Abstract
Context
Amputations are routine in orthopedics, specifically during trauma and when patients have recurrent surgical site infections. When undergoing amputations, patients must combat the psychosocial factors associated with the loss of an extremity, including stigmatization.
Objectives
This study analyzes the presence of person-centered language (PCL) within amputation-related orthopedic publications in the top orthopedic journals.
Methods
We conducted a cross-sectional analysis with a database search on February 14, 2021 utilizing PubMed. Utilizing a previously published search string, we isolated studies that were published in the top 20 orthopedic journals based on the Google h5-index. In addition to the top 20 orthopedic journals, we included the top two hand and foot & ankle journals in our search to incorporate more amputation literature. Our search yielded 687 returns. The sample was then randomized, and the first 300 studies that fit our inclusion criteria were examined for prespecified non-PCL terminology.
Results
Our results show that 157 (52.2%) studies were adherent to PCL according to the American Medical Association’s Manual of Style 10th Edition (AMAMS). Of the 143 (47.7%) studies that were not adherent to PCL, 51 studies (35.7%) had more than one type of non-PCL language. The term “amputee,” which is being labeled as identity-first language (IFL), was found in 101 articles (33.7%). Further investigation found that 73.3% (74/101) of the studies containing IFL were found to have other non-PCL terms. Of the other studies in the sample, non-PCL was found 34.7% (88/199) of the time. This analysis was done due to the discrepancies in stigmatization of the term “amputee.” No statistical association was found between adherence to PCL and study characteristics.
Conclusions
Our findings show that amputation literature within the top orthopedic journals has limited adherence to PCL. Additionally, the use of the term “amputee,” which is widely accepted by the amputation community, resulted in a greater rate of non-PCL terminology within orthopedic amputation literature. Efforts should be implemented within orthopedics to avoid the use of stigmatizing language, regarding individuals that underwent amputations, to minimize psychosocial stressors.
Amputations are commonplace in medicine, with almost 185,000 individuals requiring amputations each year in the United States. The main causes of amputations in the majority of people are peripheral vascular disease and diabetes [1, 2]. It is also anticipated that the prevalence of people with amputations will double by the year 2050, which will result in a prevalence of 1 in 120 individuals [2]. Within orthopedics, other reasons for limb amputations are trauma and surgical site infections [3], [4], [5]. When undergoing amputation, patients must combat physical and psychological factors with the loss of an extremity. The psychological factors that people must face include depression, embarrassment, and social stigmatization [6], [7], [8].
Stigma is described as a power imbalance that results in the devaluation of a group of individuals, resulting in social inequities and negative physical and mental health impacts [9]. As this power imbalance persists, normalization of the stigma can result within society [10]. Stigma has been shown to result in negative social and health equities; therefore, stigmatization of medical conditions could result in decreased patient self-esteem and support [11, 12]. A review written by Room [11] specifically talks about individuals that are outside of social constructs are susceptible to stigmatization and highlights studies that show that health services given to people fitting under specific stigmatizing factors such as heavy alcohol use and being homeless are inferior [13], [14], [15]. Due to the influence, it is imperative that medical professionals avoid the use of stigmatizing language.
There have been various efforts to limit stigmatization in the medical literature. The American Psychological Association (APA) defined the use of person-centered language (PCL), which is placing individuals ahead of disabilities in verbiage. Examples of non-PCL stigmatizing language in orthopedics are highlighted by Leopold et al. [16] who state that manuscripts should avoid utilizing terms such as “diabetics” and instead utilize terminology such as “patients with diabetes.” The APA had the goal of maintaining individuals’ integrity as humans and avoiding objectification [17]. In addition, the American Medical Association (AMA) incorporated guidelines to emphasize the avoidance of labeling diseases or conditions to people [18]. As a result, many journals have adopted the requirement of PCL in manuscripts [19]. The concept of PCL also aligns with osteopathic principles because it is a consideration toward the psychosocial aspect of a patient’s care [20]. The proposed osteopathic principles were stated by Rogers et al. [21] in 2002, outlining the principles that osteopathic physicians should abide by when caring for patients. The first of those principles states, “The patient is the focus for healthcare” [21]. PCL falls within these tenets and the approach to patient care because it prevents patients from being labeled based on their medical condition and emphasizes the individual. However, previous investigations show that non-PCL language is prevalent in various aspects of medicine [22], [23], [24], [25]. For example, Headley et al. [26] looked at the use of PCL within amputation-related literature, finding that 64.6% of the studies were nonadherent.
PCL has been discussed in orthopedics through various editorials. However, there is no literature looking at the presence of stigmatizing language within orthopedic literature [16, 27]. In addition, although there is literature looking at PCL within amputation literature, only one of the included journals was related to orthopedic surgery. Amputations by nature are difficult procedures to undergo from a psychosocial standpoint because they cause drastic changes to one’s lifestyle, alter ones self-concept, and cause patients to lose physical function [28]. Because stigmatization is inherently the devaluation of a group, PCL use can help minimize the psychosocial repercussions of stigmatization against people with amputations [19]. Therefore, our study looks to identify the use of PCL within orthopedic-related amputation literature.
