Abstracts DGU
DGU: Innovations in trauma surgery
EASY (Endoscopic Approach to the Symphysis): a new minimally-invasive approach for the plate-osteosynthesis of the symphysis and the anterior pelvic ring - a cadaveric study and a case report
(Abstract ID: 18)
M. Kuper1, A. Trulson1, B. Hirt2, U. Stöckle1, F. Stuby1
1BG Unfallklinik Tübingen
2Institut für Anatomie, Tübingen
Background:
Minimally invasive surgical approaches to reduce approach-associated morbidity are an interdisciplinary goal in surgery. In principle, the endoscopic approach for the extraperitoneal repair of groin hernias is the minimally invasive variant of the modified Stoppa-approach, which is used for the treatment of pelvic ring injuries in traumatology.
Materials and methods:
Anatomical feasibility study regarding the plate osteosynthesis of the anterior pelvic ring via a minimally invasive variant of the modified Stoppa-approach.
Results:
In a human cadaver, who donated himself for scientific and educational purposes, we present the minimally invasive variant of the modified Stoppa-approach step by step, both photographically and radiologically. Feasibility of the plate osteosynthesis of the symphysis is presented in a patient with open book injury via the minimally invasive approach using standard laparoscopic instruments.
Conclusion:
The plate osteosynthesis of the anterior pelvic ring via the minimally invasive variant of the modified Stoppa-approach is feasible with existing standard laparoscopic instruments.
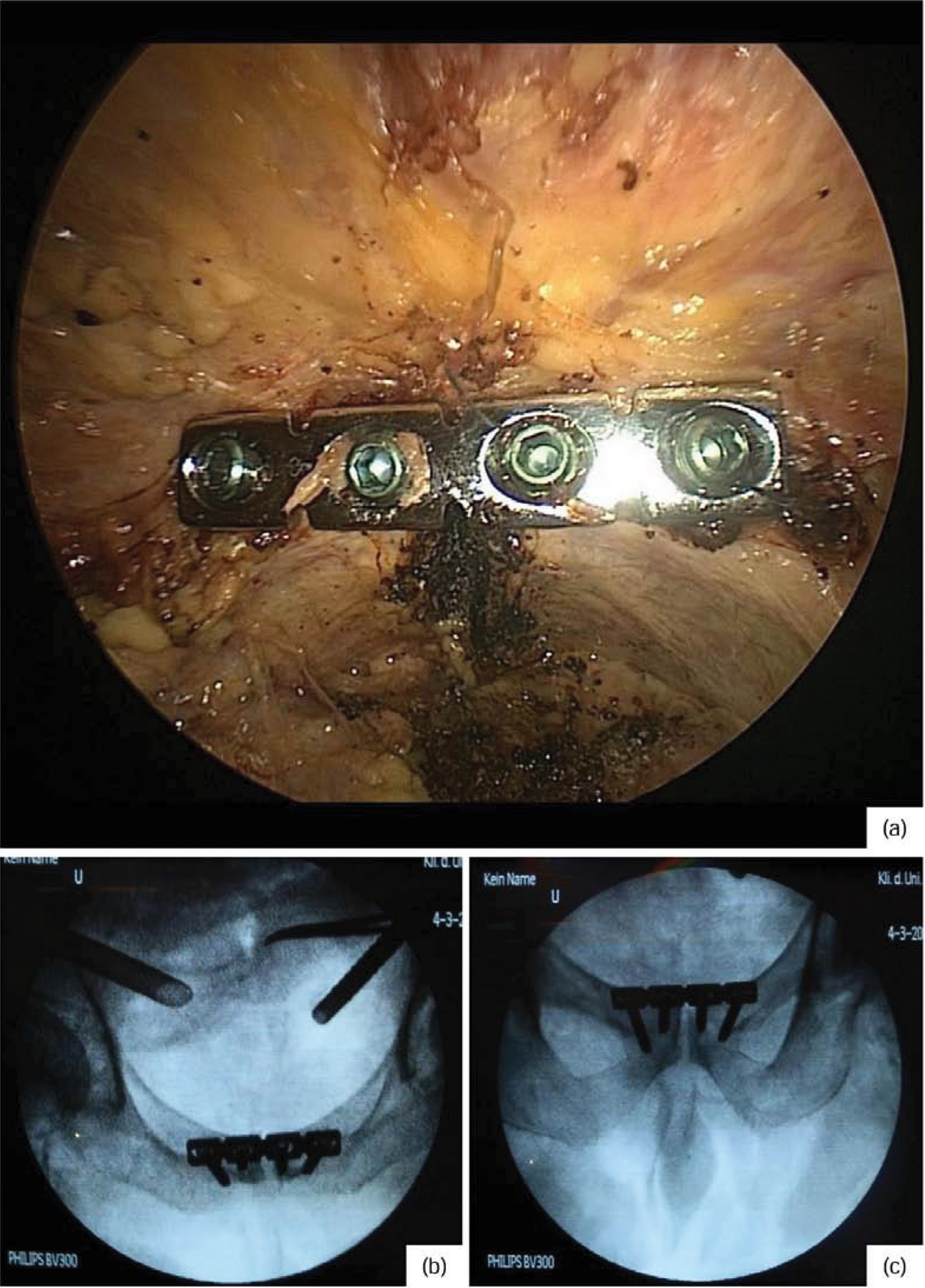
Final documentation with endoscopic view of the plate (a), as well as radiological control of the plate position in 2 levels (inlet / outlet recording, b and c)
Completely endoscopic plate osteosynthesis of the acetabulum - an anatomical feasibility study
(Abstract ID: 890)
M. Küper1, A. Trulson1, C. Minarski1, L. Grünwald1, U. Stöckle1, F. Stuby1
1BG Unfallklinik Tübingen
Background:
Minimally invasive surgical approaches to reduce approach-associated morbidity are an interdisciplinary goal in surgery. Recently, we presented a completely endoscopic plate osteosynthesis of the symphysis on a patient with a bilateral open-book-injury of the pelvis. Aim of this anatomical feasibility study was to extend the EASY-approach (Endoscopic Approach to the Symphysis) to the plate osteosynthesis of acetabular fractures.
