Abstract
Objectives
Problem-based learning (PBL) is widely used in medicine instruction worldwide. Little research has been done on video-triggered cases in medical education in China. The aim of this study is to determine whether video-triggered cases are to be preferred over text-based cases and to evaluate their effectiveness in PBL.
Methods
A questionnaire was designed to investigate the attitudes toward video-triggered cases. The respondents were 30 instructors and 320 third-year students of the five-year and eight-year undergraduate programs at Shanghai Jiao Tong University School of Medicine.
Results
The majority of the students and instructors reported that this was their first time using a video-triggered case in PBL. The students considered the video-triggered case to be helpful for developing an understanding of the cases and motivating the respondents to learn compared to text-based cases previously used.
Conclusions
Video-triggered cases are much preferred over text-based cases in PBL, even by students and instructors who are accustomed to text-based cases. The strategic use of video-triggered cases in PBL may be an effective approach for guiding self-directed learning in undergraduate medical education.
Introduction
Problem-based learning (PBL) was pioneered in 1969 by the American neurology professor Howard Barrows, working at McMaster University in Canada, and it is now one of the most popular teaching methods in the world [1]. PBL is a teaching strategy in which students collect and develop knowledge and problem-solving skills through contextualized and realistic scenarios [2]. This strategy is student-centered educational approach emphasizing self-directed problem solving. In typical PBL setting, students begin by solving a problem from a clinical scenario through a text-based case. The students then present, elaborate, and synthesize their self-study findings through brain-storming. PBL has the advantage of cultivating students’ ability to think independently, critical thinking and teamwork skills [3], 4].
Given the many advantages of PBL, it has been applied widely in various fields of medical education in China, and it has achieved good results. However, its effectiveness varies across different studies, and some limitations have been noted [5], [6], [7], [8]. There is evidence of a decline in student interest in the PBL process [2], and the approach currently fails to cognitively engage students. One main reason for this is the lack of student engagement resulting from the monotonous format of scenario introduction through text-based cases [2], 9], 10]. Cases that are presented in textual form cannot fully convey the authenticity of clinical scenarios and the patient’s existence as an individual, which is why enriching the format of PBL cases is encouraged [11].
The use of video-triggered cases is suggested as an alternative solution [12], 13]. However, compared with more traditional teaching methods, such as text-based case studies, we currently know very little concerning the implementation and effectiveness of this pedagogical approach. To deepen the reform of clinical medicine teaching and explore new teaching models and methods, for the first time, this study constructs and implements video-triggered cases in the “Organ Integration of the Endocrine System” course at Shanghai Jiao Tong University School of Medicine. Through a questionnaire survey and data analysis, this study also evaluates the students’ engagement in PBL sessions using a video-triggered case and identifies their perception of this case vs. a traditional text-based case in PBL, exploring methods of optimizing the PBL approach.
Methods
Participants and settings
The participants were 320 third-year students, including undergraduate students of the five-year and eight-year Clinical Medicine and Stomatology program at Shanghai Jiao Tong University School of Medicine, and 30 instructors who participated in the PBL teaching.
Course design and implementation
Design of the PBL case
The PBL case used in this study, named “Give Me a Glass of Iced Cola”, was based on a real clinical case. The patient was a 26-year-old male who first came to the Department of Oral Mucosal Diseases due to parched mouth and scorched tongue having continued for two weeks that had been aggravated for two days. An oral mucosal doctor conducted preliminary physical examinations and laboratory tests and reported that the patient’s blood sugar was significantly elevated and that there could be an acid-base balance disorders. During referral to the Emergency Internal Medicine Department, the patient suddenly fell unconscious, and his condition worsened rapidly, bringing him to the brink of death. The final diagnosis of Type 2 diabetes mellitus with ketoacidosis was made on the basis of the patient’s medical history, clinical features, and laboratory examination results. Soon thereafter, the patient was transferred to the Endocrinology Department for further treatment. After a series of timely and effective treatments, the patient returned to stability. Finally, he was provided with diabetes health education.
Video-triggered case production in the PBL
Before the PBL course began, the trained endocrinologists and residents jointly performed and filmed a video according to clinical scenarios from the beginning of the case to the restoration of the patient’s state after treatment. The emergency of the patient’s condition was demonstrated through the transformation of different treatment scenes, the words and actions of the attending physician, and the necessary narration. Laboratory examination data and descriptions drawing on physical examination that were not fully displayed in the video were supplemented by a text version of the case. The full video was edited into several clips according to the progress of the case (Figure 1).

