Abstract
Context
Osteopathic manipulative medicine (OMM) has been shown to successfully alleviate some pregnancy-related pain. However, most of the published data focuses on the third trimester and postpartum period or musculoskeletal indications.
Objective
To explore OMM use among obstetrical providers and determine the frequency of use by trimester and by clinical indications across multiple types of women’s healthcare practices in Southern and Central Maine.
Methods
An anonymous, 43-item survey, presented in English, was emailed to 172 eligible providers (physicians, nurse practitioners, and certified nurse midwives with obstetrics privileges at one of two main delivery centers in southern and central Maine) via an encrypted database system in January 2018. Follow-up email reminders were sent weekly for three weeks. Questions addressed use of OMM for specific indications, knowledge of OMM, and perceived barriers use of OMM.
Results
The survey response rate was 73 of 172 (42%); 95% of respondents were physicians (n=69). Due to the low response rate of non-physicians, only data from physicians was included in the study. Data were summarized descriptively as frequencies (n [%]). The highest rates of OMM utilization were during the third trimester (35 [51.5%]) and postpartum (41 [60.3%]) periods, while the lowest rates of utilization were in the intrapartum (eight [11.9%]) and first trimester periods (26 [38.3%]). Osteopathic physicians (n=19) used OMM more frequently in the first, second, and third trimesters, as well as the intrapartum period (10 [52.6%]; 11 [57.9%]; 14 [73.7%]; and six [31.6%], respectively) compared with their allopathic physician (n=50) counterparts (nine [8%]; 15 [30%]; 21 [42%]; and two [4%], respectively). While osteopathic physicians reported higher frequencies of OMM use and referral for non-musculoskeletal indications such as constipation, edema, and nasal congestion (13 [68.4%]; 11 [57.9%]; 10 [52.6%], respectively), musculoskeletal complaints were the most frequently cited indication for OMM use among both osteopathic and allopathic physicians (low back, 67 [97.1%]; pelvis, 65 [94.2%]; coccyx, 50 [72.5%]; and head, 49 [71%]).
Conclusion
These results suggest that more education is needed about OMM use in the obstetric population, particularly during early trimesters and the intrapartum period, as well as for visceral and lymphatic complaints of pregnancy.
Throughout pregnancy and the postpartum period, women present with a variety of pregnancy-related concerns associated with the neuromusculoskeletal system. An estimated two-thirds of pregnant patients have low back pain and up to 20% suffer from pelvic girdle pain.1 These patients report decreased quality and length of sleep, increased absenteeism from work, increased stress, and postpartum residual symptoms, while up to one-fourth have temporary disability.1 However, patients often receive little to no treatment for neuromusculoskeletal symptoms throughout pregnancy, and report that pharmaceuticals, exercises, and reassurance given by providers do not help.1
Several studies have shown that osteopathic manipulative medicine (OMM) can alleviate specific musculoskeletal conditions related to pregnancy. A meta-analysis2 of 10 studies found a statistically significant effect of OMM in reducing lower back and pelvic girdle pain compared with usual care. A randomized, controlled study with a sample size of 144 subjects1 found that OMM lessens or halts deterioration in back-specific functioning in the third trimester. In that study, patients receiving usual obstetrical care reported mean pain levels of 6 and 11 at their initial and sixth prenatal visit, respectively, while patients receiving usual obstetrical care plus OMM reported a mean pain level decrease from 8 to 7 between the initial and sixth visits. Additionally, a systematic review including 32 published papers3 reported that musculoskeletal symptoms have been shown to extend into the postpartum period, with up to 25% of women experiencing low back pain. A randomized, controlled trial4 with a total of 80 participants demonstrated that during eight weeks and four full treatments, patients who received OMM postpartum reported a 73% reduction in pain, compared with a 7% decrease in the control group.4
While most of the evidence supporting OMM use in pregnancy involves symptoms presenting in the prenatal and postpartum periods, benefits have been demonstrated during the intrapartum period. One systematic review5 found positive effects regarding decreased pain levels during labor and delivery, as well as decreased analgesia use among patients who received OMM during labor. Furthermore, a multicenter, retrospective study6 reported that women who received prenatal OMM had significantly lower rates of meconium-stained amniotic fluid and preterm labor, as well as marginally lower rates of forceps-assisted deliveries. Martingano et al.7 demonstrated shortened labor duration for patients receiving a standardized osteopathic manipulative treatment (OMT) protocol during labor, compared with controls who received standard labor management only, supporting earlier studies8,9 that also demonstrated a shortening of labor duration with OMT. One proposed mechanism for this finding is the regulation of uterine contractions via sympathetic innervation from the thoracic spine.10 OMT of the cranium has also been shown to affect uterine contractions without inciting preterm labor.11,12
According to multiple osteopathic textbooks,13,14 indications for use of OMM during pregnancy extend beyond the commonly studied musculoskeletal concerns to include headache, nausea, vomiting, edema, gastroesophageal reflux disease, dyspnea, constipation, urinary frequency, hemorrhoids, paresthesia, hypertension, and glucose imbalance, yet few investigations have addressed OMM use for these aforementioned complaints of pregnancy, nor do they stratify use by trimester. In this study, we explore potential underuse of OMM during the prenatal, intrapartum, and postpartum periods, including its indications for use, characterize this use by provider type and specialty, and identify potential barriers to OMM use.
Methods
Obstetrical care providers from Portland, Augusta, and Waterville, Maine, were eligible for inclusion in this cross-sectional study if they had obstetrics privileges at one of two main delivery centers in Southern and Central Maine. Providers included attending and resident physicians, as well as family nurse practitioners (FNPs) and certified nurse midwives (CNMs). Both delivery centers were located at training hospitals: one with a dually-accredited (American Osteopathic Association/Accreditation Council for Graduate Medical Education [ACGME]) family medicine residency program, and one with ACGME-accredited residency programs for both family medicine and obstetrics/gynecology. The study was determined to be exempt by the institutional review boards at both Maine Medical Center and Maine General Medical Center.