Methods
Journal selection and article inclusion
Our study is a cross-sectional analysis design that we conducted utilizing a systematic search on PubMed on February 14, 2022. Our study did not require IRB approval due to the secondary nature of the research. We utilized a similar search string to Headley et al. [26] to isolate amputation studies. To focus on orthopedic-related amputation papers, we localized our search to the top 20 orthopedic journals on the Google h5-index [29]. Our search string also included the top two indexed foot and ankle/hand orthopedic journals. The search string is found in Figure 1 and includes studies published over the past 10 years. After searching for the items, we randomized our sample utilizing the “RAND” function on Google Sheets and included the first 300 articles that fit our inclusion criteria. We chose 300 articles to provide adequate power to our study; this was decided based on previously published literature looking at PCL [22, 30]. The article must be (1) about or related to amputation procedures, associated complications, or individuals with amputations; (2) published between 2012 and February 2022; and (3) written in English. The study types must also be primary or secondary in nature; commentaries and editorials were excluded from our sample. Our date range was decided based on having a sample that contained an even 10 years of data.
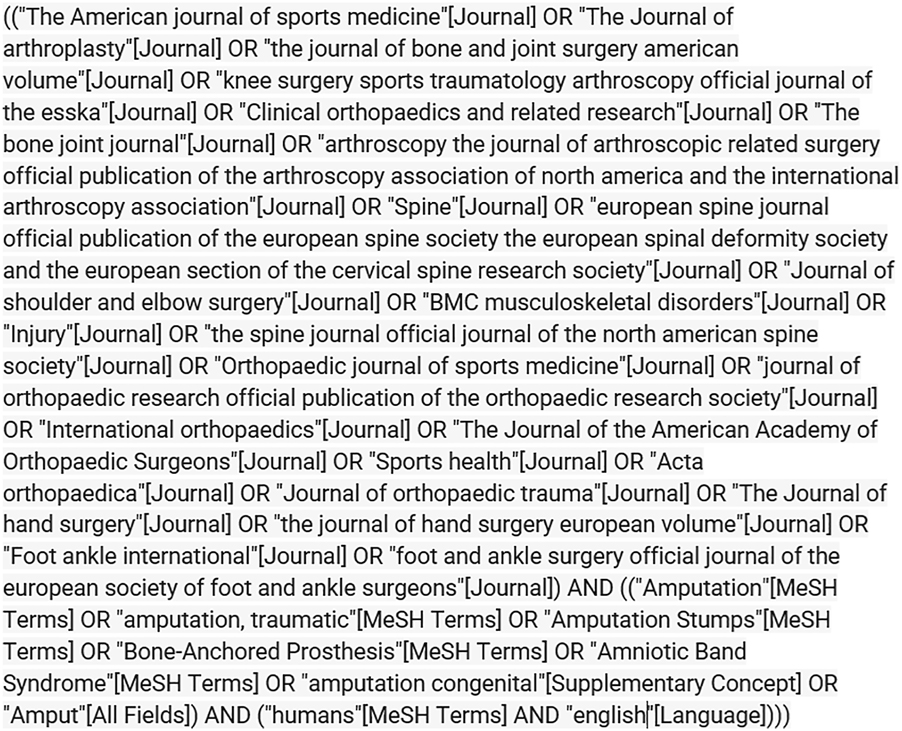
Search string.
Data extraction
Two investigators screened the articles for inclusion criteria. Next, the same investigators searched the full text of the article for the following predetermined non-PCL terms: “amputee,” (condition) “person/patient,” “cripple,” “stump,” “disabled,” “deformed,” “homebound,” “maimed,” “injured,” “victim/victim of,” “limb loss,” “burden,” “confined to,” “suffer/sufferer,” “afflicted by,” and “problem with.” The terms were chosen based on new recommendations suggested by the American Medical Association’s Manual of Style (AMAMS). For each included article, we also gathered characteristic data, such as journal AMA/International Committee of Medical Journal Editors (ICMJE) requirements, the first author’s location (continent) according to institutional affiliation and their type of employment, the article type, whether the article followed a methodological guideline, funding statements, and journal of publication. A third-party investigator would arbitrate for discrepancies, resulting in 100% interrater reliability.
Statistical analysis
After data extraction, we calculated the number of articles that adhered to PCL within their manuscript and thus avoided the use of stigmatizing language. In our analysis, we did not include “amputee” when used as a label in our assessment because some individuals and groups within the community prefer this identity-first style. Further, organizations that help, advocate for, and represent people with amputations often refer to people with amputations as “amputees” and utilize this term within the names of organizations, such as “the Amputee Coalition.” However, we still identified the number of articles that utilized the term due to the National Center on Disability and Journalism suggesting the term “amputee” as “offensive and often is not used correctly.” We then used Fisher’s exact tests to compare variables such as study type, funding, AMA/ICMJE journal requirements, or the first author’s country to the frequency of non-PCL terminology usage in articles. We also conducted a regression analysis to determine if the percentage of PCL fidelity had changed by the year of study publication. Alpha was set at 0.05 for all analyses and were conducted utilizing STAT 16.1 (StataCorp LLC, College Station, TX) and Google Sheets [31].