Materials and methods:
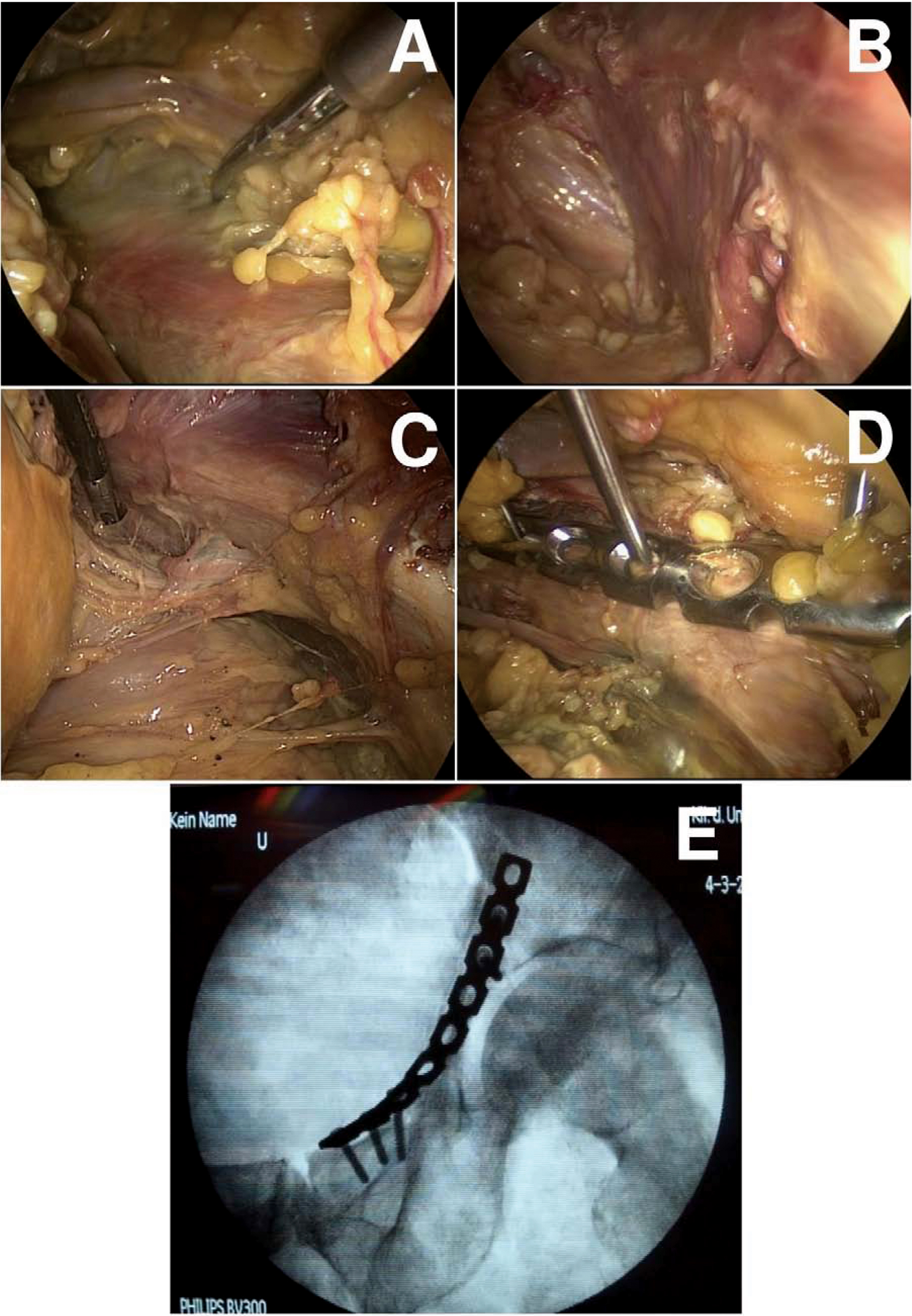
In 4 human cadavers, who donated themselves for scientific and educational purposes, we established the completely endoscopic preparation and visualization of all relevant structures of the complete pelvic ring from the symphysis to the iliosacral joint including the quadrilateral face and the greater sciatic notch with the sciatic nerve. Then, a plate osteosynthesis of the acetabulum along the iliopectineal line was done with standard laparoscopic instruments.
