Abstract
Objectives
Interdisciplinary medical-engineering education is critical for driving scientific innovation and cultivating next-generation medical-engineering talents. This study aimed to evaluate medical-engineering education models at universities in China through case studies, core competency development, and questionnaire surveys and analyzed key indicators such as curriculum design, international collaboration, and university-industry partnerships.
Methods
A combination of quantitative and qualitative methods was used for data collection and analysis. A questionnaire survey including multi-dimensional investigations was administered to 80 students, 15 student supervisors, and 10 administrators, yielding 100 valid responses. Case studies were conducted to explore the best practices in interdisciplinary talent development.
Results
The survey revealed that although over 80 % of respondents acknowledged the discipline’s importance, curriculum satisfaction was inadequate (23.08 %), and practical engagement was limited (19.23 %). Students identified “resource allocation” and “professional practice” as key influencing factors, while supervisors and administrators emphasized the importance of “scientific research” and “academic exchange.” Case studies indicated that leading universities promote high-quality medical-engineering talent through flexible curricula, international collaborations, and practice-oriented approaches.
Conclusions
Optimizing curriculum design, improving university-industry collaboration, strengthening practical training, and refining policy support are crucial for cultivating interdisciplinary talent equipped to meet modern requirements and drive medical-engineering innovation.
Introduction
The concept of medical-engineering disciplines emerged in the 1970s [1]. The term “medical” refers to fields within the medical field, including clinical medicine and molecular biology, while “engineering” encompasses science and engineering disciplines such as materials science, artificial intelligence, and mechanical engineering. This intersection represents the integration and joint innovation between medical and engineering sciences [2]. In 2009, Susan Hockfield, the president of the Massachusetts Institute of Technology (MIT), emphasized the importance of this convergence in her speech at the Science and Technology Policy Forum of the American Academy of Arts and Sciences [3]. She claimed that the third revolution in life sciences has begun, characterized by a significant convergence of medical and engineering in the fields of life sciences, physical sciences, and engineering. Hockfield also emphasized that funding this research is a vital investment in human health, environmental well-being, and economic prosperity [3]. The convergence of medicine and engineering has facilitated the emergence of diverse application areas such as intelligent diagnostics, advanced medical devices, rehabilitation systems, and biomedical data modeling, which collectively reflect the expanding frontiers of interdisciplinary research in healthcare innovation (Figure 1).
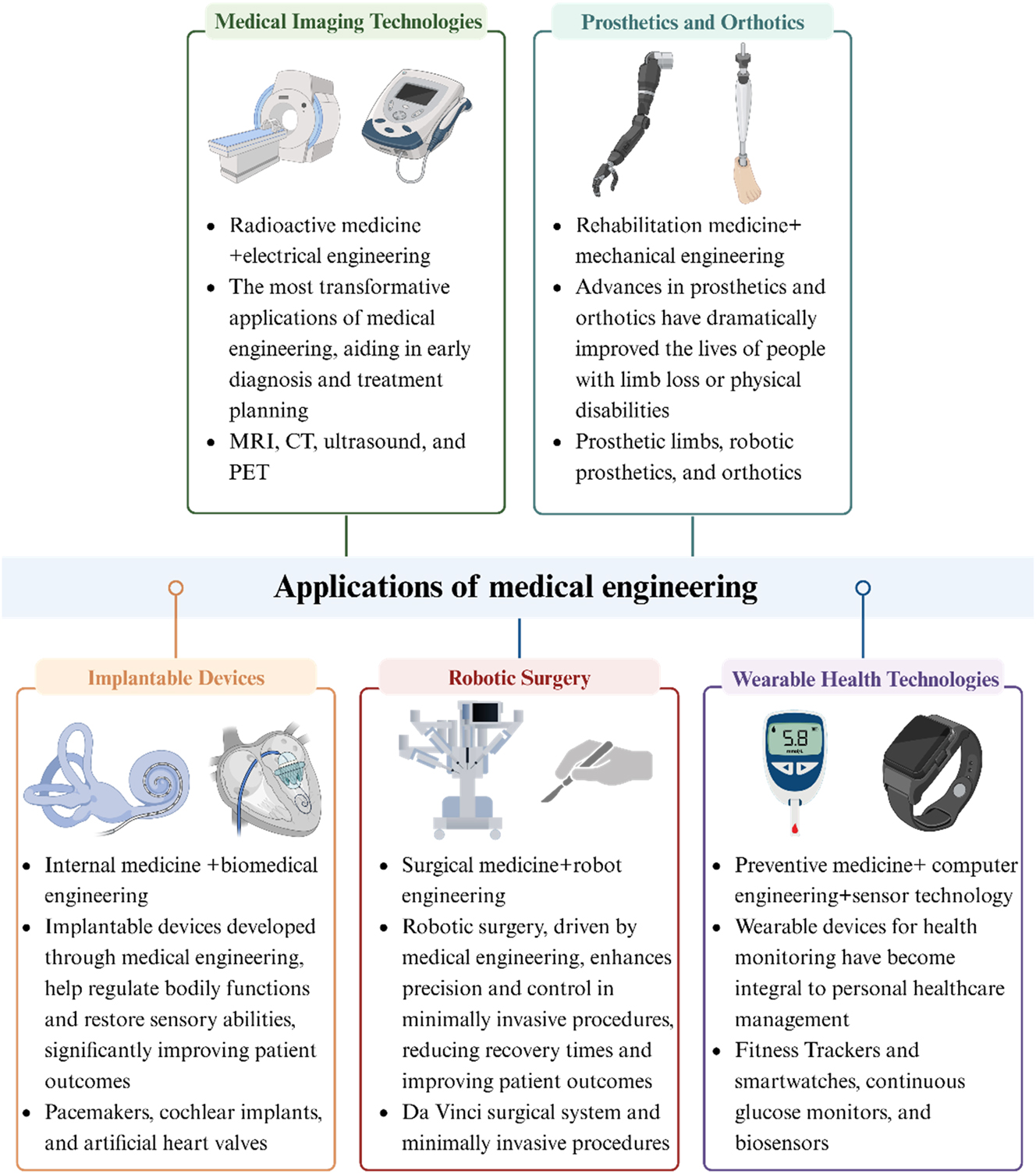
Applications of medical-engineering.
Since the 1970s, leading universities around the world have established research institutes and centers to promote interdisciplinary research [4]. For example, the Bio-X Research Center at Stanford University, established in 1998, focuses on addressing challenges in life sciences [5]. According to the Accreditation Board for Engineering and Technology (ABET), 148 universities in the United States offer a total of 150 ABET-accredited education programs in Biomedical Engineering (BME) or Bioengineering [6]. In recent years, several top universities in China, such as Peking University, Tsinghua University, Shanghai Jiao Tong University, Xi’an Jiao Tong University, and Zhejiang University have established interdisciplinary research institutes, creating important platforms for such research [4]. In parallel with global trends, China’s higher education landscape has witnessed a structured evolution in interdisciplinary medical-engineering education, characterized by the progressive establishment of degree programs, institutional platforms, and policy frameworks that support talent cultivation and translational research (Figure 2). For instance, the Med-X Research Institute of Shanghai Jiao Tong University, which was officially founded in November 2007, focuses on four main areas: Biomedical Engineering, Biology, Imaging, Nuclear Medicine, and Materials Science and Engineering. By leveraging the university’s strengths in clinical medicine, science, and engineering, the institute aims to address clinical and medical challenges, conduct cutting-edge interdisciplinary research, and develop advanced medical technologies [7]. As of 2024, approximately 200 universities in China offer Biomedical Engineering programs, 75 have received approval for the Intelligent Medical Engineering degree program, and 113 have degree programs in Medical Imaging Technology [8].