Results
Our search yielded 687 returns. After randomization of the sample, we coded the first 300 studies that fit our inclusion criteria. There were 61 studies that were excluded due to being nonorthopedic-related or commentary articles. A flowchart can be seen in Figure 2 showing the route to obtaining our included studies. Among the studies in our sample, observational studies were the most included (61%; 183/300). Other study types included case series/case reports (12.7%; 38/300), clinical trials (4.7%; 14/300), literature reviews (6.7%; 20/300), basic science (0.7%; 2/300), systematic reviews (6.0%; 18/300), and surgical techniques (8.3%; 25/300). The rest of the characteristics extracted can be found in Table 1.
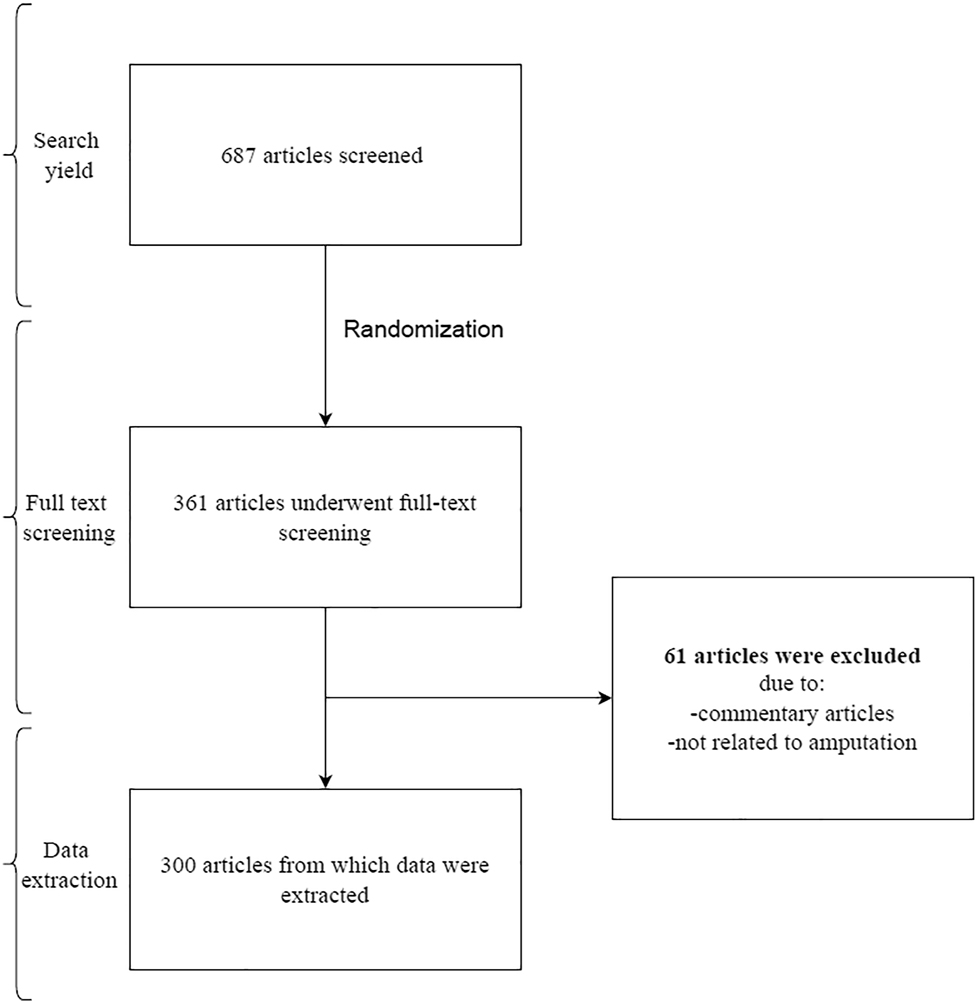
Flow diagram of study selection.