Results:
The visualization of the relevant anatomical structures for surgery of the acetabulum (iliac and femoral vessels, femoral nerve, obturator vessels, quadrilateral face, pelvic brim with the iliopectineal line until the iliosacral joint and the greater sciatic notch with the sciatic nerve; Fig A-C) as well as the completely endoscopic plate osteosynthesis along the iliopectineal line (Fig. D+E) can be done with standard laparoscopic instruments using 3 up to 10mm wide skin incisions.
Conclusion:
The endoscopic visualization of the relevant anatomical structures is well possible. The plate osteosynthesis of the acetabulum itself requires an extracorporal forming of the plate using an anatomical specimen. The creation of such a specimen could be done using 3D-printing of 3D-data acquired out of CT-scans. Before introducing this endoscopic technique into a clinical setting, the question of reducing acetabular fractures is under investigation in anatomical and biomechanic studies.
DGU: Classic osteosynthesis procedures
Novel technique for posterior C1-C2 fixation
(Abstract ID: 406)
A. Harati1
1Klinikum Dortmund
Background:
Several techniques for treating atlantoaxial instability have been described. The most accepted treatment modalities are the Magerl transarticular screw fixation and the Harms/Goel C1-C2 rod technique. Based on these established posterior atlantoaxial fixation techniques, we present a novel technique that uses a polyaxial screw rod system and utilizes a combination of C1 lateral mass and C1-C2 transarticular screws.
Materials and methods:
Retrospective review of seven men and five women (mean age: 63, range: 20-86). Indication for surgery was type II odontoid fractures (n = 6), pseudarthrosis after anterior odontoid screw placement (n = 3), atlantoxial instability after C3-C5 fusion (n = 1), Os odontoideum (n=1) and craniovertebral rheumatoid arthritis (n = 1).
Results:
The mean follow-up time was 22 months (range: 3-72). There were no intraoperative complications. Postoperative imaging showed no screw malposition. During follow-up no patient had screw loosening, screw fracture, or bone absorption around the screws. Clinically, patient neck pain improved in all cases.
| No. | Age | Sex | Diagnosis | Presentation | Surgery | Outcome/Complications |
| 1 | 56 | M | Dislocated Odontoid fracture | Acute trauma and neck pain | C1-C2 fusion | Resolution of neck pain |
| 2 | 56 | M | Dislocated Odontoid fracture | Acute trauma and neck pain | C1-C2 fusion | Resolution of neck pain |
| 3 | 63 | M | Atlantoaxial instability and Myelopathy after prior C3-C5 fusion | Neck pain and progressive myelopathy with quadriparesis | Laminectomy C2-C7 and posterior fusion C1-Th1 | Superficial infection, revision surgery Improvement of myelopathy |
| 4 | 68 | F | Pseudarthrosis after anterior odontoid screw placement | Failed prior fusion and neck pain | C1-C2 fusion | Resolution of neck pain |
| 5 | 60 | F | Atlantoaxial instability in Rheumatoid arthritis | Neck pain | C1-C2 fusion | Resolution of neck pain |
| 6 | 34 | M | Odontoid fracture and C1 anterior and posterior arch fracture | Acute trauma with severe head injury and multiple fractures | C1-C2 fusion | Resolution of neck pain |
| 7 | 20 | M | Os odontoideum | Neck pain, Transient tetraplegia | C1-C2 fusion | Resolution of neck pain |
| 8 | 86 | F | Dislocated Odontoid fracture | Acute trauma and neck pain | C1-C2 fusion | Resolution of neck pain |
| 9 | 82 | F | Dislocated Odontoid fracture | Acute trauma and neck pain | C1-C4 fusion | Resolution of neck pain |
| 10 | 67 | M | Dislocated Odontoid fracture | Acute trauma and neck pain | C1-C2 fusion | Resolution of neck pain |
| 11 | 81 | F | Pseudarthrosis after anterior odontoid screw placement | Failed prior fusion and neck pain | C1-C4 fusion | Resolution of neck pain |
| 12 | 73 | M | Pseudarthrosis after anterior odontoid screw placement | Failed prior fusion and neck pain | C1-C4 fusion | Resolution of neck pain |
Conclusion:
C1 lateral mass and C1-C2 transarticular polyaxial screw rod fixation is a novel and potentially effective surgical technique for achieving immediate rigid immobilization of the C1-C2 motion segment.
