Abstract
Context
Across eight classes at Lincoln Memorial University – DeBusk College of Osteopathic Medicine (DCOM), survey data reveal a decrease in students’ identification with osteopathy, which is what distinguishes an osteopathic physician’s values, attitudes, and commitment to the tenets of osteopathy. Without intervention, this trend of decreasing osteopathic identification may produce future generations of osteopaths who devalue the specific tenets of osteopathy.
Objectives
This study aims to determine factors that influence a student’s identification with osteopathy, as quantified by Likert-style survey response data, and to precisely quantify these factors’ predictive effect on osteopathic identification while simultaneously controlling for other possibly confounding factors. We hypothesize that preparedness and osteopathic manipulative medicine (OMM) skills will be the strongest predictors of osteopathic identification.
Methods
We utilized retrospective survey data from 1991 past DCOM students. Identifying data were redacted and replaced with research IDs. The survey contained an item that gauged respondents’ identification with osteopathy. To explore our primary objective, we utilized paired samples t tests to determine changes in osteopathic identification from matriculation to graduation within each class, as well as Pearson’s correlation coefficient to determine each item’s correlation with osteopathic identification. To explore objective 2, we utilized multiple regressions and structural equation modeling (SEM) path analyses to quantify these factors’ ability to predict osteopathic identification.
Results
Osteopathic identification decreased between matriculation and graduation for each class (10–21 % decrease, p<0.001). Feeling highly motivated to serve the community correlated best with osteopathic identification upon matriculation (r=0.2; p<0.001). One’s perception of one’s OMM skills – both in explaining OMM philosophy (r=0.5; p<0.001) and utilizing OMM (r=0.5; p<0.001) – as well as feeling happy to be an osteopath (r=0.6; p<0.001), best correlated with osteopathic identification upon graduation. OMM Skills have the greatest direct predictive effect on osteopathic identification, with an effect size of 0.4 (p<0.001). Commitment to Organization, mediated by both OMM Skills and Preparedness, has the greatest overall predictive effect on osteopathic identification, with an effect size of 0.6 (p<0.001).
Conclusions
The current study builds on past research by utilizing SEM path analysis to elucidate the predictive value of multiple factors on osteopathic identification. Application of the current study should consider looking at interventions geared toward increasing students’ OMM skills as well as their commitment to their institution, field, and career overall.
Research on professional identity formation reveals multiple factors that may influence someone’s sense of professional identity. In a survey study of 491 medical students, Draper and colleagues [1] elucidated variables involved in at least two dimensions of osteopathic identification: attitudes toward the osteopathic philosophy and plans to utilize osteopathic manipulative medicine OMM in their practice. Results showed that students who had received OMM previously identified more strongly with osteopathy and expressed greater intention to utilize OMM as part of their clinical skill sets [1]. Furthermore, students who applied solely to Doctor of Osteopathy (DO) programs expressed more positive attitudes toward the philosophy and a greater intention to utilize OMM [1]. Finally, a student’s class year also affected views within these two dimensions, with first-year students expressing more positive views toward the philosophy and a greater intention to utilize OMM relative to second-year students [1].
Looking at professional identity development more broadly, Clarkson and Thomson [2] further elaborate on past findings by suggesting an influence of stage of development in a study that included semi-structured interviews of eight fourth-year osteopathic medical students. Specifically, participants who saw their professional identity as being “constructed” were more confident in their role as osteopaths, whereas those whose professional identity development was “under construction” expressed uncertainty about their place in osteopathic medicine [2]. Furthermore, a longitudinal study surveying 85 participants looking at the development of identification with the medical profession more broadly reveals an effect of level of preparedness for clinical practice, with students who felt more prepared for clinical practice also reported a stronger subjective sense of their professional identity [3].