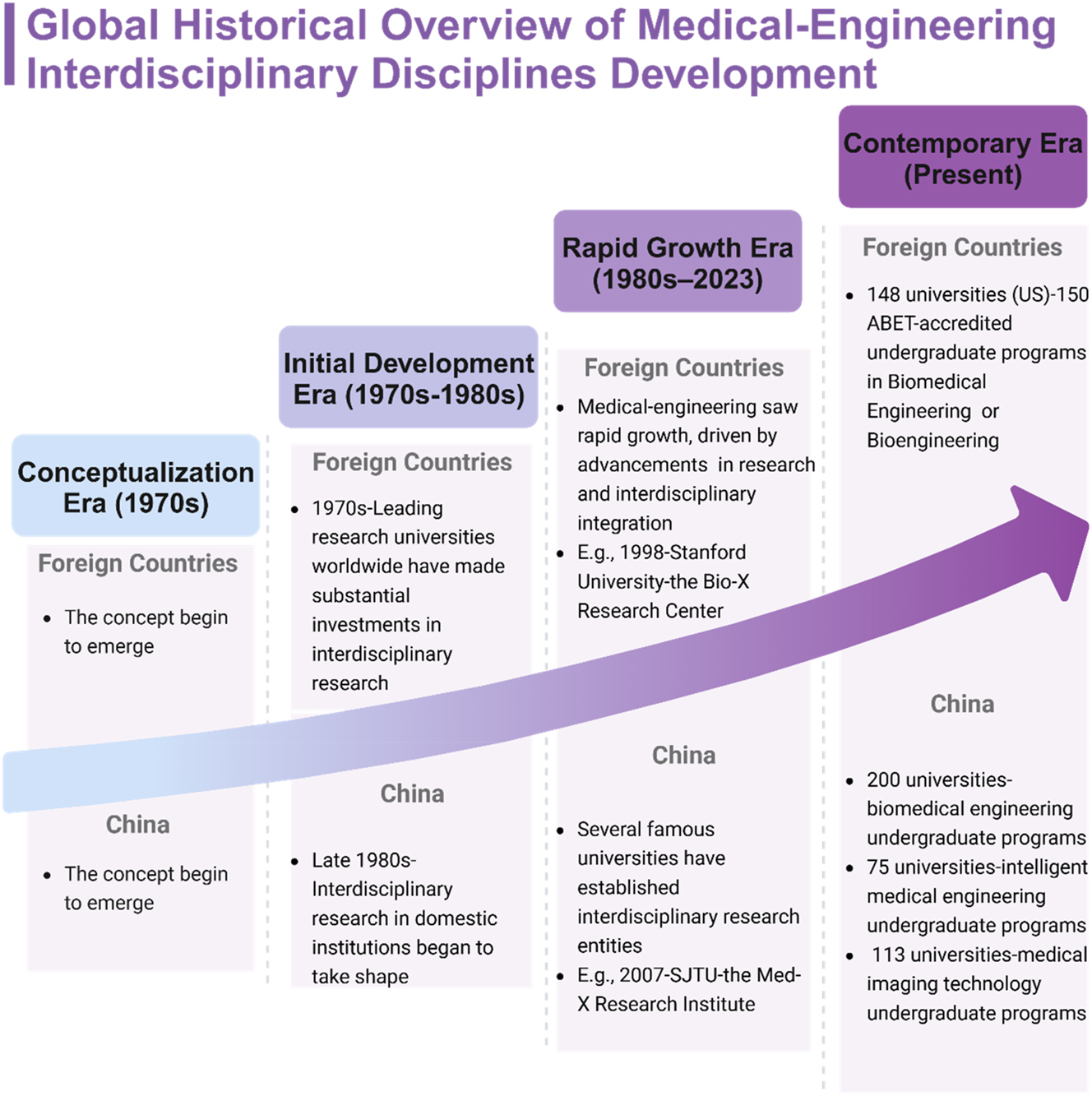
Overview of the medical-engineering discipline development.
Although interdisciplinary medical-engineering education has attracted increasing attention, most existing studies have remained theoretical, focusing on single-institution initiatives, or limited to curriculum reforms. Empirical research that integrates institutional comparisons, competency frameworks, and multi-stakeholder perspectives – particularly within the Chinese context – remains scarce [9], [10], [11]. To address this gap, our study adopts a comprehensive and pragmatic approach that not only compares leading institutional models but also triangulates survey data from students, supervisors, and administrators. This enables a deeper exploration of both structural characteristics and real-world challenges in China’s evolving landscape of interdisciplinary medical-engineering education.
Therefore, the integration of medicine and engineering has become an inevitable and compelling trend. Further promoting the development of this field and effectively educating interdisciplinary students is a major concern [4]. In this study, mature interdisciplinary programs are presented through three real-world case studies. Then, we propose the core competencies of an interdisciplinary medical-engineering model. In addition, we present the results of a survey on the attitudes and perspectives of various stakeholders towards interdisciplinary research, including students, supervisors, and administrators. Finally, the existing issues and corresponding promotion strategies are proposed based on the responses and experiences of the survey participants.
Interdisciplinary medical-engineering model based on real-world case studies
To provide a representative and diverse understanding of interdisciplinary medical-engineering education in China, we selected three leading universities – Tsinghua University, Zhejiang University, and Shanghai Jiao Tong University – as case studies. The selection was based on the following criteria: (1) each institution has a nationally recognized interdisciplinary medical-engineering program with a long development history; (2) they represent different educational models and institutional strategies; (3) all have demonstrated academic excellence and international influence in medical-engineering integration through ABET accreditation, dual-track curricula, or global collaboration initiatives [12], [13], [14], [15], [16], [17]. These institutions serve as leading examples in the Chinese context and offer a valuable lens through which to examine the best practices and challenges in cultivating interdisciplinary talent.
The School of Biomedical Engineering of Tsinghua University
The Department of Biomedical Engineering at Tsinghua University was founded in 1979 with the program officially launched in 1982. In 2024, the School of Biomedical Engineering was officially established as a standalone academic unit. The school applies engineering principles and methods to advance life sciences and medicine, focusing on the development of innovative medical instruments, diagnostic and therapeutic methods, materials, and formulations to improve human health. The program aims to cultivate academic leaders capable of pioneering breakthroughs in medical-engineering interdisciplinarity and foster leaders to drive innovation across related industries [12].
The program offers two tracks: one track for Electronic Information and the other for Chemical and Biological Science. Students must complete a minimum of 170 credits to graduate. The Electronic Information track includes 44 credits for general courses and 114 credits for specialized courses and activities, comprising core courses (33 credits), major courses (56 credits), hands-on activities and summer term courses (10 credits), a comprehensive thesis (15 credits), and self-development courses (12 credits). The Chemical and Biological Science track requires 44 credits in general courses, 116 credits in specialized courses and activities (including 38 credits in basic courses, 53 credits in major courses, 10 credits in practical training sessions and summer-term courses, and 15 credits in capstone courses), and 10 credits in self-development courses [13]. From 2020 to 2023, the program has achieved a 100 % employment rate, with graduates highly valued by academic and industry professionals for their rigorous training and solid scientific background. Alumni include professors at prestigious universities and leaders in the medical device industry, many of whom have excelled in teaching, research, industry, and management [12].
