Stressbusters: a pilot study investigating the effects of OMT on stress management in medical students
-
Robert Valencia
, Gowtham Anche
, Gabriela Do Rego Barros
, Victor Arostegui
, Henal Sutaria
, Emily McAllister
, Mary Banihashem
Abstract
Context
Medical students report high levels of perceived stress and burnout, especially during the preclinical years. The combination of physical stressors from poor posture, poor sleep quality, and mental stressors from the rigorous curriculum stimulates the sympathetic nervous system (SNS) to secrete cortisol. Previous studies have shown that persistent elevated cortisol levels are associated with negative health outcomes.
Objectives
We conducted an Institutional Review Board (IRB)-approved study to determine if regular osteopathic manipulative treatments (OMTs) could impact the stress levels of first-year osteopathic medical students (OMSs) at Touro College of Osteopathic Medicine (TouroCOM) Harlem campus by measuring physiologic stress through changes in weekly salivary cortisol levels, perceived emotional and psychological stress levels, and cognitive function.
Methods
We recruited 10 first-year OMSs who were not currently receiving external OMT outside of weekly coursework; other forms of external stress management, such as yoga or meditation, were not controlled for in this study. Utilizing a random number generator, the 10 student respondents were split into a control group that received no treatment and a treatment group that received 15 min of weekly OMT for 6 weeks. The treatment consisted of condylar decompression, paraspinal inhibition, and supine rib raising, which are techniques that are known to balance the SNS and parasympathetic nervous system (PNS). Cortisol levels were quantified by enzyme-linked immunosorbent assay (ELISA) cortisol immunoassay via salivary samples collected at the beginning of each weekly session, prior to treatment for the treatment group, at the same time of day each week. We also measured participants’ weekly subjective perception of stress utilizing the College Student Stress Scale (CSSS) and cognitive function utilizing the Lumosity Performance Index (LPI). We conducted a two-tailed, unpaired t-test as well as a U test for the cortisol levels, given the smaller sample size and potential for a nonnormal distribution.
Results
A lower cortisol level was correlated to a higher optical density (OD), the logarithmic measure of percent transmission of light through a sample; analysis of our data from the ELISA cortisol immunoassay showed an average weekly change in OD (∆OD) for the treatment group of 0.0215 and an average weekly ∆OD of −0.0044 in the control group. The t-test showed p=0.0497, and our U test showed a p=0.0317. Both tests indicated a statistically significant decrease across the weekly salivary cortisol levels in the treatment group utilizing a p<0.05. An additional effect-size analysis supported our finding of a significant decrease in weekly cortisol levels in the treatment group, Cohen’s d=1.460. Based on the CSSS responses, there was no significant difference in perceived stress between the control and treatment groups (p=0.8655, two-tailed). Analysis of the LPI revealed no statistically significant difference in cognitive performance (p=0.9265, two-tailed).
Conclusions
Our study supports the claim that OMT that targets the SNS and PNS has a significant impact on cortisol levels. While the reduction in cortisol levels was statistically significant, the broader physiological impact remains unclear. Further research is necessary to determine whether this reduction translates to meaningful clinical benefits.
Medical students regularly report high levels of stress and burnout [1]. The combination of physical stressors, such as poor studying posture and impaired quality of sleep, with the mental stress from a rigorous curriculum, stimulates the sympathetic nervous system (SNS) to secrete cortisol, the stress hormone. Previous studies have shown that persistent elevated cortisol levels are associated with adverse physical and mental health outcomes [2], 3].
This study set out to investigate the effects of osteopathic manipulative treatment (OMT) on the cortisol levels, perceived stress level, and cognitive ability of first-year osteopathic medical students (OMSs) at Touro College of Osteopathic Medicine (TouroCOM) Harlem. Osteopathic manipulation has been previously shown to acutely modulate cortisol as well as immunoglobulins in stressed populations [4], [5], [6]. In this study, we differentiated between two primary types of stress: physical stress, which refers to the physiological response to external demands that we measured through cortisol levels in saliva; and perceived stress, which represents the subjective emotional and psychological experience of stress, which we assessed utilizing the College Student Stress Scale (CSSS) [2]. The goal of osteopathic manipulative medicine (OMM) is to evaluate somatic dysfunctions, defined to be impairment in musculoskeletal or myofascial structures and their related vascular, lymphatic, or neural components, and to utilize OMT to promote healing for the patient [7].