An anonymous, 43-item survey, presented in English, was emailed to 172 eligible providers via an encrypted database system in January 2018. Follow-up email reminders were sent weekly for three weeks (Appendix A). Of the 43 questions, 23 were on a five-point Likert scale (one regarding familiarity with OMM [1=Slightly, 5=Extremely], five regarding use of or referral to OMM during pregnancy periods [1=Never, 5=Always], 12 regarding likelihood of using OMM for a specific indication [1=Extremely unlikely, 5=Extremely likely] five regarding perceived barriers of OMM use [1=Extreme barrier, 5=Not a barrier]), eight were true/false questions, one was open-ended, and the remaining nine questions were demographic.
The survey was developed internally, in collaboration with local OMM and obstetric providers, because we were unable to identify any published, validated surveys targeting the specific questions of this study. Questions about the use of OMM for specific indications were developed based on findings from prior studies1,2,3,4,5,13,14 identifying potential uses of OMM in pregnancy; these same indications were assessed for each trimester as follows: nausea, headaches, constipation, peripheral edema, carpal tunnel syndrome, De Quervain’s tenosynovitis, low back pain, pelvic girdle pain, anxiety, nasal congestion, coccydynia, intrapartum pain, and hemorrhoids. Questions about OMM knowledge were based on common misconceptions that nonosteopathic providers may have about OMM.15,16 We included questions to address perceived barriers to the use of OMM in patient care, followed by one open-ended question inquiring about the types of adjunctive treatment used by the practitioner.
Demographic data were collected categorically; practice factors were included if they were relevant to planned data stratification, such as training type and provider specialty, or if they had known associations with use of OMM or adjunctive treatment.15,16,17
Statistical analysis
Data were summarized descriptively as frequencies (n [%]). Each survey item was analyzed separately and unanswered questions were excluded. Five-point Likert data were combined into three-point scales before analysis due to low responses in some categories and to simplify presentation of the data. In assessing familiarity with OMM, the combined categories were “not at all/slightly familiar,” “somewhat familiar,” and “moderately/extremely familiar.” For frequency of referrals to, or use of, OMM, the combined categories were “never/rarely,” “occasionally,” and “often/always.” For the likelihood of using OMM for a specific indication, combined categories were “extremely unlikely/unlikely”, “neutral,” and “likely/extremely likely.” For barriers to OMM use, the combined categories were “extreme barrier,” “moderate barrier/somewhat of a barrier,” and “not a barrier.” Although this was a preliminary study and not powered to detect a specific outcome, we performed exploratory analyses to compare proportions between subgroups using χ2 test or Fisher exact test, as appropriate. All analyses were performed using SPSS Statistical Software, version 25 (IBM, Inc.).
Results
Of 172 providers to whom the survey was distributed, 73 (42%) responded (Figure 1). Due to the lower response rate of non-physician providers (n=4) compared with physician providers, we limited our analysis to the 69 physicians who completed the survey, resulting in a physician response rate of 40%. Of the 69 physicians who responded, not all questions were answered. We adjust the n for those unanswered questions in our presentation of the data accordingly. The characteristics of the physician respondents are summarized in Table 1. Of the 69 physicians who completed the survey, 53 (76.8%) were women, 16 (23.2%) were men, 50 (72.5%) were allopathic physicians, 40 (57.9%) practiced family medicine, and 40 (57.9%) worked in the context of a residency program. Experience levels varied from current resident (28 [40.6%]) to more than 20 years in practice (11 [15.9%]). Although most physicians (47 [68.1%]) reported being “moderately/extremely familiar” with OMM, this differed by training and by specialty. Twenty-eight of 49 (57.1%) allopathic physicians were “moderately/extremely familiar” with OMM compared with 19 osteopathic physicians (100%; p<0.001). (One provider did not answer this question; therefore, that person was excluded from this questions analysis, leaving a total of 49 responses.) Additionally, 31 of 40 (77.5%) family medicine physicians were “moderately/extremely familiar” with OMM, compared with 15 of 28 (53.5%) obstetrics and gynecology physicians (not significant, p=0.10). Medical training, however, differed by specialty; 15 of 40 (37.5%) family medicine physicians had osteopathic training compared with three of 28 (10.7%) obstetrics and gynecology physicians.
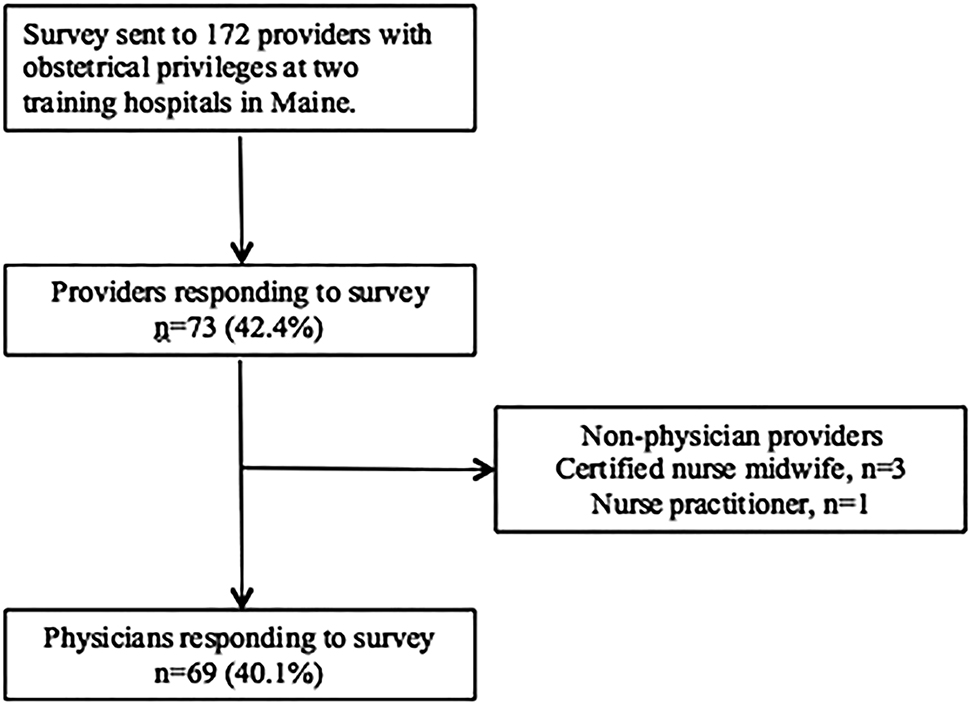
Survey distribution and responses.