Finally, the work of Kasiri-Martino and Bright [4] examined nine osteopathic educators’ views of osteopathic principles as they relate to the broader osteopathic field. Results found stark differences between educators’ attitudes among a number of dimensions, including the educational relevance and professional significance of many osteopathic principles, and even the very definition of ‘osteopathic principles’. Such results suggest that the tensions that many students face in identifying with the osteopathic approach may not be limited only to students but rather may permeate more deeply into the osteopathic profession as a whole.
The current study aims to further elucidate the mechanisms associated with the development of professional identity in osteopathic medical students. Therefore, we propose the following research question: what factor(s) are associated with Lincoln Memorial University – Debusk College of Osteopathic Medicine (DCOM) graduates’ identification with the osteopathic approach? We define the osteopathic approach as an approach to patient care that both embodies the four osteopathic tenets and the utilization of OMM as a treatment modality where appropriate. For the purposes of this study, identification with osteopathy (or osteopathic identification) will henceforth be utilized to describe respondents’ relative rating of the survey item, “To what degree do you identify with the osteopathic approach to patient care?”
The primary objective of this study is to determine factors that influence DCOM students’ osteopathic identification throughout the first four years of medical education. Based on past research, we hypothesize that items gauging preparedness and respondents’ comfortability with OMM will be the strongest predictors of osteopathic identification. Secondary objectives include quantifying these factors’ predictive effect on osteopathic identification, as well as extrapolating from the data to suggest interventions for application and further research.
Methods
This study was designated exempt by the DCOM Institutional Review Board (IRB# 1112.V0). DCOM rewarded a $2,000 grant as a stipend for summer living expenses to conduct this research.
This is a retrospective study that relied on data that had already been collected beginning in 2012. The Lincoln Memorial University –DCOM Academic Assessment team collected data through entry and exit surveys administered to all matriculating and graduating students, respectively. These data include an item gauging DCOM graduates’ identification with the osteopathic approach to patient care. The osteopathic approach to patient care is introduced to all incoming students during orientation at DCOM. It is then reinforced with a series of four courses over the two preclinical years, followed by workshops throughout the clinical years designed to immerse students in osteopathic principles and practices.
Data were collected for more than a decade, allowing the unique opportunity both to examine the differences between entrance and exit data and to examine a large pool of data on osteopathic identification. The exit survey also contains data including students’ feelings of preparedness for clinical practice, satisfaction with DCOM overall, satisfaction with the class size, and more. No compensation was granted for participating in the survey. A total of 1,991 students were surveyed, and all 1,991 students responded. The 100 % response rate was because students were required to complete the entrance and exit surveys to receive their first set of examination scores and to graduate, respectively.
Survey results were collected as averaged 4-point Likert data for the primary question, To what degree do you identify with the osteopathic approach to patient care? and related factors. Items of interest include graduates’ attitudes toward their path to osteopathy and to DCOM, their preparation at DCOM, and their confidence in performing various skills. Refer to Supplementary Tables A and B (the beginning and end of the program data, respectively) in the Appendix for a comprehensive list.
In preparing our dataset, respondents’ identifying information was redacted and replaced with Research IDs. For the Classes of 2014–2019 and the Classes of 2021–2022, Research IDs for individual students were matched in both the entry and exit surveys. This allowed us to compare each student’s responses upon matriculation to their responses upon graduation. How the data were collected for the Class of 2020 meant that matching the Research IDs was not possible.
Responses were coded on a 1–4 scale, with 1 indicating “Strongly Disagree” and 4 indicating “Strongly Agree” for most items. For the Skills portion of each survey, responses were coded on a 1–3 scale, with 1 being “Inadequate/Not Confident” and 3 being “Excellent/Very Confident” in their skills. This was done for both the entry and exit data. Entry data were aggregated in two ways. First, all classes were combined into one dataset. Then, that dataset was split into Classes of 2014–2017 and Classes of 2018–2022. The decision to split the combined dataset was made in part based on the opening of the new campus, DCOM Knoxville, which began in 2019, and the DO-MD residency merger, which began in 2020. The exit survey data were divided into two datasets for the Classes of 2014–2019 and the Classes 2020–2022, reflecting both the DO-MD merger and revisions that were made to items on the exit survey.