One shape fits all? A study concerning the contour accuracy of anatomically preformed, fixed-angle clavicle plates
(Abstract ID: 35)
D. Sauter1, M. Doppelbauer1, M. Schüler1
1Kantonsspital Münsterlingen
Background:
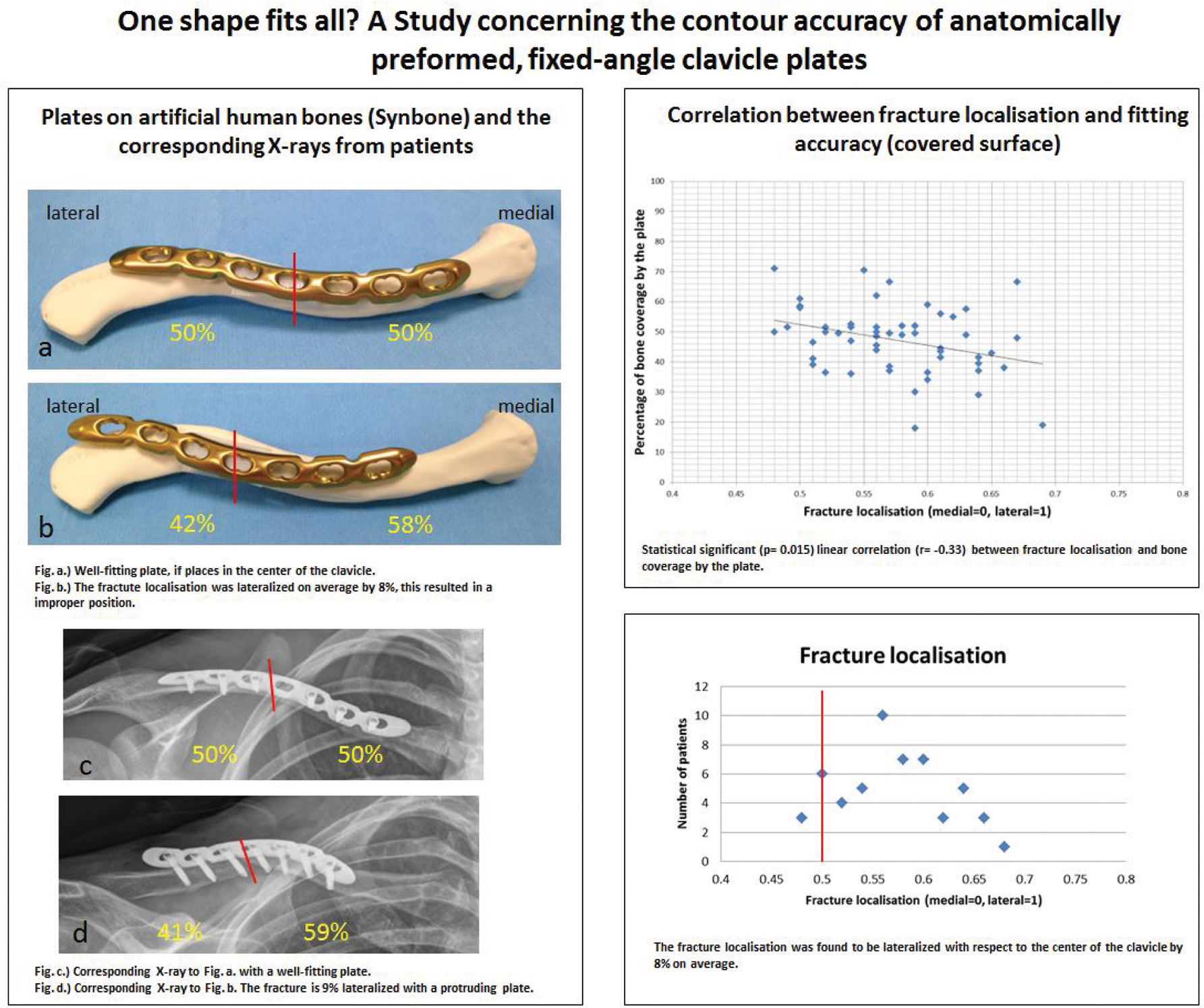
Clavicular fractures account for 2.6-4% (Kihlström et al.) of all fractures, with the middle third being affected the most frequently (69-80%). Over the past few years, there has been an increased trend towards to ORIF treatment. In Sweden alone, the operation rate increased by 705% between 2001 and 2012. Not least, through the use of new, anatomically preformed, fixed-angle implants. It has been possible to improve the performance of the plates with regard to implant failure, however its anatomical contour and accuracy of its fit have been criticised in several publications (Malhas et al.).
