Abstract
Because poor posture is a common instigating factor in back, shoulder, and neck pain, the rhomboid muscles should be considered in a complete physical evaluation. Previous techniques for treating a rhomboid tender point have addressed only one of the two main actions of the muscle, specifically retraction of the scapula utilizing shoulder abduction. This modified supine counterstrain technique for the rhomboid tender point incorporates both scapular retraction as well as superior, medial rotation of the inferior border of the scapula without abduction, providing a comprehensive treatment to accommodate patients with shoulder movement restrictions. This article discusses indications, contraindications, treatment, and a list of problem-solving strategies for the rhomboid tender point.
Poor posture is a common instigating factor in back, shoulder, and neck pain [1]. The rhomboid muscles can be inappropriately lengthened due to the shoulders being anteriorly rotated throughout most of the day. The rhomboids are a part of the deep intrinsic muscles of the back, and they can create pain and discomfort due to activation from situations such as computer work, sitting at a desk, or mobile device usage. Patients may present to the clinic with pain between the scapulae, which correlates with the location of the rhomboid musculature. Specifically, the rhomboid minor and major attach from the nuchal ligament and the spinous processes of C7-T5 to the medial border of the scapula between the scapular spine and the inferior angle [2]. The action of the rhomboids consists of inferior rotation and retraction of the scapula.
Strain/counterstrain (now called “counterstrain”), developed by Lawrence Jones, DO, in 1955, is a technique that addresses an inappropriate proprioceptive reflex found within myofascial structures such as tendons, ligaments, fascia, and muscle bellies that are tender upon palpation [3]. The location of these areas of tenderness are called “tender points” and are consistent from one patient to the next. In relation to the rhomboid tender point, common indications include upper back pain, neck pain, shoulder pain, and anterior chest pain. Previous treatment styles, according to the literature, describe placing the patient in a seated or prone position and palpating along the medial border of the scapula. For treatment, the shoulder is abducted, and the arm is pulled posteriorly to retract the scapula. This treatment position approximates the attachment points of the rhomboid on the medial border of the scapula to the midline utilizing multidirectional movements [4].
Previous treatments of this tender point address retraction of the scapula, which is one of the two main actions of the rhomboid muscles. The technique described in this article fills a gap in the understanding of this tender point because it allows a more thorough treatment approach by addressing the two main motions of the rhomboids: scapular rotation as well as retraction without having to abduct the arm. This would accommodate patients who have restricted shoulder range of motion. Although the goal of this treatment is to target the rhomboid musculature, it is important to note that the rhomboids are not the only muscles affected by the positioning of this treatment because there are multiple muscles that assist with scapular retraction and/or scapular internal rotation as well as 15 other muscles [4] that attach to the scapulae. This article further discusses the contraindications and side effects as well as a problem-solving approach.
Clinical summary
Jones et al. [4], in their book Strain and Counterstrain, describes the basic principles of treating counterstrain. These involve identifying areas of tenderness related to specific muscles (tender points) and then monitoring that area of tenderness with a finger. Many beneficial changes can be seen with this technique, including reduced pain perception and inflammation with a greater local muscular strength, reduced fascial stiffness, and improved proprioceptive input [5]. Suggested mechanisms behind counterstrain include neurologic changes mediated via mechanoreceptors, Golgi tendons, and Ruffini corpuscles, proprioceptive relationships between antagonist muscles, and altering fibroblast activity to reduce localized inflammation [5–7]. The procedure by Jones et al. [8] is as follows: the muscle of interest is taken into its position of ease, which is accomplished by approximating the origin to the insertion. The physician should appreciate a softening of the monitored area while the patient reports a reduction in tenderness. The reduction of tenderness should show a 75–100 % improvement from the initial palpation [9]. If the reduction of tenderness is not achieved, then fine-tuning of the treatment position can be done until there is 75–100 % improvement. This position is traditionally held for a minimum of 90 s. Throughout the 90 s, the physician is monitoring the tender point for warmth or pulsation. Once 90 s have passed, the patient is passively brought back to a neutral position and the tender point is reassessed for decreased tenderness.