In our study, the biomechanical, neurologic, and behavioral models are crucial to addressing how emotional and physical stress can impact our bodies [7], 8]. Our goal was to determine if weekly sessions of targeted OMT could help medical students mitigate their stress levels during the preclinical years. The neurologic model of OMT aims to modulate the autonomic nervous system through balancing sympathetic and parasympathetic responses through neuromuscular tissue tone. One systematic review showed that techniques ranging from high velocity-low amplitude (HVLA) and suboccipital inhibition can significantly impact the autonomic nervous system [9]. We aimed to target the parasympathetic nervous system (PNS) via vagus nerve tone regulation due to the role of vagal tone in adrenal gland innervation. We targeted the sympathetic nervous system via the sympathetic chain ganglia, which innervates the adrenal glands [8]. We investigated the SNS response by measuring the rate at which salivary cortisol levels fluctuate throughout the medical school semester and whether weekly cortisol level changes as a marker of physical stress were linked to changes in the perceived stress level and/or cognitive function. We aimed to test the claim that there is not a significant effect of OMT on salivary cortisol levels, perceived stress, and cognitive function in first-year OMSs.
Methods
This project was submitted to the Touro Institutional Review Board (IRB) under the title of “The Effects of Regular OMT on Stress Levels and Cognitive Function in OMS-I Students at TouroCOM NY Harlem.” It was approved by the board and given the IRB number 18777. The study was conducted from February 2023 to June 2023. This study did not receive any outside funding that required a grant. This study was also registered as a clinical trial at TouroCOM Harlem and assigned the ID number CT06125574. After participants expressed interest in this study, they were provided with physical consent forms that explained the goals, details, requirements, and risks of the study. Informed consent forms were distributed by the student researchers, who remained available to answer any questions the prospective participants had as they reviewed the consent forms. Participants received no compensation for their involvement in this study.
Study population
Participants were recruited from the first-year medical student class at the TouroCOM Harlem campus. Participants were required to be first-year students who were not already receiving regular OMT from an osteopathic physician, who were able to satisfy the time commitments, and who did not attend weekly TouroCOM Harlem OMM enhancement sessions during the duration of the study. While students participated in weekly OMT labs, the classes were standardized so that all participants received the same treatments on any given day. Participants who did not fit in the aforementioned criteria were excluded from the study. The study also excluded participants who were pregnant, had spinal surgery in the past, or had any underlying condition that would be a contraindication to OMT. While we did not perform an in-depth review of participants’ medical history, we also attempted to exclude any participants with disclosed chronic medical conditions such as anxiety, diabetes, or hypertension. This study did not involve participants from protected or vulnerable populations. This study considered all interested individuals for the study without attention to race, color, religion, sex, sexual orientation, gender identity, national origin, veteran, or disability status.
The recruitment process consisted of sending an email to the entire first-year medical student class utilizing the TouroCOM Harlem List Serv function, and interested individuals were invited to fill out a secure Google form. A total of 10 respondents were selected based on eligibility and 6-week availability. Our sample size was limited not due to lack of interest, but rather due to lack of availability for regular weekly sessions as a consequence of the rigorous medical school schedule.
Study design
Ten participants (2 males, 8 females; age range, 23–28 years; mean age, 25 years) were randomly split into two equal groups of five control (1 male, 4 females; age range, 23–28 years; mean age, 25 years) and five treatment (1 male, 4 females; age range, 23–28 years; mean age, 25 years), and they underwent a designated protocol for 6 weeks.
Participants were asked to report to an assigned private Objective Structured Clinical Examination (OSCE) room on the TouroCOM Harlem campus at their designated times. All student subjects were kept in treatment rooms for 30 min and kept the same appointment time across all weeks to avoid natural cortisol fluctuations. For the first 15 min of the session, all participants were asked to complete a cognitive workout on Lumosity to establish their baseline scores and also complete the CSSS. Participants were then asked to provide saliva samples for the cortisol assay. The subjects in the treatment cohort would then receive 15 min of OMT, whereas the nontreatment subjects stayed in the treatment rooms for 15 min before being dismissed. These samples were stored in a secure lab fridge on the TouroCOM Harlem campus. For the following 5 weeks, participants adhered to a strict schedule requiring their presence in designated private OSCE rooms at specified intervals. Figure 1 visualizes the chronological order of the experimental protocol utilized for the rest of the study.

Participant flow diagram.
