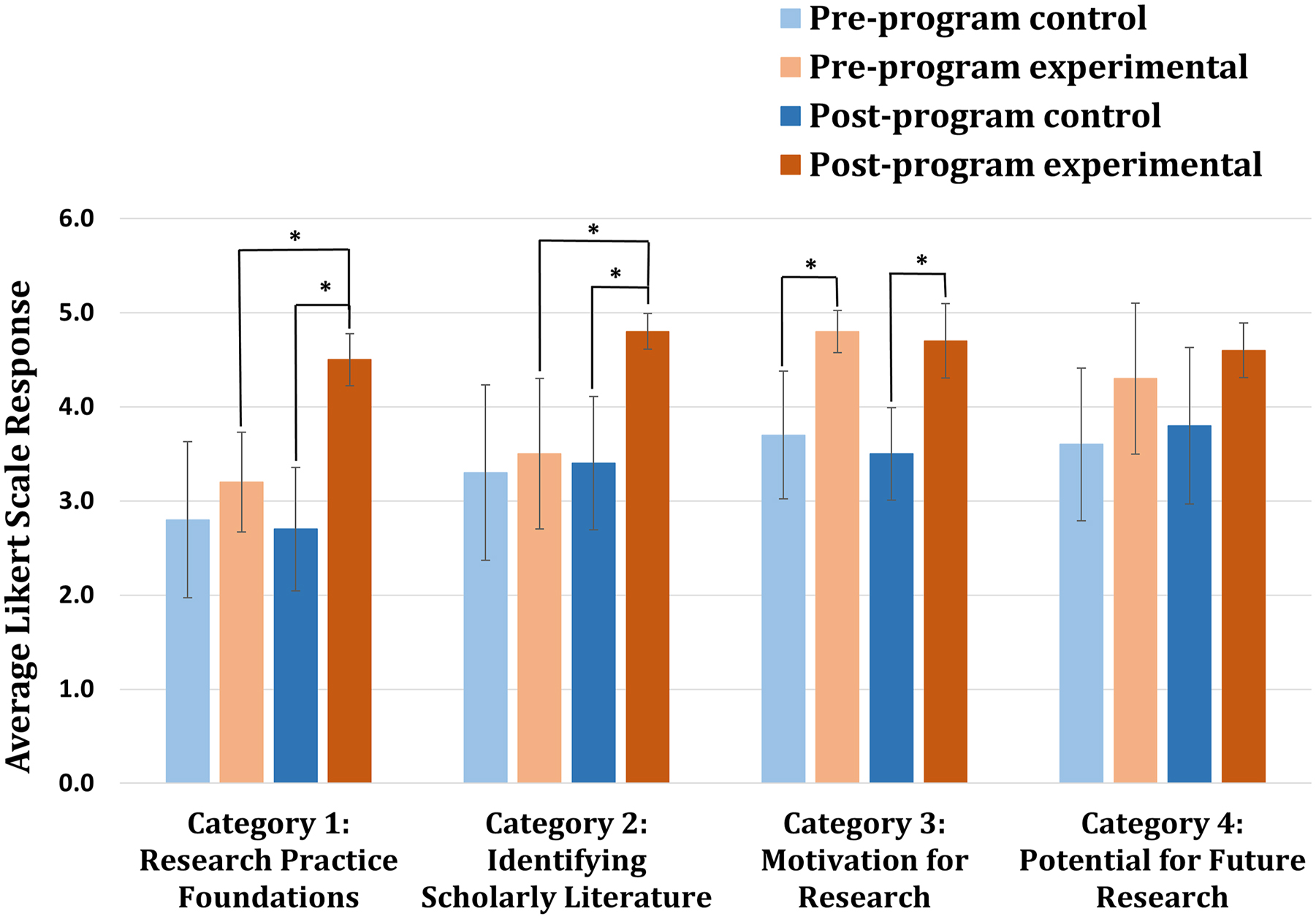
The average Likert scale responses across various research self-efficacy categories. Data are expressed as mean ± SD (n=18). *p<0.05 by paired-samples or independent-samples t-test.
Finally, the results from the participant satisfactory survey from the summer learning series are displayed in Table 4. Overall, the effectiveness of each presentation was established based on student satisfaction, which shows a Likert response of 4.6 or greater for each presenter evaluation question. Notably, the students in the program participated in an ExamSoft® survey to test their proficiency on the subject areas taught during various learning sessions. Every student in the program demonstrated a proficiency level above 70.0 % for the materials presented in all sessions.