Furthermore, the previously mentioned items were also grouped into traits, which serve as categories of similar items. This allowed us to treat our original ordinal, 4-point Likert data as a smaller set of continuously scaled data in our subsequent structural equation model (SEM) path analysis. As such, we grouped the survey items into the following traits: Preparedness, OMM Skills, Commitment to Organization, and Motivation. We adhered to a Cronbach’s alpha score >0.75 utilizing Statistical Product and Service Solutions (SPSS) for the items summed within each group (Table 1). As seen in Table 1, the OMM Skills trait measures respondents’ confidence in their own ability to utilize osteopathic diagnostic and treatment modalities, as well as their ability to articulate these osteopathic modalities to patients and colleagues.
For graduation survey data, similar items were grouped into “Traits,” which allowed us to treat our variables as continuous, rather than nominal, variables. Similarity of items comprising a Trait was measured utilizing Cronbach’s alpha with a minimum cutoff of 0.75.
| Cronbach’s alpha for grouped traits | ||
|---|---|---|
| Trait | Survey item | Cronbach’s alpha |
| OMM skills | Skills: utilizing basic OMM as diagnostic and treatment modalities | 0.870 |
| Skills: explaining OMM and the osteopathic approach to patients and other medical colleagues | ||
| Commitment to organization | I am happy that I chose to become an osteopathic physician. | 0.812 |
| I am happy I chose to attend DCOM. | ||
| DCOM treats all its students with equal fairness and consideration. | ||
| Motivation | Overall, I am satisfied with my life at the present time. | 0.768 |
| I have the coping skills and strategies needed to succeed in a challenging medical career. | ||
| I am an effective independent learner. | ||
| I am highly motivated to broadly serve my community. | ||
| Preparedness | I feel well prepared for upcoming residency/internship. | 0.850 |
| My elective rotations helped me prepare for the residency match. | ||
| DCOM staff provided adequate information to help with the residency match. | ||
| I received adequate information and guidance at/from DCOM to help me choose a realistic career path that fits my personal goals and interests. | ||
| The basic science knowledge I gained in the first 2 years of the program enabled me to succeed in my clinical rotations. | ||
| The EPC course series, especially my OSCE experiences, helped me to succeed in my clinical rotations. | ||
| During my rotations, I felt well supported by the DCOM clinical rotation staff. | ||
-
EPC, essentials of patient care; OMM, osteopathic manipulative medicine; OSCE, objective structured clinical exam.
Statistical analyses in SPSS were conducted by ZSK and CR. Statistical analyses in R were conducted by ZSK and TH. For our primary objective, we utilized paired-samples t-tests and Pearson’s r tests in SPSS. Paired-samples t-tests were utilized to pair respondents’ entry and exit responses and to compare them within each graduating class, allowing us to see how osteopathic identification changed from matriculation to graduation. Pearson’s r tests were utilized to determine which items correlated with the primary question, To what extent do you identify with the osteopathic approach to patient care? For our secondary objectives, we utilized multiple regressions in SPSS and SEM path analysis in the lavaan package in R Studio. Multiple regressions allowed us to preliminarily identify which items predicted a greater identification with osteopathy upon graduation while accounting for respondents’ identification with osteopathy upon matriculation. Multiple regressions can confirm that different variables do predict different portions of the variance in osteopathic identification, but multiple regressions cannot separate the direct and indirect effects of these variables. Thus, we also ran SEM path analyses on the trait data utilizing the lavaan package in the R programming language [5] to better elucidate direct and indirect effects of the groups of items on identification with osteopathy.
