Abstract
Background
Remote extracorporeal life support (ECLS) implantation and mobile ECLS are increasingly applied to enable the treatment of patients with refractory heart failure at specialized care centers. Giant left atrium (GLA) is a rare cause but may lead to acute and devastating heart failure.
Case report
Acute heart failure that gave rise to a prolonged period of out-of-hospital cardiopulmonary resuscitation in a patient who underwent remote ECLS implantation was found to have resulted from a GLA of impressive dimensions. There having no reasonable option for immediate surgical therapy, the patient was successfully bridged to recovery with a view to subsequent heart transplantation.
Conclusions
The threshold to rapid institution of ECLS should be low in patients with acute refractory heart failure, including those with uncommon pathologies. Remote ECLS implantation and interhospital transfer on mobile ECLS increase the chances of survival in cases requiring treatment by specialized care centers.
1 Introduction
Giant left atrium (GLA) is commonly defined as a left atrium with a diameter of ≥65 mm and found most frequently as a result of mitral valve disease. The condition may be asymptomatic or manifest itself by different symptoms, including atrial fibrillation, thrombus formation, and heart failure [1], [2].
Surgical therapy aims at reducing the size of GLA and relies on a variety of techniques for plicating or resecting parts of the left atrium [1]. Due to the difficulty of exposing a heart with a left atrium of excessive dimensions, the surgical therapy of GLA was variously reported to have required (partial) autotransplantation [3], [4].
With regard to extracorporeal life support (ECLS), there is wide agreement not only on its use in patients with severe heart failure refractory to conventional therapy but also that it should be instituted before the onset of multiorgan failure [5]. In patients with acute refractory heart failure or after cardiopulmonary resuscitation (CPR) in whom diagnosis and/or neurological status are not clear or the further course of therapy is yet to be determined, ECLS may serve as a bridge to decision. Over the past decade, remote ECLS implantation and interhospital transfer on mobile ECLS have come to play an increasing role [6].
2 Case report