The College of Biomedical Engineering and Instrument Science of Zhejiang University
The Biomedical Engineering Program at Zhejiang University, established in 1977, was the first biomedical engineering program in China. The School of Biomedical Engineering and Instrument Science was established in 1998. The school aims to promote students’ innovative capabilities and self-development, train interdisciplinary talent capable of applying engineering technologies to address challenges in biology and medicine and advancing the development of medical instruments. These efforts aim to provide engineering solutions for disease prevention, diagnosis, monitoring, treatment, healthcare, and rehabilitation. The school has established extensive research collaborations with international universities and institutions. It hosts numerous international conferences and maintains exchange and joint training programs with prestigious universities in the United States, the United Kingdom, Japan, the Netherlands, Australia, and Republic of Singapore [14].
The program requires a minimum of 178.5 credits for graduation, including 83.5 credits in general education, 23 credits in basic professional courses, 52 credits in specialized courses, 6 credits in personalized courses, 3 credits in interdisciplinary courses, 3 credits in international courses, and 8 credits in other courses [15]. Graduates secure high-quality employment, with many joining top companies such as General Electric Company, Siemens, Philips, and United Imaging in the medical instrument and imaging fields. Others pursue careers in information technology (IT) at Alibaba, Huawei, Baidu, or Google, or work in leading hospitals. Approximately 60 % of the graduates choose to pursue further studies, often at top institutions such as MIT, Yale University, Johns Hopkins University, Georgia Institute of Technology, and the National University of Singapore [16].
The School of Biomedical Engineering of Shanghai Jiao Tong University
The origin of Biomedical Engineering at Shanghai Jiao Tong University can be traced back to the founding of the Biomedical Instrumentation Program in 1979. In 2011, the School of Biomedical Engineering was established, which remains the only Biomedical Engineering program in China that received international ABET accreditation in 2019 [7]. The school is dedicated to interdisciplinary research between medicine and engineering and the promotion of innovative talents. Through collaboration with industry, international exchange programs, and other initiatives, the school provides extensive learning and exchange platforms for students and continuously improves the quality of education in line with the ABET international professional accreditation standards [17].
The program requires a minimum of 162 credits for graduation, consisting of general education courses (42 credits), specialized education courses (87 credits), professional practice courses (21 credits), interdisciplinary modules (6 credits), and personalized modules (6 credits). Professional practice courses account for 12.96 % of the total credits. To date, the program has trained over 1,600 students, more than 65 % of whom have gone on to graduate study at leading institutions such as Harvard University, Stanford University, Columbia University, Johns Hopkins University, Duke University, Tsinghua University, and Shanghai Jiao Tong University School of Medicine (which offers a four-year Doctor of Medicine program). Graduates achieve nearly 100 % employment, excelling in the fields of medical technology, hospitals, Internet industries, and investment banking (Table 1) [17].
Career paths for graduates in medical-engineering interdisciplinary fields.
| Career path | Institutions/organizations |
|---|---|
| Master or PhD study | Massachusetts Institute of Technology, Yale University, Georgia Institute of Technology, the National University of Singapore, Harvard University, Stanford University, Columbia University, Johns Hopkins University, Duke University, Tsinghua University, and Shanghai Jiao Tong University School of Medicine |
| Tertiary hospitals | Peking Union Medical College Hospital, West China Hospital of Sichuan University, The First Affiliated Hospital of Zhejiang University, Shanghai Jiao Tong University School of Medicine Affiliated Ruijin Hospital, and Shanghai Jiao Tong University School of Medicine Affiliated Renji Hospital |
| IT industries | Alibaba, Huawei, Baidu, and Google |
| Medical device industries | General Electric Company, Siemens, Philips, and United Imaging |
| Investment banking | Goldman Sachs, Morgan Stanley, China International Capital Corporation, and China International Trust and Investment Corporation Securities |
-
IT, information technology.
Core competencies of the interdisciplinary medical-engineering model
Competency framework
The competency framework for interdisciplinary medical-engineering education emphasizes the integration of multi-disciplinary knowledge and the cultivation of innovative thinking. Mastery of key theories and methodologies in both medicine and engineering is essential. In medicine, this includes fundamental disciplines, such as molecular biology, anatomy, physiology, and pathology, whereas in engineering, it includes areas such as signal processing, materials science, and systemic modeling. Additionally, the ability to translate medical challenges into technical solutions is crucial. This requires professionals to identify and define problems from a medical perspective and develop viable technical solutions. In addition, interdisciplinary teamwork and effective communication are equally important, as they enable researchers to bridge disciplinary gaps and ensure the successful completion of projects.
Awareness and attitudes
Awareness and attitudes form the cornerstone of core competencies in interdisciplinary medical-engineering education. These attributes reflect a comprehensive understanding of interdisciplinary integration and a proactive action-oriented mindset. The key components include sensitivity to interdisciplinary challenges, recognition of the value of integration, and a clear vision for achieving interdisciplinary goals.
Skills and knowledges
Professionals in interdisciplinary medical-engineering fields require a broad range of skills and knowledge spanning medicine, engineering, and science. Addressing complex health problems requires expertise in the clinical and basic medical sciences (e.g., anatomy, physiology, and disease mechanisms), engineering (e.g., biomechanics, signal processing, and medical device design), and natural sciences (e.g., physics, chemistry, and materials science). This multi-dimensional knowledge base enables a comprehensive understanding of the technical challenges in the healthcare sector and their solutions.
Collaboration skills
Effective collaboration among interdisciplinary teams is central to the success of medical-engineering projects. Team members must bridge disciplinary boundaries by understanding and respecting each other’s terminology and culture. Therefore, project management is one of the core collaborative skills that facilitates the coordination of resources and time and innovative thinking by helping team members cross traditional disciplinary boundaries and propose solutions. Continuous collaboration and learning improve research quality and promote technological progress.
Principles of communication
Efficient communication is a basic principle of interdisciplinary collaboration. This requires respect for diverse perspectives and the ability to convey information clearly and precisely across disciplines. An inclusive environment should be created to encourage open discussion and innovative thinking. When technical terminology is used, providing appropriate explanations ensures mutual understanding among collaborators.
Principles of collaboration
Interdisciplinary collaboration in medical technology emphasizes shared goals and collective responsibilities. Participants from different fields, including medicine, academia, industry, and government, should be treated equally to foster mutual respect and trust. The open exchange of knowledge, experience, and resources is crucial for addressing global health challenges and achieving sustainable development. Long-term stable partnerships are essential to advance the field and ensure the continuity of joint efforts.
Strategies for competency enhancement
Improving core competencies in medical-engineering interdisciplinary education requires a multi-faceted approach that includes education, training, and practical experience. Universities should offer interdisciplinary courses that integrate basic knowledge and emerging technologies in medicine, engineering, and life sciences. Continuing education opportunities such as workshops and seminars allow practitioners to update their skills. Practical experience in the form of internships and research projects bridges the gap between theory and real-world applications, fostering innovative problem-solving skills.
Building knowledge systems
Developing a robust knowledge system in interdisciplinary medical-engineering education means training professionals who can tackle complex health and technical challenges. Core subjects in medicine, engineering, and science provide a solid theoretical foundation, whereas electives in areas such as health promotion, engineering technology, and artificial intelligence offer opportunities for specialization. Practical applications through internships and research projects enhance understanding and promote innovation.
Developing leadership and teamwork skills
Leadership and teamwork are critical in interdisciplinary endeavors. Leaders must define research goals, facilitate collaboration, and translate results into practical applications. Effective leadership includes fostering talent development through structured plans and growth opportunities. Teamwork ensures the efficient integration of diverse expertise and contributes to the success of interdisciplinary projects.