Characteristics of physicians responding to survey.
| Variable | Frequency, n (%) |
|---|---|
| N | 69 |
| Female sex | 53 (76.8) |
| Experience (years in practice) | |
| Current resident | 28 (40.6) |
| <5 | 6 (8.7) |
| 5–10 | 9 (13.0) |
| 11–20 | 15 (21.7) |
| 21–30 | 11 (15.9) |
| Specialty | |
| Family medicine | 40 (57.9) |
| Obstetrics and gynecology | 28 (40.6) |
| Other | 1 (1.4) |
| Degree | |
| DO | 50 (72.5) |
| MD | 19 (27.5) |
| Practice setting | |
| Residency clinic | 40 (57.9) |
| Private practice | 17 (24.6) |
| Hospital-affiliated practice | 10 (14.5) |
| Other/unknown | 2 (2.9) |
| Familiarity with OMM | |
| Slightly/not at all | 9 (13.0) |
| Somewhat | 13 (18.8) |
| Moderately/extremely | 13 (18.8) |
DO, doctor of osteopathic medicine; OMM, osteopathic manipulative medicine; MD, doctor of [allopathic] medicine
Out of 60 respondents who answered the question, 59 (98.3%) providers agreed that OMM is useful for helping neuromusculoskeletal pain related to pregnancy; actual OMM usage was less frequent, however. Overall, 50 of 68 (73.5%) providers reported that they “often/always” used OMM or referred patients to an OMM specialist at some point during pregnancy or postpartum. This rate varied slightly, though not significantly, with provider training; 34 of 49 (69.4%) allopathic physicians reported any use of, or referral to, OMM during pregnancy and postpartum, compared with 16 of 19 (84.2%) osteopathic physicians (p=0.36). Table 2 summarizes providers’ reported use of and referral to, OMM at different stages of pregnancy, both overall and after stratification by training. OMM use and referral increased monotonically with trimester. Of the 67 physicians who responded, 19 (27.5%) reported that they “often/always” used, or referred to, OMM in the first trimester, 26 (38.2%) in the second trimester, and 35 (51.5%) in the third trimester. This same trend was seen among both osteopathic and allopathic physicians. Use of, or referral to, OMM was least frequent intrapartum (“often/always”: eight of 67; 11.9%) and most frequent postpartum (“often/always”: 41 of 67; 60.3%). At each stage of pregnancy, OMM usage was higher among osteopathic physicians than allopathic physicians; this was significant in the first trimester (p=0.017) and third trimester (p=0.048). The discrepancy was largest for the intrapartum period, with two of 48 (4.2%) allopathic physicians “often/always” using, or referring to, OMM, compared with six of 19 (31.6%) osteopathic physicians (p=0.003). A similar trend was seen when data were stratified by specialty, with higher rates of OMM usage among family medicine physicians than among obstetrics and gynecology physicians at all stages of pregnancy (Appendix B).
Physicians’ use of or referrals for osteopathic manipulative medicine (OMM) in pregnancy.
| Use of, or referral to, OMM | Frequency, n (%) | |||
|---|---|---|---|---|
| Overall | Osteopathic | Allopathic | p-Valueb | |
| N | 67 | 48 | 19 | |
| 1st trimesterb | ||||
| Never/rarely | 27 (40.3) | 23 (47.9) | 4 (21.1) | 0.017 |
| Occasionally | 21 (31.3) | 16 (33.3) | 5 (26.3) | |
| Often/always | 19 (27.5) | 9 (18.8) | 10 (52.6) | |
| 2nd trimester | ||||
| Never/rarely | 13 (19.1) | 11 (22.4) | 2 (10.5) | 0.13 |
| Occasionally | 29 (42.6) | 23 (46.9) | 6 (31.6) | |
| Often/always | 26 (38.2) | 15 (30.6) | 11 (57.9) | |
| 3rd trimester | ||||
| Never/rarely | 8 (11.8) | 6 (12.2) | 2 (10.5) | 0.048 |
| Occasionally | 25 (36.8) | 22 (44.9) | 3 (15.8) | |
| Often/always | 35 (51.5) | 21 (42.9) | 14 (73.7) | |
| Intra-partum1 | ||||
| Never/rarely | 49 (73.1) | 40 (83.3) | 9 (47.4) | 0.003 |
| Occasionally | 10 (14.9) | 6 (12.5) | 4 (21.1) | |
| Often/always | 8 (11.9) | 2 (4.2) | 6 (31.6) | |
| Postpartum | ||||
| Never/rarely | 3 (4.4) | 2 (4.1) | 1 (5.3) | 0.51 |
| Occasionally | 24 (35.3) | 19 (38.8) | 5 (26.3) | |
| Often/always | 41 (60.3) | 28 (57.1) | 13 (68.4) | |
aFirst trimester data were analyzed by χ2 test; all other analyses used Fisher exact test.
Table 3 summarizes physicians’ responses to questions about their use of, and referral to, OMM for common conditions occurring during pregnancy. Among 69 physicians, OMM was used most frequently during pregnancy for four pain-related conditions associated with the axial skeleton (low back, 67 [97.1%]; pelvis, 65 [94.2%]; coccyx, 50 [72.5%]; and head, 49 [71%]). There was no significant difference in usage rates between osteopathic and allopathic physicians for these conditions (Table 3, p>0.05). For all other listed conditions, there was significantly higher usage of OMM among osteopathic physicians. Musculoskeletal conditions such as carpal tunnel syndrome (31 [44.9%]; p=0.008) and De Quervain tenosynovitis (26 [37.7%]; p<0.001) had intermediate usage, while OMM was less frequently used for visceral or lymphatic symptoms such as nausea (10 [14.5%]) or peripheral edema (18 [26.1%]). Similar findings were observed when data were stratified by specialty, with higher rates of use for most conditions cited by family medicine providers (Appendix B).
