Abstract
Young adults frequently face mental health challenges due to high expectations, self-doubt, and uncertainties about the future. With advancements in digital communication, artificial intelligence (AI)-based conversational agents (CAs) could play a role for those struggling with grief, anxiety or loneliness. This study investigates the current use of CAs (e. g. ChatGPT, Siri) for mental health purposes and the preferred communication modes among young adults in Germany. A quantitative online survey was conducted from August 6 to September 17, 2023, involving 216 participants aged 18 to 27 (120 females, 95 males, 1 non-binary). The findings reveal that 82 % of respondents use CAs, with 17 % having asked help from these agents when feeling depressed or anxious. While verbal communication is preferred for sharing grief with humans, written interaction is favoured when engaging with CAs. Notably, participants with preexisting anxiety or psychological distress showed an increased tendency to communicate about it and a stronger preference for writing about their concerns. These findings suggest that CAs could be a valuable tool for mental health support, especially for young male adults who may be less inclined to openly share their concerns. Further exploration is needed to understand the evolving role of CAs in mental health support, particularly in how to interact with them effectively.
1 Introduction
Adolescence is a critical period marked by challenges, changes, and increased vulnerability to mental health issues. 1 , 2 Factors such as worsening income, inequality, family conflicts, social media, and increasing pressure within contemporary school settings can lead to mental health problems. Furthermore, the COVID-19 pandemic may have contributed to a rise in psychiatric disorder, such as depressive and anxiety disorders as well as symptoms related to grief. 3 , 4 During young adulthood, individuals strive to achieve financial independence, secure employment, establish romantic relationships, and actively contribute as valued and engaged members of their communities. This period is characterized by numerous opportunities and choices as individuals navigate various paths to shape their future. However, high expectations, self-doubt as well as an uncertain future can lead to personal crises. Young people face various individual barriers that hinder their ability to seek and access of professional help, such as waiting times, limited availability, costs, and concerns related to stigma and privacy. 5 , 6 , 7 These barriers can vary based on individual circumstances and challenges when attempting to engage with professional mental health services.
These disorders are not caused by a single factor but arise from a complex interplay of biological, genetic, psychological, and environmental factors. 1 , 2 , 8 Psychological disorders have wide-ranging impacts on individuals, extending beyond work disability. 9 , 10 They significantly affect overall well-being and are associated with an increased risk of chronic physical illnesses and premature death. 11 The global prevalence of mental disorders is substantial, with an estimated 13.4 % of the population affected. 12 Anxiety disorders and depressive disorders are among the most prevalent, affecting 6.5 % and 2.6 % of individuals, respectively. 12 The prevalence of mental health problems among children and young people is also significant, with rates ranging from 10 % to 20 % worldwide. 2 These statistics highlight the urgent need for effective strategies and interventions to address mental health issues and support the well-being of individuals, particularly in the younger population.
1.1 E-health on the rise
Aschbrenner et al. explored how young people utilize technologies such as smartphones and social media to address mental health concerns. 13 Participants were asked about their interest in connecting with other teenagers receiving treatment at a mental health centre through a private social media group. Results showed that 32 % expressed interest, 33 % showed no interest, and 35 % remained unsure. The concept of online peer-to-peer support holds promise in reducing stigma, fostering social connections, and ultimately improving the well-being of individuals with mental illness. However, qualitative interviews conducted as part of the study revealed that many participants expressed concerns about potential risks associated with joining a social media group of peers from a mental health center. 13
Lydia Seifert, the executive director of TelefonSeelsorge® Deutschland e. V. (TSD), a free counselling service for people living in Germany, also fears “that we have already become a society of the lonely”. 14 Young people have expressed a tendency to rely on self-reliance when confronted with challenges and show reluctance to fully engage in the process of seeking help or accessing support services. 8 , 15 Consequently, digital health interventions (DHI), telepsychotherapy, and e-mental health services have emerged as a diverse and rapidly expanding field, encompassing a wide range of technological tools and platforms such as websites, games, computer-assisted programs, mobile apps, virtual reality, and text messages. 8 , 16 , 17 , 18 , 19 The field of mobile health (mHealth) is growing, with a notable increase in psychological tools within Human-Computer Interaction (HCI). 20 , 21 , 22 The range is broad and serves various purposes, spanning from identifying symptoms and helping individuals manage their mental health to promoting help-seeking behaviours and providing preventive or therapeutic interventions. 21 , 23 Potential advantages are enhanced effectiveness, accessibility, anonymity, prompt feedback, cost-effectiveness, applicability in real-life contexts, adherence to therapy, and reach of a broader population. 8 , 24
1.2 Digital conversational agents for mental health
The proliferation of mobile applications addressing mental health issues is on the rise. Existing evidence regarding CAs in psychiatry indicates both potential benefits and associated risks. 7 , 13 , 25 CAs are programs designed to communicate with users to provide or collect information. They can be activated by natural language input such text, voice or image and respond with an output. 15 However, the preferences for these various modalities seem to be unknown. 25
In the mid-1960s, ELIZA was the first prominent chatbot that enabled certain kinds of natural language conversation between human and computers. 26 Josef Weizenbaum chose the psychiatric interview as one example of categorized dyadic natural language communication, where one participant could assume limited knowledge of the real world. The utilization of AI and machine learning (ML) algorithm in CAs allows for more complex dialogue management and greater conversational flexibility and individuality for users. 24 , 27
Aguilera highlighted the significant growth in the use of digital technology in health applications, driven in part by the limitations of traditional one-on-one therapy in meeting the mental health needs of the population. There are calls to develop innovative ways to enhance the quality and reach of effective clinical interventions using tools like mobile phones and smartphones. 28
On the other hand, security risks, data usage and ethical concerns are partly unclear, and the potential of this technology is supposedly not yet exhausted. Because this technology and its potential are quite new, no long-term studies exist. A study by Samantray found that digital cognitive-behaviour therapy (dCBT) intervention had a large positive impact on the overall symptoms of clients enrolled in a mental wellness care program. 29 This is consistent with previous meta-analyses on the potential of digital mental health interventions to improve mental health outcomes by Lewis et al. 30
Although the most popular chatbot, Chat Generative Pre-Trained Transformer (ChatGPT), is not designed to answer questions related to healthcare or mental health, users are willing to use it for self-diagnosis. 31 However, it is important to acknowledge that these opportunities come with safety concerns. There is a risk of incorrect self-assessment or therapy that could result in significant harm or even fatal outcomes. 27 , 32 Additionally, algorithm ethics raises issues of bias, responsibility, transparency, and explainability of algorithms, as well as validation and evaluation. Biased training data or unfiltered data from the internet can lead to biased results. 33 Over-reliance with blind faith on ChatGPT may adversely affect patients’ health. Inaccurate content could potentially lead to incorrect self-diagnosis and even greater harm due to hallucinations of digital interlocutors.
The use of clinical best practices, warranty of the accuracy, reliability, and validity of the content generated by these algorithms, and a code of ethics for the responsible use of ChatGPT is strongly recommended. 34 , 35 Additionally, emphasizing Fairness, Accountability, and Transparency (FAT*) in the corresponding context is essential. 36 Approaches for prevention and early intervention should be explored for mental health issues to reduce restrictions in social and professional life.
A comprehensive understanding of the potential advantages and limitations of AI-based CAs, such as ChatGPT, in the context of mental health is crucial for optimizing their use and maximizing their potential to support well-being. The mode of communication can play an important role in promoting well-being and avoiding misunderstandings.
1.3 Changing communication behaviour
Over the past decade, there has been a remarkable surge in interpersonal communication facilitated by internet-connected mobile devices. 37 Younger generations, including children, adolescents, and emerging adults, have grown up in an era saturated with digital communication tools. These tools have profoundly impacted the dynamics of interpersonal relationships within families and among friends. 38 Almost everybody owns a smartphone and can be reached quite easily if desired. This trend has been accompanied by a significant shift in communication preferences, with mobile instant messaging applications like WhatsApp gaining prominence and, in some cases, even displace traditional communication channels such as phone calls. More recently, a new mode of communication has gained popularity: voice messaging. 39 This emerging channel allows individuals to exchange recorded voice messages, offering a convenient and alternative method of conveying information and engaging in asynchronous interpersonal communication. According to a 2019 study, 39 69 % of Germans have engaged in sending voice messages through messaging services such as WhatsApp. The primary advantages of voice messaging include reduced effort compared to typing text messages, minimized chances of misunderstandings compared to written text, and the convenience of time independence compared to phone calls. Users can express themselves more naturally and convey a broader range of emotions. Notably, Haas et al. have indicated that nearly half of voice message interactions occur while individuals are engaged in activities such as walking, driving, or bicycling, highlighting the convenience and flexibility of this medium. 37 Users have reported a heightened sense of closeness and joyfulness when using voice messages to connect with others. However, concerns related to privacy and the inconvenience of reviewing or editing recorded messages have also been raised, underscoring the need to address these issues for a more seamless and secure user experience.
In their in-the-wild study, 37 the researchers found that the relationship between emotional stability and the frequency of voice message usage was not as straightforward, while extroversion appeared to align more closely with its use. To further analyse this phenomenon, the theoretical framework proposed by Nardi et al. can be applied. 40 This framework distinguishes between interactional and outeractional message usage. Interactional message usage involves the rapid exchange of information, quick questions, clarifications and staying in touch with friends and family. On the other hand, outeraction refers to communicative processes that go beyond information exchange, where individuals reach out to others in explicitly social ways to foster connection. Human speech can evoke a sense of connection, even in situations where romantic partners or family members are temporarily separated, thus contributing to the concept of outeraction.
In 2022, Nummer gegen Kummer e. V., a free telephone counselling service in Germany for children, young people, and parents, observed a significant surge in chat requests compared to the previous year. This increase demonstrates a notable rise of 18 % in the demand for their chat services. 41 According to the statistics provided by TSD, there was a notable rise in contacts through mail and chat services between 2019 and 2020. 42 Mail contacts experienced a 28 % increase, while chatting witnessed a remarkable surge of over 70 % compared to the year 2019. Notably, these communication channels were predominantly utilized by younger individuals within the age range of 15–40. Furthermore, similar values were also recorded in 2021 compared with the previous year. Engaging in purely text-based communication, whether with a human coach or a supposed chatbot, can present challenges and occasionally result in misunderstandings. 43 , 44 As communication preferences shift, it raises the question of which mode would best support well-being.
1.4 Research questions
To address the relevance and research gap, this study presents a quantitative investigation focusing on young adults aged 18 to 27 in Germany and their help-seeking behaviours for common mental health challenges such as depression, anxiety, and general emotional distress. The research examines the current usage and potential of AI-based CAs in promoting mental health, with a key aspect being the evaluation of preferences for spoken or written interaction. By collecting empirical data, the study aims to provide insights into the preferences and needs of this age group, contributing to a deeper understanding of how AI-based CAs can support mental health. The central research questions addressed are:
RQ1:
To what extent do young adults in Germany use CAs when experiencing depression or anxiety?
