Immersive learning in dentistry — evaluating dental students’ perceptions of virtual reality for crown preparation skill development: a multi-institution study
-
Lamyia Anweigi
Abstract
Objectives
To explore and compare student perceptions of virtual reality dental simulation (VRDS) with haptic feedback in preclinical prosthodontics at two dental institutions.
Methods
A cross-sectional exploratory study investigated the impact of VRDS for crown preparations in two dental schools. Purposive sampling targeted third-year undergraduate dental students; 181 were included in analysis. All students performed crown preparation exercises on the mandibular first molar on both the VRDS and acrylic teeth on dental mannequins. A pre-piloted questionnaire was used to evaluate the participants’ perceptions and experiences.
Results
Participants’ mean score was (0.448 ± 0.086). Analysis of variance confirmed significant differences in participants’ scores by location (p<0.001). The key benefits of the VRDS included the convenience of repeating exercises, haptic feedback, cost-effectiveness, and improved confidence. Main limitations were related to handling of virtual reality equipment and less realistic experience than when working with natural teeth.
Conclusions
This study provides useful insights into the learning experiences of undergraduate students regarding crown preparation using a VRDS. These findings support the use of the VRDS to introduce tooth preparation skills in a risk-free environment.
Introduction
Undergraduate dental education involves training dental students to perform irreversible and invasive dental procedures on real patients supervised by dental faculty [1]. To protect patients, simulated dental learning environments provide a safe space for learning and consolidating operative skills [2], [3], [4]. Once students can demonstrate their competence in performing operative procedures on mannequins, they may be allowed to develop their skills in clinical settings [5], 6]. Undergraduate students typically consider tooth preparation for crown and bridge work challenging, requiring considerable technical expertise, spatial orientation, hand–eye coordination, and application of geometrical principles while protecting the adjacent teeth and soft tissues [7], [8], [9], [10], [11].
Clinical dental training plays a crucial role in developing core clinical competencies for providing safe and effective dental care [12], [13], [14]. Dental students typically begin their clinical skill training by treating live patients under the guidance and supervision of experienced clinical tutors. They are expected to attain proficiency in various operative procedures to ensure safe and effective delivery of clinical dental care [10], 11], 13], 15]. This involves invasive procedures that, if performed incorrectly, can cause irreversible harm to patients. To mitigate these risks, a fundamental strategy in dental education is to provide preclinical training in simulated dental learning environments. Simulated settings offer a secure learning space and are essential for training students in irreversible dental procedures before they progress to real clinical settings [6].
To bridge the gap between preclinical dental education and real clinical practice, simulation laboratories have emerged as a vital component. These laboratories provide a pivotal transition from theoretical learning to hands-on clinical care. Traditionally, training in simulated dental learning environments involves mannequins and physical jaw models to teach manual dexterity and core practical skills. However, a notable disparity remains between the psychomotor skills acquired in preclinical dental education and the demands of real clinical situations [5].
As technology continues to advance, virtual simulation training is increasingly emphasized, offering a promising solution for enhancing dental education and training. Virtual reality dental simulation (VRDS) with haptic feedback is gaining popularity in dental schools and has the potential to address some of the limitations associated with traditional teaching using mannequins [2], 5], 16]. This technology provides an immersive learning experience, enabling dental students to practice and refine their skills in a virtual, yet highly authentic, clinical environment. Beyond receiving haptic feedback during exercises, students benefit from the opportunity for repeated practice at no additional cost [3]. Additionally, they gain immediate access to multi-dimensional feedback, including audio; written assessments; and three-dimensional insights into their work involving artificial teeth (such as cavities, crowns, and endodontic access preparations) [17], 18]. By leveraging these technological advancements, dental educators can prepare future practitioners to deliver safe and effective care [19].
Multiple studies have assessed the validity and effectiveness of VRDS technology. A previous study showed overall improved performance in psychomotor skills evidenced by improved cavity preparation scores and cavity design features and less time for cavity preparation after haptic virtual reality (VR) simulation training [5]. Virtual simulation training has also been shown to be effective in training dental students on inlay preparations followed by further training on mannequins [20]. Other studies have highlighted the use of VRDS to complement conventional methods of preclinical training in simulated laboratory settings [21], [22], [23].