Likelihood of using OMM for specific conditions during pregnancy.
| Condition | Likely/Extremely likely to use or refer to OMM, n (%) | |||
|---|---|---|---|---|
| Overall | Physician training | p-valuea | ||
| Allopathic | Osteopathic | |||
| N | 68 | 50 | 18 | |
| Nausea | 10 (14.5) | 4 (8.0) | 6 (31.6) | 0.013 |
| Headaches | 49 (71.0) | 32 (64.0) | 17 (89.5) | 0.071 |
| Constipation | 22 (31.9) | 9 (18.0) | 13 (68.4) | <0.001 |
| Peripheral edema | 18 (26.1) | 7 (14.0) | 11 (57.9) | <0.001 |
| Carpal tunnel syndrome | 31 (44.9) | 15 (30.0) | 16 (84.2) | <0.001 |
| DeQuervains tenosynovitis | 26 (37.7) | 13 (26.0) | 13 (68.4) | 0.008 |
| Low back pain | 67 (97.1) | 48 (96.0) | 19 (100.0) | 1.00 |
| Pelvic girdle pain | 65 (94.2) | 47 (94.0) | 18 (94.7) | 0.17 |
| Anxiety | 11 (15.9) | 6 (12.0) | 5 (26.3) | 0.020 |
| Nasal congestion | 15 (21.7) | 5 (10.0) | 10 (52.6) | <0.001 |
| Coccydynia/tailbone pain | 50 (72.5) | 35 (70.0) | 15 (78.9) | 0.91 |
| Hemorrhoids | 5 (7.2) | 1 (2.0) | 4 (22.2) | 0.005 |
aFisher’s exact test.
To explore barriers to the use of OMM for pregnant patients, we used data only from physicians who gave a definitive response to a given question; those who did not answer the question or who reported that they were “unsure” were excluded. Access to OMM was the largest perceived barrier to use, with 45 of 66 physicians (68.2%) reporting some extent of an access as a barrier (Table 4). In contrast, the least frequently-reported barrier by physicians (22/63; 34.9%) was working in a setting where use of, or referral to, OMM was not part of routine practice. There was no significant difference detected between osteopathic and allopathic physicians in their perception of routine practice patterns (seven/17 [41.2%], and 15/46 [32.6%], respectively) or patient compliance (12/17 [7.6%], and 24/48 [50%], respectively) as barriers to OMM use. In contrast, compared with their osteopathic counterparts, allopathic physicians more frequently cited barriers to OMM use as follows: access to OMM (38/49 [77.6%] vs. seven/17 [41.2%]; p=0.013); cost/insurance (35/53 [66%] vs. seven/15 [46.7%]; p=0.040); and referrals (30/47 [63.8%] vs. two/16 [12.5%]; p=0.001). Additionally, many participants, osteopathic and allopathic physicians alike, noted “time” as a barrier to use in the comments section.
Perceived barriers to use of OMM among physicians providing obstetric services.
| Barrier type | Overalla | Physician training | p-valueb | |
|---|---|---|---|---|
| Allopathic | Osteopathic | |||
| Access | ||||
| Extreme barrier | 8 (12.1) | 8 (16.3) | 0 (0.0) | 0.013 |
| Moderate/somewhat | 37 (56.1) | 30 (61.2) | 7 (41.2) | |
| Not a barrier | 21 (31.8) | 11 (22.4) | 10 (58.8) | |
| Cost/Insurance | ||||
| Extreme barrier | 5 (8.6) | 4 (9.3) | 1 (6.7) | 0.040 |
| Moderate/somewhat | 37 (63.8) | 31 (72.1) | 6 (40.0) | |
| Not a barrier | 16 (27.6) | 8 (18.6) | 8 (53.3) | |
| Referral | ||||
| Extreme barrier | 1 (1.6) | 1 (2.1) | 0 (0.0) | 0.001 |
| Moderate/somewhat | 31 (49.2) | 29 (61.7) | 2 (12.5) | |
| Not a barrier | 31 (49.2) | 17 (36.2) | 14 (87.5) | |
| Not routine in practice setting | ||||
| Extreme barrier | 2 (3.2) | 2 (4.3) | 0 (0.0) | 0.66 |
| Moderate/somewhat | 20 (31.7) | 13 (28.3) | 7 (41.2) | |
| Not a barrier | 41 (65.1) | 31 (67.4) | 10 (58.8) | |
| Patient compliance | ||||
| Extreme barrier | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.17 |
| Moderate/somewhat | 36 (55.4) | 24 (50.0) | 12 (70.6) | |
| Not a barrier | 29 (44.6) | 24 (50.0) | 5 (29.4) | |
aPhysicians not answering a question or responding “unsure” to a question were excluded from the analysis of that question.
bFisher exact test.
Discussion
Use of OMM was highest among all providers in the third trimester and postpartum period, with the lowest overall use during the first trimester and intrapartum period. Our data further revealed that osteopathic physicians were more likely to use OMM during all trimesters, and intrapartum, compared with allopathic physicians. Both allopathic and osteopathic physicians were equally likely to use and refer to OMM postpartum.
Each stage of pregnancy carries unique indications for OMM use because of various physiologic changes taking place.13,14 For instance, in the first trimester, morning sickness is a common complaint, thought secondary to increased progesterone levels.18 Common presenting problems of the second trimester include sciatica, as the uterus begins to grow out of the pelvis and increases the axial strain on the lumbar spine and sacrum; round ligament pain, which may correspond to anterior lumbar counterstrain points or pelvic dysfunction; and carpal tunnel syndrome, resulting from localized edema, which occurs more commonly in women with preeclampsia and hypertension.18 One confounding factor to consider may be that patients with pregnancy-related complaints do not present as frequently during the early trimesters. A study exploring the time periods when patients present and when treatment is initiated would provide more insight into the data presented by our current study. For instance, the PROMOTE study19 revealed that OMM plus usual OB care can halt back-specific dysfunction when compared with usual OB care alone.1,20 Future studies could also assess whether initiation of OMM during the first trimester would help halt further deterioration in subsequent trimesters for pre-existing back pain.