RQ2:
Speaking or writing, what are the preferred communication modes for young adults when interacting with CAs?
2 Methods
This study explores communication preferences and mental health interactions with AI-based CAs. To achieve this, we outline the participant recruitment process and survey methodology for a quantitative study targeting young adults aged 18 to 27 in Germany. Recruitment was conducted through various channels, including social media, online panels, and paid advertising, resulting in 216 eligible participants. We collected data on current CA usage, communication preferences, mental health assessments, and sociodemographic information to identify predictors. These findings offer insights into young adults’ mental health, communication preferences, and the acceptance of CAs for promoting well-being.
2.1 Participants
In Germany, young adulthood is defined as the age range between 18 and 27 years. This aligns approximately with the MIT young adult development project. 45 According to the German Demography Portal, 46 in 2021, there were an estimated 4,683,208 men and 4,298,535 women aged 18 to 27 in Germany, comprising roughly 10.7 % of the total population. This demographic has been exposed to mobile applications from a young age and is receptive to new technologies. Additionally, this life stage is often marked by significant changes and experiences, making it a crucial target group for the study.
To achieve the largest and most diverse sample size, identical questionnaires were distributed through three different URL access points, encouraging voluntary participation via advertising, an online panel, or social media distribution among acquaintances and study groups. To ensure high data quality, only responses meeting the following criteria were considered: participants answered all required questions, were within the specified age range, and either resided in Germany or held German citizenship. Participants from the online panel were also required to pass an attention test.
According to the vendor, paid digital and print advertising on Facebook and Instagram reached a total of 18,048 people. However, only data from two participants recruited through this method met the quality criteria and were included in the analysis. The collection distributed under personal responsibility had an access rate of 651 visitors, with 193 participating in the survey and 163 successfully completing it. Data from 135 participants (84 female) met the quality criteria and were included in the analysis. The final collection from the paid online panel had a view count of 100, with 88 participants and 81 successful completions. Data from 81 participants (36 female) met the criteria for further analysis.
Since the questions in the three surveys were identical and compensation did not influence the research question, the usable results from all three surveys were combined into a single dataset of 216 participants (120 female).
2.2 Materials
This section outlines the materials and methods employed to conduct the study, addressing the research questions and ensuring the quality of all measurements.
2.2.1 Behaviour and addressing concerns and discomfort to human
In addition to providing insights into preferred communication modes when interacting with humans and CAs, this research aims to determine the most suitable communication mode for promoting mental health with CAs. Not only the form of interaction changes, but the number of communication media is increasing. Understanding which communication medium users prefer is a crucial question for designers and software developers. 47 In conjunction with existing surveys on the use of voice messages in Germany 39 and statistics related to the Nummer gegen Kummer helpline 41 this survey can help identify the preferred modes of communication for topics related to well-being.
To address this the initial phase of the study examines the distant communication behaviours of young adults, focusing on the frequency of using messaging, voice messaging, and phone calls. To understand how participants address concerns and discomfort with others, they were asked about their preferred communication modes: talking, writing, both, or neither. Similarly, participants were asked about their preferred feedback formats: verbal, written, both, or neither. Additionally, participants rated the importance of immediate feedback on a scale from 1 (unimportant) to 7 (important). Lastly, in this section, participants indicated their tendency to keep feelings and concerns to themselves, with response options ranging from ’yes’ to ‘no’ on a five-point scale.
2.2.2 Usage and communication with AI-based conversational agents
To evaluate whether participants already use digital assistants such as OpenAI’s ChatGPT, Apple’s Siri, Amazon’s Alexa, and Microsoft’s Cortana, they were asked to rate their experience on a five-point scale ranging from ‘yes’ to ‘no’. The survey did not distinguish between these technologies, as the primary focus was on their role as non-human communication partners. Participants were also asked to rate, on a similar scale, whether they had sought support from these digital assistants when feeling depressed or anxious. Additionally, participants were asked about their willingness to share their worries, fears, and needs with these technologies. Finally, participants indicated their preferred communication mode with these digital assistants: talking, writing, both, or neither.
2.2.3 Mental health status
As a secondary outcome, the mental health status of the participants was measured. To analyse symptoms of psychological distress, anxiety, and depression severity, several methods were employed using short questions and answers provided as Likert scales. 48
The Kessler Psychological Distress Scale (K6) is a commonly used self-report questionnaire for measuring psychological distress. 49 It consists of six questions that assess the frequency and intensity of various symptoms experienced over the past 30 days on a 5-point Likert scale, including feelings of tiredness, nervousness, sadness, and worthlessness. This scale is widely employed in research and clinical settings, including the WHO World Mental Health Surveys, to screen for mental health issues and evaluate individuals’ psychological well-being. It provides a reliable and efficient method for assessing psychological distress and is a valuable tool for understanding individuals’ mental health status.
The Generalized Anxiety Disorder 2-item (GAD-2) scale is a reliable and effective method used to assess the severity of generalized anxiety disorder, one of the most prevalent mental disorders. 50 , 51 This brief questionnaire consists of two questions that measure the frequency of anxiety symptoms experienced over the past two weeks. Participants rate their symptoms on a 4-point Likert scale, providing valuable information about the level of anxiety experienced.
For both K6 and GAD-2, the questions were designed to be easy to understand and to provide a reliable assessment of psychological distress or anxiety symptoms. 48 Using K6, a total score greater than or equal to 14 indicates generalized psychological distress. 52 For GAD-2 a sum scores greater than or equal to three indicates generalized anxiety symptoms. 52 The two questions provided for GAD-2 demonstrated adequate internal consistency, with a Cronbach’s alpha of 0.713. Furthermore, the K6 scale showed good internal consistency, with a Cronbach’s alpha of 0.863.
Additionally, the Sense of Coherence (SOC) framework by Aaron Antonovsky is proposed as a valuable theoretical foundation for adopting a salutogenic perspective in health research. 53 In contrast to the other two methods, SOC assesses how people view their lives and identifies how they use their resilience resources to maintain and develop their health. Thus, the salutogenic model of health can explain why people remain healthy in stressful situations and are even able to improve their health status. 54
The original form contains 29 items, measuring the three components comprehensibility, manageability, and meaningfulness on a 7-point scale to explore the factors that contribute to the ability of individuals to maintain and promote their health and well-being, as well as deal with stressors in a health-promoting manner. 54 , 55 Many studies with different reduced sets of these questions exist to enable screening for large populations. 56 , 57 , 58 , 59
For this survey, one question was selected from each of the three components. The selection criteria for these three questions were comprehensibility, timeliness, and age appropriateness. A 7-point scale with two verbal anchors (1 = high resistance; 7 = low resistance) allowed participants to rate their current feelings (details in Appendix B. SOC Questions). This adjustment was made to better align the questions and response options with the overall context of the study and the preceding questions. Consequently, a higher score on this scale indicates a lower sense of coherence and lower resilience. To prevent any potential misunderstandings, the term “Low SOC” will be employed in the subsequent sections. The internal consistency for these three questions was reasonable, with a Cronbach’s alpha of 0.724.
2.2.4 Sociodemographic data
To better understand the participant’s context, background characteristics were collected as additional secondary outcomes. Sociodemographic data included questions about age, gender, education level, employment status, and whether participants live in or hold citizenship in Germany.
2.3 Design and procedure
To enhance the utility and transparency of data collection in this research paper, the Checklist for Reporting the Results of Internet E-Surveys (CHERRIES) is employed. 60 To address both research questions, a quantitative, anonymous, web-based online survey was conducted among young adults aged 18–27 living in Germany, adhering to the principles of the Declaration of Helsinki. 61 Although an ethics application was not submitted prior to conducting the study, the authors are committed to ensuring the responsible and ethical conduct of research. Notes on the survey aim, contact details of the responsible scientists, an estimated duration of 5 min, and guidance for those seeking help and advice were provided in the introduction. Participation was voluntary, anonymous, and could be aborted at any time without giving reasons. Every participant had to confirm a declaration of consent before starting, and it was ensured that answers could not be traced back to any individual. Finally, the contact details of the researcher responsible were provided. Technical measures taken by the tool provider prevent the same person from submitting multiple contributions within the framework of the online tool used.
From July 30, 2023 to August 5, 2023, a pre-study was conducted with 21 volunteers from within the known network to assess usability, technical functionality, comprehension of the questions, and timing. The main survey, available in German and English, was carried out from August 6, 2023, to September 17, 2023, and was made publicly accessible via a specific link. Three different collections of links, each with a unique URL, were created to facilitate the distribution of the online survey through various media and allow for result comparisons. The different links were disseminated through:
The social media platforms Facebook and Instagram, WhatsApp, university email groups, the SurveyCircle research platform
The online panel provider ClickWorker
Paid digital advertising on social media (Facebook and Instagram) and distributed as leaflet in Munich
It’s important to note that only individuals recruited through ClickWorker were compensated in accordance with the statutory minimum wage in Germany for their participation. There was no competitive element or other financial incentive for survey engagement.
In addition to the homepage, the survey contained five pages to guide respondents through a total of 20 questions (overview in Appendix A. Survey Structure). The questions were not randomized, and each page contained four to six questions. Only the mental health questions were optional; all others were mandatory. Respondents could review and change their answers at any time during the process until final confirmation on the closing page.
The collected data were examined for correlations to gain insights into various aspects of mental health, acceptance of CAs, and preferred forms of interaction. Patterns between current mental health disorders and the mode of communication with the respective CA were identified. Internal consistencies, descriptive statistics, and t-tests were calculated using Excel (Microsoft® Excel® for Microsoft 365 MSO (version 2308 Build 16.0.16731.20182) 64 bit). To compare the means of two or more groups, t-test or ANOVA were used with a level of significance set at (alpha) p < 0.05.
3 Results
This chapter presents the study’s results, focusing on the communication preferences of young adults in Germany. It explores their feelings and worries, experiences with AI-based CAs, and the potential influence of mental health status and sociodemographic characteristics on communication behaviour.