The literature shows that many strategies have been employed in teaching preclinical fixed prosthodontics, encompassing both theoretical and practical teachings related to preparing teeth for crowns and fixed partial dentures. Traditionally, various parameters, such as occlusal reduction, axial reduction, two-plane reduction, taper, margin placement, finishing, preservation of adjacent teeth, and time management for optimal tooth preparation, have been assessed visually. It is challenging for faculty members to teach students to correctly visualise all parameters together during their consolidation sessions [23]. This has recently been addressed by advanced assessment techniques such as computer-assisted design/computer-assisted manufacturing (CAD/CAM) and VR-based systems [24]. Crown preparation assessment software has been reported to potentially accelerate dental students’ learning and benefit their expertise in achieving optimal parameters for crown preparation [25]. Integrating CAD/CAM technology within preclinical dentistry – specifically, utilising taper and undercut tools within the prepCheck learning system for assessing tooth preparation – has been shown to be beneficial [25]. Research has revealed a correlation between students’ perceptions of prepCheck and their performance in preclinical prosthodontics, suggesting a positive relationship between students’ perception of the technology and their actual performance in these dental exercises [24].
However, deeper exploration is needed to comprehend how the relationship between traditional preclinical prosthodontic teaching using mannequins and the integration of VR affects undergraduate dental students’ learning journeys. This study aimed to explore and compare student perceptions of VRDS with haptic feedback in preclinical prosthodontics at two dental institutions.
Materials and methods
Research ethics
Ethical approval was obtained from the Institutional Review Board of Qatar University (reference number: QU-IRB 1652-EA/22). Participation was voluntary, and students who declined to participate were not disadvantaged in any way. All participants provided informed consent before responding to the questionnaire. All data were recorded, stored, and processed anonymously to prevent the identification of individual participants.
Study design
This multi-institution study was conducted at Qatar University (Qatar) and Ankara University (Türkiye) in dental simulation laboratory settings. A cross-sectional exploratory study design was used to investigate the effects of VR dental haptics on crown preparation. The students performed crown preparation on the mandibular first molar using SIMtoCare (Vreeland, Netherlands) and Simodont VR (Nissin Dental Products, Kyoto, Japan) dental haptic simulators.
Sampling technique and participants
A nonrandomized selective sampling technique was used to target third-year undergraduate dental students at two universities. Undergraduate dental students who had completed training in crown preparation using both the VRDS and conventional training on dental mannequins at the participating institutions were eligible to participate. Students who were repeating the course or had interrupted their study were excluded. Invitations to participate in the research, along with information sheets explaining the purpose and scope of the study, were sent to all participants through institutional e-mail.
Research instrument
Four experienced clinical dental academics on the study team drafted the English questionnaire. The questionnaire consisted of 10 closed-ended items based on a Likert scale consisting of five categories: strongly agree, agree, unsure, disagree, and strongly disagree (scored as 2, 1, 0, −1, and −2, respectively). In addition, three open-ended items were used to evaluate students’ perceptions of and experiences related to the VRDS. The questionnaire focused on the learning experiences of the undergraduate students in developing their competencies in crown preparation using conventional techniques and dental haptics.
The face and content validity of the items was specified through a detailed comparison between the essence themes related to the learning outcomes of crown preparation. The questionnaire was developed to eliminate biases related to personal factors by implementing the following strategies:
Ensured recall of relevant skills and behaviors was easy for the respondents;
Allowed blind reporting by the participants so that they felt confident in disclosing information. Moreover, researchers did not influence their responses.
Items were pre-tested according to established practices to generate potential questionnaire items. An electronic pre-test questionnaire was sent to undergraduate dental students (n=5) and dental academics (n=5). The purpose of this pretesting was to determine the content and face validity of scale items, the clarity and consistent interpretation of the questionnaire by the participants, and the clarity of the scoring categories.
The final questionnaire consisted of 10 closed-ended questions based on a five-point Likert scale: strongly disagree, disagree, uncertain, agree, and strongly agree (See Table 1). In addition, three open-ended items were used to explore participants’ views regarding the benefits and limitations of the VRDS and recommendations for future improvements.
Descriptive values (all respondents).
| No. | Question | Mean | SD | 95 % CI (lower limit) | 95 % CI (upper limit) |
|---|---|---|---|---|---|
| 1 | The case presentation on VR allowed me to clearly comprehend the tasks expected from me | 0.52 | 0.83 | 0.40 | 0.64 |
| 2 | The hardness and texture of teeth in the VR models are similar to natural teeth | 0.43 | 0.92 | 0.30 | 0.57 |
| 3 | The hardness and texture of teeth in the VR models are similar to artificial teeth | −0.09 | 1.01 | −0.24 | 0.05 |
| 4 | The anatomical structures on VR accurately simulated real structures | 0.69 | 0.89 | 0.56 | 0.82 |
| 5 | Tooth preparation on VR was easier compared to artificial teeth on mannequin | −0.18 | 1.14 | −0.35 | −0.01 |
| 6 | The training exercise on VR improved my fine motor skills | 0.71 | 0.98 | 0.56 | 0.85 |
| 7 | Training on the VR improved my confidence in learning tooth preparation | 0.50 | 1.00 | 0.36 | 0.65 |
| 8 | VR training may be used to supplement standard preclinical training on artificial teeth on mannequin models | 1.02 | 0.85 | 0.90 | 1.15 |
| 9 | VR can replace the preclinical fixed prosthodontics training on mannequins and models | −0.12 | 1.25 | −0.30 | 0.07 |
| 10 | I would like to have more VR sessions in fixed prosthodontics | 1.00 | 1.07 | 0.84 | 1.16 |
| Overall | 0.448 | 1.086 | 0.289 | 0.607 | |
-
VR, virtual reality; SD, standard deviation; CI, confidence interval.