All participants were assigned one of five OMM student-teaching assistants for weekly assessment. Treatment providers were not blinded as to which participants were to receive treatment and which participants were not. The OMM student-teaching assistants treated the same participants for the duration of the study; there were no substitutions. All treatment providers were standardized with their level of training and protocol adherence.
Individuals in the experimental cohort received OMT on a weekly basis based on a systematic treatment protocol consisting of paraspinal inhibition, rib raising, and condylar decompression techniques performed by OMM student-teaching assistants with attending supervision. The control cohort was not given any form of therapeutic intervention. Concurrently, participants’ salivary cortisol levels were collected at the beginning of each session at a standardized time prior to any treatment or survey data collection and analyzed utilizing an Invitrogen enzyme-linked immunosorbent assay (ELISA) Immunoassay Kit. Additionally, cognitive function was assessed weekly via Lumosity, whereas perceived stress levels were gauged utilizing the CSSS. Control group participants were isolated for the same amount of time as the treatment group participants but did not receive OMT.
All five student researchers participated in providing the three-technique OMM treatment regimen to the participants, collecting salivary samples for the cortisol assay, and administering the CSSS survey and Lumosity assessment. RV performed the statistical analysis on all the collected data utilizing Prism 10. The two faculty members served as supervisors during the participants’ treatment slots and reviewed every stage of the treatment process.
Data collection
All participant salivary samples were collected at the beginning of each session at 2 pm for 6 weeks and stored in a (−4 °C) refrigerator. These samples were analyzed utilizing an Invitrogen ELISA Immunoassay Kit. 100 uL of each sample was diluted in 200 uL of Assay Buffer and processed according to the procedure outlined by the manufacturer. The samples were actually analyzed using the SoftMax 7.2 software tool. The standard cortisol concentration samples provided with the assay showed an inversely proportional exponential relationship to the optical density (OD) at 450 nm. The line of best fit for standard cortisol concentration (y axis) against OD at 450 nm (x axis) was calculated to be y=9,667.93, * 0x with a correlation coefficient of 0.99.
Changes in participant cognitive function was assessed each week utilizing Lumosity, a website designed to assess and strengthen cognitive function through a series of games. Despite claims by the website to improve cognitive function, studies conducted by Florida State University showed that short-term usage of Lumosity did not significantly improve cognitive performance; however, a review conducted on the use of brain games in attention and cognition rehabilitation showed that Lumosity is a commonly utilized tool for cognitive assessment [10], 11]. Due to the short-term nature of this investigative study, we utilized Lumosity as a benchmark rather than a cognitive improvement tool, to measure weekly cognitive function. Each week, participants completed a “workout” consisting of three different exercises that assessed various cognitive functions to receive a Lumosity Performance Index (LPI) and subscores for speed, memory, attention, flexibility, and problem solving.
In addition to salivary cortisol measurements for physical stress, perceived stress levels of the participants were also measured utilizing the CSSS. CSSS is a subjective 11-item survey that utilizes a scale of 1–5 to measure undergraduate student stress over an academic year due to various factors [12]. The survey was modified to ask how often the participant perceived an aspect of stress within the last week. A score of 1 indicated no stress while 5 indicated significant stress; the scores were added together for subsequent analysis.
Treatment description
Certain treatment modalities of OMM focus on treatments designed to regulate sympathetic tone. Regulation of sympathetic tone is crucial in managing stress promoting a balanced physiological state through regulation of the autonomic nervous system [13].
An example of a sympathetic regulatory technique is paraspinal inhibition, a gentle, passive technique targeting the fascia surrounding the spine, aimed at reducing sympathetic output by affecting the sympathetic chain ganglia in the paraspinal region from T1-L2. Another technique, supine rib raising, was employed to address the restricted excursion of the rib cage, a direct method to regulate thoracic sympathetic chain ganglia activity by encouraging normalized articulation with the thoracic spine. Additionally, condylar decompression, a passive, direct cranial technique, is aimed at freeing local restrictions around the occipitoatlantal joint to normalize parasympathetic tone in the vagus nerve, a mechanism that is a focus in this study to decrease cortisol levels given its innervation of hormone-producing organs. While the sacrum is a prominent region for parasympathetic innervation, we believed that omission of sacral regulation techniques would not significantly impact our ability to assess parasympathetic modulation through vagal tone [13].
The rationale behind employing these osteopathic techniques is rooted in the overarching goal of OMM to restore functionality and to normalize physiologic barriers in range of motion by utilizing the relationship between the neuromusculoskeletal system and other bodily systems [14].