3.1 Communication behaviour and addressing concerns and discomfort to human
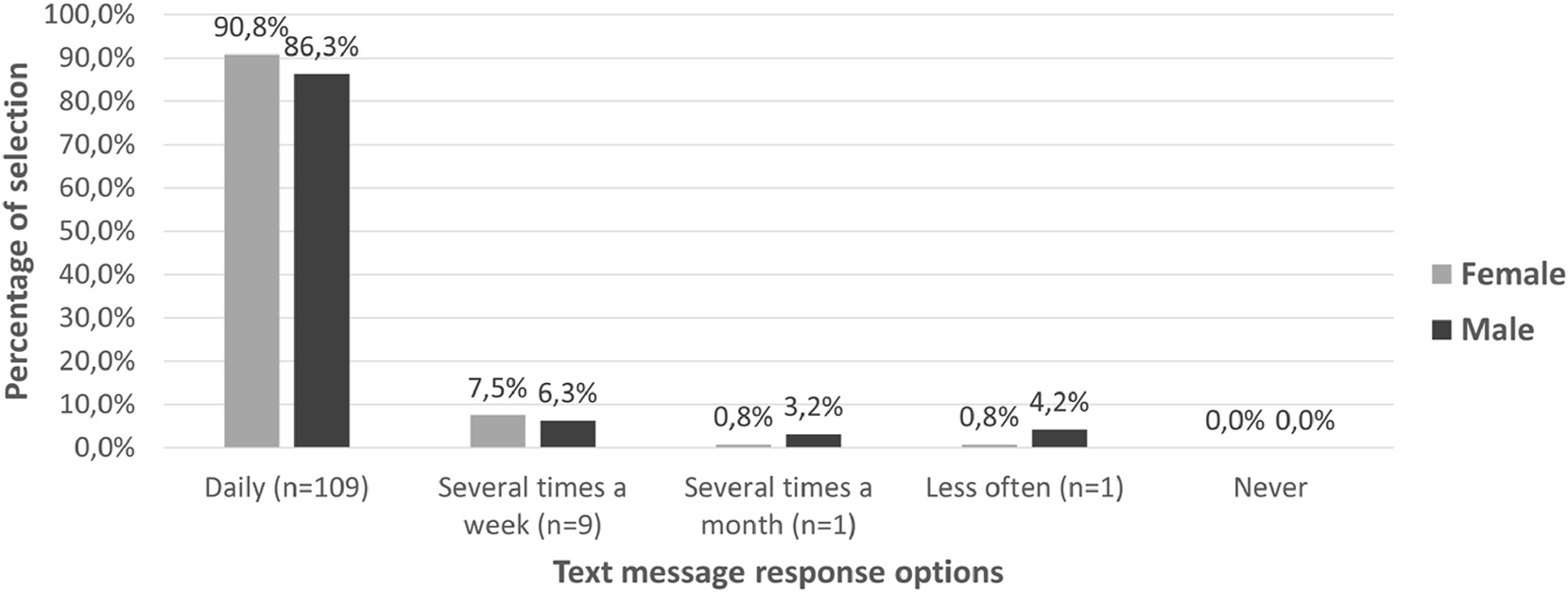
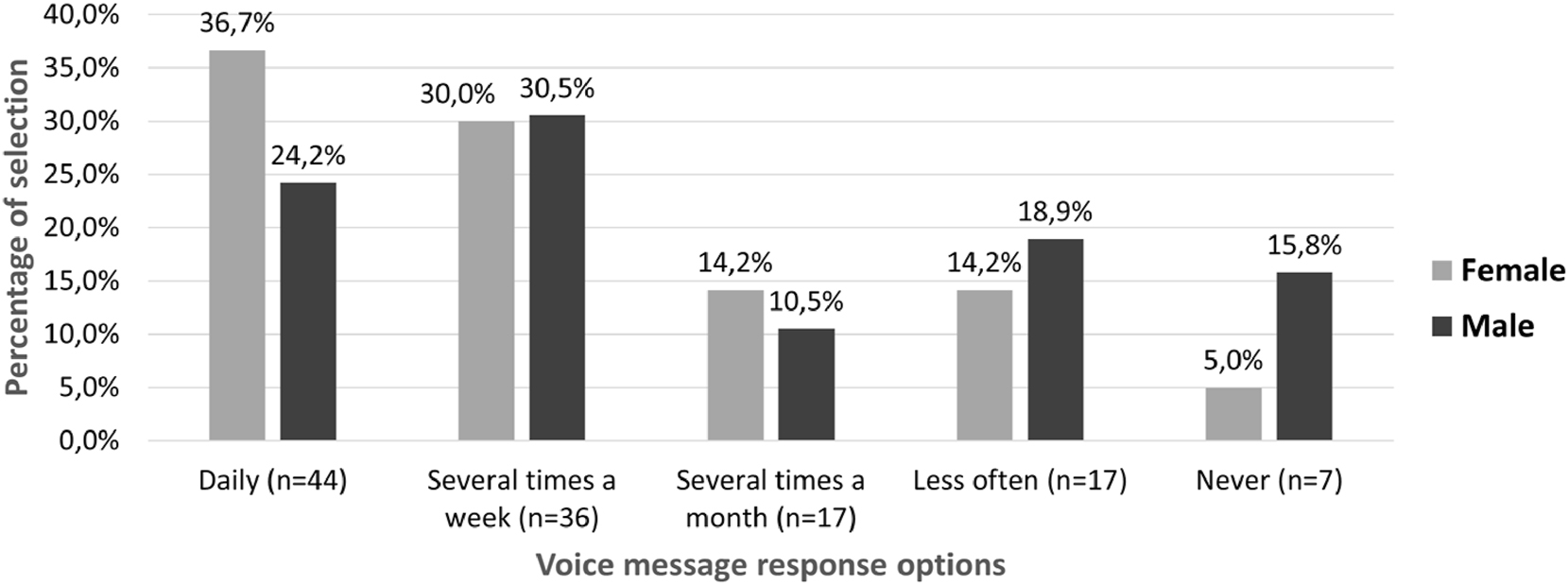
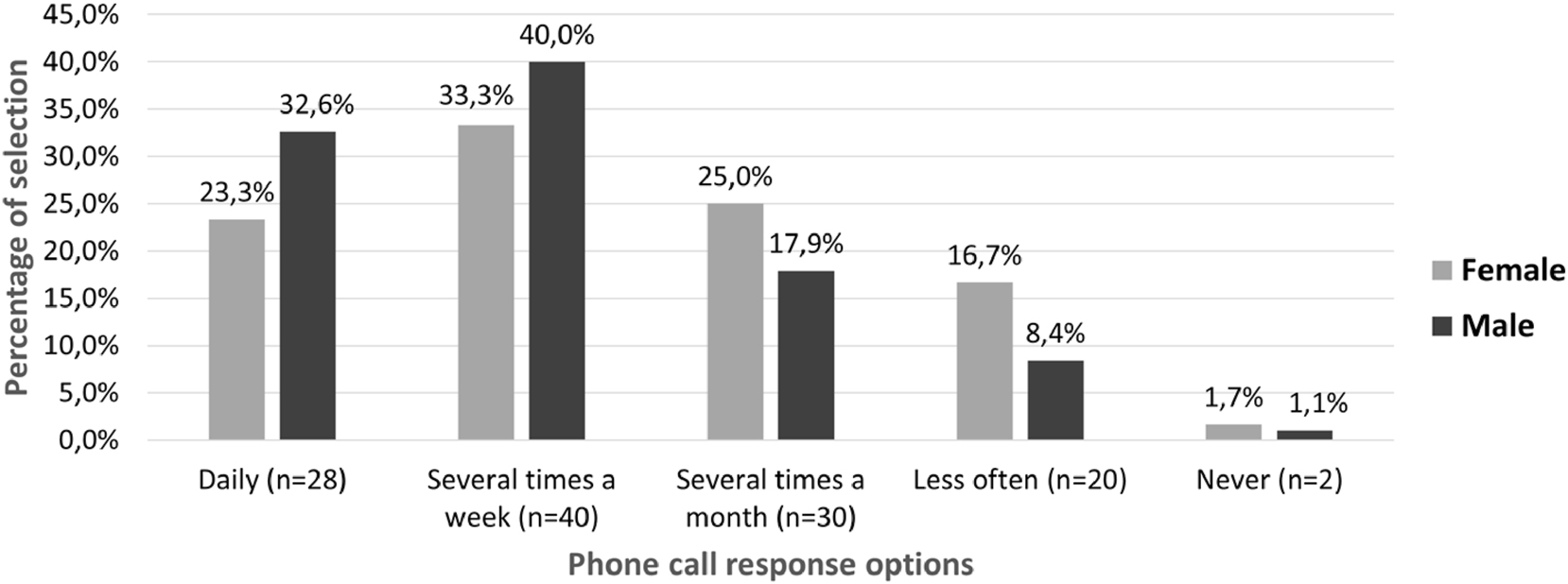
The first question was about current messaging behaviour to get an overview of how often text messages; voice messages and calls are made. Respondents could choose between daily, several times a week, several times a month, less often and never. 89 % of respondents use text messaging daily, 7 % several times a week and 2 % each several times a month and less often. 31 % use voice messages daily and 30 % several times a week, 10 % never use voice messages. Phone calls are made by 26 % of respondents daily and 36 % several times a week, 22 % several times a month, 13 % less often and only 1 % never. There is no difference in the frequency of text messaging between men and women (t(214) = −1.72; p = 0.09), whereas women send voice messages more often (t(214) = −2.71; p = 0.007) and men use phone calls more often as a synchronous communication medium (t(214) = 2.46; p = 0.01) (details in Appendix C. Messaging Behaviour).
To gather more specific information about whether people prefer to write or talk when communicating their feelings and concerns to a person, participants were asked to rate their communication preference. The results show that 48 % of respondents prefer to talk to a person about their feelings and concerns, 29 % favour both talking and writing, 19 % prefer to write, and 4 % would rather neither talk nor write to share their feelings and concerns with a person. Preferences are identical for both genders, with no differences found within the sociodemographic data.
Communication also involves receiving messages and feedback. To this end, respondents were asked to indicate their preference for receiving verbal or written feedback from another person after expressing their feelings and concerns. The results showed that 56 % of respondents favour verbal feedback after expressing their feelings and concerns, 28 % prefer both verbal and written feedback, 15 % prefer written feedback only, and 1 % of respondents would rather not receive either verbal or written feedback. No difference in preference was found between men and women. The importance of immediate feedback on a scale of 1 (unimportant) to 7 (very important) shows a mean of 5.54 (n = 216; SD = 1.32). Women have a mean of 5.73 (SD = 1.26) and men 5.29 (SD = 1.36). From this it can be concluded that immediate feedback is important as soon as concerns and discomfort have been expressed, as well as that this should preferably be done in verbal form.
To find out if young adults prefer to keep their feelings and worries to themselves, they were asked this question using a 5-point Likert scale. 22.2 % prefer to keep their feelings and worries to themselves, 39.4 % prefer to keep them rather, 16.2 % indicate neither yes nor no, 20.8 % say rather no, and 1.4 % say no. Gender specific details are visualised in Figure 1. The distribution strongly indicates that men are more likely to keep their worries to themselves (t(214) = 3.19; p = 0.002), whereas women have a higher tendency to share them.