Data collection
Students performed crown preparation in the mandibular first molar using SIMtoCare at Qatar University and Ankara University in Türkiye. Students used Simodont VR dental haptics to perform the same exercise. Both systems provide haptic feedback. Subsequently, the students carried out full ceramic crown preparation on the mandibular first molar using mannequin‐based phantom head and acrylic typodont teeth (Frasaco, ANKA-4 Z, Tettnang, Germany).
After completing the learning activities, participants completed an online questionnaire using Google Forms.
Data analysis
All data were analyzed and visualized using R Studio software (version 2023.06.2), incorporating R (version 4.0.5). Descriptive statistics, including confidence intervals, were calculated for each closed-ended item and the combined dataset. Analysis of variance (ANOVA) was used to determine any significant variation in results by location. The estimated marginal means were calculated from the ANOVA results. The responses to the open-ended items were analyzed thematically.
Results
A total of 181 participants participated in this study. Of the 164 students in Türkiye, 152 participated, and 29 of the 37 students in Qatar participated, yielding response rates of 92.68 % and 78.37 %, respectively.
Descriptive statistics
Descriptive values for individual items are summarized in Table 1.
The mean score for all items was 0.448 (95 % confidence interval [CI]: 0.289–0.607), indicating positive perceptions and experiences with the VRDS overall. The presentation on the VRDS allowed the participants to be clear about the tasks expected of them. The VR experience improved participants’ motor skills and confidence, and they considered it a useful supplement to training on physical models mounted on mannequins. The participants also indicated a preference for more consolidation sessions using the VRDS. However, the participants did not feel that the texture and hardness of the teeth in the VRDS accurately simulated artificial teeth, and they did not consider it suitable for completely replacing training on crown preparations using teeth mounted on physical models.
The descriptive values for each item by location are summarized in Table 2 and depicted in Figure 1.
Descriptive values by location.
| Question | Mean | SD | 95 % CI (lower limit) | 95 % CI (upper limit) | ||||
|---|---|---|---|---|---|---|---|---|
| Qatar | Türkiye | Qatar | Türkiye | Qatar | Türkiye | Qatar | Türkiye | |
| 1 | 0.45 | 0.53 | 1.06 | 0.78 | 0.06 | 0.41 | 0.83 | 0.66 |
| 2 | −0.28 | 0.57 | 1.13 | 0.81 | −0.69 | 0.44 | 0.14 | 0.70 |
| 3 | −0.83 | 0.05 | 0.89 | 0.98 | −1.15 | −0.11 | −0.50 | 0.20 |
| 4 | 0.34 | 0.76 | 1.11 | 0.83 | −0.06 | 0.62 | 0.75 | 0.89 |
| 5 | −1.03 | −0.02 | 0.98 | 1.10 | −1.39 | −0.20 | −0.67 | 0.16 |
| 6 | 0.03 | 0.84 | 1.15 | 0.89 | −0.39 | 0.69 | 0.46 | 0.98 |
| 7 | 0.00 | 0.60 | 1.22 | 0.93 | −0.45 | 0.45 | 0.45 | 0.75 |
| 8 | 0.48 | 1.13 | 1.18 | 0.73 | 0.05 | 1.01 | 0.92 | 1.24 |
| 9 | −1.38 | 0.13 | 0.86 | 1.16 | −1.70 | −0.06 | −1.06 | 0.31 |
| 10 | −0.17 | 1.22 | 1.36 | 0.84 | −0.67 | 1.09 | 0.33 | 1.36 |
| Overall | −0.238 | 0.579 | 1.249 | 1.000 | −0.421 | 0.432 | 0.055 | 0.726 |
-
SD, standard deviation; CI, confidence interval.