Results
Aggregate survey data of the classes of 2014–2022 showed that being highly motivated to broadly serve correlated most with osteopathic identification (n=1987; r=0.2; p<0.001) upon matriculation. In the 2014–2017 group, both life satisfaction (n=789; r=0.2; p<0.001) and being highly motivated to broadly serve (n=788; r=0.2; p<0.001) correlated with osteopathic identification. In the 2018–2022 group, being highly motivated to broadly serve correlated with osteopathic identification (n=1199; r=0.2; p<0.001) as well as life satisfaction (n=1197; r=0.1; p<0.001), which did not meet our minimal effect cutoff value of 0.2.
Paired-samples t-tests showed a decrease in respondents’ identification with osteopathy from matriculation to graduation across all years, and this decrease was consistently observed across all classes. The largest decreases in identification with osteopathy were observed in the Class of 2021 (entry mean=3.58, exit mean=2.82; mean difference=−0.76; 21 % decrease). Table 2 shows the results of the 2-tailed paired t tests; no corrections were performed for multiple comparisons.
A paired samples t-test showing change in osteopathic identification from matriculation (Entry Mean) to graduation (Exit Mean) within each graduating class. Due to how data were collected for the Class of 2020, paired samples t testing was not possible. Paired samples t-tests revealed a decrease in osteopathic identification in each graduating class, with the greatest difference being −21 % in the class of 2021.
| Paired-samples t-test: change in osteopathic identification between matriculation and graduation | |||||
|---|---|---|---|---|---|
| Class | Entry mean | Exit mean | Mean difference | % change | p-Value |
| 2014 | 3.6 | 3.1 | −0.5 | −15 % | <0.001 |
| 2015 | 3.7 | 3.2 | −0.5 | −13 % | <0.001 |
| 2016 | 3.6 | 3.3 | −0.4 | −10 % | <0.001 |
| 2017 | 3.6 | 3.1 | −0.5 | −13 % | <0.001 |
| 2018 | 3.6 | 3.0 | −0.6 | −17 % | <0.001 |
| 2019 | 3.5 | 2.9 | −0.6 | −16 % | <0.001 |
| 2020 | N/A | N/A | N/A | N/A | N/A |
| 2021 | 3.6 | 2.8 | −0.8 | −21 % | <0.001 |
| 2022 | 3.5 | 3.0 | −0.4 | −13 % | <0.001 |
Looking at graduate data, the correlations with osteopathic identification that were greatest in the 2014–2019 cohorts were comfort with rural living (n=1134; r=0.3; p<0.001) and being highly motivated to broadly serve (n=1134; r=0.3; p<0.001), followed by life satisfaction (n=1135; r=0.2; p<0.001). In the 2020–2022 cohort (Table 3), the three items that correlated most with osteopathic identification were feeling happy to be an osteopath (n=645; r=0.6; p<0.001), a component of trait: Commitment to Organization, followed by skills in both utilizing OMM (n=645; r=0.5; p<0.001) and explaining the OMM philosophy (n=645; r=0.5; p<0.001), both of which comprised the trait: Osteopathic Skills. Furthermore, other components of the trait: Commitment to Organization correlated moderately with osteopathic identification, including being happy with DCOM (n=645; r=0.5; p<0.001) and feeling that DCOM treats students fairly (n=645; r=0.4; p<0.001). Lastly, several components of the trait: Preparedness correlated moderately with osteopathic identification, including feeling that clinical coursework and practicals, such as Essentials of Patient Care (EPC) and the Objective Structured Clinical Exams (OSCEs), prepared students for rotations (n=645; r=0.4; p<0.001), and feeling that the school was instrumental in helping students both choose a career path (n=645; r=0.4; p<0.001) and complete the residency match (n=645; r=0.4; p<0.001).