Materials and methods:
In the context of a retrospective study, we examined the plate position by means of postoperative X-rays. Between 2015 and 2016 we analyzed 54 patients (45male, 9female) who were treated with an anterior-superior LCP clavicle plate from Synthes. Both the fracture localisation as well as the fitting accuracy (in terms of surface area with respect to the clavicle contour) were measured in the conventional X-ray image. We radiologically validated our measuring methods beforehand using original plates on SYNBONE bones.
Results:
31 8-hole and 23 7-hole LCP clavicle plates were implanted. The fracture localisation was found to be lateralized with respect to the middle of the clavicle by 8% on average (-2% to +19%). Without exception, the plates themselves were applied centrally with respect to the fracture. Correspondingly, this resulted in a consecutive lateralisation of the plate. By means of linear regression (correlation coefficient r = -0.33) and/or an ANOVA test (p= 0.015), we were able to show in a statistically significant way that the more laterally the plate was applied, the less surface coverage of the bone (by the plate) there was. This was the case, even though a plate modification was performed intraoperatively by the surgeons in 91% of all cases.
Conclusion:
Although the anatomically preformed clavicle plates display good material properties, considerable trade-offs have to be accepted with regard to the fit and scope for modification. Last but not least, whereas the examined plate only fits well when placed in the centre of the clavicle - in our examination, almost all of the fractures occurred laterally to the centre line. These data are consistent with our clinical observations of aggravating implants in soft tissue.
DGU: Spine and plevic injuries
Venous paravasation after augmentation of pedicle screws - a underestimated risk
(Abstract ID: 53)
A. Prokop1
1Kliniken Sindelfingen
Background:
Cement-augmented pedicle screws can increase the stability of fixators for unstable vertebral fractures in the elderly. Fixators can be inserted quickly and with minimally-invasive techniques, reducing surgical risks.
Materials and methods:
From March 2012 until July 2014, we treated 40 patients with percutaneous augmented fixators for unstable vertebral fractures. Average age was 77.5 years.
Results:
During the six month observation period, no patients died. There were no neurological deficits. On VAS, average pain decreased from 8.5 to 4.1 points postoperativly. The average Cobb angle of 4.1° was improved after surgery. After 6 months, bony consolidation yielded angles of 1 to 4°, average 2.6°. In 42,5% we saw venous extravasation of cement leaking from the augmented vertebrae, even to pulmonary embolism. The emboli were usually asymptomatic.
Only in one case we saw severe reactions.
We report a case where the patient required resuscitation immediately after cement application because of pulmonary emboli. The patient survived because of the immediately-implemented critical care measures.
Conclusion:
The risk is little known in the literature, and as yet underestimated despite increasing numbers of augmented fixator operations. Reduction of risk is possible with slower cement injection, smaller cement applicators, and short term positive pressure ventilation with PEEP.
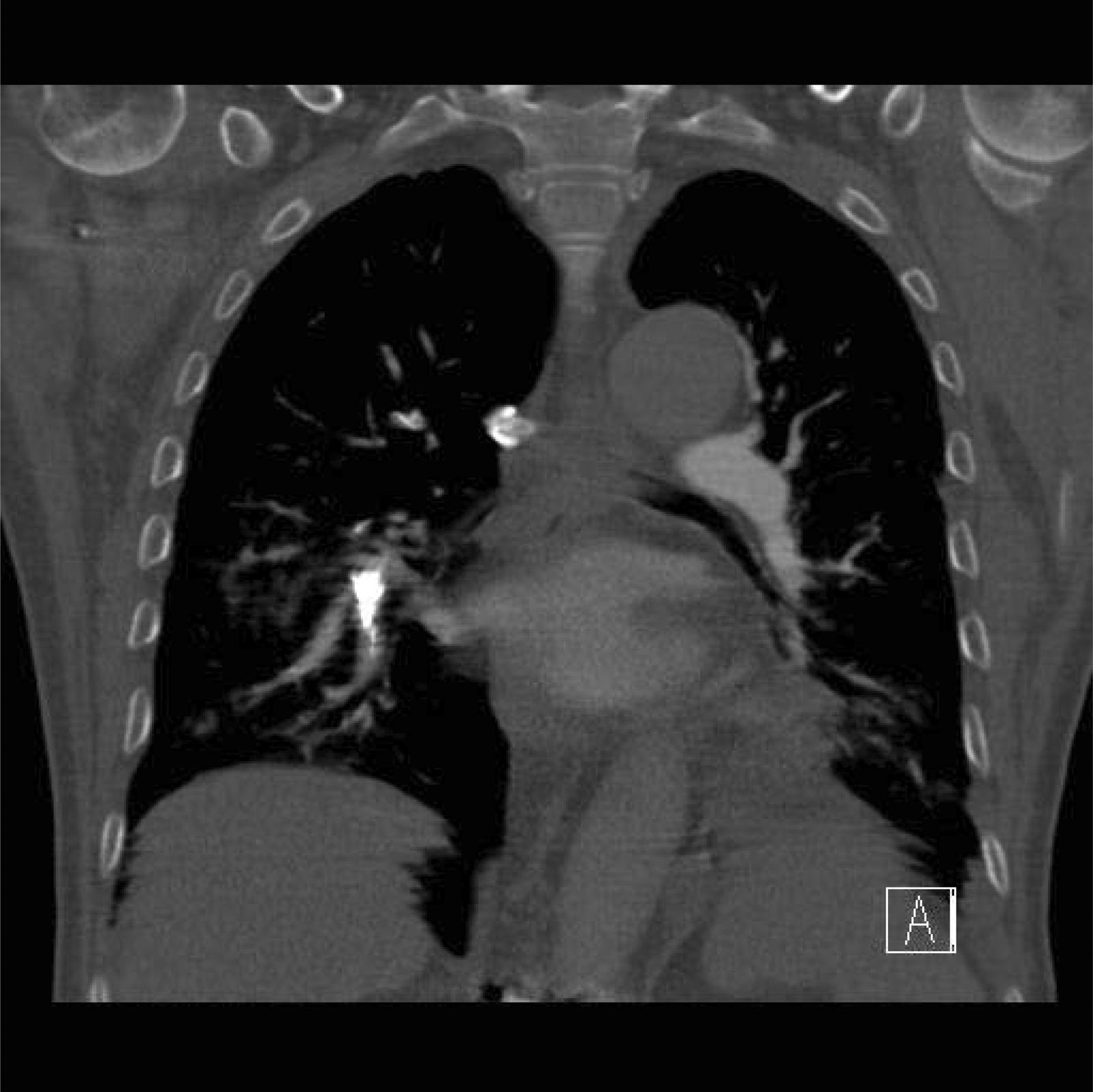