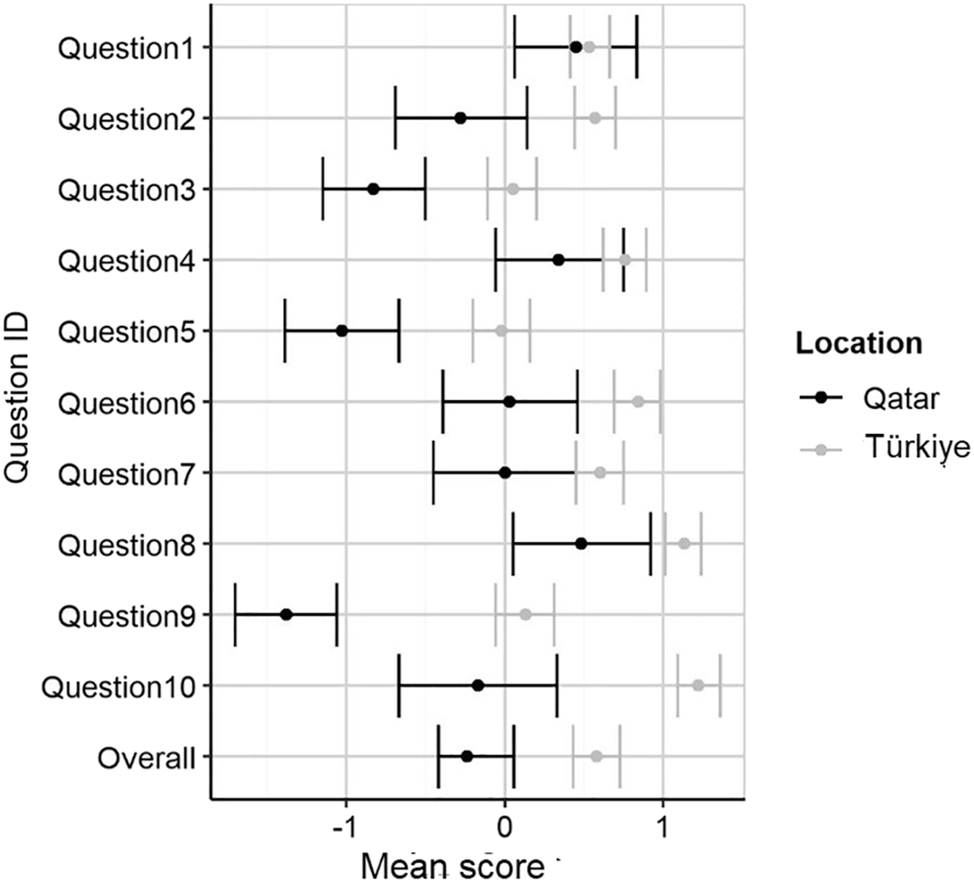
Distribution of scores by location.
The adjusted mean score was −0.24 for the participants based in Qatar and 0.58 for those in Türkiye, indicating less positive overall perceptions and experiences of participants in Qatar. An ANOVA confirmed significant variation in participants’ scores by location (p<0.001), as summarized in Table 3.
Analysis of variance in participants’ scores (all questions).
| Factor | Df | Sum of Sq | RSS | AIC | F-statistic | p-Value |
|---|---|---|---|---|---|---|
| Location | 1 | 162.509 | 2,131.618 | 298.034 | 149.213 | <0.001 |
-
Df, degree of freedom; RSS, residual sum of squares; AIC, akaike information criterion.
Responses to open-ended questions
The responses to the open-ended questions were analyzed thematically. They were collated and read systematically to identify recurring patterns. The relevant sections of the texts were coded and grouped into primary themes (subthemes), and related elements were then combined into higher-level themes.
The first open-ended question related to the advantages of the VRDS, and the participants’ responses highlighted the diverse benefits of VR in enhancing the learning experiences of dental students. The key benefits included the convenience of repeating the exercises to consolidate technical skills, haptic feedback, cost-effectiveness, and improved confidence. Participants from both institutions highlighted these benefits. These themes are summarized in Table 4.
Benefits of virtual reality dental simulation (VRDS) training on crown preparations.
| Theme | Subthemes | Frequencya |
|---|---|---|
| Opportunities for repeated practice in a low-risk environment |
|
++++ |
| Haptic feedback |
|
+++ |
| Low operational cost |
|
+++ |
-
aEach + represents 10 % of participants.
The participants also highlighted some limitations and challenges of learning crown preparations in the VRDS compared with artificial/natural teeth mounted on physical models in mannequins. The key themes related to the handling of VR equipment, a less realistic experience compared to tooth preparations on natural teeth, and the limited availability of VR stations are summarized in Table 5. While the participants from both institutions identified these challenges, those from Qatar highlighted them more frequently. In particular, participants from Qatar expressed frustration over the limited time for consolidation and a lack of arrangements to practice their skills after hours.