Article characteristics and associations of adherence to PCL.
| Article characteristics | Articles with non-PCL (171; 57%) no. (%) | Articles adhering to PCL (129; 43%) no. (%) | Total (300) no. (%) | Fisher’s exact p-Value |
|---|---|---|---|---|
| Type of article | ||||
| Basic science | 1 (50.00) | 1 (50.00) | 2 (100.00) | 0.07 |
| Case series/case reports | 15 (39.47) | 23 (60.53) | 38 (100.00) | |
| Clinical trials | 3 (21.43) | 11 (78.57) | 14 (100.00) | |
| Literature review | 14 (70.00) | 6 (30.00) | 20 (100.00) | |
| Observational | 93 (50.82) | 90 (49.18) | 183 (100.00) | |
| Systematic reviews | 8 (44.44) | 10 (55.56) | 18 (100.00) | |
| Techniques | 9 (36.00) | 16 (64.00) | 25 (100.00) | |
|
|
||||
| Continent | ||||
|
|
||||
| Africa | 4 (100.00) | 0 (0.00) | 4 (100.00) | 0.142 |
| Asia | 19 (37.25) | 32 (62.75) | 51 (100.00) | |
| Australia | 1 (50.00) | 1 (50.00) | 2 (100.00) | |
| Europe | 42 (46.15) | 49 (53.85) | 91 (100.00) | |
| North America | 76 (50.67) | 74 (49.33) | 150 (100.00) | |
| South America | 1 (50.00) | 1 (50.00) | 2 (100.00) | |
|
|
||||
| AMA/ICMJE | ||||
|
|
||||
| No | 4 (30.77) | 9 (69.23) | 13 (100.00) | 0.263 |
| Yes | 139 (48.43) | 148 (51.57) | 287 (100.00) | |
|
|
||||
| Mentions reporting guidelines | ||||
|
|
||||
| No | 142 (48.14) | 153 (51.86) | 295 (100.00) | 0.374 |
| Yes | 1 (20.00) | 4 (80.00) | 5 (100.00) | |
|
|
||||
| Funding | ||||
|
|
||||
| No funding | 78 (52.35) | 71 (47.65) | 149 (100.00) | 0.506 |
| Industry | 4 (40.00) | 6 (60.00) | 10 (100.00) | |
| No funding statement | 46 (44.23) | 58 (55.77) | 104 (100.00) | |
| Private | 3 (30.00) | 7 (70.00) | 10 (100.00) | |
| Public | 12 (44.44) | 15 (55.56) | 27 (100.00) | |
|
|
||||
| Location (lower vs. upper extremity) | ||||
|
|
||||
| Lower | 79 (53.02) | 70 (46.98) | 149 (100.00) | 0.007 |
| Multi | 30 (56.60) | 23 (43.40) | 53 (100.00) | |
| Upper | 34 (34.69) | 64 (65.31) | 98 (100.00) | |
-
AMA, American Medical Association; ICMJE, International Committee of Medical Journal Editors; PCL, person-centered language.
Our final results show that 157 (52.2%) studies adhered to PCL according to the AMAMS. Of the 143 (47.7%) studies that were not adherent to PCL, 51 studies (35.7%) had more than one type of non-PCL language. The term “amputee,” which is being labeled as identity-first language (IFL), was found in 101 articles (33.7%). Further investigation found that 73.3% (74/101) of the studies that contained IFL were found to have other non-PCL terms. Among the other studies in the sample that did not contain IFL, non-PCL was found 34.7% (69/199) of the time. This analysis was conducted due to the discrepancies in the stigmatization of the term “amputee.”
Among the statistical analyses conducted, we found no significant associations between the use of PCL and the type of study conducted, the continent of origin, journal fidelity to AMA/ICMJE guidelines, study funding, fidelity to methodological guidelines (Table 1), or year of publication (Figure 3). We did find statistical significance between non-PCL use and upper extremity amputation studies compared to lower extremity studies and multi-limb studies (p=0.007) (Table 1). This finding states that upper extremity amputation studies were more prone to utilizing non-PCL terminology compared to lower extremity and multi-limb amputation studies. The most common non-PCL terminology utilized was “(condition) person/patient.”
![Figure 3:
Regression of the percent of articles adherent of person-centered language (PCL) by year. Regression analysis for the percent of articles adherent to PCL guidelines from 2012 to 2020 was nonsignificant (coefficient: 0.72, standard error [SE]=1.06; T=0.67, p=0.517).](/document/doi/10.1515/jom-2022-0181/asset/graphic/j_jom-2022-0181_fig_003.jpg)
Regression of the percent of articles adherent of person-centered language (PCL) by year. Regression analysis for the percent of articles adherent to PCL guidelines from 2012 to 2020 was nonsignificant (coefficient: 0.72, standard error [SE]=1.06; T=0.67, p=0.517).
Discussion
Our study found that nearly 48% of the studies in our sample did not adhere to PCL guidelines. We also found that “amputee” was utilized in more than one-third of the studies within our sample. A large majority (73.3%) contained stigmatizing terminology toward patients with amputations. In comparison, 44% of the studies that did not utilize the term “amputee” had non-PCL present in the manuscript. The most common non-PCL term identified in our sample is “stump,” which was generally utilized to refer to the amputated extremity. The second most common instance of non-PCL was describing a person by the condition that they have ((condition) “patient”). Examples of this were “amputation patient” and “diabetic patient.”