Correlations with osteopathic identification in the graduation survey for classes of 2020, 2021, and 2022 aggregate data. The highest correlations with osteopathic identification were in traits osteopathic skills and commitment to organization.
| Correlations with osteopathic ID (2020–2022) graduation | |||||
|---|---|---|---|---|---|
| Trait | Item | Pearson’s r | Trait | Item | Pearson’s r |
| Osteopathic skills | Skills: utilizing OMM | 0.5 | Preparedness | Feel prepared for residency | 0.3 |
| Skills: explaining OMM philosophy | 0.5 | Felt supported during rotations | 0.4 | ||
| Satisfaction/commitment to organization | Happy to be an osteopath | 0.6 | EPC/OSCEs helped prepare me for rotations | 0.4 | |
| Life satisfaction | 0.2 | Basic sciences helped prepare me for rotations | 0.4 | ||
| Happy with DCOM | 0.5 | My elective rotations helped prepare me for residency match | 0.2 | ||
| Motivated to serve | 0.3 | DCOM helped me choose a career path | 0.4 | ||
| DCOM treats students fairly | 0.4 | DCOM helped me complete residency match | 0.4 | ||
-
DCOM, DeBusk college of osteopathic medicine; EPC, essentials of patient care; OMM, osteopathic manipulative medicine; OSCE, objective structured clinical exam.
In our multiple regressions, we wanted to see which items were most predictive of graduates’ osteopathic identification while accounting for their osteopathic identification upon matriculation. Results showed that being happy that one chose osteopathy was most predictive of graduate osteopathic identification (R2 change=0.4), followed by confidence in one’s OMM skills (R2 change=0.1).
For SEM path analysis, we utilized the traits defined above to test several hypothesized relationships between variables. Of the five models analyzed, the fifth model (Tables 4 and 5; and Figure 1) had the best fit indices. Specifically, the Akaike Information Criterion (AIC) of this fifth model was the lowest, the comparative fit index (CFI) was closest to 1, and the root mean square error of approximation (RMSEA) was not significant. The fit indices of the other four models are included in Supplementary Table D in the Appendix. Results of this model are described below in terms of the direct effects. Identification with osteopathy was predicted most by OMM Skills (0.4; p<0.001), followed by Commitment to Organization (0.4; p<0.001). OMM Skills, in turn, was also predicted by Commitment to Organization (0.3; p<0.001) and Preparedness (0.2; p<0.001). Finally, Preparedness was predicted by both Commitment to Organization (0.7; p<0.001) and Motivation (0.1; p<0.001).
Fit indices for the proposed SEM, Model 5, were the best of the tested models. This is exemplified by the relatively low AIC, the highest CFI, and the nonsignificant RMSEA. Fit indices for all tested models are included in Supplementary Table D in the Appendix.
| R fit indices | |
|---|---|
| Index | |
| Chi-square, df | 5.2 (3) |
| p value, chi-square | 0.2 |
| RMSEA | 0.034, 90 % CI [0.000, 0.081] |
| p value, RMSEA | 0.7 |
| SRMR | 0.0 |
| CFI | 1.0 |
| TLI | 1.0 |
| AIC | 6,650.1 |
-
AIC, Akaike information criterion; CFI, comparative fit index; RMSEA, root mean square error of approximation; SEM, structural equation model; SRMR, standardized root mean square residual; TLI, Tucker–Lewis index.
The standard effect sizes for each SEM path plotted, with the dependent variable of each SEM path in the far-left column.
| R standard effect size | |||
|---|---|---|---|
| Dependent variable | Independent variable | Standard effect size | p-Value |
| Preparedness | |||
|
|
|||
| Commitment to organization | 0.7 | 0.000 | |
| Motivation | 0.1 | 0.000 | |
| OMM skills | |||
| Commitment to organization | 0.3 | 0.000 | |
| Preparedness | 0.2 | 0.000 | |
| Osteopathic ID | |||
| OMM skills | 0.4 | 0.000 | |
| Commitment to organization | 0.4 | 0.000 | |
-
OMM, osteopathic manipulative medicine; SEM, structural equation model.