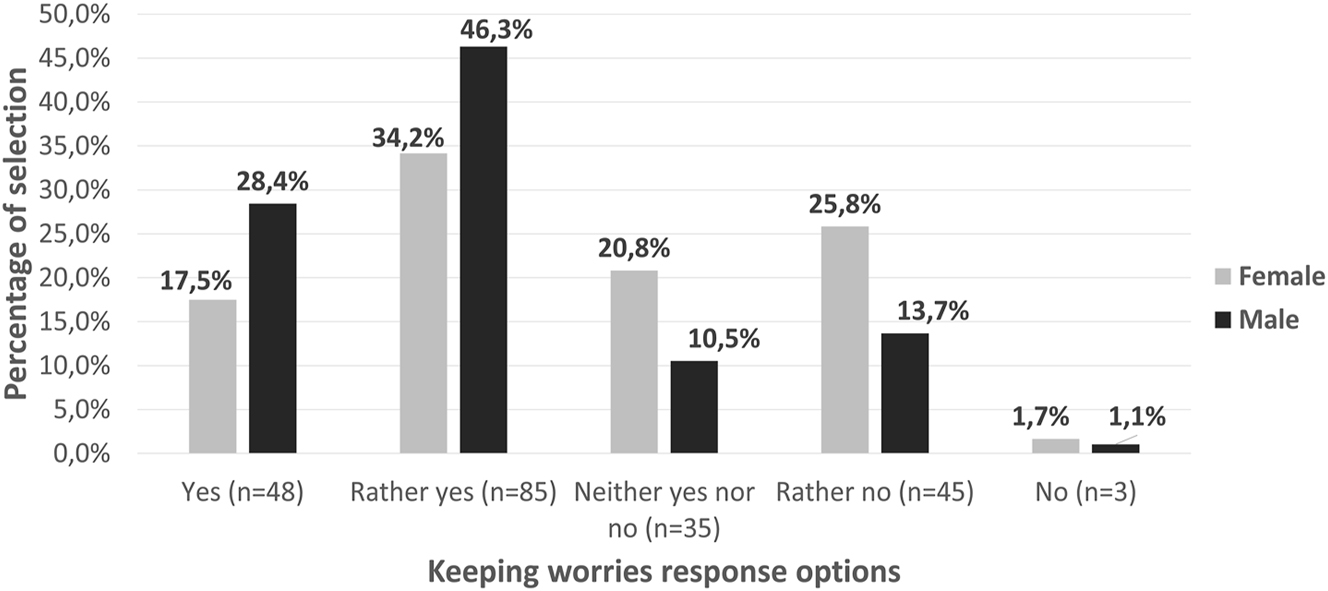
Young men (n = 95) and women (n = 120) deal differently with keeping worries to themselves.
3.2 Usage and communication with AI-based conversational agents
Additionally, this study explores whether digital conversation partners, such as ChatGPT or Siri, are or would be used to share worries, fears, or depression. Participants were asked if they had ever used a CA, whether they used it for mental health support, and how likely they might be to do so. Ratings on a 5-point Likert scale provided insights into this, also in combination with mental health status. The next section of questions examines whether communication behavior differs between human-to-human and human-to-CA interactions, focusing on communication mode, mental health status, and potential impact.
3.2.1 Using a CA to promote mental health
First, participants were asked if they had ever used a CA. Results showed that 69 % affirmed, 13 % responded “rather yes”, 3 % selected “neither yes nor no”, 6 % chose “rather no”, and 9 % answered “no”. To address RQ1 and determine whether CAs had already been used to help with depression or anxiety, respondents rated this specific use. Findings indicate that 9 % answered “yes”, 8 % selected “rather yes”, 4 % rated “neither yes nor no”, 15 % chose “rather no” and 64 % answered “no”. Most participants (82 %) had already used a CA, and 17 % sought support when feeling depressed or anxious.
When asked if they would trust a CA with their worries, fears, and needs in the future, 7 % of respondents answered “yes”. An additional 12 % indicated that they would tend to trust a CA, 9 % responded “neither yes nor no”, 28 % indicated they would tend not to trust, and 44 % stated that they would not trust a CA.
To investigate whether mental health status affects the experience and willingness to ask a CA for help when feeling anxious or depressed, GAD-2, K6 and Low SOC were examined as potential predictors for RQ1.
Participants with increased GAD-2 (t(214) = 3.08; p = 0.002) or K6 (t(214) = 3.27; p = 0.001) were more inclined to ask a CA for support when they felt depressed or anxious (Table 1). Additionally, Low SOC was highest for individuals who responded “yes” and “rather yes” compared to “rather no”, “no”, and “neither yes nor no”.
Participants with increased GAD-2 (t(214) = 3.08, p = 0.002) and K6 (t(214) = 3.267, p = 0.001) are more likely to have already asked a CA for help with worries. Additionally, those with Low SOC scores are more likely to have sought assistance.
| Already asked CA for help with worries | GAD-2 < 3 n [%] | GAD-2 ≥ 3 n [%] | K6 < 14 n [%] | K6 ≥ 14 n [%] | Low SOC mean (SD) |
|---|---|---|---|---|---|
| Yes | 10 [6.7] | 9 [13.89] | 13 [7.0] | 6 [20.0] | 13.21 (3.69) |
| Rather yes | 10 [6.7] | 7 [10.8] | 12 [6.5] | 5 [16.7] | 12.71 (2.91) |
| Neither yes nor no | 3 [2.0] | 4 [6.2] | 7 [3.8] | 1 [3.3] | 9.88 (3.76) |
| Rather no | 18 [12.0] | 15 [23.1] | 28 [15.1] | 5 [16.7] | 11.15 (3.90) |
| No | 109 [72.7] | 30 [46.2] | 126 [67.7] | 13 [43.3] | 9.79 (3.67) |
Furthermore, the results indicate that individuals with elevated anxiety disorder, mental disorders, or low resilience are more willing to ask a CA for help when feeling unwell (Table 2). Participants with increased GAD-2 are more likely to seek support from CAs (t(214) = 2.29, p = 0.02) compared to those below the threshold. A similar trend is observed for K6 (t(214) = 1.86, p = 0.06). Additionally, Low SOC scores are highest for individuals who responded “yes” and “rather yes”.
There is an increasing tendency to ask a CA for help in cases of anxiety (GAD-2: t(214) = 2.29, p = 0.02) or distress (K6: t(214) = 1.86, p = 0.06). Additionally, Low SOC is highest among participants willing to use a CA.
| Probably would ask CA for help with worries | GAD-2 < 3 n [%] | GAD-2 ≥ 3 n [%] | K6 < 14 n [%] | K6 ≥ 14 n [%] | Low SOC mean (SD) |
|---|---|---|---|---|---|
| Yes | 10 [6.7] | 6 [9.2] | 13 [7.0] | 3 [10.0] | 12.25 (3.67) |
| Rather yes | 15 [10.0] | 10 [15.4] | 19 [10.2] | 6 [20.7] | 12.24 (2.90) |
| Neither yes nor no | 10 [6.7] | 9 [13.8] | 16 [8.6] | 3 [10.0] | 11.63 (3.72) |
| Rather no | 41 [27.3] | 19 [29.2] | 51 [27.4] | 9 [30.0] | 10.33 (4.26) |
| No | 74 [49.3] | 21 [32.3] | 87 [46.8] | 9 [30.0] | 9.71 (3.56) |
3.2.2 Communication mode to promote mental health
To compare human-to-human communication with human-to-CA communication and address RQ2, participants were asked whether they preferred speaking or writing to a CA. The results indicate that 46 % prefer writing, 26 % would neither speak nor write with a CA, 16 % prefer speaking, and 11 % prefer both speaking and writing. All questions showed no difference in preference between on sex, education level or occupation status. Unlike human-to-human communication, participants prefer writing to their digital counterparts rather than speaking.
To evaluate the potential influence of anxiety or mental disorders on communication behaviour with humans and CAs, and to examine predictors for RQ2, the threshold values of GAD-2, K6, and mean values of Low SOC were compared.
When asked if participants were more likely to keep their worries to themselves, no differences were found at higher GAD-2 (t(214) = 0.663; p = 0.508) or K6 (t(214) = 0.530; p = 0.596) scores. However, as shown in Table 3, participants with elevated GAD-2 or K6 tend to be more willing to communicate with others about their distress. GAD-2, K6, and Low SOC have no significant influence on direct preference, although there is a slight tendency to use written communication. Similar observations can be made for human feedback after confiding worries (Table 4). Additionally, GAD-2 (t(214) = 1.566; p = 0.119) and K6 (t(214) = −1.175; p = 0.241) scores have no influence on the immediateness of feedback.
Effect of GAD-2 (t(213) = −0.207, p = 0.84), K6 (t(214) = −0.215, p = 0.83) and Low SOC on the mode of communication with humans when expressing feelings and concerns.
| Communication mode with human | GAD-2 < 3 n [%] | GAD-2 ≥ 3 n [%] | K6 < 14 n [%] | K6 ≥ 14 n [%] | Low SOC mean (SD) |
|---|---|---|---|---|---|
| Talk | 75 [50.0] | 27 [41.5] | 90 [48.4] | 13 [43.3] | 9.69 (3.85) |
| Write | 24 [16.0] | 17 [26.2] | 35 [18.8] | 6 [20.0] | 11.44 (3.58) |
| Talk and write | 43 [28.7] | 20 [30.8] | 52 [28.0] | 11 [36.7] | 11.57 (3.49) |
| Neither talk nor write | 8 [5.3] | 1 [1.5] | 9 [4.8] | 0 [0.0] | 8.78 (4.39) |
Effect of GAD-2 (t(214) = −1.454, p = 0.15), K6 (t(214) = −1.370, p = 0.17) and Low SOC on the mode of communication with human when receive feedback after expressing feelings and concerns.
| Feedback communication mode with human | GAD-2 < 3 n [%] | GAD-2 ≥ 3 n [%] | K6 < 14 n [%] | K6 ≥ 14 n [%] | Low SOC mean (SD) |
|---|---|---|---|---|---|
| Verbal | 90 [60.0] | 29 [44.6] | 107 [57.5] | 13 [43.3] | 10.11 (3.73) |
| Written | 18 [12.0] | 14 [21.5] | 27 [14.5] | 5 [16.7] | 11.59 (4.27) |
| Verbal and written | 39 [26.0] | 22 [33.8] | 49 [26.3] | 12 [40.0] | 10.87 (3.64) |
| Neither verbal nor written | 3 [2.0] | 0 [0.0] | 3 [1.6] | 0 [0.0] | 9.33 (4.78) |
In Table 5 GAD-2, K6, and Low SOC scores are compared with the preferred general communication mode over CAs. Individuals with elevated GAD-2 or K6 show less reluctance to talk or write with it. Low SOC is also lowest for these individuals. The preferred mode of conversation remains writing.