The video-triggered case production in the problem-based learning process. Several trained endocrinologists and residents jointly performed and filmed a video according to clinical scenarios. The full video of the video-triggered case was edited into several clips according to the progress of the case and played in order of course progress.
Implementation of the video-triggered case in the PBL course
From December 2022 to March 2023, this video-triggered case was used in a PBL session for “Organ Integration of the Endocrine System” course for students in their third year of the five-year and eight-year Clinical Medicine and Stomatology program at the Shanghai Jiao Tong University School of Medicine. PBL sessions were conducted in groups that consisted of 8–12 students and two trained instructors (clinical and basic instructors).
The entire PBL course was divided into three sessions. In the first session (80 min), the instructor distributed the QR codes on pages one and two of the first scenario of the case according to the learning progress, and the students scanned the QR codes to obtain the corresponding video-triggered cases and the supplementary text cases. In the second session (120 min), the students reported the learning points of the case in the form of a 5–6 min PowerPoint slide presentation, during which other students could ask questions, express their opinions, or interact with each other. Then, the instructors distributed the second scenario of the case. During the discussion taking place in the first two sessions, under the auspices of the student chair, the students were able to summarize the key content, ask questions and then solve the problems independently. In the third session (40 min), the author summarized the PBL. The complete video of the case (including the development, diagnosis, treatment, and prognosis of the disease) was played for the students, and a representative of a group of students was invited to share and elaborate on the diagram of the mechanism of this case. Finally, the instructor summarized the course and relative knowledge points (basic medicine, clinical medicine, and medical humanities) according to the preset teaching objectives and provided feedback and comments concerning the diagrams of the mechanism that were made by the students.
Learning assessment and data collection
This study used a questionnaire survey method, consisting of two parts, one for the students and one for the instructors. The first part evaluated the video-triggered case and its effect of implementation, consisting of several questions with response options given as agree, neutral, or disagree. The second part is fill in the blank questions, regarding opinions and suggestions on video-triggered cases. The questionnaires were distributed through WJX (a Chinese online survey platform similar to Amazon Mechanical Turk) during the PBL summary class, and students and instructors completed it independently and anonymously, emphasizing the confidentiality of the questionnaire to ensure the credibility of the results. A total of 30 instructor questionnaires and 320 student questionnaires were collected.