Limitations and challenges of virtual reality dental simulation (VRDS) training on crown preparations.
| Theme | Subthemes | Frequencya |
|---|---|---|
| Challenges related to the use of VR equipment |
|
++++ |
| Unrealistic experience |
|
+++ |
| Limited number of VR stations |
|
++ |
-
aEach + represents 10 % of participants. VR, virtual reality.
Discussion
The current multi-institutional study involving over 181 undergraduate students is among the few studies exploring the learning experiences of dental students on crown preparations on virtual teeth along with acrylic teeth mounted on dental models [26], [27], [28], [29]. Although the participating institutions used different VRDS systems, the exercises performed by the participants were similar. Both VRDS also simulated dental tissues and incorporated a touchscreen, dental handpiece, burs space mouse, dental mirror, and speed pedal. Overall, the participants reported positive perceptions and experiences of the VRDS training, suggesting the use of the VRDS to complement the conventional methods of preclinical training in simulated laboratory preclinical training using acrylic and natural teeth. These findings agree with those of other studies that recommend VRDS as an adjunct rather than an alternative to conventional phantom head simulators [19], 22].
The rationale for including two dental institutions was to compare the learning experiences of students in institutions with different ages and geographical locations. Significant differences in the perceptions and experiences of the participants between the participating institutions were observed, with participants from Türkiye reporting more positive experiences [22]. A previous study on endodontic training at the same institution reported similar findings. A multitude of factors could potentially influence the participants’ learning experiences.
The institution in Türkiye was established more than 70 years ago and is a much larger institution with an annual intake of 200 dental students. With its longstanding institutional history, Türkiye has a strong culture of peer tutoring and learning, which facilitates the transfer of knowledge and skills both vertically (from senior students) and horizontally (among peers of the same cohort). The diverse body of students, along with a large academic faculty, contributes significantly to social interactions among students in the learning environment, allowing them greater opportunities to learn from each other and provide peer support.
The College of Dental Medicine in Qatar, on the other hand, was founded only five years ago and has space for a maximum of 35 students annually. It is still in its formative years and requires time to build an institutional memory. Another reason for the less positive learning experiences of participants from Qatar relates to limited consolidation time, as current institutional policies do not permit student access to dental simulation laboratories after working hours. Many dental institutions allow students to practice in a simulation laboratory around the clock, and the dental faculty must work on suitable options to increase the availability of the laboratory to students.
The VRDS technology offers several benefits, and the findings of the current study support its use in providing an immersive experience to novice students in a non-threatening learning environment. Dental education and training are provided in a wide variety of settings, and students learn from social interactions with their peers [30], 31]. Learning operative dental techniques in simulated dental learning environments facilitates legitimate peripheral participation of students and enables them to develop into safe and competent clinicians [30]. This allows for repeated practice and consolidation of skills in a risk-free environment, reducing the need for dental consumables, and promoting a green environment [32]. VRDS enables dental students to refine their skills without having to replace the models, eliminating the possibility of irreversible damage to teeth or vital tissue structures. There is no risk of irreversible damage to teeth or vital tissue structures. Beyond receiving haptic feedback during exercises, students benefit from the opportunity for repeated practice at no additional cost, which is in agreement with previous studies [2], 20], 21]. Notwithstanding the initial cost of purchasing the VRDS equipment, the reduced need for direct faculty supervision is an additional benefit of the VRDS, as reported in previous studies [21], 33], 34].
In the current study, most participants did not consider VRDS training to have the potential to replace conventional dental mannequin training in a preclinical laboratory setting. The main limitation is the differences in the texture and hardness of virtual teeth in the VRDS compared to natural teeth. This issue has also been reported in previous studies [4], which call for dental educators to work with manufacturers to improve the quality of haptic feedback in VRDS to simulate the tactile feedback experienced in the preparation of natural teeth. Additionally, the participants in the current study recommended ergonomic improvements to the design of the VRDS equipment to optimize the visual clarity and control of virtual instruments, such as the handpiece, rest support, and dental mirror. The proposed enhancements aim to further enrich the learning experience and effectiveness of VRDS training. Although the VRDS is unlikely to replace conventional training on physical models in the near future, there is merit to using the VRDS to familiarize students with core dental operative procedures in a safe environment. This may be followed by further training on physical models using a combination of artificial and natural teeth [4], 5], 20]. It is recommended that VRDS be introduced early in the curriculum to provide additional time for students to consolidate their skills.
Another exciting development is the use of patient-centered VR training to enable students to prepare for the requirements of their patients and practice them in VR before attempting them in real life [35]. Such innovations have potential to contribute positively to the learning experiences and confidence of students [36].