Participant satisfaction with summer learning session presentations.a
| Evaluation items | Response for each presenter | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Presenter demonstrated knowledge of the subject. | 4.9 ± 0.32 | 4.8 ± 0.42 | 4.8 ± 0.42 |
| Presenter exhibited enthusiasm about the subject. | 4.9 ± 0.32 | 4.9 ± 0.32 | 4.7 ± 0.48 |
| Topics were presented in a clear and organized manner. | 4.9 ± 0.32 | 4.8 ± 0.42 | 4.7 ± 0.48 |
| Presenter made effective use of time. | 4.7 ± 0.48 | 4.8 ± 0.42 | 4.8 ± 0.42 |
| Presenter spoke clearly and at a comfortable pace. | 4.9 ± 0.32 | 4.9 ± 0.32 | 4.9 ± 0.32 |
| Presenter emphasized key points. | 4.9 ± 0.32 | 4.8 ± 0.42 | 4.9 ± 0.32 |
| Presenter summarized the session effectively. | 4.8 ± 0.42 | 4.9 ± 0.32 | 4.7 ± 0.48 |
| Presenter engaged students during the presentation(s). | 4.9 ± 0.32 | 4.9 ± 0.32 | 4.6 ± 0.52 |
| Presenter created an environment that allowed questions and discussion as well as demonstrated respect for learners. | 4.9 ± 0.32 | 4.9 ± 0.32 | 4.9 ± 0.32 |
| Presenter utilized educational technology effectively. | 4.8 ± 0.42 | 4.8 ± 0.42 | 4.8 ± 0.42 |
| Overall, the session(s) was (were) effective. | 4.7 ± 0.48 | 4.9 ± 0.32 | 4.9 ± 0.32 |
-
aResponses were based on the Likert Scale: 1=strongly disagree, 2=somewhat disagree, 3=neutral, 4=somewhat agree, 5=strongly agree. Results are expressed as mean ± SD.
Discussion
This study examined the success of LECOM-Bradenton Summer Research Internship Program through the use of surveys that assessed research experience, research self-efficacy, and presentation effectiveness of the faculty presentations. The results showed that significant positive changes in the experimental group (student research interns) were observed in comparison to the control group. This includes improvements in research experiences, greater knowledge of research practice foundations, identifying scholarly sources, and greater motivation to perform scholarly activities in the present as well as in the future.
It is important to acknowledge potential selection bias in interpreting these results. Students in the experimental group applied to and were accepted into the program, and they demonstrated higher baseline motivation toward research. This method of selection was necessary for a novel program requiring a significant time commitment and demonstrated interest. The reliance on self-reported data from Likert scale could also introduce a response bias because participants may overestimate or underestimate their attitudes, as previously reported in the literature [26]. To mitigate other forms of bias, survey data were collected from all participants utilizing the same procedures before and after the program. The use of random identification numbers assigned by an external source helped reduce the potential for researcher bias in data collection and analysis.
Three main conclusions can be gleaned from the results of the study. First, the initial goals of the Summer Research Internship Program were met. The program did provide a structured and mentored research experience for each DO student who participated in the program, through activities and experiences as well as faculty mentoring. A previous study has shown that osteopathic medical students have reported a lack of access to research opportunities and mentors and a deficit in knowledge of research methodology as barriers to conducting research [12]. Creation of the summer research program tackled these barriers head on by providing guidance in the research conduction process and facilitation of the formation of longitudinal relationships with mentors. The knowledge and mentorship gained from this experience extends well beyond the duration of the program, setting up participants for potential success in future research endeavors.
Secondly, the internship was a success in that the experimental group was able to build upon their existing research experiences. This was evident by their positive responses to the surveys postprogram (Figures 2–4). Overall, the results from this study underscore the positive influence that the Summer Research Internship Program had on DO students at LECOM-Bradenton. Significant improvements in the abilities to analyze data, write a manuscript, and choose a journal for publication highlight the positive impact of structured research opportunities provided to the osteopathic medical students. These skills can be transferred to future projects during rotations, residency, and beyond.