Lung embolism
Stratified treatment protocol: Dens fractures
(Abstract ID: 365)
A. Kanovsky1, E. Mueller1
1KABEG Klinikum Klagenfurt
Background:
Based on the literature and on our own experience we established a treatment protocol for dens fractures. We carried out a retrospective study to correlate between our treatment algorithm based on initial displacement and angulation of the odontoid and fracture gap, and the observed treatment outcome.
Materials and methods:
There were 152 patients who presented at our institution from 2003 until 2017 (70 male, 82 female patients; age range: 19-99 yrs.; mean: 71 yrs). We retrospectively categorized each patient with radiographs and CT-scans to evaluate the type of fracture according to the Anderson-D´Alonzo classification system, fracture gap (mm), fracture angulation (degrees), fracture displacement (mm), fracture displacement direction (anterior, posterior). The fractures were stratified as stable (displacement <5mm, angulation <11°, fracture gap < 2mm) or unstable. Stable fractures were treated with a non-rigid immobilization. Unstable fractures were treated surgically. In patients >75 yrs. we preferred a posterior transarticular C1-C2 fixation, in younger patients a direct anterior screw fixation was the method of choice if suitable. Follow up time: 1 month-11 years.
Results:
We encountered 89 patients with a stable (1 Type I, 40 Type II, 48 Type III fractures) and 63 patients with an unstable fracture (32 Type II, 31 Type III fractures). For stable fractures the average fracture gap was 0.7mm, the dens angulation 11° and the fracture displacement 1.8mm. All stable fractures underwent conservative treatment with a cervical collar. The observed non-union rate was 18% (16/89 patients; 10 Type II, 6 Type III fractures) of which 3 patients with a type III fracture underwent a secondary posterior transarticular fixation. The other 13 patients had either stable nonunions (n=9), or could not undergo a surgical intervention due to preliminary health conditions. Surgical intervention was performed in 63 unstable fractures (32 Type II, 31 Type III fractures) with an average fracture gap of 1.1 mm, dens angulation of 20° and fracture displacement of 5.1mm. A posterior C1-C2 fusion was carried out in 44 patients (26 male, 18 female; mean age 71; dens angulation 22°; fracture displacement 5.2mm). Three patients were treated by a C0 onto C4 stabilization (3 females, mean age 86; dens angulation 25°; fracture displacement 8.2mm). An anterior odontoid screw fixation was performed in 14 patients (11male, 3 female; mean age 62; dens angulation 14°; fracture displacement 4.6mm). For direct anterior screw fixation there were 3 non-unions, which were revised, for posterior C1/2 fixation the union rate was 100%. 12 patients (7.9%) died within 4 weeks after injury (7 non-operative, 5 operative).
Conclusion:
Our stratified treatment protocol is associated with a high success rate. The need for surgical intervention is a ventral or dorsal fracture dislocation >4.5mm with a dens fracture angulation of >11 degrees, as has been published previously. Non-rigid immobilization was appropriate for stable fractures with a low rate of non-union. Posterior transarticular fixation is highly successful with a low complication rate. Direct anterior screw fixation is associated with a high rate of non-union.