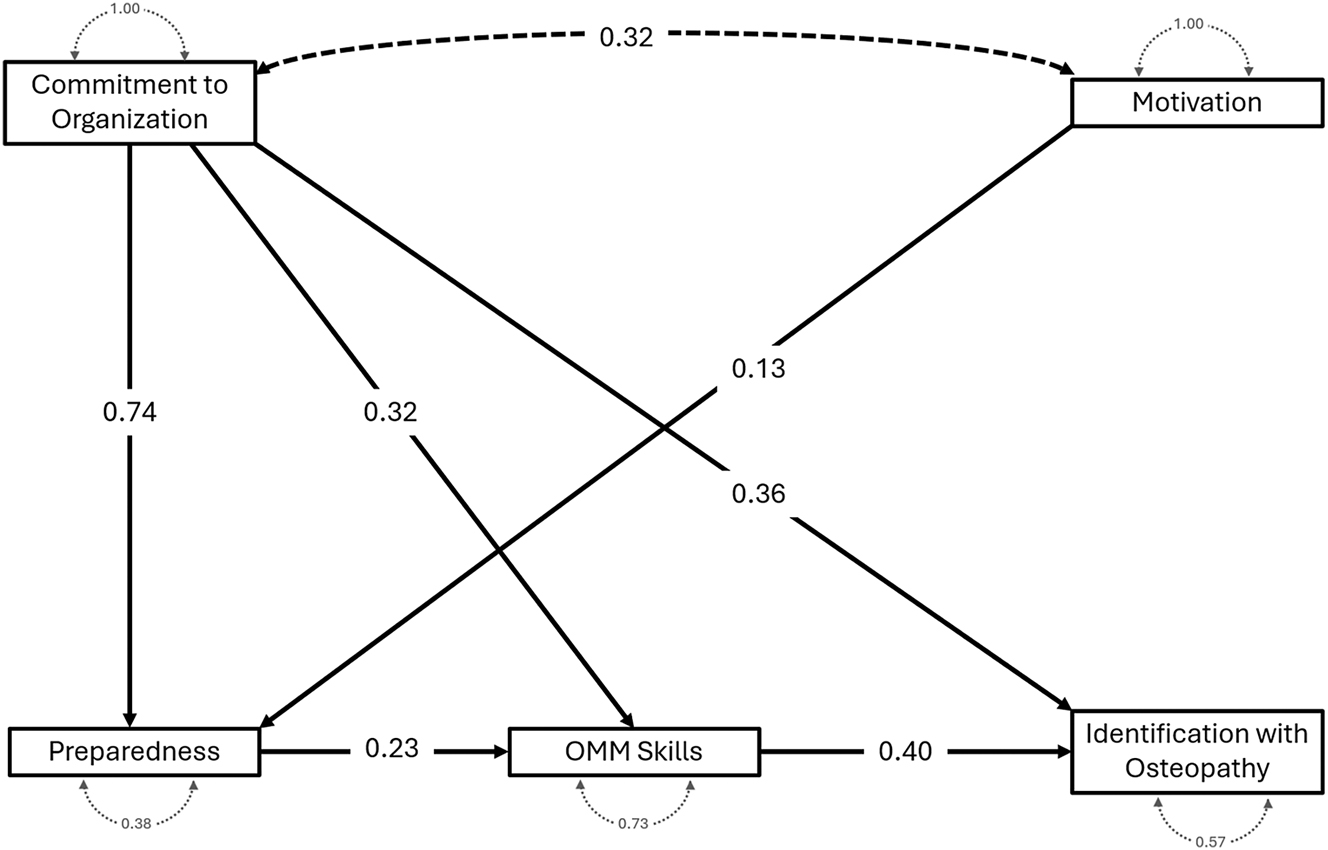
Structural equation modeling (SEM) path analysis showing the direct effects (black lines) with the standard effect size (labeled on each black arrow).