Fostering logical and systemic thinking skills
Logical and systemic thinking is essential for the comprehensive management of health challenges. Systemic thinking enables professionals to analyze problems holistically, identify critical issues, and develop effective solutions. Logical thinking is sharpened through involvement in practical projects, where theoretical knowledge is applied to real-life scenarios. Exposure to different perspectives further enhances problem-solving skills.
Enhancing communication and conflict resolution skills
Strong communication and conflict-resolution skills are essential for successful interdisciplinary collaboration in medical technologies. Professionals must understand and apply the communication principles to ensure clarity and mutual understanding. Resolving conflicts requires active listening, empathy, and the ability to propose constructive solutions to avoid misunderstandings and promote common goals.
Status of interdisciplinary medical-engineering models in China
Research methods
A comprehensive questionnaire survey was administered to 105 respondents, including 80 students, 15 supervisors, and 10 administrators. Three different questionnaires were designed for each group, comprising five sections: “respondent category,” “basic information,” “perceptions of medical-engineering education,” “factors affecting medical-engineering education,” and “recommendations to promote medical-engineering education.” The questionnaires contained 39, 55, and 57 questions for the students, supervisors, and administrators, respectively. A total of 100 valid responses were collected and subjected to statistical analysis. This study aimed to evaluate the views of these stakeholders and identify obstacles and opportunities to optimize interdisciplinary medical-engineering models in China.
The sample size of 100 was determined based on data saturation principles and guided by a pilot study, which indicated sufficient variability across stakeholder groups. Participants were recruited from 11 universities (Table 2) that offer programs related to medicine, engineering, or interdisciplinary training. Stratified purposive sampling was used to ensure diversity in geography, university type (e.g., research-intensive and application-oriented), and disciplinary background. This selection strategy aimed to reflect the varied landscape of interdisciplinary education in China and enhance the representativeness of the findings.
The demographic characteristics of students.
| University | No. | Majors | No. |
|---|---|---|---|
| Shanghai Jiao Tong University | 68 | Aerospace engineering | 64 |
| Sichuan Agricultural University | 1 | Clinical medicine | 2 |
| Henan University | 1 | Preventive medicine | 2 |
| China Pharmaceutical University | 1 | Automation | 2 |
| Wenzhou Medical University | 1 | Pharmacy | 1 |
| University of Science and Technology Beijing | 1 | Pharmaceutical preparations | 1 |
| Dalian University of Technology | 1 | Marine pharmacy | 1 |
| Fujian Medical University | 1 | Clinical pharmacy | 1 |
| Central South University | 1 | Nursing | 1 |
| Xiamen University | 1 | Aircraft propulsion engineering | 1 |
| Nanjing University of Science and Technology | 1 | Process equipment and control | 1 |
| Robotics engineering | 1 |
To ensure the quality and clarity of the instruments, the questionnaires underwent expert review and were piloted with a small group of respondents (n=10) from different roles (students, supervisors, and administrators). Feedback from the pilot was used to refine item wording, structure, and response scales. The final versions of the questionnaires demonstrated good content validity and were structured to capture perceptions across five domains, as detailed in the section above.
Analysis of respondents’ demographic characteristics
Of the 100 valid responses, 78 were from students, 14 from supervisors, and 8 from administrators. In the student group, 62 respondents were male (79.4 %) and 16 were female (20.5 %). The participants came from 11 universities, including Shanghai Jiao Tong University, Dalian University of Technology, and Central South University (Table 2), representing 10 schools (e.g., aerospace engineering, medicine, and automation) and 12 majors (e.g., aerospace engineering, clinical medicine, and pharmacy) (Table 2). Academic levels included first year (20.5 %), second year (35.9 %), third year (19.2 %), fourth year (9.0 %), and graduates (15.4 %). Most students had a Bachelor of Engineering (89.7 %), followed by Bachelor of Medicine (5.1 %) and Bachelor of Science (5.1 %).
Among the supervisors, 57.1 % were male and 42.9 % were female. Age groups included ≤30 years (14.3 %), 31–45 years (42.9 %), 46–59 years (35.7 %), and ≥60 years (7.1 %) (Figure 3A). Professional ranks varied, with five senior, three associate senior, three mid-level, and three junior faculty members (Figure 3C). Most supervisors held doctoral degrees (92.9 %), and 7.1 % had a master’s degree. Current research areas included medicine (71.4 %), engineering (21.4 %), and others (7.14 %). In terms of academic background, 78.6 % had obtained degrees in the same field, whereas 14.3 % had degrees in a related field. Supervisors worked predominantly at traditional academic schools (50 %), with 42.9 % of them affiliated with medical institutions.
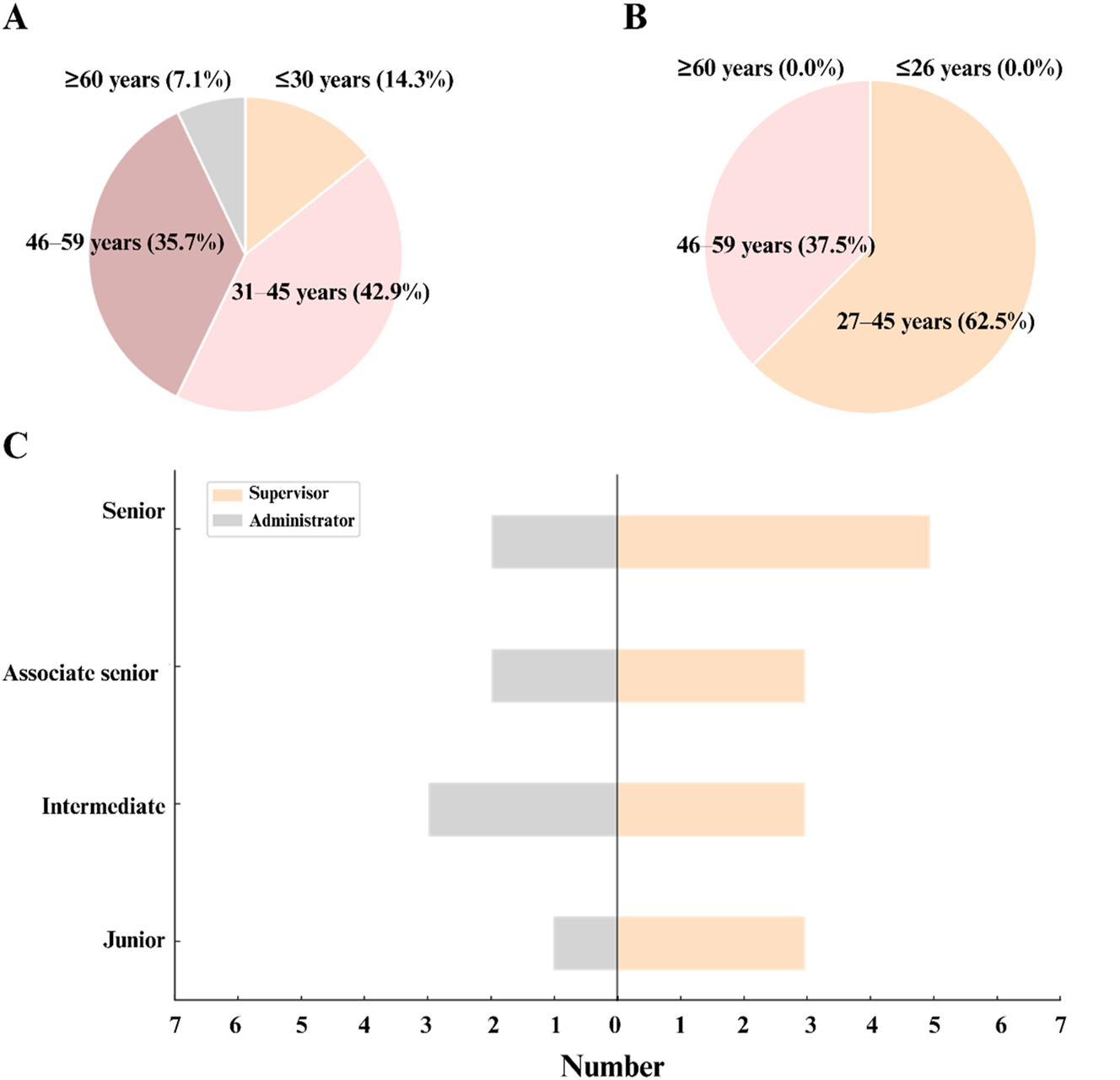
The demographic characteristics of respondents. (A) Age distribution of supervisors; (B) age distribution of administrators; (C) professional rank categories of supervisors and administrators.