Although there has been a study looking at PCL within the amputation literature [26], to our knowledge, there have been no studies looking at PCL within the orthopedic literature. Editorials have been written about the use of stigmatizing language within orthopedics, but our study is the first primary study to identify it within research. This is essential because we understand that stigmatizing language can negatively affect various populations. An example is when patients experiencing alcohol use disorder are referred to as “addicts.” The term “addicts” has been shown to be associated with reduced patient compliance, lower patient care due to clinician bias, and lower health outcomes [32], [33], [34], [35], [36]. As a result, researchers must be careful with their word selection to minimize the level of stigmatization and social bias within their manuscripts. For example, one of the non-PCL terms we looked at was “stump.” The term “stump” is appropriate to utilize when describing a medical procedure, such as when describing “suturing of the stump” at the end of the surgery, or “fitting a prosthesis for the stump.” However, when the term “stump” is associated with a person who has had an amputation, the term becomes a euphemistic descriptor (non-PCL). Therefore, we agree with studies such as Headley et al. [26] that recommend the use of the term “residual limb” instead of “stump.” By following this, orthopedic and osteopathic physicians are adhering to steps that minimize psychosocial stressors on patients that have to undergo amputations.
One study we want to highlight within our sample was the American Academy of Orthopaedic Surgeons Clinical Practice Guideline Summary for Limb Salvage or Early Amputation published by Potter and Bosse [37]. The clinical practice guidelines (CPGs) for orthopedics is published by the American Academy of Orthopaedic Surgeons (AAOS). Our study found that the summary for the CPG contained non-PCL terminology such as “burden,” and IFL terminology not recognized by amputation organizations such as “HELET patients” (high-energy lower extremity trauma). The use of the term “burden” is problematic due to the negative connotation that it brings and an implication of helplessness [38]. Stigmatization has been shown to have psychological and health implications [8, 39], [40], [41]. In addition, Potter and Bosse [37] show that patients that experienced HELET require screening for psychosocial risk factors, suggesting susceptibility to psychologic distress. Due to CPGs guiding orthopedic clinical decision-making, stigmatizing language should be especially avoided within these manuscripts to prevent the introduction of social bias to patient care [32, 42]. Therefore, we ask that future CPG authors avoid the use of stigmatizing language within the guidelines and summaries.
The terminology surrounding amputations is complicated. Terminology such as “amputee” has been shown to be accepted by the community, as shown by organizational names such as the Amputee Coalition [43]. Therefore, we do not want to infringe on the rights of an individual to identify themselves. However, it should be noted that our data found that the use of the term “amputee” had a higher rate of non-PCL terms being incorporated into a manuscript compared to when it was not utilized. This shows that authors were more prone to utilizing stigmatizing language when utilizing the term “amputee.” These results could be due to authors not having a clear understanding of the appropriate language for individuals experiencing amputations; therefore, it would be beneficial for authors to learn about stigmatizing language through courses. In addition, stigmatizing language can be avoided by journals implementing direct policies through their author guidelines, requiring the use of PCL. Finally, reviewers can help with removing stigmatizing language from literature by identifying its use during the review process.
Osteopathic medicine was built with an emphasis on patient-centered care. With this emphasis, it is essential for osteopathic physicians to follow PCL. The Institute of Medicine and the APA led a movement to shy away from labeling people based on their condition, and they have an emphasis on care toward a patient’s needs and preferences [17, 44]. This movement was conducted as a means of rejecting the stigma present in the scientific community when referring to patients with various disorders [22], [23], [24], [25], [26, 30, 45]. This rejection of patient stigma is a push to highlight the patient as an individual rather than a disorder and is in line with the philosophy of osteopathic medicine. Rogers et al. [21] promote that patients deserve individualized attention that is highlighted by a quality relationship with their physician. Also, it is highlighted that an “osteopathic physician is the advocate for the patient” [21]. By following PCL, physicians promote the individuality of the patient by highlighting that they are not a disorder. In addition, by removing the stigma of non-PCL verbiage, osteopathic physicians are given the opportunity to advance the advocacy of the patient.
Although we conducted our study with methodological rigor, there are a few limitations we have identified to our research. First, our study includes the potential for subjective analysis of non-PCL terminology. We attempted to reduce this effect by utilizing predefined terminology and search criteria. Secondly, due to our cross-sectional study design, results should not be generalized beyond the scope of our study. Due to our initial study identifying PCL within orthopedic literature, more research is warranted to determine the extent of stigmatizing language usage within orthopedic research. Also, although we have a sample with substantial power of 300 articles, we did not search all 687 articles. In addition, there is the possibility of bias with our search terms in identifying amputation literature by adding our non-PCL terminology; however, that was done as a means of extracting all literature published within the 22 journals of our sample set related to amputations.
For future directions, we would like to see research looking at other forms of non-PCL language within the orthopedic literature. Examples can be related to diabetes-related literature utilizing “diabetic patients” rather than “patients with diabetes.” Also, we ask for literature summarizing other common non-PCL terminology that can be identified within orthopedics. Finally, we ask that journals identify and highlight non-PCL terminology during the review process to prevent utilizing it in final manuscripts.