Results
Students’ evaluation of video-triggered cases in the PBL process
Among the 320 students, 306 (95.6 %) stated that this was their first time receiving a video-triggered case in PBL. Most of the students considered the video clips to be interesting, and they preferred video-triggered cases over text-based cases in the PBL. The majority of the students expressed a high degree of acceptance of the application of this video-triggered PBL case and recognized the effectiveness of this learning model (Figure 2).
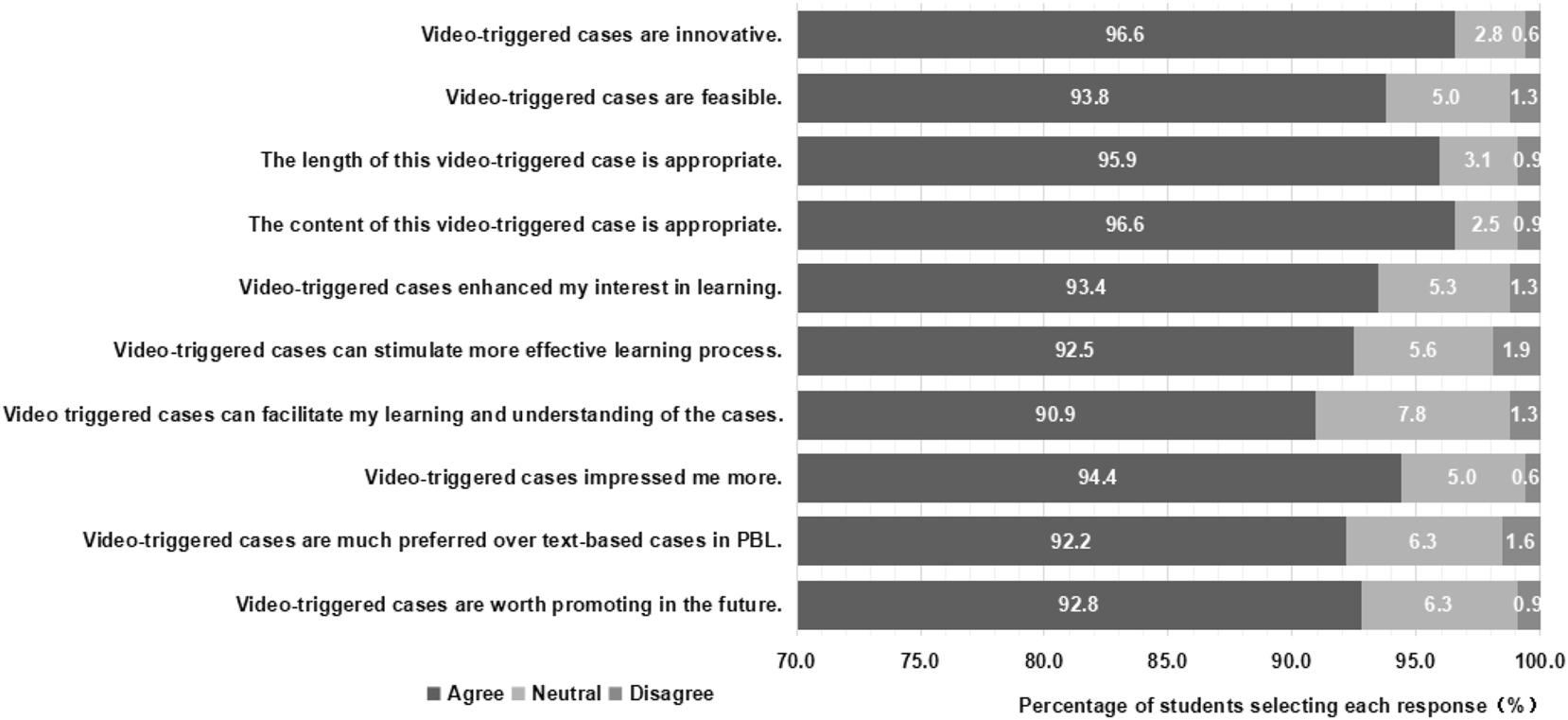
Students’ evaluation of video-triggered cases in the problem-based learning process (%).
The students’ opinions and suggestions regarding this video-based teaching process could be categorized into two major types: (1) video production needs to give more attention to details, including the image of the actors (such as the obese body shape of the patient in this case), the expression of the patient’s physical signs (such as the deep and large breaths that the patient takes in this case), etc.; (2) the video and text cases contain some duplicated information and should be optimized.
Instructors’ evaluation of video-triggered cases in the PBL process
All 30 instructors (100 %) used and conducted video-triggered PBL for the first time. The instructors set a high value on the implementation and effectiveness of the video-triggered case (Table 1).
Instructors’ evaluation of video-triggered cases in the problem-based learning (PBL) process.
| Question | Agree n (%) | Neutral n (%) | Disagree n (%) |
|---|---|---|---|
| Video-triggered cases are innovative. | 30 (100.0) | 0 (0.0) | 0 (0.0) |
| Video-triggered cases are feasible. | 27 (90.0) | 3 (10.0) | 0 (0.0) |
| The length of this video-triggered case is appropriate. | 28 (93.3) | 2 (6.7) | 0 (0.0) |
| The content of this video-triggered case is appropriate. | 27 (90.0) | 3 (10.0) | 0 (0.0) |
| Video-triggered cases enhance students’ interest in learning. | 29 (96.7) | 1 (3.3) | 0 (0.0) |
| Video-triggered cases can stimulate a more effective learning process. | 28 (93.3) | 2 (6.7) | 0 (0.0) |
| Video-triggered cases make it easier for students to understand the cases. | 27 (90.0) | 2 (6.7) | 1 (3.3) |
| Video-triggered cases are much preferred over text-based cases in PBL. | 27 (90.0) | 2 (6.7) | 1 (3.3) |
| Video-triggered cases are worth promoting in the future. | 27 (90.0) | 3 (10.0) | 0 (0.0) |
The instructors also provided some opinions and suggestions for this video-based teaching process: (1) establishing a video case library in the future would be preferable; (2) adding appropriate humanistic care content, such as doctor-patient communication or conflicts, is necessary.