Statistical methods description
In our study, we employed an unpaired t-test, the Mann–Whitney U test, and effect-size calculation to analyze the impact of OMTs on cortisol levels in medical students. The unpaired t-test was utilized to compare the average weekly changes in cortisol levels (measured through OD) between the treatment and control groups, assessing whether the difference in means was statistically significant. Considering our small sample size and the potential for a nonnormal distribution of cortisol levels, we also applied the Mann–Whitney U test, a nonparametric alternative to the t-test, to validate our findings. Finally, to quantify the magnitude of OMT’s effect on cortisol levels, we calculated the effect size utilizing Cohen’s d. This provided a standardized measure of the treatment’s efficacy, indicating a significant effect of OMT on reducing cortisol levels in the treatment group compared to the control group.
Results
Changes in optical density
The study assessed the weekly change in optical density (∆OD) measured at 450 nm for both the treatment and control groups. The sample size for each group was n=5. The treatment group exhibited a mean ∆OD of 0.02 (median, 0.01; range, −0.005 to 0.05) with a standard deviation (SD) of 0.02, while the control group exhibited a mean ∆OD of −0.004 (median, −0.005; range, −0.003 to 0.005) with an SD of 0.006. The average ∆OD of the treatment and control groups, along with the ∆OD change of each participant, is shown in Table 1.
Average weekly ∆OD of each participant.
| Group | Participant ∆OD | Avg ∆OD | ||||
|---|---|---|---|---|---|---|
| Treatment | 0.05465 | 0.0062167 | −0.00477 | 0.01327 | 0.038 | 0.02147334 |
| Control | −0.0096 | 0.0052 | −0.00515 | −0.00297 | −0.009483 | −0.0044 |
-
∆OD, change in optical density.
Based on the CSSS responses, there was no statistically significant difference in perceived stress between the control and treatment groups (p=0.9, two-tailed). The mean weekly change in perceived stress scores was −1.1 (median, −1.7; range, −1.8 to 1; SD=1.2) for the treatment group and a mean of −1.2 (median, −1.4; range, −2.2 to 0.7; SD=1.1) for the control group, with a negligible effect size (R2=0.003). The CSSS score change for both groups is visualized in Figure 2.
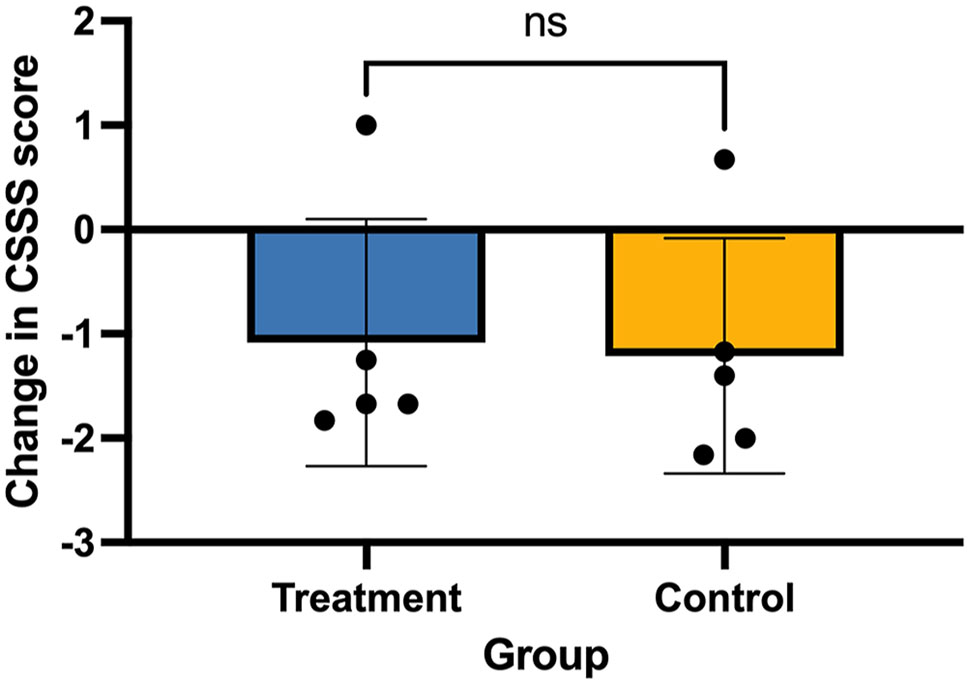
Average weekly changes in College Student Stress Scale (CSSS) score.