Among the administrators, there were five males (62.5 %) and three females (37.5 %). The age distribution was 27–45 years (62.5 %) and 46–59 years (37.5 %) (Figure 3B). The professional ranks included seniors (25 %), associate seniors (25 %), intermediates (37.5 %), and juniors (12.5 %) (Figure 3C). Regarding educational background, 50 % had degrees in the same field, 25 % from related field, and 25 % from unrelated field. The highest degrees were in medicine (37.5 %), science (37.5 %), and literature (25 %).
Evaluation of perceptions on the cultivation of medical-engineering students
Interdisciplinary medical-engineering education is of crucial importance for overcoming complex social challenges. However, the perception of those involved shows that there are gaps between expectations and implementation.
The results of the survey showed that although over 50 % of students were familiar with medical-engineering interdisciplinarity, their understanding was only superficial. Despite this, 58.97 % expressed an interest in interdisciplinary programs and 60.26 % viewed their current education as conducive to development. Notably, about 80 % emphasized the need for interdisciplinary programs (Figure 4A), although only 23.08 % were satisfied with the current efforts (Figure 4B), indicating a disconnection between student aspirations and the practical limitations of institutions.
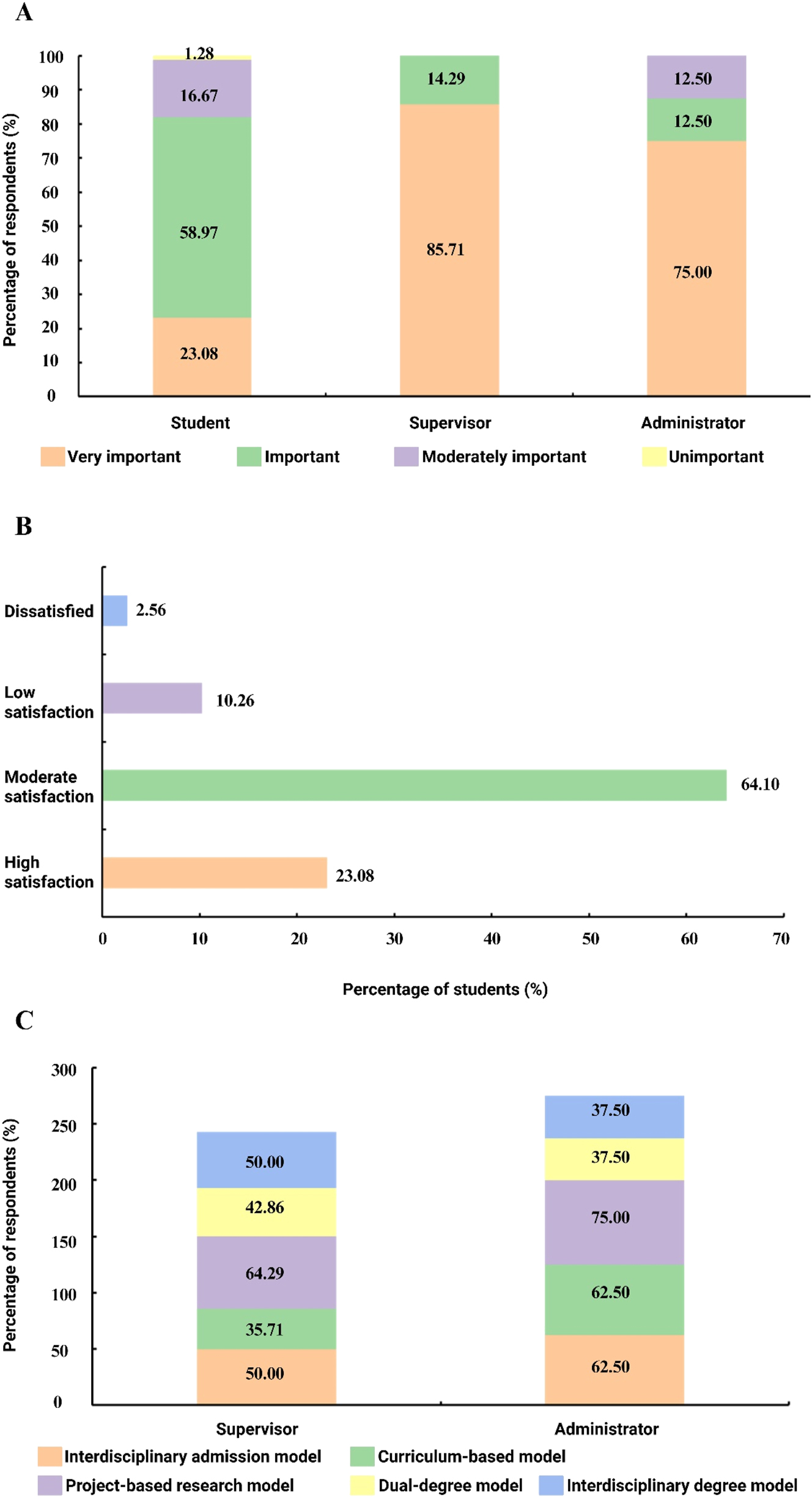
Stakeholders’ perceptions of interdisciplinary medical-engineering education. (A) Proportion of students, supervisors, and administrators who perceive interdisciplinary medical-engineering education as important; (B) students’ satisfaction level with current interdisciplinary training in their programs; (C) preferred interdisciplinary education models among supervisors and administrators. Values indicate the percentage of respondents selecting each option.
More than 70 % supervisors showed interest in interdisciplinary education and unanimously recognized its importance (Figure 4A). However, 50 % rated their current efforts as moderate, and 64.29 % perceived their discipline’s integration as suboptimal. Project-based models, interdisciplinary degrees, and interdisciplinary admissions, which were endorsed by over 90 % of the supervisors, were identified as the most effective strategies (Figure 4C).
Although 87.5 % of the administrators expressed concerns about interdisciplinary education and recognized its importance (Figure 4A), only 25 % felt that current efforts were effective. All respondents emphasized the need for dedicated national modules, endorsing project-based and curriculum-driven models as impactful (Figure 4C).
These findings underscore the growing consensus on the significance of interdisciplinary medical-engineering education while highlighting systemic shortcomings in implementation. Addressing these challenges requires a concerted effort to align stakeholder expectations, optimize institutional frameworks, and create supportive national policies, paving the way for robust and effective educational models in this critical domain.