Studies targeting the use of OMM during the intrapartum period are also needed. One systematic review5 suggested decreased levels of pain during labor and delivery and decreased use of analgesia among patients receiving OMM during labor. Even more compelling are shortened labor duration times, with applied OMT during the intrapartum period, as demonstrated by Martingano et al.,7 Hart,8 and Whiting.9 While a study performed by Hensel et al.12 reported an increase in labor duration, compared with the prior studies,7,8,9 labor duration was not reported in terms of hours and minutes due to notable discrepancies found in the medical records among multiple history taker; labor duration was instead defined as precipitous (<3 hours) or prolonged labor (>20 hours). Further, in Hensel et al.,12 OMT was not performed by the same physician who managed the labor and delivery, unlike other studies.7,8,9 Future research specifically targeting larger study cohorts could prove useful in the management of labor and delivery ongoing.
Our study also identified areas of decreased utilization when assessing specific indications for use. Although osteopathic physicians were more likely to use and refer to OMM for all indications compared with allopathic physicians, both groups cited musculoskeletal complaints as the highest indication for use and referral. This finding is further supported by a study21 that revealed OMT is most frequently directed at the musculoskeletal system (51.5%), and that OMT was less frequently used for other conditions including edema (0.14%), hemorrhoids (0.5%), constipation (0.18%), and GERD (0.14%). This same study cited pregnancy as accounting for only 0.5% of treated conditions.21
The decreased use of OMM for visceral and lymphatic complaints demonstrated by our study, along with increased use for musculoskeletal conditions, appears consistent with the breadth of literature supporting OMM use for lower back pain and pelvic girdle pain in the obstetric population. Given that studies have shown a benefit for visceral and lymphatic treatments outside of pregnancy,22,23 we conclude that these treatments would also benefit the obstetric population. Targeting future studies toward pregnant patients and enhancing education around the varied indications for OMM use could serve as a nidus for further research efforts.
We also observed the trend that family medicine physicians were more likely than obstetrics physicians to use and refer to OMM during the third trimester and intrapartum periods, and for non-musculoskeletal conditions. However, the incidence of osteopathic training was much higher among the family medicine physician cohort (37.5% vs. 10.7% in obstetrics physicians), which may explain this finding. Regardless, the trend is similar to a previous study,24 which reported that 69.9% of family medicine physicians used or referred to OMM on 5% or more of their patients, while only 31.3% of specialists did. While our study supports the evidence that family medicine physicians are more likely to use and refer to OMM, a larger cohort study would be necessary to examine the effects of specialty on OMM use, independent of medical training type.
The highest perceived barriers to OMM use cited among allopathic respondents were access to care, cost, and familiarity with indications for referral. Several respondents listed in the comments section that time is a barrier to use. This disclosure is supported by a previous study24 comprised solely of osteopathic physicians, in which 62% of respondents cited time constraints as a major factor limiting OMT use in their practices. It is worth considering how the results of this study might change if these barriers were mitigated. However, this undertaking would require a systems-based change beyond the scope of this project.
Potential weaknesses of this study include the use of self-reported data and our small study sample. However, the total response rate of 42% was greater than the mean rate of 30% for non-incentivized surveys.25 Also worth mentioning is the increased prevalence of OMM use in the northeastern United States, where osteopathic physicians provide more than a third of general and family medicine patient visits.26 This number is high, considering osteopathic physicians comprise only 8.5% of all licensed physicians in the US.27
Conclusion
Data from this study demonstrated the highest use of, and referral to, OMM during pregnancy in the third trimester and postpartum periods for musculoskeletal complaints such as back pain. These data suggest an explanation for the fact that most publications studying OMM in pregnancy target musculoskeletal complaints, specifically during the third trimester and postpartum periods. Our study also demonstrated that osteopathic physicians were more likely to use or refer to OMM for all indications, compared with allopathic physicians. Our findings therefore suggest that providers with more exposure to, and familiarity with, OMM are more likely to use or refer to OMM during times of lowest use in pregnancy, as evidenced by osteopathic physicians reporting higher frequencies of OMM use during all trimesters and antepartum, as well as higher frequencies of referral for non-musculoskeletal indications, such as constipation, edema, and nasal congestion, This finding has not been represented in prior studies, thereby revealing a significant potential for educational expansion, particularly considering the recent transition to a single accreditation body which allows residency programs to opt for “osteopathic recognition,” effectively exposing more physicians in training to the practice of OMM and its indications for use. Our data thereby suggests that education on the benefits of OMM throughout all stages of pregnancy could prove useful for the future care of obstetric patients, improving outcomes regarding pain and other associated morbidities.
Acknowledgements
The authors wish to thank the respondents to this survey; attending physicians Bryan Beck, DO, Kiran Mangalam, DO, Daniel Spratt, MD, for encouraging this study; and Kathryn Lohmann, MD, for editorial assistance.
Research funding: None declared.
Ethical Approval: The study was determined to be exempt by institutional review boards at both Maine Medical Center and Maine General Medical Center.
Author contributions: Drs Faloon, Brock, and Craig provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; Drs Faloon, Brock, and Bishop drafted the article or revised it critically for important intellectual content; Drs Faloon and Bishop gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests: Authors state no conflict of interest.