Discussion
In the present study, students and instructors preferred the modified PBL delivery approach, video-triggered cases, over traditional, text-based cases. By presenting the patient as a real person with a face, who talks, feels and worries, instead of a character on paper, the video-triggered case received unanimous praise and recognition from students and instructors, along with proposed further optimization plans. This method of teaching not only retains the advantages of the original PBL method but also keeps pace with the demands of the times for reform and innovation, laying a foundation for future clinical work and promoting the development of students’ comprehensive abilities and cultivation of quality.
As shown in this study, the majority of students and instructors experienced a video-triggered case for the first time. Text-based cases are used as a conventional and traditional method for PBL in medical schools in China. The production costs of text-based cases are much lower than those of video-triggered cases, and they are much easier to produce and implement. The production of video-triggered cases generally requires professional staff and actors, the production of text records and subtitles, and the purchase of hardware for dissemination and playback. The major problem with text-based cases is that they cannot realistically simulate the challenges of solving problems in clinical environments [10]. In real clinical environments, doctors rarely make diagnosis and treatment decisions on the basis of textual descriptions, as seen in text-based cases. Before they make a diagnosis, doctors need to communicate with the patient, perform a physical examination, and explain the symptoms and investigation results.
As many previous studies have shown, video-triggered cases may have many advantages that text-based cases lack.
First, a video-triggered case provides a real clinical scenario. When a patient comes in for a consultation, information concerning that patient comes in many different ways at the same time, both verbal and nonverbal. Unlike the case of the PBL course triggered by text-based cases, in which patients’ opinions are interpreted and summarized, video-triggered cases allow students to listen to patients’ actual complaints and actively extract relevant information before they participate in discussion. In addition to verbal information, nonverbal information on the patient is equally important. Many types of nonverbal information, such as the appearance of patients, facial expressions, gestures, gait, movement, mental status and even their emotional states, should receive attention. In text-based cases, some or all of these clues may be lost. Video of a real scene combined with patients’ reports supplemented in paper is much closer to the problem-solving process as it is experienced in an actual clinical environment. The use of video-triggered cases may not only enhances students’ observational power but also encourages their integration of information [10].
Second, video-triggered cases can increase students’ motivation to solve problems and stimulate their cognitive processes. PBL emphasizes students’ autonomous learning. After students have identified learning problems, they need to find new information and build new knowledge to solve these problems. The entire process of self-directed learning is mainly driven by motivation. Studies have shown that video-triggered cases in PBL may stimulate students’ interest and desire in learning, and students may also be more motivated [10], 14]. In addition, critical thinking is very important in PBL. Unlike the case of students exposed to text-based cases, the verbal interaction between students exposed to video-triggered cases contains more terms related to data exploration, theory construction and theory evaluation, and critical thinking increases [15], 16]. The learning process is thus more effective in video-triggered cases than in text-based cases for PBL.
Third, video-triggered cases can preserve nonverbal information and allow students to observe the interactions between patients and doctors. In the text-based case, the results of doctor-patient interactions, that is, the medical history and physical examination results, are sorted and presented to the students. However, this interactive process is an opportunity for students to learn how doctors interact with patients: how patients ask questions, how doctors listen and talk to patients, how problems can be explained, etc. Therefore, video-triggered cases may be better suited than text-based cases in terms of the goal of directly showing students the clinical interaction, guided by the doctor’s reasoning process.
Although the video-triggered cases discussed above have many advantages, they also have several limitations. Video-triggered cases cannot replace real interactions between students and real patients. Text-based cases detach students from the messiness of real patients’ lives and emotions [11]. The most ideal solution is to use real patients and reception scenes in PBL, but due to patient privacy and clinical medical safety considerations, this method is impractical. The duration of receiving patients in real clinical settings may far exceed a few minutes, and owing to time, filming, and production costs, video-triggered cases may still simplify the actual clinical experience with patients to a certain extent. Moreover, video-triggered cases that include scenarios with vibrant and sensory-rich data may lead to sensory saturation and cognitive overload [17], 18], as well as the use of videos, multi-media, and computers, may disrupt the PBL [19].