Diagnosis
With the patient supine or seated, the physician palpates the muscle attachment along the medial border of the scapula, which can be identified between the spine of the scapula and the inferior angle. Figure 1 demonstrates the location on a skeleton in a seated position, whereas Figure 2 demonstrates the location on a patient in a supine position.
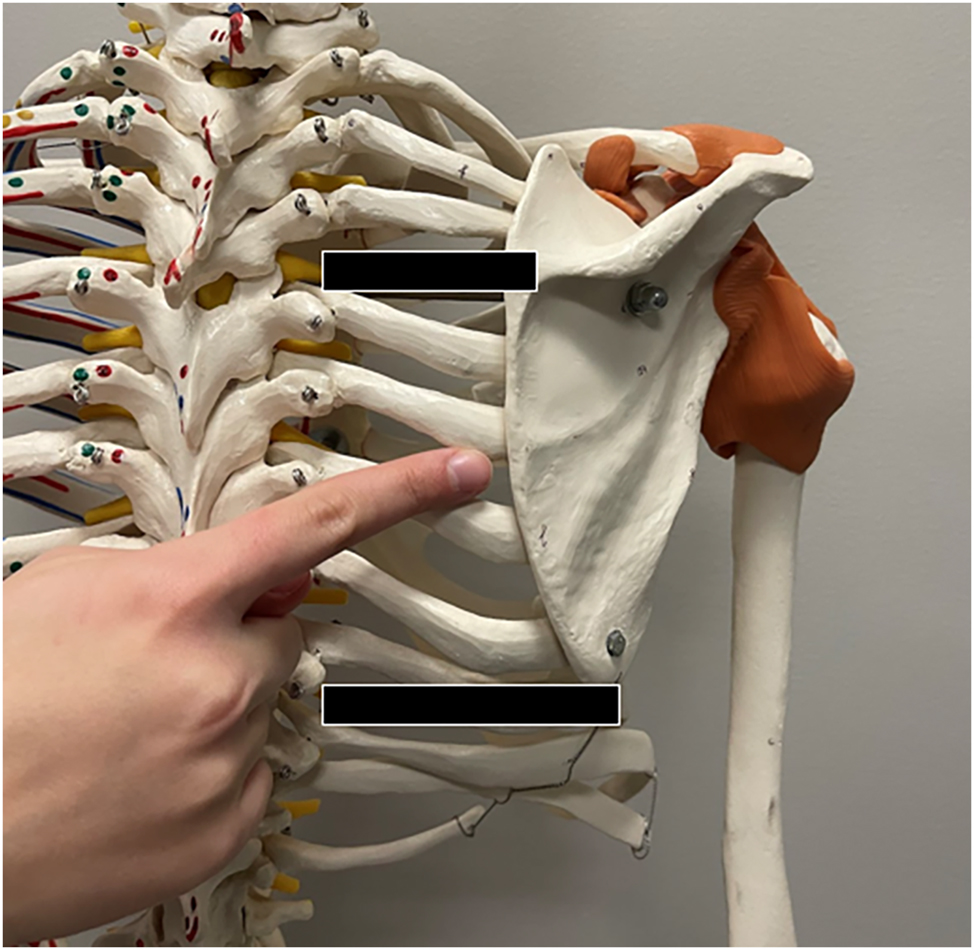
The location of the tender point on the skeleton is found along the medial border of the scapula between the spine of the scapula and the inferior angle. The spine and inferior angle of the scapula are demarcated with the black bars.