Effects of GAD-2 (t(214) = 1.843, p = 0.07) and K6 (t(214) = 0.805, p = 0.42) indicate a preference for written communication, with a decrease in negative attitudes. Low SOC is lowest for individuals who do not wish to talk or write.
| Communication mode with CA | GAD-2 < 3 n [%] | GAD-2 ≥ 3 n [%] | K6 < 14 n [%] | K6 ≥ 14 n [%] | Low SOC mean (SD) |
|---|---|---|---|---|---|
| Talk | 23 [15.3] | 12 [18.5] | 29 [15.6] | 6 [20.0] | 10.63 (3.83) |
| Write | 66 [44.0] | 34 [52.3] | 86 [46.2] | 14 [46.7] | 10.78 (3.60) |
| Talk and write | 16 [10.7] | 8 [12.3] | 20 [10.8] | 4 [13.3] | 10.88 (4.53) |
| Neither talk nor write | 45 [30.0] | 11 [16.9] | 51 [27.4] | 6 [20.0] | 9.89 (3.89) |
3.3 Mental health status
Measurement of GAD-2 revealed that 30.2 % of respondents (n = 65/215, mean = 2.03, SD = 1.47) scored three or higher, indicating a high proportion of individuals with an anxiety disorder. The internal consistency of the two questions was adequate, with a Cronbach’s alpha of 0.713. Distinguishing between female (n = 40/65) and male (n = 24/65) participants showed that 62 % of those with an anxiety disorder were women. Thus, female respondents showed a higher tendency for anxiety (t(213) = 2.212, p = 0.028) than males.
According to K6, 13.9 % of respondents (n = 30/216, mean = 7.88, SD = 4.92) experienced psychological distress. A Cronbach’s alpha value of 0.863 shows a good internal consistency. Among these, 73 % of participants with psychological stress are women (n = 22/30), compared to men (n = 7/30). Female respondents were more likely to experience psychological stress (t(213) = 2.713, p = 0.007).
For the Low SOC measurement, scores ranged from one (high resilience) to seven (low resilience). The overall mean score for all three questions from 216 participants was 10.53 (SD = 3.85). Breaking down the scores for comprehensibility (n = 216; mean = 3.48; SD = 1.46), meaningfulness (n = 216; mean = 3.31; SD = 1.63), and manageability (n = 216; mean = 3.74; SD = 1.70) showed moderate results, with manageability having a slightly lower SOC. The internal consistency for these three questions was reasonable, with a Cronbach’s alpha of 0.724. Comparing female (n = 120; mean = 10.86; SD = 3.75) and male (n = 95; mean = 10.11; SD = 3.94) data shows no significant difference between genders (t(213) = 1.422, p = 0.156).
3.4 Sociodemographic data
During the 42-day period, the survey links were accessed by 912 people. Of these, 287 participated, 248 completed the survey, and 216 data were usable. Participants included 120 females (55.6 %), 95 males (44.0 %) and one non-binary person (0.5 %). The mean age was 23.6 years (SD 2.58), with 64 participants (30 %) aged between 18 and 22 years, and 152 (70 %) aged between 23 and 27 years.
In terms of education, 181 participants (83.8 %) had a high level, 32 (14.8 %) had a medium level, and three (1.4 %) had a low level. Regarding occupational status, 19 (9 %) were currently in education, 102 (47 %) were undergraduate or graduate students, 73 (34 %) were employed, 13 (6 %) were self-employed, four (1 %) were unemployed, and five (2 %) reported other employment types such as working student jobs.
All participants lived in Germany, 207 (96 %) had German citizenship, and eleven (5 %) used the English version of the survey instead of the German version.
4 Discussion
This chapter presents the main findings of the study, comparing them with previous research, and outlines limitations and areas for future research. Key insights include communication preferences among young adults, gender differences in coping with distress, and the use of CAs for mental health support.
4.1 Principal findings
Communication is constantly evolving. Currently, text messages are the primary mode of long-distance communication among young adults using mobile phones. However, immediate responses cannot always be expected, even with voice messages, which offer richer communication due to the potential for more personal conversations based on voice and expression. This richer communication can also help reduce misunderstandings. The participating young males tend to prefer traditional telephone calls more frequently than females. In contrast, women are slightly more inclined to use voice messages, as also shown in a survey by the German Bundesverband Digitale Wirtschaft e. V. 39
Gender differences are evident in how individuals cope with grief and worry. Men tend more to internalize and discuss their concerns with themselves, while women tend to share them with others. When expressing discomfort to another person, both typically prefer verbal communication. This study did not identify significant differences between genders, nor were there variations in the threshold values for GAD-2 and K6 as measured in the study. However, to address RQ2, a more detailed analysis of the results reveals that as anxiety or psychological distress increases, so does the preference for written communication or a combination of written and verbal communication, whether with human or artificial counterparts. Respondents exhibiting these patterns may also display greater insecurity or lower resilience, as indicated by Low SOC scores. These findings suggest a link between SOC and mental health behaviors in young adults, as also observed by Henrique da-Silva-Domingues et al. 62
In contrast to communication with humans, respondents in the random sample showed a preference for written communication or even no communication at all when interacting with CAs. The reasons behind this choice were not explored in this survey. Unlike written communication with people, users can typically expect immediate feedback when engaging with CAs, although the potential for misunderstandings remains. It’s important to note that the current state of AI technology is not yet fully mature, and voices generated by AI can often sound artificial. As this new technology continues to advance and becomes more established, the future path of communication will become clearer.
However, to address RQ1, the results of the online survey indicate that CAs are currently used by most young adults (82 %) and 17 % used them to consult for help or advice when experiencing mental health challenges. However, it should be emphasized that the tendency to use this new technology as a communication partner appears to be significantly higher among people with pre-existing anxieties, mental health problems or low resilience.
Presently, the available evidence suggests that written communication is the preferred mode when interacting with a CA about grief. As technology continues to advance the preferred mode of communication will require further exploration and examination of using AI-based CAs for mental health purposes.
4.2 Comparison with previous work
Compared to previous studies, the findings from this survey confirm that asynchronous voice messages are increasingly common in Germany. As of 2019, 69 % of 1,051 Germans had sent voice messages through messaging services like WhatsApp. 38 In this current study, over 90 % of young adults in Germany are already using voice messages. Like trends noted in the survey of 2019, 39 women in our study also utilize voice messages more frequently than men (t(214) = −2.71; p = 0.0072). According to the TSD 2021 statistics, 42 the slight increase in preference for writing about worries can also be attributed to the rise in written traffic related to sorrow. The concept of outeractional message usage to evoke a sense of connection seems to hold true when communicating with people, but this does not appear to apply to digital counterparts. 40 In their empirical study, Zhu et al. utilized the Theory of Consumption Values (TCV) to observe satisfaction and continuance intention towards mHealth chatbots during the COVID-19 pandemic in China. Contrary to their expectations, voice interaction between citizens and the chatbot Xiaolv did not play a significant role. 63
Regarding keeping worries and problems to themselves, our survey aligns with earlier research. Approximately 22 % prefer to keep their concerns to themselves, and 39 % lean towards self-reliance in handling their worries. 8 , 13 , 15
The prevalence of mental health problems among children and young people is a significant concern, with reported rates ranging from 10 % to 20 % worldwide, and these rates are still on the rise. 1 , 2 , 64 Large-scale epidemiological studies have shown that women may have a two to three-fold higher incidence of GAD compared to men. 65 In this study, most respondents with increased GAD-2 and K6 scores were female. However, no significant difference was observed between female and male participants (t(213) = 1.422; p = 0.156) regarding measured Low SOC.
Furthermore, in their study, Abd-alrazaq et al. assessed 41 chatbots for mental health, most of which provided written text input and mixed media (written, spoken, and visual) as output. 64 The reasons for this decision were not provided, but it can be assumed that it is due to simpler technical implementation. Additionally, the study mentioned that 92.5 % of the chatbots relied on decision trees to generate their responses for therapy, training, and screening. The authors note that these chatbots have less AI integration compared to chatbots in other fields, such as customer service, possibly because they are less error-prone and more secure.
In a study by Shahsavar et al., 78.4 % of the 475 respondents expressed a willingness to use ChatGPT for self-diagnosis in health-related topics. 31 Although this study did not specifically focus on mental health-related topics, it is worth noting that, in contrast, approximately 72 % of the 216 German participants indicated a disinclination to use a CA for mental health-related topics. In their online survey conducted in 2021 with a total of 100 mental health professionals from Northern Ireland, Ireland, Scotland, Sweden, and Finland, Sweeney et al. found that as years of experience increased, there was a corresponding increase in the belief that chatbots in the mHealth environment could help clients better manage their own mental health, improve quality, access, and timeliness of mental healthcare, and assist mental healthcare workers and professionals in their daily occupational roles. Additionally, a total of 80 % of the professional respondents indicated that they would be very likely or somewhat likely to prescribe a chatbot for mental health in the next five years. 66 The results of the previous conducted study in 2019 with a total of 100 practicing physicians across the United States from Palanica et al. were less optimistic. 67 A total of 44 % of the respondents believed that chatbots for mental health would become very likely or somewhat likely in the next five years. Furthermore, the majority (70 %) of the physicians expressed concerns about risks associated with chatbots for mental health. They worry that patients may abuse the use of chatbots and self-diagnose too often, understand the diagnose inaccurately, and that the digital assistant cannot provide detailed clarification on patient assessment. It becomes evident that experts’ perceptions and views vary based on culture, time, and knowledge of innovations and may differ from the view of their patients.
4.3 Limitations
It’s worth noting that current technology, including platforms like ChatGPT, is still relatively young and in an immature stage of development. A significant limitation of this study is the lack of differentiation between AI-based CA technologies. While chatbots like ChatGPT utilize LLMs to provide more comprehensive and personalized responses, voice assistants such as Siri, Alexa, and Cortana do not. These voice assistants primarily rely on predefined commands and lack the advanced conversational capabilities of LLM-based CAs. Despite this crucial technological difference, voice assistants were included as an example in this study to capture a broader range of user experiences with AI-based CAs. We recognize that users may interact with different types of CAs in their daily lives, and this survey was not about the technology behind it, but rather the fact that there is technical intelligence at the other end instead of a human. In addition, LLM-based CAs did not offer natural and s communication via voice at that time. However, we acknowledge that this approach may have introduced variability in responses, as participants’ experiences with LLM-based CAs and non-LLM-based voice assistants are inherently different. Like our follow up study in 2024, 68 future research should focus specifically on LLM-based CAs to provide more targeted insights into their potential for mental health support. In addition, the advantages and disadvantages of asking a digital counterpart for help with grief should be identified.
An additional influence could have happened during the survey introduction. There, the research question regarding the ability of CAs to provide written or verbal support for grief was presented relatively clearly. However, this clarity may have deterred individuals who have a fear or aversion to chatbots or similar technologies. This also might be a reason for the small size of participants, successfully finished the survey. Cause of this, our findings must be interpreted with caution. Achieving the right balance between transparency and impartiality is a challenge.
Although an ethical application was not made in advance, we are convinced that this is safe and therefore responsible research for the respondents involved. For this we took several steps to ensure the responsible and ethical conduct of our research. These measures included:
Informed Consent: All participants were provided with detailed information about the study’s aims, the voluntary nature of participation, and the right to withdraw at any time without consequences. Participants had to confirm their consent before proceeding with the survey.
Anonymity: The survey was designed to be completely anonymous, with no personally identifiable information collected. This ensured that responses could not be traced back to individual participants.
Support Resources: We provided contact information for mental health support services in case participants felt distressed during or after the survey.