Some of the advantages of the video-triggered cases listed above are based on theoretical analysis, while others are based on research on a limited number of students. Many video-triggered cases have been developed worldwide, but relatively little research has been conducted on the implementation of video-triggered cases in China. Therefore, one aim of this study is to understand the overall preferences of students and instructors who are accustomed to text-based cases and the reasons for their preferences, attempting to find optimal solutions for video-triggered cases in PBL.
In this study, we attempted to find an optimization plan for video-triggered cases through questionnaires. First, situational performance should be closer to the real cases. For example, the presentation of general physical features and clinical manifestations should be closer to the real state. Second, when video is used in combination with supplementary text cases, the repetitive presentation of content can be avoided. Third, medical humanities education can be included in video-triggered cases, such as doctor–patient communication.
However, this study also had limitations. First, as a new teaching mode, the evaluation criteria for the effect of video-triggered cases in PBL are all subjective. Objective evaluations, such as tests, should be introduced to compare the effects of video-triggered cases and traditional text-based ones. Second, this study did not adopt a randomized controlled design. In our following research, two randomly assigned groups of students and instructors will be arranged to receive video-triggered or text-based cases simultaneously to test the efficacy of different teaching methods based on similar clinical scenarios. Additionally, a quiz will be administered immediately after teaching to obtain instant feedbacks from the students and instructors. Lastly, the availability of high-quality videos is also a problem that needs to be addressed in PBL in the future.
Conclusions
Video-triggered cases are much preferred to text-based cases in PBL learning by both students and instructors. Video-triggered cases can stimulate not only a more effective learning process but also students’ motivation to engage in self-directed learning. The strategic use of video-triggered cases in PBL may be an effective approach for medical education.
Funding source: Medical Education Development and Research Project of Shanghai Ninth People's Hospital
Award Identifier / Grant number: JYJX03202301
Funding source: Teaching Physician Program of Shanghai Ninth People's Hospital
Award Identifier / Grant number: JXXYS-2021-4
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: Yi Chen – designed the study, analyzed the data, drafted the manuscript. Lin Ye, Hui Zhu, Chenyu Cao – participated in video recording and course implementation. Yingli Lu and Bing Han – conceptualized the study and revised the manuscript. The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: This study was supported by the Teaching Physician Program of Shanghai Ninth People’s Hospital [grant number JXXYS-2021-4], the Medical Education Development and Research Project of Shanghai Ninth People’s Hospital [grant number JYJX03202301].
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Barrows, HS, Mitchell, DL. An innovative course in undergraduate neuroscience. Experiment in problem-based learning with ‘problem boxes’. Br J Med Educ 1975;9:223–30. https://doi.org/10.1111/j.1365-2923.1975.tb01930.x.Search in Google Scholar PubMed
2. Fatima, SS, Ghias, K, Jabeen, K, Sabzwari, S. Enhancing cognitive engagement of pre-clinical undergraduate medical students via video cases and interactive quizzes in problem-based learning. Cureus 2019;11:e3832. https://doi.org/10.7759/cureus.3832.Search in Google Scholar PubMed PubMed Central
3. Alrahlah, A. How effective the problem-based learning (PBL) in dental education. A critical review. Saudi Dent J 2016;28:155–61. https://doi.org/10.1016/j.sdentj.2016.08.003.Search in Google Scholar PubMed PubMed Central