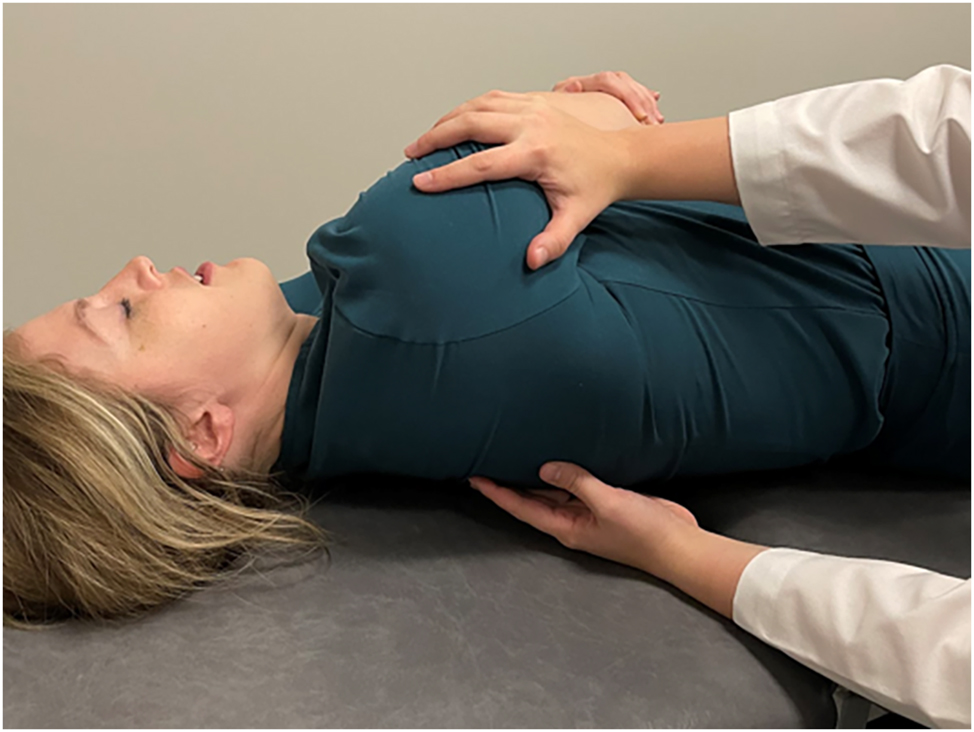
The location of the tender point on a supine patient. For the exact location of the tender point, please refer to Figure 1 for the location in an upright position. Because this is a supine treatment, the tender point is usually found in a supine position.
Correcting the dysfunction
After obtaining informed consent, the physician will grasp the arm just proximal to the elbow on the side of the tender point. Internal rotation of the arm is achieved, followed by inferior traction of the arm (Figure 3), bringing the arm down alongside the patient’s body while monitoring the tender point with the opposite hand. The internal rotation of the arm allows the humerus to lock into the scapula, and the inferior traction tilts the scapula at an oblique angle, causing the medial border of the scapula to become closer to the spinous processes of C7-T5. The superior, medial motion of the scapula allows for the shortening of the origin and insertion of the rhomboids. The physician will appreciate a softening and/or warmth as the rhomboids are placed in their position of ease and the patient will report a 75–100 % improvement in their tenderness. If the tenderness is not 75–100 % better, fine-tuning can occur with additional inferior traction or internal rotation of the arm. After holding this position for 90 s, the patient’s arm is returned passively to a neutral position.