References
1. Licciardone, JC, Buchanan, S, Hensel, KL, King, HH, Fulda, KG, Stoll, ST. Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: a randomized controlled trial. Am J Obstet Gynecol. 2010;202(1):43 e41-48. https://doi.org/10.1016/j.ajog.2009.07.057.Search in Google Scholar
2. Hall, H, Cramer, H, Sundberg, T, et al.. The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain: A systematic review with meta-analysis. Medicine (Baltimore). 2016;95(38):e4723. https://doi.org/10.1097/MD.0000000000004723.Search in Google Scholar
3. Wu, WH, Meijer, OG, Uegaki, K, et al.. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13(7):575-589. https://doi.org/10.1007/s00586-003-0615-y.Search in Google Scholar
4. Schwerla, F, Rother, K, Rother, D, Ruetz, M, Resch, KL. Osteopathic manipulative therapy in women with postpartum low back pain and disability: a pragmatic randomized controlled trial. J Am Osteopath Assoc. 2015;115(7):416-425. https://doi.org/10.7556/jaoa.2015.087.Search in Google Scholar
5. Ruffini, N, D’Alessandro, G, Cardinali, L, Frondaroli, F, Cerritelli, F. Osteopathic manipulative treatment in gynecology and obstetrics: A systematic review. Complement Ther Med. 2016;26:72-78. https://doi.org/10.1016/j.ctim.2016.03.005.Search in Google Scholar
6. King, HH, Tettambel, MA, Lockwood, MD, Johnson, KH, Arsenault, DA, Quist, R. Osteopathic manipulative treatment in prenatal care: a retrospective case control design study. J Am Osteopath Assoc. 2003;103(12):577-582.Search in Google Scholar
7. Martingano, D, Ho, S, Rogoff, S, Chang, G, Aglialoro, GC. Effect of osteopathic obstetrical management on the duration of labor in the inpatient setting: a prospective study and literature review. J Am Osteopath Assoc. https://doi.org/10.7556/jaoa.2019.066.2019;119(6):371-378.Search in Google Scholar
8. Hart, L. Obstetrical Practice. J Am Osteopath Assoc. 1918(1918):609-614.Search in Google Scholar
9. Whiting, L. Can the length of labor be shortened by osteopathic treatment? J Am Osteopath Assoc. 1911;11:917-921.Search in Google Scholar
10. Guthrie, RA, Martin, RH. Effect of pressure applied to the upper thoracic (placebo) versus lumbar areas (osteopathic manipulative treatment) for inhibition of lumbar myalgia during labor. J Am Osteopath Assoc. 1982;82(4):247-251.10.1515/jom-1982-821219Search in Google Scholar
11. Gitlin, R, Wolf, D. Uterine contractions following osteopathic cranial manipulation - a pilot study. J Am Osteopath Assoc. 1992;92:1183.Search in Google Scholar
12. Hensel, KL, Roane, BM. Does Compression of the Fourth Ventricle Cause Preterm Labor? Analysis of Data From the PROMOTE Study. J Am Osteopath Assoc. 2019;119(10):668-672. https://doi.org/10.7556/jaoa.2019.114.Search in Google Scholar
13. Sandler, S. Osteopathy and Obstetrics. Anshan Ltd; 2012.Search in Google Scholar
14. Tettambel, M. Obstetrics. In: Foundations for Osteopathic Medicine Second Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:450-461.Search in Google Scholar
15. Reeves, RR, Burke, RS. Perception of osteopathic medicine among allopathic physicians in the deep central southern United States. J Am Osteopath Assoc. 2009;109(6):318-323.Search in Google Scholar
16. Allee, BA, Pollak, MH, Malnar, KF. Survey of osteopathic and allopathic residents’ attitudes toward osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105(12):551-561.Search in Google Scholar
17. McPartland, JM, Pruit, PL. Opinions of MDs, RNs, allied health practitioners toward osteopathic medicine and alternative therapies: results from a Vermont survey. J Am Osteopath Assoc. 1999;99(2):101-108. https://doi.org/10.7556/jaoa.1999.99.2.101.Search in Google Scholar
18. Voitk, AJ, Mueller, JC, Farlinger, DE, Johnston, RU. Carpal tunnel syndrome in pregnancy. Can Med Assoc J. 1983;128(3):277-281.10.1097/00006254-198309000-00006Search in Google Scholar
19. Hensel, KL, Buchanan, S, Brown, SK, Rodriguez, M, Cruser, dA. Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects: the PROMOTE study. Am J Obstet Gynecol. 2015 Jan;212(1):108.e1-9. https://doi.org/10.1016/j.ajog.2014.07.043. Epub 2014 Jul 25.Search in Google Scholar
20. Licciardone, JC, Aryal, S. Prevention of progressive back-specific dysfunction during pregnancy: an assessment of osteopathic manual treatment based on Cochrane Back Review Group criteria. J Am Osteopath Assoc. 2013;113(10):728-736. https://doi.org/10.7556/jaoa.2013.043.Search in Google Scholar
21. Johnson, SM, Kurtz, ME. Conditions and diagnoses for which osteopathic primary care physicians and specialists use osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102(10):527-532, 537-540.Search in Google Scholar
22. Muller, A, Franke, H, Resch, KL, Fryer, G. Effectiveness of osteopathic manipulative therapy for managing symptoms of irritable bowel syndrome: a systematic review. J Am Osteopath Assoc. 2014;114(6):470-479. https://doi.org/10.7556/jaoa.2014.098.Search in Google Scholar
23. da Silva, RC, de Sa, CC, Pascual-Vaca, AO, et al.. Increase of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal reflux. Dis Esophagus. 2013;26(5):451-456. https://doi.org/10.1111/j.1442-2050.2012.01372.x.Search in Google Scholar
24. Johnson, SM, Kurtz, ME. Diminished use of osteopathic manipulative treatment and its impact on the uniqueness of the osteopathic profession. Acad Med. 2001;76(8):821-828. https://doi.org/10.1097/00001888-200108000-00016.Search in Google Scholar
25. Brtnikova, M, Crane, LA, Allison, MA, Hurley, LP, Beaty, BL, Kempe, A. A method for achieving high response rates in national surveys of U.S. primary care physicians. PLoS One. 2018;13(8):e0202755. https://doi.org/10.1371/journal.pone.0202755.Search in Google Scholar
26. Licciardone, JC. A comparison of patient visits to osteopathic and allopathic general and family medicine physicians: results from the National Ambulatory Medical Care Survey, 2003-2004. Osteopath Med Prim Care. 2007;1:2. https://doi.org/10.1186/1750-4732-1-2.Search in Google Scholar
27. Young, A, Pei, X, Arnhart, K, Dugan, M, Snyder, GB. A census of actively licensed physicians in the United States, 2016. J Med Reg. 2017;103(2):14.10.30770/2572-1852-103.2.7Search in Google Scholar
The survey is printed in this Appendix as it was distributed by the authors, with no editorial changes.