Conclusions
Our findings show that amputation literature within the top orthopedic journals has limited following of PCL. In addition, we found that the use of the term “amputee,” which is widely accepted by the amputation community, resulted in a greater rate of non-PCL terminology within orthopedic amputation literature. Words should be utilized with proper attention and care within the medical literature to eliminate the incorporation of structural stigma within orthopedic research and care. Efforts should be implemented within orthopedics to avoid the use of stigmatizing language, regarding individuals who underwent amputations, in order to minimize psychosocial stressors such as the loss of self-esteem and feelings of isolation.
-
Research funding: None reported.
-
Author contributions: A.K.R., G.R.N., R.N., and N.S. provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; A.K.R., J.X.C., J.T.S., and M.H. drafted the article or revised it critically for important intellectual content; A.K.R., N.S., and M.H., gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None reported.
References
1. Owings, MF, Kozak, LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat 1998;13:1–119.Search in Google Scholar
2. Ziegler-Graham, K, MacKenzie, EJ, Ephraim, PL, Travison, TG, Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89:422–9. https://doi.org/10.1016/j.apmr.2007.11.005.Search in Google Scholar PubMed
3. Inkellis, E, Low, EE, Langhammer, C, Morshed, S. Incidence and characterization of major upper-extremity amputations in the national trauma data bank. JB JS Open Access 2018;3:3e0038. https://doi.org/10.2106/JBJS.OA.17.00038.Search in Google Scholar PubMed PubMed Central
4. Osmon, DR, Berbari, EF, Berendt, AR, Lew, D, Zimmerli, W, Steckelberg, JM, et al.. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis 2013;56:e1–25. https://doi.org/10.1093/cid/cis803.Search in Google Scholar PubMed
5. Maale, GE, Eager, JJ, Srinivasaraghavan, A, Mohammadi, DK, Kennard, N. The evolution from the two stage to the one stage procedure for biofilm based periprosthetic joint infections (PJI). Biofilms 2020;2:100033. https://doi.org/10.1016/j.bioflm.2020.100033.Search in Google Scholar PubMed PubMed Central
6. Robbins, JM, Strauss, G, Aron, D, Long, J, Kuba, J, Kaplan, Y. Mortality rates and diabetic foot ulcers: is it time to communicate mortality risk to patients with diabetic foot ulceration? J Am Podiatr Med Assoc 2008;98:489–93. https://doi.org/10.7547/0980489.Search in Google Scholar PubMed
7. Bennett, J. Limb loss: the unspoken psychological aspect. J Vasc Nurs 2016;34:128–30. https://doi.org/10.1016/j.jvn.2016.06.001.Search in Google Scholar PubMed
8. Mullerpatan, R, Sonkhia, M, Thomas, B, Mishra, S, Gupta, A, Agarwal, B. Review of contextual factors influencing function following lower extremity amputation in low to middle income countries. Crit Rev Phys Rehabil Med 2019;31:173–83. https://doi.org/10.1615/critrevphysrehabilmed.2019031127.Search in Google Scholar
9. Smith, LR, Earnshaw, VA, Copenhaver, MM, Cunningham, CO. Substance use stigma: reliability and validity of a theory-based scale for substance-using populations. Drug Alcohol Depend 2016;162:34–43. https://doi.org/10.1016/j.drugalcdep.2016.02.019.Search in Google Scholar PubMed PubMed Central
10. Phelan, JC, Lucas, JW, Ridgeway, CL, Taylor, CJ. Stigma, status, and population health. Soc Sci Med 2014;103:15–23. https://doi.org/10.1016/j.socscimed.2013.10.004.Search in Google Scholar PubMed PubMed Central
11. Room, R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev 2005;24:143–55. https://doi.org/10.1080/09595230500102434.Search in Google Scholar PubMed
12. Kulesza, M. Substance use related stigma: what we know and the way forward. Addict Behav 2013;02:782. https://doi.org/10.4172/2324-9005.1000106.Search in Google Scholar PubMed PubMed Central
13. Sudnow, D. Dead on arrival. Society 1967;5:36–43. https://doi.org/10.1007/bf03180093.Search in Google Scholar
14. Strong, PM. Doctors and dirty work–the case of alcoholism. Sociol Health Illness 1980;2:24–47. https://doi.org/10.1111/1467-9566.ep11340296.Search in Google Scholar PubMed
15. Santana, P. Poverty, social exclusion and health in Portugal. Soc Sci Med 2002;55:33–45. https://doi.org/10.1016/s0277-9536(01)00218-0.Search in Google Scholar PubMed
16. Leopold, SS, Beadling, L, Gebhardt, MC, Gioe, TJ, Potter, BK, Rimnac, CM, et al.. Editorial: words hurt–avoiding dehumanizing language in orthopaedic research and practice. Clin Orthop Relat Res 2014;472:2561–3. https://doi.org/10.1007/s11999-014-3802-8.Search in Google Scholar PubMed PubMed Central