Evaluation of influential factors affecting the cultivation of medical-engineering students
To comprehensively evaluate the factors that influence the effectiveness of interdisciplinary medical-engineering education, a matrix covering 11 key aspects was used. These include training objectives, curriculum design, scientific research, academic exchange, professional practice, thesis supervision, mentoring, institutional arrangements, assessment and evaluation, disciplinary organization, and resource allocation. Each factor was scored on a scale ranging from 1 (significant obstacle) to 5 (highly favorable), and feedback from students, supervisors, and administrators was analyzed.
For students, the average score of all factors was 3.97, with professional practice and resource allocation scoring the highest at 4.01 (Figure 5A). However, collaborative teaching (19.23 % satisfaction) and teamwork (12.85 % satisfaction) were significant weaknesses. Only 6.41 % of the students frequently participated in interdisciplinary activities and none of them had led research projects. Insufficient facilities and support for interdisciplinary training have also been highlighted. Despite these challenges, 98 % of the students believed that interdisciplinary education improved their skills, research outcomes, and career prospects.
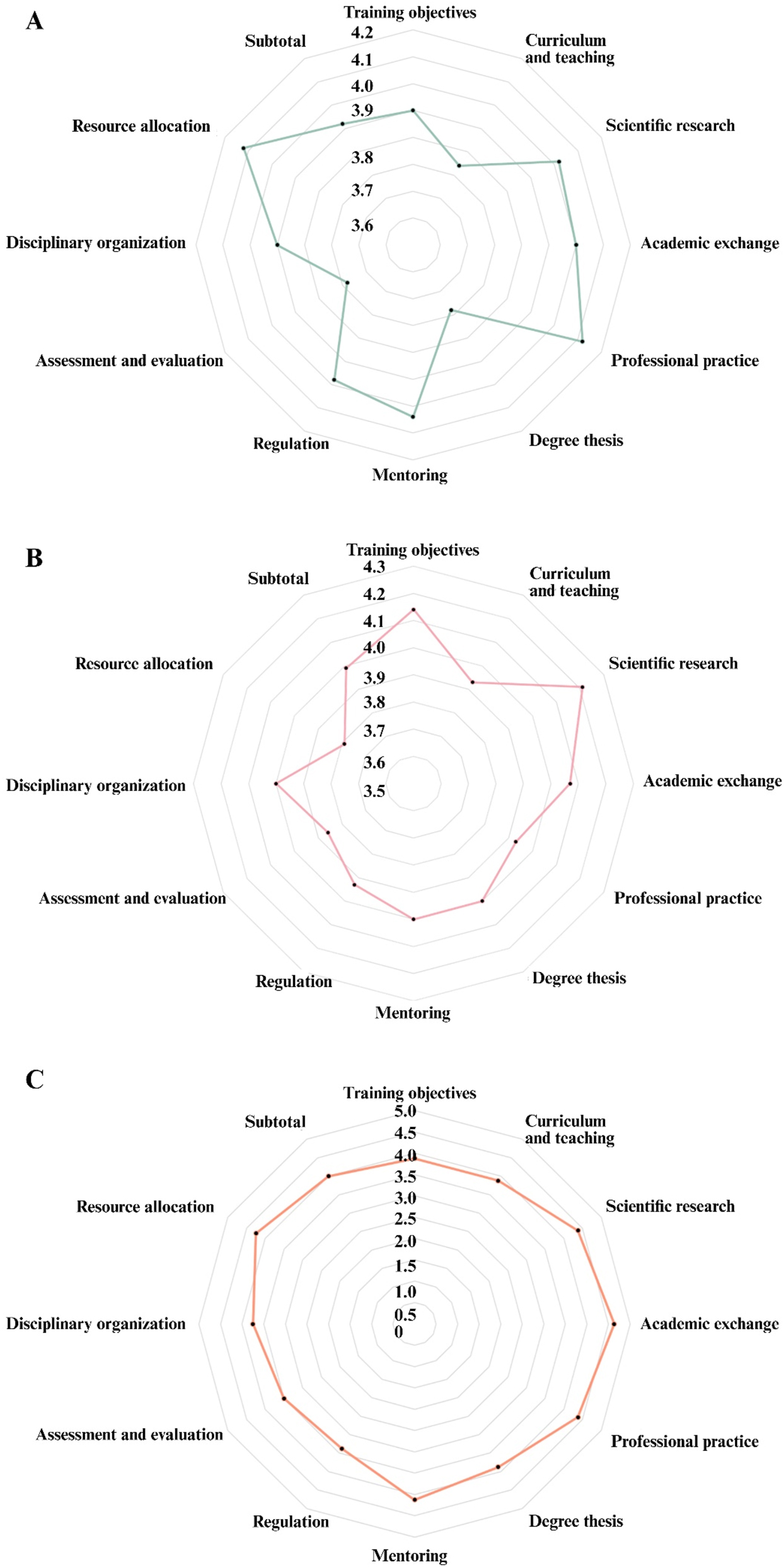
Evaluation of key factors influencing interdisciplinary education by different stakeholder groups. (A) Mean scores reported by students; (B) mean scores reported by supervisors; (C) mean scores reported by administrators. 1=significant obstacle, 5=highly favorable; “Subtotal” represents the average score across all 11 dimensions for each group.
Supervisors provided an average score of 3.99 for all factors, with scientific research and training objectives scoring highest at 4.21 and 4.14, respectively (Figure 5B). Supervisors emphasized promoting innovative thinking, enhancing practical skills, and improving research capabilities as key objectives for medical-engineering education. Most supervisors were in favor of interdisciplinary course offerings and actively encouraged student participation. They identified specific combinations of disciplines, such as Cardiovascular Medicine and Biomedical Engineering, Medical Imaging and Biomedical Engineering, and Pharmacy and Chemical Engineering, as most suitable for interdisciplinary training. An estimated 65 % of supervisors reported involvement in interdisciplinary research, with the majority participating in projects supported by national, provincial, or industrial sponsors. Supervisors also highlighted the dual-supervisor system as a preferred mentoring approach and agreed that interdisciplinary education significantly improves student skills, research outcomes and thesis quality.
The administrators rated the influencing factors at an average of 4.00, with academic exchange (4.63), scientific research (4.38), and professional practice (4.38) receiving the highest ratings (Figure 5C). Despite these ratings, only 25 % of administrators reported that their institutions clearly defined interdisciplinary training objectives. Funding, information-sharing platforms, technical support, and organizational structures were identified as insufficient to support interdisciplinary programs. Administrators recognized key indicators for evaluating progress in interdisciplinary education, including the value and volume of research outcomes, talent cultivation, and number of funded projects. While most institutions still rely on single-supervisor system, staff members consider the dual-supervisor system to be more effective for interdisciplinary education.
These findings indicated critical gaps in collaborative teaching, institutional support, and practical opportunities, emphasizing the need for targeted improvements to enhance interdisciplinary medical-engineering education.
Evaluation of recommendations for advancing the cultivation of medical-engineering students
After analyzing the perceptions of those involved and the influencing factors, specific challenges and recommendations were identified to promote interdisciplinary medical engineering education.
Students pointed out three main challenges: incomplete curriculum systems, insufficient depth of scientific research, and weak professional practice components (Figure 6A). They emphasized the need to strengthen professional practice opportunities, clarify educational objectives, and optimize curriculum design (Figure 6B). Other recommendations include the establishment of specific interdisciplinary programs supported by national policies. These programs would allow students to earn dual degrees in medicine and engineering, qualify for certifications in both fields, and access diverse career opportunities. Students also called for increased investment in cross-disciplinary research, with an emphasis on practical applications and not just publications. Enhanced facilities and resources, including laboratories and training sites, are also strongly recommended to meet the demands of interdisciplinary education.