You are being asked to participate in research
STUDY TITLE: Characterizing the Utilization of Osteopathic Manipulative Medicine in the Obstetric population in Portland, ME
PRINCIPAL INVESTIGATOR: Jordan Faloon, DO
WHAT ARE MY RIGHTS AS A PARTICIPANT?
Taking part in this study is your choice. You may choose not to take part or may leave the study at any time. Choosing to participate or not will not affect your employment status.
WHY IS THIS STUDY BEING DONE?
The purpose of the study is to investigate the use of and barriers to utilization of osteopathic manipulative medicine in the obstetric population in Portland. OMM encompasses a set of manual manipulative techniques that uses scientific and medical knowledge to treat neuromuscular complaints and alleviate conditions that are associated with somatic dysfunction.
WHY ARE YOU BEING ASKED TO PARTICIPATE IN THIS STUDY?
You are being asked to participate in this research as you have been identified as an obstetric provider in the Portland area.
WHAT IS INVOLVED IN THE STUDY?
You will be asked to complete a survey that should take 10 min to complete. Answers to the survey are confidential and are not linked in any way to your identity.
WHAT ARE THE RISKS OF THE STUDY?
Risks of the study include loss of confidentiality and emotional risks, however minimal. This survey is de-identified to maintain confidentiality. You may skip any question that makes you feel uncomfortable or stop and exit the survey at any time.
WHO WILL SEE THIS INFORMATION?
Study personnel, members of the Maine Medical Center Institutional Review Board, personnel from the Office of Human Research Protections or any regulatory agency may see the results of the study. The information collected is the property of the researcher, and you will not be able to get it back. In the event of any publication regarding this study, your identity will not be disclosed. Efforts will be made to keep your personal information confidential including de-identification, password protection and secured storage. We cannot guarantee absolute confidentiality.
WHOM DO I CALL IF I HAVE QUESTIONS OR PROBLEMS?
For questions about the study contact Jordan Faloon at 207-731-3442
For questions about your rights as a research participant, contact the Maine Medical Center Institutional Review Board (which is a group of people who review the research to protect your rights) at (207) 396-8128.
Participation in this study is voluntary and you can withdraw or stop at any time. Completion and return of the survey implies voluntary consent. The Maine Medical Center IRB has approved both the study and survey. We appreciate your participation and honest answers in this survey.
Please answer the following questions, making sure not to include any identifying information
How many years have you been in practice?
Currently a resident
Less than 5 years
5–10 years
11–20 years
21–30 years
31+ years
What is your gender?
Male
Female
What is your degree?
MD
DO
NP
CNM
What specialty do you work in?
Family Medicine
Obstetrics and Gynecology
Other
What practice setting do you work in?
Residency
Private practice
Maine Health affiliated practice
Other
How familiar are you with OMM?
Not at all familiar
Slightly familiar
Somewhat familiar
Moderately familiar
Extremely familiar
| 8. I believe the following is true about OMT: | ||
|---|---|---|
| Agree | Disagree | |
| OMM is useful for helping neuromuscular pain related to pregnancy. | ||
| OMM focuses on the muscular system throughout the entire body including soft tissues and joints. | ||
| By using viscerosomatic pathways, OMM can evoke visceral reactions to help alleviate a variety of symptoms related to pregnancy | ||
| OMM uses a variety of techniques such a soft tissue manipulation, myofascial release, counterstain techniques, and high velocity/low amplitude techniques. | ||
I would consider seeking OMM for my own neuromuscular problems
Would not consider
Might or might not consider
Definitely consider
I would consider utilizing the following educational activities to increase my knowledge of OMM:
Grand Rounds presentation
Free ∼30 minute OMM session on myself
Patient testimonials
Educational emails
Other
I would not consider utilization of any educational material
Use of OMM in pregnancy, by provider specialty.a
| Survey question | Frequency, n (%) | |
|---|---|---|
| Obstetrics and gynecology | Family medicine | |
| I use/refer to OMM in the first trimester | ||
| n | 27 | 39 |
| Never/rarely | 14 (51.9) | 12 (30.8) |
| Occasionally | 7 (25.9) | 14 (35.9) |
| Often/always | 6 (22.2) | 13 (33.3) |
| I use/refer to OMM in the second trimester | ||
| n | 28 | 39 |
| Never/rarely | 9 (32.1) | 3 (7.7) |
| Occasionally | 10 (35.7) | 19 (48.7) |
| Often/always | 9 (32.1) | 17 (43.6) |
| I use/refer to OMM in the third trimester | ||
| n | 28 | 39 |
| Never/rarely | 4 (14.3) | 3 (7.7) |
| Occasionally | 13 (46.4) | 12 (30.8) |
| Often/always | 11 (39.3) | 24 (61.5) |
| I use/refer to OMM intra-partum | ||
| n | 27 | 39 |
| Never/rarely | 26 (96.3) | 22 (56.4) |
| Occasionally | 1 (3.7) | 9 (23.1) |
| Often/always | 0 (0.0) | 8 (20.5) |
| I use/refer to OMM postpartum | ||
| n | 28 | 39 |
| Never/rarely | 0 (0.0) | 2 (5.1) |
| Occasionally | 10 (35.7) | 14 (35.9) |
| Often/always | 18 (64.3) | 23 (59.0) |
| Any prior use of/referral to OMM in pregnancy | ||
| n | 28 | 39 |
| No (answered 1-3 on all usage questions) | 6 (21.4) | 11 (28.2) |
| Yes (answered 4-5 on any usage questions) | 22 (78.6) | 28 (71.8) |
aExcluded n=1 physician with specialty = other
Likelihood of using OMM for specific conditions, by provider specialty.a
| Survey question | Frequency, n (%) | |
|---|---|---|
| Obstetrics and gynecology | Family medicine | |
| Nausea | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 24 (85.7) | 18 (45.0) |
| Neutral | 2 (7.1) | 14 (35.0) |
| Likely/extremely likely | 2 (7.1) | 8 (20.0) |
| Headaches | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 8 (28.6) | 2 (5.0) |
| Neutral | 7 (25.0) | 3 (7.5) |
| Likely/extremely likely | 13 (46.4) | 35 (87.5) |
| Constipation | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 21 (75.0) | 9 (22.5) |
| Neutral | 4 (14.3) | 13 (32.5) |