A two-tailed t-test to compare the average ∆OD between the treatment and control groups. The t-test yielded a t value of 2.3 with 8 degrees of freedom (df), resulting in a p value of 0.049, which is statistically significant at the p<0.05 level, as shown in Figure 3. This test produced a p value of 0.03, further supporting statistical significance. The effect sizes were calculated utilizing the means and SDs. Cohen’s d was found to be 1.5, and the effect-size r was 0.6. The power of this study is calculated to be 53 %.
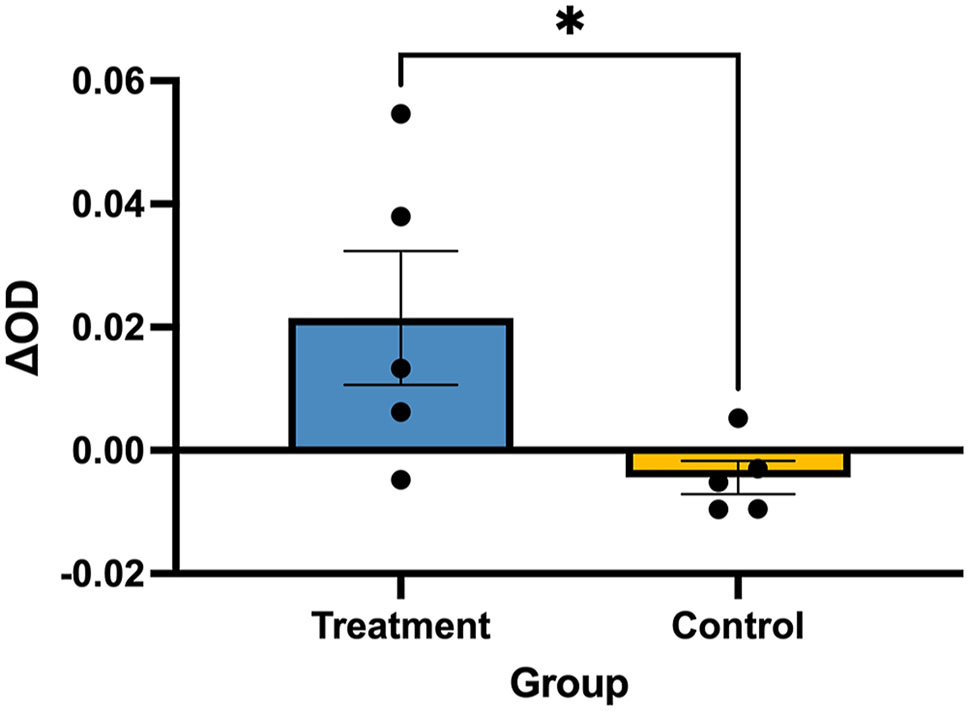
Average weekly changes in optical density (∆OD).
Analysis of the change in LPI revealed no statistically significant difference in cognitive performance between the treatment and control groups (p=0.9, two-tailed). The mean change in LPI scores was 85.6 (median, 67.5; range, 39–196; SD, 68.5) for the treatment group and 81.1 (median, 82.2; range, 13–173; SD=38.3) for the control group, with a minimal effect size (R2=0.001). The LPI score change for both groups is visualized in Figure 4.
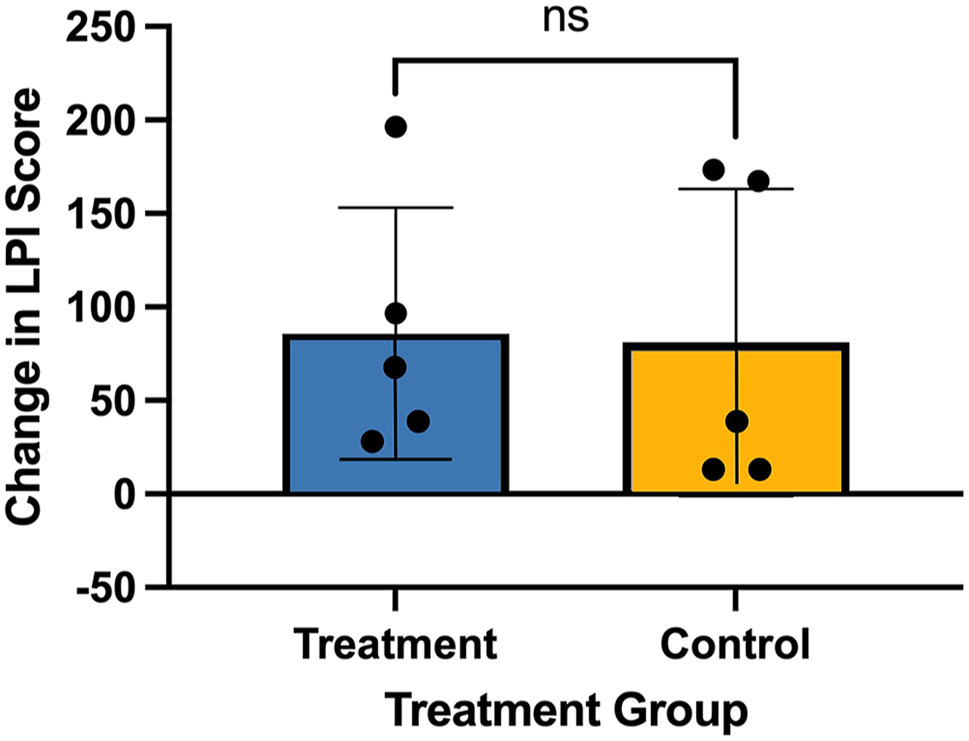
Average weekly change in Lumosity Performance Index (LPI).