The initial financial cost of purchasing VRDS pods is a recognized barrier limiting its widespread use in dental education, particularly in developing countries [22]. As highlighted in the present study, most students expressed the need for additional practice on VRDS. However, the financial cost of the VRDS means that most dental institutions can purchase only a limited number of VRDS pods. This often restricts the consolidation time available to students to improve their technical skills, and dental institutions must work with the industry to reduce the financial cost of purchasing VRDS [25].
This study had some limitations. It explored students’ perceptions and experiences of using the VRDS but did not capture the longitudinal performance of students throughout the course. Moreover, the findings were based on a single exercise in crown preparation using both the VRDS and physical models with artificial teeth. Future studies should collect longitudinal data to explore whether the VRDS provides added value to enhance the translation of students’ crown preparation skills in clinical settings. Nevertheless, this study provided a useful comparison of students’ learning experiences with crown preparation using the VRDS.
Conclusions
This research offers valuable insights into the effectiveness of VRDS for preclinical prosthodontic training in undergraduate dental education and identifies its merits, challenges, and limitations. The results underscore the need to integrate the VRDS with traditional approaches in simulated laboratory environments for preclinical training. Additionally, the recommendations provided by the participants can be helpful in further developing VRDS technology to enhance students’ future learning experiences. It is imperative for dental educators to collaborate closely with manufacturers to optimize the VRDS for undergraduate dental education and expand its use in dental education.
Acknowledgments
The authors would like to acknowledge the dental students and supervisors for their participation in this study. Open access funding for this study was provided by the Qatar National Library.
-
Research ethics: Ethical approval was obtained from the Institutional Review Board Qatar University. (Reference number: QU-IRB 1652-EA/22).
-
Informed consent: Informed consent obtained from all participants.
-
Author contributions: Conceptualization, methodology, and study supervision: Kamran Ali, Lamyia Anweigi, Kaan Orhan. Data Collection: Nidhi Gupta, Fehmi Gonuldas, Dilek Yigit, Hanin Das, Raidan Ba Hattab. Formal analysis: Rebecca Glanville. Corresponding and Senior Author: Kamran Ali. All authors reviewed and approved the manuscript.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: All other authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The data underlying this study is available from the authors on a reasonable request.
References
1. Ali, K, Raja, M, Watson, G, Coombes, L, Heffernan, E. The dental school learning milieu: students’ perceptions at five academic dental institutions in Pakistan. J Dent Educ 2012;76:487–94. https://doi.org/10.1002/j.0022-0337.2012.76.4.tb05281.x.Search in Google Scholar
2. Mirghani, I, Mushtaq, F, Allsop, MJ, Al-Saud, LM, Tickhill, N, Potter, C, et al.. Capturing differences in dental training using a virtual reality simulator. Eur J Dent Educ 2018;22:67–71. https://doi.org/10.1111/eje.12245.Search in Google Scholar PubMed
3. Rhienmora, P, Haddawy, P, Khanal, P, Suebnukarn, S, Dailey, MN. A virtual reality simulator for teaching and evaluating dental procedures. Methods Inf Med 2010;49:396–405. https://doi.org/10.3414/ME9310.Search in Google Scholar PubMed
4. Daud, A, Matoug-Elwerfelli, M, Daas, H, Zahra, D, Ali, K. Enhancing learning experiences in pre-clinical restorative dentistry: the impact of virtual reality haptic simulators. BMC Med Educ 2023;23:948. https://doi.org/10.1186/s12909-023-04904-y.Search in Google Scholar PubMed PubMed Central
5. Farag, A, Hashem, D. Impact of the haptic virtual reality simulator on dental students’ psychomotor skills in preclinical operative dentistry. Clin Pract 2022;12:17–26. https://doi.org/10.3390/clinpract12010003.Search in Google Scholar PubMed PubMed Central