A 57-year-old male with acute heart failure was admitted to a community hospital after return of spontaneous circulation (ROSC) following cardiac arrest and approximately 65 min of out-of-hospital CPR. Although his cardiac rhythm at the time of ROSC was not documented, he was in atrial fibrillation upon arrival at the community hospital. It turned out that he had undergone redo mitral valve replacement with a mechanical valve and tricuspid valve repair 5 years preceding the event. Nearly two decades earlier, he had undergone mitral valve replacement for mitral regurgitation in the setting of cardiomegaly. Echocardiography (ECG) and computed tomography (CT) showed a grotesque case of GLA (Figures 1 and 2 ) that had gone undiagnosed because the patient had not presented for follow-up examinations after the most recent surgical procedure (i.e. for 5 years). ECG findings included sludge in GLA and a left ventricular ejection fraction of 10%. Fluoroscopy showed a normal motion of mitral valve leaflets.

Transversal section of GLA on initial CT after cardiac arrest and CPR (dimensions: 240×176 mm).
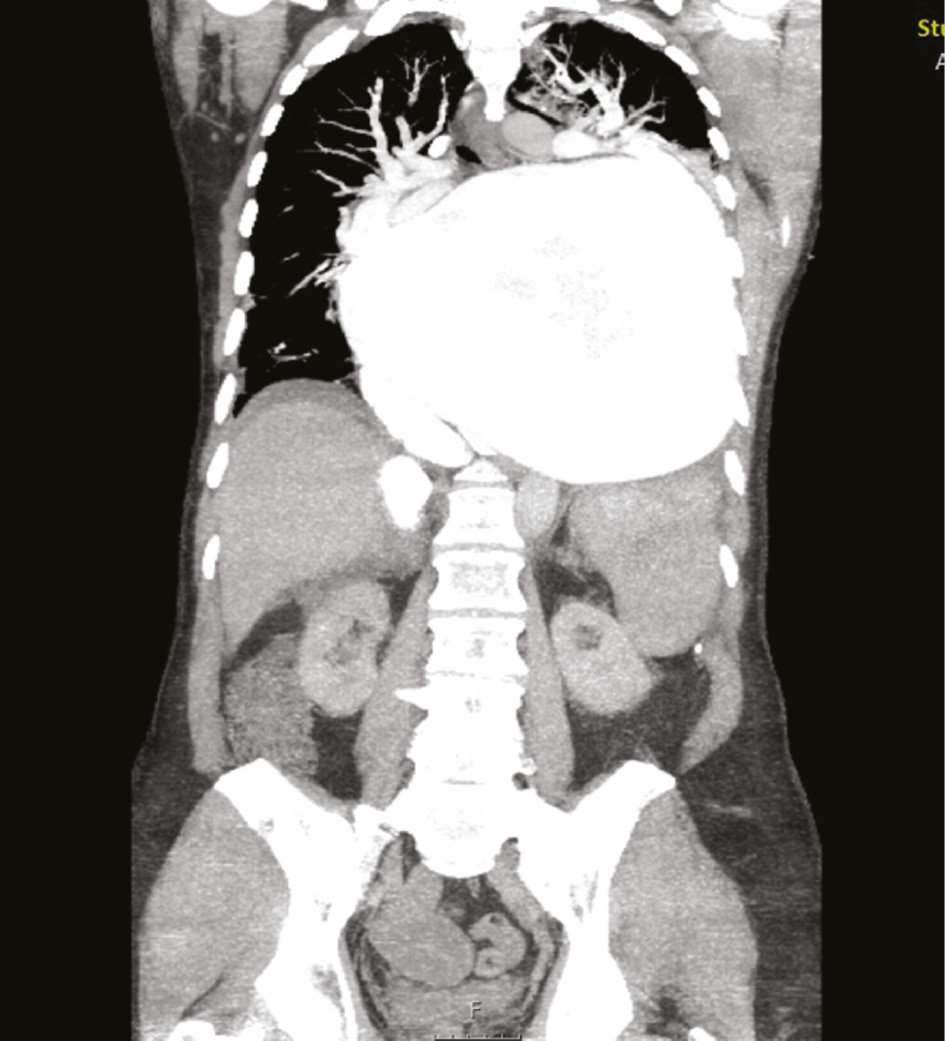
Frontal section of GLA on initial CT.
When the patient remained in severe cardiogenic shock, our mobile ECLS team was called for ECLS implantation and subsequent air transport to enable further treatment at our tertiary care center. The inflow and outflow for the ECLS system (Stöckert Centrifugal Pump and Centrifugal Pump Console) were instituted by percutaneous placement of a 17 Fr NovaPort cannula in the left femoral artery and a 21 Fr Biomedicus cannula in the left femoral vein.
Both ECLS implantation and interhospital transfer were implemented without complications. In the further course, preventing thromboembolic complications while at the same time controlling an increasingly dramatic hemorrhagic tendency turned out to be a challenge. ECG showed spontaneous contrast/sludge in the left atrium (Figure 3), although the patient’s initial international normalized ratio (INR) of 3.3 was accompanied by moderate thrombocytopenia and his partial thromboplastin time (PTT) was 50.2 s after receiving 2000 IU unfractionated heparin for ECLS implantation. Over the next 2 days, his INR climbed to 8.9 and extensive spontaneous oropharyngeal, pulmonary, and gastrointestinal bleeding required transfusion of several units of packed red blood cells and moderate correction of his coagulation status.
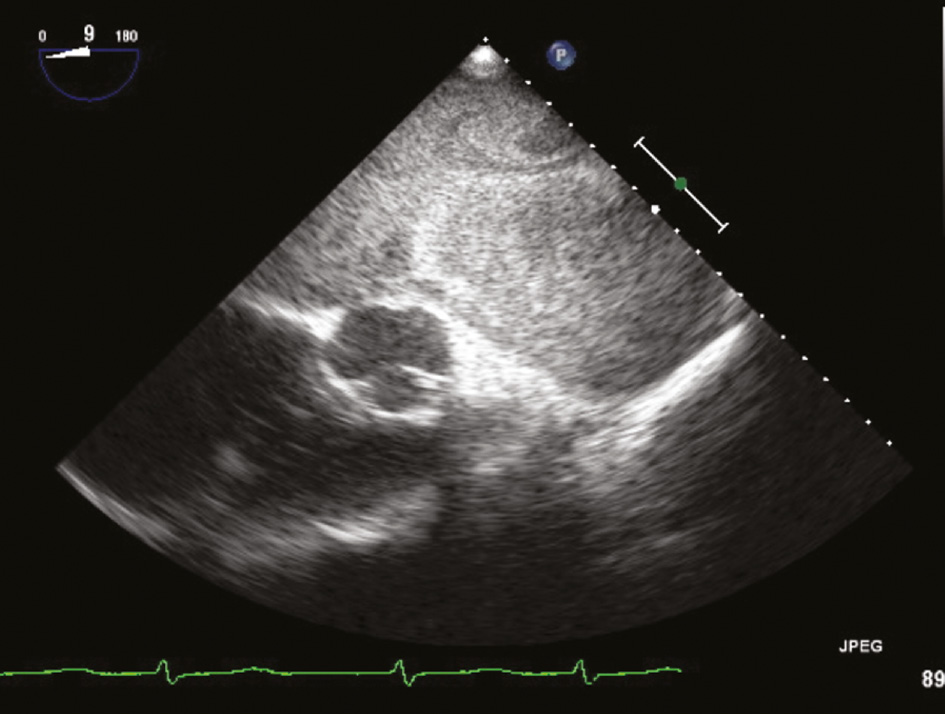
ECG view of GLA with spontaneous contrast/sludge.