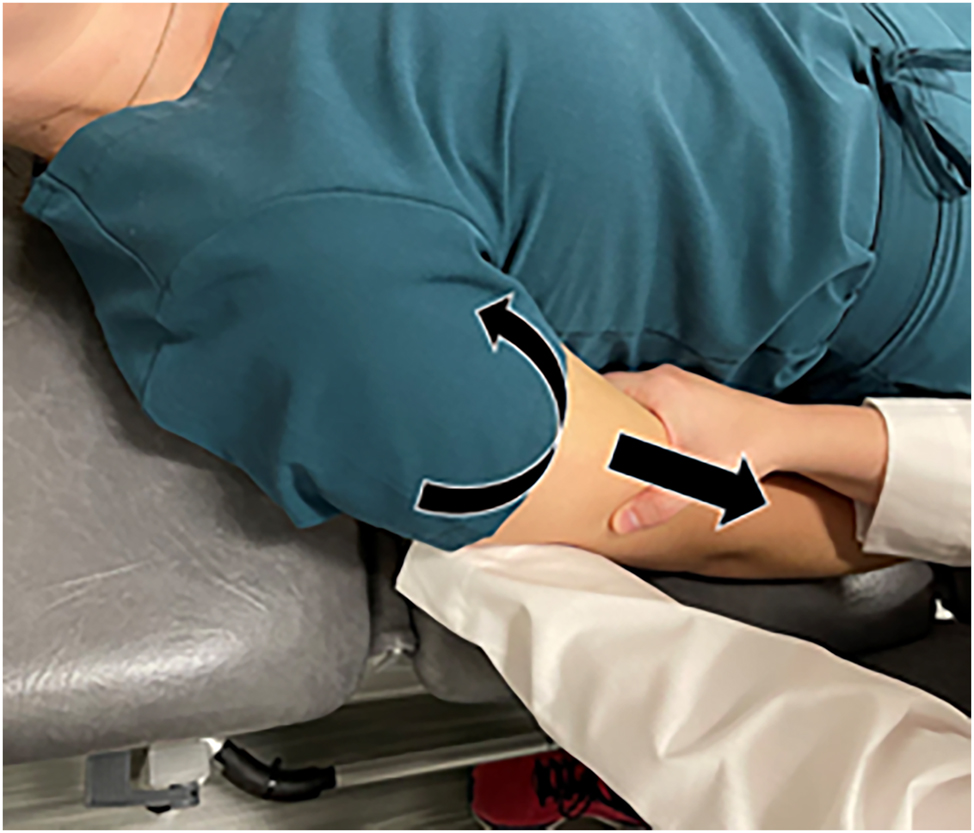
Internal rotation (curved arrow) and inferior traction (straight arrow) are applied to the arm from holding above the elbow.
Re-evaluation
With the physician’s hand still on the tender point, where the rhomboid muscle attaches along the medial border of the scapula, the tender point is reassessed for tenderness with palpation. After the treatment is complete, there should be a decreased or minimal tenderness compared to when initially palpated. Improvement from baseline tenderness is expected to be 75–100 % for a successful treatment.
Discussion
Previous methods of treatment have addressed the rhomboid motion of scapular retraction through shoulder abduction and retraction, but neglected the rotational action. This treatment allows the practitioner to address both retraction and rotational motions of the rhomboid muscles without abduction of the arm. It is important to note that the rhomboids are not the only muscles affected by the positioning of this treatment because there are multiple muscles that assist with scapular retraction and/or scapular internal rotation, such as the trapezius/latissimus dorsi and the subscapularis/pectoralis major/latissimus dorsi/teres major/anterior deltoid, respectively [2]. Additionally, the patient is treated in a supine position, which allows for better relaxation of the patient because other postural muscles, such as the erector spinae, are not in use and there is not as much torque through abduction applied to the shoulder. Finally, this modified approach allows for physician ease during treatment as the weight of the upper extremity can be supported by the table instead of the physician.
Relative limitations for this technique include shoulder instability and adhesive capsulitis; however, if the patient is moved slowly, this concern is minimalized. If technical difficulties arise, such as lack of a manipulation table or the inability of the patient to lay down, this treatment can be converted into a seated treatment. If there is pain or paresthesia during the treatment, the physician should stop the treatment, bring the patient back to a neutral position, and reassess. As with other treatment modalities, trauma, fractures, or inability to relax may lead to deferment. Although counterstrain is generally considered a safe technique, side effects may include posttreatment soreness or numbness/tingling in the arm or hand during treatment. Posttreatment soreness can be reduced by hydration and rest for 24–48 h after treatment [5]. If paresthesia is appreciated, the physician should stop the treatment, bring the patient back to a neutral position, and reassess.
There may be several reasons why this tender point does not resolve. The tender point might be on an adjacent muscle such as the serratus anterior or posterior, levator scapulae, supraspinatus, latissimus dorsi, or the erector spinae group. Surrounding somatic dysfunctions may be present such as sternal or clavicular restrictions or inhalation/exhalation restrictions of the rib cage. Poor posture, such as anteriorly rotated shoulders, has the potential to lead to frequent recurrence of this tender point [8].