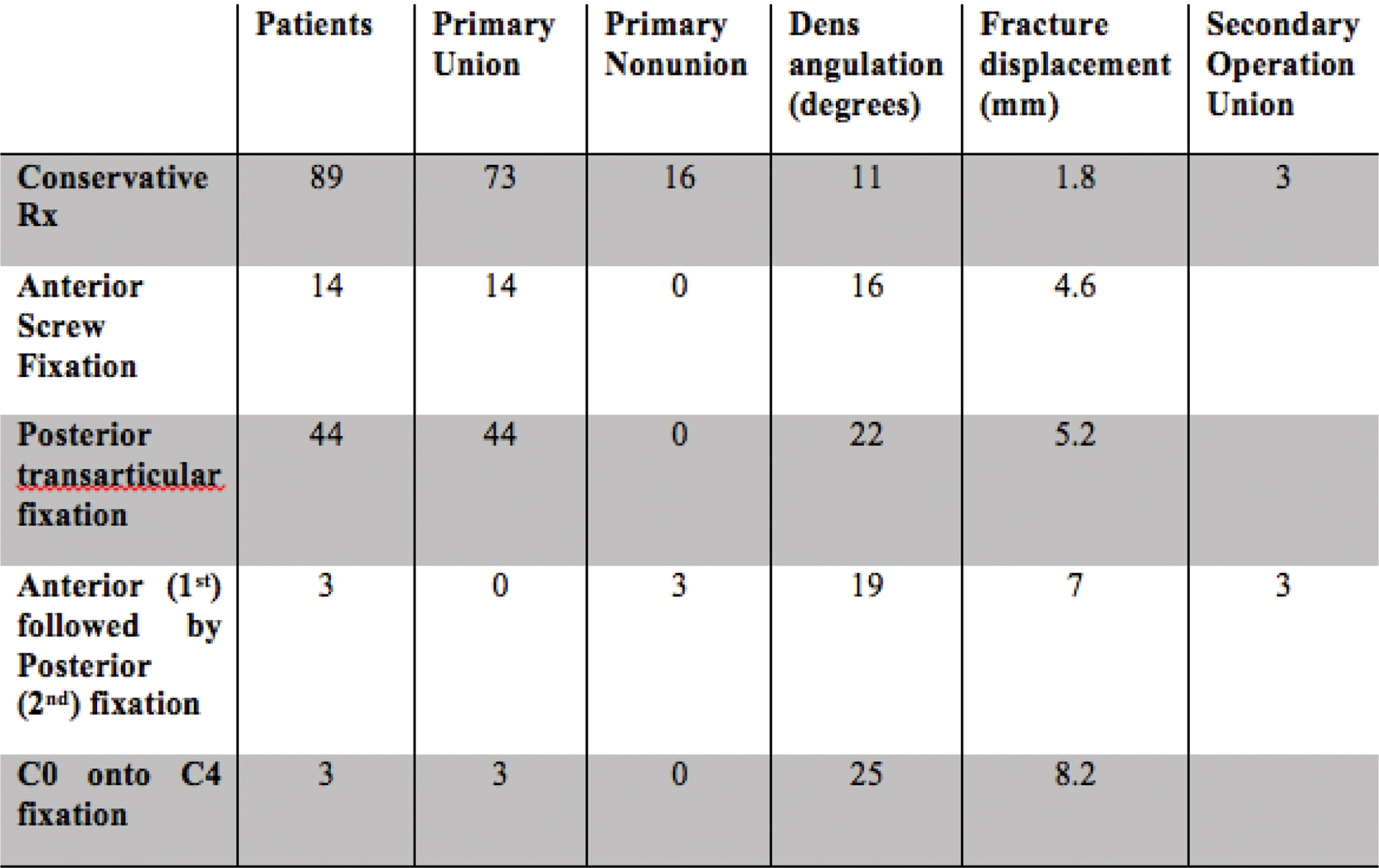
Summarized Dens Fracture Treatment algorythm results
DGU: Pediatric traumatology
Management of Distal Forearm Fractures in Children - Retrospective analysis of 265 Fractures reported to the Public Accident Insurance in Saxony
(Abstract ID: 210)
M. Lorenz1, J. Schultz1, P. Schwerk1, G. Fitze1
1Universitätsklinikum Dresden
Background:
Distal forearm fractures are the most common fractures during infancy and childhood. Incidence rates peak around puberty. Due to the lack of standardized treatment protocols, pediatric surgeons and orthopedic surgeons develop different concepts to handle these fractures.
The primary objective of this study is to elicit how pediatric distal forearm fractures are treated in Saxony. We also wanted to assess the clinical outcomes of different treatment modalities.