Thirdly, participation in the internship program positively influenced the experimental groups’ ability to learn new skills and knowledge to successfully complete a scholarly research project within one year. This was evident not only by increased positive responses to the research-efficacy survey, but also through the successful poster creation and presentation at the 2024 LECOM Interprofessional Research Day. A total of 11 posters were presented at the LECOM Interprofessional Research Day on April 25, 2024, and nine posters were presented at various national conferences to date. Moreover, at least two articles [27], 28] based on completed projects have been published in peer-reviewed journals so far, one manuscript is under review, and several manuscripts are in preparation. These scholarly outputs are consistent with current literature suggesting that structured research opportunities can improve both confidence and competence in research practices [23], 24]. The experimental group was also highly motivated to conduct research from the start of the program, and the motivation for research remained high in the experimental group after completion of this formal, structured research program. Existing evidence suggests that medical students have a high level of motivation for conducting research [29], 30]. This also stems from increased motivation to pursue research to increase competitiveness for residency [31], 32]. However, an important consideration is the role of baseline differences in motivation. The experimental group exhibited higher motivation to conduct research even before the program began. This suggests that at least part of the observed gains in self-efficacy may reflect pre-existing interest. Nevertheless, the program appears to have reinforced this motivation according to our data.
Interestingly, both the experimental and control groups expressed the necessity of conducting research to advance the field of medicine (Category 4, Table 3). However, the experimental group stated that they were more likely to conduct research as a future practicing physician compared with the control group. These findings corroborate with a previous study that showed that many osteopathic medical students recognize the importance of research, but not all of them wish to pursue research opportunities [13]. The differences in responses for the experimental and control groups possibly indicates an extrinsic motivation to perform research in the experimental group. This group was also given the necessary tools and experiences to help nurture a culture of scholarship in these individuals through the LECOM Summer Internship Program.
The relatively small sample size, with only 18 participants in the experimental group and 20 in the control group, may limit the generalizability of the results. In the future, this program plans to increase sample size by expanding cohort sizes. This study only analyzes the short-term effects immediately following program completion. The long-term impact of this program remains unexplored. However, there are plans for longitudinal follow-up to evaluate outcomes aligned with the program’s goals. Namely, students will be followed for continued participation in poster/podium presentation, manuscript submissions and publications, and residency application performance. In addition to pre-residency outcomes, we hope to track research engagement during residency to help evaluate the durability of the program’s impact on research engagement beyond medical school.
Conclusions
The LECOM-Summer Research Internship Program was successful in improving research experience and self-efficacy among its participants, especially across the metrics of research practice foundations and identifying scholarly literature. This success can be attributed to how the program provided LECOM-Bradenton medical students in the graduating class of 2026 a structured research mentorship and education. The program’s success in increasing research experience and self-efficacy among this cohort of osteopathic medical students shows promise that the implementation of a structured research program can bridge the gap between osteopathic and allopathic medical students in terms of research accessibility, productivity, and increasing residency competitiveness. Given its clearly defined structure and measurable outcomes, this program may serve as a scalable model for other osteopathic institutions seeking to enhance student research engagement and foster a culture of scholarship.
Acknowledgments
The authors are indebted to Mark Kauffman, DO (Dean of Academic Affairs, LECOM-Bradenton, FL) and other participating faculty at LECOM-Bradenton, FL, for support with the Summer Research Internship Program; Irv Freeman, PhD, JD (LECOM Health, Erie, PA), for critical discussion about the study design; and Nathan Quint (Research Analyst, LECOM-Erie, PA) for assistance with data analysis.
-
Research ethics: This study (protocol # 30-103) was approved as exempt by the LECOM Institutional Review Board.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: The following authors contributed equally: Michael A. Wallace, MMS, MS; Adam K. Bobak, BS, and Tianna L. Sasher, BS. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: Data is available upon request.