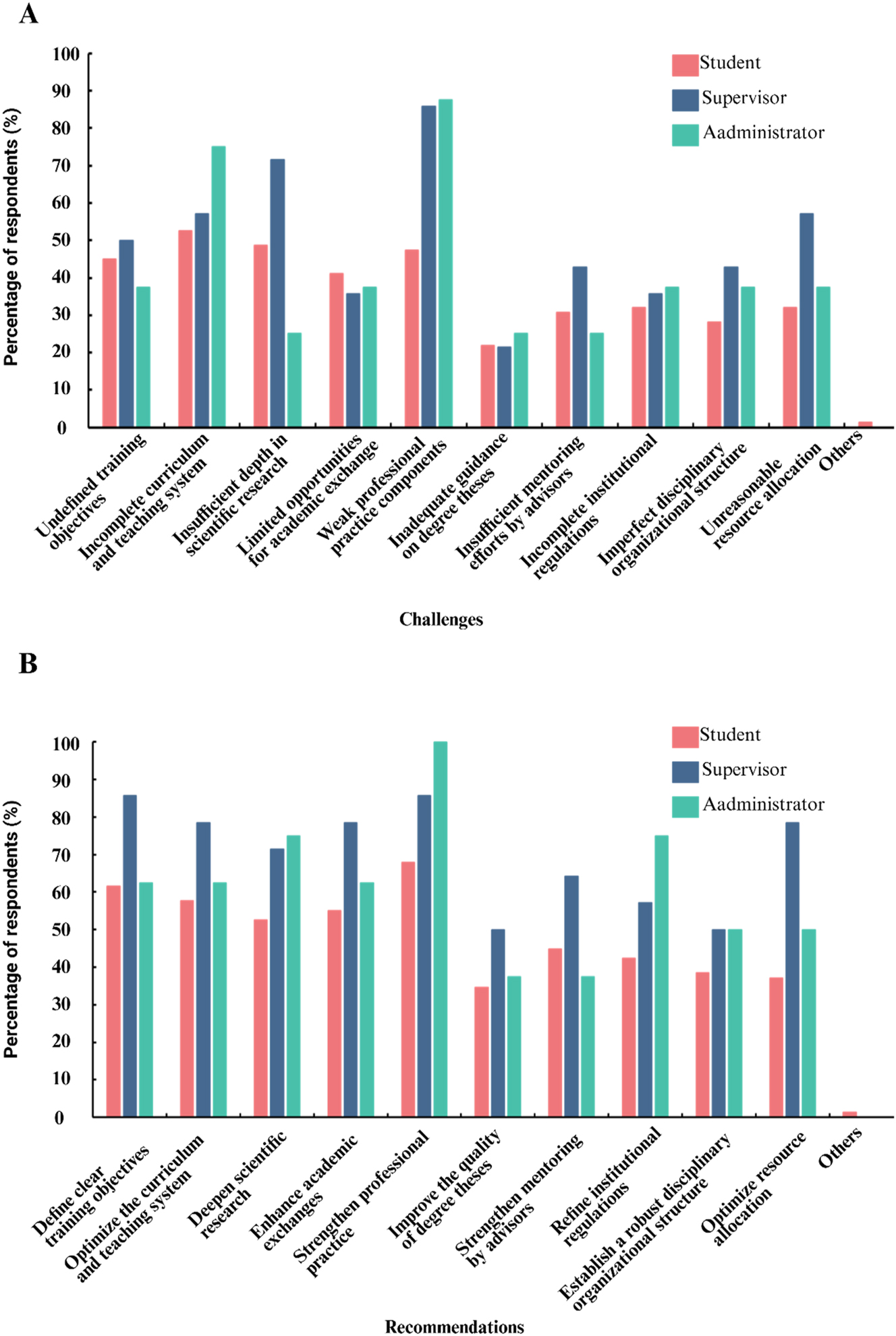
Identified challenges and recommended strategies for improving interdisciplinary medical-engineering education. (A) Percentage of respondents identifying each issue as a major challenge; (B) percentage of respondents endorsing each strategy for improvement. Values indicate the proportion of respondents from each stakeholder group who selected each item.
Supervisors identified similar challenges including weak components of professional practice, insufficient integration of scientific research, and inadequate resource allocation (Figure 6A). They recommended strengthening professional practice, refining education objectives, and improving resource distribution (Figure 6B). Supervisors also suggested fostering stronger collaborations between universities and industries to provide students with practical enterprise-based learning opportunities. In addition, they advocated minimizing administrative interference in interdisciplinary research projects to allow more autonomy and flexibility. The supervisors were unanimous in their support for the inclusion of specific modules for medical-engineering in the national disciplinary catalog, which would formalize the field and promote sustainable development.
Administrators emphasized weak professional practice components, inadequate institutional arrangements, and incomplete curriculum systems as major barriers (Figure 6A). They recommended strengthening professional practice, deepening scientific research integration, and refining institutional policies to better support interdisciplinary education (Figure 6B). Specific suggestions include improving communication between departments, supervisors, and students to address mismatches between needs and expectations. The staff also called for the establishment of platforms to facilitate interdisciplinary collaboration and create mechanisms for effective supervisor selection to improve the quality of mentorship.
These recommendations underline the urgency of addressing structural and operational challenges in interdisciplinary education. By aligning training objectives, optimizing institutional frameworks, and implementing supportive national policies, medical-engineering programs can better meet the demands of modern society and prepare professionals to address complex health challenges.
Theoretical strategies for improvement
Defining specific educational objectives and promoting interdisciplinary synergies
To create an effective interdisciplinary medical-engineering education framework, institutions must define targeted training objectives that are consistent with societal needs and emerging technological advances [9]. These objectives should prioritize the training of professionals capable of integrating medical insights with engineering solutions to address complex healthcare challenges. The focus should be placed on promoting analytical and creative thinking, interdisciplinary collaboration, and technological adaptability. To achieve cross-disciplinary synergies, traditional academic silos must be broken down by fostering collaboration among faculties, co-developing integrated curricula, and implementing strategies that incentivize interdisciplinary teaching and research. These strategies ensure a comprehensive approach to education and innovation.
Building evaluation mechanisms and strengthening quality assurance systems
Robust evaluation mechanisms are essential for assessing the effectiveness and relevance of interdisciplinary education programs. Metrics should be used to evaluate academic achievement, problem-solving skills, research contributions, and industry preparedness [18]. Regular feedback from students, faculty members, and external stakeholders should lead to iterative program improvements. Aligning quality assurance systems with internationally recognized standards, such as ABET accreditation for engineering programs, enhances program credibility and competitiveness. In addition, interdisciplinary steering committees can provide consistent oversight and ensure alignment with institutional goals, fostering accountability and continuous improvement.
Practical strategies for improvement
Innovating teaching approaches and refining practical training models
Innovative teaching methods, tailored to the unique challenges of integrating medicine and engineering, are crucial for effective interdisciplinary education. Active learning approaches, such as design-thinking workshops, problem-based learning, and interdisciplinary hackathons, foster creativity and practical application [10]. Practical training should align with industry and clinics by offering internships in hospitals, biomedical companies, and research laboratories. Incorporating emerging technologies, such as virtual reality simulations and AI-driven data analysis, enriches the learning experience and prepares students for future career requirements [11].