| Likely/extremely likely | 3 (10.7) | 18 (45.0) |
| Peripheral edema | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 21 (75.0) | 15 (37.5) |
| Neutral | 4 (14.3) | 11 (27.5) |
| Likely/extremely likely | 3 (10.7) | 14 (35.0) |
| Carpal tunnel syndrome | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 10 (35.7) | 13 (32.5) |
| Neutral | 6 (21.4) | 8 (20.0) |
| Likely/extremely likely | 12 (42.9) | 19 (47.5) |
| DeQuervains tenosynovitis | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 9 (32.1) | 16 (40.0) |
| Neutral | 9 (32.1) | 8 (20.0) |
| Likely/extremely likely | 10 (35.7) | 16 (40.0) |
| Low back pain | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 0 (0.0) | 0 (0.0) |
| Neutral | 1 (3.6) | 1 (2.5) |
| Likely/extremely likely | 27 (96.4) | 39 (97.5) |
| Pelvic girdle pain | ||
| n | 27 | 40 |
| Extremely unlikely/unlikely | 10 (37.0) | 0 (0.0) |
| Neutral | 3 (11.1) | 2 (5.0) |
| Likely/extremely likely | 0 (0.0) | 38 (95.0) |
| Anxiety | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 23 (82.1) | 16 (40.0) |
| Neutral | 4 (14.3) | 14 (35.0) |
| Likely/extremely likely | 1 (3.5) | 10 (25.0) |
| Nasal congestion | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 23 (82.1) | 21 (52.5) |
| Neutral | 3 (10.7) | 6 (15.0) |
| Likely/extremely likely | 2 (7.1) | 13 (32.5) |
| Coccydynia/tailbone pain | ||
| n | 28 | 40 |
| Extremely unlikely/unlikely | 8 (28.6) | 2 (5.0) |
| Neutral | 3 (10.7) | 5 (12.5) |
| Likely/extremely likely | 17(60.7) | 33 (82.5) |
| Intra-partum (labor) pain | ||
| n | 27 | 39 |
| Extremely unlikely/unlikely | 24 (88.9) | 19 (48.7) |
| Neutral | 0 (0.0) | 9 (23.1) |
| Likely/extremely likely | 3 (11.1) | 11 (28.2) |
| Hemorrhoids | ||
| n | 28 | 39 |
| Extremely unlikely/unlikely | 26 (92.9) | 29 (74.4 |
| Neutral | 1 (3.6) | 6 (15.4) |
| Likely/extremely likely | 1 (3.6) | 4 (10.3) |
aExcluded n=1 physician with specialty = other.
© 2020 Jordan Faloon et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Journal of Osteopathic Medicine: a refreshed and refocused publication for our profession
- Cardiopulmonary Medicine
- Original Article
- QTc interval prolongation associated with inpatient azithromycin therapy for pneumonia
- General
- Original Article
- Adherence to the RIGHT statement in Society of Interventional Radiology guidelines
- General
- Commentary
- “Somebody who does something other than osteopathy”
- Innovations
- Brief Report
- Robotic microsurgical spermatic cord denervation for chronic orchialgia: a case series
- Medical Education
- Original Article
- Impact of an osteopathic presence in a large categorical pediatric residency training program
- Medical Education
- Clinical Practice
- Transforming a clerkship with telemedicine
- Musculoskeletal Medicine and Pain
- Original Article
- First-time sports-related concussion recovery revisited: management changes and impact on recovery
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment (OMT) use among osteopathic physicians in the United States
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Use of osteopathic manipulative treatment for low back pain patients with and without pain medication history
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment in individuals with vertigo and somatic dysfunction: a randomized, controlled, comparative feasibility study
- Obstetrics and Gynecology
- Original Article
- Characterizing the use of osteopathic manipulative medicine in the obstetric population by trimester and indications for use
- Pediatrics
- Original Article
- Pilot study assessing the effect of osteopathic manipulative treatment (OMT) on length of stay in neonates after therapeutic hypothermia
- Public Health and Primary Care
- Review Article
- Recognizing postoperative nutritional complications of bariatric surgery in the primary care patient: a narrative review
- Public Health and Primary Care
- Brief Report
- Clinical characteristics and lifestyle behaviors among individuals with arthritis: an analysis of 2017 Behavioral Risk Factor Surveillance System data
Articles in the same Issue
- Frontmatter
- Editorial
- Journal of Osteopathic Medicine: a refreshed and refocused publication for our profession
- Cardiopulmonary Medicine
- Original Article
- QTc interval prolongation associated with inpatient azithromycin therapy for pneumonia
- General
- Original Article
- Adherence to the RIGHT statement in Society of Interventional Radiology guidelines
- General
- Commentary
- “Somebody who does something other than osteopathy”
- Innovations
- Brief Report
- Robotic microsurgical spermatic cord denervation for chronic orchialgia: a case series
- Medical Education
- Original Article
- Impact of an osteopathic presence in a large categorical pediatric residency training program
- Medical Education
- Clinical Practice
- Transforming a clerkship with telemedicine
- Musculoskeletal Medicine and Pain
- Original Article
- First-time sports-related concussion recovery revisited: management changes and impact on recovery
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment (OMT) use among osteopathic physicians in the United States
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Use of osteopathic manipulative treatment for low back pain patients with and without pain medication history
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Osteopathic manipulative treatment in individuals with vertigo and somatic dysfunction: a randomized, controlled, comparative feasibility study
- Obstetrics and Gynecology
- Original Article
- Characterizing the use of osteopathic manipulative medicine in the obstetric population by trimester and indications for use
- Pediatrics
- Original Article
- Pilot study assessing the effect of osteopathic manipulative treatment (OMT) on length of stay in neonates after therapeutic hypothermia
- Public Health and Primary Care
- Review Article
- Recognizing postoperative nutritional complications of bariatric surgery in the primary care patient: a narrative review
- Public Health and Primary Care
- Brief Report
- Clinical characteristics and lifestyle behaviors among individuals with arthritis: an analysis of 2017 Behavioral Risk Factor Surveillance System data