Conclusions
The rhomboid tender point should be considered when doing a comprehensive evaluation of upper back and shoulder pain. With this modified treatment, the rhomboid muscles can be thoroughly and efficiently treated due to addressing both main actions in a position that allows for complete patient relaxation.
-
Research ethics: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: None declared.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Posture and Back Health. Harvard Health Publishing; 2014. https://www.health.harvard.edu/pain/posture-and-back-health [Accessed 21 November 2022].Search in Google Scholar
2. Moore, KL, Dalley, AF. Neck. In: Clinically oriented anatomy, 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:1078 p.Search in Google Scholar
3. Seffinger, MA. Strain/counterstrain. In: Foundations of osteopathic medicine, 4th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011:864–84 pp.Search in Google Scholar
4. Borms, D, Maenhout, A, Cools, AM. Incorporation of the kinetic chain into shoulder-elevation exercises: does it affect scapular muscle activity? J Athl Train 2020;55:343–9. https://doi.org/10.4085/1062-6050-136-19.Search in Google Scholar PubMed PubMed Central
5. Chaitow, L, ed. Fascial dysfunction: manual therapy approaches, 2nd ed. Edinburgh: Handspring Publishing; 2018:282 p.Search in Google Scholar
6. Macefield, VG, Knellwolf, TP. Functional properties of human muscle spindles. J Neurophysiol 2018;120:452–67. https://doi.org/10.1152/jn.00071.2018.Search in Google Scholar PubMed
7. Chaitow, L. Ligaments and positional release techniques? J Bodyw Mov Ther 2009;13:115–6. https://doi.org/10.1016/j.jbmt.2009.01.001.Search in Google Scholar PubMed
8. Jones, LH, Kusunose, RS, Goering, EK. Practice of counterstrain. In: Jones strain–counterstrain. Boise, ID: Jones Strain-Counterstrain, Inc.; 1995:21–3 pp.Search in Google Scholar
9. Myers, HL, Devine, WH, Glover, JC, Kusunose, RS. Treatment of shoulder pain and dysfunction with counterstrain; rhomboid. In: Clinical application of counterstrain. Tucson, AZ: Osteopathic Press, a division of Tucson Osteopathic Medical Foundation; 2012:57 p.Search in Google Scholar
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- The role of osteopathic principles and practice in upper extremity injuries of the overhead athlete
- General
- Original Article
- Delayed discovery: the COVID-19 pandemic’s influence on osteoarthritis clinical trials
- Medical Education
- Original Article
- Cognitive empathy of osteopathic students: a longitudinal study with data comparisons to the Project in Osteopathic Medical Education and Empathy (POMEE)
- Musculoskeletal Medicine and Pain
- Original Articles
- Retrospective analysis of robotic unicompartmental and total knee arthroplasties: patient demographics and outcomes
- Association between steroid use and concussions among high school athletes: a cross-sectional analysis of the Youth Risk Behavior Surveillance System
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Supine counterstrain technique for rhomboid tender point
- Public Health and Primary Care
- Commentary
- Issues of informed consent for non-specialists conducting colorectal cancer screenings
- Clinical Image
- Raynaud’s phenomenon
Articles in the same Issue
- Frontmatter
- Editorial
- The role of osteopathic principles and practice in upper extremity injuries of the overhead athlete
- General
- Original Article
- Delayed discovery: the COVID-19 pandemic’s influence on osteoarthritis clinical trials
- Medical Education
- Original Article
- Cognitive empathy of osteopathic students: a longitudinal study with data comparisons to the Project in Osteopathic Medical Education and Empathy (POMEE)
- Musculoskeletal Medicine and Pain
- Original Articles
- Retrospective analysis of robotic unicompartmental and total knee arthroplasties: patient demographics and outcomes
- Association between steroid use and concussions among high school athletes: a cross-sectional analysis of the Youth Risk Behavior Surveillance System
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Supine counterstrain technique for rhomboid tender point
- Public Health and Primary Care
- Commentary
- Issues of informed consent for non-specialists conducting colorectal cancer screenings
- Clinical Image
- Raynaud’s phenomenon