Given the direct effects of Commitment to Organization on other traits that either directly or indirectly predicted Osteopathic Identification, we analyzed indirect effects to quantify Commitment to Organization’s total effect on Osteopathic Identification. Accounting for Commitment to Organization’s indirect effect on Osteopathic Identification with OMM Skills alone as a mediator (0.1; p<0.001) and with Preparedness and OMM Skills together as mediators (0.1; p<0.001), the total effect of Commitment to Organization on Osteopathic Identification was 0.6 (p<0.001). Furthermore, because Preparedness and Motivation had no direct effect on Osteopathic Identification in this model, we calculated the indirect effect of Preparedness as 0.0 (p<0.01) and the indirect effect of Motivation as 0.1 (p<0.001).
Discussion
Our study demonstrates that osteopathic identification decreased during the 4 years at DCOM in all graduating classes upon which the paired-samples t-tests could be conducted; the degree to which identification decreased did not show any specific trend across cohorts. Furthermore, identification with osteopathy is most predicted by students’ commitment to their institution; students’ self-assessment of their OMM skills is the second strongest predictor.
The paired-samples t-tests that we ran comparing osteopathic identification upon matriculation with osteopathic identification upon graduation showed a consistent decline for each cohort in these values, which corroborates our problem statement that the current curriculum is not optimally fostering professional identity. When looking at entry correlations with osteopathic identification, being highly motivated to broadly serve was the only correlation across the aggregated data. This observation may result from there being a sense of excitement and accomplishment with matriculating to medical school. As such, future physicians just beginning this next step in their career may feel a greater sense of both motivation to serve and a greater identification with their future careers. When splitting the aggregate data at the Class of 2018, we saw that life satisfaction correlated well with osteopathic identification only prior to the Class of 2018. This may be because the MD/DO residency merger, or Single Accreditation System, was announced in 2015 and began to take effect shortly thereafter. Although the Single Accreditation System was not solidified until 2020, the changing landscape may have detracted from these later classes’ sense of life satisfaction. Specifically, the Single Accreditation System posed a hurdle to DO graduates interested in surgical and subspecialty programs, as well as a decrease in the number of DOs in educational leadership positions [6], 7].
Grouping our data into traits allowed us to focus our SEM analysis on a smaller set of summary “trait” variables. For example, Chaou et al. [3] found that students who reported a greater sense of preparedness were more likely to report a greater subjective sense of professional identity, whereas Draper et al. [1] found a correlation between experience with OMM and professional identity. As such, this grouping allows our study to be more directly comparable with this past research. Graduate data show that osteopathic identification correlates most with the items within the traits OMM Skills and Commitment to Organization. Utilizing SEM path analyses to look at direct effects only, it originally appeared that OMM Skills was the most predictive factor of Osteopathic Identification.
However, both direct and indirect effects of these traits on Osteopathic Identification showed that the total effect of Commitment to Organization predicted over half the variance of these traits on Osteopathic Identification, mediated by Preparedness and OMM skills. This suggests that, overall, Commitment to Organization is the most predictive factor influencing osteopathic identification. Thus, incentives geared toward fostering osteopathic identification should address the facets of the trait Commitment to Organization, including sentiments such as feeling one’s school treated them fairly and feeling that their institution adequately prepared them not only for osteopathic medicine, but also for the rest of their careers.
Another interesting finding from the SEM path analysis was that the models that examined direct effects of Preparedness and Motivation on Osteopathic Identification had worse fit indices than the current model. Furthermore, the indirect effects of these traits on the current model were small. This finding runs contrary to previous research [3], as well as to the trend that we saw in our own research when running correlations (Table 3), which showed large and significant correlations between multiple items within the trait: Preparedness with Osteopathic Identification. One explanation for this is that the items in the trait: Preparedness correlated well with other items that were in fact predictive of Osteopathic Identification, namely the traits: OMM Skills and Commitment to Organization. As our SEM analyses show, however, both Preparedness and Osteopathic Identification were predicted by Commitment to Organization, rather than Osteopathic Identification being directly predicted by Preparedness and Commitment to Organization.