4. Wood, DF. Problem based learning. BMJ 2003;326:328–30. https://doi.org/10.1136/bmj.326.7384.328.Search in Google Scholar PubMed PubMed Central
5. Nicolaou, SA, Televantou, I, Papageorgiou, A, Albert, AP, Hitchings, AW, McCrorie, P, et al.. Factors affecting pharmacology learning in integrated PBL in diverse medical students: a mixed methods study. BMC Med Educ 2024;24:324. https://doi.org/10.1186/s12909-024-05289-2.Search in Google Scholar PubMed PubMed Central
6. Solano, J, Zuniga Gutierrez, M, Pinel-Guzman, E, Henriquez, G. Barriers and solutions to successful problem-based learning delivery in developing countries – a literature review. Cureus 2023;15:e43187. https://doi.org/10.7759/cureus.43187.Search in Google Scholar PubMed PubMed Central
7. Lim, WK. Problem based learning in medical education: handling objections and sustainable implementation. Adv Med Educ Pract 2023;14:1453–60. https://doi.org/10.2147/amep.s444566.Search in Google Scholar
8. Trullas, JC, Blay, C, Sarri, E, Pujol, R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ 2022;22:104. https://doi.org/10.1186/s12909-022-03154-8.Search in Google Scholar PubMed PubMed Central
9. Pedersen, K, Moeller, MH, Paltved, C, Mors, O, Ringsted, C, Morcke, AM. Students’ learning experiences from didactic teaching sessions including patient case examples as either text or video: a qualitative study. Acad Psychiatry 2018;42:622–9. https://doi.org/10.1007/s40596-017-0814-1.Search in Google Scholar PubMed
10. Chan, LK, Patil, NG, Chen, JY, Lam, JC, Lau, CS, Ip, MS. Advantages of video trigger in problem-based learning. Med Teach 2010;32:760–5. https://doi.org/10.3109/01421591003686260.Search in Google Scholar PubMed
11. Kenny, NP, Beagan, BL. The patient as text: a challenge for problem-based learning. Med Educ 2004;38:1071–9. https://doi.org/10.1111/j.1365-2929.2004.01956.x.Search in Google Scholar PubMed
12. Kononowicz, AA, Zary, N, Edelbring, S, Corral, J, Hege, I. Virtual patients-what are we talking about? A framework to classify the meanings of the term in healthcare education. BMC Med Educ 2015;15:11. https://doi.org/10.1186/s12909-015-0296-3.Search in Google Scholar PubMed PubMed Central
13. Berman, NB, Durning, SJ, Fischer, MR, Huwendiek, S, Triola, MM. The role for virtual patients in the future of medical education. Acad Med 2016;91:1217–22. https://doi.org/10.1097/acm.0000000000001146.Search in Google Scholar
14. de Leng, B, Dolmans, D, van de Wiel, M, Muijtjens, A, van der Vleuten, C. How video cases should be used as authentic stimuli in problem-based medical education. Med Educ 2007;41:181–8. https://doi.org/10.1111/j.1365-2929.2006.02671.x.Search in Google Scholar PubMed
15. Balslev, T, de Grave, WS, Muijtjens, AM, Scherpbier, AJ. Comparison of text and video cases in a postgraduate problem-based learning format. Med Educ 2005;39:1086–92. https://doi.org/10.1111/j.1365-2929.2005.02314.x.Search in Google Scholar PubMed
16. Kamin, C, O’Sullivan, P, Deterding, R, Younger, M. A comparison of critical thinking in groups of third-year medical students in text, video, and virtual PBL case modalities. Acad Med 2003;78:204–11. https://doi.org/10.1097/00001888-200302000-00018.Search in Google Scholar PubMed
17. Kamin, CS, O’Sullivan, PS, Younger, M, Deterding, R. Measuring critical thinking in problem-based learning discourse. Teach Learn Med 2001;13:27–35.10.1207/S15328015TLM1301_6Search in Google Scholar PubMed
18. Balslev, T, de Grave, W, Muijtjens, AM, Eika, B, Scherpbier, AJ. The development of shared cognition in paediatric residents analysing a patient video versus a paper patient case. Adv Health Sci Educ Theory Pract 2009;14:557–65. https://doi.org/10.1007/s10459-008-9138-y.Search in Google Scholar PubMed
19. Basu Roy, R, McMahon, GT. Video-based cases disrupt deep critical thinking in problem-based learning. Med Educ 2012;46:426–35. https://doi.org/10.1111/j.1365-2923.2011.04197.x.Search in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/gme-2025-0012).