Discussion
Our findings demonstrate a statistically significant increase of ∆OD averaged from the entire treatment group compared to the decrease in ∆OD averaged from the control group that was found utilizing the unpaired, two-tailed t-test. The inverse relationship between cortisol concentration and ∆OD, established utilizing the manufacturer standard samples, means that cortisol levels increased at a greater rate in the control group compared to cortisol level changes in the experimental group. This finding supports our study’s investigatory claim that regular OMT is shown to significantly reduce the week-to-week rise in cortisol levels throughout the course of a semester.
There were no statistically significant patterns observed in the self-reported stress perception scores measured utilizing the CSSS between the two groups. The absence of a direct correlation additionally suggests that an alternative physiological marker of stress like hemoglobin A1C or C-reactive protein might be a better indicator of subjective stress perception [15]. Alternatively, a supplemental method to measure stress levels, such as an EEG, could be utilized to determine if there is a link between cortisol levels and self-perception of stress [16].
Changes in cortisol levels, which are known indicators of physiological stress levels, did not correlate with changes in cognitive performance, as there were no statistically significant trends detected in LPI between the treatment and control groups [17]. The lack of a trend between the cortisol level changes and cognitive function suggests that receiving regular OMT did not lead to any meaningful changes in cognitive function.
Limitations
The major limitation of this study was the 10-person sample size. Even though a statistically significant difference in ∆OD (and indirectly cortisol levels) was found between the experimental and control groups, a larger sample size could have provided a stronger correlation between OMT and a reduced rate of cortisol increase in first-year medical students. Despite achieving a statistically significant difference in cortisol levels between the treatment and control groups (p=0.0317), the power analysis revealed a power of approximately 53 %, suggesting that while the findings are promising, a larger sample size would be needed to confirm these results. A large sample size could have also helped determine if there was a correlation between subjective perception of stress and OMT or a link between OMT and cognitive performance.
Another major limitation of this study arises due to the difficult nature of stress quantification. Even though cortisol is regarded as the gold standard of physiological stress markers, salivary cortisol levels fluctuate throughout the day and can be affected by external factors such as caffeine intake, physiological health, and daily activities [18], 19]. We chose not to exclude caffeine intake or stimulant use, because doing so would have significantly limited the study population. Instead, we focused on observing longitudinal changes in cortisol levels relative to each participant’s personal baseline.
Additionally, the study design only allowed us to obtain weekly salivary cortisol samples, which provides only a snapshot at the participant’s cortisol levels and indirectly their physiological stress level. The weekly measurements made it more difficult to account for external influencers of cortisol levels during the data analysis due to limited data points. More frequent or continuous salivary cortisol measurements would have provided better insight into how participants’ salivary cortisol levels and physiological stress levels change in the control and experimental groups due to OMT.
One limitation of the survey methodology was that it did not account for any stress management activities and techniques that each participant utilized in their everyday lives. A future study can expand on this pilot study and see whether OMT can work adjunctively with other stress management techniques or to compare the efficacy of OMT vs. other activities such as yoga, meditation, or regular exercise.