Data Security: All data were stored securely, and access was limited to the research team to protect participant confidentiality.
We are committed to upholding the highest ethical standards in our research and believe that these measures ensured the responsible conduct of this study. Nevertheless, an ethics application was successfully submitted for the subsequent study in 2024 before it was carried out. 68
A potential limitation of our study is the reliance on self-reported data, particularly from participants recruited through paid advertising channels – 100 of which 81 met the quality criteria. To mitigate the risk of dishonest or invented responses, we implemented several quality control measures:
Attention Checks: Participants from the online panel were required to pass an attention test to ensure they were engaged and attentive during the survey.
Consistency Checks: We examined the internal consistency of responses using established scales (K6 and GAD-2) and found adequate to good reliability (Cronbach’s alpha of 0.863 for K6 and 0.713 for GAD-2).
Data Cleaning: We excluded responses that did not meet the quality criteria, such as incomplete or inconsistent answers.
While these measures help ensure the reliability of our data, we acknowledge that the risk of dishonest responses cannot be eliminated. Future research could benefit from additional validation methods, such as cross-referencing self-reported data with clinical assessments. Despite these limitations, the internal consistency of our results and the alignment with existing literature suggest that our findings are valuable and provide meaningful insights into the use of AI-based CAs for mental health support.
4.4 Future research
AI against worries? Future research should shed more light on the reasons for the relatively high reluctance to use CAs for sorrow compared to health-related purposes. Furthermore, extending the study to different age groups may lead to further insights into this phenomenon. It would be interesting to compare whether AI-based CAs can provide added value over traditional psychotherapeutic methods or pose a real danger as things stand. The potential of CAs as supportive therapists needs to be further explored, considering aspects such as safety, acceptability, control, quality, and cost. Furthermore, ethical considerations in the application of AI in healthcare highlight the need to address ethical issues such as transparency, accountability, bias, privacy, and responsibility when using AI in healthcare. 69 , 70 , 71 These ethical concerns must be carefully considered to ensure the safe and responsible integration of AI into healthcare practices for both patients and specialists.
Furthermore, a comparison to teletherapy, which promises already increased access, quality, and cost reduction, should be evaluated from an ethical and effectivity perspective. Especially socioeconomic and educational barriers may limit technology use and therefore access to healthcare resources. 72 By collaborating with healthcare workers, scholars can apply their qualitative and quantitative skills to address a variety of ethical issues in healthcare.
Beside transparency, accountability, and trust, as well as values of fairness, justice, and equality are necessary to integrate AI not only in medical topics but also into daily practice. In their systematic review of published empirical studies of medical AI ethics, Tang et al. aimed to map the main approaches, findings and limitations of existing scholarship to inform future practice considerations. During this they figured out that generally clinicians report more ethical concerns related to the use of AI in health than patients. 73 To address questions of legal responsibility, Müller et al. have developed 10 easy understandable commandments as practical guideline, which were agreed upon in an online survey of 121 computer experts (47 %) and medical doctors (33 %). Among other things, they emphasize the need for recognizability regarding which part of the communication is performed by a CA and that humans should never be deceived by these systems. 74 Therefore, future research should also consider collecting opinions, information, and considerations from both patients and specialists. This can help ensure a comprehensive understanding of the challenges and inform the development of appropriate guidelines and frameworks.
Certainly, only long-term studies can provide insight into whether an AI can really assist with mental problems or other related issues, such as relapse prevention for alcohol, drug or other addictions. 75 Furthermore, evaluation on the effectivity for promoting resilience and well-being with the use of this technology combined with SOC could be considered. 76 , 77
However, digital communication partners must not and can never replace friends, family, therapists, coaches, or other trusted persons and specialists. Nonetheless, perhaps they can serve as valuable writing or speaking partners for those people who are struggling with worries and individually address the problems to prepare ways out of the negative spiral of thoughts or bridge the gap between therapy slots. Various possibilities to integrate AI-based CAs in the patient-expert interaction should be rated for acceptance by both involved groups to gain insights about possibilities to improve mental health. Although, in a scholarly publication from 2015, both professionals and drug-dependent patients confirmed the high relevance of information system – like teletherapy – research, related to relapse prevention. 75 Potentially, the Action Research (AR) approach can help to move from ‘pilotitis’ to sustainable solutions, thereby reducing the current limited resources for therapy. 78 Nevertheless, the responsibility for an AI decision, action, or communicative process must be explainable and transparent, and it must be taken by a competent physical or legal person. 74 Possibilities of combining artificial intelligence with human intelligence should be considered in future research instead of providing standalone AI mental health applications.
Particularly worrying is the fact that young adult men tend to keep their worries to themselves (75 %) compared to young women (52 %). This is most relevant considering that the suicide rate among young men aged 15–29 years in Germany in 2021 is significantly higher (77 %, n = 609/794) than among women. 11 The lack of access to mental health services, not only in low-income countries, may contribute to suicidal behaviour, resulting in increased mortality rates. 64 Better education on mental health topics and social acceptance are needed, especially among young men who find it harder to share their concerns and seek help. This cannot be achieved through technology alone, but possible approaches combining human and artificial intelligence can help to widen bottlenecks and provide preventative or remedial support.
-
Research ethics: Not applicable but adhering to the principles of the Declaration of Helsinki. While an ethics application was not submitted prior to conducting the study, the authors are committed to ensuring the responsible and ethical conduct of research.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission. Christina Lukas: Conceptualization, Methodology, Investigation, Formal analysis, Writing – Original draft preparation. Zeynep Tuncer: Conceptualization, Writing – Review & Editing Rüdiger Breitschwerdt: Conceptualization, Writing – Review & Editing, Supervision.
-
Use of Large Language Models, AI and Machine Learning Tools: Use of DeepL to improve the language.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
Appendix A: Survey structure and questions
The survey structure comprises several pages, each with a specific set of questions designed to gather information on different aspects of the research (Table 6). The complete questionnaire can be downloaded at https://www.dropbox.com/scl/fi/yyt9svy9imyjaq4w6qwhv/To_Write_To_Speak_Survey_German.pdf?rlkey=yc71hxt53vch178qamh4h0azx&st=40m4sjhk&dl=0.
Number and intention of questions per page.
| Page no. | Question count | Intention |
|---|---|---|
| 1. | 1 | Home page with description, scope details and confirmation of survey participation (informed consent) |
| 2. | 5 resp. 6 | Current asynchronous or synchronous messaging behaviour with people |
| 3. | 4 | Use and acceptance of CAs and messaging behaviours with them |
| 4. | 5 | Current state of mental health |
| 5. | 6 | Sociodemographic information |
| 6. | 0 | Notice of completion and contact information for the study director |
Appendix B: SOC questions
For measuring the SOC three questions – one of each component – of the original 29 item set was used in the online survey Table 7.
Questions to measure Low SOC.
| Question | Scale | Component | No. of origin |
|---|---|---|---|
| When you talk to people, do you have the feeling that they don’t understand you? | 1 = Never have this feeling. 7 = Always have this feeling |
Comprehensibility | 1 |
| How often do you have the feeling that there’s little meaning in the things you do in your daily life? | 1 = Never have this feeling 7 = Always have this feeling |
Meaningfulness | 28 |
| When something unpleasant happened in the past your tendency was…? | 1 = To say “ok that’s that, I have to live with it and go on” 7 = “to eat yourself up” about it |
Manageability | 18 |
References
1. Bor, W.; Dean, A. J.; Najman, J.; Hayatbakhsh, R. Are Child and Adolescent Mental Health Problems Increasing in the 21st Century? A Systematic Review. Aust. N. Z. J. Psychiatr. 2014, 48, 606–616; https://doi.org/10.1177/0004867414533834.Search in Google Scholar PubMed
2. Kieling, C.; Baker-Henningham, H.; Belfer, M.; Conti, G.; Ertem, I.; Omigbodun, O.; et al.. Child and Adolescent Mental Health Worldwide: Evidence for Action. Lancet 2011, 378, 1515–1525.10.1016/S0140-6736(11)60827-1Search in Google Scholar PubMed
3. Anmella, G.; Sanabra, M.; Primé-Tous, M.; Segú, X.; Cavero, M.; Morilla, I. Vickybot, a Chatbot for Anxiety-Depressive Symptoms and Work-Related Burnout in Primary Care and Health Care Professionals: Development, Feasibility, and Potential Effectiveness Studies. J. Med. Internet Res. 2023, 25, e43293; https://doi.org/10.2196/43293.Search in Google Scholar PubMed PubMed Central