6. Cheng, HC, Yen, AMF, Lee, YH. Factors affecting patient safety culture among dental healthcare workers: a nationwide cross-sectional survey. J Dent Sci 2019;14:263–8. https://doi.org/10.1016/j.jds.2018.12.001.Search in Google Scholar PubMed PubMed Central
7. Liu, L, Li, J, Yuan, S, Wang, T, Chu, F, Lu, X, et al.. Evaluating the effectiveness of a preclinical practice of tooth preparation using digital training system: a randomised controlled trial. Eur J Dent Educ 2018;22:e679–86. https://doi.org/10.1111/eje.12378.Search in Google Scholar PubMed
8. Seet, RH, Soo, PR, Leong, KJM, Pang, JJH, Lee, FKF, Tan, MY. Crown preparations by undergraduate dental students: a comparison of conventional versus digital assessment via an intraoral scanner. J Dent Educ 2020;84:1303–13. https://doi.org/10.1002/jdd.12285.Search in Google Scholar PubMed
9. Ali, K, Cockerill, J, Zahra, D, Qazi, HS, Raja, U, Ataullah, K. Self-perceived preparedness of final year dental students in a developing country – A multi-institution study. Eur J Dent Educ 2018;22:e745–50. https://doi.org/10.1111/eje.12389.Search in Google Scholar PubMed
10. Mat Yudin, Z, Ali, K, Wan Ahmad, WMA, Ahmad, A, Khamis, MF, Brian Graville Monteiro, NA, et al.. Self-perceived preparedness of undergraduate dental students in dental public universities in Malaysia: a national study. Eur J Dent Educ 2020;24:163–8. https://doi.org/10.1111/eje.12480.Search in Google Scholar PubMed
11. Javed, MQ, Abulhamael, AM, Ahmad, Z, Muhammad, M, Faridi, MA, Khan, KI, et al.. Self-reported preparedness of final year undergraduate dental students and interns in Saudi Arabia: a multi-institutional study. BMC Med Educ 2024;24:282. https://doi.org/10.1186/s12909-024-05246-z.Search in Google Scholar PubMed PubMed Central
12. Javed, MQ, Nawabi, S, Bhatti, UA, Atique, S, AlAttas, MH, Abulhamael, AM, et al.. How well prepared are dental students and new graduates in Pakistan-a cross-sectional national study. Int J Environ Res Public Health 2023;20:1506. https://doi.org/10.3390/ijerph20021506.Search in Google Scholar PubMed PubMed Central
13. Ali, K, Slade, A, Kay, E, Zahra, D, Tredwin, C. Preparedness of undergraduate dental students in the United Kingdom: a national study. Br Dent J 2017;222:472–7. https://doi.org/10.1038/sj.bdj.2017.272.Search in Google Scholar PubMed
14. Mariño, R, Delany, C, Manton, DJ, Reid, K, Satur, J, Crombie, F, et al.. Preparedness for practice of newly qualified dental practitioners in the Australian context: an exploratory study. BMC Med Educ 2022;22:625, https://doi.org/10.1186/s12909-022-03684-1.Search in Google Scholar PubMed PubMed Central
15. Ali, K, Slade, A, Kay, EJ, Zahra, D, Chatterjee, A, Tredwin, C. Application of Rasch analysis in the development and psychometric evaluation of dental undergraduates preparedness assessment scale. Eur J Dent Educ 2017;21:e135–41. https://doi.org/10.1111/eje.12236.Search in Google Scholar PubMed
16. Yang, PY, Chang, YC. The haptic 3D virtual reality dental training simulator as a good educational tool in preclinical simulation learning. J Dent Sci 2022;17:618–19. https://doi.org/10.1016/j.jds.2021.10.016.Search in Google Scholar PubMed PubMed Central
17. Monterubbianesi, R, Tosco, V, Vitiello, F, Orilisi, G, Fraccastoro, F, Putignano, A, et al.. Augmented, virtual and mixed reality in dentistry: a narrative review on the existing platforms and future challenges. Appl Sci (Switzerland) 2022;12:877. https://doi.org/10.3390/app12020877.Search in Google Scholar
18. Gottlieb, R, Lanning, SK, Gunsolley, JC, Buchanan, JA. Faculty impressions of dental students’ performance with and without virtual reality simulation. J Dent Educ 2011;75:1443–51. https://doi.org/10.1002/j.0022-0337.2011.75.11.tb05201.x.Search in Google Scholar
19. Gal, GB, Weiss, EI, Gafni, N, Ziv, A. Preliminary assessment of faculty and student perception of a haptic virtual reality simulator for training dental manual dexterity. J Dent Educ 2011;75:496–504. https://doi.org/10.1002/j.0022-0337.2011.75.4.tb05073.x.Search in Google Scholar
20. Sheng, J, Zhang, C, Gao, Z, Yan, Y, Meng, Y, Ren, S, et al.. Virtual versus jaw simulation in inlay preparation preclinical teaching: a randomised controlled trial. BMC Med Educ 2022;22:841. https://doi.org/10.1186/s12909-022-03930-6.Search in Google Scholar PubMed PubMed Central