17. Granello, DH, Gibbs, TA. The power of language and labels: “the mentally ill” versus “people with mental illnesses”. J Counsel Dev 2016;94:31–40. https://doi.org/10.1002/jcad.12059.Search in Google Scholar
18. The JAMA Network Editors. AMA manual of style: a guide for authors and Editors. Oxford University Press; 2019. Available from: https://play.google.com/store/books/details?id=Dy3JDwAAQBAJ.Search in Google Scholar
19. Jensen, ME, Pease, EA, Lambert, K, Hickman, DR, Robinson, O, McCoy, KT, et al.. Championing person-first language: a call to psychiatric mental health nurses. J Am Psychiatr Nurses Assoc 2013;19:146–51. https://doi.org/10.1177/1078390313489729.Search in Google Scholar PubMed
20. Philosophy of osteopathic medicine. Available from: https://www.aacom.org/become-a-doctor/about-osteopathic-medicine/philosophy-tenets-of-osteopathic-medicine [Accessed 1 Oct 2022].Search in Google Scholar
21. Rogers, FJ, D’Alonzo, GEJr, Glover, JC, Korr, IM, Osborn, GG, Patterson, MM, et al.. Proposed tenets of osteopathic medicine and principles for patient care. J Am Osteopath Assoc 2002;102:63–5. https://doi.org/10.7556/jaoa.2002.102.2.63.Search in Google Scholar
22. Hartwell, M, Naberhaus, B, Arnhart, C, Ottwell, R, Dunn, K, Rogers, TC, et al.. The use of person-centered language in scientific research articles focusing on alcohol use disorder. Drug Alcohol Depend 2020;216:108209. https://doi.org/10.1016/j.drugalcdep.2020.108209.Search in Google Scholar PubMed
23. Ottwell, R, Heigle, B, Reddy, AK, Sajjadi, N, Wirtz, A, Cook, C, et al.. The use of person-centered language in medical research journals focusing on psoriasis: cross-sectional analysis. JMIR Dermatology 2021;4:e28415. https://doi.org/10.2196/28415.Search in Google Scholar
24. Traxler, B, Nicks, S, Puckett, M, Dunn, K, Croff, JM, Hartwell, M. The use of person-centered language in scientific research articles focusing on opioid use disorder. Drug Alcohol Depend 2021;228:108965. https://doi.org/10.1016/j.drugalcdep.2021.108965.Search in Google Scholar PubMed
25. Nicks, S, Johnson, AL, Traxler, B, Bush, ML, Brame, L, Hamilton, T, et al.. The use of person-centered language in medical research articles focusing on hearing loss or deafness. Ear Hear 2022;43:703–11. https://doi.org/10.1097/AUD.0000000000001168.Search in Google Scholar PubMed
26. Headley, S, Potter, I, Ottwell, R, Rogers, T, Vassar, M, Hartwell, M. Adherence rates of person-centered language in amputation research: a cross-sectional analysis. Disabil Health J 2022;15:101172. https://doi.org/10.1016/j.dhjo.2021.101172.Search in Google Scholar PubMed
27. Ring, DC, Dobbs, MB, Gioe, TJ, Manner, PA, Leopold, SS. Editorial: how the words we use affect the care we deliver. Clin Orthop Relat Res 2016;474:2079–80. https://doi.org/10.1007/s11999-016-4993-y.Search in Google Scholar PubMed PubMed Central
28. Desmond, DM. Coping, affective distress, and psychosocial adjustment among people with traumatic upper limb amputations. J Psychosom Res 2007;62:15–21. https://doi.org/10.1016/j.jpsychores.2006.07.027.Search in Google Scholar PubMed
29. English - Google Scholar Metrics. Available from: https://scholar.google.com/citations?view_op=top_venues [Accessed 16 Mar 2022].Search in Google Scholar
30. Sowah, E, Delgado, P, Adewumi, MT, Greenough, MC, Gajjar, S, Pasha, J, et al.. Use of person-centered language among scientific research focused on sickle cell disease. J Emerg Med 2022;62:725–32. https://doi.org/10.1016/j.jemermed.2021.12.013.Search in Google Scholar PubMed
31. Google Sheets. Free online spreadsheet editor. Available from: https://www.google.com/sheets/about/ [Accessed 16 Mar 2022].Search in Google Scholar
32. Goddu, PA, O’Conor, KJ, Lanzkron, S, Saheed, MO, Saha, S, Peek, ME, et al.. Do words matter? Stigmatizing Language and the transmission of bias in the medical record. J Gen Intern Med 2018;33:685–91. https://doi.org/10.1007/s11606-017-4289-2.Search in Google Scholar PubMed PubMed Central
33. Ashford, RD, Brown, AM, Curtis, B. Substance use, recovery, and linguistics: the impact of word choice on explicit and implicit bias. Drug Alcohol Depend 2018;189:131–8. https://doi.org/10.1016/j.drugalcdep.2018.05.005.Search in Google Scholar PubMed PubMed Central
34. Kelly, JF, Westerhoff, CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Pol 2010;21:202–7. https://doi.org/10.1016/j.drugpo.2009.10.010.Search in Google Scholar PubMed
35. Johnson, ME, Dowling-Guyer, S. Effects of inclusive vs. exclusive language on evaluations of the counselor. Sex Roles 1996;34:407–18. https://doi.org/10.1007/BF01547809.Search in Google Scholar
36. Avery, JD, Avery, JJ. The stigma of addiction: an essential guide. Springer; 2019. Available from: https://play.google.com/store/books/details?id=JxyDDwAAQBAJ.10.1007/978-3-030-02580-9Search in Google Scholar