4. Guessoum, S. B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L. Adolescent Psychiatric Disorders during the COVID-19 Pandemic and Lockdown. Psychiatr. Res. 2020, 291; https://doi.org/10.1016/j.psychres.2020.113264.Search in Google Scholar PubMed PubMed Central
5. Gulliver, A.; Griffiths, K. M.; Christensen, H. Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review. BMC Psychiatry 2010, 10.10.1186/1471-244X-10-113Search in Google Scholar PubMed PubMed Central
6. Musiat, P.; Goldstone, P.; Tarrier, N. Understanding the Acceptability of E-Mental Health – Attitudes and Expectations towards Computerised Self-Help Treatments for Mental Health Problems. BMC Psychiatry 2014, 14 (1); https://doi.org/10.1186/1471-244x-14-109.Search in Google Scholar PubMed PubMed Central
7. Wozney, L.; McGrath, P. J.; Gehring, N. D.; Bennett, K.; Huguet, A.; Hartling, L. EMental Healthcare Technologies for Anxiety and Depression in Childhood and Adolescence: Systematic Review of Studies Reporting Implementation Outcomes. JMIR Ment. Health 2018, 5, e48; https://doi.org/10.2196/mental.9655.Search in Google Scholar PubMed PubMed Central
8. Liverpool, S.; Mota, C. P.; Sales, C. M.; Čuš, A.; Carletto, S.; Hancheva, C. Engaging Children and Young People in Digital Mental Health Interventions: Systematic Review of Modes of Delivery, Facilitators, and Barriers. J. Med. Internet Res. 2020, 22, e16317; https://doi.org/10.2196/16317.Search in Google Scholar PubMed PubMed Central
9. Alonso, J.; Petukhova, M.; Vilagut, G.; Chatterji, S.; Heeringa, S.; Üstün, T. B. Days Out of Role Due to Common Physical and Mental Conditions: Results from the WHO World Mental Health Surveys. Mol Psychiatry 2011, 16 (12), 1234–1246; https://doi.org/10.1038/mp.2010.101.Search in Google Scholar PubMed PubMed Central
10. Whiteford, H. A.; Degenhardt, L.; Rehm, J.; Baxter, A. J.; Ferrari, A. J.; Erskine, H. E. Global Burden of Disease Attributable to Mental and Substance Use Disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382 (9904), 1575–1586.10.1016/S0140-6736(13)61611-6Search in Google Scholar PubMed
11. Statistisches Bundesamt. Todesursachen – Anzahl der Suizide nach Altersgruppen [Internet], 2022. [cited 2024 Jun 4]. Available from: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Todesursachen/Tabellen/sterbefaelle-suizid-erwachsene-kinder.html.Search in Google Scholar
12. Polanczyk, G. V.; Salum, G. A.; Sugaya, L. S.; Caye, A.; Rohde, L. A. Annual Research Review: A Meta-Analysis of the Worldwide Prevalence of Mental Disorders in Children and Adolescents. J. Child Psychol. Psychiatry 2015, 56 (3), 345–365; https://doi.org/10.1111/jcpp.12381.Search in Google Scholar PubMed
13. Aschbrenner, K. A.; Naslund, J. A.; Tomlinson, E. F.; Kinney, A.; Pratt, S. I.; Brunette, M. F. Adolescents’ Use of Digital Technologies and Preferences for Mobile Health Coaching in Public Mental Health Settings. Front. Public Health 2019, 7 (JUL); https://doi.org/10.3389/fpubh.2019.00178.Search in Google Scholar PubMed PubMed Central
14. TelefonSeelsorge® Deutschland e.V. TelefonSeelsorge veröffentlicht statistische Angaben zu 2021 [Internet] 2021 [cited 2023 Jun 25]. Available from: https://www.telefonseelsorge.de/telefonseelsorge-veroeffentlicht-statistische-angaben-zu-2021/.Search in Google Scholar
15. Radez, J.; Reardon, T.; Creswell, C.; Lawrence, P. J.; Evdoka-Burton, G.; Waite, P. Why Do Children and Adolescents (Not) Seek and Access Professional Help for Their Mental Health Problems? A Systematic Review of Quantitative and Qualitative Studies. Eur. Child Adolesc. Psychiatr. 2021, 30, 183–211; https://doi.org/10.1007/s00787-019-01469-4.Search in Google Scholar PubMed PubMed Central
16. Bao, H.; Lee, E. W. J. Examining the Antecedents and Health Outcomes of Health Apps and Wearables Use: an Integration of the Technology Acceptance Model and Communication Inequality. Behav. Inf. Technol. 2024, 43 (4), 695–716; https://doi.org/10.1080/0144929x.2023.2183062.Search in Google Scholar
17. Mayer, G.; Hummel, S.; Oetjen, N.; Gronewold, N.; Bubolz, S.; Blankenhagel, K. User Experience and Acceptance of Patients and Healthy Adults Testing a Personalized Self-Management App for Depression: A Non-randomized Mixed-Methods Feasibility Study. Digit Health 2022, 8; https://doi.org/10.1177/20552076221091353.Search in Google Scholar PubMed PubMed Central
18. Szekely, R.; Mason, O.; Frohlich, D.; Barley, E. The Use of Virtual Reality to Reduce Mental Health Stigma Among Healthcare and Non-Healthcare Students: A Systematic Review. Behav. Inf. Technol. 2023, 44, 2116–2133; https://doi.org/10.1080/0144929x.2023.2232049.Search in Google Scholar
19. Van Daele, T.; Karekla, M.; Kassianos, A. P.; Compare, A.; Haddouk, L.; Salgado, J.; et al. Recommendations for Policy and Practice of Telepsychotherapy and E-Mental Health in Europe and beyond. J. Psychother. Integrat. 2020, 30 (2), 160–173; https://doi.org/10.1037/int0000218.Search in Google Scholar
20. Grist, R.; Porter, J.; Stallard, P. Mental Health Mobile Apps for Preadolescents and Adolescents: A Systematic Review. J. Med. Internet Res. 2017, 19, e176; https://doi.org/10.2196/jmir.7332.Search in Google Scholar PubMed PubMed Central
21. Olff, M. Mobile Mental Health: A Challenging Research Agenda. Eur. J. Psychotraumatol. 2015, 6, 27882; https://doi.org/10.3402/ejpt.v6.27882.Search in Google Scholar PubMed PubMed Central
22. Qu, C.; Sas, C.; Roquet, C. D.; Doherty, G. Functionality of Top-Rated Mobile Apps for Depression: Systematic Search and Evaluation. JMIR Ment. Health 2020, 7, e15321; https://doi.org/10.2196/15321.Search in Google Scholar PubMed PubMed Central
23. Sanches, P.; Janson, A.; Karpashevich, P.; Nadal, C.; Qu, C.; Roquet, C. D. HCI and Affective Health Taking Stock of a Decade of Studies and Charting Future Research Directions. In Conference on Human Factors in Computing Systems – Proceedings; Association for Computing Machinery: Glasgow, Scotland, UK, 2019.10.1145/3290605.3300475Search in Google Scholar
24. Thieme, A.; Belgrave, D.; Doherty, G. Machine Learning in Mental Health: A Systematic Review of the HCI Literature to Support the Development of Effective and Implementable ML Systems. ACM Trans. Comput. Hum. Interact. 2020, 27, 1–53; https://doi.org/10.1145/3398069.Search in Google Scholar
25. Vaidyam, A. N.; Wisniewski, H.; Halamka, J. D.; Kashavan, M. S.; Torous, J. B. Chatbots and Conversational Agents in Mental Health: A Review of the Psychiatric Landscape. Can. J. Psychiatr. 2019, 64, 456–464; https://doi.org/10.1177/0706743719828977.Search in Google Scholar PubMed PubMed Central
26. Weizenbaum, J. Eliza–A Computer Program for the Study of Natural Language Communication. Commun. ACM 1966, 9, 36–45; https://doi.org/10.1145/365153.365168.Search in Google Scholar
27. Laranjo, L.; Dunn, A. G.; Tong, H. L.; Kocaballi, A. B.; Chen, J.; Bashir, R. Conversational Agents in Healthcare: A Systematic Review. J. Am. Med. Inf. Assoc. 2018, 25, 1248–1258; https://doi.org/10.1093/jamia/ocy072.Search in Google Scholar PubMed PubMed Central
28. Aguilera, A. Tecnología digital e intervenciones para la salud mental: Oportunidades y barreras. Arbor 2015, 191 (771), a210; https://doi.org/10.3989/arbor.2015.771n1012.Search in Google Scholar
29. Samantray, S. Efficacy of Digital Cognitive Behavior Therapy Intervention on Adults Enrolled in Mental Wellness Care Program on Mfine Application. World J. Adv. Res. Rev. 2023, 18 (3), 1159–1169; https://doi.org/10.30574/wjarr.2023.18.3.1179.Search in Google Scholar
30. Lewis, S.; Ainsworth, J.; Sanders, C.; Stockton-Powdrell, C.; Machin, M.; Whelan, P. Smartphone-enhanced Symptom Management in Psychosis: Open, Randomized Controlled Trial. J. Med. Internet Res. 2020, 22 (8), e17019; https://doi.org/10.2196/17019.Search in Google Scholar PubMed PubMed Central
31. Shahsavar, Y.; Choudhury, A. User Intentions to Use ChatGPT for Self-Diagnosis and Health-Related Purposes: Cross-Sectional Survey Study. JMIR Hum Factors [Internet] 2023, 10, e47564. Available from: https://humanfactors.jmir.org/2023/1/e47564.10.2196/47564Search in Google Scholar PubMed PubMed Central
32. Biswas, S. S. Role of Chat GPT in Public Health. Ann. Biomed. Eng. 2023, 51, 868–869; https://doi.org/10.1007/s10439-023-03172-7.Search in Google Scholar PubMed
33. Dingler, T.; Kwasnicka, D.; Wei, J.; Gong, E.; Oldenburg, B. The Use and Promise of Conversational Agents in Digital Health. Yearb. Med. Inform. 2021, 30 (1), 191–199; https://doi.org/10.1055/s-0041-1726510.Search in Google Scholar PubMed PubMed Central
34. Sallam, M., Snygg, J. ChatGPT Utility in Healthcare Education, Research, and Practice: Systematic Review on the Promising Perspectives and Valid Concerns. In Healthcare; MDPI: Switzerland, Vol. 11, 2023.10.3390/healthcare11060887Search in Google Scholar PubMed PubMed Central
35. Wang, C.; Liu, S.; Yang, H.; Guo, J.; Wu, Y.; Liu, J. Ethical Considerations of Using ChatGPT in Health Care. J. Med. Internet Res. 2023, 25, e48009; https://doi.org/10.2196/48009.Search in Google Scholar PubMed PubMed Central
36. Van Berkel, N.; Tag, B.; Goncalves, J.; Hosio, S. Human-Centred Artificial Intelligence: A Contextual Morality Perspective. Behav. Inf. Technol. 2022, 41, 502–518; https://doi.org/10.1080/0144929x.2020.1818828.Search in Google Scholar
37. Haas, G.; Gugenheimer, J.; Rixen, J. O.; Schaub, F.; Rukzio, E. ‘they like to Hear My Voice’: Exploring Usage Behavior in Speech-Based Mobile Instant Messaging. In Conference Proceedings – 22nd International Conference on Human-Computer Interaction with Mobile Devices and Services: Expanding the Horizon of Mobile Interaction, MobileHCI 2020; Association for Computing Machinery, Inc: Oldenburg, Germany, 2020.10.1145/3379503.3403561Search in Google Scholar
38. Sherman, L. E.; Michikyan, M.; Greenfield, P. M. The Effects of Text, Audio, Video, and In-Person Communication on Bonding between Friends. Cyberpsychol.: J. Psychosoc. Res. Cyberspace 2013, 7; https://doi.org/10.5817/cp2013-2-3.Search in Google Scholar