Materials and methods:
Retrospectively, we analyzed all distal forearm fractures reported to the public accident insurance “Unfallkasse Sachsen”. We included all children 15 years or younger injured in 2012 and 2013. Initial and final values for angulation and displacement were collected; cast types, methods of operation, complication rates; complaints at the time of injury and after finishing the treatment were also recorded among various other variables.
Results:
265 children were included in our analysis. The mean age was 10.2years. 29 percent (n=78) of the distal forearm fractures were metaphyseal buckle fractures. The initial treatment mostly happened in hospitals in bigger cities. Of all fractures but buckle fractures (n=187), 38% (n=71) were treated operatively. Of these patients, 57 were initially treated operatively. This was mostly due to dislocated complete metaphyseal fractures (n=30) and Aitken I fractures (n=25) while another 14 patients were operated after conservative management had failed. 82 percent of the operated children were treated with Kirschner-wires. After finishing the treatment, only 7% of the conservatively treated patients complained about functional limitations in contrast to 17% of the operated patients. Complications were reported in 22 cases, mainly due to redislocations. However, the complication rates did not differ greatly in between primarily operatively treated patients (6 out of 57) and primarily conservatively treated patients (16 out of 194). The highest complication rates were seen in primarily conservatively treated greenstick fractures (5 out of 22).
Conclusion:
We conclude that distal forearm fractures in children are mostly treated conservatively. Clinical outcomes differ according to the treatment method chosen.
Case Report: A 6-year-old boy in Ghana with extensive crush injury of the lower extremities
(Abstract ID: 404)
V. Ativor1, N. Koenemann2, E. Adu1, M. Amoah1, J. Adabie-Appiah1, M. Richter-Turtur3, D. Hartmann3
1Komfo Anokye Teaching Hospital, Kumasi
2Universitätsklinikum der LMU München
3Klinikum rechts der Isar München
Background:
A 6-year-old boy presented to the Accident & Emergency Department of Komfo Anokye Teaching Hospital (KATH) Kumasi, Ghana with hemorrhagic shock and severe crush injury of both lower extremities following a roll-over accident by a motor vehicle while crossing a highway.
Materials and methods:
Initial therapy included aggressive resuscitation with IV fluids and hemotransfusion. He was quickly brought to the OR for assessment of injury extent: 1.) Severe crush injury of both lower limbs with gross soft tissue injuries beyond limb salvage. 2) Huge degloving injury extending from the lower half of the back to the perineum, sparing skin of scrotum and penis. Disarticulation at the left hip joint level of the left lower limb and a trans-femur amputation of the right lower limb were performed as well as a debridement of the degloving injury of the back. The patient was treated in the Clinical Decision Unit for 16 days due to unavailable vacancy in the pediatric ICU (PICU). During this time, he developed sepsis, wound infections, and an infection of the anal region, for which surgical re-debridement and colostomy were done together with pediatric surgeons. He was then transferred to the PICU for acute wound care, management of colostomy, control of E. coli sepsis and anemia. Nine weeks after his initial presentation, split-thickness skin grafting (STSG) using skin from his arms was performed in collaboration of trauma and plastics surgeons of KATH.
Results:
First review of STSG post-surgery showed a good response and no signs of graft rejection or infection. 14 days later he showed 85% STSG take, all the donor sites of the skin graft including both arms and both fore arms showed healing without complications. A colostomy reversal was performed about four months after the initial procedure. Due to multiple wounds around the perineum and the anal region, he developed anal canal stenosis. Repetitive dilation treatments over the course of three weeks were performed with sufficient results. The patient started to mobilize using a mini wheel chair and was transferred to the pediatric surgical ward where he integrated well with other children. He remained in good spirits and was discharged 4 ½ months after the initial accident.
Conclusion:
Long term graft survival will determine management success. The future therapy strategy will include rehabilitation to ensure mobility under the current circumstances and the provision of an adequate wheel chair, perhaps even a form of sustainable prosthesis.
The patient and his family will continue to face several socio-economic and cultural challenges (family burden, cost of medical equipment and medication, hospital bills, rehabilitation, social integration).
The survival of this child is the result of effective interdisciplinary teamwork. Furthermore, it demonstrates success and challenges of trauma care under the socio-economic conditions of a lower middle-income country.

Initial Presentation on arrival at KATH, Copyright V. Ativor
© The Author(s) 2018, published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 License.
Articles in the same Issue
- Abstracts DGAV
- Abstracts DGCH
- Abstracts DGG
- Abstracts DGKCH
- Abstracts DGMKG
- Abstracts DGNC
- Abstracts DGPRÄC
- Abstracts DGT
- Abstracts DGTHG
- Abstracts DGU
Articles in the same Issue
- Abstracts DGAV
- Abstracts DGCH
- Abstracts DGG
- Abstracts DGKCH
- Abstracts DGMKG
- Abstracts DGNC
- Abstracts DGPRÄC
- Abstracts DGT
- Abstracts DGTHG
- Abstracts DGU