References
1. Beauchemin, M, Cohn, E, Shelton, RC. Implementation of clinical practice guidelines in the healthcare setting: a concept analysis. ANS Adv Nurs Sci 2019;42:307–24. https://doi.org/10.1097/ANS.0000000000000263.Search in Google Scholar PubMed PubMed Central
2. Hu, VH. Why does research matter? Community Eye Health 2022;35:1–3.Search in Google Scholar
3. Lee, GSJ, Chin, YH, Jiang, AA, Mg, CH, Nistala, KRY, Iyer, SG, et al.. Teaching medical research to medical students: a systematic review. Med Sci Educ 2021;31:945–62. https://doi.org/10.1007/s40670-020-01183-w.Search in Google Scholar PubMed PubMed Central
4. D’Arrietta, LM, Vangaveti, VN, Crowe, MJ, Malau-Aduli, BS. Rethinking health professionals’ motivation to do research: a systematic review. J Multidiscip Healthc 2022;15:185–216. https://doi.org/10.2147/JMDH.S337172.Search in Google Scholar PubMed PubMed Central
5. Berg, EJ, Ashurst, J. Patterns of recent national institutes of health (NIH) funding in general surgery: analysis using the NIH RePORTER system. Cureus 2019;11:e4938. https://doi.org/10.7759/cureus.4938.Search in Google Scholar PubMed PubMed Central
6. Cuoco, JA, Klein, BJ, Kar, A, Gosnell, HL, Guilliams, EL, Benko, MJ, et al.. Factors affecting R01 grant funding among academic neurosurgeons over the last decade. Ann Med Surg (Lond) 2020;55:260–4. https://doi.org/10.1016/j.amsu.2020.06.002.Search in Google Scholar PubMed PubMed Central
7. Iwai, Y, Lenze, NR, Becnel, CM, Mihalic, AP, Stitzenberg, KB. Evaluation of predictors for successful residency match in general surgery. J Surg Educ 2022;79:579–86. https://doi.org/10.1016/j.jsurg.2021.11.003.Search in Google Scholar PubMed
8. Huang, A, Gunther, JR, Lin, LL. Analyzing the role of research in the radiation oncology match. Adv Radiat Oncol 2022;7. https://doi.org/10.1016/j.adro.2021.100891.Search in Google Scholar PubMed PubMed Central
9. Colosimo, C, Mann, DR, Bhuller, S, Opie, D, Beam, Z, Yon, J, et al.. Bridging the gap: how to get osteopathic residents into fellowships. Cureus 2022;14. https://doi.org/10.7759/cureus.27980.Search in Google Scholar PubMed PubMed Central
10. Ahmed, AK, Adashi, EY. Research Fever-An ever more prominent trend in the residency match. JAMA Surg 2023;158:6–8. https://doi.org/10.1001/jamasurg.2022.3190.Search in Google Scholar PubMed
11. Research Requirement for Medical Students. AAMC. Available from: https://www.aamc.org/data-reports/curriculum-reports/data/research-requirement-medical-students.Search in Google Scholar
12. Ho, A, Auerbach, A, Faulkner, JJ, Guru, SK, Lee, A, Manna, D. Barriers to research opportunities among osteopathic medical students. J Osteopath Med 2023;123:187–94. https://doi.org/10.1515/jom-2022-0116.Search in Google Scholar PubMed
13. Nguyen, V, Kaneshiro, K, Nallamala, H, Kirby, C, Cho, T, Messer, K, et al.. Assessment of the research interests and perceptions of first-year medical students at 4 colleges of osteopathic medicine. J Osteopath Med 2020;120:236–44. https://doi.org/10.7556/jaoa.2020.040.Search in Google Scholar PubMed
14. Burch, J, Leavitt, R, Smith, F, Curtis, JP. Common paths in medical education: an updated look at the training of allopathic, osteopathic, and naturopathic physicians. Integr Med (Encinitas) 2022;21:20–9.Search in Google Scholar
15. Cummings, M. The single accreditation system: risks to the osteopathic profession. Acad Med 2021;96:1108–14. https://doi.org/10.1097/ACM.0000000000004109.Search in Google Scholar PubMed
16. Taparra, K, Ebner, DK, De La Cruz, D, Holliday, EB. Away rotations, interviews, and rank lists: radiation oncology residency applicant perspectives on the 2020 match process. Adv Radiat Oncol 2021;6:100696. https://doi.org/10.1016/j.adro.2021.100696.Search in Google Scholar PubMed PubMed Central
17. White, PB, Henry, JP, Partan, MJ, Choy, K, Hogge, CA, Katsigiorgis, G, et al.. Differences in fourth-year orthopaedic away rotation opportunities and fees among osteopathic and allopathic medical students 1 year after the implementation of the single accreditation system. JB JS Open Access 2022;7:e22.00057. https://doi.org/10.2106/JBJS.OA.22.00057.Search in Google Scholar PubMed PubMed Central