39. Bundesverband Digitale Wirtschaft (BVDW) e.V. BVDW-Studie: 69 Prozent der Deutschen verschicken Sprachnachrichten per Whatsapp & Co [Internet], 2019. [cited 2023 Jul 1]. Available from: https://www.bvdw.org/der-bvdw/news/detail/artikel/bvdw-studie-69-prozent-der-deutschen-verschicken-sprachnachrichten-per-whatsapp-co/.Search in Google Scholar
40. Nardi, B. A.; Whittaker, S.; Bradner, E. Interaction and Outeraction: Instant Messaging in Action. In Proceedings of the 2000 ACM conference on Computer supported cooperative work; Association for Computing Machinery: New York, NY, United States, 2000.10.1145/358916.358975Search in Google Scholar
41. Nummer gegen Kummer e.V. Presse [Internet], 2023. [cited 2023 Jun 25]. Available from: https://www.nummergegenkummer.de/aktuelles/presse/#studien.Search in Google Scholar
42. TelefonSeelsorge® Deutschland e.V. Unsere Statistiken [Internet], 2021. [cited 2023 Jun 25]. Available from: https://www.telefonseelsorge.de/unsere-statistiken.Search in Google Scholar
43. Hill, J.; Randolph Ford, W.; Farreras, I. G. Real Conversations with Artificial Intelligence: A Comparison between Human-Human Online Conversations and Human-Chatbot Conversations. Comput. Human Behav. 2015, 49, 245–250; https://doi.org/10.1016/j.chb.2015.02.026.Search in Google Scholar
44. Mitchell, E. G.; Maimone, R.; Cassells, A.; Tobin, J. N.; Davidson, P.; Smaldone, A. M. Automated vs. Human Health Coaching. Proc. ACM Hum. Comput. Interact. 2021, 5 (CSCW1), 1–37; https://doi.org/10.1145/3449173.Search in Google Scholar PubMed PubMed Central
45. MIT Massachusetts Institute of Technology. Young Adult Development Project [Internet], 2018. [cited 2023 Jun 25]. Available from: https://hr.mit.edu/static/worklife/youngadult/index.html.Search in Google Scholar
46. Bundesinstitut für Bevölkerungsforschung. Altersstruktur der Bevölkerung [Internet], 2022. [cited 2023 Jun 25]. Available from: https://www.demografie-portal.de/DE/Fakten/bevoelkerung-altersstruktur.html.Search in Google Scholar
47. El-Shinnawy, M.; Markus, M. L. The Poverty of Media Richness Theory: Explaining People’s Choice of Electronic Mail vs. Voice Mail. Int. J. Human-Comput. Stud. 1997, 46, 443–467; https://doi.org/10.1006/ijhc.1996.0099.Search in Google Scholar
48. Van Heyningen, T.; Honikman, S.; Tomlinson, M.; Field, S.; Myer, L. Comparison of Mental Health Screening Tools for Detecting Antenatal Depression and Anxiety Disorders in South African Women. PLoS One 2018, 13 (4), e0193697; https://doi.org/10.1371/journal.pone.0193697.Search in Google Scholar PubMed PubMed Central
49. Kessler, R. C.; Andrews, G.; Colpe, L. J.; Hiripi, E.; Mroczek, D. K.; Normand, S. L. T. Short Screening Scales to Monitor Population Prevalences and Trends in Non-specific Psychological Distress. Psychol. Med. 2002, 32 (6), 959–976; https://doi.org/10.1017/s0033291702006074.Search in Google Scholar PubMed
50. Sapra, A.; Bhandari, P.; Sharma, S.; Chanpura, T.; Lopp, L. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a Primary Care Setting. Cureus 2020, 12; https://doi.org/10.7759/cureus.8224.Search in Google Scholar PubMed PubMed Central
51. Spitzer, R. L.; Kroenke, K.; Williams, J. B. W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder the GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097; https://doi.org/10.1001/archinte.166.10.1092.Search in Google Scholar PubMed
52. Staples, L. G.; Dear, B. F.; Gandy, M.; Fogliati, V.; Fogliati, R.; Karin, E. Psychometric Properties and Clinical Utility of Brief Measures of Depression, Anxiety, and General Distress: The PHQ-2, GAD-2, and K-6. Gen. Hosp. Psychiatry 2019, 56, 13–18; https://doi.org/10.1016/j.genhosppsych.2018.11.003.Search in Google Scholar PubMed
53. Antonovsky, A. The Salutogenic Model as a Theory to Guide Health Promotion. Health Promot. Int. 1996, 11 (1), 11–18; https://doi.org/10.1093/heapro/11.1.11.Search in Google Scholar
54. Eriksson, M.; Lindström, B. A Salutogenic Interpretation of the Ottawa Charter. Health Promot. Int. 2008, 23, 190–199; https://doi.org/10.1093/heapro/dan014.Search in Google Scholar PubMed
55. Eriksson, M. The Sense of Coherence in the Salutogenic Model of Health. In The handbook of salutogenesis; Springer International Publishing: Cham, CH, 2017; pp 91–96.10.1007/978-3-319-04600-6_11Search in Google Scholar PubMed
56. Kivimäki, M.; Elovainio, M.; Vahtera, J.; Nurmi, J. E.; Feldt, T.; Keltikangas-Järvinen, L. Sense of Coherence as a Mediator between Hostility and Health Seven-Year Prospective Study on Female Employees. J. Psychosom. Res. 2002, 52, 239–247.10.1016/S0022-3999(01)00305-1Search in Google Scholar
57. Klepp, O. M.; Mastekaasa, A.; Sørensen, T.; Sandanger, I.; Kleiner, R. Structure Analysis of Antonovsky’s Sense of Coherence from an Epidemiological Mental Health Survey with a Brief Nine-Item Sense of Coherence Scale. Int. J. Methods Psychiatr. Res. 2007, 16 (1), 11–22; https://doi.org/10.1002/mpr.197.Search in Google Scholar PubMed PubMed Central
58. Lerdal, A.; Opheim, R.; Gay, C. L.; Moum, B.; Fagermoen, M. S.; Kottorp, A. Psychometric Limitations of the 13-item Sense of Coherence Scale Assessed by Rasch Analysis. BMC Psychol. 2017, 5 (1); https://doi.org/10.1186/s40359-017-0187-y.Search in Google Scholar PubMed PubMed Central
59. Lin, M.; Bieda, A.; Margraf, J. Short Form of the Sense of Coherence Scale (SOC-L9) in the US, Germany, and Russia Psychometric Properties and Cross-Cultural Measurement Invariance Test. Eur. J. Psychol. Assess. 2020, 36 (5), 796–804; https://doi.org/10.1027/1015-5759/a000561.Search in Google Scholar
60. Eysenbach, G. Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34; https://doi.org/10.2196/jmir.6.3.e34.Search in Google Scholar PubMed PubMed Central
61. World Medical Association. 13A chemin du Levant, 01210 Ferney-Voltaire. World Medical Association Declaration of Helsinki. JAMA [Internet] 2024. Available from: https://jamanetwork.com/journals/jama/fullarticle/2825290.Search in Google Scholar
62. da-Silva-Domingues, H.; del-Pino-Casado, R.; Palomino-Moral, P. Á.; López Martínez, C.; Moreno-Cámara, S.; Frías-Osuna, A. Relationship between Sense of Coherence and Health-Related Behaviours in Adolescents and Young Adults: a Systematic Review. BMC Public Health 2022, 22 (1); https://doi.org/10.1186/s12889-022-12816-7.Search in Google Scholar PubMed PubMed Central
63. Zhu, Y.; Wang, R.; Pu, C. “I Am Chatbot, Your Virtual Mental Health adviser.” what Drives Citizens’ Satisfaction and Continuance Intention toward Mental Health Chatbots during the COVID-19 Pandemic? an Empirical Study in China. Digit Health 2022, 8; https://doi.org/10.1177/20552076221090031.Search in Google Scholar PubMed PubMed Central
64. Abd-alrazaq, A. A.; Alajlani, M.; Alalwan, A. A.; Bewick, B. M.; Gardner, P.; Househ, M. An Overview of the Features of Chatbots in Mental Health: A Scoping Review. Int. J. Med. Inf. 2019, 132; https://doi.org/10.1016/j.ijmedinf.2019.103978.Search in Google Scholar PubMed
65. Jalnapurkar, I.; Allen, M.; Pigott, T. Sex Differences in Anxiety Disorders: A Review. Psychiatry, Depress. Anxiety 2018, 4, 3–16.10.24966/PDA-0150/100011Search in Google Scholar
66. Sweeney, C.; Potts, C.; Ennis, E.; Bond, R.; Mulvenna, M. D.; O’Neill, S. Can Chatbots Help Support a Person’s Mental Health? Perceptions and Views from Mental Healthcare Professionals and Experts. ACM Trans. Comput. Healthc. 2021, 2 (3), 1–15; https://doi.org/10.1145/3453175.Search in Google Scholar
67. Palanica, A.; Flaschner, P.; Thommandram, A.; Li, M.; Fossat, Y. Physicians’ Perceptions of Chatbots in Health Care: Cross-Sectional Web-Based Survey. J. Med. Internet Res. 2019, 21 (4), e12887; https://doi.org/10.2196/12887.Search in Google Scholar PubMed PubMed Central
68. Lukas, C. A Study about Distribution and Acceptance of Conversational Agents for Mental Health in Germany: Keep the Human in the Loop? 2025. Available from: http://arxiv.org/abs/2502.00005.Search in Google Scholar
69. Reddy, S.; Allan, S.; Coghlan, S.; Cooper, P. A Governance Model for the Application of AI in Health Care. J. Am. Med. Inf. Assoc. 2020, 27, 491–497; https://doi.org/10.1093/jamia/ocz192.Search in Google Scholar PubMed PubMed Central
70. Elendu, C.; Amaechi, D. C.; Elendu, T. C.; Jingwa, K. A.; Okoye, O. K.; John, O. M. Ethical implications of AI and Robotics in Healthcare: A Review. Vol. 102, Medicine (United States); Lippincott Williams and Wilkins: Philadelphia, Pennsylvania, USA, 2023; p E36671.10.1097/MD.0000000000036671Search in Google Scholar PubMed PubMed Central
71. Hee Lee, D.; Yoon, S. N. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int. J. Environ. Res. Public Health 2021, 18 (1), 1–18; https://doi.org/10.3390/ijerph18010271.Search in Google Scholar PubMed PubMed Central
72. White-Williams, C.; Oetjen, D. An Ethical Analysis of Telemedicine: Implications for Future Research. J. Telemed. Clin. Pract. 2015, 1 (1), 4–16; https://doi.org/10.1504/ijtmcp.2015.069470.Search in Google Scholar
73. Tang, L.; Li, J.; Fantus, S. Medical Artificial Intelligence Ethics: A Systematic Review of Empirical Studies. Digital Health 2023, 9; https://doi.org/10.1177/20552076231186064.Search in Google Scholar PubMed PubMed Central
74. Müller, H.; Mayrhofer, M. T.; Van Veen, E. B.; Holzinger, A. The Ten Commandments of Ethical Medical AI. Computer (Long Beach Calif) 2021, 54, 119–123; https://doi.org/10.1109/mc.2021.3074263.Search in Google Scholar
75. Gerhardt, U.; Breitschwerdt, R.; Thomas, O. Relapse Prevention in Drug Addiction: Addressing a Messy Problem by IS Action Research. AI Soc. 2015, 30 (1), 31–43; https://doi.org/10.1007/s00146-014-0544-9.Search in Google Scholar
76. Guo, C.; Deng, M.; Yu, M. Interventions Based on Salutogenesis for Older Adults: An Integrative Review. J. Clin. Nurs. 2024, 33, 2456–2475; https://doi.org/10.1111/jocn.17028.Search in Google Scholar PubMed
77. Fekete, O. R.; Kinn, L. G.; Larsen, T. M. B.; Langeland, E. Salutogenesis as a Theoretical Framework for Psychosocial Rehabilitation: the Case of the Clubhouse Model. Int. J. Qual. Stud. Health Well-being 2020, 15 (1), 1748942; https://doi.org/10.1080/17482631.2020.1748942.Search in Google Scholar PubMed PubMed Central
78. Gerhardt, U.; Breitschwerdt, R.; Thomas, O. Engineering Sustainable mHealth: the Role of Action Research. AI Soc. 2017, 32 (3), 339–357; https://doi.org/10.1007/s00146-015-0640-5.Search in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.