Starting at 2800 rpm, the ECLS system provided sufficient blood flow (of ~4 L) to keep up adequate perfusion. Sedation was terminated and the patient was weaned from catecholamines within 48 h while his renal and hepatic functions simultaneously recovered. He woke up and turned out to be responsive though slightly delirious.
Surgical options were evaluated but appeared little promising due to the very size of GLA and the patient’s risk constellation. Therefore, it was resolved to wean him from ECLS and retransfer him to the community hospital for further recovery and subsequent evaluation for heart transplantation. The ECLS system was kept at about 2800 rpm for about 24 h and at 1900–2200 for another period of about 24 h. Then, the pump speed was reduced to 1500 rpm (1.3 L) before the ECLS system was finally removed a few hours later.
Early mobilization was initiated and mechanical respiration was terminated as soon as oropharyngeal and pulmonary bleeding were under control. Intravenous (i.v.) heparin was continued to prevent thrombus formation within GLA, and after a total intensive care unit stay of 6 days, the patient was retransferred and arrived in stable condition at the community hospital. At the time of retransfer, he was on i.v. unfractionated heparin (PTT 59.9 s) and had an INR of 1.7.
Follow-up for the present case report revealed that he had taken a fatal course due to mesenteric ischemia suspected to have been caused by thromboembolism from GLA within a few days from arriving at the community hospital.
3 Discussion
The relevance of heart failure in patients with GLA was demonstrated by Kim et al. [2], who followed a cohort of 163 patients up for a median of 22 months. Eighteen (11%) patients were admitted to hospital due to heart failure, and the fact that nearly 30% of those hospitalized for heart failure in this series took a fatal course is in keeping with the devastating character of the condition we observed in our patient.
Mortality is moreover known to be extremely high in patients who sustained out-of-hospital cardiac arrest. Survival-to-discharge after adult out-of-hospital cardiac arrest in Europe was found to be as low as 9% by a review of 67 prospective studies [7], whereas register data from the United States suggested a survival of 8.3% for the year 2012 [8]. Given the low probability of surviving out-of-hospital cardiac arrest and the severity of our patient’s underlying pathology, we conclude that an early institution of ECLS made a relevant contribution to his initial survival and recovery.
Simultaneously, our case illustrates the advantages of remote ECLS implantation and interhospital transfer on mobile ECLS. The benefits of pretransfer institution of and transport on ECLS we saw in our patient are in keeping with an increasing number of reports on interhospital transfer on ECLS, suggesting favorable results and demonstrating that pretransfer ECLS implantation enables an immediate improvement of cardiorespiratory parameters, prevents delays in hemodynamic stabilization, and increases transport safety [9], [10], [11].
The fact that our patient’s neurological status was unclear and, in combination with his extremely unfavorable cardiac anatomy and high-risk profile, required careful evaluation of surgical therapy options addressing GLA on the one hand and candidacy for heart transplantation on the other illustrates the notion of ECLS as a bridge to decision. The ECLS thus served not only to achieve hemodynamic stability but also to gain time to evaluate neurological recovery, investigate medical issues and therapy options, and obtain information on questions such as social support and patient consent to further therapies.
4 Conclusion
In summary, the fast recovery our patient made on ECLS leads us to conclude that the threshold to rapid institution of mechanical circulatory support should be low in patients with acute refractory heart failure, including those with unusual and rare pathologies. We conclude that ECLS weaning should be attempted and that surgical therapy options including heart transplantation should be carefully evaluated. Sufficient anticoagulation is mandatory. The fact that follow-up revealed subsequent death from thromboembolic complications highlights the danger of thromboembolism inevitably associated with GLA.
Author Statement
Funding: Authors state no funding involved. Conflict of interest: Authors state no conflict of interest. Informed consent: Informed consent has been obtained from the individual‘s relatives.
Author Contributions
Andres Beiras-Fernandez: Conceptualization; Formal analysis; Supervision; Validation; Writing – review & editing; Hazem El Beyrouti: Conceptualization; Data curation; Formal analysis; Methodology; Supervision; Martin Oberhoffer: Conceptualization; Data curation; Supervision; Writing – review & editing; Angela Kornberger: Supervision; Validation; Writing – original draft; Christian-Friedrich Vahl: Conceptualization; Validation; Writing – review & editing.
Publication Funding
The German Society of Surgery funded the article processing charges of this article.