18. Vaysburg, DM, Cortez, AR, Hanseman, DJ, Delman, AM, Morris, C, Kassam, AF, et al.. An analysis of applicant competitiveness to general surgery, surgical subspecialties, and integrated programs. Surgery 2021;170:1087–92. https://doi.org/10.1016/j.surg.2021.03.035.Search in Google Scholar PubMed
19. Hamby, T, Wilson, DP, Bui, P, Lowery, J, Basha, R. Medical student research opportunities: a survey of osteopathic medical schools in the United States. J Osteopath Med 2022;122:289–95. https://doi.org/10.1515/jom-2021-0242.Search in Google Scholar PubMed PubMed Central
20. Matthews, CN, Estrada, DC, George-Weinstein, M, Claeson, KM, Roberts, MB. Evaluating the influence of research on match success for osteopathic and allopathic applicants to residency programs. J Am Osteopath Assoc 2019;119:588–96. https://doi.org/10.7556/jaoa.2019.102.Search in Google Scholar PubMed
21. Facts | The Lake Erie College of Osteopathic Medicine (LECOM) |Erie, PA. Lake Erie college of osteopathic medicine. Available from: https://lecom.edu/facts/.Search in Google Scholar
22. LECOM Mission. Lake Erie college of osteopathic medicine. Available from: https://lecom.edu/about/mission/.Search in Google Scholar
23. Cain, L, Kramer, G, Ferguson, M. The medical student summer research program at the university of Texas medical branch at galveston: building research foundations. Med Educ Online 2019;24:1581523. https://doi.org/10.1080/10872981.2019.1581523.Search in Google Scholar PubMed PubMed Central
24. Black, ML, Curran, MC, Golshan, S, Daly, R, Depp, C, Kelly, C, et al.. Summer research training for medical students: impact on research self-efficacy. Clin Transl Sci 2013;6:487–9. https://doi.org/10.1111/cts.12062.Search in Google Scholar PubMed PubMed Central
25. Smith-Barbaro, P, O-Yurvati, AH. Programmatic approach to increasing osteopathic medical student participation in research: the TCOM experience. J Am Osteopath Assoc 2016;116:747–52. https://doi.org/10.7556/jaoa.2016.14626.Search in Google Scholar
26. Fowler, FJ. Survey research methods, 5th ed. Thousand Oaks, CA, USA: SAGE Publications; 2013.Search in Google Scholar
27. Bishayee, A, Kavalakatt, J, Sunkara, C, Johnson, O, Zinzuwadia, SS, Collignon, TE, et al.. Litchi (Litchi chinensis Sonn.): a comprehensive and critical review on cancer prevention and intervention. Food Chem 2024;457:140142. https://doi.org/10.1016/j.foodchem.2024.140142.Search in Google Scholar PubMed
28. Bobak, A, Steves, M, McMahon, E, Spahiu, M, Rahman, ASW, Casarcia, N, et al.. Potential of phytochemicals for pharmacotherapy of glioblastoma multiforme: progress, pitfalls, and promise. Phytomedicine 2025;144:156850. https://doi.org/10.1016/j.phymed.2025.156850.Search in Google Scholar PubMed
29. Carter, J, McClellan, N, McFaul, D, Massey, B, Guenther, E, Kisby, G. Assessment of research interests of first-year osteopathic medical students. J Am Osteopath Assoc 2016;116:472–8. https://doi.org/10.7556/jaoa.2016.09128.Search in Google Scholar
30. Jimmy, R, Palatty, PL, D’Silva, P, Baliga, MS, Singh, A. Are medical students inclined to do research? J Clin Diagn Res 2013;7:2892–5. https://doi.org/10.7860/JCDR/2013/6698.3786.Search in Google Scholar PubMed PubMed Central
31. Mahmood Shah, SM, Sohail, M, Ahmad, KM, Imtiaz, F, Iftikhar, S. Grooming future physician-scientists: evaluating the impact of research motivations, practices, and perceived barriers towards the uptake of an academic career among medical students. Cureus 2017;9:e1991. https://doi.org/10.7759/cureus.1991.Search in Google Scholar PubMed PubMed Central
32. Pathipati, AS, Taleghani, N. Research in medical school: a survey evaluating why medical students take research years. Cureus 2016;8:e741. https://doi.org/10.7759/cureus.741.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