37. Potter, CBK, Bosse, MJ. American Academy of orthopaedic Surgeons clinical practice guideline summary for limb salvage or early amputation. J Am Acad Orthop Surg 2021;29:e628–34. https://doi.org/10.5435/JAAOS-D-20-00188.Search in Google Scholar PubMed
38. American Medical Association. AMA manual of style: a guide for authors and. Oxford, England: Oxford University Press; 2019.10.1093/jama/9780190246556.001.0001Search in Google Scholar
39. Ostrow, L, Manderscheid, R, Mojtabai, R. Stigma and difficulty accessing medical care in a sample of adults with serious mental illness. J Health Care Poor Underserved 2014;25:1956–65. https://doi.org/10.1353/hpu.2014.0185.Search in Google Scholar PubMed PubMed Central
40. Phelan, SM, Burgess, DJ, Yeazel, MW, Hellerstedt, WL, Griffin, JM, van Ryn, M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015;16:319–26. https://doi.org/10.1111/obr.12266.Search in Google Scholar PubMed PubMed Central
41. van Boekel, LC, Brouwers, EPM, van Weeghel, J, Garretsen, HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013;131:23–35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.Search in Google Scholar PubMed
42. Grol, R, Hutchinson, A, Eccles, M, Grimshaw, J. Clinical guidelines, potential benefits, limitations, and harms of guidelines. BMJ 1999;318:527–30. https://doi.org/10.1136/bmj.318.7182.527.Search in Google Scholar PubMed PubMed Central
43. Amputee Coalition. learn about amputation & prosthetic care & request support for people living with limb loss, their families, caregivers and clinicians who care for amputees: Amputee Coalition; 2014. Available from: https://www.amputee-coalition.org/ [Accessed 6 Mar 2022].Search in Google Scholar
44. Institute of Medicine, Institute of medicine. Committee on Data Standards for Patient Safety. Board on Health Care Services, Board on Health Care Services, et al.. Patient safety: achieving a new standard for care. National Academies Press; 2004.Search in Google Scholar
45. McPherson, KA, Reddy, AK, Sajjadi, NB, Deboy, K, Gajjar, S, Lad, M, et al.. Person-centered language and HIV research: a cross-sectional examination of stigmatising terminology in medical literature. Sex Transm Infect 2022. https://doi.org/10.1136/sextrans-2021-055391.Search in Google Scholar PubMed
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Beyond burnout: a four-year survey of osteopathic medical student mental health and the implications for the development of wellness and mental health programs
- General
- Original Article
- The presence of person-centered language in orthopedic-related amputation research: a cross-sectional analysis
- Medical Education
- Original Article
- Establishing a baseline for multilingual capabilities of medical students at the Michigan State University College of Osteopathic Medicine
- Musculoskeletal Medicine and Pain
- Original Article
- Retrospective analysis of whole-body cryotherapy adverse effects in Division I collegiate athletes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment of patients with chronic low back pain in the United States: a retrospective cohort study
- Public Health and Primary Care
- Clinical Practice
- Anatomy-based approach to the thyroid examination
- Letters to the Editor
- Osteopathic manipulative techniques in the treatment of vestibular dizziness not related to the cervical spine
- Response to “Osteopathic manipulative techniques in the treatment of vestibular dizziness not related to the cervical spine”
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Beyond burnout: a four-year survey of osteopathic medical student mental health and the implications for the development of wellness and mental health programs
- General
- Original Article
- The presence of person-centered language in orthopedic-related amputation research: a cross-sectional analysis
- Medical Education
- Original Article
- Establishing a baseline for multilingual capabilities of medical students at the Michigan State University College of Osteopathic Medicine
- Musculoskeletal Medicine and Pain
- Original Article
- Retrospective analysis of whole-body cryotherapy adverse effects in Division I collegiate athletes
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment of patients with chronic low back pain in the United States: a retrospective cohort study
- Public Health and Primary Care
- Clinical Practice
- Anatomy-based approach to the thyroid examination
- Letters to the Editor
- Osteopathic manipulative techniques in the treatment of vestibular dizziness not related to the cervical spine
- Response to “Osteopathic manipulative techniques in the treatment of vestibular dizziness not related to the cervical spine”