References
[1] Apostolakis E, Shuhaiber JH. The surgical management of giant left atrium. Eur J Cardiothorac Surg 2008;33:182–90.10.1016/j.ejcts.2007.11.003Search in Google Scholar PubMed
[2] Kim H, Park YA, Choi SM, Chung H, Kim JY, Min PK, et al. Associates and prognosis of giant left atrium; single center experience. J Cardiovasc Ultrasound 2017;25:84–90.10.4250/jcu.2017.25.3.84Search in Google Scholar PubMed PubMed Central
[3] Pan J, Li QG, Li J, Wang DJ. Partial cardiac autotransplantation with a concomitant mitral valve, aortic valve replacement and tricuspid plasty. Interact Cardiovasc Thorac Surg 2013;17:906–7.10.1093/icvts/ivt287Search in Google Scholar PubMed PubMed Central
[4] Lessana A, Scorsin M, Scheublé C, Raffoul R, Rescigno G. Effective reduction of a giant left atrium by partial autotransplantation. Ann Thorac Surg 1999;67:1164–5.10.1016/S0003-4975(99)00122-8Search in Google Scholar PubMed
[5] Beckmann A, Benk C, Beyersdorf F, Haimerl G, Merkle F, Mestres C, et al. Position article for the use of extracorporeal life support in adult patients. Eur J Cardiothorac Surg 2011;40:676–81.10.1016/j.ejcts.2011.05.011Search in Google Scholar PubMed
[6] Guenther SP, Buchholz S, Born F, Brunner S, Schramm R, Hoechter DJ, et al. Remote ECLS-implantation and transport for retrieval of cardiogenic shock patients. Air Med J 2017;36:320–6.10.1016/j.amj.2017.06.007Search in Google Scholar PubMed
[7] Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010;81:1479–87.10.1016/j.resuscitation.2010.08.006Search in Google Scholar PubMed
[8] Chan PS, McNally B, Tang F, Kellermann A; CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation 2014;130:1876–82.10.1161/CIRCULATIONAHA.114.009711Search in Google Scholar PubMed PubMed Central
[9] Schopka S, Philipp A, Hilker M, Müller T, Zimmermann M, Arlt M, et al. Clinical course and long-term outcome following venoarterial extracorporeal life support-facilitated interhospital transfer of patients with circulatory failure. Resuscitation 2015;93:53–7.10.1016/j.resuscitation.2015.05.021Search in Google Scholar PubMed
[10] Javidfar J, Brodie D, Takayama H, Mongero L, Zwischenberger J, Sonett J, et al. Safe transport of critically ill adult patients on extracorporeal membrane oxygenation support to a regional extracorporeal membrane oxygenation center. ASAIO J 20122;57:421–5.10.1097/MAT.0b013e3182238b55Search in Google Scholar PubMed
[11] Formica F, Avalli L, Redaelli G, Paolini G. Interhospital stabilization of adult patients with refractory cardiogenic shock by veno-arterial extracorporeal membrane oxygenation. Int J Cardiol 2011;147:164–5.10.1016/j.ijcard.2010.09.062Search in Google Scholar PubMed
Supplementary Material
The article (https://doi.org/10.1515/iss-2018-0029) offers reviewer assessments as supplementary material.
©2018 El Beyrouti H., et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 License.
Articles in the same Issue
- Original Articles
- Young surgeons’ challenges at the start of their clinical residency: a semi-qualitative study
- Intermittent Pringle maneuver may be beneficial for radiofrequency ablations in situations with tumor-vessel proximity
- Computed tomography donor liver volumetry before liver transplantation in infants ≤10 kg: does the estimated graft diameter affect the outcome?
- Reversible biliary occlusion in a small animal model: first description of a new technique
- Short- and long-term outcomes for the surgical treatment of acute pulmonary embolism
- Serum markers for early detection of patients with mesenteric ischemia after cardiac surgery
- Case Report
- Acute heart failure due to giant left atrium: remote ECLS implantation for interhospital transfer and bridging to decision
Articles in the same Issue
- Original Articles
- Young surgeons’ challenges at the start of their clinical residency: a semi-qualitative study
- Intermittent Pringle maneuver may be beneficial for radiofrequency ablations in situations with tumor-vessel proximity
- Computed tomography donor liver volumetry before liver transplantation in infants ≤10 kg: does the estimated graft diameter affect the outcome?
- Reversible biliary occlusion in a small animal model: first description of a new technique
- Short- and long-term outcomes for the surgical treatment of acute pulmonary embolism
- Serum markers for early detection of patients with mesenteric ischemia after cardiac surgery
- Case Report
- Acute heart failure due to giant left atrium: remote ECLS implantation for interhospital transfer and bridging to decision