Conclusions
The effectiveness of osteopathic techniques targeting the nervous system has often been confirmed by patients’ subjective experience, but quantifiable, objective data have been limited. This study set out to determine whether there may be a quantitative change in physiologic stress biomarkers, perceived psychologic stress, and cognition. Given the statistically significant reduction in salivary cortisol, we reject the null hypothesis that OMT has no effect on physiologic stress measured through salivary cortisol in first-year OMSs.
However, data from both the subjective stress scale and LPI show no significant differences between the control and treatment groups. Given the small sample size, the results should be interpreted cautiously, and although a statistically significant reduction in cortisol levels was observed, larger studies are necessary to draw stronger and more generalizable conclusions.
Future studies can expand upon this research by increasing the sample size. In addition to greater statistical power, a larger sample size would have allowed the creation of multiple experimental groups in which each group receives a different OMT regimen that would have helped determine if a particular set of OMT techniques were more effective at reducing the rise in cortisol levels throughout the duration of the study. Additionally, a more comprehensive OMT protocol with different metrics for measuring perceived and psychologic stress markers may be utilized for a more comprehensive assessment that the CSSS may not have addressed [20]. However, given the observed impact of OMT on salivary cortisol levels of medical students shown in this study, we hope that we can encourage DO students to utilize OMT as a way to help them mitigate the physiologic stress they face during medical school, and we hope they continue this practice in their personal and professional lives even after graduation.
Acknowledgments
We would like to thank Kamilah Ali, PhD, for assisting with storage and assessment of cortisol samples and use of ELISA immunoplate reader.
-
Research ethics: TouroNYIRB Listing: 18777 Clinical Trial Registry: NCT06125574 The study was conducted in accordance with the Declaration of Helsinki (2013).
-
Informed consent: Written informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: Datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Obregon, M, Luo, J, Shelton, J, Blevins, T, MacDowell, M. Assessment of burnout in medical students using the maslach burnout inventory-student survey: a cross-sectional data analysis. BMC Med Educ 2020;20:376. https://doi.org/10.1186/s12909-020-02274-3.Search in Google Scholar PubMed PubMed Central
2. Abraham, C, Sloan, SNB, Coker, C, Freed, B, McAuliffe, M, Nielsen, H, et al.. Osteopathic manipulative treatment as an intervention to reduce stress, anxiety, and depression in first responders: a pilot study. Mo Med 2021;118:435–41.Search in Google Scholar
3. Schoorlemmer, RMM, Peeters, GMEE, Van Schoor, NM, Lips, P. Relationships between cortisol level, mortality and chronic diseases in older persons. Clin Endocrinol 2009;71:779–86. https://doi.org/10.1111/j.1365-2265.2009.03552.x.Search in Google Scholar PubMed
4. Saggio, G, Docimo, S, Pilc, J, Norton, J, Gilliar, W. Impact of osteopathic manipulative treatment on secretory immunoglobulin a levels in a stressed population. J Am Osteopath Assoc 2011;111:143–7.Search in Google Scholar
5. Thibaut, D, Santarlas, V, Hoppes, J, Vásquez-Castillo, A, Morrow, A, Oviedo, E, et al.. Osteopathic manipulation as a method of cortisol modification: a systematic review. Cureus 2023;15:e36854. https://doi.org/10.7759/cureus.36854.Search in Google Scholar PubMed PubMed Central
6. Fornari, M, Carnevali, L, Sgoifo, A. Single osteopathic manipulative therapy session dampens acute autonomic and neuroendocrine responses to mental stress in healthy male participants. J Osteopath Med 2017;117:559–67. https://doi.org/10.7556/jaoa.2017.110.Search in Google Scholar PubMed
7. Roberts, A, Harris, K, Outen, B, Bukvic, A, Smith, B, Schultz, A, et al.. Osteopathic manipulative medicine: a brief review of the hands-on treatment approaches and their therapeutic uses. Medicine (Baltim) 2022;9:33. https://doi.org/10.3390/medicines9050033.Search in Google Scholar PubMed PubMed Central
8. Bordoni, B. The five diaphragms in osteopathic manipulative medicine: neurological relationships, Part 1. Cureus 2020;12:e8697. https://doi.org/10.7759/cureus.8697.Search in Google Scholar PubMed PubMed Central
9. Rechberger, V, Biberschick, M, Porthun, J. Effectiveness of an osteopathic treatment on the autonomic nervous system: a systematic review of the literature. Eur J Med Res 2019;24:36. https://doi.org/10.1186/s40001-019-0394-5.Search in Google Scholar PubMed PubMed Central