Optimizing resource allocation and establishing sustainable support systems
Efficient resource allocation is critical to creating a supportive environment for interdisciplinary education. Consolidating funding for interdisciplinary projects, establishing shared facilities, and providing access to advanced tools and technologies are essential. Collaborative partnerships with industry, government agencies, and international research institutions can enhance resource availability and expand opportunities for students and faculty members. Universities should develop centralized platforms to facilitate resource sharing, interdisciplinary networking, and cross-sector collaboration. Long-term financial and administrative strategies are necessary to support interdisciplinary initiatives and to cultivate a culture of innovation and integration [19].
Conclusions
This study comprehensively examines interdisciplinary medical-engineering education using a multi-faceted approach that integrates real-world case studies, core competency analyses, and stakeholder interviews. Case studies from leading programs at Tsinghua University, Zhejiang University, and Shanghai Jiao Tong University have illustrated diverse and effective education models. These examples highlight the importance of tailored curricula, international collaboration, and industry partnerships in fostering interdisciplinary talent. Tsinghua University’s dual-track curriculum, Zhejiang University’s focus on innovative medical devices, and Shanghai Jiao Tong University’s accredited program demonstrate the potential of structured practice-oriented education to advance this field.
The analysis of core competencies highlights the critical need for robust interdisciplinary frameworks that integrate multi-disciplinary knowledge, innovative thinking, and collaborative skills. Essential competencies, such as logical reasoning, systemic thinking, and conflict resolution, have emerged as pivotal for addressing complex challenges at the interface of medicine and engineering. These findings underscore the importance of education models that deliver technical expertise and promote holistic professional development.
Stakeholder surveys revealed critical gaps in existing programs, including inadequate resources, incomplete curricula, and limited opportunities for professional practice. Despite these challenges, students, supervisors, and administrators unanimously recognized the importance of interdisciplinary education and proposed actionable strategies for improvement. The key recommendations include increasing investment in interdisciplinary research, strengthening collaboration between industry and academia, and refining institutional framework to better support interdisciplinary initiatives. Although based on diverse stakeholder inputs, the findings may still be influenced by limited institutional coverage and the absence of longitudinal follow-up, which could be addressed in future multi-institutional and time-series studies.
By synthesizing findings from case studies, competency analyses, and stakeholder feedback, this research presents a roadmap to promote interdisciplinary medical-engineering education. Addressing the existing gaps and leveraging proven practices can help institutions cultivate a new generation of professionals with the skills and vision needed to drive innovation in healthcare and engineering. Such efforts are important not only to meet the demands of modern society, but also to promote sustainable progress in global health and technology.
Funding source: National Key Research and Development Program of China
Award Identifier / Grant number: 2022YFC2804300
-
Research ethics: The local Institutional Review Board deemed the study exempt from review.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: This research was funded by the National Key Research and Development Program of China [grant number 2022YFC2804300].
-
Data availability: Not applicable.
References
1. Lehrer, RI. Phagocytes and the “bench-bedside interface”. N Engl J Med 1968;278:1014–6.10.1056/NEJM196805022781811Search in Google Scholar PubMed
2. Sonntag, KC. Implementations of translational medicine. J Transl Med 2005;3:33. https://doi.org/10.1186/1479-5876-3-33.Search in Google Scholar PubMed PubMed Central
3. Hockfield, S. The next innovation revolution. Sci Technol Humanit 2009;323:1147. https://doi.org/10.1126/science.1170834.Search in Google Scholar PubMed
4. Yue, X, Liang, K, Zhao, M, Zhao, J, Zhu, L. Medical-engineering cross-innovation postgraduate talent training. Educ Rev USA 2023;7:372–4. https://doi.org/10.26855/er.2023.03.017.Search in Google Scholar
5. Stanford University. Stanford Bio-X [Online]. https://biox.stanford.edu/ [Accessed 13 Aug 2024].Search in Google Scholar
6. ABET. Accredited programs [Online]. https://amspub.abet.org/aps/category-search?disciplines=9°reeLevels=B&countries=US [Accessed 13 Aug 2024].Search in Google Scholar
7. Shanghai Jiao Tong University. Overview of the school of biomedical engineering. Shanghai Jiao Tong University [Online]. https://en.bme.sjtu.edu.cn/page-resoverview.html [Accessed 13 Aug 2024].Search in Google Scholar
8. China Education Online. Search the major [Online]. https://gaokao.eol.cn/ [Accessed 13 Aug 2024].Search in Google Scholar
9. Albert, M, Rowland, P, Friesen, F, Laberge, S. Interdisciplinarity in medical education research: myth and reality. Adv Health Sci Educ 2020;25:1243–53. https://doi.org/10.1007/s10459-020-09977-8.Search in Google Scholar PubMed PubMed Central
10. Spoelstra, H, Stoyanov, S, Burgoyne, L, Bennett, D, Sweeney, C, Drachsler, H, et al.. Convergence and translation: attitudes to inter-professional learning and teaching of creative problem-solving among medical and engineering students and staff. BMC Med Educ 2014;14:14. https://doi.org/10.1186/1472-6920-14-14.Search in Google Scholar PubMed PubMed Central
11. Oudenampsen, J, van de Pol, M, Blijlevens, N, Das, E. Interdisciplinary education affects student learning: a focus group study. BMC Med Educ 2023;23:1. https://doi.org/10.1186/s12909-023-04103-9.Search in Google Scholar PubMed PubMed Central
12. School of Biomedical Engineering, Tsinghua University. The history of department of biomedical engineering of Tsinghua university [Online]. https://bme.tsinghua.edu.cn/zsjx/jyqk.htm [Accessed 4 Feb 2025].Search in Google Scholar
13. School of Biomedical Engineering, Tsinghua Medicine, Tsinghua University. The training of undergraduates [Online]. https://www.med.tsinghua.edu.cn/info/1063/1860.htm [Accessed 15 Aug 2024].Search in Google Scholar
14. Zhejiang University. About CBEIS [Online]. http://www.cbeis.zju.edu.cn/cbeisen/2018/1118/c23748a902225/page.htm [Accessed 15 Aug 2024].Search in Google Scholar
15. Zhejiang University. The training of biomedical engineering program [Online]. https://ugrs.zju.edu.cn/_upload/article/files/a0/16/e399b033466995faf3a551ea2988/3970dbcb-7819-4a73-b4d3-ddceefa86347.pdf [Accessed 15 Aug 2024].Search in Google Scholar
16. Zhejiang University. Reasons to choose the biomedical engineering program of Zhejiang University [Online]. https://zdzsc.zju.edu.cn/2023/0623/c57922a2775230/page.htm [Accessed 15 Aug 2024].Search in Google Scholar
17. School of Biomedical Engineering, Shanghai Jiao Tong University. Overview of the alumni [Online]. https://bme.sjtu.edu.cn/Web/Content/349 [Accessed 15 Aug 2024].Search in Google Scholar
18. Ferreira, S, Phelps, E, Abolmaali, S, Reed, G, Greilich, P. Opportunities to apply systems engineering to healthcare interprofessional education. Front Med (Lausanne) 2023;10:1241041. https://doi.org/10.3389/fmed.2023.1241041.Search in Google Scholar PubMed PubMed Central
19. Aldriwesh, MG, Alyousif, SM, Alharbi, NS. Undergraduate-level teaching and learning approaches for interprofessional education in the health professions: a systematic review. BMC Med Educ 2022;22:13. https://doi.org/10.1186/s12909-021-03073-0.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