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Medical education embraces new transformative opportunities
- Review Articles
- Artificial intelligence in medical problem-based learning: opportunities and challenges
- Primary exploration of the One Science integrated curriculum system construction
- Structural and policy overview of medical education in Germany
- Scaling up and dissemination of pre-service education in mental, neurological, and substance use disorders: the way moving forward
- Overview and summary of AI competency framework for teachers
- Shaping the future of healthcare: insights into Japan’s medical education system
- Study on the performance of medical disciplines in Chinese universities based on the data of ShanghaiRanking’s Global Ranking of Academic Subjects
- Basic theoretical frameworks of health education, research needs and practice implications in China
- Koch’s postulates: from classical framework to modern applications in medical microbiology
- Plastic surgery at the crossroads: historical roots and emerging frontiers
- Beyond technical efficacy: challenges and critical concerns of large language model’s impact on medical education in China: a systematic review
- Research Articles
- Impact of early clinical exposure and preclinical tutorial guide on undergraduate dental students in Shanghai
- Capable exam-taker and question-generator: the dual role of generative AI in medical education assessment
- Teaching design for chapter “primary liver cancer” in surgery course based on the clinical theory and clerkship synchronization model in the era of New Medicine
- Integration of a “cardiovascular system” curriculum into an eight-year medical education program: exploration and the experience in China
- AI agent as a simulated patient for history-taking training in clinical clerkship: an example in stomatology
- Student-centered, humanities-guided teaching of the “Medical Practical English” course and its assessment
- The teaching design and implementation of “Intravenous Therapy” in “Fundamental Nursing”
- Biomedical engineering teaching: challenges and the NICE strategy
- Exploratory research on the reform of diversified teaching methods in residency training education: a case study of orthopedics
- Innovative strategies for interdisciplinary medical-engineering education in China
- Construction and optimization of video-triggered cases in problem-based learning
- Exploration and innovation in integrating medical humanities into undergraduate Medical English education
- Innovative application of generating instrument operation videos using QR code technology in experimental teaching
- Constructing a medical humanistic competency framework for medical undergraduate students in China: a grounded theory approach
- Evolution and reform of Medical Microbiology education in New Medical Science era
- Immersive learning in dentistry — evaluating dental students’ perceptions of virtual reality for crown preparation skill development: a multi-institution study
- Enhancing surgical education through output-driven input: implementation and evaluation of the O-SITE teaching model in clinical medical students
Articles in the same Issue
- Frontmatter
- Editorial
- Medical education embraces new transformative opportunities
- Review Articles
- Artificial intelligence in medical problem-based learning: opportunities and challenges
- Primary exploration of the One Science integrated curriculum system construction
- Structural and policy overview of medical education in Germany
- Scaling up and dissemination of pre-service education in mental, neurological, and substance use disorders: the way moving forward
- Overview and summary of AI competency framework for teachers
- Shaping the future of healthcare: insights into Japan’s medical education system
- Study on the performance of medical disciplines in Chinese universities based on the data of ShanghaiRanking’s Global Ranking of Academic Subjects
- Basic theoretical frameworks of health education, research needs and practice implications in China
- Koch’s postulates: from classical framework to modern applications in medical microbiology
- Plastic surgery at the crossroads: historical roots and emerging frontiers
- Beyond technical efficacy: challenges and critical concerns of large language model’s impact on medical education in China: a systematic review
- Research Articles
- Impact of early clinical exposure and preclinical tutorial guide on undergraduate dental students in Shanghai
- Capable exam-taker and question-generator: the dual role of generative AI in medical education assessment
- Teaching design for chapter “primary liver cancer” in surgery course based on the clinical theory and clerkship synchronization model in the era of New Medicine
- Integration of a “cardiovascular system” curriculum into an eight-year medical education program: exploration and the experience in China
- AI agent as a simulated patient for history-taking training in clinical clerkship: an example in stomatology
- Student-centered, humanities-guided teaching of the “Medical Practical English” course and its assessment
- The teaching design and implementation of “Intravenous Therapy” in “Fundamental Nursing”
- Biomedical engineering teaching: challenges and the NICE strategy
- Exploratory research on the reform of diversified teaching methods in residency training education: a case study of orthopedics
- Innovative strategies for interdisciplinary medical-engineering education in China
- Construction and optimization of video-triggered cases in problem-based learning
- Exploration and innovation in integrating medical humanities into undergraduate Medical English education
- Innovative application of generating instrument operation videos using QR code technology in experimental teaching
- Constructing a medical humanistic competency framework for medical undergraduate students in China: a grounded theory approach
- Evolution and reform of Medical Microbiology education in New Medical Science era
- Immersive learning in dentistry — evaluating dental students’ perceptions of virtual reality for crown preparation skill development: a multi-institution study
- Enhancing surgical education through output-driven input: implementation and evaluation of the O-SITE teaching model in clinical medical students