Limitations
The current study is not without limitations. We utilized only previously collected data, which allowed us to garner hundreds of responses at the expense of being able to gear the survey items to our particular research question. Furthermore, for the Class of 2020, data were not collected in such a way as to allow the paired sample t-tests that we performed on other class years. A third limitation is that the data were collected utilizing an independent survey that has not been standardized or validated, leaving items open to ambiguity. Supplementary Tables A and B contain the items utilized in the survey. A fourth limitation of the study is that it was conducted entirely at a single osteopathic medical school. However, a potential benefit of utilizing such a sample is that all survey respondents were exposed to an identical curriculum for any given graduating class. Finally, data collection was continued unchanged throughout the COVID-19 pandemic. During the pandemic, many institutions underwent curriculum changes that limited in-person instruction in favor of virtual instruction, and it is worth considering whether these curriculum changes may have influenced responses during this time. Importantly, responses during the COVID-19 pandemic followed a trendline that had begun years prior to the pandemic, and this trend continued after the COVID-19 restrictions were lifted.
Conclusions
The current study shows that osteopathic identification does decrease from matriculation to graduation, suggesting that these 4 years are fertile ground for improvements geared toward increasing osteopathic identification. The current study has shown that one’s comfortability with their OMM skills has a direct predictive effect on osteopathic identification, and commitment to one’s institution has direct and indirect predictive effects on osteopathic identification. As such, application of the current study might take the form of an intervention geared toward capitalizing on this effect by including more frequent self-assessments of students’ OMM skills, which could help them develop a confidence and comfort with performing and explaining OMM. Furthermore, institutional improvements geared toward capitalizing on this effect could include activities and events that strengthen students’ connections with their academic community and institution. Finally, future research should also aim to elucidate the predictors of the items with the greatest effects on osteopathic identification (i.e., OMM skills and commitment to organization) such that interventions may be geared toward those predictors, which would in turn increase OMM skills and commitment to organization, ultimately bolstering student identification with osteopathic principles.
-
Research ethics: This study was designated exempt by the DeBusk College of Osteopathic Medicine Institutional Review Board (IRB# 1112.V0).
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: A grant of $2,000 was awarded by Lincoln Memorial University – DeBusk College of Osteopathic Medicine to serve as a stipend for summer living expenses to conduct research.
-
Data availability: The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Draper, BB, Johnson, JC, Fossum, C, Chamberlain, NR. Osteopathic medical students’ beliefs about osteopathic manipulative treatment at 4 colleges of osteopathic medicine. J Am Osteopath Assoc 2011;111:615–30.Search in Google Scholar
2. Clarkson, HJ, Thomson, OP. Sometimes I don’t feel like an osteopath at all’- a qualitative study of final year osteopathy students’ professional identities. Int J Osteopath Med 2017;26:18–27.10.1016/j.ijosm.2017.09.001Search in Google Scholar
3. Chaou, CH, Yu, SR, Chang, YC, Ma, SD, Tseng, HM, Hsieh, MJ, et al.. The evolution of medical students’ preparedness for clinical practice during the transition of graduation: a longitudinal study from the undergraduate to postgraduate periods. BMC Med Educ 2021;21:260.10.1186/s12909-021-02679-8Search in Google Scholar PubMed PubMed Central
4. Kasiri-Martino, H, Bright, P. Osteopathic educators’ attitudes towards osteopathic principles and their application in clinical practice: a qualitative inquiry. Man Ther 2021;21:233–40.10.1016/j.math.2015.09.003Search in Google Scholar PubMed
5. Rosseel, Y. lavaan: an R package for structural equation modeling. J Stat Software 2012;48:1–36. https://doi.org/10.18637/jss.v048.i02.Search in Google Scholar
6. Cummings, M. The impact of the ACGME/AOA single accreditation system on osteopathic surgical specialties, residents, and DO students. J Surg Educ 2021;78:1469–75.10.1016/j.jsurg.2021.02.006Search in Google Scholar PubMed
7. Cummings, M. The single accreditation system: risks to the osteopathic profession. Acad Med 2021;96:1108–14.10.1097/ACM.0000000000004109Search in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2024-0197).
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