10. Shute, VJ, Ventura, M, Ke, F. The power of play: the effects of Portal 2 and Lumosity on cognitive and noncognitive skills. Comput Educ 2015;80:58–67. https://doi.org/10.1016/j.compedu.2014.08.013.Search in Google Scholar
11. Shahmoradi, L, Mohammadian, F, Rahmani Katigari, M. A systematic review on serious games in attention rehabilitation and their effects. Behav Neurol 2022;2022:2017975. https://doi.org/10.1155/2022/2017975.Search in Google Scholar PubMed PubMed Central
12. Feldt, RC. Development of a brief measure of college stress: the college student stress scale. Psychol Rep 2008;102:855–60. https://doi.org/10.2466/pr0.102.3.855-860.Search in Google Scholar PubMed
13. Henderson, AT, Fisher, JF, Blair, J, Shea, C, Li, TS, Bridges, KG. Effects of rib raising on the autonomic nervous system: a pilot study using noninvasive biomarkers. J Am Osteopath Assoc 2010;110:324–30.Search in Google Scholar
14. Bath, M, Owens, J. Physiology, viscerosomatic reflexes. PubMed. Published; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559218/.Search in Google Scholar
15. Noushad, S, Ahmed, S, Ansari, B, Mustafa, UH, Saleem, Y, Hazrat, H. Physiological biomarkers of chronic stress: a systematic review. Int J Health Sci 2021;15:46–59.Search in Google Scholar
16. Saeed, SMU, Anwar, SM, Khalid, H, Majid, M, Bagci, U. EEG based classification of long-term stress using psychological labeling. Sensors 2020;20:1886. https://doi.org/10.3390/s20071886.Search in Google Scholar PubMed PubMed Central
17. Lee, BK, Glass, TA, McAtee, MJ, Wand, GS, Bandeen-Roche, K, Bolla, KI, et al.. Associations of salivary cortisol with cognitive function in the Baltimore memory study. Arch Gen Psychiatr 2007;64:810–18. https://doi.org/10.1001/archpsyc.64.7.810.Search in Google Scholar PubMed
18. Pritchard, BT, Stanton, W, Lord, R, Petocz, P, Pepping, GJ. Factors affecting measurement of salivary cortisol and secretory immunoglobulin A in field studies of athletes. Front Endocrinol 2017;8:168. https://doi.org/10.3389/fendo.2017.00168.Search in Google Scholar PubMed PubMed Central
19. Tammayan, M, Jantaratnotai, N, Pachimsawat, P. Differential responses of salivary cortisol, amylase, and chromogranin A to academic stress. PLoS One 2021;16:e0256172. https://doi.org/10.1371/journal.pone.0256172.Search in Google Scholar PubMed PubMed Central
20. Hope-Bell, J, Draper-Rodi, J, Edwards, DJ. Applying an osteopathic intervention to improve mild to moderate mental health symptoms: a mixed-methods feasibility study protocol. BMJ Open 2023;13:e071680. https://doi.org/10.1136/bmjopen-2023-071680.Search in Google Scholar PubMed PubMed Central
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Original Article
- Effects of the Strong Hearts program at two years post program completion
- General
- Original Article
- Incidence of fall-from-height injuries and predictive factors for severity
- Medical Education
- Original Article
- Recent and future trends in osteopathic orthopedic surgery residency match rates following the transition to a single accreditation system
- Musculoskeletal Medicine and Pain
- Review Article
- Elbow injuries in overhead throwing athletes: clinical evaluation, treatment, and osteopathic considerations
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Stressbusters: a pilot study investigating the effects of OMT on stress management in medical students
- Obstetrics and Gynecology
- Original Article
- Reduction in deep organ-space infection in gynecologic oncology surgery with use of oral antibiotic bowel preparation: a retrospective cohort analysis
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Original Article
- Effects of the Strong Hearts program at two years post program completion
- General
- Original Article
- Incidence of fall-from-height injuries and predictive factors for severity
- Medical Education
- Original Article
- Recent and future trends in osteopathic orthopedic surgery residency match rates following the transition to a single accreditation system
- Musculoskeletal Medicine and Pain
- Review Article
- Elbow injuries in overhead throwing athletes: clinical evaluation, treatment, and osteopathic considerations
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Stressbusters: a pilot study investigating the effects of OMT on stress management in medical students
- Obstetrics and Gynecology
- Original Article
- Reduction in deep organ-space infection in gynecologic oncology surgery with use of oral antibiotic bowel preparation: a retrospective cohort analysis