21. Philip, N, Ali, K, Duggal, M, Daas, H, Nazzal, H. Effectiveness and student perceptions of haptic virtual reality simulation training as an instructional tool in pre-clinical paediatric dentistry: a pilot pedagogical study. Int J Environ Res Public Health 2023;20:4226. https://doi.org/10.3390/ijerph20054226.Search in Google Scholar PubMed PubMed Central
22. Ba-Hattab, R, Helvacioglu-Yigit, D, Anweigi, L, Alhadeethi, T, Raja, M, Atique, S, et al.. Impact of virtual reality simulation in endodontics on the learning experiences of undergraduate dental students. Appl Sci (Switzerland) 2023;13:981. https://doi.org/10.3390/app13020981.Search in Google Scholar
23. Mays, KA, Crisp, HA, Vos, P. Utilizing CAD/CAM to measure total occlusal convergence of preclinical dental students’ crown preparations. J Dent Educ 2016;80:100–7. https://doi.org/10.1002/j.0022-0337.2016.80.1.tb06063.x.Search in Google Scholar
24. Park, CF, Sheinbaum, JM, Tamada, Y, Chandiramani, R, Lian, L, Lee, C, et al.. Dental students’ perceptions of digital assessment software for preclinical tooth preparation exercises. J Dent Educ 2017;81:597–603. https://doi.org/10.21815/jde.016.015.Search in Google Scholar
25. Tiu, J, Cheng, E, Hung, T-C, Yu, C-C, Lin, T, Schwass, D, et al.. Effectiveness of crown preparation assessment software as an educational tool in simulation clinic: a pilot study. J Dent Educ 2016;80:1004–11. https://doi.org/10.1002/j.0022-0337.2016.80.8.tb06181.x.Search in Google Scholar
26. Suebnukarn, S, Phatthanasathiankul, N, Sombatweroje, S, Rhienmora, P, Haddawy, P. Process and outcome measures of expert/novice performance on a haptic virtual reality system. J Dent 2009;37:658–65. https://doi.org/10.1016/j.jdent.2009.04.008.Search in Google Scholar PubMed
27. Wang, F, Liu, Y, Tian, M, Zhang, Y, Zhang, S, Chen, J. Application of a 3D haptic virtual reality simulation system for dental crown preparation training. In: Proceedings – 2016 8th international conference on information technology in medicine and education, ITME 2016; 2017.10.1109/ITME.2016.0101Search in Google Scholar
28. Liu, L, Zhou, R, Yuan, S, Sun, Z, Lu, X, Li, J, et al.. Simulation training for ceramic crown preparation in the dental setting using a virtual educational system. Eur J Dent Educ 2020;24:199–206. https://doi.org/10.1111/eje.12485.Search in Google Scholar PubMed
29. Kikuchi, H, Ikeda, M, Araki, K. Evaluation of a virtual reality simulation system for porcelain fused to metal crown preparation at Tokyo medical and dental university. J Dent Educ 2013;77:782–92. https://doi.org/10.1002/j.0022-0337.2013.77.6.tb05530.x.Search in Google Scholar
30. Lave, J, Wenger, E. Situated learning: legitimate peripheral participation. Cambridge: Cambridge University Press; 1991.10.1017/CBO9780511815355Search in Google Scholar
31. Egan, T, Jaye, C. Communities of clinical practice: the social organization of clinical learning. Health N Hav 2009;13:107–25. https://doi.org/10.1177/1363459308097363.Search in Google Scholar PubMed
32. Khanna, SS, Dhaimade, PA. Green dentistry: a systematic review of ecological dental practices. Environ Dev Sustain 2019;21:2599–618. https://doi.org/10.1007/s10668-018-0156-5.Search in Google Scholar
33. Jasinevicius, TR, Landers, M, Nelson, S, Urbankova, A. An evaluation of two dental simulation systems: virtual reality versus contemporary non-computer-assisted. J Dent Educ 2004;68:1151–62. https://doi.org/10.1002/j.0022-0337.2004.68.11.tb03860.x.Search in Google Scholar
34. Daud, A, Matoug-Elwerfelli, M, Khalid, A, Ali, K. The impact of virtual reality haptic simulators in pre-clinical restorative dentistry: a qualitative enquiry into dental students’ perceptions. BMC Oral Health 2024;24:988. https://doi.org/10.1186/s12903-024-04704-w.Search in Google Scholar PubMed PubMed Central
35. Serrano, CM, Wesselink, PR, Vervoorn, JM. First experiences with patient-centered training in virtual reality. J Dent Educ 2020;84:607–14. https://doi.org/10.1002/jdd.12037.Search in Google Scholar PubMed
36. Towers, A, Dixon, J, Field, J, Martin, R, Martin, N. Combining virtual reality and 3D-printed models to simulate patient-specific dental operative procedures – A study exploring student perceptions. Eur J Dent Educ 2022;26:393–403. https://doi.org/10.1111/eje.12715.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


